Documente Academic
Documente Profesional
Documente Cultură
CPR and FBAO Final Lecture
Încărcat de
Ash CampiaoDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
CPR and FBAO Final Lecture
Încărcat de
Ash CampiaoDrepturi de autor:
Formate disponibile
CARDIOPULMONARY RESUSCITATION (CPR)
and
FOREIGN-BODY AIRWAY OBSTRUCTION
Kierstine O Garcia, RN
FO1 BFP
EMS STAFF
CHAIN OF SURVIVAL
CARDIOPULMONARY RESUSCITATION
FOREIGN-BODY AIRWAY OBSTRUCTION
CPR
CARDIOPULMONARY RESUSCITATION
1. Chain of Survival
Cardiopulmonary resuscitation (CPR) can save the lives of victims in cardiac arrest. Two
thirds of heart attack victims (due to heart disease) die outside the hospital, most within two
hours of the onset of symptoms. Though CPR itself is not enough to save the life of a victim of
heart attack, it is a vital link in the chain of survival.
The chain of survival has hour links, and the patients chances for surviving are the greatest
when all the links come together.
1. Early access
2. Early CPR
3. Early defibrillation
4. Early advanced life support
The need for these interventions should not be limited to victims of heart disease .Many
victims of drowning, trauma, electrocution, suffocation, airway obstruction, allergic reaction,
etc., may be saved by prompt intervention.
2. Heart Attack Risk Factors
Risk factors that cannot be changed (non-modifiable)
Heredity
Age
Gender
Risk factor that can be changed (modifiable)
Smoking
Hypertension
Exercise
High cholesterol
Contributing factors
Obesity
Diabetes
Stress
3. Breathing
Adequate breathing is characterized by:
Chest and abdomen rise and fall with each breath
Air can be heard and felt exiting the mouth and or nose
Inadequate breathing is characterized by:
Inadequate rise and fall of the chest
Noisy breathing:bubbles,rales,stridor,whistling,etc.,
Absent breathing is characterized by:
No chest or abdominal movement
Air cannot be heard or felt exiting the mouth or nose
4. Cyanosis
A bluish discoloration of the skin and the mucous membranes caused by a lack of oxygen in
the blood and tissues.
This condition can be the result of the patient breathing in an environment poor in oxygen,
suffering from illness or respiratory injury, or airway obstruction.
Cyanosis can be more easily noticed on the lips, ears and nostrils or nailbeds. In patients with
dark pigmentation, it is necessary to inspect the nostrils, palm, and nailbeds, and the mouth and
tongue.
5. Clinical and Biological Death
Clinical Death: Occurs when a patient is in respiratory arrest (not breathing)or in cardiac
arrest(heart not beating).The patient has a period of 4 to 6 minutes to be resuscitated without
brain damage. Clinical death can be reversed.
Biological Death: The moment the brain cells begin to die. Biological death cannot be reversed.
6. Signs of Certain Death
Lividity: pooling of blood from the lower areas of the body
Purple to bluish color
Rigormortis: Stiffening of body and limbs, occurs usually 4-10 hours after death.
Decomposition: the breakdown of substance into simpler chemical forms.
Other: Mortal wounds such as decapitation, severe crashing injuries
Technique for Opening the Airway
Head-Tilt Chin-Lift
Jaw Thrust
When opening the airway, use the correct method:
Medical case: (any part of the body is affected none in particular)
Head-Tilt Chin-Lift
Trauma case: (specified like head or neck injury)
Jaw Thrust
Head-Tilt Chin-Lift
This is the method of choice for opening the airway.
Do not use this method if you suspect head, neck or spinal injury.
1. Position the patient lying face up (supine position).
2. Kneel by the patients shoulder toward the head.
3. Place hand on the forehead and place the fingertips of your other hand under the bony
part of the patients jaw.
4. Lift on the chin, support the jaw, and at the same time, tilt the head back as far as
possible.
For infants and children: Place in the sniffing positiondo not over-extend.
Important Precautions:
Always keep the patients mouth slightly openuse your thumb to hold down the
patients lower lip.
Never dig into the soft tissue under the patients chin.
Once the airway is open, check breathing.Look, listen and feel. If patient is not breathing,
artificial ventilation should be started. If unable to ventilate, assume the airway is obstructed.
J aw Thrust
The jaw thrust is the only maneuver recommended on an unconscious patient with suspected
head, neck, or spinal injury.
1. Position the patient lying face up.
2. Kneel above the patients head. Place your elbows next to the patients head on the surface
where the patient is lying. Place both hands on either side of the patients head.
3. Grasp the angle of the patients jaw on both sides. For an infant or child use two or three
fingers.
4. Use a lifting motion to move the jaw forward (up) with both hands.
5. Keep the patients mouth slightly open by using your thumbs if needed.
Artificial Ventilation (Rescue Breathing)
Once the patient has an open airway, you can provide artificial ventilation for a patient
breathing inadequately or not at all.
How is it possible to maintain a patient alive with exhaled air? Natural air contains
approximately 21% oxygen and the body only utilises about 5%.Therefore,exhaled air contains
16%oxygen.This exhaled air can resuscitate a person who is not breathing, until a high-
concentration oxygen source is available.
Techniques for Artificial Ventilation
Mouth to mouth and nose
Mouth to mouth
Mouth to mouth
Mouth to stoma
Cardiopulmonary Resuscitation Management
1. Survey the scene, introduce and ask permission
2. Check for responsiveness
a. Tapping of shoulders (2x)
b. Calling of names
3. Shout for help or activate EMS if patient is unresponsive
4. If available get Automated External Defibrillator
5. Perform 30 chest compression for about 15-18 seconds
a. Proper position should be at the midsternum area of the chest
b. Always observe the proper depth of the compression not to deep
c. Allow the chest to return to its normal position
d. Position shoulders over hand with elbows lock and arm straight
e. Keep hand in contact with the chest all the times
6. Opening the airway (head-tilt, Chin-lift maneuver)
a. Proper position is observe
b. Hand on the forehead
c. Fingers on the chin
7. After every 30 chest compressions give two 1 second breath (1,1001,1,1002)
8. While giving ventilation observe:
a. Nose maintained pinch
b. Full slow breaths (1sec)x 2
c. Cover the whole mouth
9. Repeat cycles of chest compressions and 2 ventilations for 5 seconds (approximately 2
minutes)
10. Check the carotid pulse for 10 seconds every 2 minutes (equivalent to 5 cycles of CPR)
11. If pulse is positive and breathing is negative give artificial respirations:
a. Give one full breath every 5 seconds for 24 cycles (blow, 1,1002,1003,1001 up to 24
cycles)
12. While giving artificial ventilation:
a. Nose maintained pinch
b. Full slow breaths (1sec)x 2
c. Cover the whole mouth
13. Recheck the carotid pulse for 10 seconds
14. Place the patient in recovery position if pulse and breathing are both present.
CPR for Infant
1. Survey the scene, introduce and ask permission
2. Check for the infants responsiveness
a. Gently tap the bottom of the infants feet
b. Shout hey baby are you OK?
If there is no response
3. Ask someone to call EMS
4. Perform 30 chest compressions at about 15-18 seconds
a. Position two fingers on the compression area (one finger width below the
imaginary nipple line)
b. Depth of compression at 1/3 to
c. Allow the chest to return to its normal position
d. Maintain open airway with one hand while compressing the chest with two
fingers of the other hand.
e. Keep fingers at contact with the chest at all times.
5. Open the airway (head-tilt, chin-lift maneuver)
a. Proper head-tilt should be observe (neutral or slightly extended position)
b. Hand should be at the infants forehead
c. Fingers should be place at the infants chin
6. Give two puffs after each 30 compressions
7. While giving ventilation:
a. Slow breath 1 second x 2
b. Mouth seal over the infants mouth and nose
8. Repeat cycles of chest compressions and 2 ventilations for 5 cycles (approximately
for 2 minutes)
9. Check the brachial for 10 seconds every 2 minutes (equivalent to 5 cycles of CPR)
10. If pulse is positive and breathing is negative give artificial respiration:
Give 1 breath every 3 seconds for 40 cycles (blow, 1, 1001 up to 40 cycles)
11. While giving ventilation:
a. Slow breath 1 second x 2
b. Mouth seal over the infants mouth and nose
12. Recheck the brachial pulse for 10 seconds
13. Place the infant in recovery position if the pulse and breathing is present.
Recognizing Foreign Body Airway Obstruction (FBAO)
Foreign-Body Airway Obstruction
Foreign-body airway obstruction should be considered in any victimespecially
a younger victim who suddenly stops breathing, becomes cyanotic, or loses
consciousness for no apparent reason.
Two types of FBAO:
Partial:
An object caught in the throat that does not totally block breathing. A patient with
partial obstruction may have adequate or poor air exchange. With adequate air
exchange, the patient may cough forcefully, though there may be wheezing
between coughs. Do not interfere with patients attempt to clear the airway. With
poor air exchange ,the patient will exhibit a weak, ineffective cough, high pitched
noise while inhaling, increased respiratory difficulty and possible cyanosis. Treat
this situation as a complete airway obstruction.
Complete
The patient is unable to speak, breath, or cough. May clutch the neck with thumb and
finger. Air movement will be absent.
Heimlich maneuver
The Heimlich maneuver (sub diaphragmatic abdominal thrusts) is
recommended for relieving foreign-body airway obstruction. By elevating the
diaphragm, the Heimlich maneuver can force air from the lungs to create an
artificial cough intended to expel a foreign body obstructing the airway. Each
individual thrust should be administered with the intent of relieving the
obstruction. It may be necessary to repeat the thrust several times to clear the
airway. Five thrusts per sequence is recommended.
When you perform this maneuver, you should guard against damage to internal
organs, such as rupture or laceration of abdominal or thoracic viscera. To minimize this
possibility, your hands should never be placed on the xiphoid process of the sternum or on the
lower margins of the rib cage. They should be below this area but above the navel and in the
midline. Regurgitation may occur as a result of abdominal thrusts. Be prepared to position
the patient so aspiration does not occur.
HEIMLICH MANEUVER WITH VICTIM STANDING OR SITTING.
To perform the Heimlich maneuver with victim standing or sitting, stand behind the
victim, wrap your arms around the victims waist, and proceed as follows:
Step 1Make a fist with one hand.
Step 2Place the thumb side of the fist against the victims abdomen, in the midline slightly
above the navel and well below the tip of the xiphoid process.
Step 3Grasp the fist with the other hand and press the fist into the victims abdomen with a
quick upward thrust.
Step 4Repeat the thrusts and continue until the object is expelled from the airway or
the patient becomes unconscious.
Each new thrust should be a separate and distinct movement
HEIMLICH MANEUVER WITH VICTIM LYING DOWN.
To perform the Heimlich maneuver with victim lying down, proceed as follows:
Step 1Place the victim in the supine position (face up).
Step 2Kneel astride the victims thighs and place heel of one hand against the victims
abdomen, in the midline slightly above the navel and well below the tip of the xiphoid.
Step 3Place the second hand directly on top of the first.
Step 4Press into the abdomen with a quick upward thrust.
Responsive Adult/Child
1. Introduce, ask for consent and determine complete or partial airway obstruction
2. Get in position, stand behind the patient and place one leg between the patients leg
3. Reach around and locate the navel
4. With the other hand, make a fist and place it against the abdomen, thumb side in, just
above the navel
5. Grasp your fist with the first hand and give up to five abdominal thrust/Heimlich
Maneuver in quick inward and upward direction
6. Observe, the patient will cough or speak if the object is removed or dislodged
7. If still obstructed repeat the thrust until the airway is clear or the patient becomes
unconscious.
Unresponsive Adult/Child
1. Place the patient into supine position
2. Activate EMS
3. Open the airway using the appropriate technique (head-tilt, chin-lift)
4. Assess breathing for ten (10) seconds
5. Attempt to provide one full slow breath
6. If unable to provide adequate chest rise/air bounces back, reposition the head
7. Give again one full slow breath
8. If air still bounces back, give thirty (30) chest compressions
9. Check airway, if obstruction is visible perform finger sweep. If obstruction is not visible
go back to step number 5
10. If object was removed and patient still unconscious:
a. Give two (2) confirmatory blows
b. Check breathing for ten (10) seconds
c. If breathing is adequate, put the patient into recovery position
11. If object was removed and patient becomes conscious, put him/her into recovery position
(side lying).
FBAO in I nfant
1. Survey the scene, introduce and ask permission
2. Pick up the infant and determine if partial or complete obstruction:
a. No strong cry
b. Weak, ineffective cough
c. Difficulty of breathing
3. Support the infants head as you place him down on your forearm. Use your thigh to
support your forearm. Keep the infants head lower than the body.
4. Rapidly deliver 5 back blows just between the shoulder blades. If this fails to expel the
object proceed to the next step.
5. While supporting the infant between your forearms, turn him over onto his back. Perform
5 chest thrust (at about 15-18 seconds).
a. Position two fingers on the compression area (one finger width below the imaginary
nipple line)
b. Depth of compression at 1/3 to
c. Allow the chest to return to its normal position
d. Maintain open airway with one hand while compressing the chest with two fingers of
the other hand.
e. Keep fingers at contact with the chest at all times.
6. Continue with this sequence of back slaps and chest thrust until the object is expelled or
the infant loses consciousness
Unresponsive I nfant
1. Position the infant lying face up, the open the airway by placing the infants head in
neutral or sniffings position
2. Activate EMS if you are not alone (ask someone to call for help)
3. Check breathing for 10 seconds. Open the airway (head-tilt, chin-lift maneuver)
a. Proper head-tilt should be observe (neutral or slightly extended position)
b. Hand should be at the infants forehead
c. Fingers should be place at the infants chin
4. If there are no signs of breathing attempt to ventilate.
a. Slow breath 1 second x 2
b. Mouth seal over the infants mouth and nose
5. If air bounce back reposition the head and ventilate again.
6. If still bounces back proceed to the next procedure
7. Perform 30 chest compressions
8. Open the airway and look for the object. If the object is not visible repeat step 4
9. If the object is visible, do finger sweep. If object is removed proceed
10. Provide two (2) confirmatory blows
11. Check breathing for 10 seconds
12. Place infants into recovery position if infants coughed or becomes responsive.
S-ar putea să vă placă și
- Business Feasibility Study OutlineDocument14 paginiBusiness Feasibility Study OutlineMohamed AbbasÎncă nu există evaluări
- Seed Plants Gymnosperms and Angiosperms 1 PDFDocument17 paginiSeed Plants Gymnosperms and Angiosperms 1 PDFBharatiyaNaari67% (3)
- Peak Flow MeterDocument3 paginiPeak Flow MeterNicole PramonoÎncă nu există evaluări
- Bladder Irrigation CystoclysisDocument4 paginiBladder Irrigation Cystoclysisme meÎncă nu există evaluări
- Understanding the Pathophysiology of Coronary Artery DiseaseDocument14 paginiUnderstanding the Pathophysiology of Coronary Artery DiseasejohnhenryvÎncă nu există evaluări
- Teledentistry 3Document4 paginiTeledentistry 3Annisa DiniÎncă nu există evaluări
- Omaha System Journal ReadingDocument4 paginiOmaha System Journal ReadingAya PaquitÎncă nu există evaluări
- Patient ProfileDocument6 paginiPatient ProfileHardeep KaurÎncă nu există evaluări
- NCPDocument10 paginiNCPCristina L. JaysonÎncă nu există evaluări
- Formulating HypothesisDocument3 paginiFormulating HypothesisMatthew Lim MontenegroÎncă nu există evaluări
- Juvenile CataractDocument12 paginiJuvenile CataractSofea Mustaffa100% (1)
- Nursing InterventionsDocument18 paginiNursing InterventionsMark BellÎncă nu există evaluări
- HypothermiaDocument5 paginiHypothermiaSäbïná D. GabätöÎncă nu există evaluări
- Evidence-Based Nursing: I. Clinical QuestionDocument4 paginiEvidence-Based Nursing: I. Clinical QuestionRay Jorge MarmetoÎncă nu există evaluări
- ICU Case Study: 53-Year-Old Male with Organophosphate PoisoningDocument11 paginiICU Case Study: 53-Year-Old Male with Organophosphate PoisoningPrasyaanth RajanÎncă nu există evaluări
- What Is Meningitis?Document7 paginiWhat Is Meningitis?laujeroÎncă nu există evaluări
- NR 283 Unit 1 DefinitionsDocument3 paginiNR 283 Unit 1 DefinitionsLeksis LoveÎncă nu există evaluări
- Management of SepsisDocument34 paginiManagement of SepsisTamim IshtiaqueÎncă nu există evaluări
- Background of The StudyDocument4 paginiBackground of The StudyRodelen MarañoÎncă nu există evaluări
- Hematology and Systemic Pathology - Paper IIDocument1 paginăHematology and Systemic Pathology - Paper IIrichuÎncă nu există evaluări
- WHO - Acute Diarrhea - Racecadotril - Utk Stop DiareDocument29 paginiWHO - Acute Diarrhea - Racecadotril - Utk Stop Diaremarkus_danusantosoÎncă nu există evaluări
- Anthrax Clinical PathwayDocument4 paginiAnthrax Clinical PathwayNeurologianak HarkitÎncă nu există evaluări
- Health Assessment - General SurveyDocument73 paginiHealth Assessment - General Surveymamiyo71Încă nu există evaluări
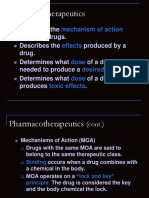
- Pharmaco TherapeuticsDocument19 paginiPharmaco TherapeuticsJareena BegumÎncă nu există evaluări
- Guide To IV SolutionsDocument1 paginăGuide To IV SolutionsKim BadillesÎncă nu există evaluări
- Oxygen Therapy For ChildrenDocument18 paginiOxygen Therapy For ChildrenUday KumarÎncă nu există evaluări
- Respiratory Physiology GuideDocument21 paginiRespiratory Physiology GuideKingsley UdeajaÎncă nu există evaluări
- NCP Cardio PrintDocument7 paginiNCP Cardio PrintNicole MapiliÎncă nu există evaluări
- Toxic Megacolon: Emergency Surgery Indications for Severe ColitisDocument10 paginiToxic Megacolon: Emergency Surgery Indications for Severe ColitisVikas MataiÎncă nu există evaluări
- KMB Diabetes InsipidusDocument24 paginiKMB Diabetes InsipidusNur Rofikoh Bil Karomah100% (1)
- Mews ScoreDocument13 paginiMews Score2009nicoleta100% (2)
- 17 - Enhanced Recovery PrinciplesDocument7 pagini17 - Enhanced Recovery Principlesbocah_britpopÎncă nu există evaluări
- Status Asthmaticus in ChildrenDocument76 paginiStatus Asthmaticus in ChildrenJesterCruzÎncă nu există evaluări
- Interactive Session On Sodium Homeostasis: Dr.M.Emmanuel Bhaskar Assistant Professor in Medicine SRMC & RiDocument64 paginiInteractive Session On Sodium Homeostasis: Dr.M.Emmanuel Bhaskar Assistant Professor in Medicine SRMC & Ridrbhaskar100% (4)
- Nursing Care Plan for a Patient with Hemorrhagic StrokeDocument5 paginiNursing Care Plan for a Patient with Hemorrhagic StrokeKhim BalcitaÎncă nu există evaluări
- Correlation of pulmonary pressure and hemoglobin in ASD patientsDocument28 paginiCorrelation of pulmonary pressure and hemoglobin in ASD patientsIzharIsmailÎncă nu există evaluări
- Nursing Programs: Lactated Ringers (Also Known As LR, Ringers Lactate, or RL)Document5 paginiNursing Programs: Lactated Ringers (Also Known As LR, Ringers Lactate, or RL)KiaBlancheTahud100% (1)
- Green SerumDocument1 paginăGreen SerumDocAxi Maximo Jr AxibalÎncă nu există evaluări
- Long Case PresentationDocument3 paginiLong Case PresentationAkshat WaranÎncă nu există evaluări
- Inserting NG tube guide stepsDocument1 paginăInserting NG tube guide stepsKay BristolÎncă nu există evaluări
- DengueDocument34 paginiDengueNa YamzonÎncă nu există evaluări
- Congenital Diaphragmatic Hernia (CDH) Information For Health ProfessionalsDocument5 paginiCongenital Diaphragmatic Hernia (CDH) Information For Health ProfessionalsMangku Liong GuanÎncă nu există evaluări
- ExtubationDocument7 paginiExtubationbalab2311Încă nu există evaluări
- Final ResearchDocument65 paginiFinal ResearchHarbrinder GurmÎncă nu există evaluări
- AOA ConjunctivitisDocument33 paginiAOA ConjunctivitiseloooyiyÎncă nu există evaluări
- Operating Room Write UpDocument2 paginiOperating Room Write UpEnrico Sapitula Del RosarioÎncă nu există evaluări
- Anaphylaxis (Case)Document4 paginiAnaphylaxis (Case)drkmwaiÎncă nu există evaluări
- Heat StrokeDocument8 paginiHeat StrokePrateek Barapatre0% (1)
- 10 EncephalopathyDocument18 pagini10 EncephalopathyAbdullah ShiddiqÎncă nu există evaluări
- Glasgow Coma Scale Assessment and UsesDocument13 paginiGlasgow Coma Scale Assessment and UsesSofianÎncă nu există evaluări
- Quizzes ForDocument14 paginiQuizzes Forohsnapitslei100% (1)
- ABDOMINAL PARACENTESIS PROCEDUREDocument5 paginiABDOMINAL PARACENTESIS PROCEDUREVijith.V.kumar100% (1)
- Cardiopulmonary Resuscitation PresentationDocument29 paginiCardiopulmonary Resuscitation PresentationolelÎncă nu există evaluări
- Cardiopulmonary ResuscitationDocument6 paginiCardiopulmonary ResuscitationHonelie Tomagan DasiganÎncă nu există evaluări
- Basic Life Support HandoutDocument13 paginiBasic Life Support HandoutmdavaoÎncă nu există evaluări
- CPR and Airway Mgt.Document26 paginiCPR and Airway Mgt.Pierenne Virgil Suarez PinlacÎncă nu există evaluări
- CPR ReportingDocument39 paginiCPR ReportingNheler SonÎncă nu există evaluări
- Cardiopulmonary Resuscitation (CPR), Is Emergency First Aid For An Unconscious Person On WhomDocument10 paginiCardiopulmonary Resuscitation (CPR), Is Emergency First Aid For An Unconscious Person On WhompusbajivaÎncă nu există evaluări
- Cardiopulmonary Resuscitation: By: Dr. Mohita SinghDocument19 paginiCardiopulmonary Resuscitation: By: Dr. Mohita Singhkhanfayiq11Încă nu există evaluări
- Basic Life SupportDocument9 paginiBasic Life Supportaina_boydonÎncă nu există evaluări
- BPAT April 2Document3 paginiBPAT April 2Ash CampiaoÎncă nu există evaluări
- Lecture in TOGDocument55 paginiLecture in TOGAsh CampiaoÎncă nu există evaluări
- GUIDELINES ON PROPER ACCOMPLISHMENT OF PHILHEALTH CLAIM FORM 1Document4 paginiGUIDELINES ON PROPER ACCOMPLISHMENT OF PHILHEALTH CLAIM FORM 1Ash CampiaoÎncă nu există evaluări
- Leg MedDocument12 paginiLeg MedAsh CampiaoÎncă nu există evaluări
- Bureau of Fire Protection - ARMM: Basic First AidDocument50 paginiBureau of Fire Protection - ARMM: Basic First AidAsh CampiaoÎncă nu există evaluări
- Ignition Temperature (Temperature Needed To Burn), and If There Is Enough Oxygen Present, TheDocument24 paginiIgnition Temperature (Temperature Needed To Burn), and If There Is Enough Oxygen Present, TheRalph CelesteÎncă nu există evaluări
- Indices DNL: Slight Underperformance in 1Q15 On Lingering Effects of Port CongestionDocument10 paginiIndices DNL: Slight Underperformance in 1Q15 On Lingering Effects of Port CongestionAsh CampiaoÎncă nu există evaluări
- Wao Lecture and Training Course June 24 2016Document3 paginiWao Lecture and Training Course June 24 2016Ash CampiaoÎncă nu există evaluări
- Service Record HEPEDocument2 paginiService Record HEPEJohn CaezarÎncă nu există evaluări
- Terms of Reference For Sajahatra BangsamoroDocument5 paginiTerms of Reference For Sajahatra BangsamoroOffice of the Presidential Adviser on the Peace ProcessÎncă nu există evaluări
- LANDBANK Iaccess FAQsDocument16 paginiLANDBANK Iaccess FAQsAsh Campiao100% (1)
- Checklist of Requirements For Hospital Accreditation (Secondary)Document4 paginiChecklist of Requirements For Hospital Accreditation (Secondary)pamgelÎncă nu există evaluări
- Fire Code of The Philippines 2008Document475 paginiFire Code of The Philippines 2008RISERPHIL89% (28)
- Partnership Agency and TrustDocument29 paginiPartnership Agency and TrustAsh CampiaoÎncă nu există evaluări
- Comprehensive Fire Investigation ProceduresDocument9 paginiComprehensive Fire Investigation Procedureshailglee192571% (7)
- Summary of Water CodeDocument11 paginiSummary of Water CodeAsh CampiaoÎncă nu există evaluări
- 111222Document3 pagini111222Ash CampiaoÎncă nu există evaluări
- FF Sample TestDocument16 paginiFF Sample TestAsh CampiaoÎncă nu există evaluări
- Separate Opinion Chico-Nazario, J.Document4 paginiSeparate Opinion Chico-Nazario, J.Ash CampiaoÎncă nu există evaluări
- Disqualification of CandidatesDocument2 paginiDisqualification of CandidatesRaffyMondragonÎncă nu există evaluări
- 2243 Industrial Instrument Technicians and MechanicsDocument2 pagini2243 Industrial Instrument Technicians and MechanicsAsh CampiaoÎncă nu există evaluări
- FireDocument11 paginiFireAsh CampiaoÎncă nu există evaluări
- Abbas V ComelecDocument8 paginiAbbas V ComelecAsh CampiaoÎncă nu există evaluări
- What Is FireDocument11 paginiWhat Is FireAsh CampiaoÎncă nu există evaluări
- Personal Data SheetDocument4 paginiPersonal Data SheetLeonil Estaño100% (7)
- Law On Natural Resources ReviewerDocument130 paginiLaw On Natural Resources ReviewerAsh CampiaoÎncă nu există evaluări
- What Is FireDocument11 paginiWhat Is FireAsh CampiaoÎncă nu există evaluări
- Omnibus Election Code of The PhilippinesDocument64 paginiOmnibus Election Code of The PhilippinesElfenLiedFanGirlÎncă nu există evaluări
- Negotiable Instruments CasesDocument7 paginiNegotiable Instruments CasesAsh CampiaoÎncă nu există evaluări
- Legal Ethics and Practical Exercises - I - (10%) What Are The Duties of An Attorney?Document7 paginiLegal Ethics and Practical Exercises - I - (10%) What Are The Duties of An Attorney?Ash CampiaoÎncă nu există evaluări
- Necropsy - Killer Whale WinstonDocument4 paginiNecropsy - Killer Whale WinstonThe Orca Project Corp100% (2)
- Myocardial Infarction Covid Heart Failure Quiz RLE 5-6-2021Document58 paginiMyocardial Infarction Covid Heart Failure Quiz RLE 5-6-2021MuhyeeSalaIdjadÎncă nu există evaluări
- NCLEX QuestionsDocument5 paginiNCLEX QuestionsMeganÎncă nu există evaluări
- Rehabilitasi Pasca CABGDocument23 paginiRehabilitasi Pasca CABGPaulina WowilingÎncă nu există evaluări
- Cardiovascular Pathology The Perfect Preparation For USMLE Step 1Document256 paginiCardiovascular Pathology The Perfect Preparation For USMLE Step 1Bea SphÎncă nu există evaluări
- Drug-Study NCPDocument5 paginiDrug-Study NCPMURILLO, FRANK JOMARI C.Încă nu există evaluări
- Patent Ductus ArteriosusDocument5 paginiPatent Ductus ArteriosusAisyahKautsarIlmiÎncă nu există evaluări
- Fins'12 1 2Document125 paginiFins'12 1 2Brutus AntonyÎncă nu există evaluări
- St. Luke's College of Medicine Cognitive and Mental Disorders LectureDocument8 paginiSt. Luke's College of Medicine Cognitive and Mental Disorders LectureDane Mikhael CalicaÎncă nu există evaluări
- Coagulation Tests: Clotting Time, Bleeding Time, Prothrombin Time, Activated Partial Thromboplastin TimeDocument15 paginiCoagulation Tests: Clotting Time, Bleeding Time, Prothrombin Time, Activated Partial Thromboplastin TimeAnastasiaÎncă nu există evaluări
- First Year MBBSDocument25 paginiFirst Year MBBSTofik MohammedÎncă nu există evaluări
- Announcement List Displayed Poster 32nd ASMIHADocument36 paginiAnnouncement List Displayed Poster 32nd ASMIHADewi AmeliaÎncă nu există evaluări
- Esophagus: Pipe or Gullet, Is An Organ in Vertebrates Through Which Food PassesDocument12 paginiEsophagus: Pipe or Gullet, Is An Organ in Vertebrates Through Which Food PassesCrow LordÎncă nu există evaluări
- Topic 9 - Transport in Animals: Blood and Lymph VesselsDocument15 paginiTopic 9 - Transport in Animals: Blood and Lymph Vesselsgytfnhj.comÎncă nu există evaluări
- Dysrhythmias ChartDocument6 paginiDysrhythmias Chartjkrix100% (1)
- Rheumatic FeverDocument26 paginiRheumatic FeverAhmed Ben Bella100% (2)
- Antiadrenergic DrugsDocument19 paginiAntiadrenergic DrugsshivanshpandeÎncă nu există evaluări
- TOG 2007 915-20 Review Cardiac Disease in Pregnancy Part 1 CongenitalDocument6 paginiTOG 2007 915-20 Review Cardiac Disease in Pregnancy Part 1 Congenitalsaeed hasan saeedÎncă nu există evaluări
- Circulatory System LabDocument3 paginiCirculatory System LabMatt Joseph CabantingÎncă nu există evaluări
- 84 Questions - With Answer - Gloucestershire HospitalsDocument171 pagini84 Questions - With Answer - Gloucestershire HospitalsŞahin EmerÎncă nu există evaluări
- ACLS Post Test (Copy) 낱말 카드 - QuizletDocument18 paginiACLS Post Test (Copy) 낱말 카드 - Quizlet김민길Încă nu există evaluări
- Medication AdherenceDocument14 paginiMedication Adherencemunish narangÎncă nu există evaluări
- CMH 2019 0010nDocument45 paginiCMH 2019 0010nTerran00 :DÎncă nu există evaluări
- Case Studies: Case 1 Feline 8 Month Old Intact Male DSHDocument34 paginiCase Studies: Case 1 Feline 8 Month Old Intact Male DSHGuilherme Oliveira BjjÎncă nu există evaluări
- 31 - DINAMAP SuperSTAT NIPB - White Paper - JB26543XX - Dec8Document4 pagini31 - DINAMAP SuperSTAT NIPB - White Paper - JB26543XX - Dec8Jorio LemosÎncă nu există evaluări
- Hypertensive Disorders in PregnancyDocument10 paginiHypertensive Disorders in PregnancyRwabugili ChrisÎncă nu există evaluări
- 4 EpistaxisDocument51 pagini4 EpistaxisNicÎncă nu există evaluări
- Hema 2 - Prelim Topic 1-Intro To HemostasisDocument4 paginiHema 2 - Prelim Topic 1-Intro To HemostasisLowenstein JenzenÎncă nu există evaluări
- MRCP Recall May 19Document9 paginiMRCP Recall May 19Ophthalmology PLUSÎncă nu există evaluări
- The Importance of Non-Exercise Movement For Longevity: by Dr. MercolaDocument4 paginiThe Importance of Non-Exercise Movement For Longevity: by Dr. MercolaSellappan MuthusamyÎncă nu există evaluări
- Roxane Gay & Everand Originals Presents: Good Girl: Notes on Dog RescueDe la EverandRoxane Gay & Everand Originals Presents: Good Girl: Notes on Dog RescueEvaluare: 5 din 5 stele5/5 (12)
- The Obesity Code: Unlocking the Secrets of Weight LossDe la EverandThe Obesity Code: Unlocking the Secrets of Weight LossEvaluare: 5 din 5 stele5/5 (4)
- Dog Training Journeys: A Guide to Training and Bonding with Your Mix-Breed DogDe la EverandDog Training Journeys: A Guide to Training and Bonding with Your Mix-Breed DogEvaluare: 4.5 din 5 stele4.5/5 (77)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingDe la EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingEvaluare: 3.5 din 5 stele3.5/5 (33)
- 10% Human: How Your Body's Microbes Hold the Key to Health and HappinessDe la Everand10% Human: How Your Body's Microbes Hold the Key to Health and HappinessEvaluare: 4 din 5 stele4/5 (33)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDe la EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingDe la EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingEvaluare: 5 din 5 stele5/5 (5)
- Mastering Parrot Behavior: A Step-by-Step Guide to Building a Strong Relationship with Your Avian FriendDe la EverandMastering Parrot Behavior: A Step-by-Step Guide to Building a Strong Relationship with Your Avian FriendEvaluare: 4.5 din 5 stele4.5/5 (69)
- Horse Training 101: Key Techniques for Every Horse OwnerDe la EverandHorse Training 101: Key Techniques for Every Horse OwnerEvaluare: 4.5 din 5 stele4.5/5 (27)
- Cats Can Learn Too: A Simple Guide to Training Your Furry FriendDe la EverandCats Can Learn Too: A Simple Guide to Training Your Furry FriendEvaluare: 4.5 din 5 stele4.5/5 (55)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDe la EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisEvaluare: 4.5 din 5 stele4.5/5 (41)
- Roxane Gay & Everand Originals Presents: Good Girl: Notes on Dog RescueDe la EverandRoxane Gay & Everand Originals Presents: Good Girl: Notes on Dog RescueEvaluare: 5 din 5 stele5/5 (2)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisDe la EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisEvaluare: 5 din 5 stele5/5 (8)
- All That Remains: A Renowned Forensic Scientist on Death, Mortality, and Solving CrimesDe la EverandAll That Remains: A Renowned Forensic Scientist on Death, Mortality, and Solving CrimesEvaluare: 4.5 din 5 stele4.5/5 (397)
- This Is Your Brain On Parasites: How Tiny Creatures Manipulate Our Behavior and Shape SocietyDe la EverandThis Is Your Brain On Parasites: How Tiny Creatures Manipulate Our Behavior and Shape SocietyEvaluare: 3.5 din 5 stele3.5/5 (31)
- Crypt: Life, Death and Disease in the Middle Ages and BeyondDe la EverandCrypt: Life, Death and Disease in the Middle Ages and BeyondEvaluare: 4 din 5 stele4/5 (3)
- DSM-5-TR Diagnostic And Statistical Manual Of Mental Disorders: DSM 5 TR Desk Reference to the Diagnostic CriteriaDe la EverandDSM-5-TR Diagnostic And Statistical Manual Of Mental Disorders: DSM 5 TR Desk Reference to the Diagnostic CriteriaÎncă nu există evaluări
- Will's Red Coat: The Story of One Old Dog Who Chose to Live AgainDe la EverandWill's Red Coat: The Story of One Old Dog Who Chose to Live AgainEvaluare: 4.5 din 5 stele4.5/5 (18)
- The Dog Listener: Learn How to Communicate with Your Dog for Willing CooperationDe la EverandThe Dog Listener: Learn How to Communicate with Your Dog for Willing CooperationEvaluare: 4 din 5 stele4/5 (37)
- Lies My Doctor Told Me: Medical Myths That Can Harm Your HealthDe la EverandLies My Doctor Told Me: Medical Myths That Can Harm Your HealthEvaluare: 5 din 5 stele5/5 (1)
- Multiple Choice Questions in Paediatric SurgeryDe la EverandMultiple Choice Questions in Paediatric SurgeryEvaluare: 1 din 5 stele1/5 (1)
- An Eagle Named Freedom: My True Story of a Remarkable FriendshipDe la EverandAn Eagle Named Freedom: My True Story of a Remarkable FriendshipÎncă nu există evaluări
- Seeking Heaven: Sound Journeys into the BeyondDe la EverandSeeking Heaven: Sound Journeys into the BeyondEvaluare: 5 din 5 stele5/5 (26)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisDe la EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisEvaluare: 4 din 5 stele4/5 (9)
- Uncontrolled Spread: Why COVID-19 Crushed Us and How We Can Defeat the Next PandemicDe la EverandUncontrolled Spread: Why COVID-19 Crushed Us and How We Can Defeat the Next PandemicÎncă nu există evaluări
- The Other End of the Leash: Why We Do What We Do Around DogsDe la EverandThe Other End of the Leash: Why We Do What We Do Around DogsEvaluare: 5 din 5 stele5/5 (63)
- The Intuitive Eating Workbook: 10 Principles for Nourishing a Healthy Relationship with FoodDe la EverandThe Intuitive Eating Workbook: 10 Principles for Nourishing a Healthy Relationship with FoodEvaluare: 4.5 din 5 stele4.5/5 (20)