Documente Academic
Documente Profesional
Documente Cultură
High Risk Pregnancy
Încărcat de
gracie_greys57550 evaluări0% au considerat acest document util (0 voturi)
1K vizualizări5 paginiThis document discusses nursing care for women with high-risk pregnancies. It identifies various medical conditions, family histories, and complications that can increase risk during pregnancy. It also outlines tools to assess risk factors and monitor the health of the mother and fetus, such as the Hobel risk assessment tool, ultrasounds, alpha-fetoprotein testing, amniocentesis, non-stress tests, and contraction tests. The responsibilities of nurses include obtaining consent, providing comfort, ensuring aseptic technique for invasive procedures, and interpreting test results to identify any fetal compromise or reduced oxygenation.
Descriere originală:
Notes about NURSING CARE FOR WOMEN W/ COMPLICATIONS DURING PREGNANCY
Drepturi de autor
© Attribution Non-Commercial (BY-NC)
Formate disponibile
DOC, PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentThis document discusses nursing care for women with high-risk pregnancies. It identifies various medical conditions, family histories, and complications that can increase risk during pregnancy. It also outlines tools to assess risk factors and monitor the health of the mother and fetus, such as the Hobel risk assessment tool, ultrasounds, alpha-fetoprotein testing, amniocentesis, non-stress tests, and contraction tests. The responsibilities of nurses include obtaining consent, providing comfort, ensuring aseptic technique for invasive procedures, and interpreting test results to identify any fetal compromise or reduced oxygenation.
Drepturi de autor:
Attribution Non-Commercial (BY-NC)
Formate disponibile
Descărcați ca DOC, PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
1K vizualizări5 paginiHigh Risk Pregnancy
Încărcat de
gracie_greys5755This document discusses nursing care for women with high-risk pregnancies. It identifies various medical conditions, family histories, and complications that can increase risk during pregnancy. It also outlines tools to assess risk factors and monitor the health of the mother and fetus, such as the Hobel risk assessment tool, ultrasounds, alpha-fetoprotein testing, amniocentesis, non-stress tests, and contraction tests. The responsibilities of nurses include obtaining consent, providing comfort, ensuring aseptic technique for invasive procedures, and interpreting test results to identify any fetal compromise or reduced oxygenation.
Drepturi de autor:
Attribution Non-Commercial (BY-NC)
Formate disponibile
Descărcați ca DOC, PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 5
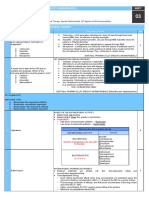
NURSING CARE FOR WOMEN W/ • Moderate to severe renal disease
COMPLICATIONS DURING PREGNANCY • Previous endocrine ablation 10
• Sickle cell disease 5
High-risk pregnancy • Epilepsy 5
-One in which the health of the mother/fetus • Heart disease NYHA class I (no
is in Jeopardy symptoms) 5
-increased risk of morbidity/mortality
• Hx of TB/PPD >10mm 5
before/after delivery
• Positive serology (for syphilis) 5
-leading cause of death and disability among
women (515,000 women/yr) • Pulmonary disease 5
-women: 30-endure injuries; infection and • Thyroid disease 5
disabilities
-early and consistent assessment for risk Family Hx
factors during prenatal visits • DM 1
Ways for identification clients at risks Physical risk factors
1. Assessment of risk factors • Incompetence cervix 10
a. Physiological • Uterine malformalities 10
b. Psychological • Maternal weight <100lbs or >200 lbs
C. Social 5
• Maternal age 35 and over 15 and
Risk Assessment Tool under 5
-Hobel, 1973 • Small pelvis 5
-risk factors are assigned a score
corresponding to the degree of risk Current pregnancy risk factors
-A score 19 or more indicates a high risk • Abnormal fetal position 10
that should receive more than routine • Moderate to severe preeclamsia 10
prenatal care • Multiple pregnancy 10
• Placenta abruption 10
OB Hx
• polylydromnios/oligohydromnios 10
Risk Factor
• excessive use of drugs/alcohol 5
• Previous still birth 10
• gestational diabetes (A1) 5
• Previous neonatal death 10
• kidney infection 5
• Previous premature infant 10
• mild preeclampsia 5
• Post term.42 weeks 10
• Rh sensitization only 5
• Fetal blood transfusion for hemolytic
disease 10 • Severe anemia <9g/dl hemoglobin
• Repeated miscarriages 5 5
• Severe flu syndrome/viral disease 5
• Previous infant >10lbs 5
• Vaginal spotting 5
• Six/more completed pregnancy 5
• Bladder infection 1
• Hx of eclampsia 5
• Emotional problem 1
• Previous cesarean section 1
• Mild anemia 9g/dl hemoglobin 1
• Hx of preeclampsia 1
• Moderate alcohol use 1
• Hx of preeclampsia 1
• Smoking > = 1 pack/day
• Hx of fetus w/ anomalies 1/0
Fetal diagnostic tests
Medical Hx
-birth defects
Risk factor
-diagnostic/screening test
• Abnormal PAP Test 10
• Chronic HPT 10 Diagnostic vs. screening
• Heart disease NYHA class II-IV Diagnostic – whether a fetus has a particular
(symptomatic) 10 condition w/ certainty but may provide
• Insulin dependent diabetes (>A2) limited information about the other types of
10 birth defects
Screening- not accurate, help to identify
patient at risk who light benefit from Low levels of AFP
diagnostic test -abnormal chromosomal or gestational
trophoblastic disease
Fetal well-being -Trisomy 21 (Down syndrome)
-fetus movements are directly r/t infant’s -Trisomy 18 (Edward's syndrome)
sleep-wake cycle vary from mother
-typical active fetal period lasts 40 min and Chorionic Villi Sampling (CVS)
peaks between 9PM and 10 PM in response -obtain a small part of developing placenta
to maternal hypoglycemia to analyze fetal cells
-10-12 weeks
Ultrasound -results = 24-48 hours
-non-invasive procedure;uses intermittent -can't determine spina bifida/anecephaly
ultrasonic waves transmitted by an -identify chromosome (abnormal)
alternating current to a transducer applied to -newborn: limb reduction defects
abdomen -Rh (D) immune globulin given to Rh-
-ultrasonic waves: defect off tissues w/in negative woman
abdomen, showing structures of varying -↑ rate spontaneous abortion than
densities amniocentesis
-requires full bladder (1-2 qts of water)
Amniocentesis
Transvaginal Ultrasound -insertion of thin needle through abdominal
-detect shortened cervical length/funelling and uterine walls (sample on amniotic fluid);
(predict preterm labor) invasive
-uses a probe inserted into vagina -15-17 weeks
-done early is pregnancy (fetal age, -early: 11-14 weeks of some disorder
suspected etopic pregnancy)
Usage (Amniocentesis)
Transabdominal Ultrasound -identify chromosome abnormalities,
-transducer biochemical disorders and level of AFP
-often scanned with full bladder (water every -spontaneous abortion
15 mins. 90mins before examination) -identify severity of maternal fetal blood
incompatibility and assess fetal lung maturity
Nursing Responsibility (UT2) -Rh (D) immune globulin given to Rh-
-inform patient about the procedure negative woman
-provide comfort and privacy
Nursing Responsibilities (Amniocentesis)
*empty bladder (transvaginal UT2) -dorsal -obtain informed consent
recumbent -provide comfort and privacy
*full bladder (transabdominal UTV) -supine full bladder, position, drape
*position -aseptic technique (hand wash, gloves)
*drape
Non-stress Test (NST)
Alpha-Fetoprotein Testing (AFP) -response of FHR to fetal movement
-maternal alpha-fetoprotein test -monitor FHR
-determine level of fetal protein in women's
serum/sample of amniotic fluid Usage of (NST)
-16-22 weeks of pregnancy -identify fetal compromise (poor placenta
function)
High levels of AFP -reassess placenta is functioning well and
-a neural tube defect oxygenated, intact CNS
spinabifidy (open supine)
anecephaly (incomplete division of *Non-reactive at risk = not good
skull and brain) *1 fetal movement = +45FHR
-defects with esophagus
-gastroschisix (baby's failure) -30-32 weeks
*Reactive= 2 accelerations of FHR with fetal -identify reduced fetal oxygenation in
movements of 15 beats/min, lasting 15 sec conditions associated with poor placental
or more for 20 min functioning
*2-15 beats-15sec-20min -↑FHR → deprivation of oxygen
-fetal hypoxia increases, FHR changes,
Contraction Test (CT) cessation
-evaluating respiratory function of placenta -amniotic fluid is reduced when placental
-identify risk for intrauterine asphyxia by function is poor
observing response of FHR to stress of fbrem, gross body movement, loss of FT
contraction A-mniocentesis
L-/S ratio
Negative- shows 3 contractions good quality O-xytocin Test
lasting 40 or more secs in 10 min without N- on-stress Test
evidence of late decelerations E-steriol level
-fetus can handle the hypoxic stress of
uterine contractions PREGNANCY AT
RISK:PREGESTAITIONAL PROBLEMS
Positive – shows repetitive persistent late
deceleration with more than 50% of Sexually Transmitted Disease (STD)
contractions -15-24y/o
-hypoxic stress cause showing FHR -↑ STD group: Sexually active youth
-Pregnant: miscarriage, premature delivery
Equivocal – non persistent late
decelerations or with hyper stimulation (2 Risk factors:
min frequency of duration longer than 90) 1. lower socio-economic status
2. lower education level
Percutaneous Umbilical Blood Sampling 3. sexual activity with multiple partners
(PUBS) 4. unsafe sexual intercourse
-anemic fetus (maternal fetal blood
incompatibility, placenta previa, abrupt Etiologic Agent: Candida Albicaus (fungus)
placentae) Candidiasis – thick yellow vaginal disharge
-blood sample from placental vessel − extreme pruritus (yeasty
or no odor)
Lecithin to Sphingomyelin (l/S) ratio Med management:
-respiratory complications in adapting 1. application of an over-the-counter
extrauterine life anti-fungal cream (Monistat) for 7
34-38 weeks days
-lung mature → ↑ lecithin ↓ Sphingomyelin 2. oral flucanozole (anti fungal)
-2:1 (normal value)
Trichomoniasis – irritation, itching
Phosphatidyl glycerol (+) - baby will not Etiologic agent: Trichomonas vagindlis
suffer respiratory distress syndrome on Signs and symptoms – profuse greenish-
delivery yellow discharge with foul odor
Effects – preterm labor, premature rapture of
Biophysical Profile (BPP) membranes, post cesarean infection
1. FHR and reactivity (NST) [reactive -
2] Med management:
2. Fetal Breathing Movement 1. metronidazole ( anti fungal)
[breathing/60sec – 2]
3. Fetal Body Movement [3 Nursing management:
movements of arms, legs, body – 2] 1. Verbalize feelings
4. Fetal Tone [ return of flexion – 2]
5. Volume of amniotic fluid [>1cm – 2] Bacterial Vaginosis
Etiologic agent – Gardenella Vaginalis
Signs and symptoms – gray discharge, fishy
odor/musty
-pruritus 2. procaine penicillin, IM, 750mg for 10
days
Effects: 3. erythromycin 500mg, 4x//day for 14
1. pelvic inflammatory disease days (allergy to penG)
2. posthysterectomy vaginal cuff 4. azithromycin 500mg, daily for 10
cellulitis days (allergy to penG)
3. endometritis
4. amniotic fluid infection Jarisch-Herxcheimer reaction
5. preterm delivery/labor -caused due to sudden destruction of
6. PROM spirochetes;last for 24 hours
7. spontaneous abortion Signs and symptoms – fever, tachycardia,
muscle aches
Med management:
1. topical – Metronidazole (Flagyl) Gonorrhea
0.75% vaginal gel etiologic agent – neissoria gonorrhoeae
Clyndamycin 2% cream Signs and symptoms – yellow-green vaginal
2. Oral – Metronidazole 500% mg (2x) discharge
- Clyndamycin 300mg (2x) effects to fetus/pregnancy:
Chlamydia
1. severe eye infection → blindness
Etiologic agent – chlamydia vaginalis 2. endocervitis
-ectopic pregnancy, preterm PROM, 3. PROM
premature delivery
-heavy gray-white discharge Med management
-cervicitis, urethritis, vaginalis, pelvic 1. oral cefixime (Suprax) 400mg, once
inflammatory disease (clinical 2. ceftriaxone (rocephin) 125-250mg,
manifestations) IM, once
-60-70% risk → infected birth canal
Effects – conjunctivitis, pneumonia Side effects: nausea, vomiting
Med management HIV/AIDS
1. tetracydin and deoxycycline -4th leading cause of death among women
2. amoxicillin – pregnant 25-44 y/o
3. aztromycin (1g) -pregnant -leading cause of death and disease world
wide, main risk factor: unsafe sex
Syphilis
Etiologic agent – treponema pallidum Stages of HIV infection:
Signs and symptoms: 1. initial invasion – flulike symptoms
• primary stage – small, hard-based 2. serocoversion- converts from having
sore no HIV antibodies
• secondary stage – skin rashes, loss -happens 6weeks-1year after exposure
of patches of hair, malaise, fever 3. asymptomatic period -weight loss,
• latent stage – asymptomatic fatigue (3-11yrs)
• tertiary stage – gumma formation 4. symptomatic period – oppurtunistic
(rubbery mass of tissue) infection occur oral and vaginal
Effects: candidiasis, Kaposi sarcoma...
1. spontaneous abortion Dx procedure:
2. still born infant a. ELISA(screening test)
3. premature labor enzyme-linked immunoabsorbent assay
4. congenital syphilis (enlarged liver, antibody detection test
spleen, skin lesions, rashes, b. western blot analysis – confirmatory test
pneumonia, hepa)
Dx:risk for infection r/t dysfunction immune
Med management: system
1. benzathine penicillinG (pregnant) Nursing management:
1. aseptic technique -ascites (leak of fluid to peritoneal act)
2. administration of med as prescribed -peripheral edema
3. provide health care education on:
-breastfeeding Effect to fetus:
-protected sexual activity 1. low birth weight
2. abortion
Nursing management for STD 3. intrauterine growth retardation
1. assessment Hx taking (multiply 4. still birth
partners, unprotected sex) 5. premature labor
2. Dx = knowledge deficit Med management:
3. intervention: 1. Digoxin – to slow ventricular
-discuss causes of STD:multiply partners response and to increase
-teach about proper hygiene:perineal and myocardial contractility
hand washing 2. diuretics -for acute and chronic
-sensitivity, confidentiality heart failure
-counseling before and after testing allay 3. beta-adrenergic blockers
fears (propandol) – arrhythmia associated
-provide accurate information with ischemic heart disease
-provide referral to needed medical and 4. amonophylline – relives
psychological services bronchospasm
5. heparin- with artificial valves or
Cardiovascular Diseases artrial fibrillation
-total blood volume: at least 30%
-iron requirement: 800mg Surgical management:
-cardiac output by 25%-50%, increase heart 1. therapeutic abortion -Class II and IV
rate 2. cardiac surgery – alternative to the
therapeutic abortion
NYHA -closed cardiac surgery is preferred
Class I – no discomfort (dyspnea,
palpitation, anginal pain) on ordinary act Nursing management:
Class II – discomfort on ordinary act 1. monitor fetal well being (9PM-10AM)
Class III- discomfort on less than ordinary 2. promote rest
act 3. promote healthy nutrition – low
Class IV- dyspnea at rest. Patient is sodium diet
decompensated 4. instruct about avoiding infection
Effects to mother:
Left-sided H.F.
-edema
-Prod cough of blood-speckled sputum
-orthopnea
-increase RR
-fatigue
-dizziness
-weakness
-paroxysmal nocturnal dyspnea
Right-sided H.F. -there you go. Aralin niyo yan! :))
-jugular vein distension
-hepatomegaly ©BSN-2H notes
-extreme dyspnea
-pain
S-ar putea să vă placă și
- Preparation and Education for Parenthood: A Pathway to Understanding the Carer's Role in Infant EducationDe la EverandPreparation and Education for Parenthood: A Pathway to Understanding the Carer's Role in Infant EducationEvaluare: 5 din 5 stele5/5 (1)
- Stages of Labor Nursing ConsiderationsDocument5 paginiStages of Labor Nursing Considerationsneleh gray100% (2)
- 1st Lecture High Risk Prenatal Client (NCM102)Document6 pagini1st Lecture High Risk Prenatal Client (NCM102)Jc Mendiola100% (3)
- High Risk PregnancyDocument2 paginiHigh Risk PregnancyCaren ReyesÎncă nu există evaluări
- Intrapartum 2003Document76 paginiIntrapartum 2003Karla Jane100% (2)
- Lesson 2 Care of The FetusDocument28 paginiLesson 2 Care of The FetusJohn CarloÎncă nu există evaluări
- Dona 1 CmcaDocument29 paginiDona 1 CmcaKyra MercadoÎncă nu există evaluări
- Amniotic Band SyndromeDocument47 paginiAmniotic Band SyndromeNazrul Islam JhinukÎncă nu există evaluări
- Rubella and PregnancyDocument6 paginiRubella and PregnancyKABERA RENEÎncă nu există evaluări
- Postpartum Complications FinalDocument30 paginiPostpartum Complications Finaljacquelinearah100% (1)
- Normal Postpartum Changes Parameter First 24 H Clinical Heart RateDocument14 paginiNormal Postpartum Changes Parameter First 24 H Clinical Heart RatemiacajÎncă nu există evaluări
- Immediate Newborn Care-DOH 2010Document2 paginiImmediate Newborn Care-DOH 2010fegerilene100% (2)
- Maternal and Child Health CareDocument73 paginiMaternal and Child Health CareKaren Mae Santiago AlcantaraÎncă nu există evaluări
- NURS 1124 Sp17Document81 paginiNURS 1124 Sp17Orange AlvarezÎncă nu există evaluări
- Health Educ Handout #11Document3 paginiHealth Educ Handout #11Ram AugustÎncă nu există evaluări
- Essential Newborn CareDocument5 paginiEssential Newborn CareElaine Iris AbastaÎncă nu există evaluări
- Management of Normal Labor and DeliveryDocument40 paginiManagement of Normal Labor and Deliveryrendyprimananda840Încă nu există evaluări
- Physiology of MenstruationDocument6 paginiPhysiology of MenstruationgmindalanoÎncă nu există evaluări
- Newborn ScreeningDocument20 paginiNewborn Screeningfeva55Încă nu există evaluări
- Intrapartum AssesmentDocument71 paginiIntrapartum AssesmentHusain ChherawalaÎncă nu există evaluări
- RH IncompatibilityDocument3 paginiRH IncompatibilityMima Fatimah LuthfieÎncă nu există evaluări
- Maternal Nursing Care - CHPT 12 The Process of Labor and BirthDocument45 paginiMaternal Nursing Care - CHPT 12 The Process of Labor and Birththubtendrolma100% (6)
- Unang YakapDocument7 paginiUnang YakapApol AstigÎncă nu există evaluări
- BSN Level III Clinical InstructorDocument33 paginiBSN Level III Clinical InstructorChristine Bell JapitanaÎncă nu există evaluări
- Week 8.4 MCNDocument12 paginiWeek 8.4 MCNZxiayieee JeonÎncă nu există evaluări
- PostpartumDocument3 paginiPostpartumMuhammad RifaiÎncă nu există evaluări
- CPM16TH Intrapartum and Immediate Postpartum CareDocument25 paginiCPM16TH Intrapartum and Immediate Postpartum CarespringdingÎncă nu există evaluări
- Postpartum HemorrhageDocument7 paginiPostpartum Hemorrhagekman0722Încă nu există evaluări
- Assessing The Newborn and Infant-NewDocument11 paginiAssessing The Newborn and Infant-NewJan Jamison ZuluetaÎncă nu există evaluări
- Complications in PregnancyDocument81 paginiComplications in PregnancyTia TahniaÎncă nu există evaluări
- Ch10Document38 paginiCh10Bridget Shienne DaculaÎncă nu există evaluări
- Maternal and Child HealthDocument60 paginiMaternal and Child HealthStar AcademyÎncă nu există evaluări
- Ps of LaborDocument28 paginiPs of LaborErvina Luisa Delias CampusÎncă nu există evaluări
- 5 - Care of The Mother and The FetusDocument36 pagini5 - Care of The Mother and The FetusMa Nelia P Magsino100% (2)
- Postpartum Blues: by DR Wangari KuriaDocument9 paginiPostpartum Blues: by DR Wangari KuriaRahul Kumar DiwakarÎncă nu există evaluări
- Assessment of The BreastDocument11 paginiAssessment of The BreastSIR ONEÎncă nu există evaluări
- 3rd and 4th Stage of LaborDocument8 pagini3rd and 4th Stage of LaborMarco Paulo Reyes NaoeÎncă nu există evaluări
- Malpresentation and Malposition - PostmaturityDocument29 paginiMalpresentation and Malposition - PostmaturityNishaThakuriÎncă nu există evaluări
- IntrapartumDocument17 paginiIntrapartumIris CaberteÎncă nu există evaluări
- Abortion Nursing Care Planning and ManagementDocument11 paginiAbortion Nursing Care Planning and ManagementSyamsiah ChandrawatiÎncă nu există evaluări
- Maternal and Child Nursing 1 Skills Lab Modele s1Document3 paginiMaternal and Child Nursing 1 Skills Lab Modele s1Crystal MaidenÎncă nu există evaluări
- Abruptio Placenta and AbortionDocument10 paginiAbruptio Placenta and Abortiondanica grace gubaÎncă nu există evaluări
- Physical AssessmentDocument90 paginiPhysical AssessmentReann LeeÎncă nu există evaluări
- Newborn AssessmentDocument10 paginiNewborn Assessmentapi-508446364Încă nu există evaluări
- Maternal Notes Google DocsDocument24 paginiMaternal Notes Google DocsOracion, Bernette Meiji B.Încă nu există evaluări
- High Risk Newborn2Document15 paginiHigh Risk Newborn2Catherine Villanueva Sta Monica100% (1)
- Postpartum Nursing PowerpointDocument3 paginiPostpartum Nursing PowerpointAntonella VitaleÎncă nu există evaluări
- Pharamacology Notes 3Document7 paginiPharamacology Notes 3Martinet CalvertÎncă nu există evaluări
- NonStress TestDocument2 paginiNonStress TestRama_ichiÎncă nu există evaluări
- Family PlanningDocument13 paginiFamily PlanningYana PotÎncă nu există evaluări
- High Risk Pregnancy FinaleDocument149 paginiHigh Risk Pregnancy FinaleQuolette Constante100% (1)
- RH IncompatibilityDocument9 paginiRH IncompatibilityJohn BardeenÎncă nu există evaluări
- Hyperemesis GravidarumDocument16 paginiHyperemesis GravidarumBabi PanggangÎncă nu există evaluări
- 2 - Maternal Fetal Triage Index - RuhlDocument26 pagini2 - Maternal Fetal Triage Index - RuhlGirish SinghÎncă nu există evaluări
- Antepartum BleedingDocument37 paginiAntepartum BleedingMae Importers IncÎncă nu există evaluări
- Fanconi Anemia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDe la EverandFanconi Anemia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsÎncă nu există evaluări
- MATERNAL AND CHILD HEALTH NURSE: Passbooks Study GuideDe la EverandMATERNAL AND CHILD HEALTH NURSE: Passbooks Study GuideÎncă nu există evaluări
- Health History Form: Personal Information - Applicant Complete This SectionDocument2 paginiHealth History Form: Personal Information - Applicant Complete This SectionFilip MeđimorecÎncă nu există evaluări
- Pelvic Inflammatory DiseaseDocument5 paginiPelvic Inflammatory DiseaseRahma Rafina100% (2)
- BMBL-5th EditionDocument421 paginiBMBL-5th EditionBryan OngÎncă nu există evaluări
- Peripheral Neuropathy Diff Diagnosis and Management AafpDocument6 paginiPeripheral Neuropathy Diff Diagnosis and Management Aafpgus_lions100% (1)
- NARRATIVE REPORT-scouts Against Dengue2013Document4 paginiNARRATIVE REPORT-scouts Against Dengue2013larybagsÎncă nu există evaluări
- Diagnosa Icd - 10Document2 paginiDiagnosa Icd - 10Yoery SadewoÎncă nu există evaluări
- Early Diagnosis of CancerDocument15 paginiEarly Diagnosis of Cancerkishore13Încă nu există evaluări
- HTMLEDocument8 paginiHTMLEkthmntsÎncă nu există evaluări
- Sparvix Publishing House ProjectDocument100 paginiSparvix Publishing House ProjectDhiraj PatilÎncă nu există evaluări
- Appendicitis Clinical Presentation - History, Physical Examination, Appendicitis and PregnancyDocument7 paginiAppendicitis Clinical Presentation - History, Physical Examination, Appendicitis and PregnancyotakmesumÎncă nu există evaluări
- Important Double Fillers New Pattern Questions For Mains ExamDocument21 paginiImportant Double Fillers New Pattern Questions For Mains ExamTejashwini JÎncă nu există evaluări
- In-Vitro Anthelmintic Activity of Diplazium Esculentum (Retz.)Document4 paginiIn-Vitro Anthelmintic Activity of Diplazium Esculentum (Retz.)Nur Jannah KhairunnisaÎncă nu există evaluări
- Caso NEJM 27-2017Document9 paginiCaso NEJM 27-2017Leonardo PgÎncă nu există evaluări
- Ontimmunol09 01837Document17 paginiOntimmunol09 01837akshayajainaÎncă nu există evaluări
- 17 Alterations With Infectious Inflammatory and Immunologic ResponsesDocument100 pagini17 Alterations With Infectious Inflammatory and Immunologic ResponsesBea Bianca Cruz100% (1)
- 3 GENPATHO To Be PrintDocument25 pagini3 GENPATHO To Be PrintDENTAL REVIEWER ONLYÎncă nu există evaluări
- Drug StudyDocument9 paginiDrug StudyStephanie ValerioÎncă nu există evaluări
- Pharma S03 SBR01 Le1Document15 paginiPharma S03 SBR01 Le1sky vallartaÎncă nu există evaluări
- Technical Guide: Sputum Examination For Tuberculosis by Direct Microscopy in Low Income CountriesDocument32 paginiTechnical Guide: Sputum Examination For Tuberculosis by Direct Microscopy in Low Income CountriesRevix Adalah Ita'Încă nu există evaluări
- Date 12/jun/2021 12:38PM Unit Bio Ref Interval: Laboratory Investigation ReportDocument7 paginiDate 12/jun/2021 12:38PM Unit Bio Ref Interval: Laboratory Investigation ReportKaran PrabhakarÎncă nu există evaluări
- Impact Defense Core - Michigan7 2013 HJPPDocument221 paginiImpact Defense Core - Michigan7 2013 HJPPdeabtegoddÎncă nu există evaluări
- Answers To Virology MCQ Paper 2Document8 paginiAnswers To Virology MCQ Paper 2Idrissa ContehÎncă nu există evaluări
- Acute GlomerulonephritisDocument11 paginiAcute GlomerulonephritisppnidemakÎncă nu există evaluări
- Ebola Outbreak Analyzing The Data WorksheetDocument2 paginiEbola Outbreak Analyzing The Data Worksheetapi-262360890Încă nu există evaluări
- How to look 「皮疹」Document50 paginiHow to look 「皮疹」Satoshi KobayashiÎncă nu există evaluări
- CDCDocument116 paginiCDCRam BasanyÎncă nu există evaluări
- Red Biotechnology ProjectDocument5 paginiRed Biotechnology ProjectNeveen Kandil100% (2)
- Origin of Replication: Gram Negative Bacterial PlasmidsDocument12 paginiOrigin of Replication: Gram Negative Bacterial PlasmidsMagesh RamasamyÎncă nu există evaluări
- Prenatal Practice Guidelines: Primary Source: AAP/ACOG Guidelines For Perinatal Care, 5 Edition, 2002Document5 paginiPrenatal Practice Guidelines: Primary Source: AAP/ACOG Guidelines For Perinatal Care, 5 Edition, 2002filberts.girl9025Încă nu există evaluări
- Microbial Diseases of The Urinary and Reproductive SystemsDocument139 paginiMicrobial Diseases of The Urinary and Reproductive Systemsone_nd_onlyuÎncă nu există evaluări