Documente Academic
Documente Profesional
Documente Cultură
Intraocular Pressure-Lowering Efficacy and Safety of Bimatoprost 0.03% Therapy For Primary Open-Angle Glaucoma and Ocular Hypertension Patients in China
Încărcat de
Ayu Ersya Windira0 evaluări0% au considerat acest document util (0 voturi)
8 vizualizări9 paginijurnal kesehatan mata
Titlu original
1471-2415-14-21
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentjurnal kesehatan mata
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
8 vizualizări9 paginiIntraocular Pressure-Lowering Efficacy and Safety of Bimatoprost 0.03% Therapy For Primary Open-Angle Glaucoma and Ocular Hypertension Patients in China
Încărcat de
Ayu Ersya Windirajurnal kesehatan mata
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 9
RESEARCH ARTI CLE Open Access
Intraocular pressure-lowering efficacy and
safety of bimatoprost 0.03% therapy for primary
open-angle glaucoma and ocular hypertension
patients in China
Kaidi Wang
1
, Li Xu
2
, Zhilan Yuan
3
, Ke Yao
4
, Junmei Zhao
5
, Liang Xu
6
, Aiwu Fang
7
, Mingzhi Zhang
8
, Lingling Wu
9
,
Jian Ji
10
, Jiamin Hou
11
, Qing Liu
12
and Xinghuai Sun
1*
Abstract
Background: To report the clinical outcomes in Chinese patients with primary open-angle glaucoma and ocular
hypertension treated with bimatoprost 0.03% therapy.
Methods: Two hundred sixty-three Chinese patients with primary open-angle glaucoma and ocular hypertension
who needed initial or additional intraocular pressure (IOP) lowering were recruited in this prospective, open-label,
multicenter clinical study and were treated with bimatoprost 0.03%. Patients received bimatoprost 0.03% as initial,
replacement or adjunctive IOP-lowering therapy, and follow-up visits were performed at week 1, and month 1
and 3 of the bimatoprost treatment. The efficacy outcome measure was the post-treatment IOP level. The safety
outcome measures included the rate of medication-related symptoms, physical signs, reported adverse events,
and the level of conjunctival hyperemia.
Results: Among 240 patients who could be categorized by pre-existing therapies and the bimatoprost therapy
regimen in the study, IOP values observed in all medication conditions showed significant IOP reduction at all
study visits compared with baseline. At 3 months, 8.0 3.7 mmHg (32.0%) reduction in IOP was observed in
treatment-naive patients after bimatoprost monotherapy; in the patients previously on various therapy regimens,
1.9 2.8 mmHg (9.5%) to 6.4 6.1 mmHg (24.8%) additional IOP lowering was achieved after switching to
bimatoprost monotherapy or bimatoprost combination therapy. The most common adverse event was conjunctival
hyperemia, mainly of trace and mild intensity.
Conclusions: Our results show that bimatoprost 0.03% was effective in lowering IOP with favorable safety in
Chinese primary open-angle glaucoma and ocular hypertension patients.
Keywords: Bimatoprost, Glaucoma, Ocular hypertension, Intraocular pressure, Conjunctival hyperemia
Background
Glaucoma is a major cause of blindness in the world, and
the increasing number of cases along with an aging popu-
lation makes it a huge epidemiologic challenge [1,2]. Con-
clusive evidence from many well-conducted clinical trials
have shown that intraocular pressure (IOP) reduction is
beneficial to control the glaucomatous damage for either
glaucoma or ocular hypertension patients [3-7].
To date, the prostaglandin/prostamide (PG/PM) class
of medications has been shown to be highly effective in
IOP lowering with favorable tolerance and hence are
used as the first-line ocular antihypertensive agents for
glaucoma treatment in many countries [8]. Among these
medications, the PM bimatoprost represents a pharma-
cologically distinct drug that has been approved on the
United States market since 2001 for glaucoma and ocu-
lar hypertension (OHT) treatment. Bimatoprost lowers
IOP by increasing both uveoscleral and trabecular aque-
ous humor outflow [9]. This hypotensive effect has been
* Correspondence: xhsun.sh@hotmail.com
1
Eye & ENT Hospital, Shanghai Medical College, Fudan University, Fenyang
Road 83, Shanghai, Xuhui District 200031, China
Full list of author information is available at the end of the article
2014 Wang et al.; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative
Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and
reproduction in any medium, provided the original work is properly credited.
Wang et al. BMC Ophthalmology 2014, 14:21
http://www.biomedcentral.com/1471-2415/14/21
consistently proven by numerous clinical studies, and
results demonstrated that bimatoprost provides greater
or similar reduction in IOP compared with latanoprost
and travoprost over the course of 24 hours and over the
long term [10-19]. Bimatoprost is generally well toler-
ated with common adverse effects of mild conjunctival
hyperemia, eyelash growth and ocular pruritus [9,20]. In
some countries, but not yet in China, a new 0.01% for-
mulation of bimatoprost is available; bimatoprost 0.01%
has been demonstrated to have efficacy equivalent to the
original bimatoprost 0.03% formulation and be associ-
ated with less frequent and less severe conjunctival
hyperemia [21].
As the data on clinical outcomes of bimatoprost in
Chinese glaucoma and OHT patients are sparse [19,22],
this study was designed to evaluate the IOP-lowering
efficacy and safety of bimatoprost 0.03% therapy in OHT
and primary open-angle glaucoma (POAG) patients in a
real world clinical setting in China.
Methods
Patients
Eligible patients were those who were either previously
untreated or treated with POAG or OHT and who re-
quired initial or further IOP-lowering therapy in the judg-
ment of the treating physician. The diagnosis of POAG
and OHT was made based on the criteria listed in the
European Glaucoma Society Guidelines [23]. A baseline
IOP of less than 35 mmHg was required for study entry.
Patients were only eligible if they were 18 years or older
and had not received topical ophthalmic bimatoprost
within the 3 months prior to the enrollment.
Key exclusion criteria included uncontrolled systemic
disease; known hypersensitivity or contraindications to
any components of the study medications; obvious ocular
diseases other than POAG or OHT; any corneal lesions
precluding accurate tonometry reading; a history of sur-
gery for glaucoma or cataract treatment or any other
intraocular surgery within past 3 months; recent use of
systemic medications of potential IOP impact; systemic or
topical steroid therapy within the previous 21 days or dur-
ing the study period; participation in other drug or devices
trials within 30 days before the enrollment; having preg-
nancy planned or being pregnant or nursing; and any
other condition that, in the investigators opinion, might
be harmful to the patient or influence the outcomes.
Study design and treatment
This was a prospective, open-label, multicenter clinical
study involving POAG and OHT patients who needed
further IOP lowering, in whom bimatoprost was used
either as monotherapy or as added medication to the pre-
existing therapy regimen. The study was conducted at 11
clinical sites across Northern, North Eastern, Eastern, and
Southern China from January 2010 to June 2011. The
study protocol was approved by a centralized ethics com-
mittee, the Ethics Committee of Eye & ENT Hospital,
Shanghai Medical College, Fudan University, Shanghai,
China, and this approval was accepted at each site. The
study was conducted in compliance with the Declaration
of Helsinki and Good Clinical Practices (GCP). All re-
cruited patients provided written informed consent.
Demographic characteristics, medical history, and
ophthalmic history were recorded prior to initiation of
bimatoprost medication. Ocular examination including
visual acuity test, slit-lamp biomicroscopy, tonometry,
and conjunctival hyperemia evaluation was performed at
baseline and all study visits. IOP was measured with a
Goldmann applanation tonometer between 8 AM and
10 AM, and the mean of 3 readings (5 min apart) was
recorded for analyses. The eligible eye was determined
as the eye with higher IOP at baseline, or the right eye if
both eyes had the same IOP. Conjunctival hyperemia
was evaluated with slit-lamp examination, which was
performed before tonometry.
Without a wash-out phase, all patients received 1 drop
of bimatoprost 0.03% (Lumigan 0.03%, Allergan, Irvine,
California, USA) once daily in the evening over the 3-
month observation period. Usage of any concurrent
non-PG IOP-lowering eye drops remained unchanged.
Follow-up data including the ophthalmic examination
results, the treatment regimen, and all adverse events
were collected at the end of week 1, and months 1 and
3. Patients were withdrawn if they became pregnant or
required a change of the treatment, or if the IOP was
lower than 6 mmHg.
The study outcome for efficacy was mean IOP level at
week 12. Safety outcomes included medication-related
symptoms, physical signs, reported adverse events, and the
level of conjunctiva hyperemia, which was graded on bio-
microscopic examination by the investigator on a 5-point
hyperemia grading scale: 0 = none, 0.5 = trace, 1 = mild,
2 = moderate, 3 = severe. The standard color photographs
on the Allergan bulbar hyperemia grading guide were used
as a comparison scale for the conjunctival hyperemia
grading. Photographs of the conjunctiva were taken at the
slit lamp as documentation.
Statistical analysis
All continuous variables are presented as mean stand-
ard deviation (SD) for the data with normal distribution,
and categorical variables are shown as number (%). In
the comparison between the mean IOP of each visit and
baseline, and the comparison between the mean IOP
drop from baseline at the month-1 visit and month-3 visit
in each group, paired-sample t-test was performed for
data of normal distribution, and Wilcoxons signed rank
test was performed for data of a non-normal distribution.
Wang et al. BMC Ophthalmology 2014, 14:21 Page 2 of 9
http://www.biomedcentral.com/1471-2415/14/21
To identify possible risk factors for conjunctival hype-
remia of grades 2 and 3, univariate logistic regression
analysis was carried out to determine the contribution of
possible risk factors including age, sex, diagnosis of POAG
or OHT, history of laser treatment for glaucoma, history
of surgical treatment for glaucoma, history of comorbidi-
ties (i.e., cardiovascular disease and hypertension), blood
pressure, and pre-study ocular medications. Multivariate
logistic regression models were developed including fac-
tors with P values of < 0.25. The estimated relative risk of
hyperemia in the model was represented by the odds ratio
(OR) with a 95% confidence interval (CI). All statistical
analyses were performed with SAS 8.0 (SAS Institute Inc.,
Cary, North Carolina, USA). A P value < 0.05 was consid-
ered statistically significant.
Results
Study population and patient demographics
A total of 263 eligible patients were enrolled in the study
for bimatoprost therapy. Overall, the mean age of the
study population was 48.7 years, and 58.9% of patients
were male. The diagnoses of POAG and OHT presented
in 81.4% and 18.6% of the 263 patients, respectively. The
most common medical conditions in addition to glaucoma
at baseline included history of laser treatment for glau-
coma (9.5%), history of surgical treatment for glaucoma
(21.8%), and systemic comorbidities (12.9%). Among 263
eligible patients, 240 patients were categorized by pre-
existing therapies and the bimatoprost therapy regimen in
the study, with Group A: treatment-naive patients who
received in-trial bimatoprost monotherapy; Group B: pre-
trial PG mono-treated patients who received in-trial
switch monotherapy with bimatoprost; Group C: pretrial
non-PG mono- or combination treated patients who re-
ceived in-trial switch monotherapy with bimatoprost;
Group D: pretrial PG combination-treated patients who
received in-trial PM replacement with bimatoprost; Group
E: pretrial non-PG mono- or combination treated patients
who received bimatoprost as an adjunctive agent in
addition to the previous treatment modality (Table 1).
There was an undefined group including 19 patients with
no follow-up data, 1 newly diagnosed patient who received
bimatoprost combination therapy, and 3 patients who al-
tered their therapy over the 3-month study period. All en-
rolled patients characteristics at baseline stratified by
treatment condition are also summarized in Table 2.
Two hundred and three patients (77.2%) completed all
study visits as planned, and 60 patients dropped out due
to losses to follow-up (34/263, 12.9%), protocol violation
(14/263, 5.3%), and adverse events (13/263, 4.9%).
IOP-lowering effects
IOP in the 23 patients in the undefined group was not
analyzed due to invalid data. For the other groups (Groups
A to E), all IOP data presented for the bimatoprost
therapy efficacy evaluation are from intent-to-treat (ITT)
analyses.
Mean baseline IOP values of the patients were
24.6 4.4 mmHg in Group A, 18.6 3.4 mmHg in
Group B, 19.8 4.0 mmHg in Group C, 21.4 5.3
mmHg in Group D, and 23.6 5.7 mmHg in Group E,
respectively.
Following bimatoprost treatment, IOP values observed
in all groups were reduced as early as 1 week and were
maintained during the study period of 3 months (Figure 1).
Significant reductions in mean IOP were observed in all
treatment groups at week 1, month 1, and month 3 when
compared to baseline (P < 0.05), with mean IOP ranging
from 15.7 2.6 mmHg (Group C) to 17.2 4.4 mmHg
(Group D) at month 3.
Moreover, the mean IOP changes from baseline of all
groups were significant (P < 0.05). In comparisons of the
level of IOP reduction between visits, data from week 1
were not included since there was no washout phase
before the bimatoprost treatment. Therefore, only a
comparison between the second and third follow-up
visits was performed, and results showed no significant
difference in the groups except for Group D, indicating a
consistent IOP-lowering effect of bimatoprost during the
study period. The greatest mean IOP change was found
in Group A, with a highly significant mean IOP change
of 7.4 3.8 mmHg (29.7%) at week 1, 8.0 3.3 mmHg
(32.0%) at month 1, and 8.0 3.7 mmHg (32.0%) at
month 3 (all P < 0.0001 compared with baseline). The
smallest mean IOP change presented in Group B, with a
mean IOP change of 2.4 2.5 mmHg (12.3%) at week
1, 2.1 2.9 mmHg (10.7%) at month 1, and 1.9
2.8 mmHg (9.5%) at month 3 (all P < 0.001 compared
with baseline) (Table 3).
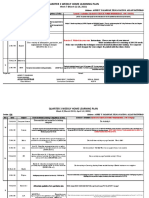
Table 1 Distribution of patients by pre-existing therapies
and the bimatoprost therapy regimen in the study, ITT
population
Baseline therapy
Bimatoprost therapy in the study
a
Bimatoprost
monotherapy
Bimatoprost combination
therapy (23 types)
None 89 (33.8%) NA
Group A
PG monotherapy 33 (12.5%) NA
Group B
PG combination therapy NA 18 (6.8%)
Group D
Non-PG monotherapy or
combination therapy
67 (25.5%) 33 (12.5%)
Group C Group E
a
Data are presented as n (%).
PG prostaglandin.
Wang et al. BMC Ophthalmology 2014, 14:21 Page 3 of 9
http://www.biomedcentral.com/1471-2415/14/21
Adverse events
Thirteen out of 263 enrolled patients failed to complete
at least one follow-up visit due to administrative reasons
or loss to follow-up. All other 250 patients were inclu-
ded in analyses of adverse events. Generally, the study
regimens with bimatoprost were well tolerated and no
serious adverse events were reported. The incidence and
types of treatment-related adverse events at each visit
are listed in Table 4.
Throughout the study, other than conjunctival hype-
remia, the most commonly reported adverse events were
eyelash growth, skin pigmentation, ocular pruritus, foreign
body sensation, and dry eyes, which occurred in 9.2%,
6.4%, 4.8%, 4.4%, and 3.6% of the 250 patients respectively.
All other adverse events occurred in less than 2% of the
patients, and most of them disappeared after continuing
therapy.
Conjunctival hyperemia
Conjunctival hyperemia was the most frequently repor-
ted side effect in the bimatoprost-treated patients. How-
ever, moderate to severe hyperemia was uncommon. The
mean percentage of patients with conjunctival hyperemia
Grade 2 (moderate) was 4.8%, 5.2%, and 4.2% of the 250
patients at week 1, month 1, and month 3 respectively;
Grade 3 (severe) conjunctival hyperemia was not noted in
any patient during the study (Figure 2A). Further-
more, the severity changes of conjunctival hyperemia
from baseline at each visit were mainly 0.5-grade increases
(Figure 2B).
The analyses of the associations between patient charac-
teristics and moderate to severe conjunctival hyperemia
(Grade 2 and 3) are shown in Table 5. In univariate logistic
regression models, no parameter was found to be signifi-
cantly associated with moderate to severe conjunctival
hyperemia, although the correlation between sex (higher
percentage of men) and moderate to severe conjunctival
hyperemia approached significance (P = 0.0711). A multi-
variate regression model using sex and history of laser
treatment as factors also identified no significant risk
factors for moderate to severe conjunctival hyperemia
(data not shown).
Discussion
In this multicenter clinical study, bimatoprost 0.3% ther-
apy was shown to provide substantial IOP lowering when
used in Chinese patients with glaucoma or OHT. The
mean IOP of patients who received either no previous
treatment (Group A) or other prior medications (Group
B-E) was significantly reduced after just 1 week of bima-
toprost treatment and maintained over the 3 months
study period. The occurrence of treatment-related adverse
Table 2 Patient characteristics at baseline
Characteristic
a
All enrolled N= 263 A N= 89 B N= 33 C N= 67 D N= 18 E N= 33 Undefined N= 23
Age (years) 48.7 16.6 44.6 15.3 48.2 20.5 52.1 15.7 52.8 12.5 54.1 18.2 44.4 14.7
Sex (male) 155 (58.9%) 47 (52.8%) 19 (57.6%) 45 (67.2%) 6 (33.3%) 22 (66.7%) 16 (69.6%)
Diagnosis
POAG 214 (81.4%) 53 (59.6%) 31 (93.9%) 64 (95.5%) 18 (100.0%) 32 (97.0%) 16 (69.6%)
OHT 49 (18.6%) 36 (40.4%) 2 (6.1%) 3 (4.5%) 0 1 (3.0%) 7 (30.4%)
Enrolled eye (OD) 141 (53.6%) 44 (49.4%) 17 (51.5%) 36 (53.7%) 13 (72.2%) 17 (51.5%) 14 (60.9%)
History of laser treatment for glaucoma 25 (9.5%) 7 (7.9%) 6 (18.2%) 6 (9.0%) 3 (16.7%) 1 (3.0%) 2 (8.7%)
History of surgical treatment for glaucoma 57 (21.8%) 10 (11.5%) 7 (21.2%) 14 (20.9%) 8 (44.4%) 11 (33.3%) 7 (30.4%)
Comorbidities 34 (12.9%) 4 (4.5%) 11 (33.3%) 10 (14.9%) 2 (11.1%) 7 (21.2%) 0
a
Continuous data are presented as mean SD and categorical data are presented as n (%).
POAG primary open-angle glaucoma; OHT ocular hypertension. Group A: treatment-naive patients received in-trial bimatoprost monotherapy; Group B: pretrial PG
mono-treated patients received in-trial switch monotherapy with bimatoprost; Group C: pretrial non-PG mono- or combination-treated patients received in-trial
switch monotherapy with bimatoprost; Group D: pretrial PG combination-treated patients received in-trial PM replacement with bimatoprost; Group E: pretrial
non-PG mono- or combination-treated patients received bimatoprost as an adjunctive agent in addition to the previous treatment modality.
14
16
18
20
22
24
26
Baseline Week 1 Month 1 Month 3
M
e
a
n
I
O
P
(
m
m
H
g
)
A
B
C
D
E
Figure 1 Mean IOP of the patients in groups A through E, ITT
population. Group A: treatment-naive patients received in-trial
bimatoprost monotherapy; Group B: pretrial PG mono-treated patients
received in-trial switch monotherapy with bimatoprost; Group C:
pretrial non-PG mono- or combination-treated patients received
in-trial switch monotherapy with bimatoprost; Group D: pretrial PG
combination-treated patients received in-trial PM replacement with
bimatoprost; Group E: pretrial non-PG mono- or combination-treated
patients received bimatoprost as an adjunctive agent in addition to
the previous treatment modality.
Wang et al. BMC Ophthalmology 2014, 14:21 Page 4 of 9
http://www.biomedcentral.com/1471-2415/14/21
Table 3 Mean IOP change from baseline and mean percentage change for groups A to E at each visit
IOP parameter
a
A N= 89 B N= 33 C N= 67 D N= 18 E N= 33
Baseline Mean IOP, mmHg 24.6 4.4 18.6 3.4 19.8 4.0 21.4 5.3 23.6 5.7
1 week IOP change, mmHg 7.4 3.8*** 2.4 2.5*** 4.5 3.6*** 4.0 4.8** 5.2 4.8***
Percentage change 29.7 13.7 12.3 11.9 21.7 16.0 15.6 18.6 20.8 18.0
1 month IOP change, mmHg 8.0 3.3*** 2.1 2.9*** 4.6 3.6*** 4.2 5.2* 6.7 6.1***
Percentage change 32.0 10.2 10.7 15.5 21.4 15.5 16.2 20.8 25.5 22.7
3 months IOP change, mmHg 8.0 3.7*** 1.9 2.8*** 4.1 3.5*** 5.3 5.1*** 6.4 6.1***
Percentage change 32.0 11.8 9.5 13.2 18.9 16.1 21.7 19.5 24.8 20.2
P value
b
0.6975 0.4192 0.1574 0.0279 0.6219
*P < 0.05, **P < 0.01, ***P < 0.001 compared with baseline IOP in this group using paired-sample t-test or Wilcoxons signed rank test.
a
Data are presented as mean SD.
b
Data comparison between the month-1 visit and month-3 visit in each group using paired-sample t-test or Wilcoxons signed rank test.
IOP intraocular pressure.
Group A: treatment-naive patients received in-trial bimatoprost monotherapy; Group B: pretrial PG mono-treated patients received in-trial switch monotherapy
with bimatoprost; Group C: pretrial non-PG mono- or combination-treated patients received in-trial switch monotherapy with bimatoprost; Group D: pretrial PG
combination-treated patients received in-trial PM replacement with bimatoprost; Group E: pretrial non-PG mono- or combination-treated patients received
bimatoprost as an adjunctive agent in addition to the previous treatment modality.
Table 4 Summary of adverse events excluding conjunctival hyperemia
AE Number (%)
Week 1 N= 250 Month 1 N= 232 Month 3 N= 212 Over the study N= 250
Eyelash growth 4 (1.6%) 16 (6.9%) 17 (8.0%) 23 (9.2%)
Skin pigmentation 5 (2.0%) 11 (4.7%) 12 (5.7%) 16 (6.4%)
Ocular pruritus 5 (2.0%) 9 (3.9%) 3 (1.4%) 12 (4.8%)
Foreign body sensation 6 (2.4%) 6 (2.6%) 1 (0.5%) 11 (4.4%)
Dry eyes 5 (2.0%) 6 (2.6%) 1 (0.5%) 9 (3.6%)
Conjunctivitis 1 (0.4%) 2 (0.9%) 1 (0.5%) 3 (1.2%)
Eye swelling pain 3 (1.2%) 1 (0.5%) 4 (1.6%)
Lachrymation 2 (0.8%) 2 (0.8%)
Ocular burning sensation 1 (0.4%) 1 (0.4%) 2 (0.8%)
Eye sore 1 (0.4%) 1 (0.4%)
Ocular stinging 2 (0.8%) 1 (0.4%) 3 (1.2%)
Ocular abnormal sensation 1 (0.4%) 1 (0.4%)
Ocular discharge 1 (0.4%) 1 (0.4%) 2 (0.8%)
Heavy feeling in eyelids 1 (0.4%) 1 (0.4%)
Corneal epithelial ulcer 1 (0.4%) 1 (0.4%)
Trichiasis 1 (0.5%) 1 (0.4%)
Conjunctival follicle 1 (0.4%) 1 (0.4%)
Subconjunctival hemorrhage 1 (0.4%) 1 (0.4%)
Slight visual acuity reduction 1 (0.4%) 1 (0.4%)
Fatigue 1 (0.4%) 1 (0.4%)
Headache 2 (0.8%) 1 (0.5%) 2 (0.8%)
Whole-body pruritus 1 (0.5%) 1 (0.4%)
Overall 28 (11.2%) 38 (16.4%) 32 (15.1%) 59 (23.6%)
AE adverse event.
Wang et al. BMC Ophthalmology 2014, 14:21 Page 5 of 9
http://www.biomedcentral.com/1471-2415/14/21
events including conjunctival hyperemia was acceptable,
with only 13 (4.9%) patients discontinuing the study medi-
cation because of adverse events.
Elevated IOP is the most significant risk factor for
optic nerve damage and visual field progression in glau-
coma patients [24,25]. The Early Manifest Glaucoma
Trial (EMGT) and Canadian Glaucoma Study have clearly
demonstrated that each 1 mmHg reduction in IOP corre-
sponds to 10% or 19% decrease in the risk of the progres-
sion of glaucomatous damage [26,27], suggesting the
importance of absolute IOP reduction during glaucoma or
OHT management. In the present study, the mean IOP
reductions from baseline IOP 3 months after in-trial
bimatoprost monotherapy were 8.0 3.7 mmHg (32.0
11.8%) in the treatment-naive patients, 1.9 2.8 mmHg
(9.5 13.2%) in pretrial PG mono-treated patients, and
4.1 3.5 mmHg (18.9 16.1%) in pretrial non-PG mono-
or combination-treated patients. After in-trial bimatoprost
combination therapy, mean IOP reductions at 3 months
were 5.3 5.1 mmHg (21.7 19.5%) in pretrial PG com-
bination-treated patients and 6.4 6.1 mmHg (24.8
20.2%) in pretrial non-PG mono- or combination treated
patients.
The IOP-lowering effects revealed in our study
were similar to the findings of other observational or
comparative clinical evaluations. Faridi and associates
found a 9.45 mmHg (36%) IOP reduction at 2 months and
a 9.23 mmHg (35%) IOP reduction at 6 months after
bimatoprost 0.03% monotherapy in newly diagnosed OHT
and POAG patients [18]. Quinones and Earl reported that
bimatoprost 0.03% monotherapy for glaucoma and OHT
provides 4.52 mmHg (21.52%) and 4.22 mmHg (19.63%)
additional IOP reduction after switching from topical
-blocker monotherapy at week 6 and week 12, respect-
ively [28]. Moreover, Feuerhake et als study with the fixed
combination of bimatoprost 0.03% and timolol 0.5% for
POAG or OHT showed 25.8% and 30.3% IOP lowering
after 3 months of replacement of previous -blocker mono-
therapy and 2-agonist monotherapy, respectively [29].
Of note, in the group of patients who underwent PG
medication treatment prior to the current study, bimato-
prost still had a significant effect on IOP lowering from
baseline, which was maintained throughout the study. A
further 1.9 mmHg (9.5%) and 5.3 mmHg (21.7%) IOP
drop was achieved after changing from PG to bimato-
prost in the monotherapy and combination therapy regi-
men groups, respectively, at month 3. Similarly, Kammer
and colleagues found an additional 1.9 mmHg and 2.1
mmHg mean diurnal IOP reduction from latanoprost
mono-treated baseline in glaucoma or OHT patients
after 1 and 3 months of bimatoprost 0.03% monotherapy
replacement, respectively, and this IOP-lowering efficacy
A
B
0
20
40
60
80
100
Baseline Week 1 Month 1 Month 3
P
e
r
c
e
n
t
a
g
e
o
f
p
a
t
i
e
n
t
s
0
0.5
1
2
3
0
10
20
30
40
Week 1 Month 1 Month 3
P
e
r
c
e
n
t
a
g
e
o
f
p
a
t
i
e
n
t
s
+ 0.5
+ 1
+ 1.5
+ 2
Figure 2 Conjunctival hyperemia scoring distribution at each visit.
A, Percentage of patients with each grade; B, Percentage of patients
with conjunctival hyperemia grade increase from baseline n = 250.
Table 5 Association between patient characteristics and
moderate to severe conjunctival hyperemia (grade 2 and 3)
in univariate logistic regression models
OR 95% CI P-value
Age, years 1.338 0.627- 2.856 0.4521
( 50 vs < 50)
Diagnosis 1.624 0.541- 4.877 0.3871
(POAG vs OHT)
Sex 2.178 0.935-5.072 0.0711
(male vs female)
History of laser treatment
for glaucoma
0.289 0.038-2.214 0.2321
(yes vs no)
History of surgical treatment
for glaucoma
0.882 0.342-2.275 0.7956
(yes vs no)
Comorbidities 1.346 0.479-3.783 0.5725
(yes vs no)
Hypertension 0.663 0.293-1.500 0.3237
(yes vs no)
Duration of pre-study antiglaucoma
medication use
1.257 0.592-2.668 0.5516
(< 1 month vs 1 month )
OR odds ratio; CI confidential interval.
Wang et al. BMC Ophthalmology 2014, 14:21 Page 6 of 9
http://www.biomedcentral.com/1471-2415/14/21
was significantly stronger when compared with switching
to travoprost monotherapy [14]. Data from a 24-month
study of OAG patients also demonstrated a 15.024.0%
additional reduction in IOP after changing latanoprost to
bimatoprost as monotherapy or in multi-therapy, before
adding a further adjunctive agent [30]. Together these
results suggest that bimatoprost may provide better IOP
control than PGs, which may be attributed in part to its
ocular distribution to outflow tissues and dual outflow
mechanism following topical administration [9,31]. Con-
sidering its highly cost-effective profile [32,33], bimato-
prost represents a promising hypotensive lipid to control
the elevated IOP in patients with POAG or OHT, espe-
cially when a substitution therapy is needed.
In this study, bimatoprost appeared to be clinically safe
and well tolerated since the overall treatment with-
drawals rate was low. The type and incidence of the
treatment-related adverse events were in agreement with
previous studies [34-37], with conjunctival hyperemia the
most commonly reported ocular adverse event. It should
be pointed out that, despite the relatively high overall inci-
dence, the majority of reported hyperemia cases were
trace or mild, and most of the patients with a hyperemia
increase from baseline had only a 0.5-grade increment. In
addition, no significant associations were found between
having moderate to severe conjunctival hyperemia and pa-
tient characteristics including age, sex, diagnosis of POAG
or OHT, history of laser treatment for glaucoma, history
of surgical treatment for glaucoma, comorbidities history,
blood pressure, and duration of pre-study antiglaucoma
medication use.
The mean age of patients in this study was 49 years. In a
previously published large, open-label study of real-world
use of travoprost in patients diagnosed with open-angle
glaucoma or ocular hypertension in China, the mean age
of patients was also 49 years [38]. The reasons that the
patients in these studies have tended to be younger than
the general glaucoma population are unknown, but beta-
blockers continue to be widely used in China because of
their good efficacy and low cost. For young patients with a
longer remaining life expectancy, physicians may be more
likely to recommend a PG or PM because of their superior
efficacy, and younger patients may be more willing to
accept the higher cost of these medications.
The study completion rate was only 77.2%, primarily
because 34 (12.9%) patients were lost to follow-up, includ-
ing 19 (7.2%) patients who had no post-baseline data and
were not included in the efficacy analysis. The patients
lost to follow-up were not contacted to determine why
they discontinued from the study, and it is possible that
some of these patients failed to return for study visits be-
cause of adverse effects, lack of efficacy, or dissatisfaction
with the study treatment. However, we believe that a more
likely explanation for the loss to follow-up is that many
patients who traveled to large cities to visit eye centers in
hospitals for diagnosis and treatment guidance were un-
willing to travel for follow-up. Patients who experienced
an intolerable adverse event may have been more likely to
return to the eye centers for guidance or a change in the
treatment regimen. Another study limitation was that
some of the reported adverse effects in patients using
more than one IOP-lowering medication may have been
caused by the other medications, rather than bimatoprost,
though the design of the study makes it difficult to
estimate how often this occurred.
Since previous clinical evaluations suggest that glau-
coma or OHT patients are rarely troubled by temporary
ocular side effects, specifically ocular redness [39,40],
the mild hyperemia after bimatoprost treatment did not
represent a clinical safety concern. The anticipated intro-
duction in China of the new bimatoprost 0.01% formula-
tion with the same efficacy and improved tolerability as
the original bimatoprost 0.03% formulation, as well as
education of patients explaining the importance of IOP
lowering and drug efficacy, may further improve their
acceptance and compliance [41].
Conclusions
The results of this 3-month multicenter clinical study
demonstrate clinically important and statistically signifi-
cant IOP-lowering efficacy of bimatoprost 0.03% for
POAG and OHT patients who were newly diagnosed or
requiring medication replacement or additional interven-
tion. Considering the efficacy together with the drugs
favorable tolerability profile, we conclude that the choice
of bimatoprost can be considered as first-line treatment
for POAG or OHT patients, and as a favorable switch or
adjunctive agent for those with a poor response to other
ocular hypotensive therapy regimens.
Competing interests
Kaidi Wang, Li Xu, Zhilan Yuan, Ke Yao, Junmei Zhao, Liang Xu, Aiwu Fang,
Mingzhi Zhang, Lingling Wu, Jian Ji, Jiamin Hou, and Xinghuai Sun have no
competing interests in bimatoprost or Allergan Information Consulting
(Shanghai) Co., Ltd. Qing Liu is employed by Allergan Information Consulting
(Shanghai) Co., Ltd.
Authors contributions
KW, LX, ZY, KY, JZ, LX, AF, MZ, LW, JJ, JH, XS: principal investigators for the
study involved in study design, data collection, data interpretation, and
drafting the manuscript; QL: data interpretation, drafting the manuscript, and
critical revision of the manuscript for English and important intellectual
content. All authors read and approved the final manuscript.
Acknowledgements
This study was sponsored by Allergan Information Consulting (Shanghai) Co.,
Ltd. Shanghai Careway Consulting Co., Ltd., performed the statistical analysis
of the data.
Author details
1
Eye & ENT Hospital, Shanghai Medical College, Fudan University, Fenyang
Road 83, Shanghai, Xuhui District 200031, China.
2
Department of
Ophthalmology, the Fourth Peoples Hospital of Shenyang, Shenyang, China.
3
Department of Ophthalmology, the Peoples Hospital of Jiangsu, Nanjing,
Wang et al. BMC Ophthalmology 2014, 14:21 Page 7 of 9
http://www.biomedcentral.com/1471-2415/14/21
China.
4
Eye Center of the 2nd Affiliated Hospital, Medical College of Zhejiang
University, Hangzhou, China.
5
Shanxi Eye Hospital, Taiyuan, China.
6
Beijing
Institute of Ophthalmology, Beijing Tongren Hospital, Capital University of
Medical Science, Beijing, China.
7
Eye Hospital, Wenzhou Medical College,
Wenzhou, China.
8
Joint Shantou International Eye Center, Shantou University
& the Chinese University of Hong Kong, Shantou, China.
9
Peking University
Third Hospital, Peking University Eye Center, Beijing, China.
10
Eye Centre of
Tianjin Medical University, Tianjin, China.
11
Eye Institute and Xiamen Eye
Center of Xiamen University, Xiamen, China.
12
Allergan Information
Consulting (Shanghai) Co., Ltd., Shanghai, China.
Received: 18 April 2013 Accepted: 19 February 2014
Published: 25 February 2014
References
1. Varma R, Lee PP, Goldberg I, Kotak S: An assessment of the health and
economic burdens of glaucoma. Am J Ophthalmol 2011, 152:515522.
2. Quigley HA, Broman AT: The number of people with glaucoma worldwide
in 2010 and 2020. Br J Ophthalmol 2006, 90:262267.
3. AGIS Investigators: The Advanced Glaucoma Intervention Study (AGIS): 7.
The relationship between control of intraocular pressure and visual field
deterioration. Am J Ophthalmol 2000, 130:429440.
4. Kass MA, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JL, Miller JP,
Parrish RK 2nd, Wilson MR, Gordon MO: The Ocular Hypertension
Treatment Study: a randomized trial determines that topical ocular
hypotensive medication delays or prevents the onset of primary
open-angle glaucoma. Arch Ophthalmol 2002, 120:701713.
5. Leske MC, Heijl A, Hussein M, Bengtsson B, Hyman L, Komaroff E, Early
Manifest Glaucoma Trial Group: Factors for glaucoma progression and the
effect of treatment: the early manifest glaucoma trial. Arch Ophthalmol
2003, 121:4856.
6. Ederer F, Gaasterland DA, Dally LG, Kim J, VanVeldhuisen PC, Blackwell B,
Prum B, Shafranov G, Allen RC, Beck A, AGIS Investigators: The Advanced
Glaucoma Intervention Study (AGIS): 13. Comparison of treatment
outcomes within race: 10-year results. Ophthalmology 2004, 111:651664.
7. Musch DC, Gillespie BW, Niziol LM, Lichter PR, Varma R, CIGTS Study Group:
Intraocular pressure control and long-term visual field loss in the
collaborative initial glaucoma treatment study. Ophthalmology 2011,
118:17661773.
8. Ishida N, Odani-Kawabata N, Shimazaki A, Hara H: Prostanoids in the
therapy of glaucoma. Cardiovasc Drug Rev 2006, 24:110.
9. Patil AJ, Vajaranant TS, Edward DP: Bimatoprosta review. Expert Opin
Pharmacother 2009, 10:27592768.
10. Konstas AG, Katsimbris JM, Lallos N, Boukaras GP, Jenkins JN, Stewart WC:
Latanoprost 0.005% versus bimatoprost 0.03% in primary open-angle
glaucoma patients. Ophthalmology 2005, 112:262266.
11. Orzalesi N, Rossetti L, Bottoli A, Fogagnolo P: Comparison of the effects of
latanoprost, travoprost, and bimatoprost on circadian intraocular
pressure in patients with glaucoma or ocular hypertension.
Ophthalmology 2006, 113:239246.
12. Stewart WC, Konstas AG, Nelson LA, Kruft B: Meta-analysis of 24-hour
intraocular pressure studies evaluating the efficacy of glaucoma
medicines. Ophthalmology 2008, 115:11171122.
13. Noecker RS, Dirks MS, Choplin NT, Bernstein P, Batoosingh AL, Whitcup SM,
Bimatoprost/Latanoprost Study Group: A six-month randomized clinical
trial comparing the intraocular pressure-lowering efficacy of bimatoprost
and latanoprost in patients with ocular hypertension or glaucoma.
Am J Ophthalmol 2003, 135:5563.
14. Parrish RK, Palmberg P, Sheu WP, XLT Study Group: A comparison of
latanoprost, bimatoprost, and travoprost in patients with elevated
intraocular pressure: a 12-week, randomized, masked-evaluator
multicenter study. Am J Ophthalmol 2003, 135:688703.
15. Cantor LB, Hoop J, Morgan L, Wudunn D, Catoira Y, Bimatoprost-Travoprost
Study Group: Intraocular pressure-lowering efficacy of bimatoprost 0.03%
and travoprost 0.004% in patients with glaucoma or ocular hypertension.
Br J Ophthalmol 2006, 90:13701373.
16. Aptel F, Cucherat M, Denis P: Efficacy and tolerability of prostaglandin
analogs: a meta-analysis of randomized controlled clinical trials.
J Glaucoma 2008, 17:667673.
17. Kammer JA, Katzman B, Ackerman SL, Hollander DA: Efficacy and
tolerability of bimatoprost versus travoprost in patients previously on
latanoprost: a 3-month, randomised, masked-evaluator, multicentre
study. Br J Ophthalmol 2010, 94:7479.
18. Faridi UA, Saleh TA, Ewings P, Venkateswaran M, Cadman DH, Samarasinghe
RA, Vodden J, Claridge KG: Comparative study of three prostaglandin
analogues in the treatment of newly diagnosed cases of ocular
hypertension, open-angle and normal tension glaucoma. Clin Exp
Ophthalmol 2010, 38:678682.
19. Huang HL, Sun XH, Xiao M: Comparison of intraocular pressure reducing
effects of three prostaglandin eyedrops in open-angle glaucoma.
Zhonghua Yan Ke Za Zhi 2011, 47:109113.
20. Curran MP: Bimatoprost: a review of its use in OAG and ocular
hypertension. Drugs Aging 2009, 26:10491071.
21. Katz LJ, Cohen JS, Batoosingh AL, Felix C, Shu V, Schiffman RM: Twelve-
month, randomized, controlled trial of bimatoprost 0.01%, 0.0125%, and
0.03% in patients with glaucoma or ocular hypertension. Am J
Ophthalmol 2010, 149:661671.
22. Chen MJ, Chen YC, Chou CK, Hsu WM: Comparison of the effects of
latanoprost and bimatoprost on intraocular pressure in chronic
angle-closure glaucoma. J Ocul Pharmacol Ther 2007, 23:559566.
23. European Glaucoma Society: Terminology and Guidelines for Glaucoma
(3rd Edition). http://www.eugs.org/eng/EGS_guidelines.asp.
24. Geringer C, Imami N: Medical management of glaucoma. Int Ophthamol
Clin 2008, 48:115141.
25. Coleman AL, Miglior S: Risk factors for glaucoma onset and progression.
Surv Ophthalmol 2008, 53(Suppl 1):S310.
26. Heijl A, Leske MC, Bengtsson B, Hyman L, Bengtsson B, Hussein M, Early
Manifest Glaucoma Trial Group: Reduction of intraocular pressure and
glaucoma progression: results from the Early Manifest Glaucoma Trial.
Arch Ophthalmol 2002, 120:12681279.
27. Chauhan BC, Mikelberg FS, Balaszi AG, LeBlanc RP, Lesk MR, Trope GE,
Canadian Glaucoma Study Group: Canadian Glaucoma Study: 2. risk
factors for the progression of open-angle glaucoma. Arch Ophthalmol
2008, 126:10301036.
28. Quinones R, Earl ML: The efficacy of bimatoprost 0.03% monotherapy
in patients previously using topical beta-blocker monotherapy for the
treatment of glaucoma or ocular hypertension. Adv Ther 2004,
21:370379.
29. Feuerhake C, Buchholz P, Kimmich F: Efficacy, tolerability and safety of the
fixed combination of bimatoprost 0.03% and timolol 0.5% in a broad
patient population: multicenter, open-label observational study. Curr Med
Res Opin 2009, 25:10371043.
30. Sonty S, Donthamsetti V, Vangipuram G, Ahmad A: Long-term IOP
lowering with bimatoprost in open-angle glaucoma patients poorly
responsive to latanoprost. J Ocul Pharmacol Ther 2008, 24:517520.
31. Ichhpujani P, Katz LJ, Hollo G, Shields CL, Shields JA, Marr B, Eagle R, Alvim
H, Wizov SS, Acheampong A, Chen J, Wheeler LA: Comparison of human
ocular distribution of bimatoprost and latanoprost. J Ocul Pharmacol Ther
2012, 28:134145.
32. Walt JG, Lee JT: A cost-effectiveness comparison of bimatoprost versus
latanoprost in patients with glaucoma or ocular hypertension.
Surv Ophthalmol 2004, 49(Suppl 1):S3644.
33. Gao Y, Wu L, Li A: Daily cost of glaucoma medications in China.
J Glaucoma 2007, 16:594597.
34. Wanichwecha-Rungruang B, Iemsomboon W: Efficacy and safety of
bimatoprost for the treatment of open-angle glaucoma and ocular
hypertension: a three-month, open-label study in community-based
practices in Thailand. J Med Assoc Thai 2005, 88:12281235.
35. Quinones R, Severin T, Mundorf T: Efficacy of bimatoprost 0.03 percent in
untreated glaucoma and ocular hypertension patients: results from a
large community-based clinical trial. J Ocul Pharmacol Ther 2004,
20:115122.
36. Whitson JT, Trattler WB, Matossian C, Williams J, Hollander DA: Ocular
surface tolerability of prostaglandin analogs in patients with glaucoma
or ocular hypertension. J Ocul Pharmacol Ther 2010, 26:287292.
37. Alagz G, Bayer A, Boran C, Serin D, Kkner A, Eliolu M: Comparison of
ocular surface side effects of topical travoprost and bimatoprost.
Ophthalmologica 2008, 222:161167.
38. Ge J, Sun XH, Wang NL, Zhao JL, Wu LL, Chen XM, Wang ZX, Li B:
Intraocular pressure lowering efficacy and safety of travoprost 0.004% as
a replacement therapy in patients with open angle glaucoma or ocular
hypertension. Chin Med J (Engl) 2010, 123:14171421.
Wang et al. BMC Ophthalmology 2014, 14:21 Page 8 of 9
http://www.biomedcentral.com/1471-2415/14/21
39. Herndon LW, Brunner TM, Rollins JN: The glaucoma research foundation
patient survey: patient understanding of glaucoma and its treatment.
Am J Ophthalmol 2006, 141(1 Suppl):S2227.
40. Abelson MB, Mroz M, Rosner SA, Dirks MS, Hirabayashi D: Multicenter,
open-label evaluation of hyperemia associated with use of bimatoprost
in adults with open-angle glaucoma or ocular hypertension.
Adv Ther 2003, 20:113.
41. Trattler W, Noecker RJ, Earl ML: A multicentre evaluation of the effect
of patient education on acceptance of hyperemia associated with
bimatoprost therapy for glaucoma or ocular hypertension.
Adv Ther 2008, 25:179189.
doi:10.1186/1471-2415-14-21
Cite this article as: Wang et al.: Intraocular pressure-lowering efficacy and
safety of bimatoprost 0.03% therapy for primary open-angle glaucoma
and ocular hypertension patients in China. BMC Ophthalmology 2014 14:21.
Submit your next manuscript to BioMed Central
and take full advantage of:
Convenient online submission
Thorough peer review
No space constraints or color gure charges
Immediate publication on acceptance
Inclusion in PubMed, CAS, Scopus and Google Scholar
Research which is freely available for redistribution
Submit your manuscript at
www.biomedcentral.com/submit
Wang et al. BMC Ophthalmology 2014, 14:21 Page 9 of 9
http://www.biomedcentral.com/1471-2415/14/21
S-ar putea să vă placă și
- Biophysical Properties in Glaucoma: Diagnostic TechnologiesDe la EverandBiophysical Properties in Glaucoma: Diagnostic TechnologiesIngrida JanulevicieneÎncă nu există evaluări
- Jurnal Mata 3Document4 paginiJurnal Mata 3Ami AntariksawatiÎncă nu există evaluări
- Pharmacoepidemiology and Pharmacovigilance: Synergistic Tools to Better Investigate Drug SafetyDe la EverandPharmacoepidemiology and Pharmacovigilance: Synergistic Tools to Better Investigate Drug SafetyEvaluare: 4.5 din 5 stele4.5/5 (3)
- Efficacy of Selective Laser Trabeculoplasty For Normal Tension Glaucoma: 1 Year ResultsDocument6 paginiEfficacy of Selective Laser Trabeculoplasty For Normal Tension Glaucoma: 1 Year ResultsdechastraÎncă nu există evaluări
- Lerner SFDocument9 paginiLerner SFAdriana FallaÎncă nu există evaluări
- Judul Skripsi 1aDocument8 paginiJudul Skripsi 1aMahmud AnshoriÎncă nu există evaluări
- JMedSci34262-4169833 - 113458 (FIX)Document4 paginiJMedSci34262-4169833 - 113458 (FIX)mas.dr90Încă nu există evaluări
- Obat GlaukomaDocument8 paginiObat GlaukomaMuhammad Farrash HadyanÎncă nu există evaluări
- Ijo 07 05 832 (1) AsddsaDocument5 paginiIjo 07 05 832 (1) AsddsaDyera JessenskyÎncă nu există evaluări
- Feldman RM, Katz G, McMenamy M, Hubatsch DADocument24 paginiFeldman RM, Katz G, McMenamy M, Hubatsch DAAdriana FallaÎncă nu există evaluări
- Imp Landmark Glauc StudiesDocument100 paginiImp Landmark Glauc StudiesASHOK KUMAR SINGHÎncă nu există evaluări
- Latanoprostene Bunod 0.024% Versus Timolol Maleate 0.5% in Subjects With Open-Angle Glaucoma or Ocular Hypertension The APOLLO StudyDocument11 paginiLatanoprostene Bunod 0.024% Versus Timolol Maleate 0.5% in Subjects With Open-Angle Glaucoma or Ocular Hypertension The APOLLO StudybungagladysÎncă nu există evaluări
- Aung T, Laganovska G, Hernandez Paredes TJ, Branch JDDocument8 paginiAung T, Laganovska G, Hernandez Paredes TJ, Branch JDAdriana FallaÎncă nu există evaluări
- Isi JurnalkuDocument8 paginiIsi JurnalkuTamsilÎncă nu există evaluări
- Jurnal Reading GlaucomaDocument6 paginiJurnal Reading GlaucomawidyawirapÎncă nu există evaluări
- Effects of Some Ophthalmic Medications On Pupil Size: A Literature ReviewDocument5 paginiEffects of Some Ophthalmic Medications On Pupil Size: A Literature ReviewOlvaria MisfaÎncă nu există evaluări
- Ni Hms 436399Document18 paginiNi Hms 436399Devanti EkaÎncă nu există evaluări
- 24-Hour Intraocular Pressure Control With Fixed-Dose Combination Brinzolamide 1%/brimonidine 0.2% A Multicenter, Randomized TrialDocument10 pagini24-Hour Intraocular Pressure Control With Fixed-Dose Combination Brinzolamide 1%/brimonidine 0.2% A Multicenter, Randomized TrialsondiÎncă nu există evaluări
- Low-Dose Cyclosporine Treatment For Sight-Threatening Uveitis: Efficacy, Toxicity, and ToleranceDocument8 paginiLow-Dose Cyclosporine Treatment For Sight-Threatening Uveitis: Efficacy, Toxicity, and ToleranceMauliza Resky NisaÎncă nu există evaluări
- tmpA9F9 TMPDocument5 paginitmpA9F9 TMPFrontiersÎncă nu există evaluări
- Medical Managaement of Pediatric GlaucomaDocument8 paginiMedical Managaement of Pediatric GlaucomaDinda Ajeng AninditaÎncă nu există evaluări
- 2015 Article 246Document15 pagini2015 Article 246RinaWulandariDjajoesmanÎncă nu există evaluări
- Effects of Postoperative Cyclosporine OphthalmicDocument7 paginiEffects of Postoperative Cyclosporine OphthalmicDr. Carlos Gilberto AlmodinÎncă nu există evaluări
- Intraocular Pressure After Phacoemulsification in Patients With Uncontrolled Primary Open Angle GlaucomaDocument6 paginiIntraocular Pressure After Phacoemulsification in Patients With Uncontrolled Primary Open Angle GlaucomaStevan Arta RisajayaÎncă nu există evaluări
- Laser in Glaucoma and Ocular Hypertension (LiGHT) Trial Six-Year Results of Primary Selective Laser Trabeculoplasty VersusDocument13 paginiLaser in Glaucoma and Ocular Hypertension (LiGHT) Trial Six-Year Results of Primary Selective Laser Trabeculoplasty VersusHanan NabilahÎncă nu există evaluări
- Risk Factors For Steroid Response Among Cataract PatientsDocument7 paginiRisk Factors For Steroid Response Among Cataract PatientsRodrigoBarreraÎncă nu există evaluări
- Critical Appraisal Nyimas Irina SilvaniDocument6 paginiCritical Appraisal Nyimas Irina SilvaniNyimas Irina SilvaniÎncă nu există evaluări
- Adherence To Fixed-Combination Versus Unfixed Travoprost 0.004%/timolol 0.5% For Glaucoma or Ocular Hypertension: A Randomized TrialDocument9 paginiAdherence To Fixed-Combination Versus Unfixed Travoprost 0.004%/timolol 0.5% For Glaucoma or Ocular Hypertension: A Randomized Trialyohanes22Încă nu există evaluări
- JurnalDocument7 paginiJurnalelita purnamaÎncă nu există evaluări
- The Effect of Prostaglandin Analogues On Central Corneal Thickness in Patients With GlaucomaDocument4 paginiThe Effect of Prostaglandin Analogues On Central Corneal Thickness in Patients With GlaucomarandyhermawanÎncă nu există evaluări
- Barber 1997 - Validation of A Questionnaire For Comparing The Tolerability of Ophthalmic MedicationsDocument9 paginiBarber 1997 - Validation of A Questionnaire For Comparing The Tolerability of Ophthalmic Medicationsflavio1Încă nu există evaluări
- First Experience With BAK-free Travoprost 0.004% in Topical Glaucoma MedicationDocument4 paginiFirst Experience With BAK-free Travoprost 0.004% in Topical Glaucoma Medicationsetiahermawan99Încă nu există evaluări
- 10mridula EtalDocument7 pagini10mridula EtaleditorijmrhsÎncă nu există evaluări
- OPTH 10337 Tolerability and Effectiveness of Preservative Free Dorzolam 061210Document10 paginiOPTH 10337 Tolerability and Effectiveness of Preservative Free Dorzolam 061210Pra BowoÎncă nu există evaluări
- Opth 9 367Document5 paginiOpth 9 367titisÎncă nu există evaluări
- Efikasi TX Gukoma 2016Document37 paginiEfikasi TX Gukoma 2016Al-Harits OctaÎncă nu există evaluări
- Clinical StudyDocument9 paginiClinical StudyNurul Dwi LestariÎncă nu există evaluări
- Kuwayama Adv Ther 2017-CompressedDocument15 paginiKuwayama Adv Ther 2017-Compressedgusnedi adamÎncă nu există evaluări
- Glaucoma 7Document7 paginiGlaucoma 7Sheila Kussler TalgattiÎncă nu există evaluări
- Menejemen Kronik Uveitis Anterior RekurenDocument6 paginiMenejemen Kronik Uveitis Anterior RekurenLuthfan HakimÎncă nu există evaluări
- R Detrimental Effect of Preservatives in Eyedrops: Implications For The Treatment of GlaucomaDocument11 paginiR Detrimental Effect of Preservatives in Eyedrops: Implications For The Treatment of GlaucomaSurendar KesavanÎncă nu există evaluări
- Pharmaco Epidemiology of Drugs Used in Post-CataraDocument5 paginiPharmaco Epidemiology of Drugs Used in Post-Catararirien refrina sariÎncă nu există evaluări
- Papers: Treatment of Ocular Hypertension and Open Angle Glaucoma: Meta-Analysis of Randomised Controlled TrialsDocument3 paginiPapers: Treatment of Ocular Hypertension and Open Angle Glaucoma: Meta-Analysis of Randomised Controlled TrialsDanil Anugrah JayaÎncă nu există evaluări
- Intraocular Pressure Elevation After Intravitreal or Posterior Sub-Tenon Triamcinolone Acetonide InjectionDocument6 paginiIntraocular Pressure Elevation After Intravitreal or Posterior Sub-Tenon Triamcinolone Acetonide InjectionMacarena AlvarezÎncă nu există evaluări
- Jurnal Mata Sodium Hyaluronate PDFDocument7 paginiJurnal Mata Sodium Hyaluronate PDFAstrid RumbiaÎncă nu există evaluări
- Pi Is 0161642016307357Document11 paginiPi Is 0161642016307357mono1144Încă nu există evaluări
- Intraocular Pressure 1 Year After Vitrectomy in Eyes Without A History of Glaucoma or Ocular HypertensionDocument7 paginiIntraocular Pressure 1 Year After Vitrectomy in Eyes Without A History of Glaucoma or Ocular HypertensionSyifa NahdiyahÎncă nu există evaluări
- Efficacy and Toxicity of Intravitreous Chemotherapy For Retinoblastoma: Four-Year ExperienceDocument8 paginiEfficacy and Toxicity of Intravitreous Chemotherapy For Retinoblastoma: Four-Year ExperienceSlr RandiÎncă nu există evaluări
- Innovations in Medical Management of GlaucomaDocument31 paginiInnovations in Medical Management of GlaucomaAnumeha Jindal100% (2)
- What We Have Learned From The Ocular Hypertension TreatmentDocument8 paginiWhat We Have Learned From The Ocular Hypertension TreatmentASHOK KUMAR SINGHÎncă nu există evaluări
- Steriod Cataract PDFDocument4 paginiSteriod Cataract PDFLisa IskandarÎncă nu există evaluări
- PT EduDocument4 paginiPT EduTasissa AyelaÎncă nu există evaluări
- PT EduDocument4 paginiPT EduTasissa AyelaÎncă nu există evaluări
- The Glymphatic System and New Etiopathogenic Hypotheses Concerning Glaucoma Based On Pilot Study On Glaucoma Patients Who Underwent Osteopathic Manipulative Treatment (OMT)Document7 paginiThe Glymphatic System and New Etiopathogenic Hypotheses Concerning Glaucoma Based On Pilot Study On Glaucoma Patients Who Underwent Osteopathic Manipulative Treatment (OMT)BOHR International Journal of Current Research in Optometry and Ophthalmology (BIJCROO)Încă nu există evaluări
- Referat HIFEMA Qowiyyu NurulDocument4 paginiReferat HIFEMA Qowiyyu NurulFahmiArifMuhammadÎncă nu există evaluări
- Comparative Study of Efficacies of Timolol Maleate and Brimonidine Tartrate in Primary Open Angle Glaucoma Patients As MonotherapyDocument6 paginiComparative Study of Efficacies of Timolol Maleate and Brimonidine Tartrate in Primary Open Angle Glaucoma Patients As MonotherapyInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- 1 s2.0 S1091853116304438 MainDocument6 pagini1 s2.0 S1091853116304438 MainMarcella PolittonÎncă nu există evaluări
- Treatment Satisfaction Among Patients Using Anti-In Ammatory Topical Medications For Dry Eye DiseaseDocument9 paginiTreatment Satisfaction Among Patients Using Anti-In Ammatory Topical Medications For Dry Eye DiseaseAndrés QueupumilÎncă nu există evaluări
- Clinical Study Ginkgo Biloba ExtractDocument7 paginiClinical Study Ginkgo Biloba ExtractHaris Cakrasana SatiadiÎncă nu există evaluări
- Efficacy of Topical Pilocarpine in The Management of Primary Aqueous Tear Deficiency: An Initial StudyDocument23 paginiEfficacy of Topical Pilocarpine in The Management of Primary Aqueous Tear Deficiency: An Initial StudytegarbondanÎncă nu există evaluări
- HIV Transmisions During SurgeryDocument1 paginăHIV Transmisions During SurgeryAyu Ersya WindiraÎncă nu există evaluări
- Hiv and AidsDocument4 paginiHiv and AidsAyu Ersya WindiraÎncă nu există evaluări
- Down Syndroms ScreeningDocument3 paginiDown Syndroms ScreeningAyu Ersya WindiraÎncă nu există evaluări
- HIV and DiscriminationDocument1 paginăHIV and DiscriminationAyu Ersya WindiraÎncă nu există evaluări
- Correspondence: Abortion Rates Still RisingDocument2 paginiCorrespondence: Abortion Rates Still RisingAyu Ersya WindiraÎncă nu există evaluări
- Vital Statisitic of BirthDocument1 paginăVital Statisitic of BirthAyu Ersya WindiraÎncă nu există evaluări
- Influenza VaccinationDocument1 paginăInfluenza VaccinationAyu Ersya WindiraÎncă nu există evaluări
- World Medical Journal Ed 9Document32 paginiWorld Medical Journal Ed 9ShalomBinyaminTovÎncă nu există evaluări
- P ('t':'3', 'I':'669094742') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Document6 paginiP ('t':'3', 'I':'669094742') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Ayu Ersya WindiraÎncă nu există evaluări
- Zidovudine in HIVDocument1 paginăZidovudine in HIVAyu Ersya WindiraÎncă nu există evaluări
- Carcinomas Diagnosed: Breast in The 1980sDocument1 paginăCarcinomas Diagnosed: Breast in The 1980sAyu Ersya WindiraÎncă nu există evaluări
- Child Sexual AbuseDocument2 paginiChild Sexual AbuseAyu Ersya WindiraÎncă nu există evaluări
- Correspondence: Abortion Rates Still RisingDocument2 paginiCorrespondence: Abortion Rates Still RisingAyu Ersya WindiraÎncă nu există evaluări
- Alcohol and Cardiovascular DiseaseDocument4 paginiAlcohol and Cardiovascular DiseaseAyu Ersya WindiraÎncă nu există evaluări
- Carcinomas Diagnosed: Breast in The 1980sDocument1 paginăCarcinomas Diagnosed: Breast in The 1980sAyu Ersya WindiraÎncă nu există evaluări
- Free Mdical in FormationsDocument95 paginiFree Mdical in FormationsmohammmmadÎncă nu există evaluări
- P ('t':'3', 'I':'669094742') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Document7 paginiP ('t':'3', 'I':'669094742') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Ayu Ersya WindiraÎncă nu există evaluări
- Gagal JantungDocument20 paginiGagal JantungAyu Ersya WindiraÎncă nu există evaluări
- Jurnal HifemaDocument10 paginiJurnal HifemaAndi NugrohoÎncă nu există evaluări
- P ('t':'3', 'I':'669094742') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Document7 paginiP ('t':'3', 'I':'669094742') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Ayu Ersya WindiraÎncă nu există evaluări
- Somatoform Disordes.Document9 paginiSomatoform Disordes.Aranda RickÎncă nu există evaluări
- P ('t':'3', 'I':'669094742') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Document6 paginiP ('t':'3', 'I':'669094742') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Ayu Ersya WindiraÎncă nu există evaluări
- Complications of Post PartumDocument49 paginiComplications of Post PartumNurulAqilahZulkifliÎncă nu există evaluări
- Complications of Post PartumDocument49 paginiComplications of Post PartumNurulAqilahZulkifliÎncă nu există evaluări
- Jurnal HifemaDocument10 paginiJurnal HifemaAndi NugrohoÎncă nu există evaluări
- 08 Anterior Segment Complications of Cataract SurgeryDocument19 pagini08 Anterior Segment Complications of Cataract SurgeryAyu Ersya WindiraÎncă nu există evaluări
- 08 Anterior Segment Complications of Cataract SurgeryDocument19 pagini08 Anterior Segment Complications of Cataract SurgeryAyu Ersya WindiraÎncă nu există evaluări
- DocumentDocument44 paginiDocumentAyu Ersya WindiraÎncă nu există evaluări
- Blok 1.5 Kuliah 2. Fisiologi ReproduksiDocument53 paginiBlok 1.5 Kuliah 2. Fisiologi ReproduksiAyu Ersya WindiraÎncă nu există evaluări
- 2 Reporting EndorsementDocument16 pagini2 Reporting Endorsementcarla yganÎncă nu există evaluări
- Anxiolytic Assessment of Centella Asiatica With Elevated Zero Maze and Elevated Plus Maze in RatsDocument6 paginiAnxiolytic Assessment of Centella Asiatica With Elevated Zero Maze and Elevated Plus Maze in RatsSanjesh kumarÎncă nu există evaluări
- Grade 10 Q2 Modules Week 1 4Document208 paginiGrade 10 Q2 Modules Week 1 4Hillary Faith GregoryÎncă nu există evaluări
- Effective Communication: Why Is It So Hard To Listen?Document3 paginiEffective Communication: Why Is It So Hard To Listen?Ariadne CulceÎncă nu există evaluări
- Authorized Test Center - Policies and Procedures PDFDocument365 paginiAuthorized Test Center - Policies and Procedures PDFNarra Venkata KrishnaÎncă nu există evaluări
- Feature WritingDocument3 paginiFeature WritingaddreenaÎncă nu există evaluări
- Hospivac 400 - 1087 400Document2 paginiHospivac 400 - 1087 400NASR EDDINE KEBDANI DIAGALÎncă nu există evaluări
- WildlifeTourism ReconnectingPeoplewithNatureDocument12 paginiWildlifeTourism ReconnectingPeoplewithNatureTarun TangoÎncă nu există evaluări
- Glioma: ClassificationDocument2 paginiGlioma: ClassificationAppas SahaÎncă nu există evaluări
- MEH EOI B1 Workbook Answer KeyDocument16 paginiMEH EOI B1 Workbook Answer KeyCarlos328Încă nu există evaluări
- BTBT4 HK2 MoiDocument63 paginiBTBT4 HK2 MoiLa ZoramÎncă nu există evaluări
- Corrosion/Undercutting Scribe Creepback: Worldwide Engineering StandardsDocument7 paginiCorrosion/Undercutting Scribe Creepback: Worldwide Engineering StandardsLynetteÎncă nu există evaluări
- Rape Epidemic in India - Woman and Criminal Law Project ReportDocument12 paginiRape Epidemic in India - Woman and Criminal Law Project ReportNimisha SajekarÎncă nu există evaluări
- Grade 10 Life Orientation 17 February 2023 Source Based Task Activity 1 ScopeDocument3 paginiGrade 10 Life Orientation 17 February 2023 Source Based Task Activity 1 ScopeMetse Pridy MatimolaneÎncă nu există evaluări
- Final Socio-Economic Feasibilty Study ReportDocument16 paginiFinal Socio-Economic Feasibilty Study ReportYousuf IÎncă nu există evaluări
- Drug Distribution To Human Tissues - Prediction and Examination of The Basic Assumption in in Vivo Pharmacokinetics-Pharmacodynamics ResearchDocument9 paginiDrug Distribution To Human Tissues - Prediction and Examination of The Basic Assumption in in Vivo Pharmacokinetics-Pharmacodynamics Researchopata edward kwameÎncă nu există evaluări
- Introduction To PLAB 1Document4 paginiIntroduction To PLAB 1Deeksha BhardwajÎncă nu există evaluări
- Boost Vocabulary Cambridge 16Document22 paginiBoost Vocabulary Cambridge 16Cẩm Tú NguyễnÎncă nu există evaluări
- Basic Sentence PatternsDocument54 paginiBasic Sentence PatternsAmalina ShadrinaÎncă nu există evaluări
- CDT Ipsita Paikaray. Od-19-Sw-A-304-336. The Role of NCC in Covid-19Document4 paginiCDT Ipsita Paikaray. Od-19-Sw-A-304-336. The Role of NCC in Covid-19Ē Vì LÎncă nu există evaluări
- Standard Renal Replacement Therapy Combined With HemoadsorptionDocument8 paginiStandard Renal Replacement Therapy Combined With HemoadsorptionMihai PopescuÎncă nu există evaluări
- Theoretical Foundation of Nursing: Environmental TheoryDocument27 paginiTheoretical Foundation of Nursing: Environmental TheoryJames Kurt CruzatÎncă nu există evaluări
- Week 7 (March 22-26, 2021)Document2 paginiWeek 7 (March 22-26, 2021)Achievers IntelligencesÎncă nu există evaluări
- IEP Example ElementaryDocument13 paginiIEP Example ElementaryArthur DumanayosÎncă nu există evaluări
- Fixed Space MaintainersDocument3 paginiFixed Space MaintainersElectricken21Încă nu există evaluări
- Psych-K Rob WilliamsDocument6 paginiPsych-K Rob WilliamsKamal Janjani67% (6)
- ID Masalah Mental Dan Emosional Pada SiswaDocument14 paginiID Masalah Mental Dan Emosional Pada SiswaDya TuyulÎncă nu există evaluări
- Clinical Internship Presentation Format - VUDocument26 paginiClinical Internship Presentation Format - VUbc180408218 MAHAM ZEHRAÎncă nu există evaluări
- C8-C10 Octocapric Acid - Safety Data SheetDocument8 paginiC8-C10 Octocapric Acid - Safety Data Sheetdaya vashishtÎncă nu există evaluări
- 2023 GKS-G Application FormsDocument13 pagini2023 GKS-G Application FormssteverÎncă nu există evaluări
- The Age of Magical Overthinking: Notes on Modern IrrationalityDe la EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityEvaluare: 4 din 5 stele4/5 (29)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDe la EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDEvaluare: 5 din 5 stele5/5 (2)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDe la EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsÎncă nu există evaluări
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDe la EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionEvaluare: 4 din 5 stele4/5 (404)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDe la EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedEvaluare: 5 din 5 stele5/5 (81)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDe la EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsEvaluare: 3.5 din 5 stele3.5/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDe la EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsEvaluare: 4.5 din 5 stele4.5/5 (170)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)De la EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Încă nu există evaluări
- The Obesity Code: Unlocking the Secrets of Weight LossDe la EverandThe Obesity Code: Unlocking the Secrets of Weight LossEvaluare: 4 din 5 stele4/5 (6)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDe la EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsEvaluare: 5 din 5 stele5/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDe la EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeEvaluare: 2 din 5 stele2/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDe la EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisEvaluare: 4.5 din 5 stele4.5/5 (42)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDe la EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessEvaluare: 4.5 din 5 stele4.5/5 (328)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDe la EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisEvaluare: 4 din 5 stele4/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDe la EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityEvaluare: 4 din 5 stele4/5 (4)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.De la EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Evaluare: 4.5 din 5 stele4.5/5 (110)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisDe la EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisEvaluare: 5 din 5 stele5/5 (8)
- To Explain the World: The Discovery of Modern ScienceDe la EverandTo Explain the World: The Discovery of Modern ScienceEvaluare: 3.5 din 5 stele3.5/5 (51)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDe la EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisEvaluare: 3.5 din 5 stele3.5/5 (2)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDe la EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Marshmallow Test: Mastering Self-ControlDe la EverandThe Marshmallow Test: Mastering Self-ControlEvaluare: 4.5 din 5 stele4.5/5 (58)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDe la EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryEvaluare: 4 din 5 stele4/5 (45)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDe la EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeEvaluare: 4.5 din 5 stele4.5/5 (253)