Documente Academic
Documente Profesional
Documente Cultură
Anterior Uveitis
Încărcat de
Margaretha RadjagoekgoEkDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Anterior Uveitis
Încărcat de
Margaretha RadjagoekgoEkDrepturi de autor:
Formate disponibile
Uveitis Anterior more about Uveitis Anterior
Uveitis Anterior is inflammation within the eyeball. The eyeball is divided into a front part (the anterior part) and a back part (the posterior part). Uveitis refers to an inflammation inside the eye that can cause eye pain and problems seeing things. This condition usually responds to treatment.
The pupil (dark part of the eye) may become irregular (instead of round) in shape Symptoms can begin suddenly or can progress slowly over time. Symptoms include pain in one eye, sensitivity to light, redness of the eye, and loss of vision. f the disease comes on slowly, people may have !lurred "ision, but only a small amount of inflammation of the eye.
The disease is due to an inflammation within the eye. The most common reason for the inflammation is that the person#s own immune system becomes overactive and attacks certain structures within the eye. $ Some of the diseases associated with an overactive immune system include Ankylosing Spondylitis, %eiter#s Syndrome, sacroiliitis, &soriasis, 'rohn#s (isease, Ulcerative 'olitis, or !ehcet#s Syndrome
At times, it can be due to an infection (i.e., bacteria, virus, fungi, or parasites), such as the )erpes virus. This is seen more often in people who do not have a normal immune system, such as those with ) ".
Using a special piece of e*uipment (slit lamp or indirect ophthalmoscopy), the doctor can look into the eye and see the inflammation and other changes
that allow them to make the diagnosis.
At times, blood may be tested for +S%, A,A, )-A$!./, "(%-, -yme serology, '!' and chemistry panels may be done depending on what the cause may be.
The patient needs to be seen by an eye specialist and treatment needs to be started as soon as possible. Uveitis Anterior can usually be treated with steroid eye drops (not to be used if an infection is suspected to be the cause). Sometimes, if the drops are not enough, steroid in0ections around the eye may be needed or the person may need to take steroid pills. (rops to dilate the eyes may be used because this will help with the pain and discomfort. ,on $$ steroidal anti inflammatory (,SA (s) such as Aspirin or 1otrin may help in some cases %esponse to treatment is usually pretty good. f the disease is due to an infection, then antibiotics or antiviral medicines will be needed.
%etinal (etachment Tumors within the eye -ymphoma that involves the nervous system
A,T+% 2% U"+ T S typical S 3,S A,( S41&T21S presentation of anterior uveitis involves pain, photophobia and tearing. &atients report a deep, dull aching of the involved eye and
ounding orbit. Associated sensitivity to lights may be severe5 often, these patients will present wearing dark glasses. The e6cessive tearing occurs secondary to increased neural stimulation of the lacrimal gland, and is not ciated with a foreign body sensation.
"isual acuity is not usually impaired to any great e6tent (.7897 or better is common), although ents may report some ha:iness. Accommodative tasks, however, may prove more difficult and uncomfortable. ection may reveal mild to moderate congestion of the lids, resulting in pseudoptosis. 4ou#ll typically see a deep limbal in0ection of the con0unctiva and episclera, although the palpebral con0unctiva is characteristically normal. cornea may display mild edema upon biomicroscopy. n more severe reactions, you may observe grayish brown othelial deposits, known as keratic precipitates.
The hallmark signs of anterior uveitis are ;cells and flare.; 'ells are leukocytes (white blood cells) ting in the convection currents of the a*ueous5 flare refers to liberated protein from the inflamed iris or ciliary y which gives the a*ueous a particulate, or smoky, appearance. The iris may adhere to the lens capsule (posterior echia) or, less commonly, to the peripheral cornea (anterior synechia). Additionally, you may see granulomatous ules within the iris stroma.
ntraocular pressure in the affected eye is initially reduced due to secretory hypotony of the ciliary y. )owever, as the reaction persists, inflammatory by$products may accumulate in the trabeculum. f this debris ds significantly, and if the ciliary body resumes its normal secretory output, the pressure may rise sharply, lting in a secondary uveitic glaucoma.
&AT)2&)4S 2-234 itis, as the name implies, represents an inflammation of the uveal tissues, chiefly the iris and ciliary body. ammation may be associated with underlying systemic disease, or it may occur as a direct result of ocular trauma. asionally, inflammatory reactions in ad0acent tissues (e.g., keratitis), can induce a secondary uveitis.
Uveitis can be either acute or chronic. The chronic form is more often associated with systemic rders including, but not limited to, ankylosing spondylitis, !eh<et#s syndrome, inflammatory bowel disease, nile rheumatoid arthritis, %eiter#s syndrome, sarcoidosis, syphilis, tuberculosis, and -yme disease. 'hronic tis most likely occurs due to an immunopathological mechanism which is not fully understood.
1A,A3+1+,T re are two primary goals when managing anterior uveitis. =irst, immobili:e the iris and ciliary body to decrease and prevent e6acerbation of the condition. Second, *uell the inflammatory response. !egin by cyclopleging the ent with homatropine >? T (8@ (, scopolamine 7..>? ! (8@ ( or atropine A? ! (, depending upon the erity of the reaction. ,e6t, prescribe a topical steroid @.$B), or more often if the reaction is severe. f there#s a erior synechia present, attempt to break the adhesion in the office using atropine A? and phenylephrine A7?. at secondary elevations in 2& using standard anti$glaucoma agents, such as timolol 7.>? ! ( or dor:olamide
Avoid pilocarpine in uveitic glaucoma, as it will only serve to worsen the inflammatory response by bili:ing the uveal tissues. After beginning treatment, re$evaluate the patient every one to seven days depending on severity of the reaction. As the uveitis resolves, discontinue the cycloplegics and taper the steroids to @ ( or T (. erally, it is better to taper slowly rather than abruptly, and patients may need to remain on steroid drops daily or y other day for several weeks. n recalcitrant uveitis which is unresponsive to conventional therapy, consider ctible steroids such as methylprednisolone C7mg or even oral steroids such as prednisone C7 to D7mg.
'- , 'A- &+A%-S
Acute anterior uveitis results most commonly as a result of blunt ocular trauma. n most ances, these cases resolve without incident and do not recur when properly managed. 'onsider any cases of recurrent uveitis, defined as three or more une6plained incidents, to be esentative of underlying systemic inflammatory disease until proven otherwise. )ematologic testing is indicated any recurrent, chronic or bilateral presentation. A standard battery of laboratory tests should includeE complete od count ('!') with differential, antinuclear antibody (A,A), )-A$!./, rheumatoid factor (%=), angiotensin$ verting en:yme (A'+), purified protein derivative (&&(), fluorescent treponemal antibody absorption (=TA$ S) and rapid plasma reagin (%&%). A chest F$ray is also important in identifying both sarcoidosis and rculosis. A -yme titer is also recommended if you suspect that the patient may have been bitten by a deer tick. Always perform a comprehensive, dilated fundus evaluation in these cases. Anterior uveitis actually constitute a ;spillover; of posterior ocular inflammation.
Non Infectious
Anterior uveitis demonstrating hypopyon.
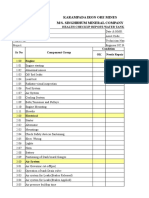
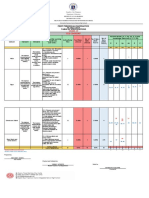
Inflammatory disease of the iris and ciliary body. There are several classifications of uveitis generally used in the literature, i.e. anatomical (anterior, intermediate, posterior and panuveitis), clinical (acute and chronic), etiologic (exogenous and endogenous) and pathologic classification (granulomatous and nongranulomatous). Clinical features o !ymptoms pain due to ciliary spasm, red eye, photophobia, decreased vision and tearing o !igns Circumcorneal ciliary in"ection, irregular pupil or miosis Cells or flare in the a#ueous and hypopyon $ithin the anterior chamber are a sign of active inflammation %ibrous sheets or strands in the anterior chamber &eratic precipitates (&') Iris nodules 'osterior synechiae
Associated systemic conditions an(ylosing spondylitis, )eiter*s syndrome, +eh,et*s disease,sarcoidosis, -erpes .oster ophthalmicus and "uvenile rheumatoid arthritis disease. /aboratory $or(-up for all patients $ith signs of bilateral and recurrent granulomatous uveitis include C+C, 0!), A1A, )'), %TA-A+!, ''2 and anergy panel, -/A +-34 test and chest 5-ray. 6anagement o Treatment is addressed to the co-existing systemic conditions in addition to the eye disease. o 7phthalmic cycloplegic drops are essential to relax ciliary spasm, decrease pain and prevent formation of posterior synechiae. o Topical steroid drops are used to treat inflammation.
If there is no clinical improvement, sub-Tenon*s in"ection or oral steroids may be necessary. &eratic 'recipitates (&'s)
Cellular deposits on the corneal endothelium. Acute, fresh &'s tend to be $hite and round, $hile old &'s are usually irregular, faded and pigmented. 6utton-fat &' large, greasy-$hite &'s (approximately 8 mm in diameter), $hich represent clusters of macrophages and epithelioid cells. Typically occur in granulomatous uveitis.
Non Infectious
Multiple koeppe's nodules lie at the pupillary margin. Iris 1odules
6ay be found as o &oeppe nodules (inflammatory cell precipitates $hich lie at the pupillary margin and could be found in non-granulomaous as $ell as granulomatous uveitis) o +ussaca nodules (lie on the iris surface) $hich are pathognomonic for granulomatous uveitis. 9hen the inflammation is treated, the nodules $ill resolve.
'osterior !ynechiae
Clinical features o Adhesions bet$een posterior iris and the anterior lens surface o 7ften seen in acute anterior uveitis and chronic posterior uveitis o 6ay be complicated $ith angle closure glaucoma due to anterior bo$ing of the
peripheral iris (iris bomb:) especially $hen ;<=-degree adhesion (seclusio pupillae) occurs
Treatment may be attempted $ith cycloplegic drops.
S-ar putea să vă placă și
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Ed Post Lab Heat of Formation of NaClDocument4 paginiEd Post Lab Heat of Formation of NaClEdimar ManlangitÎncă nu există evaluări
- Automated Dish Washer v1.1Document21 paginiAutomated Dish Washer v1.1Anonymous XXCCYAEY6M67% (3)
- Footing - f1 - f2 - Da RC StructureDocument42 paginiFooting - f1 - f2 - Da RC StructureFrederickV.VelascoÎncă nu există evaluări
- Chap9 PDFDocument144 paginiChap9 PDFSwe Zin Zaw MyintÎncă nu există evaluări
- LS01 ServiceDocument53 paginiLS01 ServicehutandreiÎncă nu există evaluări
- Lab 2 - Using Wireshark To Examine A UDP DNS Capture Nikola JagustinDocument6 paginiLab 2 - Using Wireshark To Examine A UDP DNS Capture Nikola Jagustinpoiuytrewq lkjhgfdsaÎncă nu există evaluări
- TW BT 01 - Barstock Threaded Type Thermowell (Straight) : TWBT - 01Document3 paginiTW BT 01 - Barstock Threaded Type Thermowell (Straight) : TWBT - 01Anonymous edvYngÎncă nu există evaluări
- Accounting Worksheet Problem 4Document19 paginiAccounting Worksheet Problem 4RELLON, James, M.100% (1)
- Meniere's Disease - Retinal Detatchment - GlaucomaDocument3 paginiMeniere's Disease - Retinal Detatchment - Glaucomaybet03Încă nu există evaluări
- Revit 2023 Architecture FudamentalDocument52 paginiRevit 2023 Architecture FudamentalTrung Kiên TrầnÎncă nu există evaluări
- Chem Resist ChartDocument13 paginiChem Resist ChartRC LandaÎncă nu există evaluări
- GTA IV Simple Native Trainer v6.5 Key Bindings For SingleplayerDocument1 paginăGTA IV Simple Native Trainer v6.5 Key Bindings For SingleplayerThanuja DilshanÎncă nu există evaluări
- Audi R8 Advert Analysis by Masum Ahmed 10PDocument2 paginiAudi R8 Advert Analysis by Masum Ahmed 10PMasum95Încă nu există evaluări
- 0 BA Design ENDocument12 pagini0 BA Design ENFilho AiltonÎncă nu există evaluări
- Internal Analysis: Pertemuan KeDocument15 paginiInternal Analysis: Pertemuan Kekintan utamiÎncă nu există evaluări
- Assignment Csi104Document11 paginiAssignment Csi104Minh Lê KhảiÎncă nu există evaluări
- Geotechnical Aspects of Open Stope Design at BHP Cannington: G C StreetonDocument7 paginiGeotechnical Aspects of Open Stope Design at BHP Cannington: G C StreetonJuan PerezÎncă nu există evaluări
- Water Tanker Check ListDocument8 paginiWater Tanker Check ListHariyanto oknesÎncă nu există evaluări
- Information Technology Project Management: by Jack T. MarchewkaDocument44 paginiInformation Technology Project Management: by Jack T. Marchewkadeeps0705Încă nu există evaluări
- LRAD Datasheet 2000XDocument2 paginiLRAD Datasheet 2000XOkkar MaungÎncă nu există evaluări
- Manual Samsung Galaxy S Duos GT-S7562Document151 paginiManual Samsung Galaxy S Duos GT-S7562montesjjÎncă nu există evaluări
- NHM Thane Recruitment 2022 For 280 PostsDocument9 paginiNHM Thane Recruitment 2022 For 280 PostsDr.kailas Gaikwad , MO UPHC Turbhe NMMCÎncă nu există evaluări
- MCQs - Chapters 31 - 32Document9 paginiMCQs - Chapters 31 - 32Lâm Tú HânÎncă nu există evaluări
- NGCP EstimatesDocument19 paginiNGCP EstimatesAggasid ArnelÎncă nu există evaluări
- MV Lec PDFDocument102 paginiMV Lec PDFJonas Datu100% (1)
- OVDT Vs CRT - GeneralDocument24 paginiOVDT Vs CRT - Generaljaiqc100% (1)
- Unit 1 - Lecture 3Document16 paginiUnit 1 - Lecture 3Abhay kushwahaÎncă nu există evaluări
- Obara BogbeDocument36 paginiObara BogbeOjubona Aremu Omotiayebi Ifamoriyo0% (1)
- Revised Final Quarter 1 Tos-Rbt-Sy-2022-2023 Tle-Cookery 10Document6 paginiRevised Final Quarter 1 Tos-Rbt-Sy-2022-2023 Tle-Cookery 10May Ann GuintoÎncă nu există evaluări
- Stewart, Mary - The Little BroomstickDocument159 paginiStewart, Mary - The Little BroomstickYunon100% (1)