Documente Academic
Documente Profesional
Documente Cultură
Topical Honey
Încărcat de
DR. TARIK TORKITitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Topical Honey
Încărcat de
DR. TARIK TORKIDrepturi de autor:
Formate disponibile
OBSERVATIONS FROM PRACTICE
Topical honey Jennifer J. Eddy, MD, and
Mark D. Gideonsen, MD
for diabetic foot ulcers University of Wisconsin
Medical School, Eau Claire
79-year-old man with type 2 dia- of heel osteomyelitis and multiple med-
A betes mellitus developed heel and
forefoot ulcers, for which he
received currently recommended thera-
ical complications, including acute renal
failure from culture-specific antibiotics.
The patient was eventually dis-
py,1–5 including an off-loading orthotic, charged to his home at his request,
systemic antibiotics selected by infectious after consulting with his family and the
disease consultants, and topical therapies
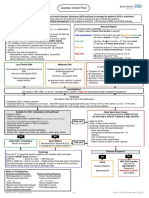
FIGURE 1
directed by a wound care expert. After 3 weeks
After 14 months of care costing more
than $390,000—which was the cost of 5
hospitalizations and 4 surgeries—the
ulcers measured 8 x 5 cm and 3 x 3 cm.
Deep tissue cultures grew methicillin-
resistant Staphylococcus aureus (MRSA),
vancomycin-resistant Enterococcus (VRE),
and Pseudomonas.
During this time the patient lost
2 toes but refused below-the-knee ampu-
tation. He was informed by 2 different
surgical teams that without this surgery
he would likely die. This opinion was
based on the patient’s recurrent episodes Forefoot ulcer after 3 weeks of honey therapy.
FIGURE 2 After 3 months FIGURE 3 After 12 months
CORRESPONDING AUTHOR
Jennifer J. Eddy, MD,
Assistant Professor of Family
Medicine, University of
Wisconsin Medical School,
617 W. Clairemont Avenue,
Eau Claire WI 54703.
Forefoot ulcer after 3 months of honey therapy. Forefoot ulcer after 12 months of honey therapy. E-mail: jjemdg@sbcglobal.net
w w w. j f p o n l i n e . c o m VOL 54, NO 6 / JUNE 2005 533
OBSERVATIONS FROM PRACTICE
FIGURE 4 After 3 weeks ■ Course of treatment
with honey
Once-daily, thick applications of ordi-
nary honey purchased at a supermarket
were smeared on gauze 4x4s and placed
on the wounds, which were then
wrapped. Oral antibiotics and saline
dressings were discontinued, but other-
wise treatment was unchanged. Since the
patient’s family purchased and applied
the honey, the cost of this therapy was
merely that of the dressings. Dressing
changes were painless and the serum glu-
cose remained in excellent control.
Heel ulcer after 3 weeks of honey therapy. Granulation tissue appeared within 2
weeks; in 6 to 12 months the ulcers
FIGURE 5 After 3 months resolved (see FIGURES 1–6 ). Two years
later, the ulcers have not recurred; the
patient ambulates with a walker and
reports improved quality-of-life.
■ Honey as wound treatment
in the medical literature
Honey has been used to treat wounds for
millennia,6 but the medical evidence
supporting its use is limited. While there
are many case reports of honey’s effec-
FAST TRACK tiveness, 7 controlled trials demonstrat-
ing effectiveness for treating burns and
Granulation tissue Heel ulcer after 3 months of honey therapy. wounds are limited by poor quality and
appeared within the use of nonstandard controls,7 while
2 weeks FIGURE 6 After 6 months another trial found minimal benefit when
of treatment with “a very thin smear” was used.8 Concerns
about wound infection from Clostridium
topical honey; spores9 appear unfounded, as no such
in 6 to 12 months complication has been described in more
the ulcers than 500 reports in the literature,10 and
honey has repeatedly been shown to sup-
were resolved press bacterial growth.11
Gamma-irradiated “medical” honey
is available, which has also been selected
for its potent antibacterial properties,
although most of the cases in the medical
literature have used raw honey. A burn-
ing or stinging sensation has been
Heel ulcer after 6 months of honey therapy. described with honey’s topical use.
As rates of diabetes increase, it is
hospital’s ethics committee. He lost a important to identify effective strategies
third toe before consenting to a trial of to reduce amputation rates, both to
topical honey. improve quality of life12 and to decrease
534 VOL 54, NO 6 / JUNE 2005 THE JOURNAL OF FAMILY PRACTICE
Topical honey for diabetic foot ulcers
▲
cost.13 Given honey’s potential for
improved outcomes, cost savings, and
Look for these topics in
decreasing antibiotic use and resistance,
we advocate publicly funded randomized
Applied Evidence
controlled trials to determine its efficacy. Coming soon in JFP
Meanwhile, we encourage others to con-
sider topical honey therapy for patients
with refractory diabetic foot ulcers. ■ ■ When might probiotic supplements
reduce adult lactose intolerance?
ACKNOWLEDGMENTS
The authors gratefully acknowledge Guido Majno, MD, for
his scholarship and generous assistance.
■ Complex regional pain syndrome:
REFERENCES Which treatments show promise?
1. Consensus Development Conference on Diabetic Foot
Wound Care: 7–8 April 1999, Boston, Massachusetts.
Diabetes Care 1999; 22:1354–1360. ■ Screening for prostate cancer:
2. Boulton AJM, Kisner RS, Vileikyte L. Clinical practice.
Neuropathic diabetic foot ulcers. N Engl J Med 2004; When and how often?
351:48–55.
3. Jeffcoate WJ, Harding KG. Diabetic foot ulcers. Lancet
2003; 361:1545–1551. ■ Herbal treatments
4. Watkins PJ. ABC of diabetes: the diabetic foot. BMJ
2003; 326:977–980. for mental illness:
5. Frykberg RG. Diabetic foot ulcers: Pathogenesis and Effectiveness and interaction
management. Am Fam Phys 2002; 66:1655–1662.
with conventional medicines
6. Majno G. The Healing Hand: Man and Wound in the
Ancient World. Cambridge, Mass: Harvard University
Press; 1975.
7. Moore OA, Smith LA, Campbell F, Seers K, McQuay ■ Earning trust and losing it:
HJ, Moore RA. Systematic review of the use of honey
as a wound dressing. BMC Comp & Alt Med 2001;
Adolescents’ views
1(1):2. on trusting physicians
8. Wood B, Rademaker M, Molan PC. Manuka honey, a
low cost ulcer dressing. NZ Med J 1997; 110:107.
9. Postmes T. Honey for wounds, ulcers, and skin graft ■ Would Isaac Newton have made a
preservation (letter). Lancet 1993; 341:756–757.
10. Molan PC. Clinical usage of honey as a wound dress-
good family doc? Embracing
ing: an update. J Wound Care 2004; 13(9):353–356. nonlinearity in family medicine
11. Molan PC. Potential of honey in the treatment of
wounds and burns. Am J Clin Dermatology 2001;
2(1):13–19.
■ Otitis externa: Maximizing relief,
12. Lindholm C. Quality of life in chronic leg ulcer patients.
Acta Derm Venereol 1993; 73:440–443. minimizing complications
13. Ollendorf AD, Kotsanos JG, Wishner WJ, et al.
Potential economic benefits of lower-extremity ampu-
tation prevention strategies in diabetes. Diabetes Care
1998; 21:1240–1245. ■ The liver transplant recipient: What
the family physician needs to know
w w w. j f p o n l i n e . c o m VOL 54, NO 6 / JUNE 2005 535
S-ar putea să vă placă și
- What Is A Diabetic Foot UlcerDocument7 paginiWhat Is A Diabetic Foot UlcerDR. TARIK TORKI100% (1)
- The Average Height and Height Distribution in The U.S. and Other Major Countries in The WorldDocument4 paginiThe Average Height and Height Distribution in The U.S. and Other Major Countries in The WorldDR. TARIK TORKI100% (1)
- Silver Dressings ForDocument2 paginiSilver Dressings ForDR. TARIK TORKIÎncă nu există evaluări
- Foot ClinicDocument12 paginiFoot ClinicDR. TARIK TORKIÎncă nu există evaluări
- Dressing Selection inDocument1 paginăDressing Selection inDR. TARIK TORKI0% (1)
- Diabetic UlcersDocument19 paginiDiabetic UlcersDR. TARIK TORKIÎncă nu există evaluări
- Diabetic Foot InfectionDocument3 paginiDiabetic Foot InfectionDR. TARIK TORKIÎncă nu există evaluări
- Diabetic Foot Ulcers 2Document11 paginiDiabetic Foot Ulcers 2DR. TARIK TORKIÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (120)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Empower 2e B1 Word List GermanDocument102 paginiEmpower 2e B1 Word List GermanOmid SofeÎncă nu există evaluări
- The Tight Tan Slacks of Dezso Ban - The Architecture of Big Arms, Part Three - Todd - AndersonDocument6 paginiThe Tight Tan Slacks of Dezso Ban - The Architecture of Big Arms, Part Three - Todd - AndersonCD KHUTIYALEÎncă nu există evaluări
- APLEY & SOLOMON'S - 5. OsteoarthritisDocument19 paginiAPLEY & SOLOMON'S - 5. OsteoarthritisOngko SetunggalÎncă nu există evaluări
- Css Week 5 Day 2 FinalcoDocument5 paginiCss Week 5 Day 2 FinalcoMGracey BayÎncă nu există evaluări
- Visual Impairment in AdultsDocument25 paginiVisual Impairment in AdultsValentina bustamanteÎncă nu există evaluări
- Eltrac 471: Traction Unit For Lumbar and Cervical TractionDocument14 paginiEltrac 471: Traction Unit For Lumbar and Cervical TractionZvonko ŠuljakÎncă nu există evaluări
- Digital ArticulatorDocument3 paginiDigital Articulatorshabeer hassimÎncă nu există evaluări
- Curriculum Vitae Britney Smith WebDocument5 paginiCurriculum Vitae Britney Smith Webapi-302322721Încă nu există evaluări
- JK Public School Humhama Budgam: Page 1 of 5Document5 paginiJK Public School Humhama Budgam: Page 1 of 5amit ratheeÎncă nu există evaluări
- Audism Unveiled Movie WorksheetDocument3 paginiAudism Unveiled Movie Worksheetapi-265632376Încă nu există evaluări
- Bing Kls 8Document5 paginiBing Kls 8Soni DwinugrohoÎncă nu există evaluări
- Social Media and Its Negative EffectsDocument25 paginiSocial Media and Its Negative EffectsRhowen Jay RamaÎncă nu există evaluări
- Sts Case StudyDocument12 paginiSts Case StudyMark Alvin Agno YangaÎncă nu există evaluări
- On The Psychology of Tiktok Use: A First Glimpse From Empirical FindingsDocument6 paginiOn The Psychology of Tiktok Use: A First Glimpse From Empirical FindingsHuyền PhanÎncă nu există evaluări
- PreviewpdfDocument88 paginiPreviewpdfHeidy Montes Galarza100% (1)
- Urinary Retention NCP GARCIA J.Document2 paginiUrinary Retention NCP GARCIA J.Jimlord GarciaÎncă nu există evaluări
- How To Make DIY Activated Charcoal For Prepping and SurvivalDocument35 paginiHow To Make DIY Activated Charcoal For Prepping and SurvivalIsrael SalubiÎncă nu există evaluări
- 2021 Obesity AlgorithmDocument143 pagini2021 Obesity AlgorithmKhishignemekhMunkhbatÎncă nu există evaluări
- Final SBFR Training PPT 19th April 2022 MoHDocument113 paginiFinal SBFR Training PPT 19th April 2022 MoHDaniel Firomsa100% (6)
- Chest PainDocument5 paginiChest PainAndrei MurariuÎncă nu există evaluări
- Ijerph 19 13877 v2Document10 paginiIjerph 19 13877 v2jigyansa ipsitaÎncă nu există evaluări
- NUR4108 Policy Brief Guideline/Rubric: Course Objectives, Program Outcomes, and AACN EssentialsDocument3 paginiNUR4108 Policy Brief Guideline/Rubric: Course Objectives, Program Outcomes, and AACN EssentialsDanson Githinji EÎncă nu există evaluări
- Final Admission List of Students To Government Health Training CollegesDocument298 paginiFinal Admission List of Students To Government Health Training CollegesThe New VisionÎncă nu există evaluări
- Kidney Cara Jaga Buah PinggangDocument17 paginiKidney Cara Jaga Buah PinggangmachevallieÎncă nu există evaluări
- Preassessment: Setting Up The Classroom For Epp/TleDocument21 paginiPreassessment: Setting Up The Classroom For Epp/TleMhazzy ReyesÎncă nu există evaluări
- Sample Care Coordination AgreementDocument2 paginiSample Care Coordination AgreementKristen LynchÎncă nu există evaluări
- Max BKG 9TH MRNDocument81 paginiMax BKG 9TH MRNPråbhåkår Ð ÅppûÎncă nu există evaluări
- Public Health ConceptsDocument9 paginiPublic Health ConceptsSucheta MitraÎncă nu există evaluări
- Acoustic Singing ContestDocument2 paginiAcoustic Singing ContestIvan SlovskieÎncă nu există evaluări
- Psychological TestingDocument149 paginiPsychological Testingxiejie22590Încă nu există evaluări