Documente Academic
Documente Profesional
Documente Cultură
Clinical Chemistry
Încărcat de
leizej290 evaluări0% au considerat acest document util (0 voturi)
637 vizualizări8 paginiCALCIUM HOMEOSTASIS AND HORMONAL REGULATION
Drepturi de autor
© © All Rights Reserved
Formate disponibile
DOCX, PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentCALCIUM HOMEOSTASIS AND HORMONAL REGULATION
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca DOCX, PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
637 vizualizări8 paginiClinical Chemistry
Încărcat de
leizej29CALCIUM HOMEOSTASIS AND HORMONAL REGULATION
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca DOCX, PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 8
Clinical Chemistry 3 Lecture 5
CALCIUM HOMEOSTASIS AND HORMONAL REGULATION
Roles of Calcium
Signal transduction pathways
acts as a second messenger, in
neurotransmitter release from neurons
Contraction of all muscle cell types
Fertilization
Enzyme cofactor
blood-clotting cascade
Proper bone formation
PRINCIPAL ORGANS INVOLVED IN CALCIUM
HOMEOSTASIS
Small Intestines
Bones (Skeletal System)
Kidneys
Normal Total Calcium: 2.2-2.6 mmol/L (9-10.5 mg/dL)
Normal Ionized Calcium: 1.1-1.4 mmol/L (4.5-5.6 mg/dL).
CALCIUM HOMEOSTASIS
HORMONAL CONTROL OF CALCIUM METABOLISM
Parathyroid Hormone
Vitamin D
A hormone
Structurally similar steroid hormones
a metabolic product of the cholesterol synthetic
pathway
Tissues involved in the synthesis:
Skin
Liver
Kidneys
Target Organs:
Gut
Bone
Parathyroids
VITAMIN D SYNTHESIS
Parathyroid Hormone
secreted from four parathyroid glands in the region of
the thyroid gland
Hormonal Control of Calcium Metabolism
HYPERCALCEMIA
the state of blood calcium levels above the expected
normal range in a healthy population
ionized or free calciumbiologically active 50%
bound calcium
Albumin
Citrate
Phosphate
Signs and Symptoms of Hypercalcemia
Central nervous system
Altered central nervous system function
Lethargy
Decreased alertness
Depression
Confusion
Forgetfulness
Obtundation
Coma
GASTRO-INTESTINAL
Anorexia
Constipation
Nausea and vomiting
Renal
Calcium acts as a diuretic and impairs the kidneys ability
to concentrate urine
Dehydration
hypercalciuria
increases the risk of calcium-
containing kidney stone
Skeletal
Patients with most causes of hypercalcemia have
increased bone resorption
increased bone
demineralization, leading to
increased fracture risk
Cardiovascular
Hypercalcemia may cause or exacerbate hypertension
ECG: shortened QT interval
Endocrine Causes of Hypercalcemia
Primary Hyperparathyroidism
parathyroid adenoma/hyperplasia
MEN 1
result in tumors of the parathyroids,
pituitary, and pancreas
loss of a tumor suppressor gene that
maps to human chromosome 11
MEN 2
result in tumors of the parathyroids,
medullary thyroid hyperplasia or
cancer, and pheochromocytoma
activating mutation in the ret proto-
oncogene, which resides on human
chromosome 10
Familial hyperparathyroidism
results in primary HPT, without other associated tumors
mapped to human chromosome 1.14
Familial hypocalciuric hypercalcemia (FHH)
result of a mutation in the calcium- sensing receptor and
thus an increased set point for calcium homeostasis
mild hypercalcemia and hyperparathyroidism
Parathyroid hormonerelated protein (PTHrP)
-substance very similar in structure to PTH
-produced by a variety of benign and malignant tumors
Breast
Lung
Kidney
Lymphoma
-PTHrP shares the N- terminal sequence homology with
PTH, it acts similarly and can cause hypercalcemia.
Milk-alkali Syndrome (Burnetts Syndrome)
results from the ingestion of large amounts of calcium
together with an absorbable alkali
patients being treated for peptic ulcers using carbonate
or bicarbonate salts with milk or cream
can lead to:
Hypercalcemia
Metabolic alkalosis
Renal impairment
HYPOCALCEMIA
the state of blood calcium levels below the expected
normal range in a healthy population
Signs and Symptoms of Hypocalcemia
Neuromuscular
Chvosteks sign
Numbness and tingling in the face,
hands, and feet may be seen
Trousseaus sign
Central nervous system
Irritability
Seizures
Personality changes
Impaired intellectual functioning
Cardiovascular
Cardiac contractile dysfunction
METABOLIC BONE DISEASES
Rickets and Osteomalacia
Rickets
refers to the disease state in growing
bone (in children).
Osteomalacia
refers to the abnormal mineralization
of bone in adults, or after closure of
the ephiphysial plates.
Osteoporosis
the most prevalent metabolic bone
disease in adults.
Clinical Chemistry 3 Lecture 4
THE THYROID GLAND
The Thyroid Gland
Produces 2 hormones:
Thyroid Hormones (T3 & T4)
produced by thyrocytes
critical in regulating body
metabolism, neurologic development, and
numerous other body functions
Calcitonin
produced by parafollicular cells C
involved in calcium homeostasis
Thyroid Anatomy and Development
Location: Lower Anterior Neck
Shape: butterfly, consisting of 2 lobes and an isthmus
Weight: 16-30 grams in adults
Embryology: outpouching of the foregut at the base of the
tongue
Thyroid Hormone Synthesis
Metabolism of Thyroxine
Three Forms Of Iodothyronine 5-deiodinase
Type 1 iodothyronine 5-deiodinase
the most abundant form
found mostly in the liver and
kidney
responsible for the largest
contribution to the circulating T3 pool
Type 2 iodothyronine 5-deiodinase
found in the brain and
pituitary gland
maintain constant levels of
T3 in the central nervous system
Type 3 iodothyronine 5-deiodinase
found in fetal tissues
prevent the rise of serum T3
they maintain high levels of
rT3 during intrauterine life
Protein Binding of Thyroid Hormone
Thyroxin-binding Globulin (TBG)
Thyroxin-binding Prealbumin
Albumin
Control of Thyroid Function
TESTS FOR THYROID EVALUATION
TSH
most useful test for assessing thyroid
function is the TSH
T3 & T4
usually measured by:
radioimmunoassay
(RIA)
chemiluminometric
assay
similar
immunometric technique
Thyroglobulin
measured by
double- antibody RIA
enzyme-linked immunoassay
(ELISA)
immunoradiometric assay
(IRMA)
immunochemilu- minescent
assay (ICMA) methods
INTERPRETATION OF THYROID TESTS
#PREVALENCE OF THYROID AUTOANTIBODIES
Hypothyroidism
Decreased free T4 with normal to elevated TSH
TYPES OF HYPOTHYROIDISM
Primary
Thyroid gland dysfunction
Secondary
Pituitary dysfunction
Tertiary
Hypothalamic dysfunction
CAUSES OF HYPOTHYROIDISM
Thyrotoxicosis
constellation of findings that result when
peripheral tissues are presented with, and
respond to, an excess of thyroid hormone.
Causes:
excessive thyroid hormone ingestion
leakage of stored thyroid hormone
from storage in the thyroid follicles
excessive thyroid gland production of
thyroid hormone
SIGNS AND SYMPTOMS OF THYROTOXICOSIS
Signs
Tachycardia
Tremor
Warm, moist, flushed, smooth skin
Lid lag, widened palpebral fissures Ophthalmopathy
(Graves disease)
Goiter
Brisk deep tendon reflexes
Muscle wasting and weakness
Dermopathy/pretibial myexedema (Graves disease)
Osteopenia, osteoporosis
Symptoms
Nervousness, irritability, anxiety
Tremor
Palpitations
Fatigue, weakness, decreased exercise tolerance
Weight loss
Heat intolerance
Hyperdefecation
Menstrual changes (oligomenorrhea)
Prominence of eyes
Graves Disease
the most common cause of thyrotoxicosis
an autoimmune disease in which antibodies are
produced that activate the TSH receptor
DISORDERS ASSOCIATED WITH THYROTOXICOSIS
Clinical Chemistry 3 Lecture 6
LIVER FUNCTION
Gross Anatomy Of The Liver
Blood Supply of the Liver
Excretory System Of The Liver
Microscopic Anatomy
BIOCHEMICAL FUNCTIONS
Four Major Functions:
Excretion/secretion
Synthesis
Detoxification
Storage
EXCRETORY AND SECRETORY
Transforms unconjugated to conjugated
bilirubin
Ligandin
responsible for transporting
unconjugated bilirubin to the
endoplasmic reticulum,
where it may be rapidly
conjugated
METABOLISM OF BILIRUBIN
SYNTHETIC
Responsible for synthesizing:
Carbohydrates
use the glucose for its own
cellular energy requirements
circulate the glucose for use
at the peripheral tissues
store glucose as glycogen
(principal storage form of
glucose) within the liver itself
or within other tissues
Lipids
approximately 70% of the
daily production of
cholesterol (roughly 1.52.0
g)
Proteins
Almost all proteins are
synthesized by the liver
except for the
immunoglobulins and adult
hemoglobin
DETOXIFICATION AND DRUG METABOLISM
serves as a gatekeeper between substances
absorbed by the gastrointestinal tract and those
released into systemic circulation
LIVER FUNCTION ALTERATIONS DURING DISEASE
JAUNDICE
Upper normal limit of total bilirubin
1.0-1.5 mg/dL
Jaundice is noticeable at 3.0 mg/dL
ICTERUS
used in the clinical laboratory to refer to a serum
or plasma sample with a yellow discoloration
due to an elevated bilirubin level
CLASSIFICATION OF JAUNDICE
GILBERT DISEASE
reduced activity of the enzyme
glucuronyltransferase, which conjugates bilirubin
and a few other lipophilic molecules
CRIGLER-NAJJAR SYNDROME TYPE 1
Mode of Inheritance:
Autosomal Recessive
characterised by:
serum bilirubin usually above 345
mol/L (310755 mg/dL)
no UGT1A1 (UDP
glucuronosyltransferase 1 family,
polypeptide A1) expression
no response to treatment with
phenobarbital*
CRIGLER-NAJJAR SYNDROME TYPE 2
Type II differs from type I in several aspects:
Bilirubin levels are generally below 345
mol/L (100430 mg/dL) and some
cases are only detected later in life.
Because of lower serum bilirubin,
kernicterus is rare in type II.
Bile is pigmented, instead of pale in
type I or dark as normal, and
monoconjugates constitute the largest
fraction of bile conjugates.
UGT1A1 is present at reduced but
detectable levels (typically <10% of
normal), because of single base pair
mutations.
Therefore, treatment with
phenobarbital is effective, generally
with a decrease of at least 25% in
serum bilirubin. In fact, this can be
used, along with these other factors, to
differentiate type I and II.
The inheritance pattern of Crigler
Najjar syndrome type II has been
difficult to determine but is generally
considered to be autosomal recessive.
[
DUBIN-JOHNSON SYNDROME
An autosomal recessive disorder
Increase of conjugated bilirubin in the serum
without elevation of liver enzymes (ALT, AST)
Defect in the ability of hepatocytes to secrete
conjugated bilirubin into the bile
Diagnosis
A hallmark of DJS is the unusual ratio
between the byproducts of heme
biosynthesis.
Unaffected subjects have a
coproporphyrin III to
coproporphyrin I ratio of
approximately 34:1.
In patients with DJS, this
ratio is inverted with
coproporphyrin I being 34x
higher than coproporphyrin
III.
ROTOR SYNDROME
CIRRHOSIS
clinical condition in which scar tissue replaces
normal, healthy liver tissue
scar tissue replaces the normal liver tissue
blocking the flow of blood through the organ and
prevents the liver from functioning properly
Causes:
Chronic Alcoholism
Chronic Hepatitis B, C, D
autoimmune hepatitis
inherited disorders (e.g., 1-antitrypsin
deficiency, Wilson disease,
hemachromatosis, and galactosemia)
nonalcoholic steatohepatitis
blocked bile ducts
Drugs
Toxins
infections
REYE SYNDROME
a term used to describe a group of disorders
caused by infectious, metabolic, toxic, or drug-
induced disease found almost exclusively in
children
Associted with:
viral syndrome
Varicella
Gastroenteritis
upper respiratory tract
infection such as influenza
aspirin during a viral syndrome
ASSESSMENT OF LIVER FUNCTION/LIVER FUNCTION
TESTS
Review:
BILIRUBIN
Ehrlichs (Diazo) Reaction
diazotized Sulfanilic Acid +
Urine colored product
(RED)= urobilinogen
Van den Bergh Reaction
determines the amount of
conjugated bilirubin in the
blood
the reaction produces
azobilirubin
Principle: diazotised sulfanilic
acid + serum + stabilizer =
produce purple colored
azobilirubin
Malloy and Evelyn Reaction
Principle: diazotised sulfanilic
acid + serum + 50% methanol
(accelerator)= RED PURPLE
Jendrassik and Grof
Principle: diazotised sulfanilic
acid + serum + caffeine-
benzoate-acetate
(accelerator)= PURPLE
REFERENCE RANGES FOR BILIRUBIN IN
ADULTS AND INFANTS
DETERMINATION OF UROBILINOGEN
(SEMIQUANTITATIVE)
Principle
Urobilinogen (Urine) + p-dimethyl
aminobenzaldehyde (Ehrlichs reagent)
= red color
Reference Range (Urine)
0.11.0 Ehrlich units every 2 hours
0.54.0 Ehrlich units per day (0.86.8
mmol/day)
Reference Range (Fecal)
75275 Ehrlich units per 100 g of fresh
feces
75400 Ehrlich units per 24-hour
specimen
LIVER ENZYMES
Most Clinically Useful:
Aminotranferases
alanine amino transferase [ALT]
SGPT
aspartate aminotransferase [AST])
SGOT
Phosphatases
alkaline phosphatase [ALP]
5- neucleotidase)
Gamma -glutamyltransferase (GGT)
Lactate dehydrogenase
AMINOTRANFERASES
ALT a more liver-specific marker than AST
the serum activity of both transaminases rises
rapidly in almost all diseases of the liver and may
remain elevated for up to 26 weeks
Markedly increased in:
viral hepatitis
drug- and toxin-induced liver necrosis
Hepatic ischemia
Normal or only mildly elevated in:
cases of obstructive liver damage
PHOSPHATASES
Alkaline Phosphatase
zinc metalloenzymes
widely distributed in all tissues
marker of extrahepatic biliary obstruction
stone in the common bile duct
intrahepatic cholestasis
drug cholestasis
primary biliary cirrhosis
moderate increase:
hepatocellular disorders such as hepatitis and
cirrhosis
5-Nucleotidase
responsible for catalyzing the
hydrolysis of neucleoside-5-phosphate
ester
serum levels become significantly
elevated in hepatobiliary disease
more liver specific compared to ALP
PHOSPHATASES
membrane-localized enzyme found in
high concentrations in the kidney, liver,
pancreas, intestine, and prostate but
not in bone
plays a role in differentiating the cause
of elevated levels of ALP
highest levels of GGT are
seen in biliary obstruction
hepatic microsomal enzyme
ingestion of alcohol or
certain drugs elevates GGT
Barbiturates
Tricyclic
Antidepressants
Anticonvulsants
a sensitive test for cholestasis caused
by chronic alcohol or drug ingestion
useful if jaundice is absent for the
confirmation of hepatic neoplasms
an enzyme with a very wide
distribution throughout the body
released into circulation when cells of
the body are damaged or destroyed
serves as a general, nonspecific marker
of cellular injury
Tests Measuring Hepatic Synthetic Ability
SERUM PROTEINS
Useful in quantitating the severity of hepatic
dysfunction
Not sensitive to minimal liver damage
SERUM ALBUMIN
correlates well with the severity of functional
impairment
chronic rather than in acute liver disease
(decreased)
SERUM -GLOBULINS
decrease with chronic liver disease
low or absent -globulin suggests -
antitrypsin deficiency as the cause of
the chronic liver disease
SERUM -GLOBULIN
transiently increased in acute liver
disease
elevated in chronic liver disease
IgG and IgM levels chronic
active hepatitis
IgM Primary Biliary
Cirrhosis
IgA Alcoholic Cirrhosis
PROTHROMBIN
Decreased
Prothrombin Time is prolonged
Indicates severe diffuse liver disease
and a poor prognosis
Tests Measuring Nitrogen Metabolism
PLASMA AMMONIA
a reflection of the livers ability to
convert ammonia to urea so that it can
be excreted through the kidneys
increase in the bloodstream and may
ultimately cause hepatic coma
HEPATITIS
Serology Of Hepatitis B Infection With Recovery
Serology Of Chronic Hepatitis With Formation Of
Antibody To HBeAg
TYPICAL INTERPRETATION OF SEROLOGIC TEST RESULTS
FOR HBV INFECTION
SEROLOGICAL PROFILES OF CHRONIC HEPATITIS B VIRUS
INFECTION
CLINICAL FEATURES OF HEPATITIS D VIRUS (HDV)
COINFECTION AND SUPERINFECTION IN HEPATITIS B
VIRUS (HBV) CARRIERS
S-ar putea să vă placă și
- Immunology & Serology Review NotesDocument4 paginiImmunology & Serology Review Notesmaria email86% (7)
- Clinical Chemistry Reviewer by MTRDocument56 paginiClinical Chemistry Reviewer by MTRRyan Pan95% (19)
- Hematology - Steininger ReviewDocument30 paginiHematology - Steininger ReviewIssa AlejoÎncă nu există evaluări
- Hematology Review NotesDocument28 paginiHematology Review NotesMeLaiyee89% (9)
- Lecture & Review Guide in HEMATOLOGY 1 & 2 (COMPLETE)Document58 paginiLecture & Review Guide in HEMATOLOGY 1 & 2 (COMPLETE)Kirt Anonuevo100% (3)
- University of The Immaculate Conception: ProteinDocument13 paginiUniversity of The Immaculate Conception: ProteinDams ZainalÎncă nu există evaluări
- Chapter 14 Red Blood CellsDocument37 paginiChapter 14 Red Blood CellsCatherine LiuÎncă nu există evaluări
- Medtech NotesDocument23 paginiMedtech NotesOnline PrometricÎncă nu există evaluări
- Reviewer - Immunohematology - Part 1Document16 paginiReviewer - Immunohematology - Part 1Joshua TrinidadÎncă nu există evaluări
- Urinalysis and Body Fluids Q & ADocument79 paginiUrinalysis and Body Fluids Q & ADarla YsavelÎncă nu există evaluări
- MUST To KNOW in Clinical ChemistryDocument53 paginiMUST To KNOW in Clinical ChemistryMonkey LuffyÎncă nu există evaluări
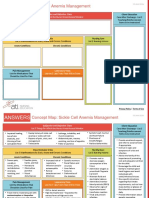
- NCC-SickleCellAnemiaManagement ConceptMap InteractivePDFDocument2 paginiNCC-SickleCellAnemiaManagement ConceptMap InteractivePDFLoggerz Arck100% (1)
- Chapter 1: An Overview of Clinical LaboratoryDocument13 paginiChapter 1: An Overview of Clinical LaboratoryAshley Tañamor100% (2)
- Clinical Microscopy ExamDocument3 paginiClinical Microscopy ExamKarla GiorlaÎncă nu există evaluări
- Immuno-Sero Lecture ReviewDocument11 paginiImmuno-Sero Lecture ReviewJohn Terrence M. RomeroÎncă nu există evaluări
- Hematology2 - Laboratory TestsDocument3 paginiHematology2 - Laboratory Testskthmnts100% (1)
- Hematology PDFDocument46 paginiHematology PDFGiannis GkouzionisÎncă nu există evaluări
- Hematology ReviewDocument4 paginiHematology ReviewAlfred ChowÎncă nu există evaluări
- Questions: 1: Blood Bank - Blood Group SystemsDocument10 paginiQuestions: 1: Blood Bank - Blood Group SystemsVincent ReyesÎncă nu există evaluări
- Clinical Chemistry NotesDocument24 paginiClinical Chemistry Notesclower112100% (3)
- Summary of Reagent Strip TestsDocument8 paginiSummary of Reagent Strip TestsDarla YsavelÎncă nu există evaluări
- Clinical Chemistry KeyNotes For Board ExaminationDocument12 paginiClinical Chemistry KeyNotes For Board ExaminationPrincess Alen Aguilar100% (2)
- MUST To KNOW in Blood Banking 1Document19 paginiMUST To KNOW in Blood Banking 1Aya Virtucio100% (1)
- 2nd Sem - Hema1 - An Overview of Clinical Laboratory HematologyDocument3 pagini2nd Sem - Hema1 - An Overview of Clinical Laboratory HematologyAisle Malibiran PalerÎncă nu există evaluări
- Hematology Ii Lectures Introduction To HemostasisDocument28 paginiHematology Ii Lectures Introduction To HemostasisJoshua Trinidad100% (1)
- Post Lab 01-09Document7 paginiPost Lab 01-09Patrick ParconÎncă nu există evaluări
- MUST To KNOW in HematologyDocument45 paginiMUST To KNOW in HematologyDen100% (4)
- Clinical Chemistry Board ReviewDocument14 paginiClinical Chemistry Board ReviewWellaBaylasÎncă nu există evaluări
- Mtap - Aubf Review Notes FinalsDocument8 paginiMtap - Aubf Review Notes FinalsMoira Pauline LibroraniaÎncă nu există evaluări
- Role of Blood Vessels in Hemostasis: Villa, M.D. MLS 4CDocument10 paginiRole of Blood Vessels in Hemostasis: Villa, M.D. MLS 4CMarianne Dennesse100% (1)
- HistopathDocument37 paginiHistopathFait HeeÎncă nu există evaluări
- Clinical ChemistryDocument12 paginiClinical ChemistryClark Lopez100% (1)
- Clinical ChemistryDocument26 paginiClinical Chemistryazoooz502Încă nu există evaluări
- Clinical Chemistry (Lecture) - PrelimsDocument12 paginiClinical Chemistry (Lecture) - Prelimsisprikitik3100% (1)
- List of Culture Media Used in Microbiology With Their UsesDocument7 paginiList of Culture Media Used in Microbiology With Their UsesImmu JiÎncă nu există evaluări
- CHEM 2 CH 29 Review QuestionsDocument2 paginiCHEM 2 CH 29 Review QuestionsthrowawyÎncă nu există evaluări
- Clinical Chemistry NotesDocument1 paginăClinical Chemistry Notesclower112Încă nu există evaluări
- MTAP ISBB - Sir JJ (Merged)Document9 paginiMTAP ISBB - Sir JJ (Merged)Nathan DrakeÎncă nu există evaluări
- Microbiology ReviewerDocument3 paginiMicrobiology ReviewerWendy Escalante100% (6)
- Reviewer in CCDocument43 paginiReviewer in CCanimateddrag08@yahoo.com86% (7)
- Hematology ReviewerDocument4 paginiHematology ReviewerAbigail Puno100% (1)
- Intro To Medtech Clinical Chemistry ReviewerDocument11 paginiIntro To Medtech Clinical Chemistry Reviewerjesanndei100% (1)
- Staphylococci: Streptococcus PyogenesDocument20 paginiStaphylococci: Streptococcus PyogenesPharmacy2015100% (2)
- Clinical Chemistry Mcqs Carbohydrates: RD THDocument20 paginiClinical Chemistry Mcqs Carbohydrates: RD THJoyce Rosette Cabutotan Vergara75% (4)
- Clinical Chemistry 2Document22 paginiClinical Chemistry 2Rubenne Miles ElagasÎncă nu există evaluări
- Lab ValuesDocument5 paginiLab Valuespragya_devkotaÎncă nu există evaluări
- MycoViro - Complete Handouts (AMCC)Document46 paginiMycoViro - Complete Handouts (AMCC)Martin Clyde100% (1)
- Bleeding: 1. Vessel Wall 2. Platelets 3. Coagulation Protein 4. Anticoagulant Protein 5. Fibrinolytic SystemDocument5 paginiBleeding: 1. Vessel Wall 2. Platelets 3. Coagulation Protein 4. Anticoagulant Protein 5. Fibrinolytic Systemsarguss14100% (3)
- Blood Bank Lab NotesDocument2 paginiBlood Bank Lab NotesSirias_black88% (8)
- CM Handouts Clinical MicrosDocument33 paginiCM Handouts Clinical Microsrenato renato100% (1)
- CLINICAL CHEMISTRY: Passbooks Study GuideDe la EverandCLINICAL CHEMISTRY: Passbooks Study GuideÎncă nu există evaluări
- Agglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4De la EverandAgglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4Încă nu există evaluări
- 5.2 Principles of Hormonal RegulationsDocument35 pagini5.2 Principles of Hormonal RegulationsSurvin KandhariÎncă nu există evaluări
- Endocrinology NotesDocument24 paginiEndocrinology NotesEmily Dong100% (1)
- Study Guide For NURS 320 Exam 2Document15 paginiStudy Guide For NURS 320 Exam 2Anthony Del RioÎncă nu există evaluări
- Intro To The Function of Thyroid GlandDocument35 paginiIntro To The Function of Thyroid Glandinka.elseÎncă nu există evaluări
- Endocrine Disorders: Harliansyah, PH.D Dept Biochemistry, FK-UYDocument23 paginiEndocrine Disorders: Harliansyah, PH.D Dept Biochemistry, FK-UYAffandi AkbarÎncă nu există evaluări
- Structure and Function of The Endocrine and Metabolic SystemDocument21 paginiStructure and Function of The Endocrine and Metabolic Systemcoy008Încă nu există evaluări
- Endocrine SystemDocument22 paginiEndocrine SystemLen Len Ochinang OchinangÎncă nu există evaluări
- SAQ 2nd Week (Thyroid Gland)Document15 paginiSAQ 2nd Week (Thyroid Gland)Josephine BediakoÎncă nu există evaluări
- 21 CP Endocrine 2Document73 pagini21 CP Endocrine 2Aman Singh RaoÎncă nu există evaluări
- Non-Invasive Prenatal Testing (NIPT)Document13 paginiNon-Invasive Prenatal Testing (NIPT)Andy WijayaÎncă nu există evaluări
- Test Bank For Maternity and Pediatric Nursing 2nd Edition Susan Scott RicciDocument7 paginiTest Bank For Maternity and Pediatric Nursing 2nd Edition Susan Scott RicciJulieJacobsrkozw100% (69)
- PLE Review OBGYN Chap 1 Overview of ObstetricsDocument2 paginiPLE Review OBGYN Chap 1 Overview of ObstetricsRemelou Garchitorena Alfelor100% (1)
- Yang 2017Document10 paginiYang 2017wendyÎncă nu există evaluări
- NCP Urinary Tract InfectionDocument4 paginiNCP Urinary Tract InfectiondollythesheepÎncă nu există evaluări
- Free Microbiology Practice Questions - Help Your Microbiology Test ScoreDocument3 paginiFree Microbiology Practice Questions - Help Your Microbiology Test ScoreDalbir SinghÎncă nu există evaluări
- TGF BDocument16 paginiTGF BmonikaÎncă nu există evaluări
- BiologyDocument9 paginiBiologyRichieÎncă nu există evaluări
- DAPI (4',6-Diamidine-2'-Phenylindole Dihydrochloride) : Cat. No. 10 236 276 001Document2 paginiDAPI (4',6-Diamidine-2'-Phenylindole Dihydrochloride) : Cat. No. 10 236 276 001Estefani BlancasÎncă nu există evaluări
- SP ACCURE InjectablesDocument8 paginiSP ACCURE Injectablessanjay_gawaliÎncă nu există evaluări
- Stenotrophomona Maltophilia y Bulkorelia Cepacia. Mnadell 2009Document8 paginiStenotrophomona Maltophilia y Bulkorelia Cepacia. Mnadell 2009Laura López Del Castillo LalydelcaÎncă nu există evaluări
- Phagocytic Immuno DefficienciesDocument38 paginiPhagocytic Immuno Defficienciesصدام حسینÎncă nu există evaluări
- Lesions of CervixDocument56 paginiLesions of Cervixvandana100% (1)
- Herpes GenitalisDocument13 paginiHerpes GenitalisNataša Ivaniš0% (1)
- QuinonesDocument2 paginiQuinonessuresh100% (1)
- B.tech. BiotechDocument23 paginiB.tech. BiotechSandhyaÎncă nu există evaluări
- Fragile X Syndrome: Group 3Document11 paginiFragile X Syndrome: Group 3mballestaÎncă nu există evaluări
- Protozoa StructuresDocument2 paginiProtozoa StructuresKyra Bianca R. FamacionÎncă nu există evaluări
- PCR, RT-PCR, Nested-Pcr, Multiplex PCR, Quantitative PCRDocument116 paginiPCR, RT-PCR, Nested-Pcr, Multiplex PCR, Quantitative PCRYunizardiÎncă nu există evaluări
- Exosome-Based Immunotherapy: A Promising Approach For Cancer TreatmentDocument16 paginiExosome-Based Immunotherapy: A Promising Approach For Cancer Treatment1810 15Marvin LionelÎncă nu există evaluări
- Diagnostic Criteria For The Behavioral Variant FTDDocument5 paginiDiagnostic Criteria For The Behavioral Variant FTDMusleh AlgarniÎncă nu există evaluări
- 16S RRNA Gene Sequencing For Bacterial IdentificationDocument4 pagini16S RRNA Gene Sequencing For Bacterial IdentificationBenjamin UcichÎncă nu există evaluări
- 1 s2.0 S1028455920301753 MainDocument4 pagini1 s2.0 S1028455920301753 MainAditi SoniÎncă nu există evaluări
- Postulat KochDocument11 paginiPostulat KochputriÎncă nu există evaluări
- RAASDocument5 paginiRAASJamaica VillonÎncă nu există evaluări
- Aphasia and DyslexiaDocument17 paginiAphasia and DyslexiaMary Christine GonzalesÎncă nu există evaluări
- Prevalence and Species Spectrum of Pulmonary Nontuberculous Mycobacteria Isolates at A Tertiary Care CenterDocument6 paginiPrevalence and Species Spectrum of Pulmonary Nontuberculous Mycobacteria Isolates at A Tertiary Care CenterHiroj BagdeÎncă nu există evaluări
- Rapid Review From Usmle ... Spotters and OnelinersDocument120 paginiRapid Review From Usmle ... Spotters and OnelinersViroop ReddyÎncă nu există evaluări
- The EBC 46 Cancer TreatmentDocument9 paginiThe EBC 46 Cancer TreatmentAnimefan TheoÎncă nu există evaluări