Documente Academic
Documente Profesional
Documente Cultură
Acls 2013
Încărcat de
rjavillarDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Acls 2013
Încărcat de
rjavillarDrepturi de autor:
Formate disponibile
ACLS123.
com
818.766.1111
!"#!
!"#$#%&' !&") *"&#+#+, !)+$)"
12/1/2012
ACLS Stuuy uuiue
Course Overview
This study guide is an outline of content that will be taught in the
American Heart Association Accredited Advance Cardiac Life Support
(ACLS) Course. It is intended to summarize important content, but since
all ACLS content cannot possibly be absorbed in a class given every two
years, it is expected that the student will have the 2010 Updated ECC
Handbook readily available for review as a reference. The student is also
required to have the AHA ACLS Textbook available for reference and
study for more in depth content.
Evidence Based Updates
Approximately every 5 years the AHA updates the guidelines for CPR
and Emergency Cardiovascular Care. These updates are necessary to
ensure that all AHA courses contain the best information and
recommendations that can be supported by current scientific evidence
experts from outside the United States and outside the AHA. The
guidelines were then classified as to the strength of evidence that
supports the recommendation.
The BLS Survey
C A - B
Assess Assessment Technique and Action
1 Check Responsiveness
Tap and shout, Are you all right?
Check for absent or abnormal breathing (no breathing or only gasping) by
looking at or scanning the chest for movement (about 5 to 10 seconds)
2
Activate the Emergency
Response System /get
AED
Activate the emergency response system and get an AED if one is available
or send someone to activate the emergency response system and get an
AED or defibrillator
3 Circulation
Check the carotid pulse for 5 to 10 seconds
If no pulse within 10 seconds, start CPR (30:2) beginning with chest
compressions
Compress the center of the chest (lower half of the sternum) hard and fast
with at least 100 compressions per minute at a depth of at least 2 inches
Allow complete chest recoil after each compression
Minimize interruptions in compressions (10 seconds or less)
Switch providers about every 2 minutes to avoid fatigue
Avoid excessive ventilation
If there is a pulse, start rescue breathing at 1 breathe every 5 to 6 seconds (10
to 12 breaths per minute). Check pulse about every 2 minutes.
4 Defibrillation
If no pulse, check for a shockable rhythm with an AED/defibrillator as soon
as it arrives
Provide shocks immediately with CPR, beginning with compressions
!"#$#%&' !-+%).$/ 0
1#,2 34&'#$5 !67
Compress Lhe chesL hard and fasL
Allow compleLe chesL recoll afLer
each compresslon
Mlnlmlze lnLerrupLlons ln
compresslons (10 seconds or less)
SwlLch provlders abouL every 2
mlnuLes Lo avold faLlgue
Avold excesslve venLllaLlon
The ACLS Survey
For unconscious patients in arrest (cardiac or respiratory):
Healthcare providers should conduct the ACLS Survey after completing the BLS
survey.
For conscious patients who may need more advanced assessment and management technique:
Health providers should conduct the ACLS Survey first.
An important component of this survey is the differential diagnosis, where identification and
treatment of the underlying causes may be critical to patient outcome.
Effective Resuscitation Team Dynamics
Role of the Team Leader is multifaceted. The team leader
Organizes the group
Monitors individual performance of team members
Back up team members
Models excellent team behavior
Trains and coaches
Facilitates understanding
Focuses on comprehensive patient care
Role of Team Member must be proficient in performing the skills authorized by their scope of
practice.
Clear about role assignment
Prepared to fulfill their role responsibilities
Well practiced in resuscitation skills
Knowledgeable about the algorithms
Committed to success
! Closed Loop Communications When communicating with resuscitation team members, the
team leader should use closed loop communication by taking these steps
The team leader gives a message, order, or assignment to a team member
By receiving a clear response and eye contact, the team leader confirms that the team
member heard and understood the message
The team leader listens for confirmation of task performance from the team
before assigning another task.
! Clear Messages Clear messages consist of concise communication spoke with distinctive
speech in a controlled tone of voice. All healthcare providers should deliver messages and
order in a calm and direct manner without yelling or shouting. Unclear communication can
lead to unnecessary delays in treatment or to medication errors.
! Clear Roles and Responsibilities Every member of the team should know his or her role and
responsibilities. Just as different shaped pieces make up a jigsaw puzzle, each team members
role is unique and critical to the effective performance of the team. When roles are unclear,
team performance suffers. Signs of unclear roles include:
Performing the same task more than once
Missing essential tasks
Freelancing of team members
! Knowing Ones Limitations Not only should everyone on the team know his or her own
limitations and capabilities, but the team leader should also be aware of them. This allows the
team leader to evaluate team resources and call for backup of team members when assistance is
needed.
! Knowledge Sharing Sharing information is a critical component of effective team
performance. Team leaders may become trapped in a specific treatment of diagnostic approach;
this common human error is called a fixation error.
! Constructive Intervention During a resuscitation attempt the team leader or a team member
may need to intervene if an action that is about to occur may be inappropriate at the time.
Although constructive intervention is necessary, it should be tactful.
! Reevaluation and Summarizing An essential role of the team leader is monitoring and
reevaluating
The patients status
Interventions that have been performed
Assessment findings
! Mutual Respect - The best teams are composed of members who share a mutual respect for
each other and work together in a collegial, supportive manner. To have a high-performing
team, everyone must abandon ego and respect each other during the resuscitation attempt,
regardless of any additional training or experience that the team leader or specific team member
may have.
System of Care
Medical Emergency Teams (METs) and Rapid Response Teams (RRTs)
! Many hospitals have implemented the use of METs or RRTs. The purpose of these
teams is to improve patient outcomes by identifying and treating early clinical
deterioration. In-hospital cardiac arrest is commonly preceded by physiologic changes.
In one study nearly 80% of hospitalized patients with cardiorespiratory arrest had
abnormal vital signs documented for up to 8 hours before the actual arrest. Many of
these changes can be recognized by monitoring routine vital signs. Intervention before
clinical deterioration or cardiac arrest may be possible.
! Consider this question: Would you have done anything differently if you knew 15
minutes before the arrest that .?
The ACLS Survey
Airway Management in Respiratory Arrest If bag-mask ventilation is adequate, providers
may defer insertion of an advanced airway Healthcare providers should make the decision to
place an advanced airway during the ACLS Survey.
Advanced airway equipment includes the laryngeal mask airway, the laryngeal tube, the
esophageal-tracheal tube and the ET tube. If it is within your scope of practice, you may use
advanced airway equipment in the course when appropriate and available.
Basic Airway Adjuncts: Oropharyngeal Airway
The OPA is used in patients who are at risk for developing airway obstruction from the
tongue or from relaxed upper airway muscle. This J-shaped device fits over the tongue to
hold it and the soft hypopharyngeal structures away from the posterior wall of the pharynx.
34&+$#$&$#8) 9&8):-";
%&.+-,"&.25 <#: 6=*!>? #/ @AB;;
1,C &$$);.$ $- #;."-8) !67 D4&'#$5E
The OPA is used in unconscious patients if procedures to open
the airway fail to provide and maintain a clear, unobstructed
airway. An OPA should not be used in a conscious or
semiconscious patient because it may stimulate gagging and
vomiting. The key assessment is to check whether the patient
has an intact cough and gag reflex. If so, do not use an OPA.
Basic Airway Adjuncts: Nasopharyngeal Airway
The NPA is used as an alternative to an OPA in patients who
need a basic airway management adjunct. The NPA is a soft
rubber or plastic uncuffed tube that provides a conduit for
airflow between the nares and the pharynx.
Unlike oral airway, NPAs may be used in conscious or
semiconscious patients (patients with an intact cough and gag
reflex). The NPA is indicated when insertion of an OPA is
technically difficult or dangerous.
Suctioning
Suctioning is an essential component of maintaining a patients
airway. Providers should suction the airway immediately if
there are copious secretions, blood, or vomit.
Suctioning attempted should not exceed 10 seconds. To avoid
hypoxemia, precede and follow suctioning attempts with a
short period of administration of 100% oxygen.
SELEC TI Nu TBE P R0P ER S I ZE
0PA
lace Lhe CA agalnsL
Lhe slde of Lhe face.
When Lhe Llp of Lhe
CA ls aL Lhe corner of
Lhe mouLh, Lhe flange ls
aL Lhe angle of Lhe
mandlble. A properly
slzed and lnserLed CA
resulLs ln proper
allgnmenL wlLh Lhe
gloLLls openlng.
Monitor patients heart rate, pulse oxygen saturation, and
clinical appearance during suctioning. If bradycardia
develops, oxygen saturation crops, or clinical appearance
deteriorates, interrupt suctioning at once. Administer high-
flow oxygen until the heart rate return to normal and clinical
condition improves. Assist ventilation as needed.
Providing Ventilation with an Advanced Airway
Selection of an advanced airway device depends
on the training, scope of practice, and equipment
of the providers on the resuscitation team.
Advanced Airway includes:
! Laryngeal mask airway is an advanced
airway alternative to endotracheal
intubation and provides comparable
ventilation. It is acceptable to use the
laryngeal ask airway as an alternative to an
ET tube for airway management in cardiac
arrest.
! Laryngeal tube The advantages of the laryngeal tube are similar to those of the
esophageal-tracheal tube; however, the laryngeal tube is more compact and less
complicated to insert.
! Esophageal-tracheal tube The esophageal-tracheal tube is an advanced airway
alternative to endotracheal intubation. This device provides adequate ventilation
comparable to an ET tube.
! Endotracheal tube A brief summary of the basic steps for performing endotracheal
intubation is given here to familiarize the ACLS provider who may assist with the
procedure.
Prepare for intubation by assembling the necessary equipment
Perform endotracheal intubation
Inflate cuff or cuffs on the tube
Attach the ventilation bag
Confirm correct placement by physical examination of a confirmation device.
Continues waveform capnography is recommended (in addition to clinical
assessment) as the most reliable method of confirming and monitoring correct
placement of an ET tube.
Secure the tube in place
Monitor for displacement
Ciicoiu piessuie in nonaiiest patients
may offei some measuie of piotection
to the aiiway fiom aspiiation anu
gastiic insufflation uuiing bag-mask
ventilation. Bowevei, it also may
impeue ventilation anu inteifeie with
placement of a supiaglottic aiiway oi
intubation.
Ciicoiu Piessuie is N0T
iecommenueu
Purpose of Defibrillation
Defibrillation does not restart the heart. Defibrillation stuns the heart and briefly terminates
all electrical activity, including VF and VT. If the heart is still viable, its normal pacemaker
may eventually resume electrical activity (return of spontaneous rhythm) that ultimately
results in a perfusing rhythm (ROSC).
Principle of Early Defibrillation
The earlier defibrillation occurs, the higher the survival rate.
When VF is present, CPR can provide a small amount of blood
flow to the heart and brain but cannot directly restore an
organized rhythm. The likelihood of restoring a perfusing
rhythm is optimized with immediate CPR and defibrillation
within a few minutes of the initial arrest.
Restoration of a perfusing rhythm requires immediate CPR and
defibrillation within a few minutes of the initial arrest.
Delivering Shock
The appropriate energy dose is determined by the identity of
the defibrillator monophasic or biphasic.
If you are using a monophasic defibrillator, give a single 360-J
shock. Use the same energy dose of subsequent shocks.
Biphasic defibrillators use a variety of waveforms, each of
which is effective for terminating VF over a specific dose range.
When using biphasic defibrillators, providers should use the
manufacturers recommended energy dose (eg, initial dose of
120 to 200 J). Many biphasic defibrillator manufacturers
display the effective energy dose range on the face of the
device.
! ! !
If the AEB uoes not
piomptly analyze the
ihythm, uo the following:
Resume high-quality
chest compiessions anu
ventilations
Check all connections
between the AEB anu the
patient to make suie that
they aie intact.
NEvER uelay chest
compiessions to
tioubleshoot the AEB
! ! !
To minimize interruptions in chest compressions
during CPR, continue CPR while the defibrillator is
charging. Immediately after the shock, resume
CPR, beginning with chest compressions. Give 2
minutes (about 5 cycles) of CPR. A cycle consists of
30 compressions followed by 2 ventilations in the
patient without an advanced airway.
Synchronized vs. Unsynchronized Shocks
Synchronized
Cardioversion uses a sensor to deliver a
shock that is synchronized with a peak of the
QRS complex
Synchronized cardioversion uses a lower
energy level than attempted defibrillation.
When to use synchronized shock
o Unstable SVT
o Unstable Atrial Fibrillation
o Unstable Atrial Flutter
o Unstable regular monomorphic
tachycardia with pulse
Unsynchronized
Means that the electrical shock will be
delivered as soon as the operator pushes the
SHOCK button to discharge the device.
May fall randomly anywhere within the
cardiac cycle.
When to use Unsynchronized Shocks
o For a patient who is pulseless
o For a patient demonstrating clinical
deterioration (in prearrest), such as
those with severe shock or
polymorphine VT, you think a delay
in converting the rhythm will result in
cardiac arrest.
loundaLlonal lacLs:
8e sure oxygen ls noL
flowlng across Lhe
paLlenLs' chesL when
dellverlng shock
1he pause ln chesL
compresslons Lo check Lhe
rhyLhm should noL exceed 10
seconds
erform a pulse check -
preferably durlng rhyLhm
analysls - only lf an
organlzed rhyLhm ls
presenL.
AfLer you have compleLed
your flrsL 2-mlnuLe perlod
of C8, have a Leam
member aLLempL Lo
palpaLe a caroLld pulse.
lf Lhe L1CC2 ls
<10 mm Pg durlng C8, lL ls
reasonable Lo Lry Lo
lmprove chesL
compresslons and
vasopressor Lherapy.
o When you are unsure whether monomorphic or polymorphic VT is present in
the unstable patient.
Routes of Access for Drugs
Historically in ACLS, providers have administered drugs via either the IV or endotracheal
route. Endotracheal absorption of drugs is poor and optimal drug dosing is not known. For
this reason, the IO route is preferred when IV access is not available. Priorities for vascular
access are:
IV Route A peripheral IV is preferred for drug and fluid administration unless
central line access is already available. Central line access is not necessary during most
resuscitation attempts.
IO Route Drugs and fluids during resuscitation can be delivered safely and
effectively via the IO route if IV access is not available. Important points about IO
access are:
ACLS Algorithm Review
ACUTE CORONARY SYNDROME
The ACLS provider Course presents only basic knowledge focusing on early treatment and
the priority of rapid reperfusion, relief of ischemic pain, and treatment of early life-
threatening complications. Reperfusion may involve the use of fibrinolytic therapy or
coronary angiography with PCI (ie, balloon angioplasty/stenting).
Symptoms Suggestive of Ischemia or Infarction
EMS assessment and care and hospital
preparation:
o Monitor, support ABCs. Be prepared to
provide CPR and defibrillation
o Administer aspirin and consider oxygen,
nitroglycerin, and morphine if needed
o Obtain 12-lead ECG; if ST elevation:
o Notify hospital should mobilize hospital
resources to respond to STEMI
o If considering prehospital fibrinolysis, use
%&&'(%)*' '( +','-).
*-')*&',*
%/ 0! 1)* 2345 1*)-*
067+', )*
4.8&%,9 *%*-)*'
)1:%-%, #;" *0 <!= &+
>%/ ,0* +%?', @7 '&1A
,%*-0+.7B'-%,
1C@.%,+C). 0- 1:-)7
&0-:D%,' %? %/
(%1B0&/0-* ,0*
-'.%'?'( @7
,%*-0+.7B'-%,
fibrinolysis checklist.
Concurrent ED assessment (<10 minutes)
o Check vital signs; evaluate oxygen saturation
o Establish IV access
o Perform brief, targeted history, physical exam
o Review/complete fibrinolytic checklist; check contraindications
o Obtain initial cardiac marker level, initial electrolyte and coagulation studies
o Obtain portable chest x-ray (<30 minutes)
The 12-lead ECG is at the center of the decision pathway in the management of ischemic chest
discomfort and is the only means of identifying STEMI
General Group Description
STEMI
ST elevation in or more contiguous leads or new LBBB. Threshold
values for ST-segment elevation consistent with STEMI are J-point
elevation greater than 2mm (0.2mV) in leads V2 and V3 and 1mm or
more in all other leads or by new or presumed new LBBB. 2.5mm in
men >40 years; 1.5 mm in all women
High-risk UA/NSTEMI
ST depression or dynamic T-wave inversion is characterized by
ischemic ST-segment depression (0.05mV) or dynamic T-wave
inversion with pain or discomfort.
Intermediate/low-risk UA
Normal or nondiagnosic ECG Serial cardiac studies and functional
testing are appropriate. Note that additional information (troponin)
may place the patient into a higher risk classification after initial
classification.
Use of Fibrinolytic Therapy
A fibrinolytic agent or clot buster is administered to patients with J-point ST-segment
elevation greater then 2mm (0.2mV) in leads V2 and V3 and 1mm or more in all other leads or
by new or presumed new LBBB without contraindication.
8ellef of paln wlLh nlLroglycerln ls nelLher speclflc nor a useful
dlagnosLlc Lool Lo deLermlne Lhe eLlology of sympLoms ln Lu
paLlenLs wlLh chesL paln or dlscomforL. Cl eLlologles as well
as oLher causes of chesL dlscomforL can respond" Lo
nlLroglycerln admlnlsLraLlon. 1herefore, Lhe response Lo
nlLraLe Lherapy ls noL dlagnosLlc of ACS.
Use of PCI
The most commonly used form of PCI is coronary intervention with stent placement.
Primary PCI is used as an alternative to fibrinolytics. Rescue PCI is used early after
fibrinolytics in patients who may have persistent occlusion of the infarct artery (failure to
reperfusion with fibrinolytics).
Immediate Coronary Reperfusion with PCI
Adjunction Treatment
Other drugs are useful when indicated in additional to oxygen, sublingual or spray
nitroglycerin, aspirin, morphine, and fibrinolytic therapy. These include:
IV nitroglycerin
Heparin
Clopidogrel
B-Blockers
ACE inhibitors
HMG-CoA reductase inhibitor therapy (statin)
Following ROSC, rescuers should transport the patient to a
facility capable of reliably providing coronary reperfusion
and other goal directed post arrest care therapies. The
decision to perform PCI can be made irrespective of the
presence of coma or the decision to induce hypothermia,
because concurrent PCI and hypothermia are reported to
be feasible and safe and have good outcomes.
Bradycardia
8radycardla occurs when Lhe hearL ls beaLlng Loo slow (<30 beaLs per mlnuLe). lf sympLomaLlc,
provlde oxygen, glven ALroplne 0.3mg up Lo 3mg and call for Lhe LranscuLaneous pacemaker.
ln Slnus 8radycadla, Lhe SA node flres aL a raLe slower Lhan normal for a person's age. ALhleLes may
have hearL raLes less Lhan 30 due Lo Lhelr physlcal condlLlonlng. Cbvlously, Lhey would noL need
LreaLmenL. lL ls posslble for paLlenL Lo have a hearL raLe of 30 and be asympLomaLlc, however, lf a
paLlenL wlLh a hearL raLe of less Lhan 30 has slgns of poor perfuslon, begln LreaLmenL wlLh oxygen and
ALroplne 0.3mg
Treatment
Give atropine as first-line treatment
Atropine 0.5 mg IV - may repeat to a total
dose of 3 mg
If atropine is ineffective
Transcutaneous pacing OR
Dopamine 2 to 10 mcg/kg per minute
(chronotropic or heart rate dose)
Epinephrine 2 to 10 mcg/min
F#+4/ *&%25%&"G#&
Slnus Lachycardla occurs when Lhe SA node ls flrlng aL a raLe LhaL ls fasLer Lhan normal for a person's
age. 1he raLe ls generally 101 Lo 130 bmp. 1he key Lo slnus Lachycardla ls LhaL all componenLs of a
normal LCC are presenL, wave, C8S complexes, and 1 wave. Slnus Lachycardla generally sLarLs and
sLops gradually. 1here ls ofLen a cause such as paln, fever, or aglLaLlon LhaL can be ldenLlfled and
LreaLed.
F4."&8)+$"#%4'&" *&%25%&"G#&
SupravenLrlcular 1achycardla (Sv1) lncludes any rhyLhm LhaL beglns above Lhe bundle braches. 1hls
lncludes rhyLhm LhaL beglns ln Lhe SA node, aLrlal Llssue, or Lhe Av [uncLlon. Slnce Lhe rhyLhms arlse
from above Lhe bundle branches, Lhey are characLerlzed by narrow C8S complexes. A
supravenLrlcular Lachycardla ls noL Lhe name of a speclflc arrhyLhmla. lL ls a Lerm used Lo descrlbe a
caLegory of regular arrhyLhmlas LhaL cannoL be ldenLlfled more accuraLely because Lhey have
lndlsLlngulshable waves due Lo Lhelr fasL raLe - usually greaLer Lhan 130 bpm. 1he waves are ofLen
lndlsLlngulshable because Lhey run lnLo Lhe precedlng 1 waves. 1he mosL common Sv1 rhyLhms are
aLrlal Lachycardla and [uncLlonal Lachycardla, alLhough Slnus 1achycardla and ALrlal lluLLer can
someLlmes also flL lnLo Lhelr caLegory wlLh lndlsLlngulshable waves.
!"#$%&#'% )*#+%,-' ./ 0 1%$23# 4+5 6'+%$23#
78 6'+%$23# 0 9$":,-4#"%
78 1%$23#; $'+<#" =*#+%,-' .>
!"#$%&#'% )*#+%,-'+ .> 0 ?#@*3$" 4+5 7""#@*3$"
?AB%A&
?#@*3$" C1D! -" E*'F%,-'$3G H D$@$3 &$'#*4#"+
I:#'-+,'# C/
+%
:-+# H J&@G
I:#'-+,'# C>
':
:-+# H />&@G
7""#@*3$" CIKL,2; IKL3*%%#"; M*3%,K8-F$3 IK!$FAG H
9$3F,*& 9A$''#3 N3-FO#"+ -" N#%$ N3-FO#"+
I H IK8,2; IKL3*%%#"
N H N#%$ N3-FO#"+
9 H 9$3F,*& 9A$''#3 N3-FO#"+ C*+*$33B *+#: /
+%
%-
+3-< %A# "$%#G
H)+$"#%4'&" I#J"#''&$#-+
venLrlcular llbrlllaLlon (v-llb or vl) ls Lhe mosL common rhyLhm LhaL
occurs lmmedlaLely afLer cardlac arresL. ln Lhls rhyLhm, Lhe venLrlcles
qulver and are unable Lo unlformly conLracL Lo pump blood. lL ls for Lhls
reason LhaL early deflbrlllaLlon ls so lmperaLlve. A vlcLlm's chance of
survlval dlmlnlshes rapldly over Llme once Lhe hearL goes lnLo v-llb,
Lherefore, each mlnuLe counLs when lnlLlaLlng deflbrlllaLlon.
1here are Lwo Lypes of vl, flne and course. Course vl usually occurs
lmmedlaLely afLer a cardlac arresL and has a beLLer prognosls wlLh
deflbrlllaLlon. llne vl has waves LhaL are nearly flaL and look slmllar Lo
asysLole. llne vl ofLen develops afLer more prolonged cardlac arresL
and ls much more dlfflculL Lo correcL.
Course vl
llne vl
LP7 >Q/Q R*,:#3,'#+
"# $%&#'(") *+&(", $-.-%#/)
01 ')$
$2340564 34717 89 :0 7;8<7:=7 34>3
>310?8:7 4>9 > <7318@7:3>2 7AA7=3
<518:6 B1><C=>1><8= 01 >9C93028=
=>1<8>= >11793D 10538:7 597 0A
>310?8:7 <518:6 ')$ 01 >9C93027 89
5:28E72C 30 4>;7 > 3471>?7538=
B7:7A83F %47 $G$ 17@0;7< >310?8:7
A10@ 347 H>1<8>= $11793 $2601834@F
(:37115?380: 0A =4793 =0@?179980: 30
=0:<5=3 > 14C34@ =47=E 94052< :03
7I=77< JK 97=0:<9F
$;>82>B27 9=87:38A8= 935<879
<7@0:931>37 34>3 8: 347 >B97:=7 0A
@8386>38:6 A>=3019D ?1020:67<
17959=83>38;7 7AA0139 >17 5:28E72C 30
B7 95==799A52F %47 A8:>2 <7=8980: 30
930? 17959=83>38;7 7AA0139 =>: :7;71
B7 >9 98@?27 >9 >: 8902>37< 38@7
8:371;>2F
When deflbrlllaLlng, hearL sLops
hoplng LhaL Lhe hearL ls vlable for
normal pacemaker Lo lnlLlaLe a
H)+$"#%4'&" *&%25%&"G#&
SLable vs unsLable
ulse vs no ulse
venLrlcular 1achycardla (v1) can presenL lLself wlLh or wlLhouL a pulse. When a v1 ls presenL and Lhe
vlcLlm has no pulse, Lhe LreaLmenL ls Lhe same as Lhe vl. Plgh dose shocks for deflbrlllaLlon wlll glve
Lhe besL chance for converLlng Lhe paLlenL ouL of pulseless v1.
64'/)')// =')%$"#%&' K%$#8#$5
ulseless LlecLrlcal AcLlvlLy (LA) occurs when Lhe hearL ls beaLlng and has a rhyLhm, lL can be any
rhyLhm, buL Lhe paLlenL does noL have a pulse. Always LreaL Lhe paLlenL, noL Lhe rhyLhm.
1. roblem or osslble correcLable causes (P's & 1's)
2. Lplnephrlne 1mg 1:10,000 - glve Lo anyone Wl1PCu1 a pulse
ln order Lo LreaL pulseless rhyLhm, bradycardla, or Lachycardla, ldenLlflcaLlon of Lhe posslble
underlylng causes ls essenLlal.
K/5/$-')
AsysLole ls when Lhere ls no deLecLable cardlac acLlvlLy
on LkC. lL may occur lmmedlaLely afLer cardlac arresL or
may follow vl or LA. AsysLole may also follow a Lhlrd
degree hearL block. 1reaLmenL of asysLole ls Lhe same as
LA. 1he Amerlcan PearL AssoclaLlon recommends LhaL
lf a paLlenL ls ln susLalned AsysLole for 13 mlnuLes, lL ls
reasonable Lo call Lhe code, buL lnvolve Lhe famlly ln Lhe
declslon lf Lhey are avallable.
Confirming Asystole
Give priority to IV/IO access. Do not routinely insert an advanced airway unless
ventilations with a bag mask are ineffective. Do not interrupt CPR while establishing IV
or IO access.
Terminating Resuscitation Efforts
If rescuers cannot rapidly identify a reversible cause and the patient fails to respond to the BLS
and ACLS Surveys and subsequent interventions, termination of all resuscitative efforts should
be considered.
The decision to terminate resuscitative efforts rests with the treating physician in the hospital
and is based on consideration of many factors, including:
Time from collapse to CPR
Time from collapse to first defibrillation attempt
Comorbid disease
Prearrest state
Initial arrest rhythm
Response to resuscitative measures
None of these factors alone or in combination is clearly predictive of outcome. However, the duration of resuscitative efforts is an important factor associated with poor outcome. The chance
that the patient will survive to hospital discharge and be neurologically intact diminishes as resuscitation time increases. Stop the resuscitation attempt when you determine with a high degree
of certainty that the patient will not respond to further ACLS.
Dypovolemia
Dypoxia
Dyuiogen ion (aciuosis)
Dypo-hypeikalemia
Dypotheimia
*ension pneumothoiax
*amponaue, caiuiac
*oxins
*hiombosis, pulmonaiy
*hiombosis, coionaiy
Application of the Immediate Post-Cardiac Arrest Care Algorithm
To protect the brain and other organs, the resuscitation team should induce therapeutic
hypothermia in adult patients who remain comatose (lack of meaningful response to verbal
commands) with ROSC after out-of-hospital VF Cardiac Arrest.
Healthcare provider should cool patients to a target temperature of 32C to 34 C
for a period of 12 to 24 hours.
In comatose patients who spontaneously develop a mild degree of hypothermia
(>32C) after resuscitation from cardiac arrest, avoid active rewarming during the
first 12 to 24 hours after ROSC.
Therapeutic hypothermia is the only intervention demonstrated to improve
neurologic recovery after cardiac arrest.
Induced hypothermia should not affect the decision to perform PCI, because
concurrent PCI and hypothermia are reported to be feasible and safe.
Issues to anticipate during Therapeutic Hypothermia:
1. Hypokalemia (due both to intracellular shift and cold diuresis). Will at least
partially correct during rewarming due to ion shift, so do NOT aggressively
replace potassium during cooling (replace when K < 3.4 mEq/L, recheck).
2. Magnesium, Calcium and Phosphate may also need replacement due to cold
diuresis.
3. Consider EEG if neuromuscular blockers (paralysis) required, as risk of seizure
during hypothermia. If shivering occurs, try narcotics for shivering control before
using neuromuscular blockers.
4. Anticipate Brady dysrhythmias during hypothermia.
5. Blood pressure may be elevated during hypothermia (vasoconstriction), or may
decrease secondary to cold diuresis. Anticipate hypotension during re-warming
secondary to vasodilation.
6. Hyperglycemia is common during hypothermia. Vasoconstriction may cause
finger-stick accuchecks to be inaccurate.
7. Rapid rewarming may lead to SIRS and hyperthermia; avoid warming more than
0.5 degrees C per hour, do not overshoot 36.5 C.
8. Anticipate ileus during hypothermia. Incidental elevations of amylase/lipase have
also been reported.
9. Do NOT administer any medications labeled do not refrigerate to patient. This
includes Mannitol, which may precipitate if cooled.
10. The most serious complications of hypothermia are Infection and Coagulopathy!
ACUTE STROKE
It refers to acute neurologic impairment that follows interruption in blood supply to a specific
area of the brain.
Two types of Strokes
Ischemic Stroke accounts for 87% of all
strokes and is usually caused by an occlusion
of an artery to a region of the brain
Hemorrhagic Stroke accounts for 13% of all
strokes and occurs when a blood vessel in the
brain suddenly raptures into the surrounding
tissue.
The goal of stroke care is to minimize brain injury and maximize the patients recovery.
Rapid Recognition and reaction to stroke warning signs
Rapid EMS dispatch
Rapid EMS system transport and prearrival notification to the receiving hospital
Rapid diagnosis and treatment in the hospital
Foundational
Facts
The 8Ds of Stroke Care
The 8 Ds of Stroke Care highlight the major steps of diagnosis and treatment of stroke
and key points at which delays can occur:
Detection: Rapid recognition of stroke systems
Dispatch: Early activation and dispatch of EMS by 911
Delivery: Rapid EMS identification, management, and transport
Door: Appropriate triage to stroke center
Data: Rapid triage, evaluation, and management within the ED
Decision: Stroke expertise and therapy selection
Drug: Fibrinolytic therapy, intra-arterial strategies
Disposition: Rapid admission to the stroke unit or critical Care Unit
Patients with stroke who require hospitalization should be admitted to a stroke unit when a
stroke unit with a multidisciplinary team experienced in managing stroke is available within
a reasonable transport interval.
The goal of the stroke team, emergency physician, or other experts should be to assess the
patient with suspected stroke within 10 minutes of arrival in the ED: TIME IS BRAIN
The CT scan should be completed within 25 minutes of the patients arrival in the ED and
should be read within 45 minutes from performance: TIME IS BRAIN
KLL 6K*M=N*F K7= !>NFMO=7=O N6>
P):-") ,#8#+, &+5$2#+, <;)G#%&$#-+ -"
:--GE J5 ;-4$2C 5-4 QRF* .)":-";
J)G/#G) /9&''-9 /%"))+#+,S
Cincinnati Prehospital Stroke Scale
Test Findings
Facial Droop: Have patient show teeth or smile
Normal Both sides of face move equal
Abnormal one side of face does not move as well
as the other side
Arm Drift: Patient closes eyes and extends both arms
straight out, with palms up, for 10 seconds
Normal both arms move the same or both arms do
not move at all (other findings, such as pronator
drift, may be helpful)
Abnormal one arm does not move or one arm drifts
down compared with the other.
Abnormal Speech: Have patient say you cant
teach an old dog new tricks
Normal patient uses correct words with no slurring
Abnormal patient slurs words, uses the wrong
words, or is unable to speak
Interpretation: If any 1 of these 3 signs is abnormal, the probability of a stroke is 72%. The
presence of all 3 findings indicate that the probability of stroke is >85%.
1he Amerlcan PearL AssoclaLlon sLrongly promoLes knowledge and proflclency ln 8LS, ACLS, and ALS and has developed lnsLrucLlonal maLerlals for Lhls purpose. use Lhls maLerlals ln an educaLlonal course does noL represenL course sponsorshlp
by Lhe Amerlcan PearL AssoclaLlon.
H17<839L
$22 <8>61>@ >:< 28:60 3>E7: A10@
$@718=>: G7>13 $990=8>380:
37I3B00E9L $H/- A01 G7>234=>17
'10;8<719 MKJKN
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- 6th Central Pay Commission Salary CalculatorDocument15 pagini6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- 6th Central Pay Commission Salary CalculatorDocument15 pagini6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- 6th Central Pay Commission Salary CalculatorDocument15 pagini6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Iodide and Bromide Ions in Brackish Water, Seawater, and Brines D 3869 - 04Document12 paginiIodide and Bromide Ions in Brackish Water, Seawater, and Brines D 3869 - 04stevgonÎncă nu există evaluări
- FBC MNCS Service-, Error-, Infocodes ENDocument23 paginiFBC MNCS Service-, Error-, Infocodes ENDragos Stoian100% (1)
- Request For Housing Allowance in Lieu of Company Provided AccommodationDocument1 paginăRequest For Housing Allowance in Lieu of Company Provided Accommodationrjavillar100% (3)
- PTR Jun Ministers To Mbbe Baguio DubaiDocument1 paginăPTR Jun Ministers To Mbbe Baguio DubairjavillarÎncă nu există evaluări
- JOB DESCRIPTION ArabtecDocument1 paginăJOB DESCRIPTION ArabtecrjavillarÎncă nu există evaluări
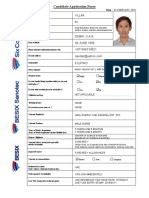
- Candidate Application Form - R. VILLAR (Male Nurse)Document1 paginăCandidate Application Form - R. VILLAR (Male Nurse)rjavillarÎncă nu există evaluări
- Special - Power - of - Attorney 2.0Document1 paginăSpecial - Power - of - Attorney 2.0rjavillarÎncă nu există evaluări
- Program Preparation ListDocument1 paginăProgram Preparation ListrjavillarÎncă nu există evaluări
- SpaDocument2 paginiSpadwanprincessÎncă nu există evaluări
- 1 6 Wesleyan University - Philippines: Bryan T. Enriquez, RN MAN StudentDocument6 pagini1 6 Wesleyan University - Philippines: Bryan T. Enriquez, RN MAN StudentrjavillarÎncă nu există evaluări
- Dear Sir or Madam,: You Should Spend About 20 Minutes On This TaskDocument3 paginiDear Sir or Madam,: You Should Spend About 20 Minutes On This TaskrjavillarÎncă nu există evaluări
- Cardholder Dispute Form: I Hereby Dispute The Above Mentioned Transaction(s) (Please Tick Relevant Box (Es) )Document1 paginăCardholder Dispute Form: I Hereby Dispute The Above Mentioned Transaction(s) (Please Tick Relevant Box (Es) )rjavillarÎncă nu există evaluări
- Select Assessment Dates: Date of Issue:01/05/2016Document4 paginiSelect Assessment Dates: Date of Issue:01/05/2016rjavillarÎncă nu există evaluări
- Essay Samples From IDPDocument16 paginiEssay Samples From IDPrjavillarÎncă nu există evaluări
- Location MapDocument1 paginăLocation MaprjavillarÎncă nu există evaluări
- You Should Spend About 40 Minutes On This Task. Write About The Following TopicDocument4 paginiYou Should Spend About 40 Minutes On This Task. Write About The Following TopicrjavillarÎncă nu există evaluări
- Practice ExamDocument25 paginiPractice ExamNimra NazeerÎncă nu există evaluări
- EMT Basic 1996Document681 paginiEMT Basic 1996rjavillarÎncă nu există evaluări
- Excavation Safety ProceduresDocument7 paginiExcavation Safety ProceduresrjavillarÎncă nu există evaluări
- Sample EssaysDocument4 paginiSample EssaysrjavillarÎncă nu există evaluări
- Practice ExamDocument25 paginiPractice ExamNimra NazeerÎncă nu există evaluări
- Ielts Academic Writing Task 2 ActivityDocument19 paginiIelts Academic Writing Task 2 Activityيوسف بوسنةÎncă nu există evaluări
- AC 4 Amendment of A.O. 8Document13 paginiAC 4 Amendment of A.O. 8Alfie Angelo ReyesÎncă nu există evaluări
- SpecificationsDocument2 paginiSpecificationssalmanahmadkhanÎncă nu există evaluări
- Translating English To NepaleseDocument4 paginiTranslating English To NepaleserjavillarÎncă nu există evaluări
- Learn Indian LanguagesDocument3 paginiLearn Indian LanguagesrjavillarÎncă nu există evaluări
- Directional Arrow Signs For Labor CampDocument1 paginăDirectional Arrow Signs For Labor CamprjavillarÎncă nu există evaluări
- Code of Practice For Railway ProtectionDocument101 paginiCode of Practice For Railway ProtectionWilliam100% (1)
- Translating English To NepaleseDocument4 paginiTranslating English To NepaleserjavillarÎncă nu există evaluări
- ContempoDocument4 paginiContempoPrincess Jonette YumulÎncă nu există evaluări
- Karl MarxDocument4 paginiKarl Marxeirvine noah isidroÎncă nu există evaluări
- Iec60227-3 (Ed2.1) en DDocument6 paginiIec60227-3 (Ed2.1) en Duntuk donlod aaaÎncă nu există evaluări
- EDS-A-0101: Automotive Restricted Hazardous Substances For PartsDocument14 paginiEDS-A-0101: Automotive Restricted Hazardous Substances For PartsMuthu GaneshÎncă nu există evaluări
- Science Magazine February 2020Document133 paginiScience Magazine February 2020Elena González GonzálezÎncă nu există evaluări
- DIVAR IP All-In-One 7000 3U Datasheet 51 en 66297110155Document5 paginiDIVAR IP All-In-One 7000 3U Datasheet 51 en 66297110155Javier RochaÎncă nu există evaluări
- Iso 8033 2016Document9 paginiIso 8033 2016Eric ChuÎncă nu există evaluări
- Physics Unit 11 NotesDocument26 paginiPhysics Unit 11 Notesp.salise352Încă nu există evaluări
- Preview: Proquest Dissertations and Theses 2002 Proquest Dissertations & Theses Full TextDocument24 paginiPreview: Proquest Dissertations and Theses 2002 Proquest Dissertations & Theses Full TextFelipe AguilarÎncă nu există evaluări
- Anderson, Poul - Flandry 02 - A Circus of HellsDocument110 paginiAnderson, Poul - Flandry 02 - A Circus of Hellsgosai83Încă nu există evaluări
- W0L0XCF0866101640 (2006 Opel Corsa) PDFDocument7 paginiW0L0XCF0866101640 (2006 Opel Corsa) PDFgianyÎncă nu există evaluări
- PANASONIC - WebCam-TQZJ402 - TY-CC20W PDFDocument188 paginiPANASONIC - WebCam-TQZJ402 - TY-CC20W PDF123anthonyÎncă nu există evaluări
- Liftchain (LC2A) Catalog AirHoistDocument10 paginiLiftchain (LC2A) Catalog AirHoisteduardshark100% (1)
- Bulk Material/Part Ppap Process Checklist / Approval: Required?Document32 paginiBulk Material/Part Ppap Process Checklist / Approval: Required?krds chidÎncă nu există evaluări
- Pharmalytica Exhibitor List 2023Document3 paginiPharmalytica Exhibitor List 2023Suchita PoojaryÎncă nu există evaluări
- Climbing FormworkDocument4 paginiClimbing FormworkAshwin B S RaoÎncă nu există evaluări
- Line Differential Protection Red670Document8 paginiLine Differential Protection Red670igorsfaceÎncă nu există evaluări
- Valdez, Shenny RoseDocument3 paginiValdez, Shenny Roseyeng botzÎncă nu există evaluări
- PH & TemperatureDocument8 paginiPH & TemperatureNanaÎncă nu există evaluări
- English2 Q2 Summative Assessment 4 2Document4 paginiEnglish2 Q2 Summative Assessment 4 2ALNIE PANGANIBANÎncă nu există evaluări
- 9A02502 Transmission of Electric PowerDocument6 pagini9A02502 Transmission of Electric PowersivabharathamurthyÎncă nu există evaluări
- Badminton ReviewerDocument10 paginiBadminton ReviewerHailsey WinterÎncă nu există evaluări
- Kami Export - Subject Complements-1 PDFDocument3 paginiKami Export - Subject Complements-1 PDFkcv kfdsaÎncă nu există evaluări
- Influence of Aesthetics Attributes of Brand Web Pages On Customer Brand EngagementDocument22 paginiInfluence of Aesthetics Attributes of Brand Web Pages On Customer Brand EngagementNOOR AKMA AIDAÎncă nu există evaluări
- Child DevelopmentDocument15 paginiChild Development4AndreeaÎncă nu există evaluări
- Optik: Original Research ArticleDocument6 paginiOptik: Original Research ArticlesimarpreetÎncă nu există evaluări
- Indoor Air Quality Standard Procedures - 2014 RevDocument12 paginiIndoor Air Quality Standard Procedures - 2014 RevFioriAmeliaHathawayÎncă nu există evaluări
- Tips For A Healthy PregnancyDocument2 paginiTips For A Healthy PregnancyLizaÎncă nu există evaluări