Documente Academic
Documente Profesional
Documente Cultură
Chirurgie
Încărcat de
Anca GuraliucDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Chirurgie
Încărcat de
Anca GuraliucDrepturi de autor:
Formate disponibile
Vijeev Vasudevan et al
250
JAYPEE
CASE REPORT
Well-differentiated Squamous Cell Carcinoma of
Maxillary Sinus
Vijeev Vasudevan, S Kailasam, MB Radhika, Manjunath Venkatappa, Devaraju Devaiah, TG Shrihari, M Sudhakara
ABSTRACT
Paranasal sinus malignancies are exceedingly rare. Chronic
respiratory tract infections, nasal congestive symptoms and
rhinosinusitis are much more prevalent in recent days and
manifest many symptoms that overlap with those of sinus
malignancy. Symptoms may be nonspecific and indolent for
months or even years, leading to delay in diagnosis and
consequent advanced diseased stage at presentation. The
majority of maxillary sinus tumors in the literature have presented
with advanced stage, resulting in generally poor survival
outcomes. Hence, it is imperative that maxillofacial stomatologist
should be aware of sinus pathologies, to diagnose early and it
should alert them to include in differential diagnosis.
Keywords: Squamous cell carcinoma, Maxillary sinus, X-ray
tomography, Diagnosis.
How t o ci t e t hi s ar t i cl e: Vasudevan V, Kailasam S,
Radhika MB, Venkatappa M, Devaiah D, Shrihari TG,
Sudhakara M. Well-differentiated Squamous Cell Carcinoma
of Maxillary Sinus. J Indian Aca Oral Med Radiol 2012;24(3):
250-254.
Source of support: Nil
Conflict of interest: None declared
INTRODUCTION
Maxillary sinus cancer is relatively rare neoplasm with an
incidence representing a small percentage (0.2%) of human
malignant tumors and only 1.5% of all head and neck
malignant neoplasms.
1
Because of the relative rarity of
carcinoma of the maxillary sinus, institutional experience
is usually limited. The incidence seems to vary in different
parts of the world, with Asian countries reporting high
numbers of cases.
2
Maxillary sinus cancer is very difficult
to treat and traditionally have been associated with a poor
prognosis. One reason for these poor outcomes is the close
anatomic proximity of the nasal cavity and paranasal sinuses
to vital structures, such as the skull base, brain, orbit and
carotid artery. This complex location makes complete
surgical resection a challenging and sometimes impossible
task. In addition, these tumors tend to be asymptomatic at
early stages, appearing more frequently at late stages once
extensive local invasion has occurred.
CASE REPORT
A healthy 50-year-old man was referred to our oral medicine
department with the chief complaint of pain and swelling
of the left maxillary quadrant with nasal discharge. The
10.5005/jp-journals-10011-1307
patient had just completed a 5 days course of antibiotics
and analgesics for a presumed infection of odontogenic
origin with minimal improvement in his symptoms. His
medical history revealed a 3 pack/day, cigarette/beedies
smoking habit since childhood. He also had a habit of using
nasal snuff. Patient is on treatment for cough and chest pain
since 5 years. Patient gave a history of tooth removal for
mobility 5 days back in same quadrant and ulcer in relation
to same post-treatment.
Clinical examination showed a moderately firm soft
tissue swelling in the area of the left maxillary region; its
maximum dimension measured 2 cm (Fig. 1A). The lesion
was mildly painful to palpation. Lymph node blocks on the
neck did not have any positive sign.
On further questioning, the patient reported slight
paresthesia involving the distribution of the left posterior
superior alveolar nerves. Ulceroproliferative growth
measuring around 4 4 cm in maximum diameter was noted
in relation to 25, 26, 28 region, some purulent drainage was
obtained from the unhealed extraction socket in relation to
26, 27 (Fig. 1B). Generalized attrition, cervical abrasion
and mobility were noted.
A preliminary panoramic radiograph revealed missing
26, 27 and 16 and few decayed teeth and generalized
moderate to severe periodontal bone loss. A poorly defined
opacification was noted in the area of the left maxillary
sinus. The floor, roof and posterior and medial walls of the
left maxillary sinus appeared to be destroyed (Fig. 2).
Waters view showed that the opacification of the left
maxillary sinus has expanded to involve the entire left
maxillary sinus. Intraoral extension of this mass was also
evident. The inferior, posterior, lateral and medial walls of
the left maxillary sinus and the left orbital floor appear to
be destroyed completely (Fig. 3).
The patient was referred to the radiology department of
a local hospital, where plain computed tomography (CT)
was performed. The scan revealed significant destruction
of the anterior, posterior, medial and lateral walls of the
maxillary sinus as well as of the left orbital floor. Features
were of carcinoma of left maxillary antrum with invasion
in to the left orbit, ethmoid air cells, hard palate, nasal cavity
and infratemporal fossa (Figs 4A and B).
In view of paresthesia and growth in the area of
complaint, a biopsy of the involved areas was deemed
Journal of Indian Academy of Oral Medicine and Radiology, July-September 2012;24(3):250-254
251
Well-differentiated Squamous Cell Carcinoma of Maxillary Sinus
JIAOMR
Fig. 1A: Extraoral photograph taken clinically. Substantial
expansion is apparent over the area of the left maxillary sinus
Fig. 1B: A sizable intraoral mass is evident in the area of the left
maxillary buccal sulcus. Extending palatally involving alveolar ridge
Fig. 2: Panoramic radiograph reveals a poorly defined opacification
located in the area of the left maxillary sinus. The inferior, posterior
and medial walls of the left maxillary sinus and the left orbital floor
all appear to be destroyed
necessary to rule out the possibility of an underlying
malignant process. Surgical exploration of the area revealed
an irregular 1 1 cm bony defect filled with granulation-
like tissue on the posterior-lateral wall of the left maxillary
sinus. This soft tissue was submitted for histopathological
examination.
Microscopic examination of the biopsy specimen
revealed pseudostratified epithelial cells with signs of
dysplasia. Invading the deeper connective tissue in the form
of well-differentiated squamous cell carcinoma, showing
numerous keratin pearls (Figs 5A and B).
A diagnosis of well-differentiated squamous cell
carcinoma was reached. The patient was referred to the head
and neck surgery department for further treatment and
explained about the surgery, chemotherapy and
brachytherapy. Patient declined of treatment due to poor
socioeconomic background. Patient was advised on for
palliative therapy. Later, the patient succumbed within an
8 months time.
DISCUSSION
Maxillary sinus carcinoma presents a diagnostic and
therapeutic challenge to the oral diagnostician, surgeon and
as well as the radiation oncologist. The early symptoms are
generally vague and consistent with benign disorders. When
the tumors are small sized, they are misdiagnosed as chronic
sinusitis, nasal polyp, lacrimal duct obstruction or even
cranial arteritis.
3
In general, clinical examination of patients presenting
with pain and swelling of the jaws will reveal lesions of
dental etiology, most commonly related to pulpal or
periodontal pathology. However, when such situation exists,
it is mandate that dental practitioner must consider the
possibility of a nonodontogenic etiology. It is often better
to determine first, by clinical and radiographic examination,
whether the enlargement originates primarily in bone or in
the extraosseous soft tissue. An infection of odontogenic
origin is the most common cause of a soft tissue swelling of
the maxillary buccal vestibule. Second, the possibility of a
malignant neoplasm of the maxillary antrum, although
uncommon, should be considered.
In the present patients case, extensive dental decay and
periodontal disease (mobility of 26, 27), it would have
initially felt that this swelling was most likely the result of
an acute dental abscess secondary to pulpal involvement.
The previous dentist has extracted the teeth. The associated
soft tissue swelling was the result of tumor expansion
through a defect in the posterolateral wall of the left
maxillary sinus. In 40 to 60% of cases, there are facial
asymmetry, oral cavity swelling and tumor extension to the
nasal cavity. These lesions extend medially toward the nasal
cavity; superiorly they may invade the orbit and ethmoid
sinus; anterolaterally, they may reach soft tissues and cheek,
and inferiorly, the maxillary sinus floor, dental alveolus and
Vijeev Vasudevan et al
252
JAYPEE
Fig. 4A: Axial view CT with soft tissues window. Heterogeneous,
expansive lesion, with infiltrative aspect, centered on the left
maxillary sinus
Fig. 4B: Coronal view CT with osseous window. Expansive
lesion of left maxillary sinus with medial and anterolateral walls
erosion
Fig. 5A: Low power photomicrograph (10) showing antral
wall lining. The epithelial cells are pseudo stratified with signs of
dysplasia
Fig. 5B: Low power photomicrograph (10) showing dysplastic
epithelium invading the deeper connective tissue in the form of
well differentiated squamous cell carcinoma showing numerous
keratin pearls
Fig. 3: Waters view shows the opacification of the left maxillary
sinus has expanded to involve the entire left maxillary sinus. Intraoral
extension of this mass is also evident. The inferior, posterior, lateral
and medial walls of the left maxillary
palate. Posteriorly, they may reach the pterygopalatine fossa
and pterygoid muscles. Through the pterygoid fossa, they
may superiorly extend toward the orbital fissure and the
cavernous sinus.
4
Symptoms that are commonly noted with involvement
of the sinonasal complex include maxillary swelling,
epistaxsis, nasal obstruction or discharge, diplopia and
proptosis. When these classic signs are not present, the
possibility of a malignant tumor may be overlooked.
5,6
In the given case, patient had maxillary swelling, nasal
discharge and paresthesia of the involved nerve. Signs that
should alert the clinician to the possibility of a malignant
tumor include paresthesia, radiographic evidence of
irregular bone resorption and localized irregular widening
of the periodontal ligament. Among these, paresthesia is an
ominous sign. Although paresthesia can be related to nerve
Journal of Indian Academy of Oral Medicine and Radiology, July-September 2012;24(3):250-254
253
Well-differentiated Squamous Cell Carcinoma of Maxillary Sinus
JIAOMR
damage secondary to previous surgical procedures,
metabolic disorders or infection, it is mandatory that the
possibility of a malignant neoplasm be ruled out in all
patients presenting with paresthesia.
7,8
In the present case, the clinical examination of lymph
nodes was not palpable for any positive sign toward
malignancy. This low incidence may be associated with the
poor lymphatic draining of the maxillary sinus or with the
clinical inaccessibility for the affected lymph nodes
diagnosis. Lymph node blocks on the neck as an initial
presentation are not frequent, appearing in 3 to 20% of cases.
The topographic distribution of lymph node metastasis in
the neck usually is dependent on the tumor site, contiguity
and high number of capillaries.
9-11
However, invasion of
the parts with rich lymphatic network, such as the oral cavity
and nasopharynx, increases the risk of lymph node
metastases.
In majority of patients, this cancer is diagnosed in
advanced stages, making it difficult to determine the origin
of the neoplasm. Although the majority of maxillary sinus
carcinomas are locally advanced at diagnosis because its
symptoms are nonspecific and these tumors tend to remain
localized to maxilla for a long time and, during evolution,
they invade adjacent structures.
4,12
The most effective
barrier against tumors propagation is the integrity of the
periosteum that is particularly more resistant in two critical
areas: The skull base and orbit.
13
Destruction of maxillary sinus walls, especially the
inferior antral wall, can be identified by panoramic
radiography. In advanced cases, this imaging modality may
not show evidence of early bone destruction. CT and
magnetic resonance imaging (MRI) is the examination of
choice in such situation. The primary reason for advising
CT and MRI studies in cases of maxillary sinus carcinoma
is for better characterizing the invasion of structures beyond
the site of origin. On CT studies, all of the cases present as
soft tissue masses in the maxillary sinus cavity, with 70 to
90% of cases evidencing bony destruction. CT provides
more details of bone involvement than MRI. At MRI, these
tumors present middle signal intensity on T1-weighted
images and high intensity signal on T2-weighted images,
and this method is of help in the evaluation of the posterior
cranial fossa, orbit and perineural/perivascular dissemi-
nation, allowing the differentiation between retained
secretions and neoplastic tissue.
3,14
CT helped us in arriving at preliminary diagnosis, but
histopathological examination of biopsied tissue gave a
definitive diagnosis. However, detailed analysis of
histological findings is beyond the scope of this article.
When formulating a differential diagnosis for maxillary
sinus carcinoma, it is mandate to include primary sinonasal
neoplasms (e.g. sinonasal undifferentiated carcinoma,
nasopharyngeal carcinoma, lymphoma, esthesioneuro-
blastoma, primary sinonasal melanoma and adenocarcinoma
of minor salivary gland origin) and metastatic disease.
15
Treating maxillary sinus cancer is challenging because of
the crowded anatomy, proximity of critical structures, such
as the eye and the brain, which preclude wide surgical
excision and high-dose radiotherapy. The clinical course is
indolent at most and low incidence of malignant disease
here, which makes a low index of suspicion, the majority
of cancers of antrum are seen in a late or moderately
advanced stage at the time of diagnosis. Combined-modality
therapy consisting of surgery and radiotherapy with or
without intra-arterial chemotherapy is generally used for
the treatment. Local control is a particularly difficult
problem, with the majority of failures occurring at the
primary site. Radiotherapy is accepted as a palliative method
in inoperable cases.
16,17
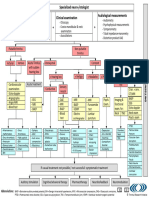
Ohngrens line is the theoretical plane joining medial
canthus of the eye with the angle of the mandible. This line
divides the maxilla into the infrastructure and superstructure
(Fig. 6). It was originally described by Dr Ohngren in 1930
to delineate the limits of resectability of a tumor in the
maxillary sinus. Tumors superoposterior to Ohngrens line
were more likely to involve the orbit, ethmoid and
pterygopalatine fossa. Malignancy behind Ohngrens line
is regarded to carry a much poorer prognosis because of the
rapid spread to the orbit and middle cranial fossae.
18
Maxillary sinus is at cross roads of dentistry and
otorhinolaryngology occupying a strategic position, as it is
connected directly to nasal cavity and indirectly to oral
cavity and maxillary alveolus. Oral diagnosticians should
be aware of the clinical signs and symptoms that might lead
one to suspect a malignant tumor might be relatively
nonspecific, potentially leading to a delay in diagnosis.
Therefore, it is important for the oral diagnostician to
maintain a high index of suspicion to allow for early
Fig. 6: Diagrammatic representation of Ohngrens line
Vijeev Vasudevan et al
254
JAYPEE
recognition and referral of these patients. One should have
eagles eye in all cases involving swellings of the head and
neck. In the presence of signs, such as pain and swelling
with associated paresthesia, or if conventional therapy fails
to resolve the swelling rapidly, prompt referral for biopsy
is needed to arrive at definitive diagnosis. It is mandate to
advise advanced imaging techniques, such as CT and MRI,
when conventional radiography fails to help in diagnosis at
the early stage of disease.
REFERENCES
1. Nunez F, Suarez C, Alvarez I, Losa J L, Barthe P, Fresno M.
Sino-nasal adenocarcinoma: Epidemiological and clinico-
pathological study of 34 cases. J Otolaryngol 1993;22(2):
86-90.
2. Sharma S, Sharma SC, Singhal S, et al. Carcinoma of the
maxillary antrum. A 10-year experience. Ind J Otolaryngol
1991;43:191-94.
3. Som PM, Brandwein M. Sinonasal cavities. Inflammatory
diseases, tumors, fractures and postoperative findings. In: Som
PM, Hugh D (Eds). Head and neck imaging (3rd ed). St Louis:
Mosby 1996;57.
4. Manrique RD, Deive LG, Uehara MA, Manrique RK, Rodriguez
J L, Santidrian C. Maxillary sinus cancer review in 23 patients
treated with postoperative radiotherapy. Acta Otorhinolaryngol
Esp 2008;59(1):6-10.
5. Hone SW, OLeary TG, Maguire A, Burns H, Timon CI.
Malignant sinonasal tumors: The Dublin Eye and Ear Hospital
experience. Ir J Med Sci 1995;164(2):139-41.
6. Selden HS, Manhoff DT, Hatges NA, Michel RC. Metastatic
carcinoma to the mandible that mimicked pulpal/periodontal
disease. J Endod 1998;24(4):267-70.
7. Georgiou AF, Walker DM, Collins AP, Morgan GJ , Shannon
J A, Veness MJ . Primary small cell undifferentiated
(neuroendocrine) carcinoma of the maxillary sinus. Oral Surg
Oral Med Oral Pathol Oral Radiol Endod 2004;98(5):572-78.
8. Morse DR. Infection-related mental and inferior alveolar nerve
paresthesia: Literature review and presentation of two cases. J
Endod 1997;23(7):457-60.
9. Stern SJ , Hanna E. Cancer of nasal cavity and paranasal sinuses.
In: Meyer EN, Suen J Y (Eds). Cancer of the head and neck (3rd
ed). Philadelphia: WB Saunders 1996;205-33.
10. Shibuya H, Yasumoto N, Gomi N, Yamada I, Ohashi I, Suzuki
S. CT features in second cancers of the maxillary sinus. Acta
Radiol 1991;32:105-09.
11. Donald PJ . Intranasal and paranasal sinus carcinoma. In:
Thawley SE, Pange WR (Eds). Comprehensive management of
the head and neck tumors. Philadelphia: WB Saunders 1987;94.
12. Frich J C. Treatment of advance squamous cell carcinoma of the
maxillary sinus. Int J Radiat Oncol 1982;8:1452-59.
13. Kimmelman CP, Korovin GS. Management of paranasal sinus
neoplasms invading the orbit. Otolaryngol Clin North Am
1988;21:77-92.
14. Maroldi R, Farina D, Battaglia G, Maculotti P, Nicolai P, Chiesa
A. MR of malignant nasosinusal neoplasms. Frequently asked
questions. Eur J Radiol 1997;24:181-90.
15. Goldenberg D, Golz A, Fradis M, Martu D, Netzer A, J oachims
HZ. Malignant tumors of the nose and paranasal sinuses: A
retrospective review of 291 cases. Ear Nose Throat J
2001;80(4):272-77.
16. Itami J , Uno T, Aruga M, Ode S. Squamous cell carcinoma of
the maxillary sinus treated with radiation therapy and
conservative surgery. Cancer 1998;82:104-07.
17. Konno A, Ishikawa K, Terada N, Numata T, Nagata H, Okamoto
Y. Analysis of long-term results of our combination therapy for
squamous cell cancer of the maxillary sinus. Acta Otolaryngol
Suppl 1998;537:57-66.
18. Ohngren LG. Malignant tumors of the maxilla-athmoid region.
Acta Otol Suppl 1933;19:1-476.
ABOUT THE AUTHORS
Vijeev Vasudevan
Professor and Head, Department of Oral Medicine and Radiology
Krishnadevaraya College of Dental Sciences and Hospital, Bengaluru
Karnataka, India
S Kailasam
Professor and Head, Department of Oral Medicine and Radiology
Ragas Dental College and Hospital, Chennai, Tamil Nadu, India
MB Radhika
Professor and Head, Department of Oral Pathology, Krishnadevaraya
College of Dental Sciences and Hospital, Bengaluru, Karnataka, India
Manjunath Venkatappa (Corresponding Author)
Senior Lecturer, Department of Oral Medicine and Radiology
Krishnadevaraya College of Dental Sciences and Hospital, Bengaluru
Karnataka, India, e-mail: manjuv79@gmail.com
Devaraju Devaiah
Senior Lecturer, Department of Oral Medicine and Radiology
Krishnadevaraya College of Dental Sciences and Hospital, Bengaluru
Karnataka, India
TG Shrihari
Senior Lecturer, Department of Oral Medicine and Radiology
Krishnadevaraya College of Dental Sciences and Hospital, Bengaluru
Karnataka, India
M Sudhakara
Senior Lecturer, Department of Oral Pathology, Krishnadevaraya
College of Dental Sciences and Hospital, Bengaluru, Karnataka, India
S-ar putea să vă placă și
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Ghanie Irwan 2019 J. Phys.: Conf. Ser. 1246 012019Document9 paginiGhanie Irwan 2019 J. Phys.: Conf. Ser. 1246 012019mellysa iskandarÎncă nu există evaluări
- GHSB2024 Superficial Structures of The Neck and Posterior TriangleDocument5 paginiGHSB2024 Superficial Structures of The Neck and Posterior Trianglekang seulgi can set me on fire with her gaze aloneÎncă nu există evaluări
- Therefore "Weakness" DOES NOT Help To Establish Whether It Is UMN or LMN lesion-FOLLOWING Pattern of Signs Help Us To EstablishDocument66 paginiTherefore "Weakness" DOES NOT Help To Establish Whether It Is UMN or LMN lesion-FOLLOWING Pattern of Signs Help Us To EstablishBaishakhi ChakrabortyÎncă nu există evaluări
- Wells Partial Denture ProsthodonticsDocument10 paginiWells Partial Denture Prosthodonticsthesabarmo100% (1)
- TRI Tinnitus FlowchartDocument1 paginăTRI Tinnitus FlowchartAdvocacia VitóriaÎncă nu există evaluări
- RespiratoryanatomyDocument5 paginiRespiratoryanatomyMary♡Încă nu există evaluări
- INTERNS NOTES - OtorhinolaryngologyDocument15 paginiINTERNS NOTES - OtorhinolaryngologyKarl Jimenez SeparaÎncă nu există evaluări
- Direct Gingivoperiosteoplasty With PalatoplastyDocument6 paginiDirect Gingivoperiosteoplasty With PalatoplastyAndrés Faúndez TeránÎncă nu există evaluări
- Cleft Lip DR RituDocument82 paginiCleft Lip DR RituRitu SamdyanÎncă nu există evaluări
- Clinical Skills Cranial Nerves I To VI Students Copy 2019Document4 paginiClinical Skills Cranial Nerves I To VI Students Copy 2019carlosÎncă nu există evaluări
- Chapter 11 Sense OrgansDocument18 paginiChapter 11 Sense OrgansMichael Oconnor100% (2)
- Lec 1 Functional Areas of Cerebral CortexDocument37 paginiLec 1 Functional Areas of Cerebral CortexMudassar RoomiÎncă nu există evaluări
- The Function of TongueDocument11 paginiThe Function of TongueAndrea LawÎncă nu există evaluări
- Unit 1 PDF People PDFDocument12 paginiUnit 1 PDF People PDFCosmic LatteÎncă nu există evaluări
- HearingDocument15 paginiHearingdisha mangeÎncă nu există evaluări
- 008 164 Anatomy of Thyroid Gland PDFDocument10 pagini008 164 Anatomy of Thyroid Gland PDFWILLIAMÎncă nu există evaluări
- The Role of Intratympanic Dexamethasone in Sudden Sensorineural Hearing LossDocument5 paginiThe Role of Intratympanic Dexamethasone in Sudden Sensorineural Hearing LossAditya HendraÎncă nu există evaluări
- Salivary GlandsDocument97 paginiSalivary GlandsSwati George100% (2)
- Chapter 8-SPECIAL SENSESDocument5 paginiChapter 8-SPECIAL SENSESrishellemaepilonesÎncă nu există evaluări
- Weinberg2001 THERAPEUTIC BIOMECHANICS CONCEPTS AND CLINICAL PROCEDURES TO REDUCE IMPLANT LOADING. PART II - THERAPEUTIC DIFFERENTIAL LOADINGDocument9 paginiWeinberg2001 THERAPEUTIC BIOMECHANICS CONCEPTS AND CLINICAL PROCEDURES TO REDUCE IMPLANT LOADING. PART II - THERAPEUTIC DIFFERENTIAL LOADINGPablo Gutiérrez Da VeneziaÎncă nu există evaluări
- PonsDocument61 paginiPonsAyberk ZorluÎncă nu există evaluări
- Occlusion in FPDDocument38 paginiOcclusion in FPDDRPRIYA007100% (4)
- Anatomy of The EarDocument10 paginiAnatomy of The EarJP SouaidÎncă nu există evaluări
- TAOMS20 Abstract BookDocument238 paginiTAOMS20 Abstract BookTaha ÖzerÎncă nu există evaluări
- Anatomy Topography of The EyeDocument46 paginiAnatomy Topography of The Eyeikayapmd100% (1)
- HANDOUT Laryngeal-MassageDocument7 paginiHANDOUT Laryngeal-MassageAnca OÎncă nu există evaluări
- MRI & CT of Facial Bones PDFDocument53 paginiMRI & CT of Facial Bones PDFdr_340802071Încă nu există evaluări
- Assessing The Nose and Sinuses: Return Demonstration Tool Evaluation ForDocument3 paginiAssessing The Nose and Sinuses: Return Demonstration Tool Evaluation Forclint xavier odangoÎncă nu există evaluări
- Patient Type: OPD: TSH Test ReportDocument1 paginăPatient Type: OPD: TSH Test ReportVeenu SehrawatÎncă nu există evaluări
- Kadasne's Textbook of Anatomy (Clinically Oriented) VOLUME 3 Head, Neck, Face and Brain (2009) (PDF) (UnitedVRG)Document365 paginiKadasne's Textbook of Anatomy (Clinically Oriented) VOLUME 3 Head, Neck, Face and Brain (2009) (PDF) (UnitedVRG)Ahmad YÎncă nu există evaluări