Documente Academic
Documente Profesional
Documente Cultură
Nursing Care For Patient With HIV AIDS
Încărcat de
Dessyana PaulusTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Nursing Care For Patient With HIV AIDS
Încărcat de
Dessyana PaulusDrepturi de autor:
Formate disponibile
NURSING CARE FOR MRS.
S WITH HUMAN IMMUNODEFICIENCY VIRUS ACQUIRED IMMUNO DEFICIENCY SYNDROME (HIV AIDS) IN BINTARO INTERNATIONAL HOSPITAL AT LILY ROOM
Written By : 2nd Year Class B 1. Siti Hayuni (1010.711.058)
2. Monanda Chyntia Rossa (1010.711.061) 3. Devi Tias Melati 4. Bani Larasati 5. Eka Wahyuningtyas 6. Mary Danila Paays 7. M. Ganda Gunawan (1010.711.064) (1010.711.068) (1010.711.072) (1010.711.074) (1010.711.086)
THE STUDY PROGRAM OF NURSING HEALTH FACULTY OF JACARTA PEMBANGUNAN NASIONAL VETERAN UNIVERSITY YEAR 2010 / 2011
PREFACE
Thank God we pray for the presence of Almighty God, because His permission is that we can finish this paper. So that the paper entitled "Nursing Care for Mrs. S with Human Immunodeficiency Virus Acquired Immuno Deficiency Syndrome (HIV AIDS) in Bintaro International Hospital at Lily Room", can be resolved. Preparation of this paper is to meet the requirements to get the seminar in English courses. In the preparation of this paper, we as writers, many experience obstacles. But thanks to the guidance and assistance and support from various parties, the end papers can be completed on time. The author realized that the preparation of this paper is both material and its structure is far from perfect. Nevertheless the authors have tried as much as possible, but considering the limited time and capacity available to the author, so that this paper still requires a lot of criticisms and suggestions which if can help improve the quality of the contents of this paper. Finally, with all its limitations, the authors hope that this paper can provide added value and benefits to its friends, as the seminar participants, as well as a lecturer in English.
Jakarta, May 28th 2012 Author
TABLE OF CONTENTS Preface Table of Contents Chapter I Introduction A. The Background B. The Purpose of Writing 1. General 2. Specific C. The Plane of Problem D. The Writing Method E. The Scope of Writing F. The Systematic of Writing Chapter II Basic of Theory A. Definition B. Etiology C. Pathophysiology D. Sign and Symptom E. Diagnosis F. Complication Chapter III Nursing Care Chapter IV Case Report Chapter V Closing A. Conclusion B. Suggestion Reference iii i ii
CHAPTER I INTRODUCTION
A. Background Science that always develops had brought peoples to new round in life more progressive. But, the reality this progress had brought peoples to a free life. As example there are cases about free sex and drugs. If it grows, it means also happen growing risk of spreading infection diseases in this moment be phenomenon in the world. One of infection diseases by free sex and drugs is HIV/AIDS diseases. It still becomes issue of health public on community in the entire world until now (Smeltzer & Bare, 2002). Based on health Department period on July September 2006 as cumulative registered suffering from HIV positive in Indonesia had grown 4.617 peoples and AIDS 6.987 peoples (Indonesian Media, 2006). HIV/AIDS is cant recovery diseases and the medicine is not yet found to make recover it until now. The HIV/AIDS sufferer in Indonesia is mistake, so it can cause pressure of physiology. Especially for the sufferer or family and around environment sufferer. As physiological HIV attack immunology system the sufferer. If add by stress physiologyspiritual to be long according to patient infection by HIV, so will be speed up AIDS, even though grow the number of death. Generally, handling HIV patient needs near similar action. But including clinic fact when patient controls to hospital show more different immunity response (CD4). It shows the other factor that influential, and its maybe stress. Nurse is the important things in stress management, especially to give facility and direct patients constructive coping in order to patient can adaptation at around patient. Besides that, nurse also to give social act support constitute emotional act, information, and material.
B. Writing Goal
1. General To enhance the knowledge and skills of nurses in providing nursing care to patients with HIV AIDS, so that we, as nurse, know the basic concept of HIV/AIDS disease and know how to treat the patient.
2. Specific Conduct assessment in patient with HIV AIDS Promoting the nursing diagnoses in HIV AIDS patients Make a nursing plan (intervention) and evaluation of nursing in patients with HIV AIDS
C. Plane of Problem
1. What is HIV AIDS? 2. How is the mechanism of the disease? 3. How is the nursing care for the patient with HIV AIDS?
D. Writing Methode In this article, we use some methods. There are literature studies; its by read books about this title article, and use method with browsing by internet, which is found any article connected with our discussion.
E. The Scope of Writing The purpose of this paper is making in order to be eligible to get the seminar in English courses. The seminar will take place in the classroom, in the presence of friends as the seminar participants, and the presence of college teacher who act as appraisers, educators, as well as participants of the seminar itself. This paper focus on nursing care to clients with HIV disease AIDS. It contains about how to provide care to clients who suffer from HIV AIDS, nursing actions are appropriate, how to diagnose the presence of the virus causing the disease, as well as nursing care.
F. Writing Systematic This article arrangement consist of four chapters, there are chapter I, chapter II, chapter III, and chapter IV. Chapter I is contain of Introduction, that consist of background, writing goal, plane of problem, writing methode, scope of writing and writing systematic. Chapter II is contain of The Basic Theory about HIV AIDS Disease. Chapter III is contain of The Nursing Care for HIV AIDS Disease. Chapter IV is contain of Closing, that consist suggestion and conclusion.
CHAPTER II BASIC THEORY OF HIV - AIDS
A. Definition Human Immunodeficiency Virus (HIV) is a virus that attack the imun system of a human body and it cant live outside human body. When the imun system is attack, the body will get weak. Any infection will get in easily inside the body and become a disease, especially AIDS (Acquired Immuno Deficiency Syndrome). AIDS is a condition and infection because of the HIV virus in the body and it cause death. 1. Candidiasis : infection around the mouth, throat, and vagina because of spore. 2. CMV virus can cause the eye disease and it also cause death. 3. Herpes around the mouth and sex organs. 4. MAC Bacteria is a bacteria infection that cause fever. 5. PCP is a spore infection that can cause lung.
B. Etiology AIDS is cause by a HIV virus, such as HTL II, LAV, RAV. This virus spread by blood and sexual activity. HIV virus destroy CD4 T cells. That cells are very needed in our body so the immun system can work properly. If the amount of these cells are below 200, so the immunity of our body will gone and AIDS will grow in easily.
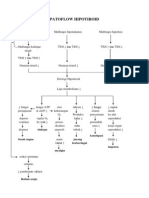
C. Pathophysiology
D. Sign and Symptom
1. Long time fatigue 2. Sweat and high fever in the night without cause. 3. Always coughing and hard to breath. 4. Diarea for 1 month.
5. 10% weight loss in a quick perode.
6. Skin disease and irritation. 7. Spore infection around the mouth and throat. The Diseases State Condition : First State : 1. No sympthom / normal 2. Generally Limfadenopati : swelling limfe in all of the body Second State : 1. 10% of weight losses 2. Lasting Diarrea for more than 1 month 3. Spore infection around the mouth 4. Tubercullosis 5. Acute bacterial infection 6. Skin cancer Major Symptom : 1. Wieght lossing 2. Lasting fever for more than 1 month 3. Chronic diarrea 4. Tubercullosis Minor Symptom : 1. Oropharingeal candidiasis 2. Always cough 3. Fatigue
4. Sweating in the night 5. Appetite losing 6. Skin infection
E. Diagnosis
1. The Quantity Of CD4 Cells Test CD4 cell is a part of the human immun system that protects the body from infection but also it is a target for the HIV virus to attack to. HIV virus controls the CD4 cells, and make them to replicate them self while the HIV virus kills the real CD4 cells. This is why the Quantity of CD4 Test is an important indicator to see wether the immun system is in perfect condition or not. The more quantity of the CD4 cells, the immun system will also get stronger. Usually people with HIV have to regurally check their CD4 cells quantity to make sure its above 200. 2. Viral Load This test is to measure the quantity of HIV in the blood. There are 2 type of this test : Polymerase Chain Reaction (PCR) and Branched DNA (b- number of the undetect is less than 50 in the blood. For the b-DNA, the number of the undetect is 400 in the blood DNA). The purpose of this test is to make sure that the HIV in the blood is detect or not. For the PCR, the. 3. Serologi CMV : to detect herpes 4. Pap Smear : To detect a cancer in female sex organ 5. ELISA : To detect the HIV virus from the antibody 6. Western Blood : Just like ELISA but it more sensitive and specific, so it has the best chance to detect the HIV virus 7. IFA (Indirect Fluorescent Antibody) : Just like ELISA, but it more expensive 8. Complete Blood Test
Complete Blood Test is really important because some of the medicine can cause the red or white blood cells to decrease so it can cause anemia or any other abnormality. This test measure the quantity of white blood cells, hemoglobin, hematocrite and blood platelet.
F. Complication 1. Oral Lesion 2. Acute Ensephalophaty 3. Neurophaty 4. Hepatitis 5. Tuberculosis 6. Blindness 7. Hearing Loss 8. Death
CHAPTER III NURSING CARE IN THEORY
A. Patient Assessment Database Data depend on the organs/body tissues involved, the current viral load, and the specific opportunistic infection (OI) or cancer. 1. ACTIVITY/REST May report : Reduced tolerance for usual activities, progressing to profound fatigue and malaise; weakness, Altered sleep patterns May exhibit : Muscle weakness, wasting of muscle massPhysiological response to activity, e.g., changes in BP, HR, respiration 2. CIRCULATION May report : Slow healing (if anemic); bleeding longer with injury May exhibit : Tachycardia, postural BP changesDecreased peripheral pulse volumePallor or cyanosis; delayed capillary refill 3. EGO INTEGRITY May report : Stress factors related to lifestyle changes, losses, e.g., family support, relationships, finances, andspiritual concerns, Concern about appearance: Alopecia, disfiguring lesions, weight loss, altered distribution of body fat(associated with protease-inhibiting drug therapy), thinning of extremities, wrinkling of skinDenial of diagnosis; feelings of powerlessness, hopelessness, helplessness, worthlessness, guilt, lossof control, depression May exhibit : Denial, anxiety, depression, fear, withdrawal , angry behaviors, dejected body posture, crying, poor eye contactFailure to keep appointments or multiple appointments for similar symptoms
4. ELIMINATION May report : Difficult and painful elimination; rectal pain, itchingIntermittent, persistent, frequent diarrhea with or without abdominal crampingFlank pain, burning on urination May exhibit : Loose-formed to watery stools with or without mucus or blood; frequent, copious diarrheaAbdominal tendernessRectal, perianal lesions or abscessesChanges in urinary output, color, character Urinary, bowel incontinence 5. FOOD / FLUID May report : Anorexia, changes in taste of foods/food intolerance, nausea/vomitingRapid/progressive weight loss, difficulty chewing and swallowing (sore mouth, toungue) dysphagia, retrosternal pain with swallowing, Food intolerance, e.g., diarrhea after dairy products, nausea, early satiation, bloating May exhibit : Hyperactive bowel soundsAbdominal distension (hepatosplenomegaly)Weight loss; thin frame; decreased subcutaneous fat/muscle massPoor skin turgor Lesions of the oral cavity, white patches, discoloration; poor dental/gum health, loss of teethEdema (generalized, dependent) 6. HYGIENE May report : Inability to complete activities of daily living (ADLs) independently May exhibit : Disheveled appearanceDeficits in many or all personal care, self-care activities 7. NEUROSENSORY May report : Fainting spells/dizziness; headache; stiff neck Changes in mental status, loss of mental acuity/ability to solve problems, forgetfulness, poor concentrationImpaired sensation or sense of position and vibrationMuscle weakness, tremors, changes in visual acuity Numbness, tingling in extremities (feet seem to display earliest changes) .Changes in visual acuity; light flashes/floaters; photophobia
May exhibit : Mental status changes ranging from confusion to dementia, forgetfulness, poor concentration, decreased alertness, apathy, psychomotor retardation/slowed responses; paranoid ideation,freefloating anxiety, unrealistic expectationsAbnormal reflexes, decreased muscle strength, ataxic gaitFine/gross motor tremors, focal motor deficits; hemiparesis, seizuresRetinal hemorrhages and exudates (CMV retinitis); blindness
8. PAIN/DISCOMFORT May report : Generalized/localized pain; aching, burning in feetHeadachePleuritic chest pain May exhibit : Swelling of joints, painful nodules, tendernessDecreased range of motion (ROM), gait changes/limpMuscle guarding 9. RESPIRATION May report : Frequent, persistent upper respiratory infections (URIs)Progressive shortness of breath, Cough (ranging from mild to severe); nonproductive/productive of sputum (earliest sign of PCP may be a spasmodic cough on deep breathing)Congestion or tightness in chestHistory of exposure to/prior episode of active TB May exhibit : Tachypnea, respiratory distressChanges in breath sounds/adventitious breath soundsSputum yellow (in sputum-producing pneumonia) 10. SAFETY May report : Exposure to infectious diseases, e.g., TB, STDsHistory of other immune deficiency diseases, e.g., rheumatoid arthritis, cancer History of frequent or multiple blood/blood product transfusions (e.g., hemophilia, major vascular surgery, traumatic incident)History of falls, burns, episodes of fainting, slow-healing woundsSuicidal/homicidal ideation with or without a plan May exhibit : Recurrent fevers; low-grade, intermittent temperature elevations/spikes; night sweatsC h a n g e s i n s k i n i n t e g r i t y , e . g . , cuts, ulcerations, rashes (eczema, exanthems,
p s o r i a s i s ) ; discolorations; changes in size/color of moles; unexplained, easy bruising; multiple injection scars (may be infected)Rectal, perianal lesions or abscesses Nodules, enlarged lymph nodes in two or more areas of the body (e.g., neck, axilla, groin)Decline in general strength, muscle tone, changes in gait 11. SEXUALITY May report : History of high-risk behavior, e.g., having sex with a partner who is HIV-positive, multiple sexual partners, unprotected sexual activity, and anal sexLoss of libido, being too sick for sex; being afraid to engage in any sexual activitiesInconsistent use of condoms Use of birth control pills (enhanced susceptibility to virus in women who are exposed because of increased vaginal dryness/friability) May exhibit : Pregnancy or risk for pregnancy (sexually active); pregnancy resulting in HIV-positive infantGenitalia: Skin manifestations (e.g., herpes, warts); discharge 12. SOCIAL INTERACTION May report : Problems related to diagnosis and treatment, e.g., loss of family/SO, friends, support; fear of tellingothers; fear of rejection/loss of incomeIsolation, loneliness, close friends or sexual partners who have died of or are sick with AIDSQuestioning of ability to remain independent, unable to plan for needs May exhibit : Changes in family/SO interaction patternDisorganized activities, difficulty with goal setting 13. TEACHING / LEARNING May report : Failure to comply with treatment, continued high-risk behavior (e.g., unchanged sexual behavior or injection drug use)Injection drug use/abuse, current smoking, alcohol abuseEvidence of failure to improve from last hospitalization
B. Nursing Diagnosis
1. Imbalanced nutrition: Less than body requirements related tosoreness in mouth o Nursing Diagnosis : Imbalanced Nutrition: Less than Body Requirements related to inability or altered ability to ingest, digest, and/or metabolize nutrientsnausea, vomiting, hyperactive gag reflex, intestinal disturbances, GI tract infections, fatigue; increased metabolic rate and nutritional needs (fever, infection) o Possibly evidenced by : Weight loss, decreased subcutaneous fat and muscle mass (wasting); Lack of interest in food, aversion to eating, altered taste sensation; Abdominal cramping, hyperactive bowel sounds, diarrhea; Sore, inflamed buccal cavity; Abnormal laboratory resultsvitamin, mineral, and protein deficiencies, electrolyte imbalances o Desired Outcomes/Evaluation CriteriaClient Will Nutritional Status Maintain weight or display weight gain toward desired goal. Demonstrate positive nitrogen balance, be free of signs of malnutrition, and display improved energy level. o Nursing intervention with rationale : 1) Assess ability to chew, taste, and swallow. Rationale : Lesions of the mouth, throat, and esophagus are often caused by candidiasis, herpes simplex, hairy leukoplakia, or KS and other cancers; and metallic or other taste changes caused by medications may cause dysphagia, limiting clients ability to ingest food and reducing desire to eat. 2) Auscultate bowel sounds. Rationale : Hypermotility of intestinal tract is common and is associated with vomiting and diarrhea, which may affect choice of diet or route. Note: Lactose intolerance and malabsorption, such as associated with CMV, MAC, or cryptosporidiosis, contribute to diarrhea and may necessitate change in diet or supplemental formula, such as Advera or Resource.
3) Weigh, as indicated. Evaluate weight in terms of premorbid weight. Compare serial weights and anthropometric measurements. Rationale : Indicator of nutritional needs and adequacy of intake. Note: Because of immune suppression, some blood tests normally used for testing nutritional status are not useful. 4) Note drug side effects. Rationale : Prophylactic and therapeutic medications can have side effects affecting nutrition, such as altered taste, nausea, and vomiting associated with ZDV; anorexia, glucose intolerance, or glossitis associated with Bactrim; altered taste and smell, nausea, vomiting, and glucose intolerance associated with Pentam; or elevated lipids and blood sugar secondary to insulin resistance associated with PIs. 5) Plan diet with client and SO, incorporating foods client likes or food from home. Encourage small, frequent meals and snacks of nutritionally dense foods and nonacidic foods and beverages, with choice of foods palatable to client. Encourage highcalorie, nutritious foods, some of which may be considered appetite stimulants. Note time of day when appetite is best, and try to serve a larger meal at that time. Rationale: Including client in planning gives a sense of control of environment and may enhance intake. Fulfilling cravings for desired food may also improve intake. Note: In this population, foods with a higher fat content may be recommended as tolerated to enhance taste and oral intake. 6) Limit food(s) that induce nausea or vomiting or are poorly tolerated by client with mouth sores or dysphagia. Avoid serving very hot liquids and foods. Serve foods that are easy to swallow such as eggs, ice cream, or cooked vegetables. Rationale : Pain in the mouth or fear of irritating oral lesions may cause client to be reluctant to eat. These measures may be helpful in increasing food intake.
7) Schedule medications between meals if tolerated and limit fluid intake with meals, unless fluid has nutritional value. Rationale : Gastric fullness diminishes appetite and food intake. 8) Provide frequent mouth care, observing secretion precautions. Avoid alcohol-containing mouthwashes. Rationale : Reduces discomfort associated with nausea or vomiting, oral lesions, mucosal dryness, and halitosis. A clean mouth may enhance appetite. 9) Review laboratory studies, such as BUN, glucose, liver function studies, electrolytes, protein, and albumin or prealbumin. Rationale : Indicates nutritional status and organ function and identifies replacement needs. Note: Nutritional tests can be altered because of disease processes and response to some medications or therapies. Note: Multiple medications are metabolized by the liver and have potential for synergistic damage. 10) Administer medications, as indicated, for example: Antiemetics, such as prochlorperazine (Compazine) Rationale : Reduces incidence of nausea and vomiting, possibly enhancing oral intake.
2. Risk for Deficient fluid volume related to decreased fluid intakeand diarrhea o Nursing diagnosis : Risk factors may include Excessive lossescopious diarrhea, profuse sweating, vomiting Hypermetabolic state, fever Restricted intakenausea, anorexia, lethargy o Possibly evidenced by : (Not applicable; presence of signs and symptoms establishes an actual diagnosis) o Desired Outcomes/Evaluation CriteriaClient Will Hydration Maintain hydration as evidenced by moist mucous membranes, good skin tugor, stable vital signs, and individually adequate urinary output.
o Nursing intervention with rationale : 1) Monitor vital signs, including central venous pressure (CVP) if available. Note hypotension, including postural changes. Rationale : Indicators of circulating fluid volume. 2) Note temperature elevation and duration of febrile episode. Administer tepid sponge baths, as indicated. Keep clothing and linens dry. Maintain comfortable environmental temperature. Rationale : Fever is one of the most frequent symptoms experienced by clients with HIV infection. Increased metabolic demands and associated excessive diaphoresis result in increased insensible fluid losses and dehydration. 3) Assess skin turgor, mucous membranes, and thirst. Rationale : Indirect indicators of fluid status. 4) Measure urinary output and specific gravity. Measure or estimate amount of diarrheal loss. Note insensible losses. Rationale : Increased specific gravity and decreasing urinary output reflects altered renal perfusion or circulating volume. Note: Monitoring fluid balance is difficult in the presence of excessive GI and insensible losses. 5) Weigh, as indicated. Rationale : Although weight loss may reflect muscle wasting, sudden fluctuations reflect state of hydration. Fluid losses associated with diarrhea can quickly create a crisis and become life threatening. 6) Monitor oral intake and encourage fluids of at least 2,500 mL/day. Rationale : Maintains fluid balance, reduces thirst, and keeps mucous membranes moist. 7) Make fluids easily accessible to client. Encourage use of fluids that are tolerable to client and that replace needed electrolytes, such as Gatorade or broth. Rationale : Enhances intake. Certain fluids such as acidic fruit juices or iced beverages may be too painful to consume because of mouth lesions.
8) Eliminate foods potentiating diarrhea, such as spicy or high-fat foods, nuts, cabbage, and milk products. Provide lactosefree products, such as Resource or Advera. Adjust rate or concentration of enteral feedings, if indicated. Rationale : May help reduce diarrhea. Use of lactose-free products helps control diarrhea in the lactose-intolerant client. 9) Encourage use of live culture yogurt or an over-the-counter (OTC) product such as Lactobacillus acidophilus (Lactaid). Rationale : Antibiotic therapies disrupt normal bowel flora balance, leading to diarrhea. Note: Must be taken 2 hours before or after antibiotic to prevent inactivation of live culture. 10) Administer fluids and electrolytes via feeding tube or intravenously (IV), as appropriate. Rationale : May be necessary to support or augment circulating volume, especially if oral intake is inadequate, or nausea or vomiting persists.
3. Risk for infection related to altered immune protection o Nursing diagnosis : risk for Infection Risk factors may include, Compromised immune system, Failure to recognize or treat infection and/or exercise proper preventive measures, Invasive procedures, environmental exposure (nosocomial) o Possibly evidenced by : (Not applicable; presence of signs and symptoms establishes an actual diagnosis) o Desired Outcomes/Evaluation CriteriaClient Will Infection Severity Achieve timely healing; be free of purulent secretions, drainage, or erythema; and be afebrile. o Nursing intervention with rationale : 1) Examine client for possible source of infection, such as sore throat, sinus pain, burning with urination, localized abdominal pain, burns, open wounds or cellulitis, presence of invasive catheters, or lines.
Rationale : Respiratory tract and urinary tract infection are the most frequent causes of sepsis, followed by abdominal and soft tissue infections. The use of intravascular devices is also a well-known cause of hospital-acquired sepsis. 2) Wash hands with antibacterial soap before and after each care activity, even when gloves are used. Rationale : Hand washing and hand hygiene reduce the risk of crosscontamination. Note: Methicillin-resistant Staphylococcus aureus (MRSA) is most commonly transmitted via direct contact with healthcare workers who fail to wash hands between client contacts. 3) Provide isolation and monitor visitors, as indicated. Rationale : BSI should be used for all infectious clients. Wound and linen isolation and hand washing may be all that is required for draining wounds. Clients with diseases transmitted through air may also need airborne and droplet precautions. Reverse isolation and restriction of visitors may be needed to protect the immunosuppressed client. 4) Encourage or provide frequent position changes, deep-breathing, and coughing exercises. Rationale : Good pulmonary toilet may reduce respiratory compromise. 5) Encourage client to cover mouth and nose with tissue when coughing or sneezing. Place in private room if indicated. Wear mask when providing direct care as appropriate. Rationale: Appropriate behaviors, personal protective equipment, and isolation prevent spread of infection via airborne droplets. 6) Limit use of invasive devices and procedures when possible. Remove lines and devices when infection is present and replace if necessary. Rationale : Reduces number of possible entry sites for opportunistic organisms. 7) Inspect wounds and sites of invasive devices daily, paying particular attention to parenteral nutrition lines. Document signs of local inflammation and infection and changes in character of wound drainage, sputum, or urine.
Rationale : Catheter-related bloodstream infections (CR-BSIs) are increasing where central venous catheters are used in both acute and chronic care settings. Clinical signs, such as local inflammation or phlebitis, may provide a clue to portal of entry, type of primary infecting organism(s), as well as early identification of secondary infections. 8) Investigate reports of pain out of proportion to visible signs. Rationale : Pressurelike pain over area of cellulitis may indicate development of necrotizing fasciitis due to group A beta hemolytic streptococci (GABS), necessitating prompt intervention. 9) Maintain sterile technique when changing dressings, suctioning, and providing site care, such as an invasive line or a urinary catheter. Rationale : Medical asepsis prevents or limits introduction of bacteria and reduces the risk of nosocomial infection. 10) Administer medications, as indicated, for example: Anti-infective agents: broad-spectrum antibiotics, such as imipenem and cilastatin (Primaxin), meropenem (Merrem), ticarcillin and clavulanate (Timentin), piperacillin and tazobactam (Zosyn), clindamycin (Cleocin), vancomycin (Vancocin); aminoglycosides, such as tobramycin (Nebcin), gentamicin (Garamycin); cephalosporins, such as cefepime (Maxipime); fluoroquinolones, such as levofloxacin (Levaquin), ciprofloxin (Cipro); antifungals, such as fluconazole (Diflucan), caspofungin acetate (Cancidas) Rationale : Specific antibiotics are determined by culture and sensitivity tests, but therapy is usually initiated before obtaining results, using broad-spectrum antibiotics and/or based on most likely infecting organisms. Antifungal therapy may be considered in client who has already been treated with antibiotics, who is neutropenic, receiving total parenteral nutrition (TPN), or who has central venous access in place.
4. Anxiety related to diagnosis and fear o Nursing diagnosis : death Anxiety related to confronting reality of potentially terminal disease; anticipating pain, suffering; concern about impact of death on others; life after death; or encounter with a higher power
o Possibly evidenced by : Negative thoughts related to death and dying Feeling powerless over dying Fear of pain or suffering related to dying, or prolonged dying Deep sadness o Desired Outcomes/Evaluation CriteriaClient Will Acceptance: Health Status Verbalize acceptance of reality of situation. Express hopefulness and sense of control. Appear calm and peaceful. Participate in decisions about care and death. o Nursing intervention with rationale : 1) Assure client of confidentiality within limits of situation. Rationale : Provides reassurance and opportunity for client to problemsolve solutions to anticipated situations. 2) Maintain frequent contact with client. Talk with and touch client. Limit use of isolation clothing and masks. Rationale : Provides assurance that client is not alone or rejected; conveys respect for and acceptance of the person, fostering trust. 3) Provide accurate, consistent information regarding prognosis. Avoid arguing about clients perceptions of the situation. Rationale : Can reduce anxiety and enable client to make decisions or choices based on realities. 4) Be alert to signs of denial or depression including withdrawal, or angry, inappropriate remarks. Determine presence of suicidal ideation and assess potential on a scale of 1 to 10. Rationale : Client may use defense mechanism of denial and continue to hope that diagnosis is inaccurate. Feelings of guilt and spiritual distress may cause client to become withdrawn and believe that suicide is a viable alternative. Although client may be too sick to have enough energy to implement thoughts, ideation must be taken seriously and appropriate intervention initiated.
5) Provide open environment in which client feels safe to discuss feelings or to refrain from talking. Rationale : Helps client feel accepted in present condition without feeling judged and promotes sense of dignity and control. 6) Permit expressions of anger, fear, and despair without confrontation. Give information that feelings are normal and are to be appropriately expressed. Rationale : Acceptance of feelings allows client to begin to deal with situation. 7) Recognize and support the stage client and family are at in the grieving process. Rationale : Choice of interventions is dictated by stage of grief and coping behaviors, such as anger, withdrawal, and denial. 8) Explain procedures, providing opportunity for questions and honest answers. Arrange for someone to stay with client during anxietyproducing procedures and consultations. Rationale: Accurate information allows client to deal more effectively with the reality of the situation, thereby reducing anxiety and fear of the unknown. 9) Identify and encourage client interaction with support systems. Encourage verbalization and interaction with family and SO. Rationale : Reduces feelings of isolation. If family support systems are not available, outside sources such as local AIDS task force may be needed. 10) Discuss advance directives and end-of-life desires and needs. Review specific wishes and explain various options clearly. Rationale : May assist client and SO to plan realistically for terminal stages and death. Note: Many individuals do not understand medical terminology or options such as percutaneous enodoscopic gastrostomy (PEG) tube for short- or long-term feeding and pain management techniques.
5. Deficient Knowledge about the HIV disease process
o Nursing diagnosis: Knowledge, deficient [Learning Need] regarding disease, prognosis,current therapies, and self-care needs, May be related to Lack of exposure/recall; information misinterpretation; Cognitive limitation; Unfamiliarity with information resource o Possibly evidenced by : Questions/request for information; statement of misconceptionInaccurate follow-through of instructions, development of preventable complications o Desired Outcomes/Evaluation CriteriaPatient Will : Knowledge: Disease Process (Noc) : Verbalize understanding of condition/disease process and potential complications.Identify relationship of signs/symptoms to the disease process and correlate symptoms with causative factors. Knowledge: Treatment Regimen (NOC) : Verbalize understanding of therapeutic needs.Correctly perform necessary procedures and explain reasons for actions.Initiate necessary lifestyle changes and participate in treatment regimen o Nursing Intervention and Rationale : 1) Review disease process and future expectations. Rationale : Provides knowledge base from which patient can make informed choices. 2) Determine level of independence/dependence and physical condition. Note extent of care and supportavailable from family/SO and need for other caregivers. Rationale : Helps plan amount of care and symptom managementrequired and need for additional resources 3) Review modes of transmission of disease, especially if newly diagnosed. Rationale : Corrects myths and misconceptions; promotes safety for patient/others. 4) Instruct patient and caregivers concerning infectioncontrol, e.g.: using good handwashing techniques for everyone (patient, family, caregivers); using gloves whenhandling bedpans, dressings/soiled linens; wearing mask if patient has productive cough; placing soiled/wet linensin plastic
bag and separating from family laundry,washing with detergent and hot water; cleaning surfaceswith bleach/water solution of 1:10 ratio, disinfecting toilet bowl/bedpan with full-strength bleach; preparing patientsfood in clean area; washing dishes/utensils in hot soapywater (can be washed with the family dishes). Rationale : Accurate epidemiological data areimportant in targeting prevention interventions.Reduces risk of transmission of diseases; promoteswellness in presence of reduced ability of immune systemto control level of flora. 5) Stress necessity of daily skin care, including inspectingskin folds, pressure points, and perineum, and of providing adequate cleansing and protective measures,e.g., ointments, padding. Rationale : Healthy skin provides barrier to infection. Measures to prevent skin disruption and associated complications arecritical 6) Ascertain that patient/SO can perform necessary oral anddental care. Review procedures as indicated. Encourageregular dental care. Rationale : The oral mucosa can quickly exhibit severe, progressivecomplications. Studies indicate that 65% of AIDS patientshave some oral symptoms. Therefore, prevention andearly intervention are critical. 7) Review dietary needs (high-protein and high-calorie) andways to improve intake when anorexia, diarrhea,weakness, depression interfere with intake. Rationale : Promotes adequate nutrition necessary for healing andsupport of immune system; enhances feeling of well- being. 8) Discuss medication regimen, interactions, and sideeffects. Rationale : Enhances cooperation with/increases probability of success with therapeutic regimen. (Refer to CP: The HIV-Positive Patient, ND: Therapeutic Regimen : [Individual] / Families, ineffective management.) 9) Provide information about symptom management thatcomplements medical regimen; e.g., with intermittentdiarrhea, take diphenoxylate (Lomotil) before going tosocial event.
Rationale : Provides patient with increased sense of control, reducesrisk of enbarrassment, and promotes comfort. 10) Stress importance of adequate rest. Rationale :Helps manage fatigue; enhances coping abilities andenergy level. 11) Encourage activity/exercise at level that patient cantolerate. Rationale : Stimulates release of endorphins in the brain, enhancingsense of well-being. 12) Stress necessity of continued healthcare and follow-up. Rationale : Provides opportunity for altering regimen to meetindividual/changing needs. 13) Recommend cessation of smoking. Rationale :Smoking increases risk of respiratory infections and canfurther impair immune system. 14) Identify signs/symptoms requiring medical evaluation,e.g., persistent fever/night sweats, swollen glands,continued weight loss, diarrhea, skin blotches/lesions,headache, chest pain/dyspnea. Rationale : Early recognition of developing complications and timelyinterventions may prevent progression to life-threateningsituation. 15) Identify community resources, e.g., hospice/residentialcare centers, visiting nurse, home care services, Meals onWheels, peer group support. Rationale : Facilitatestransfer fromacute caresetting for recovery / independence or end-of-life care.
CHAPTER V CLOSING
A. Conclusion In doctrine client with HIV/AIDS, often found fall immunity that often followed by grow of risk and degree opportunistic infection and ferocity disease. Fall immunity influence by some factors. They should have attention factor is physicosocial stressor. The goal nursing care of infection HIV (PHIV) patient is for change performer when stay in care nursing and to grow immunity responses PHIV by full physic necessity, physiologic, social, and spiritual is done by nurse in order to fall stressor. Physic aspect PHIV is fulfilling physic necessity as cause from sign and symptom happened. Care nursing aspect physic is containing: Universal precautions, medical treatment secondary infection and giving ARV (Antiretroviral), giving nutrition, activity and take a rest. Social support is very necessity especially for PHIV the condition has very dangerous. Individual include in giving social support include couple (husband/wife), parents, son/daughter, family, friend, medic team, superior, and counselor. Nursing care in spiritual aspect is press with receiving patient concerning the sickness (Ronaldson, 2000), so PHIV will receive honestly the sickness and get the wisdom.
B. Suggetion Application universal precautanius by nurse, family, and patient are very important. This thing is show to prevent infectious virus HIV. To do the plain action with HIV/AIDS patient, we should see the problems are felling by patient from result of doctrine our care nursing.
REFERENCE
Martini F. Fundamentals of Anatomy and Physiology. 7th ed. USA: Pearson Education Inc; 2006. p. 153-78. Nursalam,M.nurs (HONS) dan Ninuk Dian Murniawati.2008, Asuhan keperawatan pada pasien terinfeksi HIV AIDS Jakarta, penerbit salemba medika. Murni, Suzana dkk , 2009. Hidup dengan HIV AIDS Jakarta : yayasan spritia mandal, bibhat K dkk 2006. Penyakit terinfeksi . jakarta, penerbit Erlanga. http://id.shvoong.com/exact-sciences/biology/2099099-apa-itu-cytomegaloviruscmv/#ixzz1foXJAHVS http://asuhan-keperawatan.blogspot.com/2006/05/aids.htm http://asuhankeperawatans.blogspot.com/2011/01/asuhan-keperawatan-klien-hivaids.html http://asuhankeperawatans.blogspot.com/2011/01/asuhan-keperawatan-klien-hivaids.html http://mirahermanpsikumj2010.blogspot.com/2011/04/asuhan-keperawatan-pada-pasiendengan_22.html http://biologiendar.blogspot.com/2010/02/sistem-kekebalan-tubuh.html http://4lifeku.blogdetik.com/2011/02/21/komponen-sistem-imun/ http://hmkuliah.wordpress.com/2011/09/10/imunologi-dasar/ http://echavthree.blogspot.com/2011/06/basic-concept-in-immune-system-humoral.html http://www.majalah-farmacia.com/rubrik/one_news_print.asp?IDNews=985
S-ar putea să vă placă și
- Management of Tuberculosis: A guide for clinicians (eBook edition)De la EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)Încă nu există evaluări
- Sickle Cell Anemia 2007Document25 paginiSickle Cell Anemia 2007R-o-N-n-e-lÎncă nu există evaluări
- Herpes Simplex VirusDocument39 paginiHerpes Simplex VirusWenalyn Grace Abella LlavanÎncă nu există evaluări
- Abdominal Case Study CompiledDocument392 paginiAbdominal Case Study CompiledIshak IzharÎncă nu există evaluări
- Gerontologic Health Promotion ActivityDocument3 paginiGerontologic Health Promotion ActivityCorinne50% (2)
- Acute BronchitisDocument25 paginiAcute BronchitisCherish Panopio RoadillaÎncă nu există evaluări
- Kap StudyDocument21 paginiKap StudyFaraz SiddiquiÎncă nu există evaluări
- Case Study Burn Injury - 11Document15 paginiCase Study Burn Injury - 11Evelyn MedinaÎncă nu există evaluări
- Kristia Carpio Pulmonary TuberculosisDocument31 paginiKristia Carpio Pulmonary TuberculosiskisÎncă nu există evaluări
- Laryngitis Awareness and TreatmentDocument40 paginiLaryngitis Awareness and TreatmentMikhail Guidicelli100% (1)
- Case Study of PNEUMONIADocument12 paginiCase Study of PNEUMONIAAriaÎncă nu există evaluări
- Case Summary of Patient With Chronic Obstructive PulmonaryDocument27 paginiCase Summary of Patient With Chronic Obstructive PulmonaryUzair Muhd0% (1)
- Assessment 2 - Nursing Case Study - 2019Document2 paginiAssessment 2 - Nursing Case Study - 2019Chinney ArceÎncă nu există evaluări
- Laryngitis and Upper Airway ObstructionDocument9 paginiLaryngitis and Upper Airway Obstructionjonna casumpangÎncă nu există evaluări
- Nursing Care Plan for ChickenpoxDocument2 paginiNursing Care Plan for ChickenpoxAkeroÎncă nu există evaluări
- Case Presentation on Acid Peptic Disease and Anxiety DisorderDocument23 paginiCase Presentation on Acid Peptic Disease and Anxiety DisorderUmme habeebaÎncă nu există evaluări
- NCLFNP - Mr. Robert McClelland CaseDocument4 paginiNCLFNP - Mr. Robert McClelland CaseAiresh Lamao50% (2)
- Fundamentals of NursingDocument268 paginiFundamentals of Nursinguhta100% (1)
- HIV and Pregnancy Prevention of Mother-To-Child TransmissionDocument29 paginiHIV and Pregnancy Prevention of Mother-To-Child TransmissionSusan HepziÎncă nu există evaluări
- Aids Hiv AssignmentDocument21 paginiAids Hiv AssignmentGeetha Sarika100% (3)
- Case Study On Ibd17Document2 paginiCase Study On Ibd17api-381128376Încă nu există evaluări
- Acute BronchitisDocument38 paginiAcute BronchitisNikko MelencionÎncă nu există evaluări
- Role of An Occupational Health NurseDocument48 paginiRole of An Occupational Health Nursejaypee24Încă nu există evaluări
- Nephrotic Syndrome (Nephrosis)Document9 paginiNephrotic Syndrome (Nephrosis)Madhusmita SatapathyÎncă nu există evaluări
- Hiv AidsDocument37 paginiHiv AidsAgung PriasmoyoÎncă nu există evaluări
- Lung AbscessDocument41 paginiLung AbscessokaciaÎncă nu există evaluări
- Psychiatric Mental Health Case StudyDocument11 paginiPsychiatric Mental Health Case Studyapi-402701741100% (1)
- HIVDocument82 paginiHIVXuehua Guan100% (1)
- Status Asthmaticus CASE PRESDocument18 paginiStatus Asthmaticus CASE PRESNessa Layos MorilloÎncă nu există evaluări
- Post Op Case Studies: Malignant HyperthermiaDocument19 paginiPost Op Case Studies: Malignant HyperthermiaRenie SerranoÎncă nu există evaluări
- Case PresentationDocument89 paginiCase PresentationBakerbrown CrumbsworthÎncă nu există evaluări
- Addisons DiseaseDocument1 paginăAddisons DiseaseAndreia Palade100% (1)
- Respiratory System DisordersDocument9 paginiRespiratory System Disordersasop06Încă nu există evaluări
- Chapter Q 045Document1 paginăChapter Q 045sammm996Încă nu există evaluări
- Recurrent PAF Case StudyDocument3 paginiRecurrent PAF Case StudyDanae Kristina Natasia BangkanÎncă nu există evaluări
- Case Study (1166)Document17 paginiCase Study (1166)ساره معنÎncă nu există evaluări
- Peptic Ulcer Disease Causes, Symptoms, Diagnosis (40Document5 paginiPeptic Ulcer Disease Causes, Symptoms, Diagnosis (40George Mikhail Labuguen100% (1)
- Team Nursing StaffingDocument25 paginiTeam Nursing StaffingKatherine 'Chingboo' Leonico LaudÎncă nu există evaluări
- Chronic Bronchitis GuideDocument5 paginiChronic Bronchitis GuideJemalyn M. Saludar100% (2)
- Bullying Seminar RevisedDocument56 paginiBullying Seminar RevisedJenny Wong KainÎncă nu există evaluări
- Dengue Fever Case StudyDocument5 paginiDengue Fever Case StudyNadine PollescasÎncă nu există evaluări
- Case Study 2Document6 paginiCase Study 2JosephCernigliaÎncă nu există evaluări
- New Nursing Diagnoses 2012-2014Document11 paginiNew Nursing Diagnoses 2012-2014CarmenNoemiSantos100% (1)
- CASE STUDY (Role - in Infectious Diarrhea and Oral Thrush)Document29 paginiCASE STUDY (Role - in Infectious Diarrhea and Oral Thrush)maeya18613550% (2)
- Nursing Care Plan EportfolioDocument14 paginiNursing Care Plan Eportfolioapi-279212367Încă nu există evaluări
- MedSurg Nursing Case Study: Care Plans for Liver Disease PtDocument1 paginăMedSurg Nursing Case Study: Care Plans for Liver Disease PtShahab SaqibÎncă nu există evaluări
- NCP TetanusDocument2 paginiNCP TetanusSugar Capule - Manuel0% (1)
- Dengue Breakbone Fever Case StudyDocument53 paginiDengue Breakbone Fever Case StudyLeilani Rodriguez AmpoÎncă nu există evaluări
- A Client Care StudyDocument27 paginiA Client Care StudyTestimony WilliamÎncă nu există evaluări
- Hiv Case StudyDocument2 paginiHiv Case Studyapi-485814878Încă nu există evaluări
- Pneumonia Case PresentationDocument24 paginiPneumonia Case Presentationudanics100% (1)
- Abdominal Assessment VideoDocument4 paginiAbdominal Assessment VideoAmber Nicole HubbardÎncă nu există evaluări
- Stab Wound Case StudyDocument33 paginiStab Wound Case StudyAdrian MallarÎncă nu există evaluări
- Propranolol 1 PresentationDocument17 paginiPropranolol 1 Presentationapi-284092317100% (1)
- Nursing Care Plan FinalDocument16 paginiNursing Care Plan FinalErickson OcialÎncă nu există evaluări
- CEPHALOCAUDAL ASSESSMENT Krissha-1Document4 paginiCEPHALOCAUDAL ASSESSMENT Krissha-1Vhince Norben PiscoÎncă nu există evaluări
- Inggris RevisiDocument12 paginiInggris RevisiSiti Maria UlfahÎncă nu există evaluări
- Tugas Kelompok 5 Bahasa Inggris " Hiv/Aids ": Dosen Pembimbing: Ns Mimi M, Kep Disusun Oleh: Reski Amelda Tira WahyuniDocument14 paginiTugas Kelompok 5 Bahasa Inggris " Hiv/Aids ": Dosen Pembimbing: Ns Mimi M, Kep Disusun Oleh: Reski Amelda Tira WahyuniTira wahyuniÎncă nu există evaluări
- Makalah Bahasa InggrisDocument27 paginiMakalah Bahasa InggrisVena Nur MukaromahÎncă nu există evaluări
- English Papers "Hiv and Aids": Erna Rosalina Nirmala Putri Sariatin AsriantiDocument14 paginiEnglish Papers "Hiv and Aids": Erna Rosalina Nirmala Putri Sariatin AsriantiNirmala malaÎncă nu există evaluări
- Children Reactions To Health Care ExperienceDocument2 paginiChildren Reactions To Health Care ExperienceDessyana PaulusÎncă nu există evaluări
- Patoflow Tumor OtakDocument1 paginăPatoflow Tumor OtakDessyana PaulusÎncă nu există evaluări
- Inten Sive Readi NG: "Acade MIC Article"Document8 paginiInten Sive Readi NG: "Acade MIC Article"Dessyana PaulusÎncă nu există evaluări
- Kasus 1&2Document1 paginăKasus 1&2Dessyana PaulusÎncă nu există evaluări
- Kasus 1&2Document1 paginăKasus 1&2Dessyana PaulusÎncă nu există evaluări
- Patoflow Hipotiroid: Sinkope Konstipasi Sesak Napas Jarang Berkeringat Impoten MyalgiaDocument1 paginăPatoflow Hipotiroid: Sinkope Konstipasi Sesak Napas Jarang Berkeringat Impoten MyalgiaDessyana Paulus50% (2)
- CHF in EnglishDocument58 paginiCHF in EnglishDessyana PaulusÎncă nu există evaluări
- LampiranDocument2 paginiLampiranmpuyherawatiÎncă nu există evaluări
- NOSODESDocument5 paginiNOSODESnamkay_tenzynÎncă nu există evaluări
- FNCP Inadquate Nutrition IntakeDocument3 paginiFNCP Inadquate Nutrition Intakekat_leon_250% (2)
- PE ActivityDocument3 paginiPE ActivityApriljoy MadridanoÎncă nu există evaluări
- What Is COVID-19 and How Can I Protect Myself?: Answer From Pritish K. Tosh, M.DDocument2 paginiWhat Is COVID-19 and How Can I Protect Myself?: Answer From Pritish K. Tosh, M.DDonÎncă nu există evaluări
- Disseminated Intravascular CoagulationDocument19 paginiDisseminated Intravascular CoagulationAnna MilliziaÎncă nu există evaluări
- Soft Tissue Healing After Different Flap Designs in Periapical SurgeryDocument4 paginiSoft Tissue Healing After Different Flap Designs in Periapical SurgeryallthewayhomeÎncă nu există evaluări
- Micormedex NeoFax-neonatologieDocument869 paginiMicormedex NeoFax-neonatologiebaranclaudiaÎncă nu există evaluări
- Penerapan E-Resep Meningkatkan Mutu Farmasi RS di JakartaDocument5 paginiPenerapan E-Resep Meningkatkan Mutu Farmasi RS di JakartaIim RimbaÎncă nu există evaluări
- Helping Babies Breathe™ 06.27.2014Document18 paginiHelping Babies Breathe™ 06.27.2014Emily EresumaÎncă nu există evaluări
- Invent A RioDocument56 paginiInvent A RioJhoel Eusebio Parraga IsidroÎncă nu există evaluări
- MagnitudeDocument91 paginiMagnitudesanthiyasandyÎncă nu există evaluări
- How To Setup Biotrans ?Document21 paginiHow To Setup Biotrans ?Agoes TreeyantÎncă nu există evaluări
- CCJC BodinDocument2 paginiCCJC Bodinapi-495663503Încă nu există evaluări
- Nurs412 Ethical Issues in Nursing Paper Neuburg IntroDocument2 paginiNurs412 Ethical Issues in Nursing Paper Neuburg Introapi-452041818100% (1)
- China Oel Pil enDocument2 paginiChina Oel Pil enmiksha100% (1)
- Markel H - The Stethoscope and The Art of Listening 2006Document3 paginiMarkel H - The Stethoscope and The Art of Listening 2006GeorgianaRamonaÎncă nu există evaluări
- ESSAY&MCQDocument21 paginiESSAY&MCQBianca DwintaÎncă nu există evaluări
- Babesia Canis and Other Tick Borne Infections in Dogs in Central Poland 2009 Veterinary ParasitolDocument8 paginiBabesia Canis and Other Tick Borne Infections in Dogs in Central Poland 2009 Veterinary ParasitolGabriela Victoria MartinescuÎncă nu există evaluări
- Hypertension Related To Faulty Eating Habits As Evidence My Blood Pressure of 13080.Document2 paginiHypertension Related To Faulty Eating Habits As Evidence My Blood Pressure of 13080.Senyorita KHayeÎncă nu există evaluări
- The - Erlangen - Test - of - Activities - of - Daily - Living - in ADocument3 paginiThe - Erlangen - Test - of - Activities - of - Daily - Living - in Akwstas79Încă nu există evaluări
- EPIDEMIOLOGY OF HEAD INJURY IN COIMBATOREDocument6 paginiEPIDEMIOLOGY OF HEAD INJURY IN COIMBATOREArjun CVÎncă nu există evaluări
- Presented by Animesh Amal: Brand Plan On Salbutamol + Ambroxol + GuaifenesinDocument36 paginiPresented by Animesh Amal: Brand Plan On Salbutamol + Ambroxol + GuaifenesinAnonymous 75aETJ8OÎncă nu există evaluări
- Dina Nurhayati JournalDocument49 paginiDina Nurhayati JournalnindyarpÎncă nu există evaluări
- Sam PDFDocument134 paginiSam PDFPunit Garg100% (2)
- Principles of OncologyDocument26 paginiPrinciples of OncologyDr Shahzad Alam ShahÎncă nu există evaluări
- CV VionikaDocument3 paginiCV VionikaM. ZivantÎncă nu există evaluări
- CandidiasisDocument27 paginiCandidiasisWr Newgate50% (2)
- S. No. City Name Full Address With Contact No.: List of Our ProductsDocument3 paginiS. No. City Name Full Address With Contact No.: List of Our Productsprakashrat1962Încă nu există evaluări
- Pathology Situational EthicsDocument28 paginiPathology Situational Ethicsmohitsingla_86Încă nu există evaluări
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDe la EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionEvaluare: 4 din 5 stele4/5 (402)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDe la EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityEvaluare: 4 din 5 stele4/5 (13)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDe la EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsEvaluare: 3.5 din 5 stele3.5/5 (3)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDe la EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityEvaluare: 3.5 din 5 stele3.5/5 (2)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDe la EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedEvaluare: 5 din 5 stele5/5 (78)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDe la EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeÎncă nu există evaluări
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDe la EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsEvaluare: 5 din 5 stele5/5 (1)
- Techniques Exercises And Tricks For Memory ImprovementDe la EverandTechniques Exercises And Tricks For Memory ImprovementEvaluare: 4.5 din 5 stele4.5/5 (40)
- The Obesity Code: Unlocking the Secrets of Weight LossDe la EverandThe Obesity Code: Unlocking the Secrets of Weight LossEvaluare: 5 din 5 stele5/5 (4)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDe la EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisEvaluare: 4 din 5 stele4/5 (1)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisDe la EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisEvaluare: 5 din 5 stele5/5 (8)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDe la EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsEvaluare: 4.5 din 5 stele4.5/5 (169)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingDe la EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingEvaluare: 3.5 din 5 stele3.5/5 (33)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDe la EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsÎncă nu există evaluări
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingDe la EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingEvaluare: 5 din 5 stele5/5 (5)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.De la EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Evaluare: 4.5 din 5 stele4.5/5 (110)
- The Ultimate Guide To Memory Improvement TechniquesDe la EverandThe Ultimate Guide To Memory Improvement TechniquesEvaluare: 5 din 5 stele5/5 (34)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDe la EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDe la EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeEvaluare: 4.5 din 5 stele4.5/5 (253)
- The Happiness Trap: How to Stop Struggling and Start LivingDe la EverandThe Happiness Trap: How to Stop Struggling and Start LivingEvaluare: 4 din 5 stele4/5 (1)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsDe la EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsÎncă nu există evaluări
- Recovering from Emotionally Immature Parents: Practical Tools to Establish Boundaries and Reclaim Your Emotional AutonomyDe la EverandRecovering from Emotionally Immature Parents: Practical Tools to Establish Boundaries and Reclaim Your Emotional AutonomyEvaluare: 4.5 din 5 stele4.5/5 (201)
- The Tennis Partner: A Doctor's Story of Friendship and LossDe la EverandThe Tennis Partner: A Doctor's Story of Friendship and LossEvaluare: 4.5 din 5 stele4.5/5 (4)