Documente Academic
Documente Profesional
Documente Cultură
Myocardial Infarction
Încărcat de
larissedeleonDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Myocardial Infarction
Încărcat de
larissedeleonDrepturi de autor:
Formate disponibile
DE LEON, MARIA LARISSE S. BSN IV A-04 MR. ADRIAN M.
LAWSIN CASE 6: MYOCARDIAL INFARCTION
1. What do you think are the factors which predisposed Mrs. Mendoza into experiencing acute myocardial infarction? Explain the rationale behind each predisposing factor. Age Sex: At any given age, men are more at risk than women, particularly before menopause, but because in general women live longer than men, ischemic heart disease causes slightly more total deaths in women. Diabetes mellitus (type 1 or 2) High blood pressure Dyslipidemia/hypercholesterolemia (abnormal levels of lipoproteins in the blood), particularly high low-density lipoprotein, low high-density lipoprotein and high triglycerides Tobacco smoking, including secondhand smoke Family history of ischaemic heart disease or MI, particularly if one has a first-degree relative (father, brother, mother, sister) who suffered a 'premature' myocardial infarction (defined as occurring at or younger than age 55 years (men) or 65 (women) Obesity (defined by a body mass index of more than 30 kg/m, or alternatively by waist circumference or waist-hip ratio). Lack of physical activity Psychosocial factors including, low socioeconomic status, social isolation, negative emotions and stress increase the risk of and are associated with worse outcomes after MI. Socioeconomic factors such as a shorter education and lower income (particularly in women), and unmarried cohabitation are also correlated with a higher risk of MI. Alcohol prolonged exposure to high quantities of alcohol can increase the risk of heart attack. Oral contraceptive pill women who use combined oral contraceptive pills have a modestly increased risk of myocardial infarction, especially in the presence of other risk factors, such as smoking. Hyperhomocysteinemia (high homocysteine) in homocysteinuria is associated with premature atherosclerosis, whether elevated homocysteine in the normal range is causal is contentious 2. Aside from the manifestations experienced by Mrs. Mendoza, what are the other clinical manifestations of acute MI? Chest pain that occurs suddenly and continues despite rest and medication is the primary presenting symptoms Patients may present with a combination of symptoms, including chest pain, shortness of breath, indigestion, nausea and anxiety.
Patient may have cool, pale and moist skin; heart rate and respiratory rate may be faster than normal. These symptoms, which are caused by stimulation of the sympathetic nervous system, may be present for only short time or may persist.
3. Differentiate angina pectoris from acute myocardial infarction in terms of its pathophysiology, chest pain, manifestation and diagnosis. ANGINA PECTORIS MYOCARDIAL INFARCTION Myocardial cells become Complete of nearly complete PATHOPHYSIOLOGY ischemic within 10 sec. of occlusion of coronary artery (due coronary artery occlusion -> to rupture of atherosclerotic decrease pumping action of the plaque -> thrombus or embolus ; heart (after several mins.) -> vasospasm; decrease oxygen decrease blood supply (glucose supply; or increase demand of and oxygen) -> decrease ATP oxygen) -> profound imbalance production -> anaerobic between oxygen supply and metabolism -> production of demand -> ischemia -> infarction lactic acid (acidosis) -> pain (cell death) after 15 mins. Squeezing, pressing and Severe, sudden in onset, crushing, CHEST PAIN burning at the left retrosternal heaviness and tightness at the or substernal area radiating to substernal area radiating to arms, arms and shoulders . jaw and neck. Not relived by nitroglycerin Weakness, numbness (arms, Dyspnea, tachypnea, crackles MANIFESTATION wrists and hands), shortness of (pulmonary congestion), pallor breath, pallor, diaphoresis, diaphoresis, decrease urinary dizziness, nausea and vomiting, output, increase PR, dizziness, severe apprehension and restlessness, anxiety and feelings of impending death. impending doom. 4. Discuss the management of clients suffering from AMI. Include the pharmacologic management, treatments or other invasive procedures with their corresponding nursing considerations. Antiplatelet drug therapy such as aspirin and/or clopidogrel should be continued to reduce the risk of plaque rupture and recurrent MI. Aspirin is first-line, owing to its low cost and comparable efficacy, with clopidogrel reserved for patients intolerant of aspirin. The combination of clopidogrel and aspirin may further reduce risk of cardiovascular events, but the risk of hemorrhage is increased. Beta blocker therapy such as metoprolol or carvedilol should be commenced.[78] These have been particularly beneficial in high-risk patients such as those with left ventricular dysfunction and/or continuing cardiac ischaemia. -Blockers decrease mortality and morbidity. They also improve symptoms of cardiac ischemia in NSTEMI. ACE inhibitor therapy should be commenced 2448 hours after MI in hemodynamically stable patients, particularly in patients with a history of MI, diabetes mellitus, hypertension, anterior location of infarct (as assessed by ECG), and/or evidence
of left ventricular dysfunction. ACE inhibitors reduce mortality, the development of heart failure, and decrease ventricular remodelling. Statin therapy has been shown to reduce mortality and morbidity. The effects of statins may be more than their LDL lowering effects. The general consensus is that statins have plaque stabilization and multiple other ("pleiotropic") effects that may prevent myocardial infarction in addition to their effects on blood lipids. The aldosterone antagonist agent eplerenone has been shown to further reduce risk of cardiovascular death after MI in patients with heart failure and left ventricular dysfunction, when used in conjunction with standard therapies above. Spironolactone, another option, is sometimes preferable to eplerenone due to cost. Giving heparin to people with heart conditions like unstable angina and some forms of heart attacks reduces the risk of having another heart attack. However, heparin also increases the chance of minor bleeding.
An MI requires immediate medical attention. Treatment attempts to salvage as much myocardium as possible and to prevent further complications, hence the phrase "time is muscle". Oxygen, aspirin, and nitroglycerin may be administered. Morphine was classically used if nitroglycerin was not effective; however, it may increase mortality in the setting of NSTEMI. Reviews of high flow oxygen in myocardial infarction found increased mortality and infarct size, calling into question the recommendation about its routine use. Other analgesics such as nitrous oxide are of unknown benefit. Early treatment of heart attack patients with an inexpensive beta-blocker drug called metoprolol, while in transit to the hospital, can significantly reduce damage to the heart during an MI. STEMI Percutaneous coronary intervention (PCI) is the treatment of choice for STEMI if it can be performed in a timely manner. If PCI cannot be performed within 90 to 120 minutes then fibrinolysis, preferably within 30 minutes, is recommended. If after fibrinolysis, significant cardiogenic shock, continued severe chest pain, or less than a 50% improvement in ST elevation after 90 minutes occurs, then rescue PCI is indicated emergently. After PCI, people are generally placed on dual antiplatelet therapy for at least a year (which is generally aspirin and clopidogrel).
5. Explain the rationale behind the administration of streptokinase, heparin and nitroglycerin when giving these medications? Streptokinase: promotes fibrinolytic mechanism by converting plasminogen to plasmin that destroys the fibrin in the blood clot. It should be administered within 4-6 hours after acute MI. Heparin: This medication is used to prevent and treat blood clots. It is also known as anticoagulant. It is started before terminations of thrombolytics. Monitor aPTT. Nitroglycerin: prevent angina caused by coronary disease. This medicine is also to relieve an angina attack that is already occurring.
6. When AMI becomes severe there might be a need for the client to undergo coronary artery bypass graft (CABG). Postoperatively after CABG, client are at risk for developing cardiac tamponade. Discuss the pathophysiology and management of cardiac tamponade. The outer layer of the heart is made of fibrous tissue which does not easily stretch, and so once fluid begins to enter the pericardial space, pressure starts to increase.If fluid continues to accumulate, then with each successive diastolic period, less and less blood enters the ventricles, as the increasing pressure presses on the heart and forces the septum to bend into the left ventricle, leading to decreased stroke volume. This causes obstructive shock to develop, and if left untreated then cardiac arrest may occur (in which case the presenting rhythm is likely to be pulseless electrical activity). Pre-hospital care Initial treatment given will usually be supportive in nature, for example administration of oxygen, and monitoring. There is little care that can be provided pre-hospital other than general treatment for shock. A number of the Helicopter Emergency Medical Services (HEMS) in the UK, which have doctor/paramedic teams, have performed an emergency thoracotomy to release clotting in the pericardium caused by a penetrating chest injury. Prompt diagnosis and treatment is the key to survival with tamponade. Some pre-hospital providers will have facilities to provide pericardiocentesis, which can be life-saving. If the patient has already suffered a cardiac arrest, pericardiocentesis alone cannot ensure survival, and so rapid evacuation to a hospital is usually the more appropriate course of action. Hospital management Initial management in hospital is by pericardiocentesis. This involves the insertion of a needle through the skin and into the pericardium and aspirating fluid under ultrasound guidance preferably. This can be done laterally through the intercostal spaces, usually the fifth, or as a subxiphoid approach. Often, a cannula is left in place during resuscitation following initial drainage so that the procedure can be performed again if the need arises. If facilities are available, an emergency pericardial window may be performed instead, during which the pericardium is cut open to allow fluid to drain. Following stabilization of the patient, surgery is provided to seal the source of the bleed and mend the pericardium. In heart surgery patients post op, the nurses monitor the amount of chest tube drainage. If the drainage volume drops off, and the blood pressure goes down, this can suggest tamponade due to chest tube clogging. In that case, the patient is taken back to the operating room for an emergency reoperation. If aggressive treatment is offered immediately and no complications arise (shock, AMI or arrhythmia, heart failure, aneurysm, carditis, embolism, or rupture), or they are dealt with quickly and fully contained, then adequate survival is still a distinct possibility.
S-ar putea să vă placă și
- Nutrition in PregnancyDocument60 paginiNutrition in PregnancylarissedeleonÎncă nu există evaluări
- Care of Patients With Neurological DisordersDocument82 paginiCare of Patients With Neurological Disorderslarissedeleon100% (1)
- MNT in Diabetes and Related Disorders and StrategiesDocument122 paginiMNT in Diabetes and Related Disorders and StrategieslarissedeleonÎncă nu există evaluări
- NCM 102 Power and PsycheDocument13 paginiNCM 102 Power and Psychelarissedeleon100% (1)
- Pathophysiology FinalDocument2 paginiPathophysiology FinallarissedeleonÎncă nu există evaluări
- NCM 102 Post Partal Complications HemorrhageDocument10 paginiNCM 102 Post Partal Complications HemorrhagelarissedeleonÎncă nu există evaluări
- Pre Gestational ConditionsDocument17 paginiPre Gestational Conditionslarissedeleon100% (2)
- NCM 102 - Anesthesia and AnalgesiaDocument3 paginiNCM 102 - Anesthesia and AnalgesialarissedeleonÎncă nu există evaluări
- Prolonged Labor Complications and Fetal MalpositionsDocument9 paginiProlonged Labor Complications and Fetal Malpositionslarissedeleon100% (1)
- NCM 102 - High Risk NewbornDocument4 paginiNCM 102 - High Risk NewbornlarissedeleonÎncă nu există evaluări
- COMDISEASEDocument39 paginiCOMDISEASElarissedeleonÎncă nu există evaluări
- NCM 102 Puerperal InfectionDocument8 paginiNCM 102 Puerperal InfectionlarissedeleonÎncă nu există evaluări
- CA 2 LMR Handout 2s1314Document8 paginiCA 2 LMR Handout 2s1314larissedeleonÎncă nu există evaluări
- Acute TonsillopharyngitisDocument13 paginiAcute TonsillopharyngitislarissedeleonÎncă nu există evaluări
- CVD Infarct-HpniiDocument3 paginiCVD Infarct-HpniilarissedeleonÎncă nu există evaluări
- PRC Cases FormDocument4 paginiPRC Cases FormlarissedeleonÎncă nu există evaluări
- Ca1 - Coronary Artery Bypass GraftDocument5 paginiCa1 - Coronary Artery Bypass GraftlarissedeleonÎncă nu există evaluări
- NursesDocument2 paginiNursesDhingskie100% (5)
- Ketoacidosis, DysrhythmiasDocument39 paginiKetoacidosis, DysrhythmiaslarissedeleonÎncă nu există evaluări
- Cervical Cancer 2.0Document9 paginiCervical Cancer 2.0larissedeleonÎncă nu există evaluări
- Chapters15 20&24Document64 paginiChapters15 20&24larissedeleonÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Jazan Refinery and Terminal ProjectDocument3 paginiJazan Refinery and Terminal ProjectkhsaeedÎncă nu există evaluări
- Chapter 2Document22 paginiChapter 2Okorie Chinedu PÎncă nu există evaluări
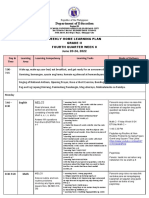
- Department of Education: Weekly Home Learning Plan Grade Ii Fourth Quarter Week 8Document8 paginiDepartment of Education: Weekly Home Learning Plan Grade Ii Fourth Quarter Week 8Evelyn DEL ROSARIOÎncă nu există evaluări
- Abinisio GDE HelpDocument221 paginiAbinisio GDE HelpvenkatesanmuraliÎncă nu există evaluări
- What is zone refining processDocument1 paginăWhat is zone refining processKeshav MadanÎncă nu există evaluări
- Supplier GPO Q TM 0001 02 SPDCR TemplateDocument6 paginiSupplier GPO Q TM 0001 02 SPDCR TemplateMahe RonaldoÎncă nu există evaluări
- Um 0ah0a 006 EngDocument1 paginăUm 0ah0a 006 EngGaudencio LingamenÎncă nu există evaluări
- APC Smart-UPS 1500VA LCD 230V: Part Number: SMT1500IDocument3 paginiAPC Smart-UPS 1500VA LCD 230V: Part Number: SMT1500IDesigan SannasyÎncă nu există evaluări
- Victron MultiPlus 48 1200-13-16 Datasheet enDocument1 paginăVictron MultiPlus 48 1200-13-16 Datasheet enBAHJARI AMINEÎncă nu există evaluări
- Brain, Behavior, and Immunity: Alok Kumar, David J. LoaneDocument11 paginiBrain, Behavior, and Immunity: Alok Kumar, David J. LoaneRinaldy TejaÎncă nu există evaluări
- Robocon 2010 ReportDocument46 paginiRobocon 2010 ReportDebal Saha100% (1)
- Environment ManagerDocument234 paginiEnvironment ManagerAbhishek kumarÎncă nu există evaluări
- NOTE CHAPTER 3 The Mole Concept, Chemical Formula and EquationDocument10 paginiNOTE CHAPTER 3 The Mole Concept, Chemical Formula and EquationNur AfiqahÎncă nu există evaluări
- Numerical Methods: Jeffrey R. ChasnovDocument60 paginiNumerical Methods: Jeffrey R. Chasnov2120 sanika GaikwadÎncă nu există evaluări
- Clogging in Permeable (A Review)Document13 paginiClogging in Permeable (A Review)Chong Ting ShengÎncă nu există evaluări
- Reservoir Rock TypingDocument56 paginiReservoir Rock TypingAffan HasanÎncă nu există evaluări
- Recycle Used Motor Oil With Tongrui PurifiersDocument12 paginiRecycle Used Motor Oil With Tongrui PurifiersRégis Ongollo100% (1)
- Planview Innovation Management Maturity Model PDFDocument1 paginăPlanview Innovation Management Maturity Model PDFMiguel Alfonso Mercado GarcíaÎncă nu există evaluări
- Artificial IseminationDocument6 paginiArtificial IseminationHafiz Muhammad Zain-Ul AbedinÎncă nu există evaluări
- ROM Flashing Tutorial For MTK Chipset PhonesDocument5 paginiROM Flashing Tutorial For MTK Chipset PhonesAriel RodriguezÎncă nu există evaluări
- Easa Ad Us-2017-09-04 1Document7 paginiEasa Ad Us-2017-09-04 1Jose Miguel Atehortua ArenasÎncă nu există evaluări
- MMW FinalsDocument4 paginiMMW FinalsAsh LiwanagÎncă nu există evaluări
- Russian Tea Market Growth and Brand PreferenceDocument6 paginiRussian Tea Market Growth and Brand PreferenceKing KhanÎncă nu există evaluări
- Land Measurement in PunjabDocument3 paginiLand Measurement in PunjabJunaid Iqbal33% (3)
- C Exam13Document4 paginiC Exam13gauravsoni1991Încă nu există evaluări
- Lesson 2 Mathematics Curriculum in The Intermediate GradesDocument15 paginiLesson 2 Mathematics Curriculum in The Intermediate GradesRose Angel Manaog100% (1)
- Programming Language Foundations PDFDocument338 paginiProgramming Language Foundations PDFTOURE100% (2)
- Vidura College Marketing AnalysisDocument24 paginiVidura College Marketing Analysiskingcoconut kingcoconutÎncă nu există evaluări
- Political Reporting:: Political Reporting in Journalism Is A Branch of Journalism, Which SpecificallyDocument6 paginiPolitical Reporting:: Political Reporting in Journalism Is A Branch of Journalism, Which SpecificallyParth MehtaÎncă nu există evaluări
- IMT Ghaziabad PGDM Timetable Term II 2020Document22 paginiIMT Ghaziabad PGDM Timetable Term II 2020Ved JhingranÎncă nu există evaluări