Documente Academic
Documente Profesional
Documente Cultură
Ca Prostat
Încărcat de
Siti Ncit0 evaluări0% au considerat acest document util (0 voturi)
14 vizualizări4 paginibedah
Titlu original
ca prostat
Drepturi de autor
© © All Rights Reserved
Formate disponibile
DOCX, PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentbedah
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca DOCX, PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
14 vizualizări4 paginiCa Prostat
Încărcat de
Siti Ncitbedah
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca DOCX, PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 4
Chemotherapy
Chemotherapy is the also used against prostate cancer.
The utility of chemotherapy in the management of metastatic prostate cancer has not been
thoroughly defined.
This therapeutic option has been explored most in patients with hormone-resistant disease.
Newer chemotherapy medicines, such asdocetaxel (Taxotere), have shown some promise in
prolonging the survival of some patients with extensive prostate cancer. They may also decrease
the pain related to widespread cancer. However, this comes at the cost of significant side effects
that may impact quality of life.
Symptom palliation: The primary approach to the management of symptoms in patients with
advanced prostate cancer is systemic therapy. For patients with castrate-resistant prostate cancer,
palliative therapy may be indicated to treat symptomatic bone metastases or symptoms arising
from progressive pelvic disease.
Prostate Cancer Follow-up
Follow-up care is especially important for patients who opted for a more conservative approach
(such as watchful waiting) to treat prostate cancer. It is imperative that a man see his urologist
for digital rectal exams, PSA level tests, and other tests as recommended to follow the
progression of cancer growth.
For men who have undergone radical prostatectomy, radiation therapy, or both, follow-up care is
important to prevent cancer recurrence.
PSA has been shown to be useful in detecting recurrences. PSA levels should be less than 0.2
ng/mL after radical prostatectomy.
PSA levels should be checked every 3 months for 1 year, every 6 months for the second year,
and annually after that.
A man should have a physical examination, including digital rectal exam, every 3 months for
1 year, then every 6 months for a year, then yearly after that.
In certain cases after radical prostatectomy, additional treatment may be required based on the
final pathology report of the removed prostate or if the PSA starts increasing after surgery.
This may be in the form of additional radiation treatment to the area where the prostate once
was and/or hormonal treatment with LHRH agonists or antiandrogens as mentioned earlier.
Prostate Cancer Prevention
The high lifetime risks of prostate cancer development, the morbidities associated with treatment
of established prostate cancer, and the inability to eradicate life-threatening metastatic prostate
cancer offer compelling reasons for prostate cancer prevention.
However, because the cause of prostate cancer is uncertain, preventing prostate cancer may not
be possible. Certain risk factors, such as age, race, sex, and family history, cannot be changed.
Nevertheless, because diet and other lifestyle factors have been implicated as a potential cause,
living a healthy lifestyle may afford some protection.
Proper nutrition, such as limiting intake of foods high in animal fats and increasing the amount
of fruits, vegetables, and grains, may help reduce the risk of prostate cancer.
The following supplements should NOT be used to prevent prostate cancer:
o Vitamin E
o Selenium
o Vitamin C
5-alpha reductase Inhibitors (5-ARI):
Using 5-ARIs for prostate cancer is controversial.
Initial studies have shown that finasteride decreased the risk of developing prostate cancer by
25% (Prostate Cancer Prevention Trial). However, initial reports indicated that high-grade
prostate cancer was more likely to occur in men treated with finasteride. Even though this
increased risk with finasteride may be due to a selection bias, there is no proof that finasteride
would not increase the true incidence of high-grade cancer.
In the Reduction by Dutasteride of Prostate Cancer Events (REDUCE) trial, dutasteride
decreased the risk of developing Gleason score 5 to 6 cancer but not Gleason 7 to 10 cancer.
In both trials 5-ARIs increased the risk of erectile dysfunction and loss of libido.
Although it is possible that 5-ARIs reduced the risk of being diagnosed with prostate cancer, it
is unknown if this will translate into reduced mortality.
5-ARIs are not FDA approved for the prevention of prostate cancer.
Prostate Cancer Prognosis
Patient
The prognosis in prostate cancer depends on the stage of the cancer and the degree of
differentiation.
Differentiation refers to how closely the cancer resembles normal tissue. This is assessed by
calculating the Gleason score as mentioned earlier. The less differentiated the cancer, the
poorer the prognosis.
The stage refers to the extent of the cancer -- whether it is localized or has spread beyond the
prostate. The greater the degree of cancer spread, the poorer the outlook.
5-year survival rates are very good for men with prostate cancer.
According to the American Cancer Society, 92% of men with these cancers survive at least 5
years.
Most prostate cancers are slow growing, as shown by the fact that 67% of men with prostate
cancer survive at least 10 years.
Sometimes, however, prostate cancers grow and spread rapidly. Therefore, early diagnosis is
essential for a cure.
If a man is elderly and has other medical conditions, watchful waiting may be the most prudent
course.
Therapy may be more harmful than the cancer.
This is especially true if a man's life expectancy is less than 10 years.
Many times, elderly men with prostate cancer actually die of something else, such as heart
disease, not the slow-growing prostate cancer.
A man and his family members should discuss this with his urologist.
Support Groups and Counseling
Living with cancer presents many new challenges for a man and for his family and friends.
A man will probably have many worries about how the cancer will affect him and his ability
to live a normal life, that is, to care for his family and home, to hold his job, and to continue
the friendships and activities he enjoys.
Many people feel anxious and depressed. Some people feel angry and resentful; others feel
helpless and defeated.
For most people with cancer, talking about their feelings and concerns helps.
Friends and family members can be very supportive. They may be hesitant to offer support
until they see how the man with cancer is coping. Don't wait for them to bring it up. If one
wants to talk about their concerns, let them know.
Some people don't want to burden their loved ones or prefer talking about their concerns with
a more neutral professional. A social worker, counselor, or member of the clergy can be
helpful if a man wants to discuss his feelings and concerns about having cancer. A urologist or
oncologist should be able to recommend someone.
Many people with cancer are profoundly helped by talking to other people who have cancer.
Sharing one's concerns with others who have been through the same thing can be remarkably
reassuring. Support groups of people with cancer may be available through the medical center
where one receives treatment. The American Cancer Society also has information about
support groups all over the U.S.
Hormone Therapy
Prostate cells are physiologically dependent on androgens hormonal stimulation to grow,
function, and proliferate. Testosterone, although not tumorigenic, is essential for the growth and
perpetuation of tumor cells. The testes are the source of most androgens. The goal of hormonal
therapy is to lower levels of testosterone or to stop testosterone from working. This can be
achieved with surgery or with drug treatment. Often, the initial response is good, but cancer may
progress over time.
Androgen deprivation therapy: This therapy is likely to be used in cases in which the cancer
has spread to distant regions. Therefore, it is not currently used among the standard options for
men with localized prostate disease.
The testes produce much of the testosterone that stimulates cancer growth. Surgical removal
of both testicles (castration, or orchiectomy) is the best way to stop hormonal stimulation of
the tumor.
Men usually prefer medical castration to surgical castration. A variety of agents have been
used to suppress androgen levels acting at different levels of hormonal production and release.
o Nowadays, GnRH agonists are the most widely used. They induce a medical castration by
suppressing luteinizing hormone production and, therefore, the synthesis of testicular
androgens. A number of GnRH agonists are available (leuprolide,goserelin, buserelin,
and triptorelin).
o GnRH antagonists (degarelix) may be beneficial in cases when immediate decrease in
testosterone levels is required.
o Estrogen, in the form of diethylstilbestrol, can also be used to suppress testosterone.
Because of its extensive side effects, estrogen is not used very often.
Antiandrogen monotherapy: Antiandrogens bind to androgen receptors and competitively
inhibit their interaction with male hormones (testosterone anddihydrotestosterone).
o Unlike medical castration, antiandrogen therapy does not decrease luteinizing hormone
(LH) levels and androgen production. Rather, testosterone levels are normal or increased.
Thus, men treated with antiandrogen monotherapy do not have the full spectrum of side
effects attributable to low levels of testosterone, and many maintain some degree of
potency.
o These agents are usually used in combination with a GnRH agonist either continuously or
for 2 to 4 weeks during the initiation of treatment with a GnRH agonist. This is also known
as "complete androgen blockade."
o The most common agents are flutamide (Eulexin), bicalutamide(Casodex) and nilutamide.
Drugs that stop the adrenal glands from making androgens are sometimes used.
Side effects of these medications vary. Orchiectomy and LHRH agonists may cause
impotence, hot flashes, and loss of sexual desire, osteoporosis, and bone fractures.
Antiandrogens may cause nausea, vomiting, diarrhea, and breast enlargement or tenderness.
Any of these therapies can weaken bones.
S-ar putea să vă placă și
- Monitoring KebersihanDocument1 paginăMonitoring KebersihanSiti NcitÎncă nu există evaluări
- Denah TanahDocument1 paginăDenah TanahSiti NcitÎncă nu există evaluări
- Drug DosesDocument2 paginiDrug DosesSiti NcitÎncă nu există evaluări
- Gut EmbryologyDocument2 paginiGut EmbryologySiti NcitÎncă nu există evaluări
- Journal ReadingDocument20 paginiJournal ReadingSiti NcitÎncă nu există evaluări
- SprainsDocument1 paginăSprainsSiti NcitÎncă nu există evaluări
- Laporan Kasus: Karsinoma Serviks Stadium IiibDocument1 paginăLaporan Kasus: Karsinoma Serviks Stadium IiibSiti NcitÎncă nu există evaluări
- Bahasan Kelainan Refraksi NcitDocument11 paginiBahasan Kelainan Refraksi NcitSiti NcitÎncă nu există evaluări
- P ('t':'3', 'I':'3054269692') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Document1 paginăP ('t':'3', 'I':'3054269692') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Siti NcitÎncă nu există evaluări
- Understanding RetinopathyDocument64 paginiUnderstanding RetinopathySiti NcitÎncă nu există evaluări
- Leuk o CoriaDocument47 paginiLeuk o CoriaAsa Ngah AsyaÎncă nu există evaluări
- Bahasan Kelainan Refraksi NcitDocument11 paginiBahasan Kelainan Refraksi NcitSiti NcitÎncă nu există evaluări
- Risk Factors and Management of Acute Kidney Injury in the ElderlyDocument15 paginiRisk Factors and Management of Acute Kidney Injury in the ElderlySiti NcitÎncă nu există evaluări
- Kala ZionDocument4 paginiKala ZionSiti NcitÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Tricorder X PrizeDocument4 paginiTricorder X PrizemariaÎncă nu există evaluări
- Shnider and Levinsons Anesthesia For Obstetrics, 5th EdDocument879 paginiShnider and Levinsons Anesthesia For Obstetrics, 5th EdSri Hari50% (2)
- The Federation of Motor Sports Clubs of India 2022 Appendix "B" - Medical HistoryDocument2 paginiThe Federation of Motor Sports Clubs of India 2022 Appendix "B" - Medical HistoryMBG No.14Încă nu există evaluări
- Branches of Medicine & Wards and Departements - EditkuDocument31 paginiBranches of Medicine & Wards and Departements - EditkuGigih Sanjaya PutraÎncă nu există evaluări
- Wojejuterer Health Assessment in Nursing 5th Edition PupegDocument3 paginiWojejuterer Health Assessment in Nursing 5th Edition Pupegace Decla100% (1)
- Interview QuestionsDocument7 paginiInterview QuestionsRitesh KumarÎncă nu există evaluări
- MCR FormDocument2 paginiMCR FormJi Keon LooiÎncă nu există evaluări
- 1457792866immediate DenturesDocument5 pagini1457792866immediate DenturesegarochmawatiÎncă nu există evaluări
- Minutes of Meeting November 2020Document2 paginiMinutes of Meeting November 2020Jonella Anne CastroÎncă nu există evaluări
- Chappuis Et Al-2017-Periodontology 2000Document11 paginiChappuis Et Al-2017-Periodontology 2000Tommaso GazzoloÎncă nu există evaluări
- 2008 Polyflux R Spec Sheet - 306150076 - HDocument2 pagini2008 Polyflux R Spec Sheet - 306150076 - HMehtab AhmedÎncă nu există evaluări
- Spotters 1Document10 paginiSpotters 1elavarkuzhali2019Încă nu există evaluări
- Grade 6 WHLP 5Document14 paginiGrade 6 WHLP 5Benj AlejoÎncă nu există evaluări
- Therapeutic and Toxic Blood Levels of Over 800 DrugsDocument28 paginiTherapeutic and Toxic Blood Levels of Over 800 DrugsAndreia AndreiutzaÎncă nu există evaluări
- Case study on Congestive Cardiac Failure managementDocument19 paginiCase study on Congestive Cardiac Failure managementk_472894540Încă nu există evaluări
- Cameroon: Maternal and Newborn Health DisparitiesDocument8 paginiCameroon: Maternal and Newborn Health Disparitiescadesmas techÎncă nu există evaluări
- 4-File3-Document 0 Dossier Robert F.Kennedy JR Du 05-02-2020 V.finaleDocument6 pagini4-File3-Document 0 Dossier Robert F.Kennedy JR Du 05-02-2020 V.finaleVINYO ADANDOGOUÎncă nu există evaluări
- The Expanded Program On ImmunizationDocument26 paginiThe Expanded Program On ImmunizationJudee Marie MalubayÎncă nu există evaluări
- Normothermia Audit Tool: AHRQ Safety Program For SurgeryDocument3 paginiNormothermia Audit Tool: AHRQ Safety Program For SurgeryDewi ListyoriniÎncă nu există evaluări
- Nursing Care StudyDocument20 paginiNursing Care StudyAnjaliÎncă nu există evaluări
- Fraktur DentoalveolarDocument25 paginiFraktur DentoalveolarfirmansyahddsÎncă nu există evaluări
- Monograph GarlicDocument2 paginiMonograph GarlicJoann PortugalÎncă nu există evaluări
- Prescription AnalysisDocument16 paginiPrescription AnalysisMohd Azfar HafizÎncă nu există evaluări
- Medicina Paliativa Walsh - Comprimido PDFDocument1.507 paginiMedicina Paliativa Walsh - Comprimido PDFMaría Isabel GarcíaÎncă nu există evaluări
- CH13 Ninenth Standard NCERT BOOKDocument26 paginiCH13 Ninenth Standard NCERT BOOKPrash ShanthÎncă nu există evaluări
- КРАТКИЙ КУРС ПАТОМОРФОЛОГИИ ЧАСТЬ 1 ENGDocument214 paginiКРАТКИЙ КУРС ПАТОМОРФОЛОГИИ ЧАСТЬ 1 ENGRishik RanaÎncă nu există evaluări
- Patofisiologi HIV Dan AIDSDocument24 paginiPatofisiologi HIV Dan AIDSElidia dewiÎncă nu există evaluări
- Swallowing Rehabilitation Following Spinal Injury A Case SeriesDocument12 paginiSwallowing Rehabilitation Following Spinal Injury A Case SeriesniekoÎncă nu există evaluări
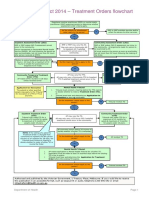
- Flowchart - Mental Health Act Treatment OrderDocument1 paginăFlowchart - Mental Health Act Treatment OrderEdwin100% (1)
- Central SensitizationDocument14 paginiCentral SensitizationdracoscribdÎncă nu există evaluări