Documente Academic
Documente Profesional
Documente Cultură
OB Exam#1Studyguide
Încărcat de
Alvin L. RozierDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
OB Exam#1Studyguide
Încărcat de
Alvin L. RozierDrepturi de autor:
Formate disponibile
1
Unit 2: Day 1:
Anticipating Newborn Needs
o Premature infants-- may need respiratory care, may need to be
intubated, may need Surfactant (phosolipid produced by lungs to help
keep alveoli from collapsing on itself), they might need to be placed in
plastic bag for warmth, do we need to transfer mom to another facility?
Transition to Extrauterine Life:
o First period of reactivity- (lasts about 30 min)- newborn is very awake,
alert, active- good time to initiate breastfeeding
o Period of decreased responsiveness- (2-4 hours)- try to initiate feeding
& ends up making mom/nurse/baby frustrated
o Second period of reactivity- (4-6 hours)
Physiological Adaptations
-RESPIRATORY: transition from fluid-filled organ to air-filled organ (once
out of womb)- fluid removed thru blood & lymph system- this process
begins in labor
Factors that help initiate feeding:
1) Mechanical factors: when the chest is compressed as it
passes through the birth canal, when the chest is
compressed some of the fluid in the lungs get pushed out.
Then, when chest recoils produces passive inspiration of air
(SOwhen compressed fluid pushes out & as it expands, air
comes back in)
2) Chemical factors: w/ cutting of cord we remove the oxygen
supply so no longer getting oxygen- SO asphyxia occurs
(increased CO2 and decreased O2 &pH)RESULTS in
Acidosis- when baby is in this state stimulates respiratory
state in brain & in arteries to initiate breathing
3) Sensory factors- going from dark/quiet environment to
bright/loud environment- stimulates breathing. Tactile-
immediately dry them off following delivery
4) Thermal factors: environment thats warm (98.6) to room-
temperature environment about 78 degrees
-CARDIAC:
-Fetal hear vs. infant heart:
-Ductus arteriosus- (passageway connecting aorta to
pulmonary artery)- closes off & turns into ligament
-Foramen ovale- (structural opening that connecting right
atria to left atria)- structurally closes so closes flap
-Ductus venosus- connection from umbilical cord to inferior
vena cava (how blood gets from mom to fetal heart)- also
turns into a ligament
2
Initial Care of the Newborn:
Start w/ the General Assessment (focusing on ABCs)- Do they
have respirations? What color are they? How is their muscle tone?
Look for S/S of respiratory distress- cyanosis, decreased or
increased respirations?
o 3 Signs Infant show of Respiratory Distress:
1) Retractions--chest indents when they breathe in (document
where they are & severity- locations can be:
intercostal/subcostal/substernal?)
2) Nasal Flaring-- nostrils flare out to sides when infant breathes
in
3) Grunting: ehh sound- rhythmic sound they will make
INTERVENTIONS:
o Suction as needed after delivery (catheter of bulb syringe
suction)
o DRY NEWBORN: Reasons= 1) To help with temperature
regulation & get rid of cold fluid, & 2) Help stimulate their
breathing
o Maintain temperature stabilityput them w/ mom, put them
under the radiant warmer
o If possible try to keep newborn w/ mom to facilitate
bondingskin-to-skin contact helps them regulate respiratory &
HR as well as warmth
o Position newborn on side or prone position- (in order to
facilitate drainage of secretions)
o Ensure Newborns safety w/ identification band (2= one on
foot & one on arm)
o Footprint newborn & fingerprint mother as per agency policy
o Place matching bracelets & security device on mother &
newborn
APGAR SCORE: (nurse assigns this)- Assigned at 1 minute of life
& 5 min of life. If 5 min score is low can do 10 min APGAR score, but
this is rare. Each category is assigned 0, 1, or 2 points (0=not present,
2= very present) (*want it towards 2 points) (10= ideal score)
A= Activity (muscle tone)
P= Pulse (only care if it is above or below 100 in this first minute of
life) (Above 100=2, Below 100=1, if not there=0)
G= Grimace or Reflex Irritability- (if they do nothing=0, if they
dont do much but grimace= 1. If react by crying/move knees=2)
A=Appearance (measured by skin color)- want them to be pink
allover, BUT this is usually uncommon b/c usually born a little blue
(cyanosis in hands/feet)= 1, (if they are blue/gray all over= 0)
(*almost no baby gets a 2 in this category)
3
R= Respirations (not actually counting respirations initiallymore
about their cry)- 1= fussy/strong cry, slow/irregular cry=1, no
respirations= 0
Interventions for APGAR Score
o 8-10: No interventions required, except to support infants
spontaneous efforts
o 4-7: Probably need to provide stimulation (rubbing them), could need
oxygen delivered (especially w/ 4way of delivery depends on if they
are breathing on their own, IF NOT BREATHING ON THEIR OWN
give positive ventilations- bag them like you would an adult- delivers
very regulated amount of pressure)
o 0-3: BAD- infant requires lot of resuscitation- if not breathing
provide bag mask/ventilation, if HR is below 60 will start chest
compressions
Interventions Performed After Initial Transition Period: (after infant
stabilized & been w/ mother)
1) Eye Prophylaxis for the Neonate: (Erythromycin ointment or rarely
Tetracycline) (bacteriostatic eye drops used to prevent eye infections
caused from gonorrhea or Chlamydia in the vaginal tract)- given b/c
can cause blindness
a. Nursing Interventions: Instill from lower lid (inner to out cantus)-
infants will clench their eyes closed SO this will be difficult.
SHOULD BE DONE WITHIN AN HOUR AFTER DELIVERY
(tips= turn all lights off so infant will more likely open their eyes,
& make sure pulling down on lower lid)
2) Vitamin K (AquaMephyton or Phytonadione) administrations
a. Description- Cant be synthesized w/out bacteria in the intestine-
so, INTESTINAL FLORA IS NEEDED- newborns gut is sterile
initially- we need this b/c infants dont have Vitamin K in 1
st
week of life
b. Uses- Vitamin K is necessary to produce prothrombin to help
them not bleed too much- used in prophylaxis of hemorrhagic
disease of newborn
c. Adverse Effects- Hyperbilirubinemia (elevated billirubin levels)
(esp. preens?)- BUT isnt something that would keep them from
giving Vitamin K
d. Nursing Interventions: Administer this within 1
st
hour as well-
administer in vastus lateralis muscle (usually meaty in
newborns). Monitor for breathing OR any signs of bleeding
Hep B Vaccine- produces antibodies to protect newborn against Hepatitis
B Virus- Recommended for all infants to prevent against Hep B- Given as
a 3 dose series (1 at birth, 2
nd
dose one month later, & 3
rd
dose 5 months
after that SO IN ALL TAKES 6 MONTHS)
4
o Adverse- Rash, fever, redness, swelling, or pain at injection site
(true for all vaccines)
o Nursing interventions- see if parents want this vaccine to be
administered or not, insert in vastus lateralis-going in usually
OPPOSITE LEG OF VITAMIN K
Hepatitis B Immune Globulin (HBIG)--(if mom is positive for Hepatitis
B)- also give Hep B. Vaccine as well, but MAKE SURE IN OPPOSITE
LEG AS HEPATITIS VACCINE, HBIG IN OPPOSITE LEG, & VITAMIN K
CAN GO IN WHICHEVER LEG)- should be given within 12 hours of birth.
Give bath to baby before giving any injections so dont risk give any of
moms fluids to baby before piercing babys skin)
Full Head-to-Toe Physical Examination:
o Vital signs= count for FULL ONE MINUTE
o Make sure baby stays warm during it make sure each body
part is covered back up before you take another article of clothing
off, OR put baby under the warmer & do your assessment there
o Body measurements-
Weight expected weight loss within 1
st
initial postpartum
period/first couple days, DONT want them to lose more than
10%
Head:
o Fontanels= soft spots. Need to assess: if they are there, if
flat/sunken in/OR bulging outAbnormal= depressed/sunken
dehydrated, bulging increased in intracranial pressure
Purpose: 1) so head can fit through birth canal, & 2) brain in
going to continue to grow for 1
st
year or two so allows for that
brain growth to happen
Anterior fontanel (front)- Larger & Diamond shape
Posterior fontanel (back)- Triangular-shaped & smaller
o Suture lines- Sagittal suture (up top), Lamboidal suture (around
the back), Squamosal suture (side above the ear)WHEN
PALPATING: bones can either meet (side-by-side), can be open
(dont meetspace or indentation u can feel), OR over-lapping
(one bone comes up over the other bone) NONE OF THESE
ARE ABNORMAL
o Feel for suture lines checking for 3 things:
1) Molding (cone head)is very normal, will resolve on its
own w/out any interventions in a few days
2) Caput (Swelling of the tissues)- usually a result of
tissue being compressed so its inflamed/swollen- not very
concerning- will resolve on its own in a few days as well
(*CAN CROSS SUTURE LINES, CAN BE ON LEFT &
5
RIGHTS SIDES OR ON SPECIFIC PLACE- just swollen
tissue
3) Cephalohematoma (blood escaping from a ruptured
blood vessel)- interventions for this depend on size &
whether or not improving or worsening (IF IMPROVING-
goes away on its own but can take months, IF
WORSENING- need to do scans, may need to go in & stop
the bleeding (*WILL NEVER CROSS THE SUTURE LINES
AKA BE ON LEFT & RIGHT SIDE OF THE HEADHere
you can also feel fluid)Leads to excessive breakdown of
RBCs which places the infant at a higher risk for Jaundice**
EYES:
Psuedostrabismus- past a couple months need to be looked at by
optomologist
Epicanthal folds- associated w/ certain genetic abnormalities (downs
syndrome is one of them)-children w/ Asian decent have these though*
EARS:
Do they look well-formed? Normally shaped?
Assess- see where they are placed in relation to the eye. Top of the ear
should generally fall in line w/ the outer cantus of the eye
o If ear is significantly lower has been associated w/ certain
genetic conditions & congenital abnormalities
o Pre-Auricular Skin tags around the ear (dimple?) Associated w/
kidney defects, SO PAY ATTENTION TO GU ASSESSMENT
NOSE:
Natal teeth
Epstein pearls- benign retention cysts on hard palate (look like little white
spots on gums- NOT CONCERNING
Inspect for circumoral cyanosis (blueness around mouth)= BAD b/c means
RESPIRATORY DISTRESS
See if tongue is freely moving or not
o Tongue-tied: can cause problems w/ feeding or w/ speech later on
NECK
Make sure trachea is midline
Inspect for webbing webbing associated w/ certain genetic alterations
(Turner Syndrome is one of these*)
6
Palpate to see if palpable masses & palpate among both sides of
clavicles to check for fractures from birthing process
CHEST
Circular in appearance? What color is it? Any extra nipples?
Witches milk- more common in full-term infants, can last a couple months,
NORMAL FINDING
Buldge at lower sternum= NORMAL to see this poking out
HANDS:
Check number of fingers- can remove webbing & extra finger if these exist
Look at palm of hand to see if there is a single palmer crease if there is
just mark that there is, but is associated w/ certain genetic conditions
(specifically Downs Syndrome)
_____________________________
SKIN:
Vernixcheesy, white substance that protects the babys skin in utero
(more pre-term more you will have this)
Lanugo- fine hair ocvers babys back, shoulders, arms (more pre-term
more you will have this)
Miliawhite spots that are formed when keratin becomes trapped under
the outer layer of skin & forms a tiny cyst- NOT CAUSE FOR CONCERN-
goes away in a few days to a few weeks on its own
Feel texture of skin
Earlier infant isstickier, thinner skin (more post-term thicker, may be
dry/cracked/peeling)
Look for any bruising, petechiae, birth-marks
Rasheserythema toxicom appears within 1-2 days after birth, often
goes away on its own within about one week, nobody knows the cause of
ittypically consists of tiny little, firm, whitish/yellow bumps surrounded by
a ring of red (sometimes bumps are vesicularmeaning filled w/ fluid),
(sometimes no bumps at all & just redness)usually on face, chest, arms
or legs **
FACIAL MARKS:
Forcep marks- use forceps (instrument that cradles the babys head &
used to help pull the baby out of the mother)-Generally not a concern, can
lead to bruising, which increase RBC, increasing risk of Jaundice (but
usually not)
Birth marks can be VASCULAR or PIGMENTED:
o VASCULAR- 3 main ones- need to assess color, whether its flat or
raised, location, and if it blanches to determine type
Angel kisses due to dilation of certain blood vessels-
usually become darker when the child cries or when the
7
temperature changes, usually light pink, flat, & typically
blanch- may be found on forehead, eyelids, nose, upper lip,
or back of the neck, NO TREATMENT NEEDED- and
usually fade by kids 2
nd
birthday *
Port wine stain darker in color (dark red or purple),
typically seen on the face, usually flat at birth, DO NOT
BLANCH, WILL NOT fade w/ time (in fact, usually get
darker), raised/pebble-like texture later in childhood or
adulthood
Can use laser-treatment w/ each of these birthmark types
Strawberry marks capillary hemangioma- raised & dark
red, typically start to grow around 2
nd
or 3
rd
week of life,
typically regress on their own (takes few months or years
though), best results are seen when they are allowed to
resolve spontaneously **
o PIGMENTED (caused by overgrowth of cells that create pigment in
the skin) (2 we will focus on)
1) Mongolian spots- flat, bluish/gray patches found often on
lower back or buttocks, MORE COMMON ON DARK SKIN
INDIVIDUALS (asian, American-indian, African, or hispanic
decent), usually fade, a lot of time go away by school-age
w/out any treatment
2) Caf au lait spots- get their name b/c or their
appearance look the color of coffee w/ milk in it, can be
anywhere on body, sometimes increase in number as child
gets older, not a problem to have one of these, BUT if child
has multiple and larger in size (more then cm) indicative
w/ genetic disorder NERUOFIBROMITOSIS (*need to look
into this further)
ABDOMEN:
o Make sure umbilical cord looks normal & look at how many vessels
are in the umbilical cord
2 holes (1 vein & 1 artery) ABONORMAL (*associated w/
other congential defects)
3 holes (2 arteries & 1 vein) NORMAL
GENITALS:
FEMALESnormal for labia to be edematous/red, could be discharge
(could be SCHMEGMA- white cheesy substance, OR blood tingued
PSEDUOMENSTRATION) BOTH NOT CONCERNING** will go away in
few weeks
Clitorus will be more prominent in pre-term** (at term, labia majora covers
minora)
MALES
o Crytorchidismtestes have not descended in scrotal sac- dont
descend until about 32-34 weeks
8
o Hydrocele- fluid around testicals in scrotal sac, very edematous,
might feel fluid,
o Looking to see where urethra opening is in relation to the penis
(can be at top or bottom**HYPOSPADIAS= opening at bottom of
the penis & or **EPISPADIAS= opening at top of the penis (*shown
w/ difficulty urinating & contraindication to being circumcised) (*if
have these- cant be circumcised until reconstruction is done)
o SCORTUM: Edematous, TERM INFANT- lots of rugae (wrinkles in
scrotal sac) *pre-term will not have as much rugae
SPINE:
Tuft-of-hair @ base of spine OR Dimpling= associated w/ Spinal Bifida
EXTREMITIES
More term- more creases they will have
Ortolani- place hands cuffing the knee w/ middle finger over greater
tronchanter (other hand is stabilizing the pelvis)abducting the hip
(pulling it out) & pushing up on hip joint (*if you hear clunk/click=positive
Ortolani, which is NOT what we want
Barlow test--Hips adducting (together) & feeling posteriorlyalso
listening for a click
BOTH of these test for Hip Dysplasia
NEWBORTN ASSESSMENT
CARDIOVASCULAR SYSTEM:
Full min apical pulse
Murmurs- could mean structures havent closed yet
NORMAL HR= 110-160
Hemoglobin 14- 20
Hematocrit- 43-63 %
REPSIRTATORY
Respiratory rate= 30-60 breaths per minute
Rhythm-- Pauses in breathing less than 10 seconds= normal
Lung sounds may have cackles in first couple hours of life until transition
to air-filled organ
RENAL SYSTEM:
Brick dust- result of excess uric acid crystals, indicates highly-
concentrated urine, OK in the first few days of life-BUT shouldnt be seen
after that point, MORE COMMON IN BREAST FEEDING moms
HEPATIC SYSTEM:
Normal Blood glucose= 40-80 mg/dL
9
IMMUNE SYSTEM:
Look for s/s of infection (around cord, around circumcision, around eyes?)
WBCs for infants = 10,000- 30,000
THERMOREGULATORY SYSTEM
Normal Temp= 36.5-37.5 degrees celcius
Assess temp every hour, then every 4 hours, then every 8 hours
NONSHIVERING THERMOGENESIS (NST): (way infants will help increase their
body temp)
Uses brown fat (brown adipose tissue- which is unique to newborns)-
brown adipose tissue starts to accumulate in 1
st
trimester in neck,
axilla, back, mediastinum, in abdomen VERY VASCULAR, heats the
babys blood
Cold stress- excessive heat loss resulting is use on compensatory
mechanisms, has NEGATIVE CONSEQUENCES FOR BABY, pre-term
and small
JAUNDICE-----
Pathological jaundice- WORST- jaundice occurs in first 24 hours of life,
surpasses the 95
th
percentile for age, OR if persists for long period of time
this is when there is a medical cause/condition that has occurred with has
lead to the high bilirubin levels. The most common cause is incompatibility
of the Rh factor (positive vs. negative in relation to blood type). This
happens when mom is Rh -, and is exposed to Rh + blood (if the blood
ever mixes, which it should not but there are instances when it does). The
mother then builds up antibodies against Rh + blood, which can cross the
placental barrier. If the baby's blood type is Rh +, then these antibodies
will attack the baby's RBCs, leading to an excess destruction of RBCs,
which then leads to excess bilirubin levels and consequently jaundice.
This is just one cause of many for pathological jaundice, but as I mentioned it is
the most common. I know in adults jaundice typically means liver issues, but that
is not necessarily the cause in newborns (although it could be the case, but this
is not as likely). Any condition that leads to excess RBC destruction could be a
cause of pathological hyperbilirubinemia.
Physiological jaundice: jaundice that occurs after first 24 hours of life, jaundice
below the 95
th
percentile, & jaundice doesnt last for long periods of time
Physiological jaundice, on the other hand is related to the normal
physiological differences that are present in all newborns that makes it so
that there may be an excess of bilirubin. These physiological differences
include an immature liver, increased RBC mass, shorter life span of RBCs
10
with fetal hemoglobin (90 vs. the usual 120 days), lack of intestinal
bacteria, and/or decreased intake from breastfeeding. There is nothing
'wrong' with the newborn that is causing the excess bilirubin, it is just their
immature systems that are unable to excrete the bilirubin levels as needed.
In terms of what the differences are clinically, pathological jaundice typically
beings within the first 24 hours of life and persists longer. Physiological jaundice
doesn't appear until AFTER 24 hours of life, and typically does not last more than
a week.
Both conditions involved excess bilirubin levels, which can cause brain damage if
the levels exceed a certain level, regardless of the cause and/or type. If the level
is ever in the high risk zone (regardless of whether it is pathological or
physiological), it will need to be treated with phototherapy.
PRINT THIS:
http://amy47.com/nclex-style-practice-questions/obgyn-nclex-type-
questions/obgyn-3/
(NEWBORN NCLEX QUESTIONS)
http://amy47.com/nclex-style-practice-questions/obgyn-nclex-type-
questions/obgyn-4/
(POSTPARTUM)
http://amy47.com/nclex-style-practice-questions/obgyn-nclex-type-questions/
(INTRAPARTUM)
http://amy47.com/nclex-style-practice-questions/obgyn-nclex-type-
questions/obgyn-2/
(ANTEPARTUM)
Look at these practice questions on overall "Overall OB Content Practice NCLEX
Questions" under practice nclex questions on blackboard
11
Unit 2: Day 2- all s/s worse earlier they are
PRETERM NEWBORN: (born prior to 38 weeks gestation) (*use new ballard
scale)
o Assessment: (more preterm, more abnormal assessment data)- could
have: low APGAR scores, Respiratory distress (more earlier they are),
Temperature (more trouble maintaining temp within normal limits),
weight gain (if before 36 weeks where sucking reflex gets well
coordinated- may be poor-feeders/trouble gaining weight), Skin= thin,
can see lots of blood vessels
o Nursing care
Diagnosis- (primary concern=immaturity of body systems),
Respirations= Primary concern, followed by ABCs. The
muscles that are needed for respirations have not fully
developed, less alveoli available for oxygen and CO2 exchange.
If infant is preterm enough, lack of surfactant (not produced
sufficiently until 35-36 weeks so w/out this alveoli collapses
on itself b/c the surfactant decreases surface tension- so will
show s/s of respiratory distress)
Risk for ineffective breathing patterns
o *Planning= infant maintains respirations
between 30-60 b/c thats normal range
Risk for impaired gas exchange
o *Planning= infant will maintain O2 saturations
between 95-100%
Risk for Unstable blood glucose (think about nutrition &
temp regulation- sucking not established until 35-36
weeks)
o *Planning= infants BG will maintain between
40-80
Risk for Imbalanced Nutrition- less than body
requirements
12
o *Planning= infant will not lose more than ____ or
not gain ____, or talk about how often they will
feed (every 3-4 hours), or will intake _______
Risk for ineffective Breastfeeding
Risk for ineffective infant breathing pattern
Risk for neonatal jaundice
o *Planning: infants billirubin levels will stay in ___
range depending on their gestational age
Risk for ineffective thermoregulation (b/c cant regulate
temp)
o *Planning= infant will maintain temp between
36.5-37.5
Risk for infection (immature immune system)
o *Planning= infant will not show s/s of infection
by absence of (____redness?)
Planning- (above)
Interventions- Monitor VS every 2-4 hours
Respiratory assess respiratory rate & pulse oxygen,
administer oxygen as prescribed
Nutritional Monitor intake & output, daily weight,
administering enteral feeds, assisting moms w/
breastfeeding
Risk for Neonatal jaundice assess for jaundice, might
be drawling billirubin levels
Thermoregulation keep swaddled, keep baby under
warmer, monitor temp
Risk for Infection handle newborn carefully, make
sure adhering to infection control measures, change
their position every couple hours, handle them very
carefully
Minimize excessive sensory stimulation low lights,
quiet, not going to handle them very often
Evaluation- (Just go back to each goal & say if you met it or
not)
POST-TERM NEWBORN: (born after 42 weeks gestation)(*use new ballard
scale) (*typically do not have feeding or respiratory issues as much as
preterm) (*similari
o Assessment: Skin= dry/cracked/not much vernix or lanugo,
fingernails=very long, extending over their fingers, skin/umbilical
cord/nails may be meconium stained, may have trouble with
hypoglycemia (s/s=jitteriness)
o Nursing Care:
Diagnoses:
13
Risk for unstable BG (same as preterm- same
interventions, planning, etc.)
Risk for ineffective thermoregulation (same as preterm-
same interventions, planning, etc.)
Risk for Injury (Babies will be larger, so more likelihood
that pass meconium in utero)
o *Planning= infant will not show s/s of
aspirations of meconium, infant will remain free
from injury during the birthing process
o Interventions: makes sense to have a C-section
b/c large size of baby, check for birth injury
(check clavicles, check nerves in arms,
symmetrical extremity movement?)
Risk for Aspiration r/t to presence of meconium (babies
will be larger, so more likelihood that pass meconium in
utero)
o *Planning= infant will not show s/s of
aspirations of meconium, infant will remain free
from injury during the birthing process
o Interventions: suction baby when it comes out,
and monitor for early s/s
SMALL FOR GESTATIONAL AGE (SGA): (neonate plotted at or below 10
th
percentile on the intrauterine growth curve)
o Typically were in intrauterine environment that was not conducive to
growthcould be b/c smoking, maternal hypertension, problems w/
placental blood flow, infection, or multiple gestation. If baby isnt
delivered yet= IUGR (Intrauterine growth restriction)=baby isnt
growing the way we would expect them to grow
o Why is it a concern? When fetus doesnt receive enough O2/nutrients
in pregnancy, overall body & organ growth is limited, & If restricted
blood flow through placenta= not enough 02
o Assessment: (some similar to preterm): Polycythemia (elevated RBC
count)will show ruddy appearance or might be jaundice b/c of
chronic lack of oxygen,
o Diagnoses: (very similar to preterm)
o Planning goals: (very similar to preterm)
o Interventions: (very similar to preterm)
*Want to maximize Stimulation- provide them w/ stimulate
that will help them grow (dont get tired from this like preterm
infants)
If have s/s polycythemia- draw blood levels to monitor their
hemoglobin & hematocrit
14
LARGE FOR GESTATIONAL AGE (LGA)- (*opposite of small for gestational
age)- (neonate plotted at or above 90
th
percentile on growth curve) (*a lot of
time born to mother who are diabetic b/c they have the extra glucose & that
glucose turns to fat, which leads them to be at an increased weightwill
have problems monitoring their glucose initially, body produces extra
insulin- takes body hours to realize it needs to stop producing so much
before the babys BG bottoms out)
o Why a concern? Delivery can be difficult b/c kid is large prolonged
vaginal delivery time, injury during birthing process, increase in
Cesarean delivery
o Assessment: Diabetes problems with BG, may have respiratory
distress (b/c diabetes causes lungs to mature slower), problems w/
hyperbilirubinemia, Clavicle may not be intact, arms not moving
symmetrically, signs of hypoglycemia?
o Diagnoses: (risk for injury, risk for unstable BG, risk for ineffective
thermoregulation b/c larger theyre losing more heat)
o Planning goals: (same as diagnosis above) (+) Monitor for
hypoglycemia, drawing blood glucoses, INITIATE EARLY FEEDINGS
(give them glucose until their insulin can level out)
MECONIUM ASPIRATION SYNDROME: (baby breaths in amniotic fluid
containing meconium
o Assessment- low APGAR scores (not specific to this disease though)
o Diagnosis:
Ineffective airway clearance r/t airway inflammation
*Planning goal= infant will maintain patent airway
during hospitalization
Ineffective breathing patterns r/t tachypnea
Impaired gas exchange
Ineffective thermoregulation (or risk for this)
Risk for infection
Risk for contamination
*Planning goal= eliminate contamination, so want to
remove pathogens from wherever they are
o Planning goals:
o Interventions: Suction the babys mouth & nose before it even takes a
breath, for temp regulation/breathing patterns/risk for infection all
apply here as well. AIRWAY CLEARANCE could administer steroids
to help inflammation, Contamination give antibiotics
HYPERBILIRUBINEMIA: (elevated bilirubin levels, corresponds w/ babys
age in hours & determined by a nomogram)
o Why is it a concern? Unbound bilirubin is able to cross the blood-
brain barrier, & the excess bilirubin will damage cells of CNS & cause
brain damagemedical term= KERNICTERUS**
15
o Assessment: Most indicative sign=jaundice (progresses from head
downward), poor intake & output (bilirubin excreted in the stool),
o Diagnoses: If infant has hyperbilirubeinemia Risk for Injury (CNS
damage)
o Planning Goals:
1) Prevent the development of hyperbilirubemia when
possible
*Interventions= Initiate feedings early (so have more
stools/output), Help w/ breastfeeding, Monitor I&O
status and make sure appropriate for infants age
2) To detect it early
Interventions: know risk factor= any condition
causing excess breakdown of RBCs, Detect for
jaundice (*Best done in natural lighting, if you see
jaundice in 1
st
24 hours-notify physician, then they
would tell you to draw bilirubin levels)
o Transcutaneous bilirubin levels drawn first
measures just through the skin, lighting needs to
be very dark if this is elevated, then draw a
serum level
3) To prevent injury/permanent damage in those who develop
hyperbilirubinemia
*Interventions:
o Phototherapy(can be bili-lights or bili-
blanket)- NI= make sure you keep genitals
convered & if bili-lights keep eyes covered as
well. *Make sure enough skin is exposed as
possible so lights can work effectively, Remove
eye-shield each shift to make sure no
infection/irritation, Pay attention to their
temperature/any skin irritation, Pay attention to
their I&O (may need to increase fluid intake),
Reposition child every 2 hours, Provide
stimulation as much as possible to help them
grow, & Check bilirubin levels frequently)
Complications of phototherapy- Skin
irritation & Over-heating
o Bilirubin levels tend to peak at about 3-5 days of
life**
DRUG-EXPOSED NEWBORN: (newborn who has become passively addicted
to drugs that have passed through placenta) (*starting in September this
year Universal Drug Screenings on all birthing mothers)
o Addicting drugs: Heroin, Methadone, &/or Cocaine
o Assessment: Signs of neonatal
16
Neuro s/s: muscle tremors/jitteriness, increased crying &
difficult to sooth, cry is typically very high-pithced, may have
seizures/frequent yawning/nasal stuffiness
GI s/s: vomiting, diarrhea, difficulties w/ eating, babies in drug
withdrawal act very hungry, BUT difficult to feed, flex back, &
uncoordinated suck/swallow reflex
Respiratory s/s- usually breath at faster rate (could be slower
as well), & s/s of respiratory distress
o Diagnoses:
Risk for ineffective breathing patterns
Risk for impaired gas exchange
Risk for injury
Risk for imbalanced nutrition (less than body requirements)
Risk for fluid volume deficit
o Planning goals: (same as before for each of these diagnoses)
o Interventions:
1) Appropriately identify infants at risk for withdrawal
If mother comes back positive, must do drug screening
on infant (can test w/ urine or stool, typically use urine),
*Important to test 1
st
or 2
nd
urine specimen baby has
2) Maintain O2 sats between 95-100% & will have respirations
between 30-60
Monitor pulse ox & respiratory rate
Give O2 as needed
3) Ensure proper nutrient consumption as evidenced by
weight gain & appropriate feeding patterns & intake and
output by age
Provide small, frequent feedings as prescribed
Monitor I&O closely
4) Infant will remain free from injury
Interventions to prevent are determined by Finnegans
scoring system, but may include the following:
o Nonpharmalogical Interventions= (*all focus on
decreasing stimulation) swaddle infant,
dark/quiet room, hold infant close when
providing care, cluster care in effort to minimize
stimulation
o Pharmacological interventions= (*look at
Finnegan withdrawal score & sleep/weight gain
patterns, & also if there is any pharmacological
therapy used from same drug class mom used)
Will also need to frequently monitor VS, respiratory &
cardiac status
May also need to provide emotional support for mother
& consult w/ social worker
17
GENETICS
ANA/ISONG Statement regarding geneticseven if you dont have a
specific job in genetics, nurses still have specific duties in relation to genetics
(*look at exactly what nurses need to do for this in PPT)
Mitosis: (takes place in somatic or TISSUE CELLS-not reproductive cells),
Responsible for cell-growth, RESULT 2 identical daughter cell & result is
same as original cell (3 total cells all w/ same information)
Meiosis: (Reduction Division) (*only occurs in reproductive cells of testes &
ovaries), this process RESULTS in formation of sperm & oocytes which are
called gametes (gametes are haploid cellsonly have 23 chromosomes vs.
the 36 in our somatic cells), Also very important to help us have genetic
diversity, does this through:
o 1) Crossing over: before the chromosomes separate, they will pair up
next to one another & exchange genetic material w/ one another (this
way you dont have exact replicas & we get genetic diversity)
o 2) Independent assortment: when cell is diving & splitting from the
46 to 23, pair separates randomly either into one gamete or another
Chromosomal Number Terms: (supposed to have 46, 23 pairs (23 from
mom & 23 from dad)
o Aneuploidy: (dont have 46 chromosomes total)
Having extra or missing chromosomes
o Monosomy: (missing one) (one condition that we know of compatible w/
life when females are missing one of their X sex chromosomes
TURNER SYNDROME)- typically end up in a miscarriage
The loss of a single chromosome from a pair
Ex= (45 chromosomes, XO)
o Trisomy: (47 chromosomes)
The gain of a single chromosome
Ex= (47 chromosomes, XY, +21= extra 21
st
chromosome= DOWNS
SYNDROME)
o Polyploidy: (extra COMPLETE SET of chromosomes present) typically
ends up in miscarriage
The condition when more than two complete sets of chromosomes
are present
o Euploidy:
The presence of the normal number of 46 chromosomes
18
Chromosomal Alterations:
o Often occur during cell division
o Classified as either structural alterations OR alterations in the number of
chromosomes
o Structural Alterations:
Inversion: piece of the chromosome breaks off, and then it flips
itself upside down & reinserts itself
No increase or decrease in genetic material, just differences
in how it is structured
Deletion/Duplication: (too much or too little genetic material
during crossing over). When crossing over deletion (missing part
of the genetic material, & duplication (extra- 2 of them on
chromosome)
Translocation: occurs when 2 non-homologous (different
numbered) chromosomes exchange segments of DNA (basically,
one chromosome gets attached to the other oneseen as one
chromosome, & will duplicate the entire genetic material thinking
its 1 chromosome)
o Alterations in Chromosome Number:
Nondisjuction- (Meiosis)- homologous chromosomes (pari of
same chromosome) do not separate as they are supposed to
during cell divisioncreate monosomic (not enough) or trisomic
cell (too many)
Instead of 2 pairs, 1 pair in each 2 cells in one & nothing
in the other
Nondisjucntion is WORSE in 1
st
cell division of Meiosis**
Mosaicism (result of nondisjuction in Mitosis specifically)-
End result= Pt will have 2 distinct cell lines (certain part of body
w/ different number of chromosomes)
Cell w/ 3 chromosomes in each cell (Trisomy), some cells
will have the typical 46 chromosomesif happens more
towards the end
o Gene Alterations:
Single-gene disorders: alteration that occurs in a single gene- can
occur either through one of Mendelians patterns of inheritance
OR can happen as a new mutation
Multifactorial disorders: alteration that occurs through gene
interactions w/ the environment (some environmental factors
could include: maternal age, nutrition, smoke exposure, exposure
to chemicals/radiation)
Ex= Clef Lip & palate, Neural tube defects, certain
congenital heart defects, congenital Hip Dysplasia, & Pyloric
stenosis
Patterns of Inheritance:
19
o MENDELIAN: Autosomal= genetic alteration not on sex chromosome (not
X or Y)
Autosomal Dominant: you only need one of your pairs of alleles
to have that alteration to be expressed (only need 1 altered gene
present)
Disease examples= Huntingtons disease & Acronoplasia
(dwarfism)
Characteristics:
o Both males & females are affected
o Males & females are usually affected in equal
numbers
o An affected child will have an affected parent and/or
all generations will have an affected individual
(appearing as a vertical pattern of affected
individuals on the family pedigree) (*will not skip
generations) (*wont have any carriershave gene &
arent showing the effects of it)
o Unaffected children of an affected parent will have
unaffected offspring
o A significant proportion of isolated cases are due to
a new mutation
Autosomal Recessive: (still not on sex chromosomes)- BUT since
recessive it is weaker, so BOTH genes must have that alteration for
person to be fully affected.
If only one of the genes has alterations & other one
doesnt= Carrier (half-shaded) dont show S/S, but can
pass it on to children
Disease examples: Sickle cell disease, Cystic fibrosis,
TaySachs disease
Characteristics:
o Both males & females are affected
o Males & females are usually affected equally
o An affected child will have an unaffected parent, but
may have affected siblings (appearing as horizontal
pattern of affected individuals on the family
pedigree)
o The condition may appear to skip a generation
o The parents of the affected child may be
consanguineous (close blood relatives)
o The family may be descendants of an ethnic group
that is known to have a more frequent occurrence of
a certain genetic condition
X-linked:
X-linked Recessive- (recessive, but now on X
chromosome), women have 2 Xs & men only have 1--> if
20
mens one X chromosome has it, they will show this
disorder (MORE COMMON IN MEN b/c of this), females
could be affected or could be carriers
o Fathers will NEVER pass it on to their sons, must be
getting it from mother if affected
o Ex= Hemophilia A & B
o Characterisics:
More males will be affected than females,
rarely seen in females
An affected male will have all carrier
daughters
There is no male-to-male inheritance
Affected males are related by carrier females
Females may report varying milder
symptoms of the condition
A new sporadic case could occur due to a new
mutation
X-linked Dominant: (isnt very common)- since its
dominant, only need one X to be affected- Males & females
DO NOT tend to be equally affected (*females are affected
less severely)
Y-linked: (hardly ever seen)- ONLY MALES ARE AFFECTED
o MITOCHONDRIAL- when mitochondrial DNA has the alteration that is
being passed down- can only be passed down from the mother b/c
children get their mitochondrial DNA just from their mother
These disorders tend to involve high energy organs (skeletal,
brain, heart, muscle)
Genetic Assessment:
o Minor anomalies: (arent very serious or life-threatening- more cosmetic
issues)
o Major anomalies: more serious/life-threatening affects
o Syndromes: groups of symptoms that are seen together & difference
between the two if have underlying cause syndromes have underlying
cause (*single underlying cause of a group of symptoms)
o Associations= syndromes grouped together, but have no single
underlying cause (* group of symptoms together, BUT NO SINGLE
UNDERLYING CAUSE)
Genetic Testing:
o Chromosomal testing:
Karyotype analysis- line all the chromosomes out in a row, then
stained to see overall picture if they have typical number of
chromosomes or not
o There are many types of genetic tests
21
Diagnostic testing- Pt would have s/s of something, so testing for
that specific genetic alteration we think it is/worried about
Prenatal testing- during it doing the prenatal period (so testing
fetus in utero)
Newborn screening- (PKU & sending that blood to test for a bunch
of different genetic disorders- NOT symptomatic at this point)
Preimplantation testing- in-vitro fertilized zygote & dont know
if you want to implant it yet b/c you want to make sure the zygote
doesnt have a genetic abnormality
Carrier testing- no s/s or dont have condition, BUT worried about
passing it on to children
Predictive testing- (not symptomatic yet, but worry they may later
develop symptoms b/c of family history)
Aims to reduce morbidity & mortality w/ targeted
prevention/surveillance, and/or Treatment
Controversial when no preventative treatment currently
exists
Down Syndromse= presence of extra chromosome 21 (affects every 1 in
1,000 live births)
o 3 causes- 1) Traditional trisomy 21 (majority of cases), 2) Translocation
(when chromosome 21 attaches to a nonhomologous chromosome), 3)
Mosaic downs syndrome (some of the cells will have 47 chromosomes
and some will have the normal 46)
o Risk factors: Maternal age over 35 at delivery, Previous child w/ downs
syndrome, OR 3) Translocation carrier (b/c can pass on to children)
o Nursing process
Assessment- (expressivity is variable)- usually some form of
cognitive impairment (how much differs depending on child),
delayed social development, hypotonia (decreased muscle tone),
characteristic facial features= upward slanted eyes, inner
epicanthal folds & low set ears. In almost cases child also has
congenital heart defect, may see a single transverse palmer crease,
short stature w/ short limbs, short neck, delayed sexual
development, shortened life-expectancy
Diagnosis (medical diagnosis w/ karyotype- prenatally or after
delivery)
Delayed growth & development
Interrupted family processes
Ineffective coping
Social isolation
Grieving
Risk for infection
Risk for ineffective cardiac output (if have associated heart
condition)
22
Imbalanced nutrition (more than body requirements)
Risk for impaired parenting
Planning:
First, want to identify those w/ disorder (assessment)
o *Implementation= assisting w/ amniocentesis, or
chorionic villi sampling, pre-implantation testing?,
drawing maternal labs for screening testing,
performing newborn assessment and recognizing
those characteristics
Enhance the highest level of functioning possible
o *Implementation= advocate for early intervention
programs, referrals to OT/PT/speech therapy as
needed, provide education on how to promote
achievement of G&D milestones
Prevent and/or treat associated medical conditions such as
(infection, hearing/visual disturbances, obesity, &
congenital heart defects)
o *Implementation= for cardiac conditions- education
& assist w/ echocardiograms, give pre & post-op
care after surgery to correct congenital defects,
might need to administer Z-pack for sleep apnea.
Since higher risk for infection importance of
immunizations & ways to decrease infection. With
hearing & visual problems help w/hearing and
visual screening. Obesity provide nutritional
education or refer to a dietician
Ensure effective patient & family coping
o *Implementation- FIRST= assess how their coping is
going, assess needed & available resources, & inform
the family of the available resources as they are
needed
Implementation:
Evaluation- individually applicable to the Pt
CONGENITAL HYPOTHYROIDISM: (thyroid hormone deficiency that is present
at birth) (thyroid is the gland that makes iodine relating hormones that help w/
growth, brain development & metabolic)- can occur when thyroid gland is
absent, abnormally developed, destroyed, reduced in size, or when production of
thyroid hormones in decreased necessary for normal brain growth,
myelination, & normal neurological connections. MOST CRITICAL PERIOD= first
few months of life
o Cause: (usually cant determine)- rarely can be from spontaneous gene
mutation or an inherited autosomal recessive condition, could be result of
hypoplasia (underdevelopment) of the thyroid gland, failure of thyroid
23
mechanism feedback to develop, or can be from an iodine deficiency
(which is needed to make these hormones)
o Risk factors- (depends on cause)-(if autosomal recessive= family
history)- low birth weight & multiple gestation
o Assessment- (not many s/s first few weeks of life)- towards next few
months thickened tongue that sticks out, thick lips, a doll appearance,
prolonged neonatal jaundice, hypotonia, respiratory distress, bradycardia,
decreased pulse pressure, hypothermia, cool extremities, mottled/pallor
on skin, skin might be dry, might have issues w/ constipation, could have
lethargy, & might have difficulty feeding or poor weight gain
o Diagnosis: medical dx made through mandatory screening tests in all 50
states TSH (thyroid stimulating hormone level)which will be
ELEVATED, free T-4which will be decreased
Impaired skin integrity
Hypothermia
Ineffective tissue perfusion
Constipation
Decreased cardiac output
Imbalanced nutrition (less than body requirements) if have poor
weight gain
o Planning:
1) Identify those w/ the disorder
*Implementation= draw the newborn screening test, draw
labs to send for TSH or free T-4, recognize abnormal
assessment data & alert physician
2) Decrease the complications of the conditions (which is
abnormal brain development)
*Implementation= replace the thyroid hormonegive
them Synthroid (* needs to be taken on empty stomach)-
you would know that if dose is effective by monitoring TSH
and free T4 levels, educate that this is a life-long need
(**will be on synthroid for life)
3) Promote normal growth & development
*Implementation=
o Implementation:
o Evaluation= TSH & free T4 levels
Phenylketonuria (PKU): absence of an enzyme that is needed to metabolize
phenalymine (an essential amino acid)- hyperphenalymine causes progressive
brain damage if gets too high
o Risk factors- autosomal recessive disorder (so family history),
Europeans/Americans have higher incidence
o Assessment- failure to thrive (malnutrition), vomiting, irritability, Neuro
s/s= hyperactivity, erratic behavior, cognitive impairment, or seizures
24
o Diagnosis (medical dx made w/ PKU newborn screening test
mandated in all 50 states)
Risk for injury
Delayed G & D
Imbalanced nutrition (more or less than body requirements)- if
about lack of enzyme= less than, if about excess phenalyamine=
more than)
Fluid volume deficit
o Planning:
Identity individuals w/ the disorder
*Implementing= perform PKU screening mandated by US
law, & pay attention to assessment data
Those identified w/ disorderavoid the brain damage associated
w/ elevated levels of phenalyamine
*Implementing= limit their consumption of phenalyamine
to 20-30 mg/kg/day (* found in things w/ proteinmeats,
dairy, beans, nuts AVOID- although milk has a lot of
protein, they can breastfeed, but need to closely observe
this & check phenalymine levels frequently. Monitor blood
levels of phenalyalmine (*blood levels need to stay between
2-8 mg/dL)
Adequate resources & coping for life-long necessary changes
*Implementing= make sure they are aware of foods, recipes
that have low protein cooking, make sure they have the
financial resources (diet can cost more money?)
o Implementing
o Evaluation: evaluate the phenalalymine levels (2-8) & making sure not
developing s/s indicating they are having brain damage
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- The CAFR Scam in Every CityDocument12 paginiThe CAFR Scam in Every CityAlvin L. RozierÎncă nu există evaluări
- Devil's Handbook Guide to Scottish Legal TrainingDocument30 paginiDevil's Handbook Guide to Scottish Legal Trainingambassador_eric_john100% (2)
- Articles of Incorporation of U S Corp Company PDFDocument7 paginiArticles of Incorporation of U S Corp Company PDFAlvin L. RozierÎncă nu există evaluări
- TPN Concept 2 MapDocument3 paginiTPN Concept 2 MapAlvin L. RozierÎncă nu există evaluări
- Lawfully Yours Ninth Edition PDFDocument70 paginiLawfully Yours Ninth Edition PDFJohn M. Smith94% (16)
- Proper Nursing Actions for Conscious Sedation ProcedureDocument3 paginiProper Nursing Actions for Conscious Sedation ProcedureAlvin L. RozierÎncă nu există evaluări
- Articles of Incorporation of U S Corp Company PDFDocument7 paginiArticles of Incorporation of U S Corp Company PDFAlvin L. RozierÎncă nu există evaluări
- Roosevelt Exec 6102 All Gold To GovernmentDocument1 paginăRoosevelt Exec 6102 All Gold To GovernmentAlvin L. RozierÎncă nu există evaluări
- Us Bankruptcy and The Moors Part2Document5 paginiUs Bankruptcy and The Moors Part2Alvin L. Rozier100% (1)
- Us Bankruptcy and The Moors Part2Document5 paginiUs Bankruptcy and The Moors Part2Alvin L. Rozier100% (1)
- Sedation Concept Map 2 PDFDocument3 paginiSedation Concept Map 2 PDFAlvin L. RozierÎncă nu există evaluări
- Pressure Ulcer Concept MapDocument3 paginiPressure Ulcer Concept MapAlvin L. RozierÎncă nu există evaluări
- Lower Respiratory MedicationsDocument74 paginiLower Respiratory MedicationsAlvin L. Rozier100% (1)
- Tele Brain PDFDocument2 paginiTele Brain PDFAlvin L. RozierÎncă nu există evaluări
- PrioritiztionDocument11 paginiPrioritiztionAlvin L. RozierÎncă nu există evaluări
- Safety Infection Control Review QsDocument3 paginiSafety Infection Control Review QsAlvin L. RozierÎncă nu există evaluări
- Mental Health RemediationDocument3 paginiMental Health RemediationAlvin L. Rozier100% (2)
- PrioritiztionDocument11 paginiPrioritiztionAlvin L. RozierÎncă nu există evaluări
- Pediatric RemediationDocument5 paginiPediatric RemediationAlvin L. Rozier67% (3)
- Newborn Packet (100 Points) (5 Points)Document2 paginiNewborn Packet (100 Points) (5 Points)Alvin L. RozierÎncă nu există evaluări
- Asthma-Peak Flow MeterDocument2 paginiAsthma-Peak Flow MeterAlvin L. RozierÎncă nu există evaluări
- DKA Emergency ManagementDocument1 paginăDKA Emergency ManagementAlvin L. RozierÎncă nu există evaluări
- Learning Contract Template-2Document4 paginiLearning Contract Template-2Alvin L. RozierÎncă nu există evaluări
- PrioritiztionDocument11 paginiPrioritiztionAlvin L. RozierÎncă nu există evaluări
- Asthma Medications TableDocument7 paginiAsthma Medications TableAlvin L. RozierÎncă nu există evaluări
- Orthopaedic Cast and BracesDocument21 paginiOrthopaedic Cast and BracesAlvin L. RozierÎncă nu există evaluări
- Misc Review QsDocument4 paginiMisc Review QsAlvin L. RozierÎncă nu există evaluări
- Samplelettertoyoursenator 2Document1 paginăSamplelettertoyoursenator 2Alvin L. RozierÎncă nu există evaluări
- Lecture For Acid BaseDocument2 paginiLecture For Acid BaseAlvin L. RozierÎncă nu există evaluări
- Arguments Against Stem Cell UseDocument4 paginiArguments Against Stem Cell UseAlvin L. RozierÎncă nu există evaluări
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Research Paper Brianna BartonDocument11 paginiResearch Paper Brianna Bartonapi-530899175Încă nu există evaluări
- Thesis On HPV VaccineDocument8 paginiThesis On HPV Vaccinegjftqhnp100% (2)
- Care for a Client with LeptospirosisDocument4 paginiCare for a Client with LeptospirosisLyndon SayongÎncă nu există evaluări
- Gallbladder and Bile Duct Anatomy, Function and DiseasesDocument16 paginiGallbladder and Bile Duct Anatomy, Function and DiseasesKadenceFreya-Charisse G PosadasBulintao100% (2)
- 155 Anaesthesia For Transurethral Resection of The Prostate (TURP)Document8 pagini155 Anaesthesia For Transurethral Resection of The Prostate (TURP)Verico PratamaÎncă nu există evaluări
- AnalgesicDocument3 paginiAnalgesicAnnaMaeVelosoÎncă nu există evaluări
- Tugas AdmissionDocument9 paginiTugas Admissionputri rahayuÎncă nu există evaluări
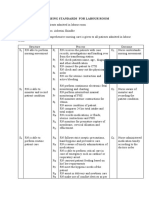
- Nursing Standards for Labour RoomDocument3 paginiNursing Standards for Labour RoomRenita ChrisÎncă nu există evaluări
- Asthma Broncial (Theophylline)Document41 paginiAsthma Broncial (Theophylline)Nadya Zahra Henni100% (1)
- Human DrugsDocument1.620 paginiHuman DrugsMohamed GameelÎncă nu există evaluări
- Nursing Documentation for Wina Purnamasari's Immunization and Vital Signs CheckDocument6 paginiNursing Documentation for Wina Purnamasari's Immunization and Vital Signs Checkilah keciÎncă nu există evaluări
- Breast and Nipple Thrush - 280720Document6 paginiBreast and Nipple Thrush - 280720Robbie WilliamsÎncă nu există evaluări
- Jdvar 08 00237Document3 paginiJdvar 08 00237Shane CapstickÎncă nu există evaluări
- How to Keep Your Heart HealthyDocument11 paginiHow to Keep Your Heart HealthyLarissa RevillaÎncă nu există evaluări
- Information Package-Nursing Practicum I STUDENTDocument36 paginiInformation Package-Nursing Practicum I STUDENTPui Pui LamÎncă nu există evaluări
- Najib Khalife - Advances in TPET and Its Immunomodulatory Effect in NMDDocument6 paginiNajib Khalife - Advances in TPET and Its Immunomodulatory Effect in NMDMarina ShinkoÎncă nu există evaluări
- Visitor Health Declaration FormDocument2 paginiVisitor Health Declaration FormKaryl Eunice Macabale IboniaÎncă nu există evaluări
- Cesarean Delivery and Peripartum HysterectomyDocument26 paginiCesarean Delivery and Peripartum HysterectomyPavan chowdaryÎncă nu există evaluări
- Diabetes TrackerDocument1 paginăDiabetes Trackerwildlifewarrior_zrsÎncă nu există evaluări
- Virtual Hematology Slide AtlasDocument57 paginiVirtual Hematology Slide Atlasdangrabell86% (7)
- ImgDocument1 paginăImgLIDIYA MOL P V100% (1)
- Lecture-4 Viral GastroenteritisDocument37 paginiLecture-4 Viral GastroenteritislolitlolatÎncă nu există evaluări
- NCA - CVA InfarctDocument126 paginiNCA - CVA InfarctRosaree Mae PantojaÎncă nu există evaluări
- CHN Exercise 1 - Paola Mariz P. CeroDocument3 paginiCHN Exercise 1 - Paola Mariz P. CeroPaola Mariz P. CeroÎncă nu există evaluări
- Amazing Health Benefits of Coconut by The Coconut Research CenterDocument6 paginiAmazing Health Benefits of Coconut by The Coconut Research CenterEuwan Tyrone PriasÎncă nu există evaluări
- Hyperglycemia in Critically Ill Management (: From ICU To The Ward)Document20 paginiHyperglycemia in Critically Ill Management (: From ICU To The Ward)destiana samputriÎncă nu există evaluări
- PsycN NBME FOrm 4 Key Points for Tardive Dyskinesia, Multiple Sclerosis, Narcolepsy, TCAsDocument2 paginiPsycN NBME FOrm 4 Key Points for Tardive Dyskinesia, Multiple Sclerosis, Narcolepsy, TCAsChristine CassidyÎncă nu există evaluări
- Atopic Dermatitis - The Epidemiology, Causes and Prevention of Atopic Eczema (PDFDrive)Document289 paginiAtopic Dermatitis - The Epidemiology, Causes and Prevention of Atopic Eczema (PDFDrive)NguyenDinh NinhÎncă nu există evaluări
- Miliaria Pustulosa (Infetrop)Document11 paginiMiliaria Pustulosa (Infetrop)Muhammad mukramÎncă nu există evaluări
- Cerebral Concussion - PresentationDocument19 paginiCerebral Concussion - PresentationAira AlaroÎncă nu există evaluări