Documente Academic
Documente Profesional
Documente Cultură
CLP
Încărcat de
Yurika HandayaniDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
CLP
Încărcat de
Yurika HandayaniDrepturi de autor:
Formate disponibile
A Cephalometric Evaluation of Lower Lip in Patients With Unilateral Cleft Lip and Palate
T. UFUK TOYGAR, D.D.S., PH.D. AM, D.D.S., PH.D. M. OKAN AKC A ARMAN, D.D.S., PH.D. AYC
Objective: The aim of this study was to evaluate cephalometrically the lower lip position and area of patients with unilateral cleft lip and palate (UCLP) comparatively with Class I skeletodental normal subjects. Patients: Lateral cephalometric and hand-wrist radiographs obtained from 24 patients with UCLP (mean age 12.86 years), along with 20 normal individuals (mean age 12.33 years) used as a control group, were examined. Design: In addition to standard cephalometric dentofacial variables, lower lip area (superior, middle, inferior) was also measured using a digital planimeter on the lateral cephalograms. Results: The superior and middle part of the lower lip areas were signicantly smaller (p .05) in the UCLP group, compared to the control group. The inferior and total lower lip areas of patients with UCLP were found to be signicantly smaller than controls. The labiomental angle was also smaller (38.79 degrees). Conclusions: The results suggest that the lower lip of patients with UCLP is smaller, retruded, and curved, with a deep labiomental sulcus, compared with normal individuals during puberty. Therefore, practitioners should focus not only on the upper lip of patients with UCLP but also should consider the lower lip as it was found distinct from normal individuals during puberty.
KEY WORDS: lower lip, unilateral cleft lip and palate
To date, studies concerning soft tissue prole in patients with cleft lip and palate (CLP) have mainly focused on normal growth and development or the effects of surgical and/or orthodontic treatment (Wada et al., 1984; Pensler and Mulliken, 1988; Tindlund and Rygh, 1993; Chaisrisookumporn et al., 1995; Smahel and Mullerova, 1995; Chen and So, 1997; Smahel et al., 1999; Heliovaara et al., 2001; Tateishi et al., 2001; Kawakami et al., 2002; Da Silva Filho et al., 2003). The characteristic nonesthetic soft tissue prole of patients with CLP has been commonly attributed to scar tissue of the upper lip. However, clinically, and in the visual assessment of the authors, both upper lip conguration and lower lip form and posture in these patients seem to diverge from normal individuals. Specically, because the upper lip may not function adequately to provide for smooth lip closure, the lower lip may be compelled to compensate for this malfunction. In such cases, the form and posture of the lower lip may appear to be
excessively large, voluminous, and curved, with an intensive labiomental sulcus. Therefore, it was hypothesized that lower lip dimensions and posture in individuals with unilateral cleft lip and palate (UCLP) might be distinct because of the increased functional movements to assure mouth closure, swallowing, and phonation when compared with normals. Consequently, this study was designed to highlight the probable differences in the lower lip of individuals with UCLP and skeletodental Class I normals to develop clinical suggestions for comprehensive treatment to improve facial esthetics and function. MATERIAL
AND
METHODS
Dr. Toygar and Dr. Akc am are Associate Professors, Ankara University, Faculty of Dentistry, Department of Orthodontics, Ankara, Turkey. Dr. Arman is an Orthodontist, Bas kent University, Faculty of Dentistry, Department of Orthodontics, Ankara, Turkey. Submitted August 2003; Accepted December 2003. niversitesi Dis Address correspondence to: Dr. T. Ufuk Toygar, Ankara U Hekimlig i Faku ltesi, Ortodonti Anabilim Dal 06500 Bes evler, Ankara, Turkey. E-mail toygar@dentistry.ankara.edu.tr. 485
Study material was obtained from the orthodontic department of the University of Ankara. Lateral cephalograms, handwrist radiographs, questionnaires, and clinical records of 24 patients with UCLP (9 girls and 15 boys, mean age 12.86 0.85 years) and 20 control individuals with harmonious proles and Class I neutral occlusions (mean age 12.33 0.65 years) were evaluated. The following selection criteria were used: 1. Nonsyndromic Turkish children (determined by questionnaire).
486
Cleft PalateCraniofacial Journal, September 2004, Vol. 41 No. 5
2. Quality cephalograms with easily recognized soft and hard tissues. 3. All patients were in the peak stage (MP3cap) of pubertal growth (Helm et al., 1971) as determined by hand-wrist lms (Greulich and Pyle, 1959). The cephalograms were obtained under standardized conditions (the lm-focus distance was 155 cm and the distance from the midsagittal plane to lm was 12.5 cm). Patients were in centric occlusion and the lips were in relaxed position (Burstone, 1967). To obtain a relaxed lip position, the patients were asked to stroke their lips gently and relax. This position was repeated several times to ensure a relaxed position without any muscular contraction. Cephalometric landmarks and the lower lip region were drawn with a 0.3-mm soft pencil on 0.003-inch frosted acetate. The horizontal reference plane (HR) was constructed 7 degrees to sella-nasion (SN) from the sella point (Looi and Mills, 1986), and the vertical reference plane (VR) was drawn perpendicular to the HR from the sella. These reference planes were used as guidance in measuring the projective distances of the reference landmarks. Cephalometric landmarks and reference planes are shown in Figure 1. Cephalometric landmarks were digitized, and the following linear and angular measurements were taken using the Purpose on request digitizer input output system (PorDios, Copenhagen, Denmark) computer program: Skeletal Measurements SN-point A (SNA; degrees): maxillary prognathism. SN-point B (SNB; degrees): mandibular prognathism. ANB (degrees): sagittal intermaxillary relationship. Cd-Gn: effective mandibular length. ML.SN (degrees): mandibular plane angle in relation to anterior cranial base. N-Me: total anterior facial height. S-Go: posterior facial height. B-HR: vertical position of B point in relation to HR. B-VR: sagittal position of B point in relation to VR. Pg-HR: vertical position of pogonion in relation to HR. Pg-VR: sagittal position of pogonion in relation to VR.
FIGURE 1 Cephalometric points and reference planes used in the study. S sella; N nasion; Cd condylion; Go gonion; A A point; B B point; Pg pogonion; Gn gnathion; U1i incisal edge of maxillary central incisor; U1a apex of maxillary central incisor; L1i incisal edge of mandibular central incisor; L1a apex of mandibular rst central incisor; L6 mesial cusp tip of mandibular rst molar Id infradentale; LI labrale inferior; B soft tissue B point; Pg soft tissue pogonion; SN sella-nasion line; HR horizontal reference plane constructed 7 degrees to SN from S; VR vertical reference plane drawn perpendicular to HR from S; ML mandibular plane constructed between landmarks Go and Gn; OP mandibular occlusal plane passing through mesial cusp tip of lower rst molar (L6) and incisal point of lower incisor (L1i).
Overjet: sagittal distance between incisal edges of the most prominent maxillary and mandibular central incisors. Overbite: vertical distance between incisal edges of the most prominent maxillary and mandibular central incisors. Lower Lip Measurements B-B: thickness of soft tissue B. Pg-Pg: thickness of soft tissue chin (pogonion). LI-L1i: thickness of lower lip. LI-HR: vertical position of lower lip point according to HR. LI-VR: sagittal position of lower lip point according to R. B-HR: vertical position of soft tissue B point according to HR. B-VR: sagittal position of soft tissue B point according to HR. Pg-HR: vertical position of soft tissue pogonion point according to HR. Pg-VR: sagittal position of soft tissue pogonion point according to HR. LI.B. Pg(degrees): labiomental angle.
Dental Measurements U1i-HR: vertical position of incisal edge of maxillary central incisor in relation to HR. U1i-VR: sagittal position of incisal edge of maxillary central incisor in relation to HR. U1.HR (degrees): upper incisor inclination in relation to HR. L1i-HR: vertical position of incisal edge of mandibular central incisor according to HR. L1i-VR: sagittal position of incisal edge of mandibular central incisor according to HR. L1.HR (degrees): lower incisor inclination in relation to HR. U1.L1 (degrees): interincisal angle.
Toygar et al., CEPHALOMETRIC EVALUATION OF LOWER LIP
487
TABLE 1 Mean Values, SEs, and Bonferroni Test Related to Cephalometric Measurements
UCLP (U) X
Sx
Control (C) X
Sx
U-C
Skeletal measurements 78.81 SNA () 74.68 SNB () 4.13 ANB () 108.77 Cd-Gn 37.81 ML.SN () 115.95 N-Me 70.80 S-Go 87.72 B-HR 53.64 B-VR 100.57 Pg-HR 53.25 Pg-VR Dental measurements U1i-HR 69.09 U1i-VR 59.00 U1.HR () 89.72 68.40 L1i-HR 60.52 L1i-VR 121.55 L1.HR () 118.70 U1.L1 () Overjet 1.52 Overbite 0.69
X mean; Sx SEM. * p .05; ** p .01; *** p .001.
1.03 0.72 0.87 1.45 0.97 1.48 1.45 1.35 1.39 1.44 1.47 1.03 1.55 3.43 0.98 1.22 1.57 1.70 0.67 0.41
78.20 76.27 1.94 115.27 36.32 122.68 76.05 92.92 57.22 106.65 57.28 75.50 67.91 110.01 73.07 65.18 122.71 127.28 2.74 2.43
0.67 0.66 0.44 1.20 0.68 1.38 0.84 1.05 1.21 1.28 1.30 0.78 1.01 1.04 0.87 1.02 1.14 1.17 0.23 0.36
** ** ** ** *
FIGURE 2 Lower lip area measurements in the study. The lower lip was divided into three (superior, middle, inferior) parts from incisal edge of mandibular central incisor (L1i), infradentale (Id), B point, and pogonion points. Lines dividing the lower lip area were constructed parallel to the mandibular occlusal plane (OP).
*** *** *** ** *
*** *
The lower lip area was evaluated as superior, middle, inferior, and total areas (Fig. 2). Lower lip area was measured in square centimeters on the lateral cephalograms using a digital planimeter (digital planimeter KP-90, Sokkisha, Kanagawa, Japan). Statistical Analysis Mean values and SEM of all measurements were calculated. Bonferroni tests (Zar, 1999) were performed to evaluate the differences between the UCLP group and the control group. Method Error The coordinates of the cephalometric reference landmarks were recorded using a Genius New Sketch digitizer (Taipei, Taiwan) of 0.125-mm resolution with a double-digitizing process to eliminate digitizing errors. Cephalometric landmarks of a lm are digitized twice simultaneously, and the program (PorDios) automatically rejects the digitizing procedure if the two digitizings do not match. Area measurements were repeated three times by the same investigator (U.T.), and the average values of the three measurements were calculated to eliminate the measurement error. All procedures for measurement calculation (landmark identication, digitization, and area measurements) were repeated on 15 randomly selected cephalograms 1 month after the rst measurements were done by the same investigator. To assess the reliability of measurements, intraclass correlation coefcients were performed, and the reliability of all measurements was found to be within clinically acceptable limits (range 0.98 to 0.99 for area measurements; 0.97 to 0.99 for cephalometric measurements).
RESULTS Skeletal Measurements Measurements indicating the sagittal position and relationship of the jaws (SNA, SNB, ANB, B-VR, Pg-VR) were statistically similar in the UCLP and control groups (Table 1). The effective mandibular length (Cd-Gn) was signicantly smaller in the UCLP group, compared with the control group. The mean values of the mandibular plane angle (ML.SN) were similar in the study groups. Anterior and posterior face heights (N-Me and S-Go) were signicantly smaller in UCLP group when compared with normals. Furthermore, the bony chin (B-HR and Pg-HR) was located more superiorly in the UCLP group. Dental Measurements Upper incisors were retruded in the UCLP group (Table 1), according to angular and linear measurements (U1.HR and U1i-VR), and positioned superiorly (U1i-HR) in comparison with the control group (p .001). Lower incisors (L1i-VR and L1i-HR) were also retruded and superiorly positioned in the UCLP patients when compared with controls. The angular measurement of the lower incisors (L1.HR) and interincisal angle (U1.L1) showed no signicant difference among groups. Negative overjet was observed in the UCLP group (1.52 0.67 mm). Overbite was smaller in the UCLP group when compared with controls (p .05).
488
Cleft PalateCraniofacial Journal, September 2004, Vol. 41 No. 5
TABLE 2 Mean Values, SEs, and Bonferroni Test Related to Lower Lip Measurements
UCLP (U) X
Sx
Control (C) X
Sx
U-C
Lower lip measurements 12.05 B-B 11.21 Pg-Pg 16.24 LI-L1i 76.10 LI-HR 74.42 LI-Vr 85.89 B-HR 65.26 B-VR 100.83 Pg-HR 63.67 Pg-VR 38.79 LI.B.Pg () Lower lip area measurements Superior area 1.28 Middle area 1.07 Inferior area 1.11 Total area 3.46
X mean; Sx SEM. * p .05; ** p .01; *** p .001.
0.44 0.49 0.46 1.12 1.46 1.16 1.42 1.58 1.65 2.83 0.08 0.09 0.10 0.27
12.65 12.46 16.59 83.04 78.16 91.17 69.54 105.33 69.30 46.34 1.59 1.25 1.58 4.42
0.25 0.49 0.29 0.97 1.14 1.06 1.24 1.19 1.53 1.57 0.06 0.08 0.10 0.24
*** **
* * ** **
Lower Lip Measurements (Table 2) Thickness. Lower lip (LI-L1i) and soft tissue chin (B-B and Pg-Pg) thickness were similar in the two groups. Sagittal and vertical position. The sagittal position of the soft tissue chin (B-VR, Pg-VR) was statistically similar in both groups. The soft tissue B point (B-HR) was positioned more superiorly in the UCLP group than in controls, like skeletal B point (p .01). The soft tissue chin (Pg-HR) was also positioned more superiorly, although the difference between the two groups was statistically insignicant. The lower lip was more superior and retrusive (LI-HR and LI-VR) in patients with UCLP when compared with controls. The labiomental angle was smaller in the UCLP groups (38.79 degrees) than in the control group (46.34 degrees), although the difference was statistically insignicant. Lower lip area. The superior, middle, and inferior lower lip areas were signicantly smaller in the UCLP group when compared with normals. Consequently, the total lower lip area was also signicantly smaller in the cleft group when compared with the control group (p .01). DISCUSSION Typical soft tissue morphology of CLP patients appears as a concave prole with a restricted upper lip and a relative protrusion of the lower lip (Pensler and Mulliken, 1988; Tind ztu lund and Rygh, 1993; O rk and Cura, 1996; Stoll et al., 2002). The main problems of facial growth in clefts have been shown to develop in particular during puberty (Smahel and Mullerova, 1995). Therefore, the patients in our study were selected in their pubertal periods. Lateral cephalometric lms have been shown to be reliable in soft tissue prole assessment, although they provide only
two-dimensional information. Other methods of soft tissue evaluation include photographs, video, panel assessments, and three-dimensional scanning methods (Bearn et al., 2002). Because cephalometry provides information about both hard and soft tissue structures, it was convenient for this study, which, in addition to the lower lip, also evaluated upper and lower incisor positions with respect to the basal bone because this may inuence lower lip position. The present study focused mainly on the lower lip; evaluation of measurements related to the upper lip was not included because of decient information related to previous surgical procedures on the cleft lip and palate. The chin (B-HR and Pg-HR) was shown to be more superiorly located in the UCLP group. This may be attributed to a reduction of vertical mandibular growth in compensation for insufcient vertical maxillary growth and to maintenance of the relation with the maxilla. Upper and lower incisors showed retroclination, which is an expected nding and in harmony with the literature (Drahoradova and Mullerova, 1997; Tateishi et al., 2001). The lower lip was shown to be retrusive and superiorly positioned in the UCLP group. This may be attributed to an altered position of the lower incisors in compensation for a negative overjet. The retruded upper incisor position may also inuence lower lip position, as mentioned in the literature (Tateishi et al., 2001). The labiomental angle was smaller in the UCLP group, indicating labiomental folds increase. This most probably occurs to improve functioning and assure mouth closure. Our study found the labiomental angle to be 34.94 degrees in unilateral patients (SEM 2.83), whereas Bearn et al. (2002) reported a labiomental angle of 48.52 degrees in patients with unilateral cleft. However, it should be noted that the standard deviation range of this measurement was very large (SD 12.99) in their study and they mentioned large random error. Contrary to our clinical observations, superior, middle, inferior, and total lower lip areas were found to be smaller in the UCLP group when compared with the control group. This nding was unexpected and in contrast to the hypothesis that patients with UCLP would have voluminous and protrusive lower lips. It also contradicts the ndings of an earlier study by Stoll et al. (2002), which reported more prominent and thicker lower lips in cleft groups. However, it should be noted that the CLP subjects within the current study were all growing individuals (mean age 12.8 0.65 years), whereas Stoll et al. (2002) studied adult patients (between 16 and 29 years). The differences in the two studies may be due to the developmental changes in the pubertal growth stage (Blanchette et al., 1996; Bishara, 2000). At this point, a longitudinal study of patients with CLP seems to be essential from puberty to early adulthood. The results of this study imply that the lower lip in patients with UCLP is signicantly smaller, retruded, and curved, with a deep labiomental sulcus when compared with normal individuals. Previous studies have shown that lower lip curvature increases with LeFort I and rigid external distraction maxillary
Toygar et al., CEPHALOMETRIC EVALUATION OF LOWER LIP
489
advancement surgery (Wen-Ching et al., 2000), whereas signicant thinning of the upper lip occurs in patients with unilateral and bilateral CLP after LeFort I maxillary advancement surgery (Heliovaara et al., 2001). Consequently, skeletal correction alone does not completely correct abnormal lower lip posture, and sagittal jaw relations deteriorate gradually up to adulthood as a result of palate surgery (Smahel and Mullerova, 1995). In light of these ndings, orthodontic as well as surgical planning and post-treatment follow-up evaluation needs to be undertaken with care and precision to monitor the developing soft tissue prole of the patients with CLP. Preventive care may involve muscular training (Altmann Elisa, 1987) to maintain lip closure, surgical restoration of the upper lip for a better function (Markus and Delaire, 1993; Kaiser et al., 1996), and preventing mandibular prognathism (Ishii et al., 1987; Chen and So, 1996; Deguchi et al., 2002). Furthermore, treatment should be undertaken to avoid protrusion of the lower incisors in patients with UCLP so as not to worsen the soft tissue prole and increase the labiomental fold. Finally, long-term research of the lower lip in patients with CLP is essential. CONCLUSIONS This study was unable to justify the hypothesis that individuals with CLP might have a voluminous lower lip in compensation for the scarred upper lip in an effort to assure mouth closure. On the contrary, the lower lip in patients with both bilateral and unilateral CLP was found to be signicantly smaller, retruded, and curved, with a deep labiomental sulcus when compared with normal subjects.
Acknowledgment. We thank Associate Professor Ensar Baspinar (Department of Genetics and Statistics, Faculty of Agriculture, Ankara University) for managing the statistical procedures of this study.
REFERENCES
Altmann Elisa BC. Myofunctional therapy and orthognathic surgery. Int J Orofacial Myology. 1987;13:212. Bearn DR, Sandy JR, Shaw WC. Cephalometric soft tissue prole in unilateral cleft lip and palate patients. Eur J Orthod. 2002;24:277284. Bishara SE. Facial and dental changes in adolescents and their clinical implications. Angle Orthod. 2000;70:471483. Blanchette ME, Nanda RS, Currier GF, Ghosh J, Nanda SK. A longitudinal cephalometric study of the soft tissue prole of short- and long-face syndromes from 7 to 17 years. Am J Orthod Dentofacial Orthop. 1996;109: 116131. Burstone CJ. Lip posture and its signicance in treatment planning. Am J Orthod. 1967;53:262284. Chaisrisookumporn N, Stella JP, Epker BN. Cephalometric prole evaluations in patients with cleft lip and palate. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:137144. Chen K, So LL. Soft tissue prole changes of reverse headgear treatment in
Chinese boys with complete unilateral cleft lip and palate. Angle Orthod. 1997;67:3138. Da Silva Filho OG, Neto JV, Filho LC, De Souza Freitas JA. Inuence of lip repair on craniofacial morphology of patients with complete bilateral cleft lip and palate. Cleft Palate Craniofac J. 2003;40:144153. Deguchi T, Kuroda T, Minoshima Y, Graber TM. Craniofacial features of patients with Class III abnormalities: growth related changes and effects of short-term and long-term chincup therapy. Am J Orthod Dentofacial Orthop. 2002;121:8492. Drahoradova M, Mullerova Z. Deviations in craniofacial morphology in patients with complete unilateral cleft lip and palate evaluated by Jarabaks analysis. Acta Chir Plast. 1997;39:121124. Greulich WW, Pyle SI. Radiographic Atlas of Skeletal Development of the Hand and Wrist. 2nd ed. Stanford, CA: Stanford University Press; 1959. Heliovaara A, Hukki J, Ranta R, Rintala A. Changes in soft tissue thickness after Le Fort I osteotomy in different cleft types. Int J Adult Orthodon Orthognath Surg. 2001;16:207213. Helm S, Siersbeak-Nielsen S, Skieller U, Bjo rk A. Skeletal maturation of the hand in relation to maximum pubertal growth in body height. Tandlaegebladet. 1971;75:12231233. Ishii S, Morita S, Takeuchi Y, Nakamura S. Treatment effect of combined protraction and chincap appliance in severe skeletal Class III cases. Am J Orthod Dentofacial Orthop. 1987;92:304312. Kaiser GL, Jost A, Scheurer T, Thuer U. Lip repair according to the principles of Delaire. What is its signicance? Eur J Pediatr Surg. 1996;6:36. Kawakami M, Yagi T, Takada K. Maxillary expansion and protraction in correction of midface retrusion in a complete unilateral cleft lip and palate patient. Angle Orthod. 2002;72:355361. Looi LK, Mills JRE. The effect of two contrasting forms of orthodontic treatment on the facial prole. Am J Orthod. 1986;89:507517. Markus AF, Delaire J. Functional primary closure of cleft lip. Br J Oral Maxillofac Surg. 1993;31:281291. ztu O rk Y, Cura N. Examination of craniofacial morphology in children with unilateral cleft lip and palate. Cleft Palate Craniofac J. 1996;33:3236. Pensler JM, Mulliken JB. The cleft lip lower-lip deformity. Plast Reconstr Surg. 1988;82:602610. Smahel Z, Hradisky D, Mullerova Z. Multivariate comparison of craniofacial morphology in different types of facial clefts. Acta Chir Plast. 1999;41:59 65. Smahel Z, Mullerova Z. Craniofacial growth and development in unilateral cleft lip and palate: clinical implications (a review). Acta Chir Plast. 1995;37: 2932. Stoll C, Opitz C, Bauer S, Petzold D. The soft-tissue facial prole of patients with unilateral clefts of the lip, alveolus, and palate compared with healthy adults. J Orofac Orthop. 2002;63:179189. Tateishi C, Moriyama K, Takano-Yamamoto T. Dentocraniofacial morphology of 12 Japanese subjects with unilateral cleft lip and palate with a severe class III malocclusion: a cephalometric study at the pretreatment stage of surgical orthodontic treatment. Cleft Palate Craniofac J. 2001;38:597605. Tindlund RS, Rygh P. Soft-tissue prole changes during widening and protraction of the maxilla in patients with cleft lip and palate compared with normal growth and development. Cleft Palate Craniofac J. 1993;30:454468. Wada T, Mizokawa N, Miyazaki T, Ergen G. Maxillary dental arch growth in different types of cleft. Cleft Palate J. 1984;21:180192. Wen-Ching Ko E, Figueroa AA, Polley JW. Soft tissue prole changes after maxillary advancement with distraction osteogenesis by use of a rigid external distraction device: a 1-year follow-up. J Oral Maxillofac Surg. 2000; 58:959969. Zar JH. Biostatistical Analysis. 4th ed. Upper Saddle River, NJ: Prentice Hall Inc.; 1999:663.
S-ar putea să vă placă și
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Arch BarDocument28 paginiArch BarFachrul Latif DentistÎncă nu există evaluări
- Abutment Evaluation in Fixed Partial DentureDocument61 paginiAbutment Evaluation in Fixed Partial DentureBharanija100% (1)
- The Relationship of Endodontic-Periodontic LesionsDocument6 paginiThe Relationship of Endodontic-Periodontic LesionsPam FNÎncă nu există evaluări
- Sequelae of Untreated MalocclusionDocument4 paginiSequelae of Untreated MalocclusionDr-Soheir Saad0% (1)
- Age Estimation Methods in Forensic Odontology: Indian Dental JournalDocument5 paginiAge Estimation Methods in Forensic Odontology: Indian Dental JournalSaatvik AtriÎncă nu există evaluări
- vital pulp therapy الشرقاويDocument3 paginivital pulp therapy الشرقاويahmed muhammadÎncă nu există evaluări
- Vita 1951 1951e Suprinity PC Va en v04 Screen enDocument44 paginiVita 1951 1951e Suprinity PC Va en v04 Screen endvlad1Încă nu există evaluări
- Flexible Denture For Partially Edentulous Arches - A Case ReportDocument4 paginiFlexible Denture For Partially Edentulous Arches - A Case ReportLoly SinagaÎncă nu există evaluări
- Called ASPA - Alumino Silicate Poly Acrylate CementsDocument52 paginiCalled ASPA - Alumino Silicate Poly Acrylate Cementsritesh_patel_pharmaÎncă nu există evaluări
- 6 Elements of Orofacial HarmonyDocument6 pagini6 Elements of Orofacial Harmonyjonathanza14Încă nu există evaluări
- Variants of Talon Cusp (Dens2017Document2 paginiVariants of Talon Cusp (Dens2017Hukjvccx JjyfdxxvbÎncă nu există evaluări
- Tip BackDocument7 paginiTip BackNievecillaNeiraÎncă nu există evaluări
- Management of Discoloured ToothDocument8 paginiManagement of Discoloured ToothAnurtha AnuÎncă nu există evaluări
- Lovejoy1985 PDFDocument10 paginiLovejoy1985 PDFIsolda Alanna RlÎncă nu există evaluări
- Dynamic Occlusion: 130 Manual Functional AnalysisDocument2 paginiDynamic Occlusion: 130 Manual Functional AnalysisdafaÎncă nu există evaluări
- Dental-Gingival Remodeling With BOPT No-Prep VeneersDocument5 paginiDental-Gingival Remodeling With BOPT No-Prep VeneersIvan CarreraÎncă nu există evaluări
- Final Exam. PRS 412 27 / 1 / 2017: Faculty of Dentistry Removable Prosthodontics DepartmentDocument11 paginiFinal Exam. PRS 412 27 / 1 / 2017: Faculty of Dentistry Removable Prosthodontics DepartmentHassan TantawyÎncă nu există evaluări
- Rubber Dam LectureDocument83 paginiRubber Dam LectureVanessa SumardiÎncă nu există evaluări
- Azar Thesis CADE PDFDocument82 paginiAzar Thesis CADE PDFRahma Aulia LestariÎncă nu există evaluări
- Plaque IndexDocument2 paginiPlaque Indexkarthik33% (3)
- Guided Endodontics: Accuracy of A Novel Method For Guided Access Cavity Preparation and Root Canal LocationDocument7 paginiGuided Endodontics: Accuracy of A Novel Method For Guided Access Cavity Preparation and Root Canal LocationCarolina RomeroÎncă nu există evaluări
- Lasers in Prosthodontics The21st CenturyDocument32 paginiLasers in Prosthodontics The21st Centuryaziz2007Încă nu există evaluări
- Surgimax® Dental CatalogueDocument144 paginiSurgimax® Dental Catalogueshahbazahmed750Încă nu există evaluări
- The International Journal of Periodontics & Restorative DentistryDocument10 paginiThe International Journal of Periodontics & Restorative DentistryAna Maria Montoya GomezÎncă nu există evaluări
- Principles of Tooth Preparation: (Lecture or Part-2)Document15 paginiPrinciples of Tooth Preparation: (Lecture or Part-2)arafapoem elmoughrabiÎncă nu există evaluări
- A Multidisciplinary Treatment of A Dental Trauma Trauma DentaraDocument6 paginiA Multidisciplinary Treatment of A Dental Trauma Trauma DentaraStefana NanuÎncă nu există evaluări
- David's ProjectDocument7 paginiDavid's Projectasulliv3Încă nu există evaluări
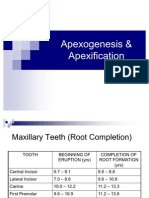
- Apexogenesis & ApexificationDocument35 paginiApexogenesis & ApexificationFaizan Ahmed50% (2)
- Introduction Dental ImplantDocument177 paginiIntroduction Dental ImplantAna Sofia Rodriguez86% (7)
- 3 - Retention of Cores - Pocket DentistryDocument7 pagini3 - Retention of Cores - Pocket Dentistrysalman azizÎncă nu există evaluări