Documente Academic
Documente Profesional
Documente Cultură
Nonoperative Management of Appendiceal Phlegmon or Abscess With An Appendicolith in Children
Încărcat de
Patrick John0 evaluări0% au considerat acest document util (0 voturi)
81 vizualizări5 paginiNonoperative Management
Titlu original
Nonoperative Management of Appendiceal Phlegmon or Abscess With an Appendicolith in Children
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentNonoperative Management
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
81 vizualizări5 paginiNonoperative Management of Appendiceal Phlegmon or Abscess With An Appendicolith in Children
Încărcat de
Patrick JohnNonoperative Management
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 5
ORIGINAL ARTICLE
Nonoperative Management of Appendiceal Phlegmon
or Abscess with an Appendicolith in Children
Hai-Lan Zhang & Yu-Zuo Bai & Xin Zhou & Wei-Lin Wang
Received: 18 October 2012 / Accepted: 2 January 2013 / Published online: 12 January 2013
#2013 The Society for Surgery of the Alimentary Tract
Abstract
Background The optimal treatment of appendiceal phlegmon or abscess with an appendicolith is controversial. This study
aimed to evaluate outcomes and prognosis of nonoperative management of appendiceal phlegmon or abscess with an
appendicolith in children.
Methods From 2007 to 2011, 105 children with appendiceal phlegmon or abscess who were treated nonoperatively without
interval appendectomy were reviewed. Average follow-up of subjects was 2.4 years. Data were compared between subjects
with and without an appendicolith or persistent presence and disappearance of an appendicolith.
Results The success rate for nonoperative therapy for appendiceal phlegmon or abscess with appendicolith was 95.9 %. The
risk of recurrent appendicitis in appendiceal phlegmon or abscess with appendicolith (19.1 %) was higher than that without
appendicolith (8.9 %, P=0.132). The rate of appendicolith disappearance during follow-up was 80.9 %. The persistent
presence of an appendicolith was associated with a significantly higher recurrence rate (66.7 %) compared with appendicolith
disappearance (7.9 %, P<0.05).
Conclusion Appendiceal phlegmon or abscess with an appendicolith can be managed nonoperatively, and most appendico-
liths can be resolved. Persistent presence of an appendicolith is a significant risk factor for recurrent appendicitis. Interval
appendectomy is recommended for persistent presence of appendicolith, but is not indicated in cases without appendicolith or
appendicolith disappearance.
Keywords Appendiceal Phlegmon
.
Appendiceal Abscess
.
Appendicolith
.
Nonoperative Management
.
Children
Introduction
The symptoms and physical signs of acute appendicitis may
overlap with other gastrointestinal or genitourinary diseases
leading to a missed or delayed clinical diagnosis, especially
in children. The appendiceal phlegmon or abscess (APA) at
presentation occurs in about 30 to 60 % of children.
1, 2
The
presence of an appendicolith is closely associated with
APA.
3
Current researches on APA with an appendicolith
are rare and controversial. The debates predominantly focus
on the effects of an appendicolith, the success rate of nonop-
erative management, and the necessity of interval appendec-
tomy (IA). The presence of an appendicolith might predict
failure of nonoperative management of APA, and immediate
appendectomy may be a better choice.
4
However, some stud-
ies found no correlation between clinical outcomes and the
presence of appendicolith.
5
Recent studies
6, 7
indicated that an
appendicolith was a risk factor for recurrent appendicitis and
patients should receive IA; however, immediate appendecto-
my was not suggested considering the difficulty of technique
associated with appendectomy before the inflammatory pro-
cess completely subsided and the relatively mild course of
recurrent appendicitis.
It is important to study the relationship of APA with an
appendicolith in order to understand the clinical outcomes
of nonoperative treatment and the necessity of IA to prevent
recurrence. To our knowledge, confirming the persistent
presence or disappearance of appendicolith in APA by sub-
sequent computed tomography (CT) scans and development
of recurrent appendicitis has not been systematically
H.-L. Zhang
:
Y.-Z. Bai
:
X. Zhou
:
W.-L. Wang (*)
Department of Pediatric Surgery, Shengjing Hospital of China
Medical University, No. 36 Sanhao St., Heping District, Shenyang,
China 110004
e-mail: wangwl@sj-hospital.org
J Gastrointest Surg (2013) 17:766770
DOI 10.1007/s11605-013-2143-3
reported. The purposes of this study were to evaluate the
outcomes and prognosis of nonoperative treatment of APA
with an appendicolith in children, with emphasis on the
success rate and the need for IA.
Patients and Methods
This retrospective study was approved by the Ethics Com-
mittee at Shengjing Hospital of China Medical University.
From January 2007 to December 2011, 170 pediatric
patients (14 years old) presented to our hospital with a
clinical diagnosis of APA. Among them, 48 were treated by
immediate appendectomy or surgical drainage because of
extensive peritonitis, apparent intestinal obstruction, and
shorter duration of symptoms (3 days). Another 122 chil-
dren with APA who underwent attempted initial nonopera-
tive treatment were reviewed. Exclusion criteria included
children with incomplete follow-up and interval appendec-
tomy after successful nonoperative management. A total of
105 patients met the study criteria. Data collected included
demographics, duration of symptoms, common symptoms
(e.g., pain, fever, vomiting, diarrhea), physical signs (e.g.,
tenderness, rebound, rigidity), white blood cell (WBC)
counts, C-reactive protein (CRP) values, antibiotics admin-
istered, length of stay (LOS), ultrasonography (USG), and
CT scan findings.
CT scans were performed on a Siemens Sensation 64 CT
(Siemens Medical Solutions, Forchheim, Germany) or a Phi-
lips Brilliance 64 CT (Philips Medical Systems, Cleveland,
USA). In order to decrease childrens exposure to radiation,
our hospital keeps the radiation dose as low as possible
without comprising the quality of CTimages. Periappendiceal
abscesses were not generally drained unless the condition of
patients did not improve or abscesses gradually increased.
Nonoperative therapy was considered a failure in those
patients who received appendectomy during the initial hospi-
talization for nonsurgical therapy because of the deterioration
of clinical symptoms and signs or intestinal obstruction.
Based on the presence or absence of an appendicolith on
admission CT imaging, children were divided into two
groups: 49 patients with appendicolith (AC group) and 56
patients with no appendicolith (NA group). The conserva-
tively treated patients were given intravenous, broad-
spectrum antibiotics, and intrarectal suppositories (gentami-
cin and metronidazole). The therapy was continued for at
least 7 days. When the patients improved, USG or CT was
again performed and reexamined. The absence of an appen-
dicolith must be confirmed by CT imaging, even if USG
indicated no appendicolith of the appendix. If regression of
appendiceal inflammation was seen on USG or CT and
patients remained afebrile, with improved physical signs
and lower WBC and CRP, they were discharged home with
oral broad-spectrum antibiotics. The patients returned to our
pediatric clinic after 1, 2, and 3 or 4, 6, and 12 months,
respectively. After the first year, the patients were examined
once every year. Each child was followed for an average of
2.4 years in our clinic.
Statistical Analysis
Data are presented as mean standard deviation. The sta-
tistical analyses were performed using Students t test or chi-
square test with Fishers exact examination. A P value of
less than 0.05 was considered as significant. The statistical
calculations were performed using SPSS software version
13.0 (SPSS Inc., Chicago, IL, USA).
Results
Among 105 children who met the study criteria, 49 children
in the AC group and 56 in the NA group were treated
nonsurgically. The AC group included 24 males and 25
females with an average age of 7.13.7 years. The NA
group included 30 males and 26 females with an average
age of 6.43.5 years. Results are summarized in Table 1.
In the AC group, duration of symptoms was 9.3
4.8 days. No significant differences were found between
the AC and NA groups when comparing common symp-
toms such as abdominal pain (100 vs. 100 %), fever (81.6
vs. 80.4 %), vomiting (51.0 vs. 64.3 %), and diarrhea (42.9
vs. 37.5 %). Excluding two children who underwent appen-
dectomy because of intestinal obstruction, LOS was 12.5
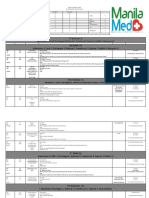
Table 1 Clinical data between the AC group and NA group
AC (n=49) NA (n=56) P value
Sex (male/female) 24:25 15:13 0.639
Age (years) 7.13.7 6.43.5 0.316
Duration of symptoms 9.34.8 8.43.6 0.239
Pain 49 (100 %) 56 (100 %) 1.000
Fever 40 (81.6 %) 45 (80.4 %) 0.868
Localized peritonitis 35 (71.4 %) 3 1(55.4 %) 0.089
WBC 20.25.4 17.65.2 0.063
CRP 122.966.7 101.764.6 0.102
Inflammatory area (cm
2
) 34.523.4 26.618.8 0.062
Percutaneous drainage 2 (4.1 %) 1 (1.8 %) 0.597
LOS (excluding
appendectomy)
12.56.0 11.63.9 0.323
Overall success 47 (95.9 %) 56 (100 %) 0.215
Recurrent appendicitis
(excluding appendectomy)
9/47 (19.1 %) 5/56 (8.9 %) 0.132
AC appendicolith, NA no appendicolith
J Gastrointest Surg (2013) 17:766770 767
6.0 days in the AC group. The rate of localized peritonitis
was slightly higher in the AC group (71.4 %) than in the NA
group (55.4 %). Similarly, WBC (20.25.4 vs. 17.65.2)
and CRP (122.966.7 vs. 101.764.6) values were slightly
higher and mean inflammatory areas of APA (34.523.4 vs.
26.618.8) on USG or CT scan were slightly larger in the
AC group compared to those in the NA group. However,
these data did not reach statistical significance. Two patients
in the AC and one patient in the NA group underwent CT-
guided percutaneous drainage and received successful con-
servative therapy.
In the AC group, two children underwent appendectomy
and surgical drainage because of aggravated intestinal ob-
struction occurring between 8 and 12 days after initial
nonsurgical management. All children in the NA group were
treated successfully with nonoperative treatment. There
were no statistically significant differences between the
AC and NA groups (95.9 vs. 100 %) in the overall success
rate for nonoperative management of APA.
All children were followed up for an average of 2.4 years
(range, 0.5 to 5.5 years). There was no significant difference in
the average follow-up time between the NA and AC groups
(2.51.4 vs. 2.21.5, P=0.358). Five patients had recurrent
appendicitis in the NA group between 2 months and 2 years
after initial conservative treatment. Of these, one patient had
another APA and was treated nonoperatively again, receiving
IAafter 3 months. In the ACgroup, nine patients had recurrent
appendicitis between 1 and 10 months after initial treatment.
Of these, four children had another APA. Two patients with
second APAs received appendectomy immediately, whereas
the remaining two patients had IA between 2 and 3 months
after another course of conservative treatment. Two cases had
appendicoliths outside the appendix in the appendectomy. The
risk of recurrence in the AC group (19.1 %) was higher than
that in the NA group (8.9 %), but without statistical
significance.
In the AC group, the appendicolith disappeared in 38
children and presented persistently in APA in nine children
during the follow-up period. Excluding two patients who
underwent appendectomy because of intestinal obstruction,
the rate of disappeared appendicolith was 80.9 %. Based on
whether appendicolith disappeared or persisted, the patients
in the AC group were divided into two subgroups: appendi-
colith disappearance and appendicolith persistent presence.
Among the appendicolith disappearance group, 57.9 % of
appendicoliths (22/38) disappeared during the initial hospital-
ization (Figs. 1 and 2). The earliest appendicolith resolution
was the fourth day of conservative management, while most
appendicoliths resolved within 614 days. The disappearance
of an appendicolith in 15 children was found in the first month
of follow-up and another appendicolith disappeared in the
fourth month of follow-up (Fig. 3). Under similar circum-
stances of age, symptomatic duration and mean inflammatory
area, risk of localized peritonitis, WBC and CRP values, and
LOS were slightly higher in the appendicolith persistent pres-
ence subgroup than in the appendicolith disappearance sub-
group (Table 2). Three patients with appendicolith
disappearance had recurrent appendicitis, for a 7.9 % recur-
rence rate. However, two patients with persistent appendico-
lith had recurrent appendicitis and four recurrent APAs. The
Fig. 1 a The admission CT
scan of a 13-year-old boy
showed an appendiceal phleg-
mon formation and a dilated
appendix with an appendicolith.
b An appendicolith disappeared
after 12 days of nonoperative
management
Fig. 2 a The initial CT image with intravenous contrast medium of a
2-year-old girl showed an appendicolith within a multilocular appen-
diceal abscess. b Intravenous contrast CT scan revealed that the
appendiceal abscess was absorbed and the appendicolith was resolved
after 17 days of nonoperative management
768 J Gastrointest Surg (2013) 17:766770
persistent presence of an appendicolith was associated with a
significantly higher rate of recurrent appendicitis (66.7 %)
compared with appendicolith disappearance, representing a
statistically significant difference (P<0.05).
Discussion
An appendicolith, or fecalith, is composed of inspissated fecal
material, mucus with entrapped calcium phosphate, and inor-
ganic salts. With the increased use of CT scans, the appendi-
coliths are detected in 40 to 50 %of children who present with
a clinical suspicion of acute appendicitis.
8, 9
The appendicolith
has long been implicated as an important cause of acute
appendicitis, especially in APA.
10, 11
Current surgical guide-
lines advise nonoperative management of APA in children.
However, the optimal treatment of APAwith an appendicolith
is not well established.
When an appendicolith is present in APA, it was believed
to predict failure of conservative therapy and immediate
appendectomy was suggested.
4
However, in our review of
children with an appendicolith in APA, the success rate of
nonoperative treatment was 95.9 %, without a statistically
significant difference compared to the NA group. This
indicates that APA with an appendicolith can be nonsurgi-
cally managed and immediate appendectomy is not neces-
sary. Our results are consistent with other studies of APA in
children,
1214
and immediate appendectomy might encoun-
ter difficulties because of distorted anatomy, inflammatory
adhesion, closing the appendiceal stump, and severe post-
operative complications.
During the mean 2.4 years of follow-up, the recurrence
rate of the AC group was 19.1 %. This is similar to previous
research on the mean risk of recurrent appendicitis after the
conservative management of APA in children.
15
In our
research, the recurrence rate was slightly higher compared
to that of the NA group but without statistical significance.
During the follow-up period, we were surprised that the
higher recurrence rate was closely associated with the per-
sistent presence of an appendicolith in APA, but not with its
disappearance.
In the AC group, the appendicolith disappeared on sub-
sequent CT scans in 38 of 47 children who had the presence
of appendicolith on admission CT exams. Among them, the
appendicoliths of 22 (57.9 %) patients were absent at the
end of the initial hospitalization. Until first month of follow-
up, 97.4 % (37/38) of appendicoliths were resolved. Hence,
the first month of follow-up was vital when the patient was
discharged with the presence of appendicolith at last reex-
amination. The interesting aspect was that the appendicolith
in APA most likely resolved spontaneously just as in simple
appendicitis or normal appendix.
10
The appendicolith still
existed in the appendiceal lumen even if the appendix in
most cases had perforated with APA. As seen in our results,
the perforated appendix should likely be able to expel an
appendicolith from its lumen depending on peristaltic
movement.
The rate of recurrent appendicitis after appendicolith
disappearance was 7.9 %, which was similar to the recur-
rence rate of the NA group. Several reviews also indicated
that IA was not necessary because of a lower recurrence
rate.
1517
When IA is performed, patients are exposed to an
1118 % complication risk in order to prevent a recurrence
of appendicitis in less than 10 % of patients.
17, 18
Also,
patients who experience recurrent appendicitis usually
Fig. 3 a The initial intravenous contrast image of a 7-year-old boy
showed an appendicolith within the multilocular gas-containing appen-
diceal abscess with an enhancing rim. b The abscess was smaller and
the appendicolith was still present on contrast-enhanced image after
7 days when he was discharged. c The inflammatory change of the
right lower quadrant and the appendicolith disappeared on the CT scan
at the fourth month of follow-up
Table 2 Clinical data between the appendicolith persistent presence
subgroup and appendicolith disappearance subgroup
APs (n=9) ADs (n=38) P value
Age (years) 6.73.5 7.33.7 0.682
Duration of symptoms 9.75.3 9.44.8 0.904
Localized peritonitis 8 (88.9 %) 25 (65.8 %) 0.244
WBC 22.23.4 19.95.8 0.258
CRP 143.577.0 116.959.7 0.262
Inflammatory area (cm
2
) 34.621.0 34.224.7 0.960
LOS 16.19.9 11.74.5 0.223
Recurrent appendicitis 6 (66.7 %) 3 (7.9 %) 0.001*
APs appendicolith persistent presence subgroup, ADs appendicolith
disappearance subgroup
*P<0.05
J Gastrointest Surg (2013) 17:766770 769
exhibit a milder clinical course at recurrence.
19
In the no
appendicolith and appendicolith disappearance groups, only
one child had another APA and IA after receiving conser-
vative management again. The other children with recurrent
appendicitis received appendectomy immediately with zero
morbidity.
Nine children in our series had persistent presence of an
appendicolith during the follow-up period. Among them,
two patients had recurrent appendicitis and four had recur-
rent APA. The recurrence rate was 66.7 % in the appendi-
colith persistent presence subgroup, which was a 8.4 relative
risk (66.7 vs. 7.9 %) for recurrent appendicitis compared
with the appendicolith disappearance with APA, and recur-
rent APAwas accounting for 66.7 %. The four children with
recurrent APA returned on months 3, 4, 3, and 7, respec-
tively. This indicated that IA was able to prevent recurrent
complicated appendicitis because the recurrence was often
after 3 months of initial conservative management. These
data suggest that the persistent presence of an appendicolith
increases recurrent risk in children with APA. IA was rec-
ommended to prevent recurrence in patients with persistent
presence of appendicolith in APA.
Our study has some limitations. One limitation is that the
data were retrospectively collected. This may have resulted
in some degree of bias. Another limitation is that the number
of patients with persistent appendicolith was lower than
expected because most cases resolved. Further large-scale,
prospective trials are needed to validate our conclusion
about the optimal treatment of APA with an appendicolith.
Conclusion
APA with an appendicolith can be managed nonoperatively
without immediate appendectomy. Most appendicoliths pres-
ent on admission CT scans will resolve. The persistent pres-
ence of an appendicolith rather than appendicolith presence
alone was a significant risk factor for recurrent appendicitis in
APA. IA was recommended for the persistent presence of an
appendicolith in APA, but IA is not indicated in APA cases
without appendicolith or disappearance of appendicolith.
References
1. Nance ML, Adamson WT, Hedrick HL. Appendicitis in the young
child: a continuing diagnostic challenge. Pediatr Emerg Care
2000;16:160162.
2. Pearl RH, Hale DA, Molloy M, Schutt DC, Jaques DP. Pediatric
appendectomy. J Pediatr Surg 1995;30:173178.
3. Alaedeen DI, Cook M, Chwals WJ. Appendiceal fecalith is asso-
ciated with early perforation in pediatric patients. J Pediatr Surg
2008;43:889892.
4. Aprahamian CJ, Barnhart DC, Bledsoe SE, Vaid Y, Harmon CM.
Failure in the nonoperative management of pediatric ruptured
appendicitis: predictors and consequences. J Pediatr Surg
2007;42:934938.
5. Levin T, Whyte C, Borzykowski R, Han B, Blitman N, Harris B.
Nonoperative management of perforated appendicitis in children:
can CT predict outcome? Pediatr Radiol 2007;37:251255.
6. Tsai HM, Shan YS, Lin PW, Lin XZ, Chen CY. Clinical analysis of
the predictive factors for recurrent appendicitis after initial nonop-
erative treatment of perforated appendicitis. Am J Surg
2006;192:311316.
7. Ein SH, Langer JC, Daneman A. Nonoperative management of
pediatric ruptured appendix with inflammatory mass or abscess:
presence of an appendicolith predicts recurrent appendicitis. J
Pediatr Surg 2005;40:16121615.
8. Friedland JA, Siegel MJ. CT appearance of acute appendicitis in
childhood. AJR Am J Roentgenol 1997;168:439442.
9. Lowe LH, Penney MW, Scheker LE, Perez R Jr, Stein SM, Heller
RM, Shyr Y, Hernanz-Schulman M. Appendicolith revealed on CT
in children with suspected appendicitis: how specific is it in the
diagnosis of appendicitis? AJR Am J Roentgenol 2000;175:981
984.
10. Rabinowitz CB, Egglin TK, Beland MD, Mayo-Smith WW.
Outcomes in 74 patients with an appendicolith who did not
undergo surgery: is follow-up imaging necessary? Emerg Radiol
2007;14:161165.
11. Williams RF, Blakely ML, Fischer PE, Streck CJ, Dassinger MS,
Gupta H, Renaud EJ, Eubanks JW, Huang EY, Hixson SD,
Langham MR. Diagnosing ruptured appendicitis preoperatively
in pediatric patients. J Am Coll Surg 2009;208:819825.
12. Roach JP, Partrick DA, Bruny JL, Allshouse MJ, Karrer FM,
Ziegler MM. Complicated appendicitis in children: a clear role
for drainage and delayed appendectomy. Am J Surg
2007;194:769772.
13. Gillick J, Velayudham M, Puri P. Conservative management of
appendix mass in children. Br J Surg 2001;88:15391542.
14. Erdoan D, Karaman I, Narci A, Karaman A, Cavuolu YH,
Aslan MK, Cakmak O. Comparison of two methods for the man-
agement of appendicular mass in children. Pediatr Surg Int
2005;21:8183.
15. Hall NJ, Jones CE, Eaton S, Stanton MP, Burge DM. Is interval
appendicectomy justified after successful nonoperative treatment
of an appendix mass in children? A systematic review. J Pediatr
Surg 2011;46:767771.
16. Meshikhes AW. Management of appendiceal mass: controversial
issues revisited. J Gastrointest Surg 2008;12:767775.
17. Andersson RE, Petzold MG. Nonsurgical treatment of appendiceal
abscess or phlegmon: a systematic review and meta-analysis. Ann
Surg 2007;246:741748.
18. Willemsen PJ, Hoorntje LE, Eddes EH, Ploeg RJ. The need for
interval appendectomy after resolution of an appendiceal mass
questioned. Dig Surg 2002;19:216220.
19. Dixon MR, Haukoos JS, Park IU, Oliak D, Kumar RR, Arnell TD,
Stamos MJ. An assessment of the severity of recurrent appendici-
tis. Am J Surg 2003;186:718722.
770 J Gastrointest Surg (2013) 17:766770
S-ar putea să vă placă și
- Census August2 - August 3, 2020Document5 paginiCensus August2 - August 3, 2020Patrick JohnÎncă nu există evaluări
- Census August 26 - August 27, 2020Document5 paginiCensus August 26 - August 27, 2020Patrick JohnÎncă nu există evaluări
- Census August 30 - August 31, 2020Document6 paginiCensus August 30 - August 31, 2020Patrick JohnÎncă nu există evaluări
- Hospital Daily Census August 18-19Document5 paginiHospital Daily Census August 18-19Patrick JohnÎncă nu există evaluări
- Census August 22 - August 23, 2020Document5 paginiCensus August 22 - August 23, 2020Patrick JohnÎncă nu există evaluări
- Census August 28 - August 29, 2020Document5 paginiCensus August 28 - August 29, 2020Patrick JohnÎncă nu există evaluări
- Census August 24 - August 25, 2020Document6 paginiCensus August 24 - August 25, 2020Patrick JohnÎncă nu există evaluări
- Census August 16 - August 17, 2020Document5 paginiCensus August 16 - August 17, 2020Patrick JohnÎncă nu există evaluări
- Census August 20 - August 21, 2020Document5 paginiCensus August 20 - August 21, 2020Patrick JohnÎncă nu există evaluări
- Census August 22 - August 23, 2020Document5 paginiCensus August 22 - August 23, 2020Patrick JohnÎncă nu există evaluări
- Census August 20 - August 21, 2020Document5 paginiCensus August 20 - August 21, 2020Patrick JohnÎncă nu există evaluări
- Census August 22 - August 23, 2020Document5 paginiCensus August 22 - August 23, 2020Patrick JohnÎncă nu există evaluări
- Census August 16 - August 17, 2020Document5 paginiCensus August 16 - August 17, 2020Patrick JohnÎncă nu există evaluări
- Census August 24 - August 25, 2020Document6 paginiCensus August 24 - August 25, 2020Patrick JohnÎncă nu există evaluări
- Census August 12 - August 13, 2020Document6 paginiCensus August 12 - August 13, 2020Patrick JohnÎncă nu există evaluări
- Census August 8 - August 9, 2020Document6 paginiCensus August 8 - August 9, 2020Patrick JohnÎncă nu există evaluări
- Census August 14 - August 15, 2020Document6 paginiCensus August 14 - August 15, 2020Patrick JohnÎncă nu există evaluări
- Census August 16 - August 17, 2020Document5 paginiCensus August 16 - August 17, 2020Patrick JohnÎncă nu există evaluări
- 9 Extension: (6) (Admission: 0 Card: 0 Discharged: 0 Referral: 0 Transferred: 0 Expired: 0 HAMA: 0 Abscond: 0Document5 pagini9 Extension: (6) (Admission: 0 Card: 0 Discharged: 0 Referral: 0 Transferred: 0 Expired: 0 HAMA: 0 Abscond: 0Patrick JohnÎncă nu există evaluări
- Hospital Daily Census August 18-19Document5 paginiHospital Daily Census August 18-19Patrick JohnÎncă nu există evaluări
- Census August 14 - August 15, 2020Document6 paginiCensus August 14 - August 15, 2020Patrick JohnÎncă nu există evaluări
- 9 Extension: (4) (Admission: 0 Card: 0 Discharged: 0 Referral: 0 Transferred: 0 Expired: 0 HAMA: 0 Abscond: 0Document6 pagini9 Extension: (4) (Admission: 0 Card: 0 Discharged: 0 Referral: 0 Transferred: 0 Expired: 0 HAMA: 0 Abscond: 0Patrick JohnÎncă nu există evaluări
- Daily admissions and discharges at Dr. Amante/Dr.Quitoy/Dr.Santos (March 30-31, 2021Document6 paginiDaily admissions and discharges at Dr. Amante/Dr.Quitoy/Dr.Santos (March 30-31, 2021Patrick JohnÎncă nu există evaluări
- Census August 12 - August 13, 2020Document6 paginiCensus August 12 - August 13, 2020Patrick JohnÎncă nu există evaluări
- Census August 10 - August 11, 2020Document6 paginiCensus August 10 - August 11, 2020Patrick JohnÎncă nu există evaluări
- Census August 6 - August 7, 2020Document6 paginiCensus August 6 - August 7, 2020Patrick JohnÎncă nu există evaluări
- 9 Extension: (3) (Admission: 0 Card: 0 Discharged: 0 Referral: 0 Transferred: 0 Expired: 0 HAMA: 0 Abscond: 0Document6 pagini9 Extension: (3) (Admission: 0 Card: 0 Discharged: 0 Referral: 0 Transferred: 0 Expired: 0 HAMA: 0 Abscond: 0Patrick JohnÎncă nu există evaluări
- 9 Extension: (5) (Admission: 0 Card: 0 Discharged: 0 Referral: 0 Transferred: 0 Expired: 0 HAMA: 0 Abscond: 0Document7 pagini9 Extension: (5) (Admission: 0 Card: 0 Discharged: 0 Referral: 0 Transferred: 0 Expired: 0 HAMA: 0 Abscond: 0Patrick JohnÎncă nu există evaluări
- 9 Extension: (4) (Admission: 0 Card: 0 Discharged: 0 Referral: 0 Transferred: 0 Expired: 0 HAMA: 0 Abscond: 0Document5 pagini9 Extension: (4) (Admission: 0 Card: 0 Discharged: 0 Referral: 0 Transferred: 0 Expired: 0 HAMA: 0 Abscond: 0Patrick JohnÎncă nu există evaluări
- 9 Extension: (9) (Admission: 0 Card: 0 Discharged: 0 Referral: 0 Transferred: 0 Expired: 0 HAMA: 0 Abscond: 0Document7 pagini9 Extension: (9) (Admission: 0 Card: 0 Discharged: 0 Referral: 0 Transferred: 0 Expired: 0 HAMA: 0 Abscond: 0Patrick JohnÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- HCCC ComplaintDocument23 paginiHCCC ComplaintPaul GallagherÎncă nu există evaluări
- Abu Dhabi DRGDocument62 paginiAbu Dhabi DRGDolly creationsÎncă nu există evaluări
- Chapter 15 - Hormones & Endocrine GlandsDocument17 paginiChapter 15 - Hormones & Endocrine Glandsapi-3728508100% (1)
- GetPdf Cgi PDFDocument9 paginiGetPdf Cgi PDFAKNTAI002Încă nu există evaluări
- Understanding-Ocd 2016 v2Document27 paginiUnderstanding-Ocd 2016 v2Samanjit Sen Gupta100% (1)
- Prescriptions On Asthma & APDDocument9 paginiPrescriptions On Asthma & APDeesha shahÎncă nu există evaluări
- How To Maintain Throat HygieneDocument9 paginiHow To Maintain Throat Hygieneankita singhÎncă nu există evaluări
- Cerebral Palsy Assessment ImportantDocument7 paginiCerebral Palsy Assessment Importantabra_arr100% (2)
- Medical certificate from Pantalan SHSDocument2 paginiMedical certificate from Pantalan SHSAngelo Villafranca67% (3)
- ImmunosuppresentsDocument13 paginiImmunosuppresentsmadeputraÎncă nu există evaluări
- Ann JeinaDocument7 paginiAnn JeinaMizumoriFumairaÎncă nu există evaluări
- Abnormal PuerperiumDocument65 paginiAbnormal PuerperiumNigus AfessaÎncă nu există evaluări
- Source Control in Emergency General SurgeryDocument21 paginiSource Control in Emergency General SurgerylaviniaÎncă nu există evaluări
- Pgmcet 2014-15 ListDocument6 paginiPgmcet 2014-15 ListEdward FieldÎncă nu există evaluări
- Dental Public HealthDocument264 paginiDental Public HealthCorina Manole DanielaÎncă nu există evaluări
- Kasus Farter 2 10 Mei 2019Document3 paginiKasus Farter 2 10 Mei 2019YonicaryanÎncă nu există evaluări
- PrimaquineDocument3 paginiPrimaquineVijayakumar NsÎncă nu există evaluări
- Myocardial InfarctionDocument18 paginiMyocardial InfarctionMarc Lorenz DucusinÎncă nu există evaluări
- Congestive Heart Failure, Pulmonary Edema, and CPAPDocument35 paginiCongestive Heart Failure, Pulmonary Edema, and CPAPSherwan R Shal100% (1)
- Community Health and Program Services (CHAPS) : Health Disparities Among Racial/Ethnic PopulationsDocument4 paginiCommunity Health and Program Services (CHAPS) : Health Disparities Among Racial/Ethnic PopulationsMuhammad Bachiar SafrudinÎncă nu există evaluări
- HEPATITIS B VACCINE NURSING RESPONSIBILITIESDocument14 paginiHEPATITIS B VACCINE NURSING RESPONSIBILITIESJannine BensiÎncă nu există evaluări
- Cardiology Case 1Document2 paginiCardiology Case 1vil62650% (2)
- 6 5 Nerves Hormones and HomeostasisDocument19 pagini6 5 Nerves Hormones and Homeostasisapi-235355872Încă nu există evaluări
- Sleep and The Risk of Chronic Kidney Disease: A Cohort StudyDocument8 paginiSleep and The Risk of Chronic Kidney Disease: A Cohort StudyEtaursaeÎncă nu există evaluări
- Buletin Farmasi 1/2014Document14 paginiBuletin Farmasi 1/2014afiq83100% (1)
- Choose 2 From The Disease Below That Are Emerging in The PhilippinesDocument4 paginiChoose 2 From The Disease Below That Are Emerging in The PhilippinesMICHELLE BIANCA PATRICE CRUZÎncă nu există evaluări
- Medication To Manage Abortion and MiscarriageDocument8 paginiMedication To Manage Abortion and MiscarriageNisaÎncă nu există evaluări
- Significance of Facebow Transfer: January 2020Document6 paginiSignificance of Facebow Transfer: January 2020Mahmoud Ibrahem maanÎncă nu există evaluări
- CNA Chapter 1 & 2 TermsDocument1 paginăCNA Chapter 1 & 2 TermsMarina ChakarÎncă nu există evaluări
- The Partograph: Dr. Rimonta F Gunanegara, SpogDocument30 paginiThe Partograph: Dr. Rimonta F Gunanegara, SpogHans Natanael PosoÎncă nu există evaluări