Documente Academic
Documente Profesional
Documente Cultură
Dyspnea
Încărcat de
Tara Wandhita0 evaluări0% au considerat acest document util (0 voturi)
40 vizualizări7 paginijkhkj
Drepturi de autor
© © All Rights Reserved
Formate disponibile
DOCX, PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentjkhkj
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca DOCX, PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
40 vizualizări7 paginiDyspnea
Încărcat de
Tara Wandhitajkhkj
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca DOCX, PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 7
Dyspnea - from Wikipedia, the free encyclopedia
Dyspnea (also spelled dyspnoea) or (shortness of breath (SOB), air hunger)
[1]
, is the
subjective symptom of breathlessness.
[2][3]
It is a normal symptom of heavy exertion however
becomes pathological if it occurs in unexpected situations.
[2]
In 85% of cases it is due to either:
asthma, pneumonia, cardiac ischemia, interstitial lung disease, congestive heart failure, chronic
obstructive pulmonary disease, or psychogenic causes.
[4]
Treatment typically depends on the
underlying cause.
[5]
Definition
Lungs and breathing activity
view talk edit
Eupnea - normal breathing
Dyspnea or shortness of breath - sensation of respiratory distress
Bradypnea - decreased breathing rate
Hyperaeration/Hyperinflation - increased lung volume
Hyperpnea - faster and/or deeper breathing
Hyperventilation - increased breathing that causes CO
2
loss
Labored breathing - physical presentation of respiratory distress
Tachypnea - increased breathing rate
Dyspnea does not have a well defined or universally accepted definition.
[4]
It is defined by the
American Thoracic Society as the "subjective experience of breathing discomfort that consists of
qualitatively distinct sensations that vary in intensity. The experience derives from interactions
among multiple physiological, psychological, social, and environmental factors, and may induce
secondary physiological and behavioral responses."
[6]
Other definitions of dyspnea include:
"difficulty in breathing"
[7]
, "disordered or inadequate breathing",
[8]
"uncomfortable awareness of
breathing",
[3]
or simple "breathlessness".
[2]
Acute breathlessness is defined as severe shortness of breath that develops over minutes to
hours.
[5]
Chronic breathlessness on the other hand comes on over weeks or months.
[9]
Differential diagnosis
Main article: Differential diagnosis of dyspnea
While shortness of breath is generally caused by disorders of the cardiac or respiratory system
other system such as musculoskeletal, endocrine, hematologic, and psychiatric maybe the
cause.
[4]
DiagnosisPro, an online medical expert system, listed 497 distinct causes in October of
2010.
[10]
The most common cardiovascular causes are acute myocardial infarction and congestive
heart failure while common pulmonary causes include: chronic obstructive pulmonary disease,
asthma, pneumothorax, and pneumonia.
[2]
Acute coronary syndrome
Acute coronary syndrome frequently presents with retrosternal chest discomfort and difficulty
catching the breath.
[2]
It however may atypically present with shortness of breath alone.
[11]
Risk
factors include: old age, smoking, hypertension, hyperlipidemia, and diabetes.
[11]
An
electrocardiogram and cardiac enzymes are important both for diagnosis and directing
treatment.
[11]
Treatment involves measures to decrease the oxygen requirement of the heart and
efforts to increase blood flow.
[2]
Congestive heart failure
Congestive heart failure frequently presents with SOB with exertion, orthopnea, and paroxysmal
nocturnal dyspnea.
[2]
It affects between 1-2% of the general United States population and occurs
in 10% of those over 65 years old.
[2][11]
Risk factors for acute decompensation include: high
dietary salt intake, medication noncompliance, cardiac ischemia, dysrhythmias, renal failure,
pulmonary emboli, hypertension, and infections.
[11]
Treatment efforts are directed towards
decreasing lung congestion.
[2]
[edit] Chronic obstructive pulmonary disease
People with chronic obstructive pulmonary disease (COPD), most commonly emphysema or
chronic bronchitis, frequently have chronic shortness of breath and a chronic productive cough.
[2]
An acute exacerbation presents with increased shortness of breath and sputum production.
[2]
COPD is a risk factor for pneumothorax thus this condition should be ruled out.
[2]
In an acute
exacerbation treatment is with a combination of anticholinergics, beta
2
-adrenoceptor agonists,
steroids and possibly positive pressure ventilation.
[2]
[edit] Asthma
Asthma is the most common reason for presenting to the emergency with shortness of breath.
[2]
It
is the most common lung disease in both developing and developed countries affecting about 5%
of the population.
[2]
Other symptoms include: wheezing, tightness in the chest, and a non
productive cough.
[2]
Inhaled beta2-adrenergic agonist (salbutamol) are first line therapy and
usually lead to prompt improvement.
[2]
[edit] Pneumothorax
Pneumothorax presents typically with pleuritic chest pain of acute onset and shortness of breath
not improved with oxygen.
[2]
Physical findings may include: absent breath sounds on one side of
the chest, jugular venous distension, and tracheal deviation.
[2]
[edit] Pneumonia
The symptoms of pneumonia are fever, productive cough, shortness of breath, and pleuritic chest
pain.
[2]
Inspiratory crackles may be heard on exam.
[2]
A chest x-ray can be useful to differential
pneumonia from congestive heart failure.
[2]
As the cause is usually a bacterial infections
antibiotics are typically used for treatment.
[2]
[edit] Pulmonary embolism
Pulmonary embolism classically presents with an acute onset of shortness of breath.
[2]
Other
presenting symptoms include: pleuritic chest pain,cough, hemoptysis, and fever.
[2]
Risk factors
include: deep vein thrombosis, recent surgery, cancer, and previous thromboembolism.
[2]
It must
always be considered in those with acute onset of shortness of breath due to its high risk of
mortality.
[2]
Diagnosis however may be difficult.
[2]
Treatment is typically with anticoagulants.
[2]
[edit] Other
Other important or common causes of shortness of breath include: cardiac tamponade, anemia,
anaphylaxis, interstitial lung disease and panic attacks.
[12][5][4]
Cardiac tamponade presents with
dyspnea, tachycardia, elevated jugular venous pressure, and pulsus paradoxus.
[12]
The gold
standard for diagnosis is ultrasound.
[12]
Anemia, that develops gradually, usually presents with
exertional dyspnea, fatigue, weakness, and tachycardia.
[12]
It may lead to heart failure.
[12]
Anaphylaxis typically begins over a few minutes in a person with a previous history of the
same.
[5]
Other symptoms include: urticaria, throat swelling, and gastrointestinal upset.
[5]
The
primary treatment is epinephrine.
[5]
Interstitial lung disease presents with gradual onset of
shortness of breath typically with a history of a predisposing environmental exposure.
[4]
Shortness of breath is often the only symptom in those with tachydysrhythmias.
[11]
Panic attacks
typically present with hyperventilation, sweating, and numbness.
[5]
They are however a diagnosis
of exclusion.
[4]
Around 2/3 of women experience shortness of breath as a part of a normal
pregnancy.
[8]
[edit] Pathophysiology
A number of different physiological pathway may lead to shortness of breath including via
chemoreceptors, mechanoreceptors, and lung receptors.
[11]
It is currently thought that there are three main components that contribute to dyspnea: afferent
signals, efferent signals, and central information processing. It is believed that the central
processing in the brain compares the afferent and efferent signals, and that a "mismatch" results
in the sensation of dyspnea. In other words, dyspnea may result when the need for ventilation
(afferent signaling) is not being met by the physical breathing that is occurring (efferent
signaling).
[13]
Afferent signals are sensory neuronal signals that ascend to the brain. Afferent
neurons significant in dyspnea arise from a large number of sources including the carotid bodies,
medulla, lungs, and chest wall. Chemoreceptors in the carotid bodies and medulla supply
information regarding the blood gas levels of O
2
, CO
2
and H
+
. In the lungs, juxtacapillary (J)
receptors are sensitive to pulmonary interstitial edema, while stretch receptors signal
bronchoconstriction. Muscle spindles in the chest wall signal the stretch and tension of the
respiratory muscles. Thus, poor ventilation leading to hypercapnia, left heart failure leading to
interstitial edema (impairing gas exchange), asthma causing bronchoconstriction (limiting
airflow) and muscle fatigue leading to ineffective respiratory muscle action could all contribute
to a feeling of dyspnea.
[13]
Efferent signals are the motor neuronal signals descending to the respiratory muscles. The most
important respiratory muscle is the diaphragm. Other respiratory muscles include the external
and internal intercostal muscles, the abdominal muscles and the accessory breathing muscles.
As the brain receives its plentiful supply of afferent information relating to ventilation, it is able
to compare it to the current level of respiration as determined by the efferent signals. If the level
of respiration is inappropriate for the body's status then dyspnea might occur. It is worth noting
that there is a psychological component of dyspnea as well, as some people may become aware
of their breathing in such circumstances but not experience the distress typical of dyspnea.
[13]
[edit] Evaluation
MRC Breathlessness Scale
Grade Degree of dyspnea
0 no dyspnea except with strenuous exercise
1 dyspnea when walking up an incline or hurrying on the level
2 walks slower than most on the level, or stops after 15 minutes of walking on the level
3 stops after a few minutes of walking on the level
4 with minimal activity such as getting dressed, too dyspneic to leave the house
The initial approach to evaluation begins by assessment of the airway, breathing, and circulation
followed by a medical history and physical examination.
[2]
Signs that represent significant
severity include: hypotension, hypoxemia, tracheal deviation, altered mental status, unstable
dysrhythmia, stridor, intercostal indrawing, cyanosis, and absent breath sounds.
[4]
A number of scales may be used to quantify the degree of shortness of breath.
[14]
It may be
subjectively rated on a scale from 1 to 10 with descriptors associated with the number (The
Modified Borg Scale).
[14]
Alternatively a scale such as the MRC Breathlessness Scale might be
used - it suggests five different grades of dyspnea based on the circumstances in which it
arises.
[15]
[edit] Blood tests
A number of labs maybe helpful in determining the cause of shortness of breath. D-dimer while
useful to rule out a pulmonary embolism in those who are at low risk is not of much value if it is
positive as it may be positive in a number of conditions that lead to shortness of breath.
[11]
A low
level of brain natriuretic peptide is useful in ruling out congestive heart failure however a high
level while supportive of the diagnosis could also be due to advanced age, renal failure, acute
coronary syndrome, or a large pulmonary embolism.
[11]
[edit] Imaging
A chest x-ray is useful to confirm or rule out a pneumothorax, pulmonary edema, or
pneumonia.
[11]
Spiral computed tomography with intravenousradiocontrast is the imaging study
of choice to evaluate for pulmonary embolism.
[11]
[edit] Treatment
In those who are none palliative the primary treatment of shortness of breath is directed at its
underlying cause.
[5]
Extra oxygen is effective in those with hypoxia however has no effect in
those with normal blood oxygen saturations.
[3]
[edit] Palliative
Along with the measure above systemic immediate release opioids are beneficial in reducing the
symptom of shortness of breath due to both cancer and non cancer causes.
[3][16]
There is a lack of
evidence to recommend midazolam, nebulised opioids, the use of gas mixtures, or cognitive-
behavioral therapy.
[17]
[edit] Epidemiology
Shortness of breath is the primary reason 3.5% of people present to the emergency department in
the United States. Of these approximately 51% are admitted to hospital and 13% are dead within
a year.
[18]
Some studies have suggested that up to 27% of people suffer from dyspnea,
[19]
while in
dying patients 75% will experience it.
[13]
Acute shortness of breath is the most common reason
people who are palliative visit an emergency department.
[3]
[edit] Etymology
Dyspnea (pronounced /dspni/ disp-NEE-), (from Latin dyspnoea, from Greek dyspnoia from
dyspnoos) literally means disordered breathing.
[4]
[edit] References
1. ^ About.com Health's Disease and Condition content > Dyspnea By Deborah Leader.
Updated August 05, 2008
2. ^
a
b
c
d
e
f
g
h
i
j
k
l
m
n
o
p
q
r
s
t
u
v
w
x
y
z
aa
ab
ac
ad
Shiber JR, Santana J (May 2006).
"Dyspnea". Med. Clin. North Am. 90 (3): 45379. doi:10.1016/j.mcna.2005.11.006.
PMID 16473100.
3. ^
a
b
c
d
e
Schrijvers D, van Fraeyenhove F (2010). "Emergencies in palliative care".
Cancer J 16 (5): 51420. doi:10.1097/PPO.0b013e3181f28a8d. PMID 20890149.
4. ^
a
b
c
d
e
f
g
h
Sarkar S, Amelung PJ (September 2006). "Evaluation of the dyspneic
patient in the office". Prim. Care 33 (3): 64357. doi:10.1016/j.pop.2006.06.007.
PMID 17088153.
5. ^
a
b
c
d
e
f
g
h
Zuberi, T. et al (2009). "Acute breathlessness in adults". InnovAiT 2 (5):
30715. doi:10.1093/innovait/inp055. http://rcgp-
innovait.oxfordjournals.org.cyber.usask.ca/content/2/5/307.full.
6. ^ American Heart Society (1999). "Dyspnea mechanisms, assessment, and management:
a consensus statement". Am Rev Resp Crit Care Med 159: 321340.
7. ^ TheFreeDictionary, retrieved on Dec 12, 2009. Citing:The American Heritage
Dictionary of the English Language, Fourth Edition by Houghton Mifflin Company.
Updated in 2009.Ologies & -Isms. The Gale Group 2008
8. ^
a
b
"UpToDate Inc.".
http://www.uptodate.com/online/content/topic.do?topicKey=adult/6520&selectedTitle=2
~150&source=search_result.
9. ^ "dyspnea - General Practice Notebook".
http://www.gpnotebook.co.uk/simplepage.cfm?ID=825557022.
10. ^ http://en.diagnosispro.com/differential_diagnosis-for/poisoning-specific-agent-
dyspnea/25103-154-100.html
11. ^
a
b
c
d
e
f
g
h
i
j
k
Torres M, Moayedi S (May 2007). "Evaluation of the acutely dyspneic
elderly patient". Clin. Geriatr. Med. 23 (2): 30725, vi. doi:10.1016/j.cger.2007.01.007.
PMID 17462519.
12. ^
a
b
c
d
e
Wills CP, Young M, White DW (February 2010). "Pitfalls in the evaluation of
shortness of breath". Emerg. Med. Clin. North Am. 28 (1): 16381, ix.
doi:10.1016/j.emc.2009.09.011. PMID 19945605.
13. ^
a
b
c
d
Harrison's Principles of Internal Medicine (Kasper DL, Fauci AS, Longo DL, et al
(eds)) (16th ed.). New York: McGraw-Hill.
14. ^
a
b
Saracino A (October 2007). "Review of dyspnoea quantification in the emergency
department: is a rating scale for breathlessness suitable for use as an admission prediction
tool?". Emerg Med Australas 19 (5): 394404. doi:10.1111/j.1742-6723.2007.00999.x.
PMID 17919211.
15. ^ Stenton C (2008). "The MRC breathless scale.". Occup Med 58 (3): 2267.
doi:10.1093/occmed/kqm162. PMID 18441368.
16. ^ Naqvi F, Cervo F, Fields S (August 2009). "Evidence-based review of interventions to
improve palliation of pain, dyspnea, depression". Geriatrics 64 (8): 810, 124.
PMID 20722311.
17. ^ DiSalvo, WM.; Joyce, MM.; Tyson, LB.; Culkin, AE.; Mackay, K. (Apr 2008).
"Putting evidence into practice: evidence-based interventions for cancer-related dyspnea."
(PDF). Clin J Oncol Nurs 12 (2): 34152. doi:10.1188/08.CJON.341-352.
PMID 18390468. http://ons.metapress.com/content/c21324512r838824/fulltext.pdf.
18. ^ Stephen J. Dubner; Steven D. Levitt (2009). SuperFreakonomics: Tales of Altruism,
Terrorism, and Poorly Paid Prostitutes. New York: William Morrow. pp. 77. ISBN 0-06-
088957-8.
19. ^ Murray and Nadel's Textbook of Respiratory Medicine, 4th Ed. Robert J. Mason, John
F. Murray, Jay A. Nadel, 2005, Elsevier
S-ar putea să vă placă și
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- Severe Sepsis and Septic Shock Management and Performance ImprovementDocument10 paginiSevere Sepsis and Septic Shock Management and Performance ImprovementTara WandhitaÎncă nu există evaluări
- Severe Sepsis and Septic Shock Management and Performance ImprovementDocument10 paginiSevere Sepsis and Septic Shock Management and Performance ImprovementTara WandhitaÎncă nu există evaluări
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Drug Treatment For Hypertensive Emergencies: New Concepts and Emerging Technologies For Emergency PhysiciansDocument0 paginiDrug Treatment For Hypertensive Emergencies: New Concepts and Emerging Technologies For Emergency PhysiciansRajihah JihahÎncă nu există evaluări
- Negative Effects of Video GamesDocument5 paginiNegative Effects of Video GamesMadeÎncă nu există evaluări
- Diana Sanchez V City & County of DenverDocument48 paginiDiana Sanchez V City & County of DenverEllyn SantiagoÎncă nu există evaluări
- HerbalismDocument18 paginiHerbalismmieÎncă nu există evaluări
- The Letter of Intent To Enter PracticeDocument4 paginiThe Letter of Intent To Enter Practicekazniels100% (1)
- 0 - Management of HyperuricemiaDocument44 pagini0 - Management of HyperuricemiaYayuk Abay TambunanÎncă nu există evaluări
- Cholelithiasis SampleDocument77 paginiCholelithiasis Samplekrischamcute67% (3)
- Varma Varmam Marma Book Full Color in English - VKRC Vol 2 Book S Ramesh Babu - Free PDF DownloadDocument14 paginiVarma Varmam Marma Book Full Color in English - VKRC Vol 2 Book S Ramesh Babu - Free PDF DownloadS Ramesh BabuÎncă nu există evaluări
- Woodford 2015Document7 paginiWoodford 2015Tara WandhitaÎncă nu există evaluări
- Where Do The Hallucination Come From PDFDocument10 paginiWhere Do The Hallucination Come From PDFTara WandhitaÎncă nu există evaluări
- Pathophysiology, Presentation and Management of Spinal Cord InjuryDocument10 paginiPathophysiology, Presentation and Management of Spinal Cord InjurynuvitaÎncă nu există evaluări
- Epidemiology, Diagnosis, NCSEDocument12 paginiEpidemiology, Diagnosis, NCSEhedyÎncă nu există evaluări
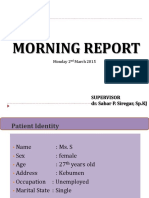
- Morning Report: Supervisor Dr. Sabar P. Siregar, SP - KJDocument49 paginiMorning Report: Supervisor Dr. Sabar P. Siregar, SP - KJTara WandhitaÎncă nu există evaluări
- How To Write A Paper For A Scientific JournalDocument10 paginiHow To Write A Paper For A Scientific JournalApam BenjaminÎncă nu există evaluări
- Spinal ShockDocument6 paginiSpinal ShockTara WandhitaÎncă nu există evaluări
- Hyponatremia in Brain InjuryDocument11 paginiHyponatremia in Brain InjuryTara WandhitaÎncă nu există evaluări
- Ann Rheum Dis-2015-Gossec-annrheumdis-2015-208337 PDFDocument13 paginiAnn Rheum Dis-2015-Gossec-annrheumdis-2015-208337 PDFTara WandhitaÎncă nu există evaluări
- Common Neurologic Disease PDFDocument41 paginiCommon Neurologic Disease PDFFerina EvangelinÎncă nu există evaluări
- 228 Career DiagramDocument3 pagini228 Career DiagramDickdoyo LankGenk WÎncă nu există evaluări
- 2015 Gout Classification CriteriaDocument12 pagini2015 Gout Classification CriteriaVico RizkytaÎncă nu există evaluări
- Guia Osteop.Document55 paginiGuia Osteop.Danu RicaldeÎncă nu există evaluări
- Ticagrelor Versus Aspirin in Acute Stroke or Transient Ischemic AttackDocument9 paginiTicagrelor Versus Aspirin in Acute Stroke or Transient Ischemic AttackTara WandhitaÎncă nu există evaluări
- Low Dose CS To Treat Septic Shock A Critical Literature ReviewDocument11 paginiLow Dose CS To Treat Septic Shock A Critical Literature ReviewTara WandhitaÎncă nu există evaluări
- Oxalate Intake and The Risk For Nephrolithiasis: Clinical ResearchDocument7 paginiOxalate Intake and The Risk For Nephrolithiasis: Clinical ResearchTara WandhitaÎncă nu există evaluări
- New Osteo Peros Is GuidelinesDocument20 paginiNew Osteo Peros Is GuidelinesTara WandhitaÎncă nu există evaluări
- Intensive Blood-Pressure Lowering in Patients With Acute Cerebral HemorrhageDocument11 paginiIntensive Blood-Pressure Lowering in Patients With Acute Cerebral HemorrhageDhiemaazth Ciccouo D'killszthÎncă nu există evaluări
- The Role of Complement System in Septic ShockDocument8 paginiThe Role of Complement System in Septic ShockTara WandhitaÎncă nu există evaluări
- Stroke 2016 Lindbohm 1975 81Document9 paginiStroke 2016 Lindbohm 1975 81Tara WandhitaÎncă nu există evaluări
- Metabolic Theory of Septic ShockDocument11 paginiMetabolic Theory of Septic ShockTara WandhitaÎncă nu există evaluări
- Metabolic Theory of Septic ShockDocument11 paginiMetabolic Theory of Septic ShockTara WandhitaÎncă nu există evaluări
- Schizophr Bull 2013 Docherty 608 16Document9 paginiSchizophr Bull 2013 Docherty 608 16Tara WandhitaÎncă nu există evaluări
- Schizophr Bull 2011 Simonsen 73 83Document11 paginiSchizophr Bull 2011 Simonsen 73 83Tara WandhitaÎncă nu există evaluări
- Schizophr Bull 2011 Chan 177 88Document12 paginiSchizophr Bull 2011 Chan 177 88Tara WandhitaÎncă nu există evaluări
- Schizophr Bull 2011 Kelly 832 8Document7 paginiSchizophr Bull 2011 Kelly 832 8Tara WandhitaÎncă nu există evaluări
- Schizophr Bull 2011 Kirkpatrick 300 5Document6 paginiSchizophr Bull 2011 Kirkpatrick 300 5Tara WandhitaÎncă nu există evaluări
- Indg 453Document11 paginiIndg 453antoÎncă nu există evaluări
- Anxiety Disorders BBDocument18 paginiAnxiety Disorders BBRyan Justin BoudreauxÎncă nu există evaluări
- AA Interview Sou Fujimoto Andreas KoflerDocument2 paginiAA Interview Sou Fujimoto Andreas KoflerLong VuÎncă nu există evaluări
- BeneFusion VP5 FP Operator's Manual V2.0 enDocument114 paginiBeneFusion VP5 FP Operator's Manual V2.0 enherbertamaya0% (1)
- Post-Operative Abdominal Infections: Epidemiology, Operational Definitions, and OutcomesDocument10 paginiPost-Operative Abdominal Infections: Epidemiology, Operational Definitions, and OutcomesJared CossioÎncă nu există evaluări
- Bishara, R. - Qualification Versus ValidationDocument4 paginiBishara, R. - Qualification Versus ValidationLuis Gustavo PachecoÎncă nu există evaluări
- Tenets and Codes of ConductDocument128 paginiTenets and Codes of ConductRodolf Dominic Serafin R. RobledoÎncă nu există evaluări
- Complex Partial SeizuresDocument5 paginiComplex Partial SeizuresNouf MohammedÎncă nu există evaluări
- Drug InteractionsDocument21 paginiDrug InteractionsPawan Deshmukh100% (1)
- Farmasi Manajemen Puskesmas KaliorangDocument5 paginiFarmasi Manajemen Puskesmas KaliorangDEA REGGIANAÎncă nu există evaluări
- Principle of Laser Application in Medicine & LASER SAFETY5Document62 paginiPrinciple of Laser Application in Medicine & LASER SAFETY5melisandrianaÎncă nu există evaluări
- Article - CVD Cardiac Arrest - Bls AclsDocument2 paginiArticle - CVD Cardiac Arrest - Bls AclsAkhosh SomarajanÎncă nu există evaluări
- Opportunity, Challenge and Scope of Natural Products in Medicinal ChemistryDocument434 paginiOpportunity, Challenge and Scope of Natural Products in Medicinal ChemistryCamilla Karen Fernandes Carneiro100% (1)
- DentistDocument3 paginiDentistuhurtuyÎncă nu există evaluări
- New Zealand Data Sheet: ActionsDocument17 paginiNew Zealand Data Sheet: Actionsheri siswanto nur sidikÎncă nu există evaluări
- Burnout: From Popular Culture To Psychiatric Diagnosis in SwedenDocument21 paginiBurnout: From Popular Culture To Psychiatric Diagnosis in SwedenRajan PandaÎncă nu există evaluări
- Traction PDFDocument31 paginiTraction PDFrushaliÎncă nu există evaluări
- Chapter 1 Essay NegligenceDocument3 paginiChapter 1 Essay NegligenceVladimir Hechavarria100% (1)
- Visual NeglectDocument2 paginiVisual NeglectPierre A. RodulfoÎncă nu există evaluări
- Daftar Pustaka NewDocument2 paginiDaftar Pustaka NewRini LianingsihÎncă nu există evaluări
- Duty Report RIWDocument41 paginiDuty Report RIWRiyan W. PratamaÎncă nu există evaluări
- Gattefossé Nov 2015 Efficient Skin Delivery No Compromise With TranscutolDocument16 paginiGattefossé Nov 2015 Efficient Skin Delivery No Compromise With TranscutolJoaozinhoMéndezÎncă nu există evaluări
- Mic Eales A Visual Enquiry Into SuicideDocument4 paginiMic Eales A Visual Enquiry Into Suicidemaribolla8015Încă nu există evaluări