Documente Academic
Documente Profesional
Documente Cultură
Successful Medical Management of Recalcitrant Fusarium Solani Keratitis: Molecular Identification and Susceptibility Patterns.
Încărcat de
Rodrigo BarreraDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Successful Medical Management of Recalcitrant Fusarium Solani Keratitis: Molecular Identification and Susceptibility Patterns.
Încărcat de
Rodrigo BarreraDrepturi de autor:
Formate disponibile
Mycopathologia (2012) 174:233237 DOI 10.
1007/s11046-012-9542-y
Successful Medical Management of Recalcitrant Fusarium solani Keratitis: Molecular Identication and Susceptibility Patterns
Hande Taylan Sekeroglu Elif Erdem Meltem Yagmur Ramazan Gumral Reha Ersoz Macit Ilkit Ibrahim Inan Harbiyeli
Received: 19 October 2011 / Accepted: 1 April 2012 / Published online: 15 April 2012 Springer Science+Business Media B.V. 2012
Abstract Fungal keratitis is a rare but sight-threatening infection of the cornea that may be caused by several fungal pathogens. A delay in diagnosis and inadequate treatment may even lead to loss of the affected eye. Fungal keratitis is often misdiagnosed as bacterial keratitis because isolation and identication of the fungal pathogen is difcult and requires experience, and fungal growth in culture requires time. In this report, a 14-year-old boy with recalcitrant Fusarium solani keratitis, unresponsive to initial therapy, is presented. CLSI M38-A2 in vitro antifungal susceptibility tests demonstrated that only amphotericin B (0.5 lg/ml) had potent activity against F. solani; however, uconazole ([64 lg/ml), itraconazole ([16 lg/ml), voriconazole (8 lg/ml), and posaconazole ([16 lg/ml) had high minimum inhibitory concentrations. In addition, caspofungin ([16 lg/ml) and anidulafungin ([16 lg/ml) exhibited high minimum effective concentrations.
H. Taylan Sekeroglu (&) E. Erdem M. Yagmur R. Ersoz I. I. Harbiyeli Department of Ophthalmology, Faculty of Medicine, C ukurova University, Sarc am 01330, Adana, Turkey e-mail: h_taylan@yahoo.com R. Gumral lhane Military Medical Department of Microbiology, Gu Academy, Ankara, Turkey M. Ilkit Division of Mycology, Department of Microbiology, Faculty of Medicine, C ukurova University, Adana, Turkey
Repeated intrastromal voriconazole injections, topical voriconazole, and caspofungin combined with systemic antifungal agents improved of the corneal lesion with a signicant increase in visual acuity. Intrastromal voriconazole injection may be used as an adjunctive treatment method for recalcitrant fungal keratitis with no prominent complications. The intrastromal route could be an effective route of administration of antifungal agents, especially for F. solani keratitis, as in this case. A combination of various antifungal agents administered by different routes prevented loss of the eye. Keywords Fungal keratitis Fusarium solani Voriconazole Caspofungin Amphotericin B Intrastromal injection
Introduction Fungal keratitis is a sight-threatening corneal infection that can lead to severe visual loss and even loss of the eye, when there is a delay in diagnosis. The most common risk factors associated with fungal keratitis, due to yeasts and yeast-like fungi, are topical steroid use or underlying ocular surface diseases, such as neurotrophic keratitis, trachoma, and peripheral ulcerative keratitis. However, in keratitis due to lamentous fungi, such as the Fusarium and Aspergillus genera, ocular trauma with organic materials is the principal
123
234
Mycopathologia (2012) 174:233237
risk factor [1]. A history of preexisting ocular disorders could predict unresponsiveness to medical treatment [2]. Herein, we present a case of severe Fusarium solani keratitis treated with systemic, topical, and intrastromally injected antifungal agents. The intervention followed the tenets of the Declaration of Helsinki; informed consent was obtained, and the case presentation was approved by the institutional review board.
Case Report A 14-year-old boy presented with redness, stinging, and a burning sensation in his right eye. He provided a history of ocular trauma 4 days prior to presentation; he had no previous ocular disorder and no concurrent systemic disease. A complete ophthalmological examination was performed. Best corrected visual acuity (BCVA) was 1/10 in his right eye (OD) and 10/10 in his left eye (OS). Slit lamp examination revealed conjunctival hyperemia, and central dense corneal inltration covered by a large epithelial defect on the right eye (Fig. 1). On examination, the left eye was normal, and the fundus examination showed no bilateral pathology. The patient was hospitalized with a preliminary diagnosis of fungal keratitis. Corneal scrapings were processed for microbiological investigation and cytological examination. The samples were sent to be investigated by various methods including potassium hydroxide (KOH) wet-mount preparation, Gram smear, and cultures on blood agar, chocolate agar, and
Sabouraud dextrose agar. The cytological examination revealed fungal hyphae, and the following treatment protocol was instituted: administration of topical fortied voriconazole (VOR, 10 mg/ml) every hour and topical natamycin (5 %) ve times daily, combined with 500 mg oral ketoconazole twice a day at 12-h intervals (1 g/day). Hypopyon never developed during follow-up. Nevertheless, at the 1-week visit, the clinical appearance had worsened (Fig. 2), and corneal scrapings and fungal cultures were repeated. The ulcer bed had enlarged, and the deep corneal inltration had expanded to the periphery. Corneal debridement was performed twice to enhance the penetration of the antifungal drugs and to accelerate the healing process. The ulceration continued, and the cornea around the lesion began thinning. Topical amphotericin B eye drops (AMB, 0.15 %) every hour and caspofungin (CAS, 1 %) eye drops every hour were added as an adjunctive treatment to topical VOR. After 4 weeks of topical VOR and 1 week of combination therapy, a decision to administer intrastromal VOR injection was made, because the recovery was unsatisfactory and slower than expected. VOR 50 lg/0.1 ml was injected circumferentially around the fungal abscess in the corneal stroma. The fungal culture revealed F. solani. At the last visit, two months after the start of antifungal therapy, the ulceration had completely resolved, the conjunctival hyperemia had disappeared, and the corneal vascularization had regressed; however, central corneal haze was still present. There was a marked
Fig. 1 The patient had conjunctival hyperemia and dense corneal inltration located paracentrally at presentation (arrow)
Fig. 2 The corneal ulcer had enlarged toward the center of the cornea and deepened at the 1-week visit (arrow). The clinical picture also revealed conjunctival hyperemia and limbal corneal neovascularization
123
Mycopathologia (2012) 174:233237
235
clinical remission of a deep, recalcitrant corneal ulcer. The cornea of the right eye regained almost total transparency after 4 months of antifungal therapy (Fig. 3); the nal visual acuity of the right eye was 3/10. Fungal DNA Isolation, PCR Amplication, Sequencing, and Analysis of the ITS Region DNA isolation and PCR amplication were performed according to the protocol described by Turin et al. [3]. The rDNA regions spanning the internal transcribed spacer (ITS) 1, 5.8S rRNA, and ITS2 regions were amplied using the universal fungal primers ITS1 and ITS4. The amplied DNA products were sequenced in both directions using PCR primers on an ABI PRISM 3130x1 Genetic Analyzer at the DNA sequencing service of Refgen Biotechnologies, Ankara, Turkey. The DNA sequences of the forward and reverse strands were analyzed and aligned with the CAP contig assembly software included in the BioEdit Sequence Alignment Editor 7.0.9.0 software package [4]. The assembled DNA sequences were examined using Basic BLAST (nucleotidenucleotide) software of the National Center for Biotechnology Information web database (http://blast.ncbi.nlm.nih.gov/Blast.cgi). The strain was identied as F. solani according to its morphological characteristics, and the DNA sequence of the strain was 100 % identical to the 537 nucleotides
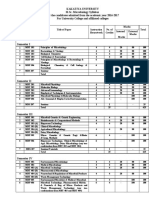
spanning the 18S rRNA gene (partial), ITS1, 5.8S rRNA gene, ITS2, and the 28S rRNA gene (partial) from F. solani ATCC 56480 (GenBank accession no: FJ 345352.1.). The strain has been deposited at the Centraalbureau voor Schimmelcultures (CBS) culture collections, Utrecht, the Netherlands (CBS number: 128989). In vitro Antifungal Susceptibility Testing In vitro antifungal susceptibility testing of the isolate was performed by microbroth dilution according to Clinical and Laboratory Standard Institute (CLSI) document M38-A2 [5], and compared to that of agarbased E test method (AB BIODISK, Solna, Sweden), as described previously [6]. Candida krusei ATCC 6258 and C. parapsilosis ATCC 22019 were used as control strains, as recommended by the CLSI. The isolate was incubated for 48 h at 35 C and then until day 7 at 26 C. The minimum inhibitory concentrations (MICs) of the antifungal drugs were as follows: AMB (0.5 lg/ml), uconazole (FLU, [64 lg/ml), itraconazole (ITR, [16 lg/ml), VOR (8 lg/ml), and posaconazole (POS, [16 lg/ml). The two echinocandins exhibited minimum effective concentrations (MECs) for CAS ([16 lg/ml) and anidulafungin (ANI, [16 lg/ml) (Table 1).
Discussion Members of the Fusarium solani species complex (FSSC) are ubiquitous plant pathogens and saprotrophs that are implicated as the etiological agents of human mycoses, particularly in patients with keratitis [7]. Zhang et al. [7] demonstrated that human and animal pathogens had origins in a broad phylogenetic spectrum, indicating the widespread ability of this diverse species complex to cause infection. However, in daily practice, less than one-third of clinically relevant Fusarium spp. can be accurately identied at the species level using phenotypic data [8]. To resolve this problem, ODonnell et al. [8] constructed a threelocus DNA sequence database to facilitate molecular identication of the 69 Fusarium species associated with human and/or animal mycoses (http://isolate. fusariumdb.org and http://www.cbs.knaw.nl/fusarium). These databases have signicantly enhanced access to internationally accessible culture collections.
Fig. 3 The clinical picture of the right eye at the last visit, showing complete remission of the corneal abscess and regression of the peripheral corneal neovascularization (arrows). The cornea regained almost all of its transparency, and the visual acuity increased. The anterior chamber details were clearly denable
123
236 Table 1 In vitro antifungal susceptibility of F. solani 128989 by the BMD and E test methods Antifungal agents Amphotericin B Fluconazole Itraconazole Voriconazole Posaconazole Caspofungin Anidulafungin BMD [MIC (lg/ml)] 24 h 0.5 [64 [16 8 [16 [16 [16 48 h 0.5 [64 [16 8 [16 [16 [16 E test [MIC (lg/ml)] 24 h 0.064 [256 [32 8 [32 [32 [32 48 h 0.125 [256 [32 24 [32 [32 [32
Mycopathologia (2012) 174:233237
BMD broth microdilution method, MIC minimum inhibitory concentration
Combined with the ndings of our study (F. solani CBS 128989), these data should enhance our understanding of the biological and clinical characteristics of Fusarium spp. These isolates also are available for further research. In an elegant study, Iqbal et al. [6] evaluated the susceptibility patterns of 85 Fusarium spp. recovered from keratitis patients, using the CLSI M38-A2 and E test methods. Notably, members of the FSSC (n = 57) showed higher MICs to triazole drugs (ITR, VOR, and POS) than did other species complexes (n = 28). In addition, the authors found that high MICs to AMB, natamycin, and echinocandins (ANI, CAS, and micafungin) were consistently obtained, with no discrimination based on species or method. Our isolate demonstrated only low MIC for AMB; however, high MICs and MECs were assigned for six antifungals tested by both the BMD and E test methods, as in those of Iqbal et al. [6]. Therefore, their clinical effectiveness in the treatment for F. solani keratitis requires further study. It should be noted that the results of in vitro antifungal susceptibility tests may not necessarily predict clinical response in fungal infections of the eye. Therefore, (1) host factors, (2) ocular penetration of the drug, and (3) drug levels may inuence the outcome of infection [6]. The present case had a severe fungal infection unresponsive to topical VOR, and a combination of antifungal medications was obligatory because of rapid clinical progression. In the literature, topical CAS and VOR are found to be effective for the treatment for fungal keratitis [911]. The main problem in ocular antifungal therapy is the limited penetration of the drugs into the deep layers of the
cornea, and different means to overcome this issue have been tried recently, such as intracameral and intrastromal injections of antifungal agents [1215]. Intrastromal injections of VOR (50 lg/0.1 ml) can provide effective and safe treatment for deep-seated fungal keratitis. Topical natamycin and AMB may not reach adequate levels in the corneal stroma because of weak penetration through intact epithelium, whereas topically administrated VOR provides sufcient therapeutic levels in the aqueous and vitreous [16, 17]. Intrastromal VOR injections also have been used for fungal keratitis [1820]. Notably, topical CAS has been used successfully for the treatment for fungal keratitis refractory to topical VOR [21, 22]. In the present case, inadequate response to topical and systemic antifungal treatment made the intrastromal injection and use of combination therapy mandatory. This procedure probably accelerated the recovery, although susceptibility testing revealed high MICs for VOR and CAS. Patient compliance is another important factor affecting the success of the treatment, because antifungal therapy continues for several weeks and requires patient awareness. Intrastromal VOR injections may be an alternative route of antifungal administration, especially for deep-seated and recalcitrant fungal corneal abscesses. In the present case, the combination of three different antifungals and intrastromal injections of VOR reversed the deteriorating clinical appearance, stopped and even reversed the worsening clinical picture, and saved the patient from corneal perforation and/or from a high-risk therapeutic keratoplasty. Combination antifungal therapy could theoretically provide an increase in antifungal activity, prevent the occurrence of possible resistance, widen the antifungal spectrum, and minimize the potential side effects of the agents by reducing the dosages of individual drugs [23]. Combination therapy may be used against recalcitrant fungal corneal ulcers. Alternative routes of administration for antifungals have been used recently for fungal keratitis to overcome the problem of intraocular penetration. Mahdy et al. [24] reported that the use of topical AMB combined with subconjunctival uconazole was related to a high success rate in the treatment for fungal corneal ulcers, with a very low incidence of side effects, such as local irritation, corneal edema, and conjunctival necrosis, by using subconjunctival
123
Mycopathologia (2012) 174:233237
237 experimental Fusarium solani keratitis. Graefes Arch Clin Exp Ophthalmol. 2008;246:2759. Yoon KC, Jeong IY, Im SK, Chae HJ, Yang SY. Therapeutic effect of intracameral amphotericin B injection in the treatment of fungal keratitis. Cornea. 2007;26:8148. Yilmaz S, Ture M, Maden A. Efcacy of intracameral amphotericin B injection in the management of refractory keratomycosis and endophthalmitis. Cornea. 2007;26: 398402. Kuriakose T, Kothari M, Paul P, Jacob P, Thomas R. Intracameral amphotericin B injection in the management of deep keratomycosis. Cornea. 2002;21:6536. Ghate D, Edelhauser HF. Ocular drug delivery. Expert Opin Drug Deliv. 2006;3:27587. Lalitha P, Shapiro LB, Srinivasan M, et al. Antimicrobial susceptibility of Fusarium, Aspergillus, and other lamentous fungi isolated from keratitis. Arch Ophthalmol. 2007;125:78993. Vemulakonda GA, Hariprasad SM, Mieler WF, et al. Aqueous and vitreous concentrations following topical administration of 1% voriconazole in humans. Arch Ophthalmol. 2008;126:1822. Jain V, Borse N, Shome D, Natarajan S. Recalcitrant fungal tunnel infection treated with intrastromal injection of voriconazole. Int Ophthalmol. 2010;30:7235. Siatiri H, Daneshgar F, Siatiri N, Khodabande A. The effects of intrastromal voriconazole injection and topical voriconazole in the treatment of recalcitrant fusarium keratitis. Cornea. 2011;30:8725. Prakash G, Sharma N, Goel M, Titiyal JS, Vajpayee RB. Evaluation of intrastromal injection of voriconazole as a therapeutic adjunctive for the management of deep recalcitrant fungal keratitis. Am J Ophthalmol. 2008;146:569. M, Duch-Samper A, Cisneros-Lanuza A, Hurtado-Sarrio et al. Successful topical application of caspofungin in the treatment of fungal keratitis refractory to voriconazole. Arch Ophthalmol. 2010;128:9412. Neoh CF, Leung L, Vajpayee RB, Stewart K, Kong DC. Treatment of Alternaria keratitis with intrastromal and topical caspofungin in combination with intrastromal, topical, and oral voriconazole. Ann Pharmacother. 2011;45:e24. Li L, Wang Z, Li R, Luo S, Sun X. In vitro evaluation of combination antifungal activity against Fusarium species isolated from ocular tissues of keratomycosis patients. Am J Ophthalmol. 2008;146:7248. Mahdy RA, Nada WM, Wageh MM, et al. Assessment safety and efcacy of a combination therapy of topical amphotericin B and subconjunctival uconazole for the treatment of fungal keratitis. Cutan Ocul Toxicol. 2010;29: 1937. OBrien TP. Therapy of ocular fungal infections. In: ocular infections: update on therapy. Ophthalmol Clin North Am. 1999;12:3341. Tu EY, McCartney DL, Beatty RF, Springer KL, Levy J, Edward D. Successful treatment of resistant ocular fusariosis with posaconazole (SCH-56592). Am J Ophthalmol. 2007;143:2227. Sponsel WE, Graybill JR, Nevarez HL, Dang D. Ocular and systemic posaconazole (SCH-56592) treatment of invasive Fusarium solani keratitis and endophthalmitis. Br J Ophthalmol. 2002;86:82930.
administration [25]. Topical and systemic POS were found to be effective for ocular fusariosis as well [26, 27]. In conclusion, molecular identication and antifungal susceptibility testing of the isolate may enhance our understanding of the epidemiology and appropriate management of fungal infections of the eye. Intrastromal administration of VOR and a topical combination of antifungal agents can lead to acceptable clinical results for fungal corneal ulcers without any serious complications, but repeated injections may be necessary.
Acknowledgments We gratefully acknowledge Professor G. Sybren de Hoogs (Centraalbureau voor Schimmelcultures, Utrecht, The Netherlands) for his kind cooperation and conrmation of the isolate examined in this study.
12.
13.
14.
15. 16.
17.
18.
References
19. 1. Kalkanci A, Ozdek S. Ocular fungal infections. Curr Eye Res. 2011;36:17989. 2. Ritterband DC, Seedor JA, Shah MK, Koplin RS, McCormick SA. Fungal keratitis at the New York eye and ear inrmary. Cornea. 2006;25:2647. 3. Turin L, Riva F, Galbiati G, Cainelli T. Fast, simple and highly sensitive double-rounded polymerase chain reaction assay to detect medically relevant fungi in dermatological specimens. Eur J Clin Invest. 2000;30:5118. 4. Hall TA. BioEdit: a user-friendly biological sequence alignment editor and analysis program for Windows 95/98 NT. Nucl Acids Symp Ser. 1999;41:958. 5. Clinical and Laboratory Standards Institute (CLSI). Reference method for broth dilution antifungal susceptibility testing of lamentous fungi. Approved Standard M38-A2. 2nd ed. Wayne, PA: CLSI; 2008. 6. Iqbal N, Boey A, Park BJ, Brandt ME. Determination of in vitro susceptibility of ocular Fusarium spp. isolates from keratitis cases and comparison of Clinical and Laboratory Standards Institute M38-A2 and E test methods. Diagn Microbiol Infect Dis. 2008;62:34850. 7. Zhang N, ODonnell K, Sutton DA, et al. Members of the Fusarium solani complex that cause infections in both humans and plants are common in the environment. J Clin Microbiol. 2006;44:218690. 8. ODonnell K, Sutton DA, Rinaldi MG, et al. Internet-accessible DNA sequence database for identifying fusaria from human and animal isolates. J Clin Microbiol. 2010;48:370818. 9. Ozbek Z, Kang S, Sivalingam J, et al. Voriconazole in the management of Alternaria keratitis. Cornea. 2006;25:2424. 10. Bunya VY, Hammersmith KM, Rapuano CJ, Ayres BD, Cohen EJ. Topical and oral voriconazole in the treatment of fungal keratitis. Am J Ophthalmol. 2007;143:1513. rk F, Ku sbeci T, et al. Antifungal efcacy 11. Yavas GF, Oztu of voriconazole, itraconazole and amphotericin B in
20.
21.
22.
23.
24.
25.
26.
27.
123
S-ar putea să vă placă și
- Accuracy of Biometry in Pediatric Cataract Extraction With Primary Intraocular Lens ImplantationDocument8 paginiAccuracy of Biometry in Pediatric Cataract Extraction With Primary Intraocular Lens ImplantationRodrigo BarreraÎncă nu există evaluări
- Novel Anticoagulants: Anesthetic Implications: A Platelet-Ligand-Platelet Matrix With FibrinogenDocument9 paginiNovel Anticoagulants: Anesthetic Implications: A Platelet-Ligand-Platelet Matrix With FibrinogenRodrigo BarreraÎncă nu există evaluări
- Usa 2Document6 paginiUsa 2Rodrigo BarreraÎncă nu există evaluări
- AfricaDocument4 paginiAfricaRodrigo BarreraÎncă nu există evaluări
- Argon Laser Phototherapy in The Treatment of Refractory Fungal Keratitis.Document3 paginiArgon Laser Phototherapy in The Treatment of Refractory Fungal Keratitis.Rodrigo BarreraÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- ID Regulasi Keamanan Hayati Produk Rekayasa PDFDocument18 paginiID Regulasi Keamanan Hayati Produk Rekayasa PDFPangihutan manaluÎncă nu există evaluări
- Ethanol Tolerance in Bacteria PDFDocument2 paginiEthanol Tolerance in Bacteria PDFReneeÎncă nu există evaluări
- 4.electrospinning A Fascinating Fiber Fabrication TechniqueDocument23 pagini4.electrospinning A Fascinating Fiber Fabrication TechniqueSergio Enrique Pichon PosadaÎncă nu există evaluări
- Grade 9 Manufacture of Yogurt Practice QuestionDocument2 paginiGrade 9 Manufacture of Yogurt Practice QuestionListya RahmawatiÎncă nu există evaluări
- 424 MicrobiologyDocument72 pagini424 MicrobiologyVignesh ReddyÎncă nu există evaluări
- Thayer Martin Agar Procedure 08Document1 paginăThayer Martin Agar Procedure 08Hadi FirmansyahÎncă nu există evaluări
- General Biology (Q1)Document3 paginiGeneral Biology (Q1)Regine B. ElculladaÎncă nu există evaluări
- Flow ChartDocument14 paginiFlow ChartHayaFathanaÎncă nu există evaluări
- Pmwasabi cx26Document4 paginiPmwasabi cx26AlleleBiotechÎncă nu există evaluări
- Bioinformatics and Computational Biology SopDocument2 paginiBioinformatics and Computational Biology SopSudev Pradhan0% (1)
- Dna - WorksheetDocument4 paginiDna - WorksheetTajul Azhar BaharudinÎncă nu există evaluări
- BDS Cell StructureDocument66 paginiBDS Cell StructurecheckmateÎncă nu există evaluări
- 4546-LacOperon InstsDocument14 pagini4546-LacOperon InstsScribd_is_GreatÎncă nu există evaluări
- Application Note: Common Cold Chain 483s & Suggested SolutionsDocument5 paginiApplication Note: Common Cold Chain 483s & Suggested SolutionsKapil Dev SaggiÎncă nu există evaluări
- Titlelist CopperDocument163 paginiTitlelist CopperArun KumarÎncă nu există evaluări
- BiopolymerDocument21 paginiBiopolymerParash LoyaÎncă nu există evaluări
- History of GeneticsDocument2 paginiHistory of GeneticsDianne JoyÎncă nu există evaluări
- Ne SkidajDocument186 paginiNe SkidajMaja BumbarÎncă nu există evaluări
- Ass AsDocument1 paginăAss AsMukesh BishtÎncă nu există evaluări
- DOE E.coli FermentationDocument3 paginiDOE E.coli FermentationBabbooÎncă nu există evaluări
- MCQ Biology - Learning Biology Through McqsDocument4 paginiMCQ Biology - Learning Biology Through McqsJunaid ahmad lucky sahaaÎncă nu există evaluări
- Proteomics in Nephrology. Towards Clinical Applications (2008)Document213 paginiProteomics in Nephrology. Towards Clinical Applications (2008)Glogogeanu Cristina AndreeaÎncă nu există evaluări
- BC Review - IDocument11 paginiBC Review - IFlorangÎncă nu există evaluări
- VarII Raspuns BaremeDocument7 paginiVarII Raspuns BaremeIancu Adina FloricicaÎncă nu există evaluări
- Recombinant DNA TechnologyDocument11 paginiRecombinant DNA TechnologyBagya kavirathneÎncă nu există evaluări
- BPS 3101 Mid 1 Study GuideDocument32 paginiBPS 3101 Mid 1 Study GuideSimon HagosÎncă nu există evaluări
- Genetic FingerprintingDocument9 paginiGenetic FingerprintingSumathi SelvarajÎncă nu există evaluări
- Indonesian Soy Sauce (Kecap)Document42 paginiIndonesian Soy Sauce (Kecap)tulus100% (1)
- Sejarah Klasifikasi Antibiotik Dewi - 2017Document58 paginiSejarah Klasifikasi Antibiotik Dewi - 2017dr.syafril SpJPÎncă nu există evaluări
- The Therapeutic Monoclonal Antibody MarketDocument7 paginiThe Therapeutic Monoclonal Antibody MarkethzluyuanÎncă nu există evaluări