Documente Academic
Documente Profesional
Documente Cultură
Gist Workshop
Încărcat de
Ruki Hartawan0 evaluări0% au considerat acest document util (0 voturi)
34 vizualizări38 paginiTitlu original
170707469 Gist Workshop
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
34 vizualizări38 paginiGist Workshop
Încărcat de
Ruki HartawanDrepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 38
WORKSHOP GIST
SEMARANG 14 SEPTEMBER 2013
INTESTINAL GIST
ANAMNESIS
Laki-laki 44 tahun,
12 bulan perut merasa tidak enak,kadang-kadang
mules, pernah berak kehitaman. Hanya diobatkan
ke dokter puskesmas
3 bulan teraba benjolan yang makin lama makin
membesar, perut terasa sebah dan mules sekali
dan berak hitam makin jelas
Nafsu makan kurang dan berat badan menurun
Riwayat family dengan tumor abdomen disangkal
PEMERIKSAAN FISIK
Laki-laki berat badan: 42 Kg, TB 165 cm, BMI :
15,44
Kurus, nampak pucat
Abdomen kembung ringan, terlihat bulging perut
dibagian tengah, gambaran dan gerakan usus
tidak terlihat.
Palpasi teraba tumor diameter sekitar 12 cm,
bulat dengan permukaan tidak rata, konsistensi
keras, nyeri tekan (-), relatif mobile
Auscultasi: Peristaltik normal, tidak terdengar
bising diatas tumor
LABORATORIUM
Hb 7,8 Mg%, Ht 24, Lekosit 6500
Alb 2,8 mg%, Glob 2,3 mg%
Na 134, K 3,2, Cl 98, Ca 2,10
Lain-lain baik.
DIAGNOSA BANDING
LYMPHOMA MALIGNA
HODGKIN DISEASE
SCWANOMA MALIGNA
LEIOMYOSARCOMA
INSTESTINAL GIST
PERLU KEPASTIAN DIAGNOSIS SEBELUM OPERASI?
PERSIAPAN PRA-BEDAH
ANEMIA:
BLOOD TRANFUSION
SEVERE MALNUTRITION
PRE-OPERATIVE NUTRITIONAL SUPPORT
LAPARATOMI
TUMOR USUS HALUS PERTENGAHAN
(PERBATASAN ILEUM-JEJENUM) SEKITAR 14
CM, KERAS, LN MESENTERIKA (-), PERITONEAL
SEEDING (-), METASTASE HEPAR (-)
TANDA PARTIAL OBSTRUKSI USUS (+)
DILAKUKAN RESEKSI USUS HALUS ISTAL DAN
PROKSIMAL TUMOR, ANASTOMOSIS END TO
END
PASCA BEDAH
PASIEN BAIK PULANG TANPA KOMPLIKASI
PA SPINDEL CELL TUMOR CURIGA GIST, BATAS
RESEKSI BEBAS TUMOR, MITOSIS(?)
IHC CD 117 (+)
PEMBAHASAN
Diagnostic procedure?
Grade?
Surgery?
Chemotherapy (preoperative? post-
operative?)
Prognosis?
DIAGNOSTIC PROCEDURE?
PREOPERATIVE DIAGNOSIS
ENDOSCOPY:
DOUBLE BALLON ENTEROSCOPY?
CAPSULE ENDOSCOPY?
LAPARATOMY/ LAPAROSCOPY BIOPSY?
NO NEED DIRECT LAPARATOMY &
RESECTION OR BIOPSY.
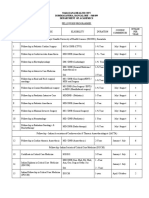
GRADING
POLSKIE ARCHIWUM MEDYCYNY WEWNTRZNEJ 2008; 118 (4)
HUMAN PATHOLOGY Volume33, No. 5 (May 2002)
NIH Classification for Risk of
Recurrence
Very Low Risk Low Risk Intermediate Risk High Risk
NIH consensus
criteria
1
Tumor size < 2 cm
Mitotic index < 5
Tumor size 2-5 cm
Mitotic index < 5
Tumor size 5-10 cm
Mitotic index < 5
OR
Tumor size < 5 cm
Mitotic index 6-10
Tumor size > 5 cm
Mitotic index > 5
OR
Tumor size > 10 cm
Mitotic index, any
OR
Tumor size, any
Mitotic index > 10
Modified NIH
consensus
classification
2
Any location:
Tumor size < 2 cm
Mitotic index 5
Any location:
Tumor size 2.1-5 cm
Mitotic index 5
Any location:
Tumor size < 5 cm
Mitotic index 6-10
Gastric:
Tumor size 2.1-5 cm
Mitotic index > 5
OR
Tumor size 5.1-10 cm
Mitotic index 5
Any location:
Tumor rupture
OR
Tumor size > 10 cm
OR
Mitotic index > 10
OR
Tumor size > 5 cm
Mitotic index > 5
Nongastric:
Tumor size 2.1-5 cm
Mitotic index > 5
OR
Tumor size 5.1-10 cm
Mitotic index 5
Abbreviations: Mitotic index, number of mitoses per 50 high-power fields; NIH, National Institutes of health.
1. Fletcher CD, et al. Hum Pathol. 2002;33(5):459-465; 2. Joensuu H. Hum Pathol. 2008;39(10):1411-1419.
24
GRADE
TUMOR > 10 CM
MITOTIC INDEX: NOT REPORTED
NEGATIVE MARGIN
LOCATION: NON GASTRIC
HIGH RISK GROUP FOR RECCURRENCE
SURGERY
Surgical treatment of gist
The radical surgical treatment is the most effective
treatment
The 5-year survival rate after surgery amounts to 2865%
It is not necessary to resect the regional lymph nodes
because GIST do not metastasize to the regional
lymphatic system
2040% of the surgery patients have intra-abdominal
dissemination or liver metastasis paliatif surgery
(sympotomatic treatment)
endoscopic dissection (submucosal-mucosal resection)
allows a radical therapy of small tumors without
malignancy features and limited to the submucosal layer.
POLSKIE ARCHIWUM MEDYCYNY WEWNTRZNEJ 2008; 118 (4)
CHEMOTHERAPY
Preoperative : need histological
diagnosis
PROGNOSIS
The 5-year survival rate after surgery of GIST
amounts to 2865%
778 patients
18 y
Localized and
primary GIST
KIT-positive
tumors 3 cm
Complete surgical
resection
Placebo for 1 y
Imatinib
400 mg/d for 1 y
Imatinib
400/800 mg/d
713 patients
randomized
Imatinib
400 mg/d
DeMatteo RP, et al. Lancet. 2009;37(9669)3:1097-1104.
Phase 3 ACOSOG Z9001: Trial Schema
Endpoints:
Primary: Recurrence-free survival
Secondary: Overall survival, safety
33
At time of
recurrence
At time of
recurrence
Abbreviations: CI, confidence interval; HR, hazard ratio.
a
All randomized patients were included in the analysis; recurrence-free survival was defined as the time from patient
registration to the development of tumor recurrence or death from any cause. Intention-to-treat analyses were done for
recurrence-free survival (ie, analyzed patients by randomized group).
Adapted from DeMatteo RP, et al. Lancet. 2009;373(9669):1097-1104.
Recurrence-Free Survival
a
HR = 0.35 (95% CI = 0.22, 0.53); P < .0001
100
90
80
70
60
50
40
30
20
10
0
R
e
c
u
r
r
e
n
c
e
-
F
r
e
e
a
n
d
A
l
i
v
e
,
%
0 6 12 18 24 30
Time, mo
36 42 48
Imatinib
Placebo
359
354
30
70
Total Events
Median follow-up: 19.7 mo
34
Size 10 cm
Size 3 and < 6 cm Size 6 and < 10 cm
Recurrence-Free Survival (Tumor Size)
Imatinib adjuvant therapy results
in significantly longer RFS in each
of the tumor size categories
compared with placebo
100
90
80
70
60
50
40
30
20
10
0
R
e
c
u
r
r
e
n
c
e
-
F
r
e
e
a
n
d
A
l
i
v
e
,
%
0 6 12 18 24 30 36 42 48
100
90
80
70
60
50
40
30
20
10
0
R
e
c
u
r
r
e
n
c
e
-
F
r
e
e
a
n
d
A
l
i
v
e
,
%
0 6 12 18 24 30 36 42 48
Imatinib, n = 143
Placebo, n = 149
HR = 0.23 (95% CI = 0.07, 0.79); P = .011
Imatinib, n = 93
Placebo, n = 86
HR = 0.29 (95% CI = 0.16, 0.55); P < .001
Time, mo
Time, mo
100
90
80
70
60
50
40
30
20
10
0
R
e
c
u
r
r
e
n
c
e
-
F
r
e
e
a
n
d
A
l
i
v
e
,
%
0 6 12 18 24 30 36 42 48
Time, mo
Imatinib, n = 123
Placebo, n = 119
HR = 0.50 (95% CI = 0.25, 0.98); P = .041
Abbreviations: CI, confidence interval; HR, hazard ratio; RFS, recurrence-free survival.
Adapted from DeMatteo RP, et al. Lancet. 2009;373(9669):1097-1104.
35
Follow-up
Follow-up
Phase 3 SSGXVIII: Study Design
Randomized
1:1
Imatinib
12 mo
400 patients
KIT-positive
histologically
confirmed GIST
High
recurrence risk
according to
modified NIH
consensus
criteria
Endpoints:
Primary: Recurrence-free survival
Secondary: Overall survival, safety
Imatinib
36 mo
Abbreviation: NIH, National Institutes of Health.
Data from Joensuu H, et al. JAMA. 2012;307(12):1265-1272.
Key Elements:
Patient stratification:
R0 resection, no tumor rupture
R1 resection OR tumor rupture
36
HR = 0.46 (95% CI = 0.32, 0.65); P < .0001
SSGXVIII: Recurrence-Free Survival
(ITT)
Abbreviations: CI, confidence interval; HR, hazard ratio; ITT, intent to treat.
Adapted from Joensuu H, et al. JAMA. 2012;307(12):1265-1272.
60.1%
47.9%
86.6%
65.6%
36 mo, n = 198
12 mo, n = 199
0 1 2 3 4 5 6
0
20
40
60
80
100
Median follow-up,
54 mo
Time, y
R
e
c
u
r
r
e
n
c
e
-
F
r
e
e
a
n
d
A
l
i
v
e
,
%
37
S-ar putea să vă placă și
- Preoperative Checklist-1Document10 paginiPreoperative Checklist-1June Faith HacheroÎncă nu există evaluări
- NCP. FistulectomyDocument2 paginiNCP. Fistulectomymitchelley80% (10)
- Intestinal Gist: Workshop Gist Semarang 14 September 2013Document38 paginiIntestinal Gist: Workshop Gist Semarang 14 September 2013TjendonohariantoÎncă nu există evaluări
- Gist Clinical DiagnosisDocument41 paginiGist Clinical DiagnosisTjendonohariantoÎncă nu există evaluări
- Jurnal Parade YurianiDocument38 paginiJurnal Parade YurianiSukoco HartonoÎncă nu există evaluări
- Bladder Preservation in Muscle Invasive Disease: Nick James University of Birmingham @prof - Nick - James #NjbladdercancerDocument38 paginiBladder Preservation in Muscle Invasive Disease: Nick James University of Birmingham @prof - Nick - James #NjbladdercancerProf_Nick_JamesÎncă nu există evaluări
- CCDuodenum Periampullary Neoplasms ChuDocument68 paginiCCDuodenum Periampullary Neoplasms ChuSahirÎncă nu există evaluări
- Dr. Ranjan GuptaDocument29 paginiDr. Ranjan GuptaRanjan GuptaÎncă nu există evaluări
- Hyperthermic Intraperitoneal Chemotherapy - Hipec-: Rusie Daniel, Medic Rezident Chirurgie GeneralaDocument23 paginiHyperthermic Intraperitoneal Chemotherapy - Hipec-: Rusie Daniel, Medic Rezident Chirurgie GeneralaDaniel RusieÎncă nu există evaluări
- Sarcomas BaldiniDocument111 paginiSarcomas BaldiniIlincaÎncă nu există evaluări
- Barb Melo SkyDocument17 paginiBarb Melo SkyAfiqah So JasmiÎncă nu există evaluări
- Bladder Preservation in Muscle Invasive Disease: Nick James University of WarwickDocument41 paginiBladder Preservation in Muscle Invasive Disease: Nick James University of WarwickProf_Nick_JamesÎncă nu există evaluări
- CHOLEDOCHAL CYST-case PresentationDocument30 paginiCHOLEDOCHAL CYST-case PresentationPawan SapkotaÎncă nu există evaluări
- Gist Bedah DigestifDocument36 paginiGist Bedah DigestifTjendonohariantoÎncă nu există evaluări
- Prostate CarcinomaDocument103 paginiProstate CarcinomaDrRajendra PatelÎncă nu există evaluări
- Lung Cancer ManagementDocument126 paginiLung Cancer ManagementdjonesthoracicÎncă nu există evaluări
- Gastrointestinal Stromal Tumors (Gists) : Surgical Management Update 2009Document40 paginiGastrointestinal Stromal Tumors (Gists) : Surgical Management Update 2009Rendy FitraÎncă nu există evaluări
- APR Technique of A Wide Perineal ResectionDocument35 paginiAPR Technique of A Wide Perineal ResectionArtemSakhnoÎncă nu există evaluări
- Pituitary Adenomas: Chien Wei OMS IV September 14, 2006Document48 paginiPituitary Adenomas: Chien Wei OMS IV September 14, 2006Irnamanda Dwipura Yaqin HÎncă nu există evaluări
- Adjuvant Chemotherapy of BCDocument110 paginiAdjuvant Chemotherapy of BCDoni KurniawanÎncă nu există evaluări
- Cytoreductive Surgery and IntraperitonealDocument11 paginiCytoreductive Surgery and IntraperitonealJorge FallasÎncă nu există evaluări
- Charles Catton, Brian O'Sullivan, Robert Dinniwell, Anthony Griffin, Peter C Ferguson, Rebecca Gladdy, David Mccready, Martin Blackstein, Abha Gupta, Lisa W Le, Peter ChungDocument15 paginiCharles Catton, Brian O'Sullivan, Robert Dinniwell, Anthony Griffin, Peter C Ferguson, Rebecca Gladdy, David Mccready, Martin Blackstein, Abha Gupta, Lisa W Le, Peter ChungRida Anita YunikawatiÎncă nu există evaluări
- Cme Code: 1Hjp6T: General Surgery ConferenceDocument43 paginiCme Code: 1Hjp6T: General Surgery ConferenceTahamqÎncă nu există evaluări
- Multidisciplinary Management of Hepatocellular CarcinomaDocument45 paginiMultidisciplinary Management of Hepatocellular CarcinomaSalmanArifÎncă nu există evaluări
- CasePres Dr. EpiliDocument5 paginiCasePres Dr. EpiliPeter PanÎncă nu există evaluări
- Gastrointestinal Stromal Tumors (Gists) : DR GaneshDocument24 paginiGastrointestinal Stromal Tumors (Gists) : DR GaneshGanesh MarutinathÎncă nu există evaluări
- Bisa 1Document8 paginiBisa 1justforuroÎncă nu există evaluări
- Faiza Hashim Soomro PG-Gen SurgeryDocument47 paginiFaiza Hashim Soomro PG-Gen SurgeryFaiza Hashim SoomroÎncă nu există evaluări
- APBIDocument31 paginiAPBIshokoÎncă nu există evaluări
- Protocol of Radiotherapy For Rectal CancerDocument3 paginiProtocol of Radiotherapy For Rectal CancerValentino PetreÎncă nu există evaluări
- Hall A DR Devilla Apasl Sirt Talk1 Luncheon PDFDocument45 paginiHall A DR Devilla Apasl Sirt Talk1 Luncheon PDFMarlon Dela CruzÎncă nu există evaluări
- Rapido DanielDocument28 paginiRapido DanielzalikhaÎncă nu există evaluări
- Cancer Gastrico AvancesDocument48 paginiCancer Gastrico AvancesSeal MachucaÎncă nu există evaluări
- Faculty of Medicine NR - Ii Department of Surgery NR - Ii: Diseases of The Biliary TractDocument40 paginiFaculty of Medicine NR - Ii Department of Surgery NR - Ii: Diseases of The Biliary TractGalina LozovanuÎncă nu există evaluări
- Tumor Board MeetingDocument17 paginiTumor Board MeetingMurk NiazÎncă nu există evaluări
- Case Study: Low-Risk Organ-Confined Prostate CancerDocument4 paginiCase Study: Low-Risk Organ-Confined Prostate CancerAce VirtusioÎncă nu există evaluări
- HepatomaDocument33 paginiHepatomaRozen RyuhaÎncă nu există evaluări
- Outcomes of Endoscopic Submucosal Dissection of PaDocument4 paginiOutcomes of Endoscopic Submucosal Dissection of Pato van quyenÎncă nu există evaluări
- 17-09-2019 Lower GI FINALDocument32 pagini17-09-2019 Lower GI FINALNaima HabibÎncă nu există evaluări
- Farmakoterapi Antiniotik Pada Infeksi BedahDocument24 paginiFarmakoterapi Antiniotik Pada Infeksi BedahdrhendyjuniorÎncă nu există evaluări
- BPH PSPD 2012Document43 paginiBPH PSPD 2012Nor AinaÎncă nu există evaluări
- Role of Radiotherapy For Hepatocellular CarcinomaDocument37 paginiRole of Radiotherapy For Hepatocellular CarcinomabahtiarhabibiÎncă nu există evaluări
- Rajeev Agarwal Senior Consultant-Surgical OncologyDocument23 paginiRajeev Agarwal Senior Consultant-Surgical OncologyPushpanjali Crosslay HospitalÎncă nu există evaluări
- HIPECDocument34 paginiHIPECBimlesh thakurÎncă nu există evaluări
- Small BowelDocument28 paginiSmall BowelpopÎncă nu există evaluări
- 172 - 04 101 13 PDFDocument8 pagini172 - 04 101 13 PDFAlexandrosÎncă nu există evaluări
- Case DiscussionDocument29 paginiCase DiscussionTjendonohariantoÎncă nu există evaluări
- Upper Gastrointestinal Cancers in The ElderlyDocument32 paginiUpper Gastrointestinal Cancers in The ElderlyRadha ChiombonÎncă nu există evaluări
- HPB 09 S2 071Document120 paginiHPB 09 S2 071Widya Dahlia JuwitaÎncă nu există evaluări
- Slide Myoma Mrs. Maimunah KirimDocument21 paginiSlide Myoma Mrs. Maimunah KirimarifsandroÎncă nu există evaluări
- Gastriccancer 160428190410Document54 paginiGastriccancer 160428190410Pranavi ShewaleÎncă nu există evaluări
- Handbook Rhabdomyosarcoma Winter2018Document14 paginiHandbook Rhabdomyosarcoma Winter2018Rizky AmaliahÎncă nu există evaluări
- GIST of The StomachDocument3 paginiGIST of The StomachLouis FortunatoÎncă nu există evaluări
- Presenter: DR Muthulingesh, SR-RO Moderator: DR Shyama Prem, ProfessorDocument51 paginiPresenter: DR Muthulingesh, SR-RO Moderator: DR Shyama Prem, ProfessorGousalyaÎncă nu există evaluări
- Management of Endometrial CarcinomaDocument46 paginiManagement of Endometrial CarcinomaSapna SÎncă nu există evaluări
- Complications of Peptic Ulcer Disease: Surgical ManagementDocument57 paginiComplications of Peptic Ulcer Disease: Surgical ManagementJoan LuisÎncă nu există evaluări
- CA Prostate by Dr. Musaib MushtaqDocument71 paginiCA Prostate by Dr. Musaib MushtaqDr. Musaib MushtaqÎncă nu există evaluări
- Prostate+Ca Updated+Aug+2017 PDFDocument17 paginiProstate+Ca Updated+Aug+2017 PDFFlorencia GuerraÎncă nu există evaluări
- Journal Reading Ii: Presentan: Dr. Viona - 1906345622Document38 paginiJournal Reading Ii: Presentan: Dr. Viona - 1906345622Alejandro TurnerÎncă nu există evaluări
- Urological Cancer Clinical ScenariosDocument27 paginiUrological Cancer Clinical ScenariosMohammed FathyÎncă nu există evaluări
- Surgery Department: Morning ReportsDocument17 paginiSurgery Department: Morning ReportsguterizalÎncă nu există evaluări
- Top Trials in Gastroenterology & HepatologyDe la EverandTop Trials in Gastroenterology & HepatologyEvaluare: 4.5 din 5 stele4.5/5 (7)
- DR - Dedi Alita Why Do We Need de ResuscitationDocument31 paginiDR - Dedi Alita Why Do We Need de ResuscitationRuki HartawanÎncă nu există evaluări
- Ards PDFDocument20 paginiArds PDFRuki HartawanÎncă nu există evaluări
- Presentation VentiDocument41 paginiPresentation VentiRuki HartawanÎncă nu există evaluări
- Cranial Neuralgia Keynote PDFDocument21 paginiCranial Neuralgia Keynote PDFRuki HartawanÎncă nu există evaluări
- Persistent Asthma - Prof DR SidhartaniDocument18 paginiPersistent Asthma - Prof DR SidhartaniRuki HartawanÎncă nu există evaluări
- Dyspnea Prof Menaldi CompressedDocument48 paginiDyspnea Prof Menaldi CompressedRuki HartawanÎncă nu există evaluări
- Herbal DR Nyoman SP PDDocument27 paginiHerbal DR Nyoman SP PDRuki HartawanÎncă nu există evaluări
- Buku Bedah UmumDocument126 paginiBuku Bedah UmumSilvia Kamal100% (7)
- DI-Imaging of Head Traum 2009 (TN)Document82 paginiDI-Imaging of Head Traum 2009 (TN)Ruki HartawanÎncă nu există evaluări
- Hand Book Gastro Ardy MoeftyDocument57 paginiHand Book Gastro Ardy MoeftyRuki HartawanÎncă nu există evaluări
- Persistent Asthma - Prof DR SidhartaniDocument18 paginiPersistent Asthma - Prof DR SidhartaniRuki HartawanÎncă nu există evaluări
- Oculoplasty Surgeon in AhmedabadDocument8 paginiOculoplasty Surgeon in AhmedabadhniramayÎncă nu există evaluări
- Knee Surgery Using Computer Assisted Surgery and Robotics PDFDocument221 paginiKnee Surgery Using Computer Assisted Surgery and Robotics PDFHendra AjahÎncă nu există evaluări
- Endoscopic Excision of Antrochoanal PolypDocument3 paginiEndoscopic Excision of Antrochoanal PolypreginalisaÎncă nu există evaluări
- Wilko Don TicsDocument7 paginiWilko Don TicsMonika SonawaneÎncă nu există evaluări
- A Prospective Analysis of Risk Factors For Post Operative Surgical Site Infection Following Implant Surgery in Closed FracturesDocument6 paginiA Prospective Analysis of Risk Factors For Post Operative Surgical Site Infection Following Implant Surgery in Closed FracturesIJAR JOURNALÎncă nu există evaluări
- Hospital Cash ClaimDocument4 paginiHospital Cash ClaimChloe Auda IbalioÎncă nu există evaluări
- Focus ChartingDocument2 paginiFocus ChartingJane Umali Tulabot83% (6)
- Staghorn CalculiDocument29 paginiStaghorn CalculiLiza M. PurocÎncă nu există evaluări
- Motor Vehicle CollisionDocument37 paginiMotor Vehicle CollisionLouisse Angeli AbucejoÎncă nu există evaluări
- UrethrocystographyDocument9 paginiUrethrocystographyyinyangdongÎncă nu există evaluări
- Summary of Staff Daily Activities According To Shift I. Staff Nurses Morning Shift (6:00am-2:00pm) With 3 Staff NursesDocument13 paginiSummary of Staff Daily Activities According To Shift I. Staff Nurses Morning Shift (6:00am-2:00pm) With 3 Staff NursesMarv Marv0% (1)
- Angio FibromaDocument11 paginiAngio FibromaNisful Lail J. AÎncă nu există evaluări
- Level 3 Hospital Research PDF FreeDocument9 paginiLevel 3 Hospital Research PDF FreekanaÎncă nu există evaluări
- Autumn Gettings ResumeDocument2 paginiAutumn Gettings Resumeapi-663930784Încă nu există evaluări
- View Tender FileDocument364 paginiView Tender FileEngy RamadanÎncă nu există evaluări
- Freehand Vs Guided Implant Surgery ResearchDocument4 paginiFreehand Vs Guided Implant Surgery ResearchSandeep Kumar SenguptaÎncă nu există evaluări
- Colonic InertiaDocument5 paginiColonic InertiaEmilio SanchezÎncă nu există evaluări
- SBARDocument2 paginiSBARJason Kai Poth100% (1)
- Foramen Magnum Meningiomas: Concepts, Classifications, and NuancesDocument9 paginiForamen Magnum Meningiomas: Concepts, Classifications, and NuancesBlessing NdlovuÎncă nu există evaluări
- Medical-Surgical Nursing Assessment and Management of Clinical Problems 9e Chapter 63Document16 paginiMedical-Surgical Nursing Assessment and Management of Clinical Problems 9e Chapter 63sarasjunkÎncă nu există evaluări
- On AdmissionDocument48 paginiOn AdmissiondeepaÎncă nu există evaluări
- 2023 01 09 23284099v1 FullDocument20 pagini2023 01 09 23284099v1 FullArchana SelviÎncă nu există evaluări
- Head Nurse EvaluationDocument26 paginiHead Nurse EvaluationRichard281981100% (1)
- Complication IntraoperativeDocument5 paginiComplication IntraoperativeizzatulhasanahÎncă nu există evaluări
- Ao Principles Principles of Internal Fixation (Of Fractures)Document18 paginiAo Principles Principles of Internal Fixation (Of Fractures)Satya NagaraÎncă nu există evaluări
- Sample Literature ReviewDocument8 paginiSample Literature Review67890ThÎncă nu există evaluări
- Narayana Health City Bommasandra, Bangalore - 560 099 Department of AcademicsDocument2 paginiNarayana Health City Bommasandra, Bangalore - 560 099 Department of AcademicsEthan AmalÎncă nu există evaluări