Documente Academic
Documente Profesional
Documente Cultură
Cardiac Diseases Complicate 1
Încărcat de
Rabani Abd AzizDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Cardiac Diseases Complicate 1
Încărcat de
Rabani Abd AzizDrepturi de autor:
Formate disponibile
Introduction Cardiac diseases complicate 1% to 4% of pregnancies in women without preexisting cardiac abnormalities.
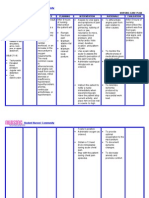
A working knowledge of the normal physiology of pregnancy is often helpful in the management of patients with heart disease. Patients with preexisting cardiac lesions should be counseled in advance about the risk of pregnancy. amiliarity with the treatment of commonly encountered cardiac diseases during pregnancy is becoming increasingly important for internists and cardiologists as they !oin the team of obstetricians and anesthesiologists in the care of these complicated patients. Normal physiologic changes during pregnancy "a!or hemodynamic alterations occur during pregnancy# labor# and delivery and the postpartum period $ %able 1 &. %hese changes begin to take place during the first ' to ( weeks of pregnancy and reach their peak late in the second trimester. )n patients with preexisting cardiac disease# cardiac decompensation often coincides with this peak. Table 1: Normal Hemodynamic Changes During Pregnancy Hemodynamic Parameter *lood volume /eart rate Cardiac output *lood pressure 2troke volume 2ystemic vascular resistance . Change During Change During Labor Change During Postpartum . $auto diuresis& . . . .
Normal Pregnancy and Delivery + 4,%-',% + + 1,-1' beats0min + + 1,%-',% above + Additional ',% baseline . 1,mm/g + + irst and second + $1,,trimesters3 . third ',,m40contraction& trimester . +
Maternal and etal !utcomes
)deally# women with preexisting cardiac lesions should discuss the impact of their heart condition on pregnancy well in advance of becoming pregnant. %hey should discuss contraception# maternal and fetal risks of pregnancy# and potential long-term maternal morbidity and mortality with their physician. Combined input from maternal fetal medicine specialists# the patient5s obstetrician# and a cardiologist may be a great asset in managing the pregnancy. Certain preexisting cardiac conditions carry an extremely high maternal risk. Pregnancy in these patients is not advised3 it is important for women with these conditions to understand the implications of pregnancy on their health. or example# women with a 67/A functional Class ))) or )8 heart condition face a mortality rate of 9% or higher and a morbidity rate higher than 1,% during pregnancy. A validated cardiac risk score has been shown to predict a woman5s chance of having adverse cardiac complications during pregnancy $ %able : &. ;ach risk factor was given a value of 1 point. %he maternal cardiac event rates for ,# 1# and higher than 1 points are '%# :9%# and 9'%# respectively. Table ": Predictors o# Maternal $is% #or Cardiac Complications Criteria Prior cardiac events Prior arrhythmia 67/A ))) or )8 or cyanosis 8alvular and outflow tract obstruction "yocardial dysfunction Aortic valve area = 1.' cm:# mitral valve area = : cm:# or left ventricular outflow tract peak gradient > 1, mm /g 48; = 4,%# restrictive cardiomyopathy# or hypertrophic cardiomyopathy &'ample /eart failure# transient ischemic attack# stroke before current pregnancy 2ymptomatic sustained tachyarrhythmia or bradyarrhythmia re<uiring treatment Points ( 1 1 1 1 1
?"aternal cardiac event rates for ,# 1# and >1 points are '%# :9%# and 9'%# respectively. LVEF, left ventricular ejection fraction; NYHA, New York Heart Association. Adapted from 2iu 2C# 2ermer "# Colman @"# et alA Prospective multicenter study of pregnancy outcomes in women with heart disease. Circulation :,,131,4A'1'-':1. Peripartum Cardiomyopathy &pidemiology and De#inition
Peripartum cardiomyopathy is a relatively rare but life-threatening disease. A wide variation in incidence rates ranging from 1 per 14(' to 1 per 1'#,,, live births has been reported although the currently accepted incidence is approximately 1 per 1,,, to 1 per 4,,, live births. 2urprisingly# a recent analysis of maternal mortality in 6orth Carolina reported at the :,,1 Annual 2BAP meeting found cardiomyopathy to be the leading cause of maternal death in that state. )t is unclear# however# if all these cases met the definition of peripartum cardiomyopathy or if some were related to preexisting heart disease. )dentified risk factors for peripartum cardiomyopathy include advanced maternal age# multiparity# obesity# multiple gestation# preeclampsia# chronic hypertension# and black race. *ased on a recent report from the 6ational /eart# 4ung# and *lood )nstitute# peripartum cardiomyopathy is defined by the presence of four criteria. %hese includeA $1& development of cardiac failure in the last month of pregnancy or within five months of delivery3 $:& absence of an identifiable cause for cardiac failure3 $1& absence of recogniCable heart disease prior to the last month of pregnancy3 and $4& left ventricular systolic dysfunction demonstrated by echocardiographic criteria such as depressed e!ection fraction. &tiology %he etiology of peripartum cardiomyopathy remains unknown despite much investigation that has focused on identifying a cause. Proposed causes include myocarditis# abnormal immune response to pregnancy# and maladaptive response to the hemodynamic stresses of pregnancy. %here is more evidence to support myocarditis or an autoimmune process as the cause of the disease than for other proposed etiologies. ;ndomyocardial biopsies in women with peripartum cardiomyopathy have demonstrated myocarditis in many patients but biopsy results differ markedly among studies. %he highest incidence of myocarditis reported was 9D%D but one of the most recent series found myocarditis in only (.(% of patients.
Diagnosis and Presentation
Patients with peripartum cardiomyopathy present with the typical signs and symptoms of left ventricular failure. %he ma!ority of cases occur after delivery and the immediate postpartum period. /owever# when the disease develops during the last month of pregnancy the diagnosis of cardiac failure is difficult to make by signs and symptoms alone since some of those symptoms# such as fatigue# orthopnea# and pedal edema# are common among normal parturients during late pregnancy. urther testing is re<uired to establish the presence of cardiac failure. A chest x-ray consistently demonstrates cardiomegaly and pulmonary edema. ;chocardiography confirms ventricular failure with increased left ventricular end-diastolic dimensions and decreased e!ection fraction. Bnce cardiac failure is identified# peripartum cardiomyopathy must be differentiated from other disease processes that lead to heart failure# such as valvular heart disease. Prognosis "aternal mortality from peripartum cardiomyopathy in the Enited 2tates has been reported to be :'-',%. %hromboembolism accounts for approximately 1,% of these deaths. Patients who survive the disease have a significantly higher e!ection fraction and smaller left ventricular end-diastolic diameter at the time of diagnosis compared with patients who succumb. 6ormaliCation of heart siCe and resolution of congestive heart failure within D months after delivery is also a good prognostic sign with mortality rare among these patients. %he incidence of resolution is unclear# however. An early series reported that ',% of patients experienced resolution but a more recent study reported only a 9% incidence of disease regression. %he ma!ority of patients in this recent series died# re<uired cardiac transplantation# or experienced continued cardiac impairment.Patients with peripartum cardiomyopathy re<uire counseling concerning the risks of subse<uent pregnancy. Patients without resolution of their cardiomyopathy are at significant risk for death or exacerbation of the disease and should be advised to avoid pregnancy. %here is no consensus on how to advise women whose cardiomyopathy has resolved. Bne of the earliest studies found that :'% of these patients experienced transient exacerbation during subse<uent pregnancy. An echocardiographic study found normal left ventricular function during and after pregnancy in patients who had previously recovered from peripartum cardiomyopathy. /owever# in a more recent study# patients who had a return to normal left ventricular function after peripartum cardiomyopathy still demonstrated impaired contractile reserve during a dobuatamine challenge test. %herefore# should these patients become pregnant# they should be cared for in collaboration with a high-risk obstetric center.
Medical and !bstetric Management "edical treatment of peripartum cardiomyopathy is similar to that for other dilated cardiomyopathies. "anagement goals include preload optimiCation# afterload reduction# and increased contractility. Anticoagulation is also considered in many patients because of the significant risk of thromboembolism. Fhen the patient develops cardiac failure before delivery# some treatment modifications are re<uired. Angiotensin-converting enCyme inhibitors are routinely used for afterload reduction in congestive heart failure. /owever# these drugs are contraindicated during pregnancy because of adverse fetal effects. Alternative treatments for afterload reduction during pregnancy include amlodipine or a combination of hydralaCine and nitroglycerin. )n addition to treatment of the cardiac failure# an obstetric plan of care must be developed when the disease occurs during pregnancy. Collaboration among the obstetrician# cardiologist# and anesthesiologist is essential to optimiCe care. )f the parturient5s cardiac status can be stabiliCed with medical therapy# induction of labor is usually recommended with cesarean section reserved for obstetric indications. /owever# in parturients who experience acute cardiac decompensation# cesarean delivery may be re<uired because of an inability of the mother to tolerate the prolonged stresses of labor.
The )tages o# Heart ailure * N+H, Classi#ication
)n order to determine the best course of of therapy# physicians often assess the stage of heart failure according to the 6ew 7ork /eart Association $67/A& functional classification system. %his system relates symptoms to everyday activities and the patient5s <uality of life.
Class Class ) $"ild&
Patient )ymptoms 6o limitation of physical activity. Brdinary physical activity does not cause undue fatigue# palpitation# or dyspnea $shortness of breath&.
Class )) $"ild&
2light limitation of physical activity. Comfortable at rest# but ordinary physical activity results in fatigue# palpitation# or dyspnea.
Class ))) $"oderate& Class )8 $2evere&
"arked limitation of physical activity. Comfortable at rest# but less than ordinary activity causes fatigue# palpitation# or dyspnea. Enable to carry out any physical activity without discomfort. 2ymptoms of cardiac insufficiency at rest. )f any physical activity is undertaken# discomfort is increased.
Hypertensive emergencies /ypertensive emergencies are severe elevations in *P# often higher than ::,014, mm /g# complicated by clinical evidence of progressive target organ dysfunction. %hese patients re<uire immediate admission and *P reduction $not necessarily to normal ranges& to prevent or limit further target organ damage. ;xamples include hypertensive encephalopathy# intracranial hemorrhage# acute myocardial infarction# acute left ventricular failure with pulmonary edema# dissecting aneurysm# acute renal failure# and eclampsia of pregnancy. )mmediate admission to a monitored unit and parenteral antihypertensive therapy are indicated. )t is the clinical state of the patientGin particular# the degree of and0or progression of target organ damageGHthat defines a hypertensive emergency and not the absolute level of blood pressure. 2evere hypertension $urgencies& are marked elevations of *P# usually higher than 1(,011, mm /g. ;vidence of target organ damage is often present# but nonprogressive and manifesting symptoms may include headache# shortness of breath# and pedal edema. "anagement in the emergency department $;I& with oral agents is suitable# depending on the individual5s presentation# and follow-up within :4 to 9: hours is recommended. )n many cases# with blood pressure higher than 1(,011, mm /g# patients present without clinical symptoms and have no clinical evidence of target organ damage. )f untreated# they may be initiated on a two-drug regimen or an existing treatment regimen may be modified. ;motional distress or nonadherence with prior treatment are often at fault. %hese patients do not re<uire *P reduction to normal and# after brief observation in the emergency room# can be discharged# with follow-up scheduled within 1 to 9 days. )igns and )ymptoms /ypertension# papilledema# retinal hemorrhages and exudate# severe headache# vomiting# vision disturbances# transient paralysis# seiCures# stupor# coma Treatment 6itroprusside# nitroglycerin# diaCoxide# hydralaCine# methyldopa
Medication Ni#edipine used over the last decade for both tocolysis and management of hypertension in pregnancy An unusual characteristic is that the higher the *P# the further it decreases after nifedipine administration A small randomiCed trial of ', pregnant women# oral nifedipine controls hypertension more rapidly than intravenous labetalol# as early as 1 hr after the initial administration Acts as a selective renal arteriolar vasodilator and natriuretic# with a significant increase in urinary output nifedipine increases cardiac index lowers *P without reducing uteroplacental blood flow and without significant fetal heart rate abnormalities reports of unpredictable decreases in blood pressure As a result of this unfavorable publicity# short-acting nifedipine $capsules& was withdrawn from some national markets $Australia& as well as from many hospital pharmacies in the Enited 2tates Hydrala-ine Peripheral arteriolar vasodilator Irug used for >4' yrs in the treatment of severe hypertension in pregnancy Bnset of action is relatively slow $1,H:, mins& Common side effectsA $',%& reflex tachycardia# hypotension# headaches# palpitations# flushing# anxiety# tremors# vomiting# epigastric pain# and fluid retention )n the neonate# thrombocytopenia and a lupus-like syndrome have been reported after maternal use in third trimester A recent meta-analysis concluded that hydralaCine may not be the best first-line drug for treatment of severe hypertension in pregnancy 4ess effective than nifedipine# e<ually effective to labetalol# but associated with poorer maternal and perinatal outcomes "ore poorly tolerated than other antihypertensives
P,TI&NT P$! IL&
Patient profileA JahfiCah bt Kasim Jegistration noA 1:D'1'11 )0card noA 91,':41,'14, Iate of birthA :4.,'.1L91 JaceA malayu AgeA 1' ;ducation levelA 2pm BccupationA ;xecutive "arital statusA :,.(.1LL' Mravida N ParaA M'P4 46"PA ,D.,L.,( ;IIA 11.,D.,L /usband nameA Ahmad 6adCri Bthman )0Card noA 91,114,D'1,1 Iate of birthA 14.1.1L91 BccupationA Iriver AddressA 6o 9-,-4# Kelumpuk "awar#!ln 1D0'D#K
*)4 7;AJ
M;2%A%)B6
P4AC; B I;4)8)J7
4ABEJ0 I;4)8;J7
CB"P4)CA%)B6
F%
2;Q
*J;2% ;I 7;206B
CB"";6%2
1LLD
%erm06P
"/K4
28I
60PE;JP
:.LLKM *B7
:01:
A4)8; R F;44
1LL(
%erm06P
"/K4
28I
60PE;JP
1.:KM
*B7
:01:
A4)8; R F;44
1LLL
%erm06P
"/K4
28I
60PE;JP
:.('KM *B7
:01:
A4)8; R F;44
:,,1
%erm06P
"/K4
42C2 BJ *J;;C/
60PE;JP
1.4KM
M)J4 401:
A4)8; R F;44
'
:,,L
PJ;M6A6C7
,.P,)T !/)&T$IC,L HI)T!$+ P,)T !/)&T$IC,L HI)T!$+ )n :,,1 "adam JahfiCah was complained that she feel tired when walking3 do house work after ' month delived but its relief after she take a rest. Iay to day she feel gastric pain and come to see the doctor. 1st time madam JahfiCah come see the doctor has been diagnose "adam JahfiCah having some mild gastric problem. "adam JahfiCah for :nd time coming to /EK" to see doctor with the same problem and the doctor has do some ;C/B to "adam JahfiCah and other medical chekup was findi that she has a heart problem Operipartum cardiomyopathyP Ioctor has give some advised to "adam JahfiCah to do *ilateral %ubal 4igation due to risk to mother and baby if she gets pregnant with this condition. *ut "adam JahfiCah has delayed to do *%4 until she become pregnant again.
M&N)T$0,L HI)T!$+ "adam rahfiCah was menarche at 1: years old %he period was regular at 1-4 days in :( days cycle M&DIC,L HI)T!$+ 6o any medical problem. )0$1IC,L HI)T!$+ 6o any surgical has been done. ,MIL+ HI)T!$+ "adam JahfiCah mother has hypertension and Iiabetis. ,NT&N,T,L CH&C20P 12% booking was at the /ospital Eniversity Kebangsaan "alaysia D !anuary :,,L S 190': R 109 "adam JahfiCah has re<uest to have a checkup at /ospital Kuala 4umpur. "adam JahfiCah has been diagnosed Post partum Iilated Cardiomyopathy and 67/A )).
S-ar putea să vă placă și
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Chest Pain. Surgical Treatment of Acute Coronary Syndrome (ACS)Document21 paginiChest Pain. Surgical Treatment of Acute Coronary Syndrome (ACS)Hanif ZamriÎncă nu există evaluări
- Concept Map Joshua ValdrizDocument1 paginăConcept Map Joshua ValdrizJoshua ValdrizÎncă nu există evaluări
- Differential Diagnosis of StrokeDocument2 paginiDifferential Diagnosis of Strokeamna_badar1Încă nu există evaluări
- ##Default - Genres.article## 28348 2 10 20210116Document14 pagini##Default - Genres.article## 28348 2 10 20210116Vega VirlyÎncă nu există evaluări
- CALIXRO, LJ NARRATIVE Ventricular Septal DefectDocument2 paginiCALIXRO, LJ NARRATIVE Ventricular Septal DefectKim SunooÎncă nu există evaluări
- Exam #4 Study Blueprint 2019Document2 paginiExam #4 Study Blueprint 2019Stephanie DeeÎncă nu există evaluări
- NCP AnginaDocument3 paginiNCP AnginaShie LA100% (1)
- ECG Made Easy - A Slow Turtle VsDocument37 paginiECG Made Easy - A Slow Turtle VsabdallahÎncă nu există evaluări
- Common Pediatric Arrhythmias Congestive Heart Failure and HypertensionDocument65 paginiCommon Pediatric Arrhythmias Congestive Heart Failure and HypertensionNakul SrivastavaÎncă nu există evaluări
- Basic Arrythmias: Prof. Maximin A. Pomperada, RN, MNDocument70 paginiBasic Arrythmias: Prof. Maximin A. Pomperada, RN, MNRellie CastroÎncă nu există evaluări
- CardiomyopathyDocument93 paginiCardiomyopathyAbnet WondimuÎncă nu există evaluări
- Congenital Heart Disease Sounds MP3sDocument2 paginiCongenital Heart Disease Sounds MP3ssra1_103Încă nu există evaluări
- Heart Valve Problems and Homeopathy - (50 PP)Document50 paginiHeart Valve Problems and Homeopathy - (50 PP)Marcelo Guerra100% (1)
- Acute Inferior Myocardial Infarction - ARTICLEDocument4 paginiAcute Inferior Myocardial Infarction - ARTICLEJonathan MorenoÎncă nu există evaluări
- Correlation of Brachial Flow Mediated Dilation With Severity of Coronary Artery DiseaseDocument8 paginiCorrelation of Brachial Flow Mediated Dilation With Severity of Coronary Artery DiseaseNaya MeoOnGÎncă nu există evaluări
- Differentiate Between: Defibrillation CardioversionDocument3 paginiDifferentiate Between: Defibrillation CardioversionStephy SojanÎncă nu există evaluări
- MTB Cardiology NotesDocument7 paginiMTB Cardiology Noteskabal321Încă nu există evaluări
- The Ehra Book of Intervntional Electrophysiology - OxfordDocument321 paginiThe Ehra Book of Intervntional Electrophysiology - Oxfordmorris njageÎncă nu există evaluări
- Truncus ArteriosusDocument4 paginiTruncus ArteriosuskemalahmadÎncă nu există evaluări
- Point-Of-Care Ultrasound in Cardiac ArrestDocument13 paginiPoint-Of-Care Ultrasound in Cardiac ArrestEgorSazhaevÎncă nu există evaluări
- ACLS Megacode Checklist For StudentsDocument3 paginiACLS Megacode Checklist For StudentsKhrisha Anne DavilloÎncă nu există evaluări
- Abnoramal ECGDocument20 paginiAbnoramal ECGImmanuelÎncă nu există evaluări
- OSCE Master List - CardiologyDocument10 paginiOSCE Master List - CardiologyRebecca WongÎncă nu există evaluări
- Position Paper: A B C D e F G H CDocument11 paginiPosition Paper: A B C D e F G H CNico IonaşcuÎncă nu există evaluări
- Newborn Screening For Critical Congenital Heart Disease Using Pulse OximetryDocument20 paginiNewborn Screening For Critical Congenital Heart Disease Using Pulse OximetryHardian RakhmawardanaÎncă nu există evaluări
- Workshop Apsc 2018 1Document4 paginiWorkshop Apsc 2018 1Maria BelladonnaÎncă nu există evaluări
- Edward K. Chung M.D., F.A.C.P., F.A.C.C. (Auth.) - Ambulatory Electrocardiography - Holter Monitor Electrocardiography-Springer-Verlag New York (1979)Document236 paginiEdward K. Chung M.D., F.A.C.P., F.A.C.C. (Auth.) - Ambulatory Electrocardiography - Holter Monitor Electrocardiography-Springer-Verlag New York (1979)Henrique MaiaÎncă nu există evaluări
- Modifiable Risk Factors Non - Modifiable Risk Factors: LegendDocument2 paginiModifiable Risk Factors Non - Modifiable Risk Factors: LegendWendy Escalante100% (1)
- Soal 5Document31 paginiSoal 5Agustinus FatollaÎncă nu există evaluări
- Decompensated Congestive Cardiac Failure Secondary To No1Document4 paginiDecompensated Congestive Cardiac Failure Secondary To No1Qi YingÎncă nu există evaluări