Documente Academic
Documente Profesional
Documente Cultură
Impulse-Control Disorders
Încărcat de
Roci ArceDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Impulse-Control Disorders
Încărcat de
Roci ArceDrepturi de autor:
Formate disponibile
I48
Impulse-Control Disorders
8. Reite M, Buyesse D, Reynolds C, Mendelson W: The use of polysomnography in the evaluation of insomnia. Sleep 18:58-70, 1995. 9. Reite M, Nagel K, Ruddy JA: A Concise Guide to the Evaluation and Treatment of Sleep Disorders, 2nd ed. Washington, DC, American Psychiatric Press, 1997. 10. Wong AH, Smith M, Boon HS: Herbal remedies in psychiatric practice. Arch Gen Psychiatry 55:1033-1044, 1998.
30. IMPULSE-CONTROL DISORDERS
Michael H.Gertdel, M.D
1. Which disorders are classified as impulse-control disorders? Intermittent explosive disorder, pyromania, kleptomania, trichotillomania (compulsive pulling of a patients own hair), and compulsive gambling. Disorders that involve the failure to resist impulses to use alcohol or drugs, eat abnormally (including purging and food restriction), or perform certain sexual behaviors are not classified in this group. 2. What fundamental features do impulse-control disorders have in common? No one knows. Presumably they are grouped together because they are disorders of behavior resulting from the failure to resist a subjective impulse to perform that behavior. However, these irresistible impulses are very different in nature (e.g., violence and hair pulling), in frequency (rare violent outbursts, hair pulling throughout the day), and resulting behavior (e.g., gambling and fire-setting). Many clinicians regard them as disorders of tension regulation.Feelings of excitement, tension, or arousal before acting; pleasure, euphoria, or relief during acting; and dysphoria or guilt after acting are more or less present in this cluster. Some empathic imagining of what this condition might be like should be attempted, if for no other reason than to help distinguish these illnesses from more ordinary experiences. For instance, in trichotillomania, one might become very agitated during any concerted attempt to stop hair pulling, such that focus on any other activity is impossible. Minutes to hours of hair removal provide only temporary relief of tension. Bitter depression and emptiness may envelop the sufferer as the day ends and he or she imagines the next day as little more than the same struggle repeated. The propensity to act rather than express feelings is another common characteristic of this group. Many afflicted individuals are not aware of their feelings and cannot name or use them (alexithymia).
3. Are these disorders biologically similar? The biologic substrate is not yet elucidated. Considerable evidence is mounting that abnormal serotonin metabolism is present, particularly low serotonin turnover with decreased CSF 5-HIAA, in some of these disorders. Intermittent explosive disorder (IED) is most clearly associated with these changes, though kleptomania, pyromania, and trichotillomania are implicated in some studies. The role of serotonin receptor subtypes also may be important. In various types of aggressive behavior, agonists of the 5-HT1A receptor and antagonists of the 5-HT2 receptor appear to reduce symptoms. It is not yet clear whether all of these disorders share a common neurobiologic basis.
4. What is an impulse? An impulse is a feeling to which an action is connected. It is an urge to act. The issue of time course or urgency is very confusing. Commonly used expressions such as impulsive decision and electrical impulse suggest urgent action or immediate discharge. Some of these disorders conform clinically to these images, such as the sudden violence in IED. In pyromania, however, a fire might be intricately planned and executed, implying either that the concept of
Impulse-Control Disorders
I49
the firesetting impulse is not easily approached through common language paradigms or that tension relief begins with the internal act of planning the fire.
5. How does one resist or fail to resist an impulse? In traditional psychiatry, impulses fail to result in actions because of adequate defenses. Defenses are ego functions, which themselves may be healthy (i.e., lead to better organismic adaptation) or less healthy (i.e., lead to problems of their own). Defenses also may be effective in preventing expression of unwanted impulses. They are unconscious operations that serve to reduce internal tension. You might imagine that people with good defensive structures do not leak unwanted behaviors, and those with poorer ones do. Unfortunately, such is not the case. Impulse-control disorders involve, by definition, truly overwhelming internal states that sometimes coexist with sound psychological defensive structures which simply do not help with these behaviors. These problems occur in a variety of people. In fact, most of these diagnoses can be made only in the absence of a primary axis I or I1 illness, which suggests that there is no pervasive or typical deficiency in defenses. Treatments based on creating healthier defense structures have a poor track record in these disorders, as they do with substance abuse and sexual disorders. Another framework from which to approach this question is that of the ability to defer an impulse-connected action. To what extent can a violent feeling be contained as just a feeling, and the urge to act on it be delayed, put off, or even permanently put aside? Here, we can examine the effect of conscious behavior-controlling schemes (such as using the knowledge that an act may be unlawful, dangerous, or unacceptable). Other such operations might include remembering a previous bad outcome, distracting oneself with other thoughts or actions, or calling a friend for support. The extent to which a patient has attempted to use such methods might help a clinician understand the extent to which a person wanted to control an impulse. It may ultimately prove more useful to examine the biology of the expression of specific behaviors, when such information becomes available. This will allow understanding of the neurochemical regulation of impulses and actions in normal and pathologic states.
6. How is Einstein connected to this discussion? General relativity teaches us to stop thinking about gravity as a force operating on an object. It
suggests other metaphors. Gravity can be conceptualized as a property of mass that alters the shape of space in the vicinity of the mass, such that the motion of neighboring massful objects is changed. The earth thus alters nearby space such that the moon (which might otherwise travel in a different trajectory) orbits it; it does not hold the moon by force of gravity. Impulse, too, is an old concept that may profit from newer conceptualizations or metaphors. Perhaps acting on impulse is experiencing a particular internal mental state that is less separable from behavior: the shape of our being would be altered by a feeling of this type. An impulse-control disorder might then be conceptualized as a condition of having more behavior-shaping feelings in which thoughts, fears, and concerns have less relevance. Although the underlying neurochemistry of such a condition is unclear, it is possible that the impulse-control-disordered phenomenon may be wired differently than ordinary feelings. If so, then gambling for the normal person may not be the same activity as gambling for the pathologic gambler.
7. What role do clinician attitudes play in impulse-control disorders? One of the difficulties of working with patients with these sorts of problems is the negative feelings we have toward the behaviors themselves. Further, the problems tend to be repetitive and difficult to treat, leading to feelings of helplessness and powerlessness in the physician. Under these conditions we are likely to view such patients in moralistic and oversimplified ways. Anything we can do to generate intellectual interest, conceptualize the issues differently, or otherwise tilt the problem on its end will aid us in the effort to approach these disorders and the afflicted patients with scientific and humane interest.
8. What diagnostic problems are associated with impulse-controldisorders? As a group, these disorders are less well studied than most psychiatric conditions. When knowledge is sparse, diagnostic difficulty is inherent. Earlier versions of the DSM emphasized neurologic
150
Impulse-Control Disorders
abnormalities in E D . In the current diagnostic schema, if a clearly diagnosable general medical condition is causing the explosive outbursts, you should diagnose Personality Change Due to a General Medical Condition rather than E D . However, soft neurologic signs and nonspecific EEG abnormalities do not constitute a diagnosable medical disorder and do not exclude the diagnosis of IED. Patients with IED demonstrate a greater frequency of EEG abnormalities when compared to various control samples. Certain of these diagnoses cannot be made if the behavior is better accounted for by another condition, yet in reality it may rarely be seen in the absence of another serious disorder. For instance, IED should not be the diagnosis if antisocial or borderline disorders, in which explosiveness and poor temper regulation are common, better account for the behavior. However, many cases that conform well to the picture of the clinical entity of IED occur in the context of these serious character pathologies. DSM-IV adds the better accounted for exception to the diagnostic criteria of all disorders in this group. For trichotillomania the accompanying condition is most likely dermatologic. For pathologic gambling, the other condition is specifically manic. A patients history is the most important diagnostic aid when two disorders may be present. If compulsive gambling clearly precedes the onset of identifiable manic symptoms, or is present in a euthymic period, both diagnoses may be appropriate. Many patients with an impulse-control disorder suffer major depression. Such depression often results from the damage created by the disorder, and historically follows the disorders onset. If the impulse disorder occurs only in the context of an affective episode, excluding or at least deferring the impulse disorder diagnosis is quite sensible. In this chapter, characterizations of the diagnostic entities are based on DSM-IV.
9. How to you differentiate intermittent explosive disorder and a bad temper?
A bad temper is not an illness; nor is explosive behavior. In IED, there are several episodes of aggression that result in serious destruction or assault and are not better accounted for by other psychiatric disorders, including substance abuse, or a medical condition. Some people known to have bad tempers may suffer from IED; most IED sufferers have bad tempers.
10. What is the difference between kleptomania and other forms of stealing?
The defining feature of kleptomania is that the sufferer steals in the absence of need for the stolen object or its monetary value. Kleptomaniacs tend to experience the impulse to steal as foreign and unwanted (ego dystonic). They steal on the spur of the moment despite the more constant pressure of the urge to steal. Any item may be stolen. The article may be kept, hoarded, thrown away, or even returned. The individual may worry about getting caught, but fail to plan the crime with such a consequence in mind. Kleptomaniacs generally are not antisocial. They steal alone, without accomplices. They are more often female than male. Other stealing behavior has many forms. Shoplifters typically are seeking the item stolen, even if it is low in value. Many individuals steal for profit, gain, or revenge. The stealing may be planned, and the thief may carefully consider the dangers and consequences of apprehension. These motives and thought patterns are not typical of kleptomania and if present should lead to doubt about such a diagnosis, as should a more general pattern of antisocial behavior. The cycle of tension building before the theft, pleasure or relief during its commission, and depression afterward usually is not present in criminal stealing, though sensation-seeking may be a factor. Accomplices are more common in other forms of stealing.
11. How do you distinguish between trichotillomania and other causes of hair loss? Trichotillomania consists of the pulling out of ones hair, resulting in noticeable hair loss, coupled with the cycle of tension preceding the act, gratification of doing so, and sometimes dysphoria afterward. A patient with trichotillomania may be quite ashamed of the condition and may not report the true source of the hair loss. Hair may be pulled from any area of the body: most often from the head (eyelashes, eyebrows, scalp), and also from the axilla, pubic, or perirectal areas. Other conditions with hair loss include alopecia areata, male-pattern baldness, chronic discoid lupus erytheniatosus, lichen planopilaris, folliculitis decalvans, pseudopelade, and alopecia mucinosa. Skin inflammation generally does not occur in trichotillomania, in contrast to alopecia areata. Biopsy in trichotillomania shows short and broken hairs, with normal and damaged follicles in the same vicinity. Follicles often show trauma, or may be empty. More catagen hairs (those hairs in
Impulse-Control Disorders
151
the short phase between growth and resting, or between anagen and telogen phases) are seen. Also look for evidence of nail biting and scratching behaviors. This condition may present with gastrointestinal symptoms caused by bezoars, generated by trichophagia (eating hairs).
12. What pharmacologictreatment@)are useful in these disorders? Medicines used to treat IED include anticonvulsants (especially carbamazepine, valproate, and phenytoin), serotonergic antidepressants, buspirone, beta blockers, lithium, neuroleptics, and calcium-channel blockers. Of these, anticonvulsants and beta blockers show promise. Antidepressants, especially SSRIs, have been found useful in trichotillomania. Some suspect trichotillomania to be related to obsessive-compulsive disorder. Anecdotally, kleptomania, pyromania, and pathologic gambling have responded to a variety of medicines, usually antidepressants, buspirone, or thymoleptics (mood stabilizers such as lithium, carbamazepine, or valproate).
13. If you suspect the diagnosis of pyromania, should steps be taken to ensure safety?
Anyone who sets fue is dangerous, whether or not they meet the criteria for pyromania. The proportion of mentally disordered arsonists diagnosed with pyromania is low, suggesting that other firesetters also represent a dangerous population. Systematically evaluate potentially dangerous behavior; suicide and homicide risk assessments are models. Query pyromaniacs about past fires, including scope, damage, and associated injuries or deaths. This information-gathering is not for the purpose of reporting to authorities, but to measure the potential for danger. Evaluate current fantasies and plans for firesetting, including specific sites and individuals who may be involved. Even a general fantasy or plan involving no definite place or person should be noted-particularly if the patient believes there is a likelihood of action. Such patients may meet criteria for involuntary commitment. Be aware of the standards for civil commitment in each state. Mental health professionals have been found liable for failure to warn possible victims of firesetting (Peck v. Counseling Service ofAddison Country, 146Vt. 61,499 A.2d 422 [1985]). The duties to warn and protect are clearly defined in some jurisdictions because of state law or case law, and you should be familiar with the applicable standards in your geographic area of practice. Depending on the jurisdiction, such duties may be camed out by warning the individual endangered, calling the police or other authorities, detaining the dangerous person, or other measures. Issues of confidentiality (and privilege, if court actions ultimately ensue) are raised if warnings are given without the patients consent. 14. Is pathologic gambling an addiction? This question is controversial in psychiatry and among addiction experts. It should not be construed to suggest that impulse-control disorders are hard to distinguish from addictive disorders. Clinically, pathologic gambling has such similarity to addictive behavior that it has been called a process addiction. This resemblance is much closer than to the other impulse-control disorders (which are so different from each other that their main commonality is that they are classified together). Below are arguments against and for this question. Against Too many problems already are miscast as addictions. The word and concept are trivialized by such usage. Such diagnosis lends an aura of respectability to behavior which is better thought of as simply impulse-ridden. Addiction is a term that should be reserved for activities in which an exogenous chemical is introduced into the body, not for any other repetitive behavior. Many conceptual models of pathologic gambling exist. No single model explains all such behavior. Any model may prove useful in a given case. Some cases might be best understood from a psychoanalytic or behaviorist perspective, as a habit disorder, or as a condition comorbid with other psychiatric illness or directly related to other psychiatric illness (especially manic state, depression, and obsessive-compulsive disorder). Diagnosis implies treatment. One may too narrowly prescribe addiction-modeled treatment for a disorder with other available approaches.
I52
Impulse-Control Disorders
For Loss of control over a compulsively repeated behavior (with resulting adverse consequences) is the hallmark of addiction. Pathologic gambling fits this model.
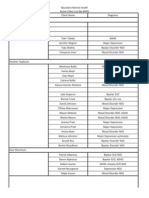
DSM-IV diagnostic criteria for pathologic gambling are strikingly similar to the criteria for addictive illness (see table). This reflects the similarity in conditions. Some studies of compulsive gamblers document that upon cessation of gambling, physical withdrawal symptoms occur similar to those of opioid and central nervous system depressant withdrawal symptoms. Gamblers Anonymous, a 12-step program modeled on Alcoholics Anonymous, has proved helpful to many pathologic gamblers, and may be the most effective intervention currently available. Gamblers have been successfully treated in programs with other addicts. Addiction itself has many conceptual models. The notion of addiction should not impede thinking conceptually or diagnostically. Medicine is eclectic and empiric. Any treatment that helps, does not pose excessive risk of harm, and is ethical should be considered. This author sides with the arguments for calling gambling an addiction. It may not be conceptually neat, but practically speaking, pathologic gambling behaves like an addiction, including its response to treatment and 12-step support programs. More knowledge or more effective treatment may lead to a reconsideration of this conclusion.
D S M - N Diagnostic Criteria
SUBSTANCE DEPENDENCE PATHOLOGIC GAMBLING
Tolerance: need for more substance to achieve desired effect or diminished effect with same amount of substance (1) Withdrawal: characteristic withdrawal syndrome or substance taken to relieve withdrawal symptoms. (2) Substance taken in larger amounts or longer than intended. (3) Persistent desire or unsuccessful attempts to cut down or control use. (4) Much time spent in obtaining, using, or recovering from substance use. ( 5 )
Need to gamble with increasing amounts of money in order to achieve the desired excitement. (2) Is restless or initable when attempting to cut down or stop gambling. (4) After losing money gambling, often returns another day to get even (chasing losses). (6) Has repeated unsuccessful efforts to control, cut back, or stop gambling. (3) Is preoccupied with gambling (e.g., preoccupied with reliving past gambling experiences, handicapping or planning the next venture, or thinking of ways to get money with which to gamble). (1) Has jeopardized or lost a significant relationship, job, or educational or career opportunity because of gambling. (9) Lies to family members, therapist, or others to coiiceal the extent of involvement with gambling. (7) Gambles as a way of escaping from problems or relieving a dysphoric mood. ( 5 ) Has committed illegal acts such as forgery, fraud, theft, or embezzlement to finance gambling. (8) Relies on others to provide money to relieve a desperate financial situation caused by gambling. (10)
Important social, occupational, or recreational activities are given up or reduced because of substance use. ( 6 )
Substance use continues despite knowledge of a physical or psychological problem likely caused or exacerbated by the substance. (7)
Numbers in parentheses correspond to numbered diagnostic criteria in DSM-IV. Grouping of criteria is for the purpose of comparison and is not part of DSM-IV, and some material has been paraphrased or shortened.
Medically Unexplained Symptoms
I53
15. True or false: The expression of an impulse disorder is more likely to occur under the influence of substances of abuse. True. Further, these disorders have considerable comorbidity with substance use disorders, as well as with mood disorders and personality disorders.
BIBLIOGRAPHY
1. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American PsychiatricAssociation, 1994. 2. DeCaria CM, Hollander E, Grossman R, et al: Diagnosis, neurobiology, and treatment of pathologic gambling. J Clin Psychiatry 57(suppl S):SSO-S84, 1996. 3. Drake ME, Hietter SA, Pakalnis A: EEG and evoked potentials in episodic-dyscontrol syndrome. Neuropsychobiology 26: 125, 1992. 4. Gerner RH: Pharmacological treatment of violent behaviors. In Rosner R (ed): Principles and Practice of Forensic Psychiatry. New York, Chapman and Hall, 1994, pp 444450. 5. Kavoussi R, Armstead P, Coccaro E: The neurobiology of impulsive aggression. Psychiatr Clin North Am 20(2):395-403, 1997. 6. Marohn RC, Custer R, Linden RD, et al: Impulse control disorders not elsewhere classified. In American Psychiatric Association: Treatments of Psychiatric Disorders: A Task Force Report of the American PsychiatricAssociation. Washington, DC, American Psychiatric Association, 1989, pp 2457-2496. 7. McElroy SL, Hudson J1, Pope HG, et al: The DSM-111-R impulse control disorders not elsewhere classified: Clinical characteristicsand relationship to other psychiatric disorders.Am J Psychiatry 149:318, 1992. 8. McElroy SL, Soutullo CA, Beckman DA, et al: DSM-IV intermittent explosive disorder: A report of 27 cases. J Clin Psychiatry 59:203-210, 1998. 9. Murray JB: Review of research on pathological gambling. Psycho1 Rep 72:791, 1993. 10. Schalling D: Neurochemical correlates of personality, impulsivity, and disinhibitory suicidality. In Hodgins S (ed): Mental Disorder and Crime. Newbury Park, CA, Sage, 1993, pp 208-226. 1 1 . Stein DJ, Hollander E, Liebowitz MR: Neurobiology of impulsivity and impulse control disorders. J Neuropsychiatry and Clin Nenrosci 5:9, 1993. 12. Virkkunen M, Linnoila M: Serotonin in personality disorder with habitual violence and impulsivity. In Hodgins S fed): Mental Disorder and Crime. Newbury Park, CA, Sage, 1993, pp 227-243.
3 1. MEDICALLY UNEXPLAINED SYMPTOMS
Ala~ M.Jacobson, M.D.
1. Define the term medically unexplained symptoms.
Patients commonly present to their primary physicians with medical symptoms that cannot be fully explained by specific somatic illnesses. Such unexplained symptoms may vary considerably in duration and severity; often they are transient and mild, resolving without specific intervention. Simple explanation and reassurance, supported by physician assessment (history, physical exam, and office-based laboratory tests), may significantly reduce others. The severity, intensity, and persistence of the symptoms dictate consideration of in-depth diagnostic evaluation, which may include more extensive medical and psychiatric work-ups. Even with detailed assessment, a clear somatic explanation may remain elusive, and the symptoms may persist. Four groups of psychiatric disorders comprise the more severe and/or persistent presentations of medically unexplained symptoms: somatoform disorders, factitious disorders, other psychiatric disorders (e.g., anxiety and depression), and malingering.When assessing patients with medically unexplained symptoms that are more than mild or transient, consider etiologies in all four spheres.
2. Do all severe andor persistent unexplained presentations have psychiatric causes? No. Some unexplained symptoms are due to biomedical syndromes that are not yet diagnosable.
Indeed, in the course of ongoing somatoform and other psychiatric disorders, patients may develop
S-ar putea să vă placă și
- Integrative Dual Diagnosis Treatment Approach to an Individual with Alcoholism and Coexisting Endogenous DepressionDe la EverandIntegrative Dual Diagnosis Treatment Approach to an Individual with Alcoholism and Coexisting Endogenous DepressionEvaluare: 2 din 5 stele2/5 (1)
- Summary of Andrew J. Wakefield's Waging War On The Autistic ChildDe la EverandSummary of Andrew J. Wakefield's Waging War On The Autistic ChildÎncă nu există evaluări
- Becoming Myself: A Soul Journey with Chronic Illness and DisabilityDe la EverandBecoming Myself: A Soul Journey with Chronic Illness and DisabilityÎncă nu există evaluări
- The Kidney Morphology, Biochemistry, PhysiologyDe la EverandThe Kidney Morphology, Biochemistry, PhysiologyCharles RouillerÎncă nu există evaluări
- Racism and Psychiatry: Contemporary Issues and InterventionsDe la EverandRacism and Psychiatry: Contemporary Issues and InterventionsMorgan M. MedlockÎncă nu există evaluări
- Advances in Cognitive—Behavioral Research and Therapy: Volume 5De la EverandAdvances in Cognitive—Behavioral Research and Therapy: Volume 5Încă nu există evaluări
- Solution Focused Harm Reduction: Working effectively with people who misuse substancesDe la EverandSolution Focused Harm Reduction: Working effectively with people who misuse substancesÎncă nu există evaluări
- Study Guide to Accompany Physiological Psychology Brown/WallaceDe la EverandStudy Guide to Accompany Physiological Psychology Brown/WallaceÎncă nu există evaluări
- Psychiatric Diagnosis: Challenges and ProspectsDe la EverandPsychiatric Diagnosis: Challenges and ProspectsIhsan M. SalloumEvaluare: 5 din 5 stele5/5 (1)
- Psychotherapy Pearls: Critical Insights for Doing PsychotherapyDe la EverandPsychotherapy Pearls: Critical Insights for Doing PsychotherapyÎncă nu există evaluări
- CLINICAL SPECIALIST IN CHILD AND ADOLESCENT PSYCHIATRIC AND MENTAL HEALTH NURSING: Passbooks Study GuideDe la EverandCLINICAL SPECIALIST IN CHILD AND ADOLESCENT PSYCHIATRIC AND MENTAL HEALTH NURSING: Passbooks Study GuideÎncă nu există evaluări
- Psychiatry Practice Boosters, Second Edition: Insights from research to enhance your clinical workDe la EverandPsychiatry Practice Boosters, Second Edition: Insights from research to enhance your clinical workÎncă nu există evaluări
- Intermittent Explosive Disorder: Etiology, Assessment, and TreatmentDe la EverandIntermittent Explosive Disorder: Etiology, Assessment, and TreatmentEmil F. CoccaroÎncă nu există evaluări
- Ocd and Me: My Unconventional Journey Through Obsessive Compulsive DisorderDe la EverandOcd and Me: My Unconventional Journey Through Obsessive Compulsive DisorderÎncă nu există evaluări
- Beyond Mental Illness: Transform the Labels Transform a LifeDe la EverandBeyond Mental Illness: Transform the Labels Transform a LifeÎncă nu există evaluări
- Tics and Tourette Syndrome: Key Clinical PerspectivesDe la EverandTics and Tourette Syndrome: Key Clinical PerspectivesÎncă nu există evaluări
- CBT For Eating Disorders and Body Dysphoric Disorder: A Clinical Psychology Introduction For Cognitive Behavioural Therapy For Eating Disorders And Body Dysphoria: An Introductory SeriesDe la EverandCBT For Eating Disorders and Body Dysphoric Disorder: A Clinical Psychology Introduction For Cognitive Behavioural Therapy For Eating Disorders And Body Dysphoria: An Introductory SeriesÎncă nu există evaluări
- Men and Depression: Clinical and Empirical PerspectivesDe la EverandMen and Depression: Clinical and Empirical PerspectivesÎncă nu există evaluări
- The Essential Handbook of Memory Disorders for CliniciansDe la EverandThe Essential Handbook of Memory Disorders for CliniciansÎncă nu există evaluări
- Behavior Therapy in Psychiatric Practice: The Use of Behavioral Procedures by PsychiatristsDe la EverandBehavior Therapy in Psychiatric Practice: The Use of Behavioral Procedures by PsychiatristsÎncă nu există evaluări
- First Aid Tips for Depression: Overcoming Depression In 4 Simple StepsDe la EverandFirst Aid Tips for Depression: Overcoming Depression In 4 Simple StepsÎncă nu există evaluări
- Hallucination, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDe la EverandHallucination, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsÎncă nu există evaluări
- Mental Testing in Clinical Practice: The Commonwealth and International Library: Mental Health and Social Medicine DivisionDe la EverandMental Testing in Clinical Practice: The Commonwealth and International Library: Mental Health and Social Medicine DivisionÎncă nu există evaluări
- Without Stigma: About the Stigma and the Identity of the Mental IllnessDe la EverandWithout Stigma: About the Stigma and the Identity of the Mental IllnessÎncă nu există evaluări
- OCPDDocument3 paginiOCPDNur Arina DayanaÎncă nu există evaluări
- Bipolar Disorder Vulnerability: Perspectives from Pediatric and High-Risk PopulationsDe la EverandBipolar Disorder Vulnerability: Perspectives from Pediatric and High-Risk PopulationsÎncă nu există evaluări
- The Psychiatric Salad Bar -Adventures in Autism and Alternative RealitiesDe la EverandThe Psychiatric Salad Bar -Adventures in Autism and Alternative RealitiesÎncă nu există evaluări
- The Diabetes Ready Reference for Health ProfessionalsDe la EverandThe Diabetes Ready Reference for Health ProfessionalsÎncă nu există evaluări
- Comprehensive Handbook of Clinical Health PsychologyDe la EverandComprehensive Handbook of Clinical Health PsychologyBret A BoyerÎncă nu există evaluări
- The Invert Formula: The Invert Formula, #1De la EverandThe Invert Formula: The Invert Formula, #1Încă nu există evaluări
- Home Environment and Early Cognitive Development: Longitudinal ResearchDe la EverandHome Environment and Early Cognitive Development: Longitudinal ResearchAllen W. GottfriedÎncă nu există evaluări
- Aboulomania, (Disorder of Indecision) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDe la EverandAboulomania, (Disorder of Indecision) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsÎncă nu există evaluări
- Asperger's Syndrome An Introduction For EducatorsDocument7 paginiAsperger's Syndrome An Introduction For EducatorsDruga DanutÎncă nu există evaluări
- Neuroprotection in Autism, Schizophrenia and Alzheimer's diseaseDe la EverandNeuroprotection in Autism, Schizophrenia and Alzheimer's diseaseIllana GozesÎncă nu există evaluări
- Biological Psychiatry: A Review of Recent AdvancesDe la EverandBiological Psychiatry: A Review of Recent AdvancesÎncă nu există evaluări
- Tardive Dystonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDe la EverandTardive Dystonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsÎncă nu există evaluări
- The Massachusetts General Hospital Textbook on Diversity and Cultural Sensitivity in Mental HealthDe la EverandThe Massachusetts General Hospital Textbook on Diversity and Cultural Sensitivity in Mental HealthÎncă nu există evaluări
- The Addicted Child: A Parent's Guide to Adolescent Substance AbuseDe la EverandThe Addicted Child: A Parent's Guide to Adolescent Substance AbuseÎncă nu există evaluări
- Improving the Mental Health Consultation: Introducing a short circuit tool to aid patient understanding and dispel stigmaDe la EverandImproving the Mental Health Consultation: Introducing a short circuit tool to aid patient understanding and dispel stigmaÎncă nu există evaluări
- Principles and Practice of Child Neurology in Infancy, 2nd EditionDe la EverandPrinciples and Practice of Child Neurology in Infancy, 2nd EditionÎncă nu există evaluări
- Disruptive Impulse Control and Conduct Disorders 2Document120 paginiDisruptive Impulse Control and Conduct Disorders 2Sana100% (1)
- Advances in Experimental Clinical Psychology: Pergamon General Psychology SeriesDe la EverandAdvances in Experimental Clinical Psychology: Pergamon General Psychology SeriesÎncă nu există evaluări
- Summary of Marlene Steinberg M.D. & Maxine Schnall's The Stranger in the MirrorDe la EverandSummary of Marlene Steinberg M.D. & Maxine Schnall's The Stranger in the MirrorÎncă nu există evaluări
- Balancing Thoughts and Feelings About Food: A Mental Health Professional’s Creative Idea Guide to Treating Adolescent Eating Disorders In Individual or Group SettingsDe la EverandBalancing Thoughts and Feelings About Food: A Mental Health Professional’s Creative Idea Guide to Treating Adolescent Eating Disorders In Individual or Group SettingsÎncă nu există evaluări
- Essential Clinical Guide to Understanding and Treating AutismDe la EverandEssential Clinical Guide to Understanding and Treating AutismÎncă nu există evaluări
- I. Approach To Clinical Interviewing and DiagnosisDocument6 paginiI. Approach To Clinical Interviewing and DiagnosisRoci ArceÎncă nu există evaluări
- Encopresis and EnuresisDocument10 paginiEncopresis and EnuresisRoci ArceÎncă nu există evaluări
- Sedative-Hypnotic DrugsDocument8 paginiSedative-Hypnotic DrugsRoci ArceÎncă nu există evaluări
- Antianxiety AgentsDocument4 paginiAntianxiety AgentsRoci ArceÎncă nu există evaluări
- Mood-Stabilizing AgentsDocument9 paginiMood-Stabilizing AgentsRoci ArceÎncă nu există evaluări
- Planned Brief PsychotherapyDocument7 paginiPlanned Brief PsychotherapyRoci ArceÎncă nu există evaluări
- Group TherapyDocument6 paginiGroup TherapyRoci ArceÎncă nu există evaluări
- DementiaDocument6 paginiDementiaRoci ArceÎncă nu există evaluări
- DeliriumDocument5 paginiDeliriumRoci ArceÎncă nu există evaluări
- Generalized Anxiety Disorder (GAD) Screening ToolDocument2 paginiGeneralized Anxiety Disorder (GAD) Screening ToolBrasa Y. de AlmiraÎncă nu există evaluări
- Homeopathic Management of Defiant and Violent ChildrenDocument119 paginiHomeopathic Management of Defiant and Violent ChildrenJacqueline Tan100% (10)
- Yllana Bay View College: Qualifying Exam Review 1 (Crim - Soc)Document2 paginiYllana Bay View College: Qualifying Exam Review 1 (Crim - Soc)Criseljosa Lacapag100% (2)
- Mental Health Awareness Speech ScriptDocument4 paginiMental Health Awareness Speech ScriptZyrine AdaÎncă nu există evaluări
- Active Clients With Diagnosis by MHPDocument4 paginiActive Clients With Diagnosis by MHPapi-173895728Încă nu există evaluări
- Attention-Deficit Hyperactivity DisorderDocument4 paginiAttention-Deficit Hyperactivity DisorderSharif AznagÎncă nu există evaluări
- Level 1 Measure Child Age 11 To 17Document3 paginiLevel 1 Measure Child Age 11 To 17waleskacrzÎncă nu există evaluări
- Lesson 4 - EatingdisorderDocument41 paginiLesson 4 - EatingdisorderAna CauinianÎncă nu există evaluări
- Adhd and AutismDocument50 paginiAdhd and AutismayunisallehÎncă nu există evaluări
- The Influence of Mental Illness in IndonesiaDocument2 paginiThe Influence of Mental Illness in IndonesiaNur SaidahÎncă nu există evaluări
- NFDN 2007 Professional PortofiloDocument3 paginiNFDN 2007 Professional Portofiloapi-320489210Încă nu există evaluări
- Dying To Be Thin Video Questions StudentDocument2 paginiDying To Be Thin Video Questions Studentjogoeh7100% (1)
- Mental Health - Anxiety DisordersDocument19 paginiMental Health - Anxiety DisordersLaddi Dhencee CareyÎncă nu există evaluări
- What Is The P-Factor of Psychopalogy - Some Risks of General Factor ModelingDocument15 paginiWhat Is The P-Factor of Psychopalogy - Some Risks of General Factor ModelingMatheus PrenassiÎncă nu există evaluări
- The Strengths and Difficulties Questionnaire (SDQ)Document2 paginiThe Strengths and Difficulties Questionnaire (SDQ)Carla HortaÎncă nu există evaluări
- ADHD & Intellectual DisabilityDocument30 paginiADHD & Intellectual DisabilityAzkaNabilaÎncă nu există evaluări
- Challenges and Prospects of Inclusive EducationDocument20 paginiChallenges and Prospects of Inclusive EducationRawoofu NishaÎncă nu există evaluări
- ADHD - Group PresentationDocument28 paginiADHD - Group PresentationDhayaneeDruAinsleyII100% (1)
- Soc. Sci. 412: Understanding Human BehaviorDocument20 paginiSoc. Sci. 412: Understanding Human BehaviorClancy HernandezÎncă nu există evaluări
- Postpartum Psychiatric DisordersDocument26 paginiPostpartum Psychiatric DisordersSyakinah SabudinÎncă nu există evaluări
- DermatillomaniaDocument7 paginiDermatillomaniaSathish Rajamani100% (2)
- Doernberg e Hollander (2016) Neurodevelopmental Disorders Asd and Adhd Dsm5 Icd10 and Icd11Document5 paginiDoernberg e Hollander (2016) Neurodevelopmental Disorders Asd and Adhd Dsm5 Icd10 and Icd11MariaClaradeFreitasÎncă nu există evaluări
- Clarkin - Levy - Schiavi - Transference Focused Psychotherapy - 2005Document8 paginiClarkin - Levy - Schiavi - Transference Focused Psychotherapy - 2005Juan Carlos Garcia SanchezÎncă nu există evaluări
- Anxiety Disorders in WomenDocument52 paginiAnxiety Disorders in WomenZakkiyatus Zainiyah100% (1)
- Borderline Personality Disorder - Epidemiology, Pathogenesis, Clinical Features, Course, Assessment, and Diagnosis - UpToDateDocument33 paginiBorderline Personality Disorder - Epidemiology, Pathogenesis, Clinical Features, Course, Assessment, and Diagnosis - UpToDateAde GomezÎncă nu există evaluări
- Anxiety Disorders Are A Group ofDocument3 paginiAnxiety Disorders Are A Group ofLime MÎncă nu există evaluări
- Internet Addiction and Other BehaviorDocument12 paginiInternet Addiction and Other BehaviorsuckeydluffyÎncă nu există evaluări
- Sample: Personality Assessment Inventory™Document13 paginiSample: Personality Assessment Inventory™kdhfsj894Încă nu există evaluări
- Obsessive Compulsive DisorderDocument11 paginiObsessive Compulsive DisorderKeti ShalikashviliÎncă nu există evaluări