Documente Academic
Documente Profesional
Documente Cultură
Cardiology Study Guide Handout
Încărcat de
alinida89Descriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Cardiology Study Guide Handout
Încărcat de
alinida89Drepturi de autor:
Formate disponibile
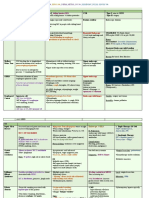
CARDIOLOGY
CARDIOMYOPATHIES
Cardiomyopathy refers specifically to
problems within the heart muscle, and
these problems usually result in heart
failure.
1. Dilated
2. Hypertrophic
3. Restrictive
Ischemic cardiomyopathy implies that the cause
of muscle damage is coronary artery disease
Dilated
Cardiomyopathy
o Dilated cardiomyopathy implies that the
muscle damage has resulted in enlargement
of the heart
Generally Idiopathic
Impaired Systolic Function
________________________
Etiologies
Most times Idiopathic (50%)
Myocarditis (in Children)
Alcohol Abuse
Cocaine Abuse
Tachycardias AFib / SVT
Autoimmune Disease - Lupus and
Rheumatoid Arthritis
Pheochromocytoma - Excess
Catecholamine release from a tumor
Coronary Artery Disease - Ischemic
Cardiomyopathy
Deficiencies of certain vitamins and
minerals - Thiamine, Calcium,
Magnesium
End-stage kidney disease
_________________________
Most common Cardiomyopathy
Dilated Cardiomyopathy is a condition in
which the heart becomes weakened and
enlarged, and it cannot pump blood
efficiently
The decreased heart function can affect
the lungs, liver, and other body systems
_________________________
Etiologies
Thyroid
Infections - HIV / Viral
Chagas Disease, and Lyme disease
Inherited Disorders - Muscular
Dystrophy
Chemotherapy Meds / Toxic
Medications **Doxorubicin **
HTN
Pregnancy - Peripartum
Cardiomyopathy
Stress-induced Cardiomyopathy
Trace elements, such as Lead,
Arsenic, or Mercury
Family History
_________________________
Dilated Cardiomyopathy
Physical Exam
Crackles
S3 Gallop
Elevated JVD
Cardiomegaly
ECHO
Global Chamber Enlargement
Mitral Regurgitation
Tricuspid Regurgitation
Ejection Fraction
Thrombosis
EKG
BBB
Poor R-wave Progression
Arrhythmias
CXR
Global Cardiomegaly
Global Heart
CHF
_________________________
Dilated Cardiomyopathy
Signs & Symptoms
CHF
Systemic Embolus
Pulmonary Embolus
Deadly Arrhythmias
Sudden Death
Treatment
Treat Underlying Disease
ETOH Abstinence
Thyroid Management
Treat CHF
Anticoagulants
Arrhythmia Prophylaxis
Heart Transplant
Medications
ACE inhibitors
Angiotensin Receptor Blockers (ARBs)
Losartan
Candesartan
Beta-blockers, such as
Carvedilol
Metoprolol
Diuretics, including thiazide, loop
diuretics, and potassium-sparing
diuretics
Digitalis glycosides
_________________________
Hypertrophic
Cardiomyopathy
Hypertrophic cardiomyopathy involves
enlargement and thickening of the heart
muscle.
A leading cause of sudden cardiac death
in young athletes
A significant cause of sudden
unexpected cardiac death in any age
group. Younger people are likely to have
a more severe form of hypertrophic
cardiomyopathy
_________________________
Etiologies
Genetic
Myocyte Disarray
Myocyte Hypertrophy
Interstitial Fibrosis
_________________________
Signs & Symptoms
Often Asymptomatic
DOE
Angina
Pre-Syncope / Syncope
CHF
Deadly Arrhythmias
Sudden Death
Physical Exam
Pulse Rapid Upstroke
Bifid Carotid Pulse
Sustained Strong PMI
LV Lift
Murmur:
Harsh, Systolic
Diamond Shaped
LLSB / Erbs Point
Increased w/ Valsalva & Standing
Hypertrophic
Cardiomyopathy
Unexplained Ventricular Hypertrophy
NOT due to HTN or Aortic Stenosis
Disease of the Myocardium - Cardiac
Muscle is Hypertrophied - without any
obvious cause.
_________________________
ECHO
*Asymmetric* Septal Hypertrophy
EKG
LVH
High Voltage
Q Waves in 1 & aVF
CXR - is Normal
Treatment
Avoid Volume Depletion
Avoid Strenuous Exercise
Beta-blockers
If refractive, Surgery is indicated
Surgical Myectomy
Septal Alcohol Ablation
Dual Chamber Pacing
Arrhythmia Prophylaxis
Amiodarone
Implanted Defibrillator
_________________________
Restrictive
Cardiomyopathy
A group of disorders in which the heart
chambers are unable to properly fill with
blood because of stiffness in the heart.
Systolic Function is preserved
_________________________
Etiologies
Infiltrative
Amyloidosis
Sarcoidosis
Non-Infiltrative
Scleroderma
Idiopathic Myocardial Fibrosis
Storage Disease
Hemochromatosis
Fabrys
Glycogen Storage
Endomyocardial
Diseases of the heart lining
(endocardium)
Endomyocardial Fibrosis
Loeffler's Syndrome
Radiation
Carcinoid
Signs & Symptoms
CHF (w/ preserved Systolic Function)
Arrhythmias
Elevated JVD
+ Kussmauls Sign
S3, S4 Gallop
Mitral Regurgitation
Tricuspid Regurgitation
_________________________
Restrictive
Cardiomyopathy
The heart is of normal size or only
slightly enlarged. However, it cannot
relax normally during the time between
heartbeats when the blood returns from
the body to the heart (diastole)
_________________________
Physical Exam
Signs of Right Heart Failure
S/S of underlying condition
ECHO
LVH, RVH, LAE, RAE
Valve Thickening
EKG
Low Voltage
CXR
Normal to Mild Enlargement
Treatment
Endo-myocardial Biopsy to determine
etiology
Exclude Constrictive Pericarditis
Treat underlying disease
Control HR / manage AFib
Supportive Care
Heart Transplant
Poor Prognosis
_________________________
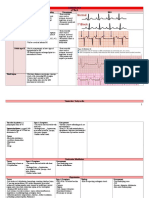
Conduction Disorders
NARROW QRS
Regular Rhythms
Sinus Tach (100 140)
Atrial Flutter (150)
SVT (160+)
NARROW QRS
Irregular Rhythms
Atrial Fibrillation
Multi-focal Atrial Tach
Atrial Fibrillation
Most common cardiac arrhythmia
Quivering of the heart muscles of the
atria
Narrow QRS,
No P-waves
Irregular Rhythm
Asymptomatic and not generally life-
threatening
May have palpitations, fainting, chest
pain, or congestive heart failure
Treated with medications which either
slow the heart rate or revert the heart
rhythm back to normal.
Synchronized electrical cardioversion
may also be used to convert AF to a
normal heart rhythm. Surgical and
catheter-based therapies may also be
used to prevent recurrence of AF in
certain individuals.
People with AF are often given
anticoagulants such as Warfarin to
protect them from stroke.
A. Fib vs. NSR
1. Narrow QRS
2. No Ps,
3. Irregular Rhythm
Wolff Parkinson White
(SVT)
Wolff-Parkinson-White syndrome is a
heart condition in which there is an extra
electrical pathway (circuit) in the heart.
Leads to episodes tachycardia
Pre-excitation Syndrome
WPW is the most common tachycardia in
infants and children
Death from WPW occurs secondary to
associated dysrhythmias or from
mistreatment of these dysrhythmias with
inappropriate medications.
S/Sx
1. Chest pain or chest tightness
2. Dizziness
3. Light-headedness
4. Syncope / Near Syncope
5. Shortness of breath
HR commonly presents @ 250 bpm
Often with associated hypotension.
Many patients are not aware of their
underlying condition
Treatment
Medication used to control or prevent
tachycardia.
1. Adenosine
2. Antiarrhythmics
3. Amiodarone.
Cardioversion
Radiofrequency Catheter ablation
RCA is curative
Wolff Parkinson White
(SVT)
Atrial fibrillation in a patient with Wolff-Parkinson-
White syndrome. Note the extremely rapid ventricular
rate and variability in QRS morphology. Several
minutes later, the patient developed ventricular
fibrillation.
Atrial Flutter
Electrical impulses take an abnormal path
through the atria, typically circulating around
the tricuspid valve in the right atrium.
The abnormal path of the impulses makes
the atria contract very rapidly, typically
about 250-350 beats per minute.
These rapid contractions are slowed when
they reach the AV node often with every
second or third contraction reaching the
ventricle.
Regular Rhythm, but Tachycardic
AF comes from the atria Supraventricular
tachycardia - (above the ventricles)
May cause decreased vital organ perfusion
May be transient - known as Paroxysmal
Atrial Flutter.
More often, AF lasts for days to weeks and
is known as Persistent Atrial Flutter.
With proper treatment, Atrial F is rarely life-
threatening.
Complications of Atrial Flutter Stroke, but
can be prevented with Anti-Thrombolytic -
Warfarin
Calcium channel blockers
Beta-blockers
Adenosine
Radio-Ablation to restore Rhythm
Atrial Flutter
Sawtooth Pattern
1
st
Degree AV Block
P for every QRS
PR > 0.20 sec
Seen in Lyme Disease
No Intervention Required
Do Not Add Digoxin
1
st
Degree AV Block
2
nd
Degree AV Block
(Mobitz II)
Note a P with no QRS after
Check PR Interval
PR Interval is equal, then Mobitz II
Treatment:
As with type I block, AV nodal agents
should be avoided, and an anti-ischemic
regimen should be instituted if ischemia is
suspected.
Transcutaneous pacing pads should be
applied to all patients, including
asymptomatic patients, as patients with
Mobitz II second-degree AV block have a
propensity to progress to complete heart
block.
2
nd
Degree AV Block
(Mobitz II)
2
nd
Degree AV Block
(Mobitz I)
(Wenckebach)
Longer, Longer, Longest
Dropped QRS
No specific therapy is required unless the
patient is symptomatic
Patients with suspected myocardial
ischemia should be treated with an
appropriate anti-ischemic regimen.
AV nodal blocking agents (including beta-
blockade) should be avoided
Symptomatic patients should be treated
with atropine and transcutaneous pacing.
However, atropine should be administered
with caution in patients with suspected
myocardial ischemia, as ventricular
dysrhythmias can occur in this situation.
2
nd
Degree AV Block
(Mobitz I)
(Wenckebach)
3rd Degree AV Block
(Complete)
P followed by P
Slow HR
P waves everywhere
Treatment:
For any symptomatic patient,
transcutaneous pacing.
Valsalva should be avoided
Atropine cautiously - likely to be ineffective
in a wide complex QRS rhythm and can be
dangerous if the patient is having a
concurrent MI.
Urgent placement of Pacemaker
LBBB
A cardiac conduction abnormality where
activation of the Left Ventricle is delayed, which
results in the left ventricle contracting later than
the Rght Ventricle.
Among the causes of LBBB are:
Aortic stenosis
Dilated cardiomyopathy
Acute myocardial infarction
Extensive cases of coronary artery
disease
Primary disease of the cardiac electrical
conduction system
Long standing hypertension leading to
aortic root dilation and subsequent aortic
regurgitation
Treatment
Medical Care: Patients with LBBB require
complete cardiac evaluation, and those
with LBBB and syncope or near-syncope
may require a pacemaker.
Surgical Care: Some patients with LBBB,
a markedly prolonged QRS, and
congestive heart failure may benefit from
a pacemaker, which provides rapid left
ventricular contractions.
LBBB
RBBB
During a right bundle branch block, the right
ventricle is not directly activated by impulses
travelling through the right bundle branch. The
left ventricle however, is still normally activated
by the left bundle branch.
These impulses are then able to travel through
the myocardium of the left ventricle to the right
ventricle and depolarise the right ventricle this
way. As conduction through myocardium is
slower than conduction through the Bundle of
His-Purkinje fibres the QRS complex is seen to
be widened.
The QRS complex often shows an extra
deflection which reflects the rapid depolarisation
of the left ventricle followed by the slower
depolarisation of the right ventricle.
Otherwise healthy people may have a right
bundle branch block and it does not appear to
cause any harm
Paroxysmal Supraventricular
Tachycardia
Supraventricular tachycardia (SVT), a common
clinical condition, is any tachyarrhythmia that
requires Atrial and/or Atrioventricular (AV) nodal
tissue for its initiation and maintenance.
Paroxysmal Supraventricular Tachycardia (PSVT)
is episodic, with an abrupt onset and termination.
It is usually a narrow-complex tachycardia that
has a regular, rapid rhythm
Exceptions include Atrial Fibrillation (AF) and
Multifocal Atrial Tachycardia (MAT). Aberrant
conduction during SVT results in a wide-complex
tachycardia.
SVT occurs in persons of all age groups, and
treatment can be challenging.
Manifestations of SVT are quite variable;
patients may be asymptomatic or they may
present with minor palpitations or more severe
symptoms.
Paroxysmal Supraventricular
Tachycardia
Premature Beats
Most common type of arrhythmia.
They're harmless most of the time and
often don't cause any symptoms.
When symptoms do occur, they
usually feel like fluttering in the chest
or a feeling of a skipped beat
Most of the time, premature beats
need no treatment, especially in
healthy people.
Premature beats that occur in the atria
are called premature atrial
contractions, or PACs.
Premature beats that occur in the
ventricles are called premature
ventricular contractions, or PVCs.
In most cases, premature beats occur
naturally, not due to any heart
disease. But certain heart diseases
can cause premature beats. They also
can happen because of stress, too
much exercise, or too much caffeine
or nicotine.
PVCs_________ ________
Ventricular Tachycardia
Wide-complex tachycardia; V tach;
Ventricular tachycardia (VT) is a rapid
heartbeat that starts in the ventricles
Defined as HR of 100 + bpm + 3 irregular
heartbeats in a row
May develop as an early or late
complication of an M.I.
Major cause of sudden cardiac death.
May occur in pts w/
Cardiomyopathy
Heart failure
Heart surgery
Myocarditis
Valvular heart disease
pts w/ no cardiac disease
Can also be caused by:
Anti-arrhythmic medications
Changes in blood chemistry -
Hypokalemia
Changes in pH (acid-base)
Hypoxia
Symptoms
Chest discomfort (angina)
Syncope
dizziness
Palpitations
Shortness of breath
Note: Symptoms may start and stop suddenly.
In some cases, there are no symptoms.
Signs:
Absent pulse
Loss of consciousness
Normal or low blood pressure
Rapid pulse
Ventricular Tachycardia
_________________
Treatment
Treatment depends on the symptoms, and the
type of heart disorder - may not need treatment.
Emergency V Tach:
CPR
Defibrillation / Cardioversion
Anti-arrhythmic medications
1. Lidocaine
2. Procainamide - IV
3. Sotalol - IV
4. Amiodarone IV
Long-term treatment may require the use of oral
anti-arrhythmic medications
1. Procainamide
2. Amiodarone
3. Sotalol
Radiofrequency Catheter Ablation
curative
Preferred treatment for many chronic VT -
Implantable Cardioverter Defibrillator
(ICD).
Torsades de Pointes
Polymorphic ventricular tachycardia with a
characteristic twist of the QRS
Ventricular Tachycardia that is often due
to congenital heart disease or the use of
certain medications.
"twisting of the points".
TdP can be:
Inherited as congenital mutations of ion
channels carrying the cardiac
impulse/action potential
Acquired as a result of drugs that block
these cardiac ion currents.
Common causes
Diarrhea
Hypomagnesemia
Hypokalemia.
Can also be the side effect of anti-arrhytmic
medications such as Sotalol, Procainamide
and Quinidine.
________________________
Other Causes:
Familial long QT syndrome
Class IA antiarrhythmics
Class III antiarrhythmics
Hypocalcemia
Hypoxia
Acidosis
Heart failure
Left ventricular hypertrophy
Slow heart rate
Female gender
Hypothermia
Subarachnoid hemorrhage
Malnourishment
Chronic alcoholics.
Drug interactions:
Erythromycin or Moxifloxacin, taken
concomitantly Nitroimidazol
Various medications like methadone,
lithium, tricyclic antidepressants or
phenothiazines may also contribute
Ventricular Fibrillation
Ventricular fibrillation (VF) begins as a quasi-
periodic reentrant pattern of excitation in the
ventricles with resulting poorly synchronized and
inadequate myocardial contractions. The heart
consequently immediately loses its ability to
function as a pump.
As the initial reentrant pattern of excitation breaks
up into multiple smaller wavelets, the level of
disorganization increases. Sudden loss of cardiac
output with subsequent tissue hypoperfusion
creates global tissue ischemia; brain and
myocardium are most susceptible. VF is the
primary cause of sudden cardiac death (SCD).
Sudden cardiac death can be viewed as a
continuum of electromechanical states of the
heart: ventricular tachycardia (VT), ventricular
fibrillation (VF), pulseless electrical activity (PEA),
and Asystole.
VF is the most common initial state, and, because
of insufficient perfusion of vital cardiac tissues, it
degenerates to Asystole if left untreated.
Fibrillation is an uncontrolled twitching or
quivering of muscle fibers (fibrils). When it
occurs in the lower chambers of the heart, it is
called ventricular fibrillation.
During ventricular fibrillation, blood is not
removed from the heart. Sudden cardiac death
results.
The most common cause of VF is a heart
attack. However, VF can occur whenever the
heart does not get enough oxygen or if a person
has other heart disorders.
Ventricular Fibrillation
(continued)
Conditions that can lead to VF include:
Congenital heart disease
Electrocution accidents or injury to the
heart
Heart attack
Heart muscle disease, including
Cardiomyopathy
Heart surgery
Ischemia
Sudden cardiac death typically
occurring in athletes after a trauma
over the surface of the heart
Most people with VF have no history of heart
disease. However, many have risk factors for
cardiovascular disease, such as smoking, high
blood pressure, and diabetes.
Ventricular Fibrillation
(continued)
Symptoms
A person who has a VF episode will suddenly
collapse or become unconscious, because the
brain and muscles have stopped receiving
blood from the heart.
The following symptoms may occur within 1
hour before the collapse:
Chest pain
Dizziness
Nausea
Rapid heartbeat
Shortness of breath
Treatment
External defibrillator.
Medicines may be given to control the
heartbeat and heart function.
Ventricular Flutter
Tachycardia affecting the ventricles with a rate
over 200 beats/min.
It is characterized on the ECG by a sinusoidal
waveform without clear definition of the QRS
and T waves.
It is considered transition stage between
Ventricular Tachycardia and V. Fibrillation
Critically unstable arrhythmia that can result in
sudden cardiac death.
Congenital Heart Diseases
Congenital Heart Diseases
Atrial Septal Defect
Hole in the Heart
The 3 major types of Atrial Septal defect (ASD)
Ostium secundum: The most common
type of ASD accounting for 75%
Ostium primum: The second most
common type of ASD commonly
associated with Mitral valve abnormalities.
Sinus venosus: The least common of the
three
Treatment
ASD may not require treatment if there
are few or no symptoms, or if the defect
is small.
Surgical closure of the defect is
recommended if the defect is large, the
heart is swollen, or symptoms occur.
Murmur
Widely Split, Fixed S2
Congenital heart defect in which the wall that
separates the upper heart chambers (atria)
does not close completely
ASD is not very common.
In fetal circulation, there is normally an opening
between the two atria to allow blood to bypass
the lungs. This opening usually closes around
the time the baby is born.
If the ASD is persistent, blood continues to flow
from the left to the right atria. This is called a
shunt.
If too much blood moves to the right side of the
heart, pressures in the lungs build up. The
shunt can be reversed so that blood flows from
right to left.
Small Atrial Septal defects often cause very few
problems and may be found much later in life
In advanced and severe cases with large shunts
the increased pressure on the right side of the
heart would result in reversal of blood flow (now
from right to left). This usually results in
significant shortness of breath.
When the person has no other congenital
defect, symptoms may be absent, particularly in
children. Symptoms may begin any time after
birth through childhood.
Individuals with ASD are at an increased risk for
developing a number of complications including:
Atrial fibrillation (in adults)
Heart failure
Pulmonary over-circulation
Pulmonary hypertension
Stroke
Coarctation of Aorta
Aortic coarctation is a congenital narrowing of
part of the aorta - whereby the Aorta narrows in
the area where the Ductus Arteriosus
inserts.Coarctation means narrowing.
The pulse in the femoral (groin) area or
feet will be weaker than the pulse in the
arms or the carotid (neck). Sometimes,
the femoral pulse may not be felt at all.
The blood pressure in your legs is
usually weaker than in the arms. Blood
pressure is usually higher in the arms
after infancy.
Hallmark
o Notching of the ribs
o Hypertension in the upper
extremities, and weak pulses in the
lower extremities.
Coarctation of Aorta
3 Types
Preductal Coarctation:
o The narrowing is proximal to the
ductus arteriosus..
o This is the type seen in approximately
5% of infants with Turner Syndrome.
Ductal Coarctation:
o The narrowing occurs at the insertion
of the ductus arteriosus
o Usually appears when the ductus
arteriosus closes.
Postductal Coarctation:
o The narrowing is distal to the insertion
of the ductus arteriosus.
.
o Notching of the ribs
o Hypertension in the upper
extremities, and weak pulses in the
lower extremities.
o This type is most common in adults
Patent Ductus Arteriosus
Condition where the Ductus Arteriosus (the
blood vessel joining the Pulmonary Artery to the
Aorta) fails to close after birth, causing a left to
right shunt with blood continuing to flow from
the aorta to the Pulmonary Artery.
When the Ductus Arteriosus is small, no
symptoms are present.
A Ductus Arteriosus with a moderate-to-
large left-to-right shunt may be
associated with a hoarse cry, cough,
lower respiratory tract infections,
Atelectasis, or pneumonia.
When the defect is large, CHF with
Dyspnea and poor weight gain or failure
to thrive are the main presentations.
Causes
Prematurity
Low birth weight
Prostaglandins
Maternal rubella in the first trimester of
pregnancy is thought to be a cause of the
seasonal incidence of PDA.
High altitude and low atmospheric
oxygen tension have been associated
with persistence of the PDA.
Hypoxia
Patent Ductus Arteriosus
Physical
Tachypnea
Tachycardia
Diaphoresis
Cyanosis
Bounding peripheral pulses
Wide Pulse Pressure
Clubbing
Murmur
Systolic Thrill
Continuous or Machinery Murmur is
best heard at the upper left sternal
border or left Infra-Clavicular area.
Systolic Ejection Murmur
Crescendo / Decrescendo
Occasionally, auscultation of the PDA
reveals numerous clicks or noises
resembling shaking dice or a bag of
rocks.
An apical diastolic rumble with a large left
to right shunt may be present.
Patent Ductus Arteriosus
Treatment
General measures
o Pulmonary support
o Oxygen to correct hypoxemia
o Sodium and fluid restriction
o Correction of anemia
Medical management consists of
amelioration of CHF symptoms.
No exercise restriction is required in the
absence of pulmonary hypertension.
Prophylaxis against infective
Endocarditis is recommended.
Medication
Medication use in PDA is based upon the
clinical status of the patient. Prostaglandins
are utilized to maintain the patency of the
Ductus Arteriosus until surgical ligation is
performed.
When surgical ligation is not indicated,
prostaglandin inhibitors (e.g., NSAIDs) are
used to close the Ductus Arteriosus.
Indomethacin is currently the drug of
choice for closure of the Ductus in
premature infants.
Other studies have shown equal
effectiveness with ibuprofen.
Patent Ductus Arteriosus
Pediatric surgery
Indications for surgical treatment include the
following:
Failure of Indomethacin treatment
Contraindications to medical therapy
(e.g., thrombocytopenia, renal
insufficiency)
Signs and symptoms of CHF
PDA found in an older infant.
Infants found to have an asymptomatic
PDA after the neonatal period should
undergo surgical ligation preferably
before the age of 1 year to prevent future
complications of a PDA.
Ductal closure is indicated for
cardiovascular compromise and for
reduction of the risk of Infective
Endocarditis
Contraindications to surgery include
pulmonary vascular obstructive disease.
Timing of surgery is at 1-2 years or
whenever the diagnosis is made in an
older infant.
In infants with CHF, failure to thrive,
pulmonary hypertension, or recurrent
pneumonia, the operation is more urgent
(i.e., within 3-6 months).
Tetralogy of Fallot
Congenital heart defect which is a complex
combination of four birth defects of the heart:
1. Ventricular Septal Defect,
2. Pulmonary Stenosis,
3. Overriding Aorta
4. Right Ventricular Hypertrophy.
Most Common form of Congenital
Cyanotic Heart Disease
At birth, infants may not show signs of
cyanosis.
Tet Spells - bluish skin from crying or feeding.
Factors that increase the risk for this
condition during pregnancy include:
Alcoholism in the mother
Diabetes
Mother who is over 40 years old
Poor nutrition during pregnancy
Rubella or other viral illnesses during
pregnancy
Tetralogy of Fallot
Symptoms
Clubbing of fingers
Cyanosis, which becomes more
pronounced when the baby is upset
Difficult feeding
Failure to gain weight
Passing out
Poor development
Squatting during episodes of
cyanosis
Almost always a Heart Murmur.
Treatment
Surgery is done when the infant is very young.
Corrective surgery is done to widen part of the
narrowed pulmonary tract and close the VSD
Complications
Delayed growth and development
Arrhythmias
Seizures during periods when there is
not enough oxygen
Death
There is a high incidence of chromosomal
disorders in children with Tetralogy of Fallot,
such as Down syndrome
Ventricular Septal Defect
Ventricular Septal Defect describes one or more
holes in the wall that separates the right and left
ventricles of the heart.
In utero, the right and left ventricles of the heart
are not separate. As the fetus grows, a wall
forms to separate these two ventricles. If the
wall does not completely form, a hole remains.
VSD is one of the most common congenital
heart defects.
May be asymptomatic, and the hole can
eventually close
If the hole is large, too much blood will be
pumped to the lungs, leading to heart failure.
In adults, VSD is a rare but serious complication
of heart attacks. These holes are related to
heart attacks - not a result from a birth defect.
Murmur
Pathognomonic holo- or pansystolic
murmur
Widely Split S2
Best heard over the tricuspid
area, or the lower left sternal
border, with radiation to the right
lower sternal border
Prevention
Except for the case of heart-attack-associated
VSD, this condition is always present at birth.
Drinking alcohol and using the Anti-seizure
medicines Depakote and Dilantin during
pregnancy have been associated with increased
incidence of VSDs.
Ventricular Septal Defect
Symptoms
Shortness of breath
Fast breathing
Paleness
Failure to gain weight
Fast heart rate
Sweating while feeding
Frequent respiratory infections
Treatment
If the defect is small, no treatment is
usually needed.
Babies with a large VSD who have
symptoms related to heart failure may
need medicine to control the symptoms
and surgery to close the hole.
Medications may include Digitalis
(Digoxin) and diuretics.
If symptoms continue despite medication,
surgery to close the defect w/ a Gore-Tex
patch is needed.
Surgery for a VSD with no symptoms is
controversial.
Complications
Heart failure
Infective Endocarditis
Aortic insufficiency
Damage to the electrical conduction
system of the heart during surgery
(causing arrhythmias)
Delayed growth and development
(failure to thrive in infancy)
Pulmonary hypertension leading to
failure of the right side of the heart
Congestive Heart Failure
Heart failure is a global term for the
physiological state in which cardiac output is
insufficient in meeting the needs of the body
and lungs. This occurs most commonly when
the cardiac output is low
Congestive Heart Failure
Fluid overload is a common problem for people
with heart failure but is not synonymous with it.
Patients with treated heart failure will often be
euvolaemic (a term for normal fluid status), or
more rarely, dehydrated.
Congestive Heart Failure
Heart failure (HF) is generally defined as
inability of the heart to supply sufficient blood
flow to meet the body's needs
Occurs as a result of:
Depressed cardiac contractility w/ fluid
retention & impaired cardiac output
or
Diastolic dysfunction with fluid retention
__________________________________
There are many different ways to categorize
heart failure, including:
The side of the heart involved - Left
Heart Failure versus Right Heart
Failure
Left heart failure compromises aortic
flow to the body and brain.
Right heart failure compromises
pulmonic flow to the lungs. Mixed
presentations are common, especially
when the cardiac septum is involved.
Systolic dysfunction vs. Diastolic
dysfunction - Whether the abnormality is
due to insufficient contraction and/or
relaxation of the heart
Whether the problem is primarily
increased venous back pressure (behind)
the heart Afterload, or failure to supply
adequate arterial perfusion (in front of)
the heart Preload
Congestive Heart Failure
Left-sided failure
Backward failure of the left ventricle
causes congestion of the pulmonary
vasculature, and so the symptoms are
predominantly respiratory in nature.
Backward failure can be subdivided into
failure of the left atrium, the left ventricle
or both within the left circuit. The patient
will have dyspnea on exertion, and in
severe cases, dyspnea at rest.
Increasing breathlessness on lying flat,
called orthopnea,
Paroxysmal nocturnal dyspnea
o a sudden nighttime attack of
severe breathlessness, usually
several hours after going to sleep.
Easy fatigueability and exercise
intolerance
"Cardiac asthma" or wheezing may
occur.
Chronic Non-Productive Cough
Compromise of left ventricular forward
function may result in symptoms of poor
systemic circulation such as dizziness,
confusion and cool extremities at rest.
Progresses from DOE to Orthopnea to
Dypsnea at Rest
Low cardiac output with high
systemic vascular resistance
(low-output heart failure)
vs.
High cardiac output with low vascular
resistance
(high-output heart failure)
the degree of Functional Impairment
conferred by the abnormality
Functional classification generally relies on the
N.Y. Heart Association Functional Classification
Class I: no limitation is experienced in
any activities; there are no symptoms
from ordinary activities.
Class II: slight, mild limitation of activity;
the patient is comfortable at rest or with
mild exertion.
Class III: marked limitation of any
activity; the patient is comfortable only at
rest.
Class IV: any physical activity brings on
discomfort and symptoms occur at rest.
Acute exacerbations of Chronic CHF are
caused by
Patient non-compliance to meds
Excessive salt and fluid intake
Arrhythmias
Excessive Activities
Pulmonary Embolus
Intercurrent Infection
Progression of Underlying Disease
Congestive Heart Failure
Right-sided failure
Backward failure of the right ventricle
leads to congestion of systemic
capillaries.
This generates excess fluid accumulation
in the body. This causes peripheral
edema or anasarca) and usually affects
the dependent parts of the body first -
causing foot and ankle swelling in people
who are standing up, and sacral edema
in people who are predominantly lying
down
Nocturia (frequent nighttime urination)
may occur when fluid from the legs is
returned to the bloodstream while lying
down at night.
In progressively severe cases, ascites
(fluid accumulation in the abdominal
cavity causing swelling) and
hepatomegaly (enlargement of the liver)
may develop.
Significant liver congestion may result in
impaired liver function, and jaundice and
even coagulopathy (problems of
decreased blood clotting) may occur.
Chronic Passive Congestion of the Liver
causes Anorexia and Nausea
Tachycardia
Hypotension
Reduced Pulse Pressure
Cold Extremities
Diaphoresis
Long-standing CHF causes Cachexia /
Cyanosis
Congestive Heart Failure
Common causes of heart failure include
myocardial infarction and other forms of
ischemic heart disease, hypertension, valvular
heart disease, and cardiomyopathy.
"High output cardiac failure" occurs when the
body's requirements for oxygen and nutrients
are increased and demand outstrips what the
heart can provide
High Output CHF is caused by:
Thyrotoxicosis
Sepsis
Beriberi Thiamine (B1) deficiency
Severe Anemia
AV Shunting / Malformations
Pagets disease
Systolic Dysfunction is caused by:
Myocardial Infarction
ETOH Abuse
Long-standing HTN
Viral Myocarditis, including HIV
Chagas Disease - tropical parasite
Idiopathic Dilated Cardiomyopathy
Diastolic Dysfunction is associated with:
Abnormal filling of Left Ventricle
Stiff Ventricle
Chronic HTN
LV Hypertrophy
Diabetes
Congestive Heart Failure
Physical Exam Findings
LV Failure
1. Crackles at Lung Bases
2. Pleural Effusions
3. Basilar Dullness on Percussion
4. Expiratory Wheezes and Rhonchi
5. Parasternal Lift
6. Enlarged & Sustained LV Impulse
7. Diminished First Heart Sound
8. S3 and S4 Gallop
RV Failure
1. Jugular Vein Distention
2. Abnormal Pulsations
3. Hepatic Enlargement
4. Heptojugular Reflux
5. Ascites
6. Peripheral Pitting Edema
Differential Diagnosis
COPD
Pneumonia
Cirrhosis
Peripheral Venous Insufficiency
Nephrotic Syndrome
Labs
CBC
BUN / Creatinine / LFTs / Electrolytes
TSH
BNP (B-Natriurectic Peptide)
elevation is sensitive indicator
symptomatic CHF, but may be non-
sensitive in women and older patients
Congestive Heart Failure
Left-sided failure
Common respiratory signs are tachypnea
and increased work of breathing (non-
specific signs of respiratory distress).
Rales or crackles, heard initially in the
lung bases, and when severe, throughout
the lung fields suggest the development
of pulmonary edema (fluid in the alveoli).
Cyanosis which suggests severe
hypoxemia, is a late sign of extremely
severe pulmonary edema.
Additional signs indicating left ventricular
failure include a laterally displaced apex
beat (which occurs if the heart is
enlarged)
a gallop rhythm (additional heart sounds)
may be heard as a marker of increased
blood flow, or increased intra-cardiac
pressure.
Heart murmurs may indicate the
presence of valvular heart disease, either
as a cause (e.g. aortic stenosis) or as a
result (e.g., mitral regurgitation) of the
heart failure.
Right-sided failure
Physical examination can reveal pitting
peripheral edema, ascites, and
hepatomegaly.
Jugular venous pressure is frequently
assessed as a marker of fluid status,
which can be accentuated by the
hepatojugular reflux.
If the right ventricular pressure is
increased, a parasternal heave may be
present, signifying the compensatory
increase in contraction strength.
Congestive Heart Failure
Imaging Studies
CXR
1. Cardiomegaly
2. Venous Dilation
3. Perivascular / Interstitial Edema
4. Alveolar Fluid
5. Pleural Effusion
Echocardiography
Radionuclide Angiography measures
LV Ejection Fraction
Stress Test
Left Heart Catheterization r/o Valvular
Disease, delineate extent of CAD
Right Heart Catheterization to select /
monitor pts that are refractory to Tx
Other Considerations
Salt Restriction
Restrict Activity Level only as tolerated
Monitor pts of diuretics and ACE
Inhibitors for Hypokalemia / Renal Failure
Complications
MI
Arrhythmias symptomatic /
asymptomatic, esp. V-Tach
Syncope
Sudden Death
Prevention
Control HTN
Control Lipids
Early Detection and Treatment of
Valvular Lesions
Congestive Heart Failure
Biventricular failure
Dullness of the lung fields to finger
percussion and reduced breath sounds
at the bases of the lung may suggest the
development of a pleural effusion.
Though it can occur in isolated left- or
right-sided heart failure, it is more
common in biventricular failure because
pleural veins drain both into the systemic
and pulmonary venous system.
When unilateral, effusions are often right
sided.
TREATMENT
Treatment commonly consists of lifestyle
measures, such as smoking cessation, light
exercise including breathing protocols,
decreased salt intake and other dietary
changes, and medications, and sometimes
devices or even surgery.
Medications
Diuretic + ACE Inhibitor (Lasix +
Catopril)
Aldosterone Blockers - (Aldactone)
Angiotensin Receptor Blockers
B Blockers start at low doses
Digoxin
Dobutamine has limited use for
hypoperfusion
Anticoagulation w/ A Fib or hx of MI
Rigorous HTN Control
Monitor Renal Function and K+ levels
Congestive Heart Failure
Diagnosis
Framingham criteria
By the Framingham criteria, diagnosis of
congestive heart failure (heart failure with
impaired pumping capability) requires the
simultaneous presence of at least 2 of the
following major criteria or 1 major criterion in
conjunction with 2 of the following minor criteria:
Major criteria:
Cardiomegaly on chest radiography
S3 gallop (a third heart sound)
Acute pulmonary edema
Paroxysmal nocturnal dyspnea
Crackles on lung auscultation
Central venous pressure of more than
16 cm H2O at the right atrium
Jugular vein distension
Positive abdominojugular test
Weight loss of more than 4.5 kg in 5 days
in response to treatment (sometimes
classified as a minor criterium
Minor criteria:
Tachycardia of more than 120 beats per
minute
Nocturnal cough
Dyspnea on ordinary exertion
Pleural effusion
Decrease in vital capacity by one third
from maximum recorded
Hepatomegaly
Bilateral ankle edema
Congestive Heart Failure
Surgery
Coronary Revascularization may improve
symptoms and slow progression
Bypass Surgery better that
Catheterization for Revascularization
Heart Transplant for Advanced CHF
Implantable Defibrillators to guard
against syncope / sudden death
Prognosis
Poor 5% mortality in Stable pts, 30-
50% mortality w/ advanced
50% of Hospitalized Pts will be
readmitted within one year
Transplant Pt - 1 year survival rate 90%,
5 year survival rate 70%
Congestive Heart Failure
Left Ventricular Failure
1. Exertional Dypsnea
2. Cough
3. Fatigue
4. Orthopnea
5. Paroxysmal Nocturnal Dypsnea
6. Cardiac Enlargement
7. Rales
8. Gallop Rhythm
9. Pulmonary Venous Congestion
Right Ventricular Failure
1. Elevated Venous Pressure
2. Hepatomegaly
3. Dependent Edema
4. Usually due to LV Failure
Hypertension
Essential / Secondary / Malignant
Hypertension
Essential / Secondary / Malignant
Essential
Hypertension
Classification Systolic Diastolic
Normal 90119 6079
Prehypertension 120139 8189
Stage 1 HTN 140159 9099
Stage 2 HTN 160 100
Persistently high blood pressures requiring:
3 separate measurements, 1 week apart
Essential Hypertension
no identifiable cause
aka
Primary or Idiopathic HTN
Most common type of hypertension, affecting
95% of hypertensive patients
Tends to be familial and is likely to be the
consequence of an interaction between
environmental and genetic factors.
Prevalence of essential hypertension increases
with age
Individuals with relatively high blood pressures
at younger ages are at increased risk for the
subsequent development of hypertension.
Secondary Hypertension
Refers to high blood pressure caused
by another medical condition
or medication
___________ __________
Secondary hypertension may be due to:
Alcohol abuse
Renal artery stenosis - narrowing of
Renal Arteries can cause severe
hypertension & irreversible kidney damage.
Pregnancy. Pregnancy can make
existing high blood pressure worse, or
may cause high blood pressure
Pre-Eclampsia - Pregnancy-induced
HTN
Atherosclerosis
Autoimmune Disorders
Periarteritis Nodosa
Chronic kidney disease
Coarctation of the aorta - forces the
heart to pump harder to get blood
through the aorta and to the rest of the
body, thus raises blood pressure
particularly the upper extremities
Cocaine use
Diabetes (if it causes kidney damage)
Endocrine Disorders
Adrenal tumors
Pheochromocytoma
Thyroid disorders
Cushing's syndrome. In this
condition, corticosteroid
medications, a pituitary tumor or
other factors cause the adrenal
glands to produce too much of the
hormone cortisol. This raises
blood pressure.
Secondary Hypertension
Secondary hypertension may be due to:
Diabetic nephropathy - Diabetes can damage
the kidneys' filtering system
Polycystic kidney disease genetic condition
forming renal cysts that prevent the kidneys from
working normally, and can raise blood pressure.
Glomerular Disease - Renal Glomeruli filter
waste and sodium become swollen and can't
work normally, raising blood pressure.
Pheochromocytoma. This rare tumor, usually
found in an adrenal gland, increases production
of the hormones adrenaline and noradrenalin,
which can lead to long-term high blood pressure
or short-term spikes in blood pressure.
Hyperparathyroidism. The parathyroid glands
regulate levels of calcium and phosphorus in
your body. If the glands secrete too much
parathyroid hormone, the amount of serum
calcium rises, & triggers a rise in blood pressure.
Sleep apnea Hypoxia may damage the lining
of the blood vessel walls making blood vessels
less effective in regulating blood pressure. Also
sleep apnea causes part of the nervous system
to be overactive and release certain chemicals
that increase blood pressure.
Obesity with weight gain, the amount of
circulating blood increases putting added
pressure on arterial walls, increasing blood
pressure. Excess weight often is associated with
an increase in heart rate and a reduction in the
capacity of blood vessels to transport blood.
Medications
Appetite suppressants
Birth control pills
Certain cold medications
Corticosteroids
Migraine medications
Aldosteronism. In this condition,
a tumor in the adrenal gland,
increased growth of normal cells
in the adrenal gland or other
factors cause the adrenal glands
to release an excessive amount of
the hormone Aldosterone
causing the kidneys to retain salt
and water and lose too much
potassium, which raises blood
pressure.
Medications and supplements. Various
prescription medications from pain
relievers to antidepressants and drugs used
after organ transplants can cause or
aggravate high blood pressure in some
people. Birth control pills, decongestants
and certain herbal supplements, including
ginseng and St. John's wort, may have the
same effect. Many illegal drugs, such as
cocaine and methamphetamine, also
increase blood pressure.
Malignant
Hypertension
Malignant hypertension is a sudden and rapid
development of extremely high blood pressure.
The lower (diastolic) blood pressure reading,
which is normally around 80 mmHg, is often
above 130 mmHg.
To diagnose Malignant Hypertension,
Papilledema must be present.
Causes
The disorder affects about 1% of people
with high blood pressure, including both
children and adults.
It is more common in younger adults,
especially African American men. It also
occurs in women with toxemia of
pregnancy, and persons with kidney
disorders or collagen vascular disorders.
You are at high risk for malignant
hypertension if you have had kidney
failure or renal hypertension caused by
renal artery stenosis.
Malignant hypertension is a medical
emergency.
Malignant
Hypertension
Tests to determine damage to the kidneys:
BUN
Creatinine
Arterial blood gas analysis
Urinalysis
CXR:
Lung congestion
Rnlarged heart.
This disease may also alter
Aldosterone
Cardiac enzymes
EKG
Renin
Urinary casts (sediment)
Treatment
Patients with malignant hypertension usually
are admitted to an intensive care unit for
continuous cardiac monitoring and frequent
assessment of Neurologic status and urine
output.
Intravenous medications are the main focus of
therapy. - Nitroprusside and Nitroglycerin.
A number of blood tests will also be checked,
probably several times, to assess the status of
the kidneys and other organs.
Malignant Hypertension
Symptoms
Abnormal sensation (numbness) of the
arms, legs, face, or other areas
Blurred vision
Change in mental status
o Restlessness
o Anxiety
o Decreased alertness, decreased
ability to concentrate
o Fatigue
o Sleepiness, stuporous, lethargic
o Confusion
Chest pain
o Mid-chest location most common
o Crushing or pressure sensation
Cough
Decreased urinary output
Headache
Nausea or vomiting
Seizure
Shortness of breath
Weakness of the arms, legs, face, or
other areas
Exams and Tests
A physical exam commonly shows:
Extremely high blood pressure
Possible swelling in the lower legs and
feet
Abnormal heart sounds and fluid in the
lungs
Changes in mental status, sensation,
muscle ability, and reflexes
An eye examination will reveal changes that
indicate high blood pressure:
Swelling of the optic nerve,
Retinal bleeding,
Narrowing of the blood vessels in the eye
area,
other problems with the Retina.
Kidney Failure may develop as a
complication of malignant hypertension.
Other complications may also develop.
Malignant Hypertension
Outlook (Prognosis)
After leaving the hospital, it is common for
patients prescribed medicines like beta blockers
or ACE inhibitors to keep the blood pressure
under control in the future.
Many body systems are in serious risk due to
the extreme rise in blood pressure. Multiple
organs of the body, including the brain, eyes,
blood vessels, heart, and kidneys may be
damaged. The blood vessels of the kidney are
highly susceptible to damage caused by
pressure, and kidney failure may develop, which
may be permanent, requiring dialysis (kidney
machine).
If treated promptly, malignant hypertension is
often controlled without permanent
complications. If it is not treated promptly,
complications may be severe and life-
threatening.
Possible Complications
Brain damage due to:
o Coma
o Hypertensive encephalopathy
o Intracerebral hemorrhage
(bleeding in the brain)
o Seizures
o Spasm or constriction of the
arteries of the brain
o Stroke
o Swelling
Heart damage, including:
o Heart attack
o Angina (chest pain due to
narrowed blood vessels or
weakened heart muscle)
o Heart rhythm disturbances
Kidney failure
Permanent blindness
Pulmonary edema
Hypotension
Abnormally low blood pressure.
This is best understood as a physiologic state,
rather than a disease.
Often associated with shock, though not
necessarily indicative of it.
Hypotension is generally considered as systolic
blood pressure less than 90 mm Hg or diastolic
less than 60 mm Hg
Three main types:
1. Orthostatic Hypotension, including
Postprandial Orthostatic
Hypotension
2. Neurally Mediated Hypotension
(NMH)
3. Severe hypotension brought on by a
sudden loss of blood (shock)
_________________________________
Orthostatic hypotension is brought on by
a sudden change in body position,
usually when shifting from lying down to
standing - lasts only a few seconds or
minutes.
After eating, its called Postprandial
Orthostatic Hypotension - commonly
affects elderly, those with high blood
pressure, & persons w/ Parkinson's
disease.
NMH most often affects young adults and
children. It occurs when a person has
been standing for a long time. Children
usually outgrow this type of hypotension.
Hypotension
The cardinal symptom of hypotension is
lightheadedness or dizziness.
If the blood pressure is sufficiently low,
fainting and often seizures will occur.
Symptoms may include:
Blurry vision
Confusion
Dizziness
Fainting (syncope)
Light-headedness
Sleepiness
Weakness
Treatment
The treatment for hypotension depends on its
cause. Chronic hypotension rarely exists as
more than a symptom. Asymptomatic
hypotension in healthy people usually does not
require treatment. Adding electrolytes to a diet
can relieve symptoms of mild hypotension. In
mild cases, where the patient is still responsive,
laying the person in dorsal decubitus (lying on
the back) position and lifting the legs will
increase venous return, thus making more
blood available to critical organs at the chest
and head. The Trendelenburg position, though
used historically, is no longer recommended.
[6]
The treatment of hypotensive shock always
follows the first four following steps. Outcomes,
in terms of mortality, are directly linked to the
speed in which hypotension is corrected. In
parentheses are the still debated methods for
achieving, and benchmarks for evaluating,
progress in correcting hypotension. A study on
Early Goal Directed Therapy provided the
delineation of these general principles.
However, since it focuses on hypotension due
to infection, it is not applicable to all forms of
severe hypotension
Hypotension
Low blood pressure is commonly caused by
drugs such as:
Alcohol
Anti-anxiety medications
Antidepressants
Diuretics
HTN and CAD Meds
Medications used for surgery
Painkillers
Other causes:
Advanced diabetes
Dehydration / Hypovolemia
Anaphylaxis
Arrhythmias
Dehydration
Fainting
Heart attack
Heart failure
Shock (from severe infection,
stroke, anaphylaxis, major trauma,
or heart attack)
_________________________________
Expectations (prognosis)
Low blood pressure can usually be treated with
success.
Prevention
If you have low blood pressure, your doctor may
recommend certain steps to prevent or reduce
your symptoms. This may include:
Avoiding alcohol
Avoiding standing for a long time (if
you have NMH)
Drinking plenty of fluids
Getting up slowly after sitting or lying
down
Using compression stockings to
increase blood pressure in the legs
Hypotension
Treatment (Continued)
1. Volume resuscitation - Crystalloid
2. Blood pressure support -
Norepinephrine or equivalent
3. Ensure adequate tissue perfusion -
maintain SvO2 >70 with use of Blood or
Dobutamine
4. Address the underlying problem (i.e.
antibiotic for infection, stent or CABG for
infarction, steroids for adrenal
insufficiency
Blood sugar control (80-150 by one
study)
Early nutrition (by mouth or by tube to
prevent ileus)
Steroid support
Hypotension in a healthy person that
does not cause any problems usually
doesn't require treatment.
Treatment depends on the cause of low
blood pressure.
Severe hypotension caused by shock is
a medical emergency.
Orthostatic hypotension caused by
medicines, change the dose or switch to
a different drug
Increasing fluids to treat dehydration
Wearing elastic hose to boost blood
pressure in the lower part of the body.
Those with NMH should avoid triggers,
such as standing for a long periods
In severe cases, Fludrocortisone.
Cardiogenic Shock
Cardiogenic shock is based upon an
inadequate circulation of blood due to
primary failure of the ventricles of the
heart to function effectively.
Insufficient perfusion of tissue leading to
cell death from oxygen starvation
1. Hypoxia
2. Hypoglycemia - (Nutrient
starvation)
May lead to cardiac arrest
Definition - sustained hypotension with
tissue hypoperfusion despite adequate
left ventricular filling pressure.
Signs of tissue Hypoperfusion
1. Oliguria (<30 mL/h)
2. Cool Extremities
3. Altered Mental Status
Etiology
Cardiogenic shock is caused by the
failure of the heart to pump effectively.
It can be due to damage to the heart
muscle, most often from a large
myocardial infarction.
Other causes:
1. Arrhythmia
2. Cardiomyopathy
3. Ventricular outflow obstruction
(eg. Aortic Stenosis)
4. Aortic dissection
5. Hypertrophic Cardiomyopathy
6. Systolic Anterior Motion (SAM)
7. Ventriculoseptal defects.
Cardiogenic Shock
Diagnosis
Electrocardiogram
An electrocardiogram helps establishing
the exact diagnosis and guides
treatment, it may reveal:
1. Cardiac arrhythmias
2. Signs of Cardiomyopathy
Ultrasound
Echocardiography may show poor
ventricular function, signs of PED,
ventricular septal rupture (VSR), an
obstructed outflow tract or
cardiomyopathy.
Swan-ganz catheter
The Swan-ganz catheter or pulmonary
artery catheter may assist in the
diagnosis by providing information on the
hemodynamics.
Biopsy
In case of suspected cardiomyopathy a
biopsy of heart muscle may be needed to
make a definite diagnosis. but biopsy
should only be done when third space is
suspected
Cardiogenic Shock
Signs and Symptoms
Anxiety, restlessness, altered mental
status due to decreased cerebral
perfusion and subsequent hypoxia.
Hypotension due to decrease in cardiac
output.
A rapid, weak, thready pulse due to
decreased circulation combined with
tachycardia.
Cool, clammy, and mottled skin (cutis
marmorata), due to vasoconstriction and
subsequent hypoperfusion of the skin.
Distended jugular veins due to increased
jugular venous pressure.
Oliguria (low urine output) due to
insufficient renal perfusion if condition
persists.
Rapid and deep respirations
(hyperventilation) due to sympathetic
nervous system stimulation and acidosis.
Fatigue due to hyperventilation and
hypoxia.
Absent pulse in tachyarrhythmia.
Pulmonary edema, involving fluid back-
up in the lungs due to insufficient
pumping of the heart..
Cardiogenic Shock
Treatment
Fluid Infusion
IV Dobutamine, which acts on
1
receptors of the heart leading to
increased contractility and heart rate.
Anti-arrhythmic agents
1. Adenosine
2. Verapamil
3. Amiodarone
4. -blocker
Glucagon
Positive inotropic agents, which
enhance the heart's pumping
capabilities, are used to improve the
contractility and correct the
hypotension
Intra-aortic balloon pump (which
reduces workload for the heart, and
improves perfusion of the coronary
arteries)
Left Ventricular Assist Device (which
augments the pump-function of the
heart).
Orthostatic / Postural
Hypotension
Blood pressure suddenly falls when the
person stands up.
Decrease is typically greater than 20/10 mm
Hg
May be most pronounced after resting
incidence increases with age.
Signs and Symptoms
Symptoms occur after sudden standing
Consequences of insufficient blood pressure
and cerebral perfusion.
Dizziness
Euphoria or Dysphoria
Bodily dissociation
Distortions in hearing
Lightheadedness
Nausea
Headache
Blurred or dimmed vision
Momentary Blindness)
Numbness/tingling and fainting
Coat hanger pain (neck / shoulders)
Vasovagal syncope
Diagnosis
Lying, Sitting, Standing BP / HR
measurements.
Tilt table test
Orthostatic Hypotension
Causes of Orthostatic Hypotension
Orthostatic hypotension is primarily
caused by gravity-induced blood pooling
in the lower extremities, which in turn
compromises venous return, resulting in
decreased cardiac output and
subsequent lowering of arterial pressure
The overall effect is an insufficient blood
perfusion in the upper part of the body.
Still, the blood pressure does not
normally fall very much, because it
immediately triggers a vasoconstriction
(baroreceptor reflex), pressing the blood
up into the body again.
Therefore, a secondary factor that
causes a greater than normal fall in blood
pressure is often the pathology.
Such factors include hypovolemia,
diseases, medications, rarely, safety
harnesses
Heat exhaustion can also be a cause of
postural hypotension.
Hypovolemia
1. Blood Lose
2. Diuretics
3. Vasodilators
4. Other drugs
5. Dehydration
6. Prolonged bed rest
7. Anemia.
Orthostatic Hypotension
Management
Medical
Fludrocortisone (Florinef) and
Erythropoietin to aid in fluid retention
Vasoconstrictors like Midodrine.
Pyridostigmine bromide (Mestinon)
Selective serotonin reuptake inhibitors
(SSRI's)
Serotonin-Norepinephrine reuptake
inhibitors (SNRI's)
Stimulants - Adderall or Ritalin
Benzodiazepines
Lifestyle factors
Standing up more slowly can give the
blood vessels more time to constrict
properly. This can help avoid incidents of
syncope (fainting).
Breathing deeply and flexing the
abdominal muscles while rising
(contraindicated in individuals with Stage
2 hypertension)
"Dangle" legs before rising from bed
Sodium supplements or electrolyte-
enriched drinks
Maintaining proper fluid intake.
Eating more, smaller meals can help, as
digestion lowers blood pressure
Take extra care when standing after
eating.
hypovolemia due to medications may be
reversed by adjusting the dosage or by
discontinuing the medication.
Orthostatic Hypotension
Diseases associated with OH
1. Addison's disease
2. Atherosclerosis Diabetes
3. Pheochromocytoma
4. Neurological disorders
5. Multiple system atrophy
6. Dysautonomia
7. Ehlers-Danlos Syndrome (genetic
mutations disrupt the production of collagen, a
chief component of connective tissue)
8. Parkinson's Disease resulting from
sympathetic denervation of the heart or
as a side effect of dopaminomimetic
therapy
9. Low level of norepinephrine but an
excess of dopamine
10. Quadriplegics / Paraplegics due to
multiple system inability to maintain a
normal blood pressure and blood flow to
the upper part of the body
11. Cerebrospinal fluid leakage
12. Inner ear problems, esp w/ elderly
Medication side effect:
Anti-depressants
1. Tricyclics
2. MAOIs
Anti-psychotics
Alpha
1
adrenergic blocking agents -
inhibition of vasoconstriction normally
initiated by the baroreceptor reflex upon
postural change and the subsequent
drop in pressure
Orthostatic Hypotension
Management (Continued)
When the condition is caused by
prolonged bed rest, improvement may
occur by sitting up with increasing
frequency each day. In some cases,
physical counterpressure such as elastic
hose (stockings) or whole-body inflatable
suits may be required.
Ability to recognize the symptoms and
quickly adopt a "squat position"
Avoiding bodily positions that impede
blood flow, such as sitting with knees up
to chest or crossing legs, can help
prevent incidents.
Orthostatic Hypotension
Harnesses
The use of a safety harness can also
contribute to orthostatic hypotension in
the event of a fall. While a harness may
safely rescue its user from a fall, the leg
loops of a standard safety or climbing
harness further restrict return blood flow
from the legs to the heart, contributing to
the decrease in blood pressure.
Other risk factors
Postpartum mothers
Bedrest
Teenagers because of their large
amounts of growth in a short period of
time
Anorexia Nervosa
Bulimia Nervosa
Alcohol consumption - (dehydrating
effects)
Ischemic Heart Disease
Acute Myocardial Infarction
Most commonly due to occlusion of a
coronary artery following the rupture of a
vulnerable atherosclerotic plaque
causing damage or death of myocardium
Classical symptoms sudden chest pain
typically radiating to the left arm or left
side of the neck shortness of breath,
nausea, vomiting, indigestion, and
fatigue, palpitations, sweating, and
anxiety
Approximately one quarter of all
myocardial infarctions are "silent",
without chest pain or other symptoms.
Among the diagnostic tests available to
detect heart muscle damage are an
electrocardiogram (ECG),
echocardiography, and various blood
tests - creatine kinase-MB (CK-MB)
fraction and the troponin levels
Immediate treatment for suspected acute
myocardial infarction includes oxygen,
aspirin, and sublingual nitroglycerin.
Can be classified into:
ST Elevation MI (STEMI)
versus
Non-ST Elevation MI - (NSTEMI)
STEMI (ST elevation MI) are treated with
Thrombolysis or Percutaneous Coronary
Intervention (PCI).
NSTEMI (non-ST elevation MI) should be
managed with medication, although PCI
is often performed during hospital
admission. In people who have multiple
blockages and who are relatively stable
Acute Myocardial Infarction
Signs and Symptoms
Onset of symptoms is usually gradual,
over several minutes, and rarely
instantaneous.
Chest pain is the most common symptom
and is often described as a sensation of
Tightness, Pressure, or Squeezing.
Chest pain due to ischemia is termed
angina pectoris.
Pain radiates most often to the left arm,
but may also radiate to the lower jaw,
neck, right arm, back, and epigastrium,
It may mimic heartburn.
Levine's sign, patient localizes the chest
pain by clenching their fist over the
sternum,
Shortness of breath (dyspnea) occurs
when the damage to the heart limits the
output of the left ventricle, causing left
ventricular failure and consequent
pulmonary edema.
Symptoms induced by a massive surge
of catecholamines from the sympathetic
nervous system
1. Diaphoresis
2. Weakness
3. Light-headedness
4. Nausea, Vomiting
5. Palpitations.
Loss of consciousness - due to
inadequate cerebral perfusion and
cardiogenic shock
Sudden Death - frequently due to the
development of ventricular fibrillation
Acute Myocardial Infarction
Risk factors:
Cardiovascular disease
Older age
Smoking
High Triglycerides and LDL
Low levels of HDL
Diabetes, HTN
Obesity
Chronic kidney disease
Heart failure
Excessive alcohol consumption
Cocaine and Methamphetamine
High stress levels
There are two basic types of acute myocardial
infarction:
Transmural: associated with
atherosclerosis involving major coronary
artery. It can be subclassified into
anterior, posterior, or inferior. Transmural
infarcts extend through the whole
thickness of the heart muscle and are
usually a result of complete occlusion of
the area's blood supply.
Subendocardial: involving a small area
in the subendocardial wall of the left
ventricle, ventricular septum, or papillary
muscles. Subendocardial infarcts are
thought to be a result of locally
decreased blood supply, possibly from a
narrowing of the coronary arteries. The
subendocardial area is farthest from the
heart's blood supply and is more
susceptible to this type of pathology
Acute Myocardial Infarction
Heparin given to people who have heart
conditions like unstable angina and some forms
of heart attack reduces the risk of having
another heart attack.
An MI is a medical emergency which requires
immediate medical attention. Treatment
attempts to salvage as much myocardium as
possible and to prevent further complications,
thus the phrase "time is muscle".
Oxygen, aspirin, and nitroglycerin may be
administered. Morphine was classically used if
nitroglycerin was not effective; however, it may
increase mortality in the setting of NSTEMI
A 2009 and 2010 review of high flow oxygen in
myocardial infarction found increased mortality
and infarct size, calling into question the
recommendation about its routine use
Percutaneous coronary intervention (PCI) or
fibrinolysis are recommended in those with an
STEMI.
Bypass surgery may be an option.
The leading cause of death for both men and
women worldwide.
Acute Myocardial Infarction
Five main types:
Type 1 Spontaneous myocardial
infarction related to ischaemia due to a
primary coronary event such as plaque
erosion and/or rupture, fissuring, or
dissection
Type 2 Myocardial infarction secondary
to ischaemia due to either increased
oxygen demand or decreased supply,
e.g. coronary artery spasm, coronary
embolism, anaemia, arrhythmias,
hypertension, or hypotension
Type 3 Sudden unexpected cardiac
death, including cardiac arrest, often with
symptoms suggestive of myocardial
ischaemia, accompanied by presumably
new ST elevation, or new LBBB, or
evidence of fresh thrombus in a coronary
artery by angiography and/or at autopsy,
but death occurring before blood
samples could be obtained, or at a time
before the appearance of cardiac
biomarkers in the blood
Type 4 Associated with coronary
angioplasty or stents:
Type 5 Myocardial infarction
associated with CABG
Causes
Heart attack rates are higher in association with
intense exertion, be it psychological stress or
physical exertion
Acute severe infection, such as pneumonia, can
trigger MI
There is an association of an increased
incidence of a heart attack in the morning hours
Acute Myocardial Infarction
Pathophysiology
Lethal arrhythmias: The most serious of these
arrhythmias is ventricular fibrillation (V-Fib/VF
ventricular tachycardia (V-Tach/VT), which may
or may not cause sudden cardiac death.
Ventricular tachycardia usually results in rapid
heart rates that prevent the heart from pumping
blood effectively. Cardiac output and blood
pressure may fall to dangerous levels, which
can lead to further coronary ischemia and
extension of the infarct.
W.H.O. Criteria fo MI:
Two = Probable MI
Three = Definite MI
1. Clinical history of ischemic type chest
pain lasting for more than 20 minutes
2. Changes in serial ECG tracings
3. Rise and fall of serum cardiac
biomarkers such as creatine kinase-MB
fraction and troponin
The WHO criteria were refined in 2000 to give
more prominence to cardiac biomarkers
According to the new guidelines, a cardiac
troponin rise accompanied by either typical
symptoms, pathological Q waves, ST elevation
or depression or coronary intervention are
diagnostic of MI.
Acute Myocardial Infarction
Risk factors
Risk factors for atherosclerosis are generally
risk factors for myocardial infarction:
Diabetes - most important risk factor
Tobacco smoking
Hypercholesterolemia
Hyperlipidemia - High LDL
Low HDL
High Triglycerides
High blood pressure
Family History
Obesity- BMI of more than 30 kg/m
Age: Men age 45, Women age 55
First-degree male relative who suffered a
coronary vascular event at or before age
55 - First-degree female relative who
suffered a coronary vascular event
before age 65
Hyperhomocysteinemia - High
Homocysteine, a toxic blood amino acid
that is elevated when intakes of vitamins
B
2
, B
6
, B
12
and folic acid are insufficient
Stress
Alcohol
Socioeconomic factors such as a shorter
education, lower income, unmarried
cohabitation may also contribute to the
risk of MI.
Women who use combined oral
contraceptive pills, especially in the
presence of other risk factors, such as
smoking
Acute Myocardial Infarction
Risk Decreases:
Lifestyle changes
BP Management
Smoking cessation
Regular exercise
Sensible diet
Limitation of alcohol intake
To reduce the risk of future MIs, CHF, or CVA
Polyunsaturated fats instead of saturated
fats
Antiplatelet drug therapy:
o Aspirin
o Clopidogrel
Beta blocker - Metoprolol or Carvedilol -
- beneficial in high-risk patients with left
ventricular dysfunction and/or continuing
cardiac ischaemia.
-Blockers decrease mortality and
morbidity.
-Blockers improve symptoms of cardiac
ischemia in NSTEMI.
ACE inhibitor therapy should be
commenced 2448 hours post-MI in
hemodynamically-stable patients,
ACE inhibitors reduce mortality, the
development of heart failure, and
decrease ventricular remodeling post-MI.
Statin therapy has been shown to reduce
mortality and morbidity post-MI.
Acute Myocardial Infarction
Risk Factors - continued
Inflammation is known to be an important
step in the process of atherosclerotic
plaque formation. C-reactive protein
(CRP) is a sensitive but non-specific
marker for inflammation.
Elevated CRP blood levels, especially
measured with high sensitivity assays,
can predict the risk of MI,
Influenza may trigger a acute myocardial
infarction
Calcium deposition is another part of
atherosclerotic plaque formation.
Calcium deposits in the coronary arteries
can be detected with CT scans.
Acute Myocardial Infarction
Risk Decreases - continued
The aldosterone antagonist agent
Spironolactone has been shown to
further reduce risk of cardiovascular
death post-MI in patients with heart
failure and left ventricular dysfunction,
Omega-3 fatty acids,
Blood donation may reduce the risk of
heart disease
Angina Pectoris
Chest pain or discomfort seen in
myocardial ischemia - Coronary arteries
are narrowed or blocked.
Angina is a sign that someone is at
increased risk of heart attack, cardiac
arrest and sudden cardiac death.
Angina pectoris is the most common
clinical manifestation of myocardial
ischemia.
Pain lasts for approximately 1-5 minutes
relieved by rest, or nitroglycerin.
Angina also can occur in people with
Valvular heart disease, Hypertrophic
Cardiomyopathy, and uncontrolled HTN
Myocardial ischemia develops when
coronary blood flow becomes inadequate
to meet myocardial oxygen demand.
This causes myocardial cells to switch
from aerobic to anaerobic metabolism,
with a progressive impairment of
metabolic, mechanical, and electrical
functions.
Adenosine induces angina mainly by
stimulating the A1 receptors in cardiac
afferent nerve endings
Most patients with angina pectoris report
of Retrosternal chest discomfort rather
than frank pain
Usually described as a pressure,
heaviness squeezing, burning, or
choking sensation.
Anginal pain may be localized primarily in
the epigastrium, back, neck, jaw, or
shoulders.
Typical locations for radiation of pain are
arms, shoulders, and neck.
Angina Pectoris
Physical
For most patients with stable angina,
physical examination findings are normal.
Diagnosing secondary causes of angina,
such as aortic stenosis, is important.
A positive Levine Sign (characterized by
the patient's fist clenched over the
sternum when describing the discomfort)
is suggestive of angina pectoris.
Pain produced by chest wall pressure is
usually of chest wall origin NOT Angina
Causes
Decrease in myocardial blood supply due
to increased coronary resistance in large
and small coronary arteries
Coronary atherosclerotic lesion in the
large coronary arteries with at least a
50% reduction in arterial diameter
Coronary spasm - Prinzmetals Angina
Abnormal constriction or deficient
endothelial-dependent relaxation of
resistant vessels associated with diffuse
vascular disease (ie, Micro-vascular
Angina)
Syndrome X - Aka - metabolic syndrome
Xis a grouping of cardiac risk factors that
result from insulin resistance
Systemic Inflammatory / Collagen
Vascular Disease
1. Scleroderma
2. Systemic Lupus Erythematous
3. Kawasaki Disease
4. Polyarteritis Nodosa
5. Takayasu Arteritis
Reduction in the oxygen-carrying
capacity of blood, such as elevated
Carboxyhemoglobin or Severe Anemia
(Hemoglobin, <8 g/dL)
Angina Pectoris
Typically, angina is precipitated by
exertion, eating, exposure to cold, or to
emotional stress.
Chest pain lasting only a few seconds is
not usually angina pectoris.
The intensity of angina does not change
with respiration, cough, or change in
position.
Pain above the mandible and below the
epigastrium is rarely anginal in nature.
Angina Decubitus is a variant of angina
pectoris that occurs at night while the
patient is recumbent..
Angina Pectoris
Risk Factors:
1. Risk factors for Atherosclerosis:
2. LV Hypertrophy
3. Obesity
4. Elevated serum levels of
5. Homocysteine
6. Lipoprotein
7. Plasminogen Activator Inhibitor
8. Fibrinogen
9. Serum Triglycerides
10. Low HDL
Precipitating Factors:
1. Severe Anemia
2. Fever
3. Tachy-arrhythmia
4. Catecholamines
5. Emotional Stress
6. Hyperthyroidism
Stable
Ischemic Heart Disease
People with stable angina (or chronic
stable angina) have episodes of chest
discomfort that are usually predictable.
They occur on exertion (such as running
to catch a bus) or under mental or
emotional stress.
Normally the chest discomfort is relieved
with rest, nitroglycerin or both.
Also known as effort angina, this refers to
the more common understanding of
angina related to myocardial ischemia.
Stable
Ischemic Heart Disease
Typical presentations of stable angina is
that of chest discomfort and associated
symptoms precipitated by some activity
(running, walking, etc.) with minimal or
non-existent symptoms at rest.
Symptoms typically abate several
minutes following cessation of
precipitating activities and resume when
activity resumes. In this way, stable
angina may be thought of as being
similar to claudication symptoms
Unstable
Ischemic Heart Disease
In people with unstable angina, the chest
pain is unexpected and usually occurs
while at rest.
The discomfort may be more severe and
prolonged than typical angina or be the
first time a person has angina.
The most common cause is reduced
blood flow to the heart muscle because
the coronary arteries are narrowed
by fatty buildups (atherosclerosis)
.
An artery may be abnormally constricted
or partially blocked by a blood clot.
Inflammation, infection and secondary
causes also can lead to unstable angina.
In a form of unstable angina called
variant or Prinzmetal's angina, the cause
is coronary artery spasm.
Definition:
Unstable
Ischemic Heart Disease
is
Angina Pectoris that changes or worsens
Unstable
Ischemic Heart Disease
Aka - "Crescendo Angina;"
It has at least one of these three features:
1. it occurs at rest (or with minimal
exertion), usually lasting >10 min;
2. it is severe and of new onset (i.e.,
within the prior 46 weeks)
3. it occurs with a crescendo pattern
(i.e., distinctly more severe,
prolonged, or frequent than
previously).
____________ ___________
UA may occur unpredictably at rest
which may be a serious indicator of an
impending heart attack.
Studies show that 64% of all Unstable
Anginas occur between 10 PM and 8 AM
when patients are at rest.
In stable angina, the developing
atheroma is protected with a fibrous cap.
This cap (atherosclerotic plaque) may
rupture in unstable angina, allowing
blood clots to precipitate and further
decrease the lumen of the coronary
vessel.
This explains why an unstable angina
appears to be independent of activity.
Prinzmetals / Variant
Variant Angina Pectoris
is also called
Prinzmetal's Angina
___________________________
Is caused by Vasospasm
Unlike typical angina, it nearly always
occurs when a person is at rest.
It usually occurs spontaneously
It doesn't follow physical exertion or
emotional stress, either. Attacks can be
very painful and usually occur between
midnight and 8 a.m.
Prinzmetals Variant angina is due to
Transient Coronary Artery Spasm.
About two-thirds of people with it have
severe coronary atherosclerosis in at
least one major vessel.
The spasm usually occurs very close to
the blockage.
Prinzmetals / Variant
Diagnosis
Echocardiography or thallium
scintigraphy is often performed.
The Gold Standard is Coronary
Angiography with injection of
provocative agents into the coronary
artery.
Provocation testing agents:
1. Ergonovine
2. Methylergonovine
3. Acetylcholine.
Exaggerated spasm is diagnostic of
Prinzmetal angina.
ECG finding will more often show ST
segment elevation than ST depression.
Elevation ST-segment in II, III and aVf.
Treatment
Prinzmetal's angina typically responds to:
1. Nitrates
2. Calcium Channel Blockers.
Amlodipine - (Norvasc, Lotrel)
Bepridil - (Vascor)
Diltiazem - (Cardizem, Tiazac)
Felodipine - (Plendil)
Nifedipine - (Adalat, Procardia)
Nimodipine - (Nimotop)
Nisoldipine - (Sular) and
Verapamil - (Calan, Isoptin, Verelan)
Takayasu's Arteritis
Aka:
1. Aortic Arch Syndrome
2. Nonspecific Aorto-arteritis
3. Pulseless Disease
A form of large vessel granulomatous
vasculitis
[
with massive intimal fibrosis
and vascular narrowing
Young or middle-aged women of Asian
decent.
Mainly affects the aorta and its branches
and the pulmonary arteries.
Females more than males - between 15
and 30 years of age.
Takayasu's Arteritis
In the US - atherosclerosis is a more
frequent cause of obstruction of the
aortic arch
vessels than Takayasu's arteritis.
Takayasu's arteritis is similar to other
forms of vasculitis, including giant cell
arteritis.
Due to obstruction of the main branches
of the aorta, including the left common
carotid artery, the brachiocephalic artery,
and the left subclavian artery,
Takayasu's arteritis can present as
pulseless , absent pulses in the upper
extremities - Pulseless Disease
Vascular Disease
This refers to diseases of blood vessels
outside the heart and brain.
It's often a narrowing of vessels that
carry blood to the legs, arms, stomach or
kidneys.
There are two types of these circulation
disorders:
1. Functional Peripheral Vascular
Disease
2. Organic Peripheral Vascular
Disease
Vascular Disease
Functional Peripheral Vascular Disease
1. Do not have an organic cause
2. Do not involve defects structural
vasculature
3. Usually short-term effects related to
"spasm" that may come and go.
4. Reynauds Disease is an example. It
can be triggered by cold
temperatures, emotional stress,
working with vibrating machinery or
smoking.
Organic Peripheral Vascular Disease
1. Caused by structural changes in the
blood vessels, such as inflammation
and tissue damage
2. Peripheral artery disease is an
example. It's caused by fatty buildups
in arteries that block normal blood
flow.
Acute Rheumatic Fever
An inflammatory disease that occurs
following a Group A streptococcal
infection such as strep throat or scarlet
fever
Involves the heart, joints, skin, and brain
Typically develops two to three weeks
after a Streptococcal A infection
Acute rheumatic fever commonly
appears in children between the ages of
5 and 17, with only 20% of first-time
attacks occurring in adults
The illness is so named because of its
similarity in presentation to rheumatism
Prevention of recurrence is achieved by
eradicating the acute infection and
prophylaxis with antibiotics.
The American Heart Association
recommends daily or monthly
prophylaxis continue long-term,
perhaps for life
Treatment for rheumatic fever is
benzylpenicillin. (Penicillin G)
Treatment
The management of acute rheumatic
fever is geared toward the reduction of
inflammation with anti-inflammatory
medications such as aspirin or
corticosteroids.
Individuals with positive cultures for strep
throat should also be treated with
Penicillin G
Aspirin is the drug of choice and should
be given at high doses of 100 mg/kg/day.
One should watch for side effects like
gastritis and salicylate poisoning.
Acute Rheumatic Fever
Diagnosis
Jones Criteria Diagnosis of Rheumatic
Fever
o Two Major criteria, OR
o One Major + Two Minor,
o plus evidence of streptococcal
infection.
Exceptions are Chorea and Indolent
Carditis, each of which by itself can
indicate rheumatic fever.
Jones Major Criteria:
Migratory polyarthritis: a temporary
migrating inflammation of the large joints,
usually starting in the legs and migrating
upwards.
Carditis: inflammation of the heart
muscle which can manifest as CHF,
Pericarditis with a rub, or a new heart
murmur.
Subcutaneous Nodules: painless, firm
collections of collagen fibers over bones
or tendons. They commonly appear on
the back of the wrist, the outside elbow,
and the front of the knees.
Erythema Marginatum: a long lasting
rash that begins on the trunk or arms as
macules and spreads outward to form a
snake like ring while clearing in the
middle. This rash never starts on the face
and it is made worse with heat.
Sydenham's Chorea (St. Vitus' dance):
a characteristic series of rapid
movements without purpose of the face
and arms. This can occur very late in the
disease.
Acute Rheumatic Fever
In children and teenagers, the use of
aspirin and aspirin-containing products
can be associated with Reye's
syndrome, a serious and potentially
deadly condition. The risks, benefits and
alternative treatments must always be
considered when administering aspirin
and aspirin-containing products in
children and teenagers.
Ibuprofen for pain and discomfort and
corticosteroids for moderate to severe
inflammatory reactions manifested by
rheumatic fever should be considered in
children and teenagers.
Steroids are reserved for cases where
there is evidence of involvement of heart.
The use of steroids may prevent further
scarring of tissue and may prevent
development of sequelae such as mitral
stenosis.
Monthly injections of longacting penicillin
must be given for a period of five years in
patients having one attack of rheumatic
fever.
If there is evidence of carditis, the length
of Penidure therapy may be up to 40
years.
Another important cornerstone in treating
rheumatic fever includes the continual
use of low-dose antibiotics (such as
penicillin, sulfadiazine, or erythromycin)
to prevent recurrence.
Heart failure
Some patients develop significant carditis which
manifests as congestive heart failure. This
requires the usual treatment for heart failure:
diuretics and digoxin. Unlike normal heart
failure, rheumatic heart failure responds well to
corticosteroids.
Jones Minor Criteria
Fever
Arthralgia: Joint pain without swelling
Raised Sedimentation Rate
Raised C-reactive protein
Leukocytosis
ECG showing features of Heart
block, such as a prolonged PR
interval
Evidence of streptococcal infection:
1. Elevated Antistreptolysin O
titre
2. Elevated DNAase
Previous episode of rheumatic fever
or inactive heart disease
Aortic Aneurysm
An Aortic Aneurysm is a general term for any
swelling / dilation of the aorta, usually
representing an underlying weakness in the wall
of the aorta at that location.
While the stretched vessel may occasionally
cause discomfort, a greater concern is the risk
of rupture, which causes severe pain; massive
internal hemorrhage; and, without prompt
treatment, death occurs rapidly.
Classification
Aortic aneurysms are classified by where on the
aorta they occur; aneurysms can appear
anywhere.
Abdominal Aortic Aneurysms, the
most common form of aortic aneurysm,
Aortic Root Aneurysm, or aneurysm of
sinus of Valsalva, appears on the
sinuses of Valsalva or aortic root.
Thoracic Aortic Aneurysms are located
in the Thoracic Cavity - classified as
Ascending, Aortic Arch, or Descending
Aneurysms depending on the location on
the thoracic aorta involved.
Thoracoabdominal Aortic Aneurysms
involve both the thoracic and abdominal
aorta.
Pathology
The physical change in the aortic
diameter can occur secondary to trauma,
infection, an intrinsic defect in the protein
construction of the aortic wall, or due to
progressive destruction of aortic proteins
by enzymes.
Aortic Aneurysm
An AAA may remain asymptomatic
indefinitely
Generally asymptomatic before rupture.
Classic Triad of Rupture:
1. Pain
2. Hypotension
3. Mass
The pain is classically reported in the
abdomen, back or flank.
Pain is acute, severe, constant, with
radiation through the abdomen to the
back
Increased risk of rupture @ 5 cm
diameter
Abdominal Bruit may be heard
Rupture is usually the first hint of AAA.
The diagnosis of Aneurysm is confirmed
at the bedside by the use of ultrasound.
Rupture confirmed by Contrast CT
Only 1025% of patients survive rupture
due to large pre- and post-operative
mortality..
U.S. Preventive Services Task Force:
Recommends one-time screening for
abdominal aortic aneurysm (AAA) by
ultrasonography in men age 65 to 75
years who have ever smoked.
Aortic Aneurysm
Signs, Symptoms and Diagnosis
Most intact aortic aneurysms are
asymptomatic
As they enlarge, symptoms such as
abdominal pain and back pain may
develop.
Compression of nerve roots may cause
leg pain or numbness.
Untreated, aneurysms tend to become
progressively larger, although the rate of
enlargement is unpredictable for any
individual.
May be found on physical examination
Pulsatile Mass
Symptoms may include: anxiety or
feeling of stress; nausea and
vomiting; clammy skin; rapid heart
rate
In patients presenting with aneurysm of
the arch of the aorta, a common
symptom is a hoarse voice as the left
recurrent laryngeal nerve winds around
the arch of the aorta.
AAAs are the most common type of
aortic aneurysm.
Most involve all three layers - tunica
intima, tunica media and tunica adventitia
Erythema Nodosum - Most common
sign for the aortic aneuysm - leg lesions
typically found near the ankle area.
Before rupture, an AAA may present as a
large, pulsatile mass above the
umbilicus.
Aortic Aneurysm
Management
Asymptomatic = Conservative Management
Surveillance with a view to eventual
repair, and immediate repair
Two modes of repair for an AAA:
1. Open aneurysm repair
2. Endovascular aneurysm repair
(EVAR).
Intervention recommended:
1. Growth of 1 cm per year
2. Lesion is greater than 5.5 cm
3. Indicated for symptomatic aneurysms
Conservative management is indicated in
patients where repair carries a high risk of
mortality and in patients where repair is unlikely
to improve life expectancy.
The mainstay of the conservative treatment
is smoking cessation.
Medical therapy - Strict blood pressure
control
Surveillance is indicated in small
asymptomatic aneurysms (less than
5.5 cm) where the risk of repair exceeds the
risk of rupture.
As an AAA grows in diameter the risk of
rupture increases.
No medical / pharmaceutical therapy has
been found to be effective at decreasing the
growth rate or rupture rate of asymptomatic
AAAs.
Blood pressure and lipids should however
be treated like in any atherosclerotic
condition.
Aortic Aneurysm
Prevention
Attention to patient's general blood
pressure, smoking and cholesterol risks
helps reduce the risk on an individual
basis.
The tetracycline antibiotic Doxycycline is
currently being investigated for use as a
potential drug in the prevention of aortic
aneurysm due to its metalloproteinase
inhibitor and collagen stabilising
properties.
Aortic Aneurysm
Studies have suggested possible protective
effects of therapy with ACE Inhibitors, B
Blockers, and Statins
Open repair is indicated in young patients as
an elective procedure, or in growing or large,
symptomatic or ruptured aneurysms.
Endovascular repairgenerally indicated in
older, high-risk patients or patients unfit for
open repair.
Aortic Dissection
Aortic Dissection is a potentially life-
threatening condition in which there is bleeding
into and along the wall of the aorta, the major
artery carrying blood out of the heart.
A tear in the inner wall of the aorta causes
blood to flow between the layers of the wall of
the aorta and force the layers apart
Dissection most commonly occurs in the
Thoracic chest portion of the aorta, but may
also occur in the abdominal portion.
Type A begins in the Ascending
Aorta.
Type B begins in the Descending
Aorta.
_____________ ______________
When a tear occurs, it creates two
channels:
1. Blood continues to travel
2. Blood remains still.
Aortic Dissection
Symptoms:
Abrupt, Sudden Onset of Severe Chest Pain
Sharp, stabbing, tearing, or ripping
Sub-sternal pain radiating to shoulder,
back, neck, arm, jaw, abdomen, or hip
Change position - pain typically
moves to the arms and legs as the
aortic dissection gets worse
Mental Status / CNS changes
Fainting / Nausea and vomiting
Pallor / Diaphoresis / Hypotension / JVD
Rapid, weak pulse / SOB
Blowing" murmur over the aorta
Blood pressure differences between the
right and left arms, or between the arms
and the legs
Signs of shock, but with normal blood
pressure
Aortic Dissection
As the aortic dissection grows bigger, the
channel with non-traveling blood can get
bigger and push on other branches of the
aorta.
An aortic dissection may also involve
abnormal ballooning of the aorta
(aneurysm).
The exact cause is unknown, but risks
include atherosclerosis and
hypertension
Traumatic injury is a major cause of aortic
dissection, especially blunt trauma to the chest
Hitting the steering wheel of a car during an
accident is a common traumatic cause.
Risk factors:
Aging
Bicuspid aortic valve
Coarctation (narrowing) of the aorta
Connective tissue disorders
Ehlers-Danlos syndrome
Heart surgery or procedures
Marfans syndrome
Pregnancy
Pseudoxanthoma Elasticum
Vascular inflammation due to
conditions such as Arteritis and
Syphilis
Imaging:
Aortic angiography
Chest x-ray mediastinal widening /
pleural effusion
MRI / CT
Doppler Ultrasonography
Echocardiogram
Transesophageal Echocardiogram
(TEE)
Aortic Dissection
Treatment
The goal of treatment is to prevent
complications. Hospitalization is required.
Type A - Immediate Surgery to repair
the aorta.
Type B - may be treated with
medication first.
IV Hypertensive Medications
Strong pain relievers are usually needed.
Beta-blockers may reduce some of the
symptoms.
Aortic Valve replacement, if necessary
CAD Bypass, if necessary
Prognosis
Aortic dissection is life threatening.
Possibly managed surgically if prior to
dissection
Survival less than 50%
Complications
Aortic rupture causing rapid blood loss,
shock
Bleeding from the aorta
Blood clots
Cardiac Tamponade
Heart attack
Not enough blood flow past the
dissection
Permanent kidney failure
Stroke
Arterial Embolism
A sudden interruption of blood flow to an
organ or body part due to an embolus
adhering to the wall of an artery thus
creating a blockage of blood flow distally.
Thromboembolism - the major type of
embolus being a blood clot
Arterial embolism is the major cause of
infarction.
Arterial Embolism
Pulmonary Embolism is sometimes
classified as arterial embolism as well in
the sense that the clot follows the
pulmonary artery carrying deoxygenated
blood away from the heart.
However, PE is generally classified as
a form of venous embolism, because
the embolus forms in veins.
Arterial Thrombosis
Thromboembolism
Is the combination of Thrombosis and
its main complication, Embolism
Thrombosis is the formation of a blood
clot inside a blood vessel, obstructing the
flow of blood through the circulatory
system.
When a blood vessel is injured, the body
uses platelets and fibrin to form a blood
clot to prevent blood loss.
Alternatively, even when a blood vessel
is not injured, blood clots may form in the
body if the proper conditions present
themselves.
If the clotting is too severe and the clot
breaks free, the traveling clot is now
known as an Embolus.
Arterial Thrombosis
Arterial thrombosis is the formation of a
thrombus within an artery.
Arterial thrombosis usually affects
individuals who already have
atherosclerosis
Atherosclerosis tends to develop in areas
where the Blood-flow is more turbulent,
for example where blood vessels branch
off.
Atherosclerosis causes the walls of the
arteries to fur up with deposits of
atheroma, a porridge-like substance.
In most cases, arterial thrombosis follows
rupture of atheroma, and is therefore
referred to as atherothrombosis.
Another common cause of arterial
thrombosis is atrial fibrillation, which
causes disturbed blood flow.
Cardioversion of atrial fibrillation carries a
great risk of thromboembolism
Arterial Thrombosis
Causes
Thrombosis is caused by abnormalities in one
or more of the following known as:
Virchow's Triad
1. Hypercoagulability / Thrombophilia
The Composition of the Blood
2. Endothelial Injury / Dysfunction
Quality of the vessel wall
3. Hemodynamic changes
Nature of the blood flow
Stasis, turbulence
1. Hypercoagulability
As seen with genetic deficiencies or
autoimmune disorders.
Cancers or malignancies like leukemia
CA Treatments - Radiation,
chemotherapy
2. Endothelial cell injury
Causes of injury to the vessel's wall
include trauma, surgery, infection or
turbulent flow at bifurcations.
3. Disturbed blood flow
Stagnation of blood flow past the point
of injury
Atrial Fibrillation causes stagnant blood
in the left atrium
___________________________________
Risk factors for arterial thrombosis
Smoking
High blood pressure
Increased levels of cholesterol
Diabetes
Increasing age
Family history
Poor diet
Excess body weight
Physical inactivity.
Arterial Thrombosis
Symptoms of arterial thrombosis
The build up of atheroma causes the
narrowing of the arteries, which can lead
to heart disease, angina, and heart
attacks, strokes or peripheral vascular
disease.
Peripheral vascular disease is a condition that
usually affects the lower part of the leg.
Although it is usually present in both legs, it is
common for symptoms to affect one side only.
Peripheral vascular disease appears to affect
men more than women and usually occurs after
the age of 50. It is particularly common in
people with diabetes and is rare in non-
smokers.
Symptoms include:
Intermittent Claudication
Cold extremities
Occasionally a blood clot may lodge in
one of the narrowed arteries. The leg
then becomes cold, numb and pale,
and loses its pulses.
When this happens it is vital to restore
the blood supply quickly, to prevent loss
of the leg. This requires surgery to
remove the clot.
CHRONIC
Arterial Occlusion
Peripheral Arterial Occlusive Disease
Claudication, is defined as reproducible
ischemic muscle pain, is one of the most
common manifestations of peripheral vascular
disease caused by atherosclerosis.
Claudication occurs during physical activity and
is relieved after a short rest.
Pain develops because of inadequate blood
flow.
Intermittent claudication typically causes pain
that occurs with physical activity.
Determining how much physical activity is
needed before the onset of pain is crucial.
Typically, vascular surgeons relate the
onset of pain to a particular walking
distance in terms of street blocks (eg, 2-
block Claudication).
Other important aspects of Claudication
pain are that the pain is reproducible
within the same muscle groups and that
it ceases with a resting period of 2-5
minutes.
Most common - Distal Superficial
Femoral Artery - corresponds to
Claudication in the calf muscle area
When atherosclerosis is distributed
throughout the Aorto-iliac area, thigh and
buttock muscle Claudication
predominates.
Atherosclerosis is a systemic disease
process. Patients who present with
claudication due to PAOD can be
expected to have atherosclerosis
elsewhere.
.
CHRONIC
Arterial Occlusion
This is the most common area for peripheral
vascular disease.
Superficial Femoral Artery occlusion on one
side
Superficial Femoral Artery stenosis on the
other side
Treatment of Claudication is medical, with
surgery reserved for severe cases
.
The goal is to impede the progression
Most effective to slow progression is to
stop tobacco use.
Extensive evidence indicates that
smoking cessation improves the
prognosis.
Improved walking distance and ankle
pressure have been attributed to
smoking cessation.
Exercise plays a vital role in the
treatment of Claudication.
Regular walking programs result in
substantial improvement (45 mins daily)
Control lipids, diabetes, and hypertension
CHRONIC
Arterial Occlusion
Risk Factors
The risk factors for PAOD are the same
as those for coronary artery disease or
cerebrovascular disease and include
diabetes, hypertension, Hyperlipidemia,
family history, sedentary lifestyle, and
tobacco use.
Smoking is the greatest of all the
cardiovascular risk factors. Counseling
patients on the importance of smoking
cessation is paramount in PAOD
management.
Physical Exam
Clues to underlying PAOD:
1. Atrophy of calf muscles
2. Loss of extremity hair
3. Shiny skin
4. Thickened toenails
Palpation of pulses should be attempted from
the abdominal aorta to the foot, with
auscultation for bruits in the abdominal
and pelvic regions.
Absence of a pulse signifies arterial
obstruction proximal to the area palpated
When palpable pulses are not present,
further assess with Doppler device.
o An audible Doppler signal assures
the clinician that some blood flow
is perfusing the extremity.
o If no Doppler signals can be
heard, a vascular surgeon should
be immediately consulted.
Ankle-Brachial Index (ABI). ABI is
calculated as the ratio of systolic blood
pressure at the ankle to that of the arm.
CHRONIC
Arterial Occlusion
Referral to a vascular surgeon
Reserved for Patients with limb-
threatening ischemia or significant life-
style limitations
Arteriogram is reserved for severe cases
warranting surgical repair.
Medications
Daily aspirin
Pentoxifylline (Trental) - 2-3 months to
produce noticeable results.
Clopidogrel (Plavix)
Enoxaparin (Lovenox) - more research
is needed to establish clinical efficacy.
Cilostazol (Pletal) may be beneficial
Statins - regardless of the baseline
cholesterol profile
Antiplatelet Agents
Decrease overall risk of cardiovascular disease
from myocardial infarction and stroke. Also
improve walking distance by enhancing
circulation.
Acute
Arterial Occlusion
This results in the sudden cessation of blood
flow to some area of the body.
The severity of ischemia and the viability of the
extremity depend on:
The location and extent of the occlusion
The presence and subsequent
development of collateral blood vessels.
There are two principal causes of acute arterial
occlusion:
1. Embolism
2. Thrombus in situ
Physical findings
Loss of pulses distal to the occlusion
Cyanosis or pallor
Mottling
Decreased skin temperature
Muscle stiffening
Loss of sensation
Weakness
Absent deep tendon reflexes.
Note:
If acute arterial occlusion occurs in the
presence of an adequate collateral circulation,
as is often the case in acute graft occlusion, the
symptoms and findings may be less impressive.
Acute
Arterial Occlusion
Acute Peripheral Arterial Occlusion
A sudden blockage of a peripheral artery.
The blockage may result from a blood
1. Clot
2. Embolism
3. Dissection
4. Trauma
Symptoms usually start suddenly
The symptoms of an acute arterial occlusion
depend on the location, duration, and severity of
the obstruction.
Severe Pain, Paresthesia, Numbness, &
Coldness
develop in the involved extremity within 1
hour.
Paralysis may occur with severe and
persistent ischemia.
The list of signs and symptoms mentioned in
various sources for Acute peripheral arterial
occlusion includes the 7 symptoms listed below:
Severe pain
Coldness
Paresthesias
Loss of sensation
Paleness in an extremity
Lack of pulse in an extremity
Blue skin in affect limb
Treatment List for Acute peripheral arterial
occlusion
The list of treatments mentioned in various
sources for Acute peripheral arterial occlusion
includes the following list. Always seek
professional medical advice about any
treatment or change in treatment plans.
Embolectomy, Thrombolysis or Bypass
Surgery
Giant Cell Arteritis
Giant-cell Arteritis / Temporal Arteritis
is an inflammatory disease of blood
vessels most commonly involving large
and medium arteries of the head.
It is a form of vasculitis.
The name Giant Cell Arteritis -
reflects the type of inflammatory cell
involved as seen on a biopsy.
The terms "Giant-Cell Arteritis" and
"Temporal Arteritis" are sometimes used
interchangeably, because of the frequent
involvement of the temporal artery.
May also involve other large vessels -
such as the aorta in "Giant-Cell Aortitis".
Temporal Arteritis - is also known as
"Cranial arteritis" and "Horton's Disease
Temporal, Giant cell, and Cranial Arteritis
occur when one or more arteries become
inflamed and die.
The condition may also be a systemic
disorder, affecting many medium-to-large
sized arteries anywhere in the body.
The cause is unknown but is believed to
be partly due to a faulty immune
response.
The disorder has been associated with
severe infections and high doses of
antibiotics.
The disorder may develop along with or
after Polymyalgia Rheumatica.
Giant Cell Arteritis is seen almost
exclusively in those over 50 years old - It
is rare in people of African descent.
Giant Cell Arteritis
Associated Conditions
Polymyalgia Rheumatica (PMR)
Polymyalgia Rheumatica is
characterized by sudden onset of
pain and stiffness in muscles (pelvis,
shoulder)
GCA and PMR are so closely linked that
they are often considered to be different
manifestations of the same disease
process.
Also:
1. Systemic Lupus Erythematosus,
2. Rheumatoid Arthritis
3. Severe Infections.
Physical Exam
Palpation of the head reveals prominent
temporal arteries with or without
pulsation.
The temporal area may be tender.
Decreased pulses may be found
throughout the body.
Evidence of ischemia may be noted on
fundal exam.
Laboratory Tests
Abnormal LFTs - particularly raised ALP-
Alkaline Phosphatase
Elevated Erythrocyte Sed. Rate
C-reactive protein, another
inflammatory marker, is also commonly
elevated.
Platelets may also be elevated.
Giant Cell Arteritis
Symptoms
It is more common in females than males by a
ratio of 3:1.
The mean age of onset is about 70 years, and it
is rare in those less than 50 years of age.
Patients present with:
Bruits
Fever
Headache
Scalp Tenderness
Jaw Claudication (pain in jaw when
chewing)
Tongue Claudication (pain in tongue
when chewing) and
Tongue Necrosis
Reduced Visual Acuity (blurred vision)
Acute Visual Loss (sudden blindness)
Diplopia
Acute Tinnitus
The inflammation may affect blood supply to
the eye and blurred vision or sudden
blindness may occur.
In 76% of cases involving the eye, the
ophthalmic artery is involved causing
anterior ischemic optic neuropathy
Loss of vision in both eyes may occur very
abruptly and this disease is therefore a
medical emergency.
Giant Cell Arteritis
Biopsy Diagnostic Gold Standard
(Examination for Giant Cells infiltrating the tissue)
Temporal Artery Ultrasound - Halo Sign
MRI and CT - Generally Negative
Treatment
This is a medical emergency
High-dose Corticosteroids, typically
prednisone (4060 mg bid), must be
started as soon as the diagnosis is
suspected to prevent irreversible
blindness secondary to ophthalmic artery
occlusion.
Steroids do not prevent the diagnosis
from later being confirmed by biopsy,
although certain changes in the histology
may be observed towards the end of the
first week of treatment and are more
difficult to identify after a couple of
months
The dose of prednisone is lowered after
24 weeks, and slowly tapered over 9
12 months.
Oral steroids are at least as effective as
intravenous steroids, except in the
treatment of acute visual loss where
intravenous steroids appear to offer
significant benefit over oral steroids
Peripheral Vascular Disease
Peripheral artery disease is a condition of the
blood vessels that leads to narrowing that
supply the legs and feet.
The narrowing of the blood vessels leads to
decreased blood flow, which can injure nerves
and other tissues.
Peripheral artery disease is caused by
arteriosclerosis
Arterial Vasculature become stiffer and cannot
dilate to allow greater blood flow when needed
Progressively Worsening Claudication is main
symptom, with eventual pain at rest
Classic Symptoms:
Pain, Fatigue, Burning, or Discomfort
in the muscles of the feet, calves, or
thighs.
These symptoms usually appear during walking
or exercise and resolve with rest.
Cool, Numb, Pale Extremities, even at rest.
Severe PAD:
Impotence
Pain and cramps at night
Pain or tingling in the feet or toes,
which can be so severe that even the
weight of clothes or bed sheets is
painful
Pain that is worse when the leg is
elevated
Improved by dangling legs over the
side of the bed
Ulcers that do not heal
Peripheral Vascular Disease
Severe PAD
Calf Muscle Atrophy
Hair loss over the toes and feet
Painful, non-bleeding ulcers on the
feet or toes
Cyanosis toes or foot
Shiny, tight skin
Thick toenails
Tests
Angiography of the arteries in the legs
Ankle-Brachial Index -Blood pressure
measured in the arms and legs for
comparison
Doppler ultrasound exam of an
extremity
Magnetic resonance angiography or
CT angiography
Treatment
Balance exercise with rest to improve
circulation
Stop smoking.
Foot Care - especially w/ diabetes.
Blood pressure control
Reduce weight
Control cholesterol
Glucose Control - diabetes
Medications:
1. Aspirin
2. Clopidogrel (Plavix)
3. Cilostazol dilates the affected artery
or arteries for moderate-to-severe
cases that are not candidates for
surgery
4. Statins
5. Analgesics
6. Hypertensives
7. Diabetic Meds
Peripheral Vascular Disease
Signs and Tests:
Arterial Bruits
Decreased blood pressure in the
affected limb
Loss of hair on the legs or feet
Weak or absent pulses in the limb
Peripheral Vascular Disease
Surgery:
May be performed if the condition is severe
(pain at rest)
Angioplasty and stent placement
Peripheral artery bypass surgery of the
leg
Leg or foot amputation.
Phlebitis
Phlebitis is an inflammation of a vein, usually in
the legs.
Phlebitis means inflammation of a vein.
Phlebitis can occur in both the surface
(superficial) or deep veins.
Thrombophlebitis is phlebitis is associated
with the formation of blood clots
Thrombophlebitis is the term used when a
blood clot in the vein causes the inflammation.
Thrombosis usually occurs in the deep veins of
the legs
Can travel to the lungs, causing Pulmonary
Embolisms
Superficial Phlebitis affects veins on the
skin surface. The condition is rarely
serious and, with proper care, usually
resolves rapidly. Sometimes people with
superficial phlebitis also get Deep Vein
Thrombophlebitis, so a medical evaluation
is necessary.
Deep Vein Thrombophlebitis affects the
larger blood vessels deep in the legs.
Blood clots (thrombi) can form, which may
break off and travel to the lungs. This is a
potentially life-threatening condition called
pulmonary embolism.
Phlebitis
May occur spontaneously, or
Complication of a medical procedure.
Local trauma and injury to a vein also
increase the risk of forming a blood clot.
Risk factors for DVT:
Prolonged inactivity
Long trips in a car or airplane
Bed rest after an operation or illness
Sedentary lifestyle
Inactivity with little or no exercise
Obesity
Smoking cigarettes
Hormone replacement therapy or birth
control pills
Pregnancy
Certain medical conditions, such as
cancer or blood disorders, that increase
the clotting potential of the blood
Injury to the arms or legs
Varicose veins may be associated with
superficial phlebitis
Phlebitis
Signs and Symptoms
Redness (erythema) and warmth with a
temperature elevation of a degree or
more above the baseline
Pain or burning along the length of the
vein
Swelling (edema
Vein being hard, and cord-like
If occurring due to an intravenous
infusion line, then slowed infusion rate
Superficial Phlebitis
Usually a slow onset of a tender red area
along the superficial veins on the skin.
A long, thin red area may be seen as the
inflammation follows the path of a
superficial vein.
This area may feel hard, warm, and
tender. The skin around the vein may be
itchy and swollen.
The area may begin to throb or burn.
Symptoms may be worse when the leg is
lowered, especially when first getting out
of bed in the morning.
A low-grade fever may occur.
Sometimes phlebitis may occur at the
site where a peripheral intravenous (IV)
line was started. The surrounding area
may be sore and tender along the vein.
If an infection is present, symptoms may
include redness, fever, pain, swelling, or
breakdown of the skin.
Phlebitis
Vasculitis:
Bacterial: Pathogenic organisms can
gain access and stimulate inflammation.
Chemical: caused by irritating or
vesicant solutions.
Mechanical: physical trauma from the
skin puncture and movement of the
cannula into the vein during insertion;
any subsequent manipulation and
movement of the cannula; clotting; or
excessively large cannula.
Medications: including celecoxib,
olanzapine, antidepressants, and others.
Genetic / Familial Risk
Alcohol abuse
Signs and symptoms
Redness (erythema) and warmth with a
temperature elevation of a degree or
more above the baseline
Pain or burning along the length of the
vein
Swelling (edema
Vein being hard, and cord-like
If occurring due to an intravenous
infusion line, then slowed infusion rate
Massage is contraindicated - manipulations
risks breaking loose a clot which could then
travel to the lungs (pulmonary embolism) or the
heart
Thrombophlebitis
Thrombophlebitis is phlebitis is
associated with the formation of blood
clots
Usually occurs in leg veins, but it may
occur in an arm.
The thrombus (clot) in the vein causes
pain and irritation and may block blood
flow in the veins.
Patients at Increased Risk:
Being hospitalized for a major surgery
or with a major illness
Disorders that make you more likely to
develop blood clots
Sitting for a long period of time (long
airplane trip)
Two Types of Thrombophlebitis
1. Deep venous thrombosis
(affects deeper, larger veins)
2. Superficial Thrombophlebitis
(affects veins near the skin surface)
Tests
Blood coagulation studies
Doppler ultrasound
Venography
Thrombophlebitis
Deep Vein Thrombophlebitis
Signs and Symptoms:
1. Redness
2. Warmth / Tenderness
3. Inflammation
4. Calf / Leg Pain
Treatment
Support Stockings
Analgesics
Antibiotics (if infection is present)
Anticoagulants to prevent new clots
NSAIDS to reduce pain & inflammation
Thrombolytic Drugs to dissolve an
existing clot
Apply moist heat to reduce
inflammation and pain
Keep pressure off of the area to
reduce pain and decrease the risk of
further damage
Elevation to reduce swelling
Surgical removal, stripping, or bypass of the
vein is rarely needed
Superficial Thrombophlebitis rarely causes
complications.
Pulmonary Embolism Complication
Chronic Leg Pain / Inflammation - Complication
Routine changing of I.V. lines helps to prevent
Thrombophlebitis
Venous Thrombosis
Deep Venous Thrombosis is the
formation of a blood clot ("thrombus") in
a deep vein.
It is a form of Thrombophlebitis
(inflammation of a vein with clot
formation)
Commonly occurs in the Femoral Vein,
Popliteal Vein, or the deep veins of the
pelvis.
Paget-Schrtter Disease - VT occuring
spontaneously in the arm
A DVT can occur without symptoms, but
in many cases the affected extremity will
be painful, swollen, red, warm and the
superficial veins may be engorged.
The most serious complication of a DVT
is that the clot could dislodge and travel
to the lungs, which is called a pulmonary
embolism (PE).
DVT is a medical emergency, so, all limb
swellings, however trivial, should be regarded
as a DVT until proven otherwise.
Late complication of DVT is the post-thrombotic
syndrome, which can manifest itself as edema,
pain or discomfort and skin problems
.
According to Virchow's triad, venous
thrombosis occurs via three mechanisms:
1. Decreased flow rate of the blood,
2. Damage to the blood vessel wall
3. Increased tendency of the blood to clot -
(Hypercoagulability).
Venous Thrombosis
Signs and symptoms
There may be no symptoms referable to the
location of the DVT
Classical symptoms of DVT include pain,
swelling and redness of the leg and dilation of
the surface veins.
To Objectivate Edema Measure the
circumference of the affected and the
contralateral limb at a fixed point
Palpate the venous tract for tenderness
Physical examination is unreliable for
excluding the diagnosis of deep vein
thrombosis.
Very extensive DVTs can extend into the Iliac
Veins or the Inferior Vena Cava.
Diagnosis
The gold standard is intravenous
venography
Because of its invasiveness, this test is rarely
performed.
Abdominal computed tomographic scan
showing a Common Iliac Vein Thrombosis.
Physical examination
Homans sign: Dorsiflexion of foot elicits pain in
posterior calf
Pratt's sign: Squeezing of posterior calf elicits
pain.
However, these medical signs do not perform
well and are not included in clinical prediction
rules that combine best findings in order to
diagnose DVT.
Venous Thrombosis
Several medical conditions can lead to DVT
Compression of the veins
Physical trauma
Cancer
Infections
Inflammatory diseases
Stroke
Heart failure
Nephrotic syndrome.
At risk for DVT:
Surgery
Hospitalization,
Orthopedic cast Immobilization
Traveller's Thrombosis
Smoking
Obesity
Age
Certain drugs
Estrogen
Erythropoietin
Genetic Thrombophilia
Factor V Leiden
Pregnancy
Diagnositic Tests of DVT
1. D-Dimer
2. Doppler Ultrasound
3. CBC
4. PT
5. PTT (Primary coagulation studies)
6. Fibrinogen
7. LFTs
8. Renal Function
9. Electrolytes
Venous Thrombosis
Management
The main issue with anticoagulation in
pregnancy is that warfarin, the most
commonly used anticoagulant in chronic
administration, is known to have teratogenic
effects on the fetus if administered in early
pregnancy.
Anticoagulation
1. Heparin for one week
2. Warfarin for 3- to 6-month
Low molecular weight heparin is preferred
Unfractionated heparin is given in patients
who have a contraindication to LMWH
(e.g., renal failure or imminent need
for invasive procedure.
Thrombolysis
Thrombolysis is generally reserved for
extensive clot, e.g. an iliofemoral thrombosis
.
Thrombectomy
Used is Thrombus can be removed with a
mechanical thrombectomy device.
Compression stockings should be
routinely applied
Inferior vena cava filter may be used
Hospitalization
Hospitalization should be considered in patients
with more than two of the following risk factors
Bilateral DVT
Renal Insufficiency
Low Body Weight (<70 kg/154 lbs)
Recent Immobility
Chronic Heart Failure
Cancer
Varicose Veins
Varicose veins are veins that have become
enlarged and tortuous.
Leg muscles pump the veins to return blood to
the heart, against the effects of gravity.
When veins become varicose, the leaflets of the
valves no longer meet properly, and the valves
do not work. This allows blood to flow
backwards and they enlarge even more
Varicose veins are most common in the
superficial veins of the legs, which are subject
to high pressure when standing.
Besides cosmetic problems, varicose veins are
often painful, especially when standing or
walking.
Non-surgical treatments:
Sclerotherapy
Elastic stockings
Elevating the legs
Exercise.
Surgical Treatment:
Vein Stripping
Ambulatory phlebectomy
Vein Ligation
Cryosurgery
Alternative Treatment Techniques
Ultrasound-guided Sclerotherapy
Radiofrequency Ablation
Endovenous Laser Treatment
Varicose veins are distinguished from
Reticular Veins (blue veins) and
Telangiectasias (spider veins)
by size and location of the veins
Varicose Veins
Signs and Symptoms
Aching, heavy legs - worse at night and
after exercise)
Appearance of spider veins
(Telangiectasia)
Ankle Edema
Stasis Dermatitis - Redness, dryness,
and itchiness of areas of skin
Leg Cramps especially with
sudden move as standing up.
Minor injuries prolonged bleeding /
slow healing
Lipodermatosclerosis - skin above the
ankle may shrink because the fat
underneath the skin becomes hard.
Atrophie Blanche - Whitened, irregular
scar-like patches can appear at the
ankles
Causes
Pregnancy
Obesity
Menopause
Aging
Prolonged standing
Leg injury
Abdominal straining
Crossing legs at the knees or ankles
Treatment is Conservative
Elevating the legs often provides
temporary symptomatic relief.
Compression Stockings - Caution
should be exercised in their use in
patients with concurrent arterial disease.
NSAIDs
Regular exercise is not supported by
any evidence
Valvular Diseases
Valvular Diseases
Aortic Stenosis
Crescendo-decrescendo
Harsh
Systolic
Best heard at the second intercostal
space
Right upper sternal border
Radiates to one or both carotid arteries.
Increased with squatting
Reduced during Valsalva strain
Aortic Stenosis
In adults, three conditions are known to cause
aortic stenosis.
1. Progressive wear and tear of a bicuspid
valve present since birth (congenital).
2. Wear and tear of the aortic valve in the
elderly.
3. Scarring of the aortic valve due to
rheumatic fever as a child or young adult.
Aortic Insufficiency
The hallmark of Aortic Regurgitation/
Insufficiency
High-pitched
Decrescendo
Diastolic
Murmur at the Left Sternal Border after
the Second Heart Sound.
Aortic Insufficiency
Rheumatic Fever
Ankylosing spondylitis
Aortic dissection
Congenital (present at birth) valve
problems
Endocarditis
High blood pressure
Marfan syndrome
Reiter syndrome
Syphilis
Systemic lupus Erythematous
Mitral Stenosis
Classic murmur of Mitral stenosis
Low-pitched, Rumbling
Loud S1
Opening Snap
Diastolic
best heard with the bell @ Apex
The length of the murmur, as opposed to
the intensity, is used as a nonspecific
guide to stenosis severity.
Mitral Stenosis
Causes of mitral stenosis include the following:
Rheumatic fever
Congenital Mitral stenosis
Systemic lupus Erythematous (SLE)
Rheumatoid arthritis (RA)
Malignant Carcinoid
Fabry disease
Whipple disease
Mitral Insufficiency
Most common cardiac problem seen in
Rheumatic Heart Disease.
Pansystolic
High-pitched
Blowing
Apical
Radiates to the left axilla.
NOTE: Pancarditis is the most serious and
second most common complication of
rheumatic fever
Mitral Insufficiency
Most common cause is Mitral Valve
Prolapse (MVP)
Ischemic heart disease
Rheumatic fever
Marfan's syndrome
Secondary mitral regurgitation is due to the
dilatation of the left ventricle, due dilated
cardiomyopathy, including aortic insufficiency,
nonischemic dilated cardiomyopathy It is also
called functional mitral regurgitation
Acute Mitral Regurgitation
most often caused by Infective Endocarditis,
mainly S. aureus
Mitral Valve Prolapse
Can occur in a multitude of disorders
Typically reflects a benign, normal variant
rather than a single disease process.
Usually is asymptomatic, nonprogressive, and
benign.
May present as:
Chest pain
Dyspnea
Fatigue
Dizziness
Near-syncope symptoms
Anxiety
Mitral Valve Prolapse
Causes
Most cases of mitral valve prolapse are primary,
idiopathic in nature, and expressed as an
autosomal dominant trait that exhibits both sex-
and age-dependent penetrance.
Connective tissue disorders
Marfan syndrome
Ehlers-Danlos syndrome
Osteogenesis imperfecta
Pseudoxanthoma elasticum
Polycystic kidney disease
Stickler syndrome
Systemic lupus erythematosus
Relapsing polychondritis
Polyarteritis Nodosa
Muscle disorders
Duchenne muscular dystrophy
Fragile X syndrome
Mucopolysaccharidoses
Myotonic dystrophy
Mitral Valve Prolapse
Murmur:
Mid-systolic click.
Crescendo-Decrescendo
Heard best at the apex.
The click is so characteristic of MVP that even
without a subsequent murmur, its presence
alone is enough for the diagnosis.
In stark contrast to most other murmurs, MVP is
enhanced by Valsalva maneuvers and
decreased by squatting.
Mitral Valve Prolapse
Congenital heart disease
Atrial Septal defect (ASD)
Epstein anomaly
Acquired heart disease
Papillary muscle dysfunction (eg,
ischemia, Myocarditis)
Cardiac trauma
Post Mitral valve surgery
Rheumatic Endocarditis
Miscellaneous
Wolff-Parkinson-White syndrome
Von Willebrand disease
Tricuspid Stenosis
A prominent right atrium may be
palpable to the right of the sternum.
Opening snap, if not obscured by
Mitral stenosis sounds
Widely Split S1
A diastolic murmur is audible along
the left sternal border or at the
Xiphoid
Increases with inspiration.
Tricuspid Regurgitation is also
present, represented by a
Holosystolic murmur in a similar
location.
Tricuspid Stenosis
Tricuspid stenosis is almost always
Rheumatic in origin
Generally accompanied by Mitral and
Aortic valve involvement.
Most Stenotic Tricuspid Valves are
associated with clinical evidence of
regurgitation
Stenotic Tricuspid Valves are always
anatomically abnormal
Cause is limited to a few conditions -
With the exceptions of congenital causes
or active Infective Endocarditis, Tricuspid
Stenosis takes years to develop
Tricuspid Insufficiency
S
3
gallop:
Jugular Venous Distention
Prominent V wave
Pansystolic murmur
Heard along the lower left sternal
border
Inspiratory accentuation.
Diminished peripheral pulse volume
Hypotension due to therapeutic
interventions used to decrease
volume overload
Pulmonary Rales
LV dysfunction
Mitral Stenosis
RV heave
S
4
gallop that increases with
inspiration
Ascites and Jaundice
Peripheral edema
Cachexia
Atrial fibrillation
Fourth intercostal Parasternal region
The murmur is usually augmented
during inspiration and is reduced in
intensity and duration in the standing
position and during a Valsalva
maneuver.
Tricuspid Insufficiency
Causes
Rheumatic heart disease
Endocarditis
Ebstein anomaly
Prolapse (floppy, redundant)
Carcinoid
Papillary muscle dysfunction
Trauma
Connective-tissue diseases
Medications
Anatomically normal tricuspid valve
1. Dilatation of the RV cavity.
2. The valve structures are normal;
Medical Treatment
The medical therapy used in the treatment of
tricuspid regurgitation is directed toward the
control of CHF that is causing or contributing to
the problem.
Diuretics
Are used to control the fluid overload associated
with the process.
Cardiac glycosides
Digoxin is used to control Atrial fibrillation and to
increase myocardial contractility.
Angiotensin-converting enzyme (ACE)
inhibitors
Are used to provide afterload reduction, thereby
decreasing the volume load on the right
ventricle.
Anticoagulants
Are used to prevent thrombosis and
embolization from the prosthetic valve used in
the treatment of tricuspid regurgitation.
Pulmonary Stenosis
Normal S1
Split S2
Systolic Ejection Click.
The Louder on expiration.
Left upper sternal border
Second left intercostal space
Crescendo-decrescendo
Prominent jugular venous a wave and a
right ventricular lift
Cyanosis may occur
Causes
Results from a Mal-development of the
Pulmonic valve tissue
Coexisting Cardiac Malformations
1. Ventricular Septal Defect
2. Atrial Septal Defect
3. Patent Ductus Arteriosus.
4. Aberrant flow patterns in utero
Rubella Embryopathy
Family history is a mild risk factor
Congenital syndromes
1. Mayer-Rokitansky-Kuster-Hauser
Syndrome.
Pulmonary Stenosis
Management depends on the degree of
stenosis
Severe stenosis requires emergent dilatation
of valves by balloon valvulotomy
Patients with mild Pulmonic Valvular stenosis
usually do not require any treatment.
Cyanotic infants with respiratory distress and
hypotension/shock undergo a workup as that
for septic patients.
Bacterial Endocarditis prophylaxis
Pulmonary Insufficiency
Wide splitting of S2
Right-sided S3 may be audible and
Accentuated with inspiration
Right-sided S4 may be audible and
accentuated with inspiration
Low-pitched murmur, usually best
heard along the third or fourth intercostal
spaces adjacent to the left sternal border;
may be accentuated with inspiration
Graham-Steell's murmur, a high-
pitched, blowing decrescendo murmur
heard best along the left Parasternal
region
Etiology
Pulmonary hypertension (causing
insufficiency secondary to dilatation of
the valve ring)
Infective Endocarditis
Rheumatic heart disease
Congenital abnormalities (e. g., Tetralogy
of Fallot, Ventral Septal Defect, Valvular
Pulmonic Stenosis)
Carcinoid heart disease
Pulmonary valve repair
Pulmonary Insufficiency
Signs and Symptoms
May be tolerated for years without
problems
Dyspnea
Complications
Right heart failure
Treatment
Pulmonary insufficiency is usually well
tolerated
Valvuloplasty / Valve replacement
Acute
Bacterial Endocarditis
Bacterial Endocarditis is a microbial infection of
the endothelial surface of the heart.
Signs and symptoms of bacterial Endocarditis
are diverse; therefore, the practitioner must
have a high degree of suspicion to make an
early diagnosis.
Features of bacterial Endocarditis are due to
bacteremia, local cardiac invasion by
organisms, peripheral embolization, and the
formation of immune complexes.
Patients present with many nonspecific
symptoms
85-99% of patients are febrile. Patients with
congenital heart disease and fever require
special consideration
Fatigue, chills, sweats, anorexia, malaise, a
cough, a headache, Myalgias, Arthralgias,
and confusion.
Acute - toxic, febrile illness and symptoms that
have lasted less than 2 weeks.
Sub acute - more nonspecific flu like illness and
symptoms that have lasted more than 2 weeks
A history of intravenous (IV) drug use may be
elicited.
S Aureus is the most common cause
In neonates, Endocarditis commonly produces
septic embolic phenomena, such as
Osteomyelitis, Meningitis, and Pneumonia
Neonates with Endocarditis may also have
feeding problems, respiratory distress,
tachycardia, or Neurologic symptoms.
Acute
Bacterial Endocarditis
Medical Care
Bacterial Endocarditis is a disease in which
complete eradication of the organism is
required.
Prolonged parenteral therapy is the only way to
achieve bactericidal serum levels for the time
needed to kill all the bacteria present in a
vegetation of endocarditis.
Treatment ranges from 4-8 weeks.
Therapy is tailored according to the etiologic
agent.
Penicillin G for 4 weeks
-or-
Penicillin or Ceftriaxone combined with
Gentamicin for 2 weeks.
Penicillin-resistant streptococcal
Endocarditis (PRSE) - Penicillin, Ampicillin, or
Ceftriaxone for 4 weeks combined with
gentamicin for the first 2 weeks
.
MRSA - infection on native valves is treated
with Vancomycin for at least 6 weeks, with or
without 3-5 days of gentamicin.
Gram negative Endocarditis:
HACEK - Ceftriaxone or Ampicillin plus
Gentamicin for 4 weeks.
Acute
Bacterial Endocarditis
Duke Criteria: used for Diagnosis:
Positive blood cultures
Positive Echo - oscillating mass
and/or vegetation, paravalvular
abscess, or dehiscence of a
prosthetic valve)
New Valvular regurgitation
Predisposition (history of IV drug
use or congenital heart disease)
Fever with a temperature of more
than 38C
Vascular phenomena (arterial emboli,
septic pulmonary infarcts, intracranial
hemorrhage, conjunctival
hemorrhage,
Janeway lesions - painless,
hemorrhagic lesions on palms and
soles
Immunologic phenomena
(Glomerulonephritis, Osler nodes,
Roth spots, positive result for
rheumatoid factor)
.
Acute
Bacterial Endocarditis
Surgical Care
Absolute indications for surgery include
progressive cardiac failure, valve
obstruction, definitive Peri-Valvular abscess,
Non-candidal Fungal infection, and
Pseudomonas infection
Relative indications include persistent
bacteremia despite appropriate antibiotic
therapy, Candidal Endocarditis, and
Vegetations larger than 10 mm.
Surgery should be performed without delay in
patients with severe congestive heart failure
(CHF) secondary to Valvular regurgitation
Sub-Acute
Bacterial Endocarditis
Subacute bacterial endocarditis is a type of
Infective Endocarditis
Summary:
In cases of subacute bacterial endocarditis,
the causative organism - Streptococcus
Viridans - needs a previous heart valve
disease to colonize and cause such disease.
In cases of acute bacterial endocarditis, the
organism can colonize on the healthy heart
valve, causing the disease.
Considered a form of Type III
hypersensitivity
Sub acute bacterial Endocarditis is
more common in patients with an
underlying congenital heart defect.
Diagnosis
Osler's nodes
Swelling, redness, and pain that characterize
these lesions of the hands and feet - The nodes
are commonly indicative of subacute bacterial
endocarditis.
Other signs:
Roth's Spots and Janeway Lesions occur on
the palms and soles, can be differentiated from
Osler's nodes because they are nontender.
Causes
Causative Agent -Streptococci Viridans -
bacteria that normally live in the mouth and
throat - Streptococcus mutans, mitis, sanguis
or milleri).
Other strains of streptococci (bovis and
equines) can also cause subacute endocarditis,
usually in patients who have a form of
gastrointestinal cancer.
Sub-Acute
Bacterial Endocarditis
Prognosis
Underlying structural valve disease is usually
present in patients before developing subacute
endocarditis.
It is less likely to lead to septic emboli than is
acute endocarditis, but subacute endocarditis
has a relatively slow process of infection and, if
left untreated, can worsen for up to one year
before it is fatal.
Treatment
The standard treatment is with a minimum of
four weeks of high-dose intravenous penicillin
with an aminoglycoside such as gentamicin.
Note:
Penicillin G vs. Pen VK
Penicillin G Benzathine (orally and
parenteral). Trade names are: Bicillin LA and
Permapen.
Penicillin V potassium (Oral) is
characteristically known for being stable in acid
(therefore, is taken orally). Trade names are:
Ledercillin VK and SK-Penicillin VK
Acute Pericarditis
Inflammation of pericardium characterized by:
1. Chest pain
2. Pericardial friction rub
3. Serial EKG changes
Caused by Serous or Hemorrhagic Effusion.
Granulomatous pericarditis
1. TB,
2. Fungal infections
3. Rheumatoid arthritis
4. Sarcoidosis.
The pericardium drainage occurs via the
thoracic duct and the right lymphatic duct into
the right pleural space.
Pericardial physiology includes 3 functions:
1. Promotes cardiac efficiency by limiting acute
dilation, maintaining ventricular compliance with
preservation of the Starling curve, and
distributing hydrostatic forces. The pericardium
also creates a closed chamber with sub
atmospheric pressure that aids Atrial filling and
lowers transmural cardiac pressures.
2. Through its membranous function, the
pericardium shields the heart by reducing
external friction and acting as a barrier against
extension of infection and malignancy.
3. Through its ligamentous function, the
pericardium anatomically fixes the heart.
Acute Pericarditis
3. Bacterial
Causes Purulent Pericarditis.
Bacterial pericarditis develops from direct
Pulmonary Extension, Hematogenous
spread, Myocardial Abscess or
Endocarditis, Penetrating injury to chest
wall from either trauma or surgery, or a
sub diaphragmatic suppurative lesion.
.
Treatment includes appropriate antibiotics for at
least 4 weeks and drainage of pericardial fluid.
4. Inflammatory Disorders
Rheumatoid arthritis
.
Systemic lupus Erythematosus
Scleroderma
o Pericardial effusions occur in 40%
of patients with scleroderma and
can be due to scleroderma,
restrictive Cardiomyopathy, and
renal failure.
o Pericardial fluid has a protein
value greater than 5 g/dL, has a
low cell count, and does not
demonstrate the antibodies found
in RA and SLE.
o These patients have a poor
prognosis.
Rheumatic fever
Sarcoidosis
Acute Pericarditis
Chest pain is the cardinal symptom.
1. Sharp, dull, aching, burning, or
pressing.
2. Worse during inspiration, when
lying flat, or during swallowing and
with body motion
.
Dyspnea, especially with Tamponade.
Fever may be present.
Abdominal pain occurs infrequently in
children.
Physical
Friction Rub is Pathognomonic.
Tachypnea
Tachycardia
Patients may have fever.
Becks Triad - (Cardiac Tamponade)
1. Hypotension
2. JVD
3. Muffled heart sounds
Especially w/ Sudden Intra-pericardial
Hemorrhage)
Pulsus Paradoxus is defined as a > 10 mm
Hg decrease in arterial systolic pressure with
inspiration.
This decrease is important in patients with
more slowly developing Tamponade
because they may lack findings of the Beck
triad.
Causes
1. Idiopathic
2. Viral - the most common cause
1. Coxsackievirus B
2. Echovirus
3. Adenoviruses
4. Influenza A and B
5. HIV
6. HSV
Acute Pericarditis
Other inflammatory conditions
o Sjgren syndrome
o Mixed connective-tissue disease
o Reiter syndrome
o Ankylosing spondylitis
o Inflammatory bowel disease
o Wegener granulomatosis
o Vasculitis (eg, giant cell arteritis,
polyarteritis)
o Polymyositis
o Behet syndrome
o Whipple disease
o Familial Mediterranean fever
o Serum sickness
Metabolic disorders
Renal failure
Hypothyroidism
Cholesterol pericarditis
Cardiovascular diseases
Myocardial infarction
Dressler Syndrome
Aortic dissection
Takotsubo Cardiomyopathy
Neoplasm
Miscellaneous causes, including iatrogenic
Drugs
Irradiation
Post Pericardiotomy syndrome
Invasive cardiac procedures
Trauma
Cardiac Tamponade
Compression of the heart that occurs
when blood or fluid builds up in the space
between the myocardium and the
pericardium
Tamponade is life-threatening
Causes
Blood or fluid collects in the pericardium.
This prevents the ventricles from
expanding fully. The excess pressure
from the fluid prevents the heart from
functioning normally.
Due to:
Dissecting aortic aneurysm (thoracic)
End-stage lung cancer
Heart attack (acute MI)
Heart surgery
Pericarditis caused by bacterial or viral
infections
Wounds to the heart
Other potential causes include:
Heart tumors
Hypothyroidism
Kidney failure
Placement of central lines
Radiation therapy to the chest
Recent invasive heart procedures
Recent open heart surgery
Systemic lupus Erythematous
Symptoms
Becks Triad - (Cardiac Tamponade)
1. Hypotension
2. JVD
3. Muffled heart sounds
Cardiac Tamponade
Other Symptoms
Anxiety, restlessness
Chest pain
CP radiating to the neck, shoulder,
back, or abdomen
CP is Sharp, stabbing
CP is worsened by deep breathing or
coughing
Difficulty breathing
Discomfort, sometimes relieved by sitting
upright or leaning forward
Fainting, light-headedness
Pale, gray, or blue skin
Palpitations
Rapid breathing
Swelling of the abdomen or other areas
Dizziness
Drowsiness
Low blood pressure
Weak or absent pulse
Echocardiogram is typically used to help
establish the diagnosis.
Signs:
Pulsus Paradoxical - Blood pressure
may fall when the person inhales
deeply
Breathing may be rapid (faster than 12
breaths in an adult per minute)
Heart rate may be over 100 (normal is
60 to 100 beats per minute)
Heart sounds are faint during
examination with a stethoscope
Neck veins may be abnormally
extended (distended) but the blood
pressure may be low
Peripheral pulses may be weak or
absent
Chest CT / MRI
Chest x-ray
Coronary angiography
ECG
Cardiac Tamponade
Treatment
Cardiac Tamponade is an emergency condition
that requires hospitalization
Pericardiocentesis - fluid must be drained
Surgical Pericardioectomy
Fluids replacement for Hypotension
The cause of the Tamponade must be
identified and treated.
Cardiac Tamponade
Wolff-Parkinson-White
Wolff-Parkinson-White syndrome is
a heart condition in which there is
an extra electrical pathway
Leads to episodes tachycardia
Wolff-Parkinson-White is one of the
most common causes of fast heart
rate disorders in infants and
children.
Wolff-Parkinson-White
Delta Wave
Patients are usually asymptomatic.
However, during supraventricular
tachycardia the individual may have
symptoms of palpitation, dizziness,
shortness of breath, and syncopy / near
syncopal episodes of supraventricular
tachycardia
.
An ECG will show the telltale "Delta
wave".
CARDIAC DRUGS
CARDIAC DRUGS
Anticoagulants
Heparin
Warfarin
Dalteparin
Danaparoid
Enoxaparin
Tinzaparin
Anticoagulants
Decreases the clotting ability of the
blood.
They do NOT dissolve existing blood
clots.
Used to treat certain blood vessel, heart
and lung conditions.
Helps to prevent harmful clots from
forming in the blood vessels.
May prevent the clots from becoming
larger and causing more serious
problems.
Often prescribed to prevent first or
recurrent stroke.
Antiplatelet Agents
Aspirin
Clopidogrel - (Plavix)
Ticlopidine
Dipyridamole
Antiplatelet Agents
Keeps blood clots from forming by
preventing blood platelets from sticking
together.
Helps prevent clotting in patients with h/o
MI, Unstable Angina, Ischemic Strokes,
TIA
Usually prescribed preventively, when
plaque buildup is evident but there is not
yet a large obstruction in the artery.
Angiotensin-Converting Enzyme
(ACE) Inhibitors
Benazepril - (Lotensin)
Captopril - (Capoten)
Enalapril - (Vasotec)
Fosinopril - (Monopril)
Lisinopril - (Prinivil, Zestril)
Moexipril - (Univasc)
Perindopril - (Aceon)
Quinapril - (Accupril)
Ramipril - (Altace)
Trandolapril - (Mavik)
Angiotensin-Converting Enzyme
(ACE) Inhibitors
Expands blood vessels and decreases
resistance by lowering levels of
Angiotensin II.
Allows blood to flow more easily and
makes the heart's work easier or more
efficient.
Used to treat or improve symptoms of
cardiovascular conditions including high
blood pressure and heart failure.
Always recommended for DM to help
protect Renal Function
Angiotensin II Receptor Blockers
(ARBS)
Candesartan - (Atacand)
Eprosartan - (Teveten)
Irbesartan - (Avapro)
Losartan - (Cozaar)
Telmisartan - (Micardis)
Valsartan - (Diovan)
Angiotensin II Receptor Blockers
(ARBS)
Rather than lowering levels of
Angiotensin II (as ACE inhibitors do)
Angiotensin II receptor blockers prevent
this chemical from having any effects on
the heart and blood vessels.
This keeps blood pressure from rising.
Used to treat or improve symptoms of
cardiovascular conditions including high
blood pressure and heart failure
Beta Blockers
Acebutolol - (Sectral)
Atenolol - (Tenormin)
Betaxolol - (Kerlone)
Bisoprolol/ HCTZ - (Ziac)
Bisoprolol - (Zebeta)
Carteolol - (Cartrol)
Metoprolol - (Lopressor, Toprol XL)
Nadolol - (Corgard)
Propranolol - (Inderal)
Sotalol - (Betapace) and
Timolol - (Blocadren)
Beta Blockers
Decreases the heart rate and cardiac
output, which lowers blood pressure and
makes the heart beat more slowly and
with less force.
Used to lower blood pressure.
Used with therapy for cardiac
arrhythmias
Used to treat chest pain (angina).
Used to prevent future heart attacks in
patients who have had a heart attack.
Do NOT use ion DM patients b/c rise in
glucose
Calcium Channel Blockers
Amlodipine - (Norvasc, Lotrel)
Bepridil - (Vascor)
Diltiazem - (Cardizem, Tiazac)
Felodipine - (Plendil)
Nifedipine - (Adalat, Procardia)
Nimodipine - (Nimotop)
Nisoldipine - (Sular) and
Verapamil - (Calan, Isoptin, Verelan)
Calcium Channel Blockers
Interrupts the movement of calcium
into the cells of the heart and blood
vessels.
May decrease the hearts pumping
strength and relax blood vessels.
Used to treat high blood pressure,
chest pain (angina) caused by
reduced blood supply to the heart
muscle
Used to treat some arrhythmias
Diuretics
Amiloride - (Midamor)
Bumetanide - (Bumex)
Chlorothiazide - (Diuril)
Chlorthalidone - (Hygroton)
Furosemide - (Lasix)
Hydrochlorothiazide - (Esidrix,
Indapamide - (Lozol)
Spironolactone - (Aldactone)
Causes the body to rid itself of excess
fluids and sodium through urination.
Helps to relieve the heart's workload.
Decreases the buildup of fluid in the
lungs and other parts of the body, such
as the ankles and legs.
Different diuretics remove fluid at varied
rates and through different methods.
Used to help lower blood pressure.
Used to help reduce edema from excess
buildup of fluid in the body.
Vasodilators
Isosorbide Dinitrate - (Isordil)
Nesiritide - (Natrecor)
Hydralazine - (Apresoline)
Nitrates
Minoxidil
Relaxes blood vessels and increases the
supply of blood and oxygen to the heart
while reducing its workload.
Prescribed to patients who cannot
tolerate ACE inhibitors
Used to for angina
Digitalis Preparations
Digoxin
Digitoxin
Lanoxin
Increases the force of the heart's
contractions, which can be beneficial in
heart failure and for irregular heart beats.
Used to relieve heart failure symptoms,
especially when the patient isn't
responding to ACE inhibitors and
diuretics.
Also slows certain types of arrhythmias,
particularly Atrial fibrillation.
Statins
(HMG-CoA Reductase Inhibitors)
Cholesterol Lowering drugs:
1. Statins
2. Resins
3. Nicotinic acid (Niacin),
______________________
Gemfibrozil
Clofibrate
Lovastatin (Mevacor)
Pravastatin (Pravachol)
Simvastatin (Zocor)
Amlodipine / Atorvastatin) (Caduet)
Rosuvastatin (Crestor)
Fluvastatin - (Lescol)
Atorvastatin (Lipitor)
Ezetimibe / Simvastatin (Vytorin)
Statins are drugs that can lower your
cholesterol.
They work by blocking a substance your
body needs to make cholesterol.
Statins may also help your body
reabsorb cholesterol that has built up in
plaques on your artery walls, preventing
further blockage in your blood vessels
and heart attacks.
Side effects
Muscle and joint aches (most common)
Nausea
Diarrhea
Constipation
Liver damage
o Gemfibrozil and Niacin, increase
the risk of liver problems when
combined with Statins -
o Monitor LFTs
Muscle problems
o Statin Myopathy
o Rhabdomyolysis
o Myoglobin can damage your
kidneys.
Certain drugs when taken with Statins can
increase the risk of Rhabdomyolysis. These
include Gemfibrozil, Erythromycin, antifungal
medications, Nefazodone, Cyclosporine and
Niacin.
S-ar putea să vă placă și
- Cardiovascular PANCE Review GuideDocument11 paginiCardiovascular PANCE Review GuidePhysician Assistant Review100% (1)
- PANCE Prep Pearls Cardio Questions PDFDocument9 paginiPANCE Prep Pearls Cardio Questions PDFkat100% (3)
- Rosh ReviewDocument125 paginiRosh ReviewPrince Du100% (2)
- Pance Prep Pearls AntibioticsDocument14 paginiPance Prep Pearls Antibioticskat100% (4)
- 750 Flashcard Questions PAPrep Copy 2 2Document54 pagini750 Flashcard Questions PAPrep Copy 2 2Mary Anne Lerma- PetersonÎncă nu există evaluări
- EENT PANCE and PANRE Content Blueprint Patient PresentationsDocument8 paginiEENT PANCE and PANRE Content Blueprint Patient PresentationsThe Physician Assistant LifeÎncă nu există evaluări
- PANCE Prep Pearls Valvular DiseaseDocument4 paginiPANCE Prep Pearls Valvular Diseasekat100% (2)
- PANCE Pearls Master 2013Document19 paginiPANCE Pearls Master 2013Haley Shields100% (7)
- Peds EORDocument17 paginiPeds EORRachel BarrosÎncă nu există evaluări
- Internal Med EORDocument57 paginiInternal Med EORAndrew BowmanÎncă nu există evaluări
- Pance Review Q&ADocument40 paginiPance Review Q&ABetsy Issac Pidugu100% (2)
- Clinical Medicine Cheat Sheet Ebook PDFDocument18 paginiClinical Medicine Cheat Sheet Ebook PDFMokaÎncă nu există evaluări
- Medgeeks: Pharmacology Cheat SheetsDocument13 paginiMedgeeks: Pharmacology Cheat Sheetsiuliaign100% (1)
- PANCE Word AssociationDocument27 paginiPANCE Word Associationt2091100% (2)
- Rutger's PANRE and PANCE Practice Questions 1 of 2Document35 paginiRutger's PANRE and PANCE Practice Questions 1 of 2nubianlocks100% (3)
- PANRE and PANCE Review Antimicrobial PharmacologyDocument27 paginiPANRE and PANCE Review Antimicrobial PharmacologyThe Physician Assistant Life100% (2)
- Class III-V EVS PDFDocument138 paginiClass III-V EVS PDFAnji KaringuÎncă nu există evaluări
- Dazai, Osamu - No Longer Human (1973)Document3 paginiDazai, Osamu - No Longer Human (1973)Stefan BoleaÎncă nu există evaluări
- Torsade De Pointes, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDe la EverandTorsade De Pointes, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsÎncă nu există evaluări
- Heart Valve Diseases, A Simple Guide to These ConditionsDe la EverandHeart Valve Diseases, A Simple Guide to These ConditionsÎncă nu există evaluări
- EKG and ECG Interpretation: Learn EKG Interpretation, Rhythms, and Arrhythmia Fast!De la EverandEKG and ECG Interpretation: Learn EKG Interpretation, Rhythms, and Arrhythmia Fast!Încă nu există evaluări
- Congenital Heart Diseases, A Simple Guide to these Medical ConditionsDe la EverandCongenital Heart Diseases, A Simple Guide to these Medical ConditionsÎncă nu există evaluări
- Stud TabDocument34 paginiStud Tabjrubin83669Încă nu există evaluări
- Pneumonia and ID PANCE ReviewDocument107 paginiPneumonia and ID PANCE ReviewFlora Lawrence100% (1)
- Sample Questions and CritiquesDocument14 paginiSample Questions and CritiquesaayceeÎncă nu există evaluări
- Cardiology - Pericardial Disease PDFDocument1 paginăCardiology - Pericardial Disease PDFPshtiwan MahmoodÎncă nu există evaluări
- Surgery EORDocument76 paginiSurgery EORAndrew BowmanÎncă nu există evaluări
- PA - Coursepack DAY 1Document352 paginiPA - Coursepack DAY 1Elly NuñezÎncă nu există evaluări
- Clinicial Thinking and Test Taking PANRE and PANCEDocument12 paginiClinicial Thinking and Test Taking PANRE and PANCEThe Physician Assistant Life100% (2)
- Word AssociationDocument27 paginiWord AssociationMilan Kolovrat100% (1)
- PANCE Prep Pearls Valvular Disease PDFDocument4 paginiPANCE Prep Pearls Valvular Disease PDFkatÎncă nu există evaluări
- PANRE and PANCE Review Infectios DiseaseDocument32 paginiPANRE and PANCE Review Infectios DiseaseThe Physician Assistant Life100% (1)
- Chapter 1 CardiologyDocument48 paginiChapter 1 CardiologyAnh100% (2)
- PANRE and PANCE Review Emergency MedicineDocument15 paginiPANRE and PANCE Review Emergency MedicineThe Physician Assistant Life100% (2)
- Sources: CardiovascularDocument117 paginiSources: CardiovascularMohannad AlfadhalÎncă nu există evaluări
- PANCE - Cardio Review 2020Document50 paginiPANCE - Cardio Review 2020Siam100% (1)
- Clin Med For PAsDocument32 paginiClin Med For PAsMaryNguyen100% (2)
- Internal Medicine NotesDocument54 paginiInternal Medicine NotesKiara Govender100% (1)
- Antimicrobial PANCE ReviewDocument40 paginiAntimicrobial PANCE ReviewFlora LawrenceÎncă nu există evaluări
- Panre and Pance Review Cardiovascular IIDocument26 paginiPanre and Pance Review Cardiovascular IIThe Physician Assistant Life100% (1)
- Soap TemplateDocument3 paginiSoap TemplaterohitÎncă nu există evaluări
- Questions: Questions All Things Pa-C - Free Practice QuizDocument12 paginiQuestions: Questions All Things Pa-C - Free Practice QuizJaellah MatawaÎncă nu există evaluări
- PANRE and PANCE Review NeurologyDocument15 paginiPANRE and PANCE Review NeurologyThe Physician Assistant Life60% (5)
- Preparing For The PANCEDocument46 paginiPreparing For The PANCEJay plÎncă nu există evaluări
- Peds EORDocument29 paginiPeds EORAndrew BowmanÎncă nu există evaluări
- Antibiotics ChartDocument10 paginiAntibiotics Chartadom09Încă nu există evaluări
- Medicine1 Grand PE ScriptDocument10 paginiMedicine1 Grand PE ScriptCarmeline Santi BeronillaÎncă nu există evaluări
- Internal Medicine End of Rotation QuestionsDocument4 paginiInternal Medicine End of Rotation Questionskt_one100% (1)
- Chapter 1 Cardiology PDFDocument48 paginiChapter 1 Cardiology PDFkatÎncă nu există evaluări
- PANRE and PANCE Review PsychologyDocument35 paginiPANRE and PANCE Review PsychologyThe Physician Assistant LifeÎncă nu există evaluări
- ED Study GuideDocument59 paginiED Study Guidemmmmz100% (1)
- Physician Assistant Cover Letter SampleDocument1 paginăPhysician Assistant Cover Letter SampleThe Physician Assistant LifeÎncă nu există evaluări
- Mksap NotesDocument64 paginiMksap NotesobishtÎncă nu există evaluări
- Rheumatology: Internal Medicine Board Review FlashcardsDocument55 paginiRheumatology: Internal Medicine Board Review FlashcardsJoyee BasuÎncă nu există evaluări
- PANCE - Endo Review 2020Document56 paginiPANCE - Endo Review 2020Siam100% (1)
- Common Cardiac Related MedicationsDocument18 paginiCommon Cardiac Related MedicationsTracy100% (2)
- PANRE and PANCE Review Cardiovascular IDocument21 paginiPANRE and PANCE Review Cardiovascular IThe Physician Assistant LifeÎncă nu există evaluări
- OMedEd - Cardiology - CAD PDFDocument2 paginiOMedEd - Cardiology - CAD PDFJohn DoeÎncă nu există evaluări
- A History of Magic (Player's Handbook)Document92 paginiA History of Magic (Player's Handbook)Jack SteadÎncă nu există evaluări
- Microscopic ExaminationDocument72 paginiMicroscopic ExaminationbubblyeivinejÎncă nu există evaluări
- Lecture 3, Principles of Cavity Preparation IDocument23 paginiLecture 3, Principles of Cavity Preparation IJustDen09100% (3)
- Stem CellDocument14 paginiStem CellsattwikaÎncă nu există evaluări
- 40 Amazing Facts About The Human BodyDocument2 pagini40 Amazing Facts About The Human BodyDr.Eswara Reddy Siddareddy100% (2)
- Circularsdear KidsDocument18 paginiCircularsdear KidskrishnaÎncă nu există evaluări
- DinasauresDocument38 paginiDinasauresAnnette Meyer100% (2)
- Hyperthermia and PregnancyDocument10 paginiHyperthermia and PregnancyAnnisa Nurfiatul AiniÎncă nu există evaluări
- PPK ILMU PENYAKIT PerinatologiDocument31 paginiPPK ILMU PENYAKIT PerinatologiRico AndreawanÎncă nu există evaluări
- Dentinogenesis (AuthorV Mazuru)Document40 paginiDentinogenesis (AuthorV Mazuru)Octavian DavidsonÎncă nu există evaluări
- Can De-Extinction Science Save The Javan or Sumatran Rhinos?Document10 paginiCan De-Extinction Science Save The Javan or Sumatran Rhinos?peilingganÎncă nu există evaluări
- Dragonary - Breeding GuideDocument7 paginiDragonary - Breeding GuideJhay ReoÎncă nu există evaluări
- Toki PonaDocument53 paginiToki PonaHannahÎncă nu există evaluări
- Makhraj Student HandoutsDocument50 paginiMakhraj Student HandoutsZakia Rehman100% (1)
- Food Borne DiseasesDocument29 paginiFood Borne DiseasesDr.Kedar Karki ,M.V.Sc.Preventive Vet.Medicine CLSU Philippines67% (6)
- Dallas Morning News PDF Version Page 1Document1 paginăDallas Morning News PDF Version Page 1api-213784103Încă nu există evaluări
- Ecology AND Environment: RA IA SDocument32 paginiEcology AND Environment: RA IA SMikuÎncă nu există evaluări
- New Text DocumentDocument63 paginiNew Text DocumentKiran TemkarÎncă nu există evaluări
- Periorbital and Orbital CellulitisDocument51 paginiPeriorbital and Orbital CellulitisJoanne BlancoÎncă nu există evaluări
- Maria Animal BookDocument23 paginiMaria Animal Bookapi-275466952Încă nu există evaluări
- History and P.E. of The Integumentary SystemDocument6 paginiHistory and P.E. of The Integumentary SystempazucenaÎncă nu există evaluări
- Ad5 Britanico Gold RT Dec 2022Document1 paginăAd5 Britanico Gold RT Dec 2022Luis Alberto Jaramillo SantillanÎncă nu există evaluări
- E - The ZooDocument4 paginiE - The ZooZabrina LuiÎncă nu există evaluări
- Cilia and FlagellaDocument4 paginiCilia and FlagellaAnurag chavan100% (1)
- Lecture #13 - Finish Sexual Selection & Genetic DriftDocument63 paginiLecture #13 - Finish Sexual Selection & Genetic DriftJenny ZhangÎncă nu există evaluări
- Introduction To Shareera Kriya PhysiologyDocument2 paginiIntroduction To Shareera Kriya PhysiologyRoshan BaskotaÎncă nu există evaluări
- Dysfunctional Uterine Bleeding History CollectionDocument4 paginiDysfunctional Uterine Bleeding History CollectionAnitha BalakrishnanÎncă nu există evaluări
- ProiecttDocument4 paginiProiecttAdriana Elena DoneÎncă nu există evaluări