Documente Academic
Documente Profesional
Documente Cultură
Devising The Optimal Preclinical Oncology Curriculum For Undergraduate Medical Students in The United States
Încărcat de
arakbae0 evaluări0% au considerat acest document util (0 voturi)
12 vizualizări9 paginiDevising the Optimal Preclinical Oncology Curriculum for Undergraduate Medical Students in the United States
Titlu original
Devising the Optimal Preclinical Oncology Curriculum for Undergraduate Medical Students in the United States
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDevising the Optimal Preclinical Oncology Curriculum for Undergraduate Medical Students in the United States
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
12 vizualizări9 paginiDevising The Optimal Preclinical Oncology Curriculum For Undergraduate Medical Students in The United States
Încărcat de
arakbaeDevising the Optimal Preclinical Oncology Curriculum for Undergraduate Medical Students in the United States
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 9
Devising the Optimal Preclinical Oncology Curriculum
for Undergraduate Medical Students in the United States
Nicholas J. DeNunzio & Lija Joseph & Roxane Handal &
Ankit Agarwal & Divya Ahuja & Ariel E. Hirsch
Published online: 18 May 2013
#Springer Science+Business Media New York 2013
Abstract A third of women and a near majority of men in
the United States will be diagnosed with cancer in their
lifetimes. To prepare future physicians for this reality, we
have developed a preclinical oncology curriculum that intro-
duces second-year medical students to essential concepts
and practices in oncology to improve their abilities to ap-
propriately care for these patients. We surveyed the oncolo-
gy and education literature and compiled subjects important
to students' education including basic science and clinical
aspects of oncology and addressing patients' psychosocial
needs. Along with the proposed curriculum content, sched-
uling, independent learning exercises, and case studies, we
discuss practical considerations for curriculum implementa-
tion based on experience at our institution. Given the chang-
ing oncology healthcare landscape, all (new) physicians
must competently address their cancer patients' needs, re-
gardless of chosen specialty. A thorough and logically or-
ganized cancer curriculum for preclinical medical students
should help achieve these aims. This new model curriculum,
with accompanying strategies to evaluate its efforts, is es-
sential to update how medical students are educated about
cancer.
Keywords Oncology
.
Curriculum
.
Undergraduate medical
students
.
United States
Introduction
Undergraduate medical education is the cornerstone for
training the next generation of physicians to care for healthy
and ailing members of our society. Medical school curricula
aim to develop students basic and clinical sciences knowl-
edge as well as their professional and clinical skills. Al-
though some fields are systems-based, many others, such as
oncology, are trans-disciplinary and demand mastery of
several topics in parallel.
Cancer patients currently compose a significant subset of
those seeking medical care. In the United States approximate-
ly half of men and a third of women will be diagnosed with
cancer during their lifetimes while about one in five will die of
cancer [1]. Furthermore, as projected by the World Health
Organization, 26 million people worldwide will receive a
cancer diagnosis in the year 2030 alone [2]. Therefore, all
practicing physicians should be able to diagnose cancer and
have at least a basic appreciation for how to address cancer
patients needs, regardless of whether they will serve as the
primary provider or refer the patient to a specialist.
Implementing a cancer curriculum for undergraduate med-
ical students to address these issues was proposed as early as
24 years ago in Europe [3] and addressed more recently by
reviewing published teaching efforts [4]. Cancer education
guidelines for undergraduate medical students over the dura-
tion of their formal education have been developed in Aus-
tralia [5]. However, the Australian recommendations do not
provide council for timely integration of concepts to appro-
priately prepare students for each stage of their schooling.
A detailed outline of basic science and clinical concepts,
as well as social and emotional issues, for training medical
oncologists in the United States [6] is too detailed in many
areas for effectively educating undergraduate medical stu-
dents. In addition, few undergraduate medical curricula
emphasizing oncology in some capacity are available from
the Curriculum Management and Information Tool available
J Canc Educ (2013) 28:228236
DOI 10.1007/s13187-012-0442-0
N. J. DeNunzio
:
R. Handal
:
A. Agarwal
:
D. Ahuja
:
A. E. Hirsch (*)
Department of Radiation Oncology, Boston University School
of Medicine, 830 Harrison Avenue, Moakley Building LL,
Boston, MA 02118, USA
e-mail: Ariel.hirsch@bmc.org
L. Joseph
Department of Pathology and Laboratory Medicine, Boston
University School of Medicine, 715 E. Concord Street,
Boston, MA 02118, USA
through the Association of American Medical Colleges [7].
Consequently, the development of a curriculum specific to
undergraduate medical students that exposes students to
basic concepts in caring for their cancer patients is essential
prior to their clinical rotations [8, 9].
Some medical schools have begun to integrate aspects of
cancer curricula into their undergraduate medical education
courses with specific learning objectives [10, 11]. At our
institution, we have developed a formal preclinical oncology
curriculum for undergraduate medical students to systemat-
ically address both traditional basic science coursework and
elements essential to providing holistic care to complex
cancer patients. Despite the increasingly blurred lines de-
marcating preclinical and clinical portions of undergraduate
medical education curricula, preclinical here refers to the
first two years during which students traditionally spend the
bulk of their time in a classroom setting.
The revised curriculum proposed here, modeled from that
mentioned above, is an attempt at tailoring concepts and
methods in oncology education to fulfill unmet needs. In an
effort to achieve this end, the curriculum addresses many of
the requirements deemed important by the Licensing Com-
mittee for Medical Education (LCME) for sound develop-
ment of an undergraduate medical curriculum [12] as well as
many of the professional competencies emphasized and
developed by the Accreditation Council for Graduate Med-
ical Education (ACGME; Fig. 1a) for residency programs
[13, 14]. We hope readers find this curriculum and sug-
gested evaluation techniques helpful in their efforts to im-
prove cancer education domestically and globally.
Cancer Education in the United States
Existing cancer curricula at some medical schools in the United
States during preclinical education focus differentially on can-
cer prevention and cancer survivorship. After the American
Association for Cancer Education published recommendations
based on a Cancer Education Survey of 126 medical schools, a
few medical schools made curriculum reforms to increase can-
cer prevention and screening education [10]. Boston University
incorporated an additional nine hours of lectures, case-based
learning, and skills laboratories on cancer prevention and
screening. As a result, self-reported skill level for counseling
tobacco cessation, tobacco prevention, sun protection and early
detection of breast, skin, and cervical cancer increased [15]. The
University of CaliforniaLos Angeles (UCLA) implemented a
similar curriculum reformand survey evaluations showed skills
practice was the greatest contributor to improvement in cancer
prevention and screening competency as perceived by the study
participants [11].
While there have been multiple advances in the area of
cancer prevention and screening, education on survivorship
has been limited. In fact, a literature search identified
only one comprehensive curriculum on the latter topic.
It describes a survey and knowledge-based examination
of 211 senior medical students from UCLA, University
of CaliforniaSan Francisco (UCSF), and Drew Univer-
sity that show that 42 % displayed no or incorrect
knowledge about basic survivorship terminology and
37 % lacked knowledge of essential elements of a
comprehensive cancer history. The majority also felt
unprepared to manage the long-term care of cancer
patients [16]. In response to this dearth in cancer survivorship
education, UCLA, UCSF, and Drew created a four-year inte-
grated cancer survivorship curriculum under the National
Cancer Institute Cancer Education Grants Program (R25).
The curriculum is based on individual units consisting of
lectures, problem-based learning exercises, and standardized
patient exercises throughout medical school [17]. However,
even this expansive and much-needed curricular innovation
focuses on only cancer survivorship education and in a scat-
tered modular style rather than in the style of a dedicated,
much more inclusive oncology block.
Fig. 1 a Pie chart depicting the six ACGME competencies fulfilled by
graduate medical education programs. b Venn diagram representing
our ideal preclinical oncology curriculum (black rectangle) that shows
how each section develops some or all of the ACGME competencies as
shown by inset pie charts
J Canc Educ (2013) 28:228236 229
How to Make It Happen: Curriculum Design
We developed this comprehensive preclinical oncology cur-
riculum from the perspectives of patients, caregivers, physi-
cians and other healthcare professionals. In deciding
whether a given topic is appropriate for inclusion we con-
sidered several factors:
Medical Knowledge
Basic and clinical science principles provide a foundation
for understanding epidemiology, carcinogenesis, and princi-
ples of surgical, radiation, and systemic treatments. Scien-
tific concepts across cancers (e.g., acquired DNA mutations,
viral infections, inherited genetic defects) should be inte-
grated while avoiding esoteric molecules and signaling
pathways. Reinforcing themes and information about spe-
cific tumors across lectures that utilize interactive audience
response systems provides repetition and student participa-
tion to facilitate students pattern recognition and long-term
retention [1821]. Framing the information in the context of
clinical case discussions prepares students to address prob-
lems as practicing physicians. Include topics such as the
pathophysiology, methods for detection, and standard
approaches to treatment. Consider emerging and niche tech-
nologies and clinical algorithms but relegate any in-depth
discussion to the third and fourth years.
Patient Care, Population Studies
Preclinical medical students need to understand the epidemi-
ology of common cancers (gender, genetics, environmental
exposures, socioeconomic status, geographic distribution,
etc.) as well as the utility of prevention, lifestyle modification
(e.g., smoking cessation) and screening. Exercise, in particu-
lar, with its many benefits in healthy and sick individuals alike
[22] provides common approaches to disease prevention and
cure and may alleviate psychosocial stressors that contribute
to comorbidities like anxiety, depression, and sleeplessness.
Given that patient populations may differ significantly,
students should be introduced to common cancers but the
preclinical oncology curriculum must have flexibility to
reflect the training environment, including cancer variants
and the resources at the medical schools principal instruc-
tional sites.
Patient Care, Psychosocial Aspects
To produce well-rounded and optimally prepared physi-
cians, students must consider how the psychosocial ele-
ments of a patients life influence their access to care,
compliance with diagnostic and treatment plans and, ulti-
mately, response to treatment. How a patients psychosocial
stressors should be treated depends on the stressor itself
[23]. Overall, the oncology literature on psychosocial stres-
sors is not terribly robust [24], but does suggest that various
stressors may amplify morbidity and mortality among can-
cer patients. In fact, mindbody interactions profoundly
influence medical outcomes for some non-cancerous pathol-
ogies like irritable bowel syndrome [25].
Students should also be introduced to palliative and end-
of-life care. They must be competent in giving bad news,
pain management and managing terminal illnesses for
patients and their families. Physicians must also be skilled
at anticipating and addressing patients psychosocial needs
given the physical, emotional, financial, and social stressors
patients are likely to encounter. Although palliation has
traditionally been reserved exclusively for the weeks or
months preceding a patients death, attention to symptom
management is worth pursuing concurrently with active
treatment to increase the quality of life, improve survival
and even reduce healthcare expenditures [26, 27]. Providing
palliative care and support to children and their families
requires special expertise and sensitivity [28] and may lie
beyond the scope of a more generalized oncology curriculum.
Integrating Professionalism and Communication to Improve
Patient Care
How physicians communicate with patients as well as how
they interact with colleagues in coordinating patient care are
both important. Medical students must learn to not only
consistently relay information to the patient that is directly
related to their disease, including treatment plan, prognosis,
and future options, but also address their psychosocial
needs, whether for adults [29] or children [30].
Medical students must be trained to deliver bad news
professionally but with a humanistic touch. Per Millers
pyramid for assessing clinical competence, clinical compe-
tence is gained in several steps (Fig. 2) [31]. In the oncology
block, small group discussions and mock patient and phy-
sician communication sessions (Topics 5658, Table 1) lay
the groundwork for the development of these skills, which
then are further developed during students third and fourth
(clinical) years of medical school. Given the complex com-
munication required, a single session is insufficient to de-
velop this skill. Rather, students must have repeated
opportunities for reflection, synthesis, and practice [13, 14,
32] although breaking bad news to patients need not occur
on a topic-specific basis [33]. Therefore, schools have great
flexibility in how and when to impart appropriate knowl-
edge and experiences during the preclinical years.
Physicians must also communicate well with both
patients and their colleagues. Certainly, given the large
number of professionals who care for a single patient, mis-
communication (or a lack of communication) is common
230 J Canc Educ (2013) 28:228236
[34] and not just in the treatment of cancer patients [35]. All
patients and specialties would benefit from attention to
better interprofessional communication.
Based on the aforementioned considerations we developed
six learning objectives to guide curriculum design and topics
(Table 2).
How to Make It Happen: Implementation
and Follow-Up
Interspersed Discussions vs. Modular/Block Format
A given curriculum may be taught in a variety of ways.
Preclinical courses may be organized by scientific discipline,
organ system, or clinical specialty. Oncology can be integrated
into that of other systems modules (e.g., pathology and clin-
ical presentation of pancreatic adenocarcinoma within the
gastrointestinal system) or relegated to an oncology-centric
block or module. We and others [4] believe that the block
format, welcomed by the students who have progressed
through and reflected upon it at our institution (unpublished
data), is more effective to cohesively present integrated mate-
rial that may otherwise be lost if dispersed throughout the
entire preclinical undergraduate medical curriculum. The one
study comparing student perceptions of interspersed discus-
sions integrated throughout the curriculum compared to a
modular format on specific subjects that a literature search
revealed showed that students in the interspersed discussion
style curriculumare significantly less satisfied with the quality
and quantity of their education on a given subject matter
compared to the modular curriculum model [36].
A consolidated cancer curriculum is particularly helpful
in introducing topics that are essential in treating many
cancers but may not warrant significant attention when
discussing any single pathology. Lectures on the principles
of surgical, chemotherapeutic, and radiation treatments are
often lost in an interspersed format. The lack of emphasis on
radiation oncology in the undergraduate medical curriculum
and strategies to address this issue were recently reviewed
[37, 38]. This is worrisome given that nearly 60 % of all
cancer patients receive radiotherapy as part of their treat-
ment regimens [39]. Students understanding of the under-
lying principles and patterns among cancers and their
treatments can be lost in the absence of an oncology block
strategy.
If an interspersed cancer curriculum must be employed, a
director or small team of faculty (to include, e.g., medical,
surgical, and radiation oncologists, psychiatrists, as well as
allied health professionals) should provide oversight.
The interspersed curriculum could also be supplemented
with the consolidated block towards the end of the preclin-
ical years if time permits. As such, the implementation of
both approaches would allow for repetition, which would
enhance retention as well as comprehension.
Sample Schedule
To efficiently incorporate the basic tenets outlined into a
cohesive program of study for undergraduate medical stu-
dents, we provide an outline of an oncology block adapted
from the current version in use at the Boston University
School of Medicine (BUSM; Table 1).
BUSM Preclinical Oncology Block
Since its inception in 2009, our preclinical oncology block
has exposed students to basic science and clinical concepts
in oncology as part of our horizontally integrated Oncology
Education Initiative (OEI) [40]. Scientific lectures are paired
with those relating to clinical aspects of a given disease or
group of diseases. For example, lectures 20, 29, and 35 are
devoted to the pathology of lung, genitourinary, and breast
cancers, respectively, while 21, 30, and 36 discuss the
epidemiology, clinical presentations, effective diagnostic
modalities, therapeutic options, and preferred treatment reg-
imens. Students thus appreciate how intricately biomedical
research and clinical care are intertwined.
A dedicated oncology block provides several opportuni-
ties for curricular integration. Indeed, schools are investi-
gating vertical and horizontal integration of disciplines in
response to blurred lines demarcating traditional disciplines
secondary to an ever-evolving medical knowledge base [41,
42]. At BUSM, gross anatomy, histology, pathology, radi-
ology and oncology are integrated and discussed in a small-
group format in the designated oncology block. Students
rotate through stations of radiology images to develop dif-
ferential diagnoses before viewing gross and microscopic
features of classic neoplasia. Data are also posted online for
students to study independently. Since BUSM uses digital
microscopy to teach histology, each of these sessions is also
Fig. 2 Millers pyramid of clinical competence. The oncology block
proposed here relies on the three base levels while relegating the top
level to clinical studies in the later years of medical school
J Canc Educ (2013) 28:228236 231
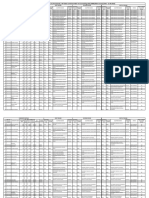
Table 1 List of topics for the preclinical oncology block
Lecture Topic Time (min)
1 Epidemiology of Cancer 50
2 Introduction to the Cell Cycle and Neoplasia 50
3 Cytopathology of Neoplasia 50
4 Principles of Cancer Biology and Tumor Immunology 50
5 Etiologies of Cancer: Molecular, Viral, and Environmental 50
6 Molecular Diagnosis (including Tumor Markers) and Laboratory Techniques 50
7 Imaging Modalities in Oncology 50
8 Self-Study: Principles of Oncology and Cancer Biology
a
9 Case Studies 50
10 Preventative Medicine's Role in Stopping Cancer Before It Starts 100
11 Classifying Cancers: Evaluating Tumor Grade and Stage 50
12 Cancer Treatment Strategies: Surgery, Radiation, Chemotherapy 50
13 Introduction to Chemotherapy 50
14 Introduction to Radiation Oncology 50
15 Self-Study: Foundations of Clinical Oncology
a
16 Case Studies 50
17 Introduction to Cancerous Tissue Types and Nomenclature 50
18 CNS Tumors Pathology 50
19 CNS Tumors Clinical 50
20 Lung Cancer Pathology 50
21 Lung Cancer Clinical 50
22 Pathology Self Study Case: Lung Cancer
a
23 Cases Lung and CNS Cancers 50
24 Esophagus and Gastric Cancer 50
25 Tumors of Pancreas/Polyps and Cancer of the Colorectum 50
26 Colon, Liver and Pancreas Cancer Clinical 50
27 Cases GI Tumors 50
28 Pathology Self Study Case: Colon Cancer
a
29 Renal, Urologic and Prostate Cancer Pathology 50
30 Renal and Urologic and Prostate Cancers Clinical 50
31 Pathology Self Study: Seminoma of Testis
a
32 Pathology Self Study: Prostate Carcinoma
a
33 Ovarian Neoplasia 50
34 Pathology Self Study Case: Cervical Cancer
a
35 Breast Cancer Pathology 50
36 Breast Cancer Clinical 50
37 Pathology Self Study Case: Breast Cancer
a
38 Cases Renal, Urologic, and Reproductive Organ Cancers 50
39 Skin Cancers 50
40 Cases Skin Cancers 50
41 Bone and Soft Tissue Cancer 50
42 Self Study: Bone, Skin, and Soft Tissue Cancers
a
43 Gross Pathology Demo Cases 50
44 Lymphomas 50
45 Leukemias 50
46 Lymphoproliferative Disorders (e.g., myeloma, MGUS, PV) 50
47 Cases 50
48 Pathology Self Study Cases: Leukemia, Lymphoma, Lymphoproliferative Disorders
b
49 HematologyOncology Pathology Slide Review 50
232 J Canc Educ (2013) 28:228236
linked online to normal histology that was learned during
first-year coursework.
Clearly, the successful coordination and implementation
of an effective oncology curriculum requires inputs from
molecular and cellular biologists, pathologists, pharmacolo-
gists, medical, surgical and radiation oncologists, epidemi-
ologists, family practitioners, radiologists, microbiologists,
psychiatrists, and others. While each individual cannot pro-
vide input on each lecture, everyones assistance is needed
to integrate the material into a cohesive course with planned
repetition across lectures to enhance the blocks overall
impact.
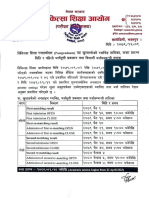
Student evaluations have strongly supported our compre-
hensive integration of the BUSM hematologyoncology
block as reflected by survey data from the Office of Medical
Education (OME) at our institution and survey data from the
radiation oncology department that is administered to third-
and fourth-year medical students (Fig. 3). The OME, among
its other functions, independently audits courses through
soliciting student feedback. Between the first two install-
ments of the oncology block (20102011 and 20112012),
student assessment improved in multiple dimensions. These
include student evaluations of good or excellent regard-
ing how well learning methods fostered learning (from 87 %
in 20102011 to 94 % in 20112012), integration of mate-
rial throughout the module (from 79 % to 87 %), and
organization of topics within the block (from 75 % to
91 %). These improvements may stem from a variety of
changes made to the module since its debut, including
providing guidance on how to approach the material in the
Table 1 (continued)
Lecture Topic Time (min)
50 Transfusion Medicine 50
51 Rare Cancers: Being Prepared for Them 50
52 Pediatric Oncology: Tumor Types and Special Considerations 100
53 Current Topics and Trends in Oncology 100
54 Integrated Summary of Organ Systems and Clinical Science Foundations 50
55 Integrated Summary of Organ Systems and Clinical Science Foundations 2 50
56 Professional Communication: Physician to Physician 50
57 Professional Communication: Physician to Patient 50
58 Providing Psychosocial Support to Patients 50
59 Palliative and End-of-Life Care 50
60 Self-Study: Communication in Oncology
a
61 Cases/Discussion: Communication in Oncology 50
62 Experiential Learning: Interviewing a Cancer Patient and Writing a Report 150
63 Oncology Examination Review 100
Outline of a mature oncology curriculum. Based on the preclinical hematology/oncology block at the Boston University School of Medicine, this
expanded curriculum is comprised of fifty-six 50-min periods coupled with independent study sessions over approximately 16 class days, excluding
review. It is composed of four subsections: Medical Knowledge of Cancer: Basic Science (19), Medical Knowledge of Cancer: Clinical
Foundations (1016), Cancers by Organ System (1755) and Cancer Patient Care (5662)
a
Independent learning by student, so it is expected that the amount of time necessary for each student to complete the task will vary. The average
student should be able to complete each self-study case in 50 min
b
Similar to other self-study cases but more comprehensive so the average target time for students to complete it is doubled, or 100 min
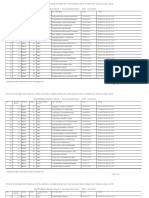
Table 2 Condensed learning objectives for the preclinical oncology block
Objective ID Description
1 Describe epidemiological concepts in relation to common cancers and the importance of prevention and screening
2 Identify the molecular basis of neoplasia in hematology and oncology
3 Recognize the pathophysiology, morphology, and clinical characteristics of common tumors that affect various organ systems
4 Understand cancer diagnosis, including clinical examination, diagnostic tools, and histopathological classification
5 Identify the basic principles of cancer therapy and multidisciplinary management
6 Develop communication skills needed to counsel and support patients and to work professionally with colleagues
Learning objectives for a preclinical oncology block. Content for lectures in the proposed block are centered around these six broad educational
aims. They canvas knowledge of the basic and clinical sciences as well as developing good communication skills
J Canc Educ (2013) 28:228236 233
block during an overview lecture, condensing the lecture
schedule and topics discussed for a more tractable syllabus
to be covered, and a modified end-of-course examination
that strove to test understanding of broad themes rather than
minute details. We are encouraged by these initial improve-
ments and aim to achieve even greater positive feedback
from future classes as further improvements are made to the
oncology block in response to student feedback.
Ideal Preclinical Oncology Curriculum Content
The preclinical oncology curriculum at BUSM addresses
many important issues and concepts and may serve as a
model for other medical schools. Many elements, notably
the high level of interdisciplinary discussions within and
between lectures, are strengths of our existing model. We
have supplemented the existing foundation at BUSM with
topics that are integral in preparing medical students to
competently care for cancer patients (Fig. 1b).
Finally, educational administrators must be flexible in
implementing this curriculum effectively into their already
packed lecture schedules. Some of the topics covered within
individual lectures could also be covered in other courses or
in small group workshops. We use the term lecture to
account for time needed to convey knowledge or develop
a skill set in whatever method is deemed most effective,
without intending to limit the instructional forum to a large
lecture hall. For example, BUSM has a weekly Integrated
Problems (IP) course to develop practical research and com-
munication skills. Focusing heavily on group discussions
and team problem solving, IP does not rely on a student
patient or facultypatient interface to achieve its goals. This
distinction enables IP to accommodate specific types of
material such as topics related to cancer patient care (lec-
tures 5662). Students presented with a case of an elderly
diabetic woman with metastatic breast cancer would re-
search treatment options for both conditions and also learn
how to best communicate with other healthcare professio-
nals and the patient in identifying treatment goals and how
to achieve them. This active learning paradigm can therefore
supplement basic science and clinical knowledge accrued in
other lectures given the emphasis on interpersonal interac-
tions and behaviors.
Additional Considerations
Insertion into the Academic Calendar
Where to insert an oncology block in the general preclinical
curriculum deserves consideration. Students lack of famil-
iarity with topics that play a central role in many cancers
(e.g., virology of EpsteinBarr virus and human papilloma
virus in causing B-cell lymphoma and cervical cancer, re-
spectively) argues against introducing oncology too early.
We begin the second year with a Fundamentals of Medical
Knowledge section that addresses essential material in
pathology, microbiology, and pharmacology to set the stage
for an oncology block later on.
Administering the block at the end of the preclinical
curriculum builds on students familiarity with basic con-
cepts in pathology, microbiology, pharmacology, patho-
physiology, and health law to optimally address such a
multifaceted topic as cancer. However, delayed scheduling
may hinder long-term memory consolidation of such com-
plex material. Providing exposure to many technical terms,
with subsequent testing, prior to the oncology curriculum
can position the oncology curriculum to organize these
concepts.
Finally, providing the block in the middle of the second
year may allow for sufficient mastery of the needed con-
cepts and vocabulary as well as time for integration of basic
medical knowledge prior to caring for oncology patients.
Incorporation of Current Topics
In addition to the typical subjects for consideration we also
scheduled time to introduce the most recent findings, and
technological advancements in cancer research and patient
care (e.g., lecture 53 in Table 1). These current topics may
be discussed in a small-group format as part of problem-
based learning sessions, common in U.S. medical schools
[43], or in a traditional lecture environment, and need not
tax a schools existing classroom time. The key is to engage
students and to stimulate interest in understanding the evo-
lution of tools available to physicians for cancer diagnosis
and treatment.
Fig. 3 Graph displaying results from a student evaluations adminis-
tered in 20092010 with the following statements: a Oncology is
important in medical education. b I am excited to be part of the
multiyear oncology block. c The oncology block was effective at
contributing towards a vertically integrated cancer curriculum. d The
oncology block was effective at contributing towards my medical
education. Black bars indicate strongly agree and agree student
responses while gray bars include neither agree nor disagree, dis-
agree, strongly disagree, and don't know responses
234 J Canc Educ (2013) 28:228236
Assessment and Follow-up of Curriculum
Despite our best efforts to improve medical student oncolo-
gy preclinical education, evaluating successes and progress
over time would be difficult without standard metrics, with-
in and among medical schools. A general exit examination
prior to graduation has been proposed in Australia to ascer-
tain equivalent achievement [44]. For similar reasons, we
recommend that an oncology-specific exam be administered
during the preclinical medical curriculum, ideally through
the National Board of Medical Examiners (NBME) [45]. An
established preclinical oncology shelf examination may
promote educational scholarship and help determine what
pedagogical methods work best. The NBME could also
provide results for individual and school performance for
oncology-based questions on Step 1 and Step 2, Clinical
Knowledge licensing exams, as it does for organ systems.
We have recently initiated collaboration with ASCO and the
NBME to assess USMLE oncology-related content.
Finally, assessment of students capacities to be empathic
towards patients as well as good communicators among
patients and fellow healthcare providers should not be
neglected. The subjective nature of these topics makes such
determination more difficult but the anticipated benefits
make the additional effort well worth it. One possible way
to test students in these areas is to make use of standardized
patients that many schools already employ to evaluate a
wide range of clinical skills.
Summary and Conclusions
We have described an overview of an oncology curriculum
for second-year medical students to prepare them to care for
oncology patients in their clinical rotations and eventual
practice. Students need sufficient basic oncology concepts,
knowledge and clinical skills to facilitate the diagnosis of
cancer and appropriate referral. Conversely, medical schools
need to avoid the temptation to include subject matter more
appropriate for residents and fellows.
Important elements of a preclinical oncology curriculum
are discussed as well as suggestions for implementation and
a proposed strategy for evaluating these efforts. An effective
preclinical oncology curriculum relies on active technology-
based lectures and team-based communication exercises to
teach medical students the essentials of cancer terminology
before entering the clinical portion of their curriculum. We
will continue to systematically establish core competencies
in cancer patient management for the medical student. As
part of a national community of physicians and educators,
we share this model curriculum and welcome feedback so it
can be improved. Through collaboration, we hope to devel-
op a consensus around content requisite for modern cancer
education of undergraduate medical students while allowing
flexibility for each school to adapt the curriculum to its
institutional learning objectives to best serve its patients.
Ethical Approval
Ethical approval has been granted by the Institutional Re-
view Board at the Boston University School of Medicine to
collect participant survey information from medical students
as part of the Oncology Education Initiative.
Acknowledgments The authors would like to thank Dean Karen
Antman for thoughtful and critical review of this manuscript. This
work is supported, in part, by a Varian Medical Systems/Radiological
Society of North America Education Seed Grant.
Conflict of interest The authors declare that they have no conflict of
interest.
References
1. American Cancer Society (2012) Cancer facts and figures 2012.
American Cancer Society, Atlanta
2. International Agency for Research on Cancer (2009) World cancer
report 2008. World Health Organization, Geneva
3. Peckham M (1989) A curriculum in oncology for medical students
in Europe. Acta Oncol 28(1):141147
4. Gaffan J, Dacre J, Jones A (2006) Educating undergraduate med-
ical students about oncology: a literature review. J Clin Oncol
24(12):19321939
5. Oncology Education Committee (2007) Ideal oncology curriculum
for medical schools. The Cancer Council Australia
6. Muss HB, Von Roenn J, Damon LE, Deangelis LM, Flaherty LE,
Harari PM, Kelly K, Kosty MP, Loscalzo MJ, Mennel R, Mitchell
BS, Mortimer JE, Muggia F, Perez EA, Pisters PW, Saltz L,
Schapira L, Sparano J (2005) ACCO: ASCO core curriculum
outline. J Clin Oncol 23(9):20492077
7. Association of American Medical Colleges (AAMC) Curriculum
Management Information Tool (CurrMIT) (2011) www.aamc.org/
currmit. Accessed November 29, 2011
8. Barton MB, Bell P, Sabesan S, Koczwara B (2006) What should
doctors know about cancer? Undergraduate medical education
from a societal perspective. Lancet Oncol 7(7):596601
9. DeNunzio NJ, Hirsch AE (2011) The need for a standard, system-
atic oncology curriculum for U.S. medical schools. Acad Med
86(8):921
10. Dajani Z, Geller AC (2008) Cancer prevention education in United
States medical schools: how far have we come? J Cancer Educ
23(4):204208
11. Wilkerson L, Lee M, Hodgson CS (2002) Evaluating curricular
effects on medical students' knowledge and self-perceived skills in
cancer prevention. Acad Med 77(10 Suppl):S5153
12. Licensing Committee on Medical Education (2010) Functions and
structure of a medical school: standards for accreditation of med-
ical education programs leading to the M.D. degree
13. Accreditation Council for Graduate Medical Education (2008)
Change and improvement in the learning environment. ACGME
Bulletin, Chicago
14. Accreditation Council for Graduate Medical Education (2008)
Envisioning the future of "competencies". ACGME Bulletin, Chicago
J Canc Educ (2013) 28:228236 235
15. Geller AC, Prout MN, Miller DR, Siegel B, Sun T, Ockene J, Koh
HK (2002) Evaluation of a cancer prevention and detection curric-
ulum for medical students. Prev Med 35(1):7886
16. Uijtdehaage S, Hauer KE, Stuber M, Go VL, Rajagopalan S,
Wilkerson L (2009) Preparedness for caring of cancer survivors:
a multi-institutional study of medical students and oncology fel-
lows. J Cancer Educ 24(1):2832
17. Uijtdehaage S, Hauer KE, Stuber M, Rajagopalan S, Go VL,
Wilkerson L (2009) A framework for developing, implementing,
and evaluating a cancer survivorship curriculum for medical stu-
dents. J Gen Intern Med 24(Suppl 2):S491494
18. Mastoridis S, Kladidis S (2010) Coming soon to a lecture theatre
near you: the 'clicker'. Clin Teach 7(2):97101
19. Rubio EI, Bassignani MJ, White MA, Brant WE (2008) Effect of
an audience response system on resident learning and retention of
lecture material. AJR Am J Roentgenol 190(6):W319322
20. Pradhan A, Sparano D, Ananth CV (2005) The influence of an
audience response system on knowledge retention: an application
to resident education. Am J Obstet Gynecol 193(5):18271830
21. Elashvili A, Denehy GE, Dawson DV, Cunningham MA (2008)
Evaluation of an audience response system in a preclinical opera-
tive dentistry course. J Dent Educ 72(11):12961303
22. Newton RU, Galvao DA (2008) Exercise in prevention and man-
agement of cancer. Curr Treat Options Oncol 9(23):135146
23. Carlson LE, Bultz BD (2008) Mindbody interventions in oncol-
ogy. Curr Treat Options Oncol 9(23):127134
24. Chida Y, Hamer M, Wardle J, Steptoe A (2008) Do stress-related
psychosocial factors contribute to cancer incidence and survival?
Nat Clin Pract Oncol 5(8):466475
25. Mayer EA (2008) Clinical practice. Irritable bowel syndrome. N
Engl J Med 358(16):16921699
26. Kelley AS, Meier DE (2010) Palliative carea shifting paradigm.
N Engl J Med 363(8):781782
27. Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S,
Jackson VA, Dahlin CM, Blinderman CD, Jacobsen J, Pirl WF,
Billings JA, Lynch TJ (2010) Early palliative care for patients with
metastatic non-small-cell lung cancer. NEngl J Med 363(8):733742
28. Himelstein BP, Hilden JM, Boldt AM, Weissman D (2004)
Pediatric palliative care. N Engl J Med 350(17):17521762
29. Hack TF, Degner LF, Parker PA (2005) The communication goals
and needs of cancer patients: a review. Psychooncology
14(10):831845, discussion 846837
30. Scott JT, Harmsen M, Prictor MJ, Sowden AJ, Watt I (2008)
Interventions for improving communication with children and
adolescents about their cancer (Review). The Cochrane Library,
The Cochrane Collaboration
31. van der Vleuten CP, Schuwirth LW, Scheele F, Driessen EW,
Hodges B (2010) The assessment of professional competence:
building blocks for theory development. Best Pract Res Clin
Obstet Gynaecol 24(6):703719
32. Rosenbaum ME, Ferguson KJ, Lobas JG (2004) Teaching medical
students and residents skills for delivering bad news: a review of
strategies. Acad Med 79(2):107117
33. Colletti L, Gruppen L, Barclay M, Stern D (2001) Teaching stu-
dents to break bad news. Am J Surg 182(1):2023
34. Fleissig A, Jenkins V, Catt S, Fallowfield L (2006) Multidisciplinary
teams in cancer care: are they effective in the UK? Lancet Oncol
7(11):935943
35. Stillman MD(2008) Physicians behaving badly. JAMA300(1):2122
36. Walsh CO, Ziniel SI, Delichatsios HK, Ludwig DS (2011)
Nutrition attitudes and knowledge in medical students after com-
pletion of an integrated nutrition curriculum compared to a dedi-
cated nutrition curriculum: a quasi-experimental study. BMC Med
Educ 11:58
37. Dennis KE, Duncan G (2010) Radiation oncology in undergradu-
ate medical education: a literature review. Int J Radiat Oncol Biol
Phys 76(3):649655
38. DeNunzio N, Parekh A, Hirsch AE (2010) Mentoring medical
students in radiation oncology. J Am Coll Radiol 7(9):722728
39. Perez C, Brady L (eds) (2007) Principles and practice of radiation
oncology, 5th edn. Lippincott-Raven, Philadelphia
40. Hirsch AE, Singh D, Ozonoff A, Slanetz PJ (2007) Educating
medical students about radiation oncology: initial results of the
oncology education initiative. J Am Coll Radiol 4(10):711715
41. Muller JH, Jain S, Loeser H, Irby DM (2008) Lessons learned
about integrating a medical school curriculum: perceptions of
students, faculty and curriculum leaders. Med Educ 42(8):778785
42. Vidic B, Weitlauf HM (2002) Horizontal and vertical integration of
academic disciplines in the medical school curriculum. Clin Anat
15(3):233235
43. Hoffman K, Hosokawa M, Blake R Jr, Headrick L, Johnson G
(2006) Problem-based learning outcomes: ten years of experience
at the University of Missouri-Columbia School of Medicine. Acad
Med 81(7):617625
44. Koczwara B, Tattersall MH, Barton MB, Coventry BJ, Dewar JM,
Millar JL, Olver IN, Schwarz MA, Starmer DL, Turner DR,
Stockler MR (2005) Achieving equal standards in medical student
education: is a national exit examination the answer? Med J Aust
182(5):228230
45. National Board of Medical Examiners (2010) Students Subject
Examinations. http://www.nbme.org/students/SubExam/subex
ams.html. Accessed January 3, 2011
236 J Canc Educ (2013) 28:228236
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Uttar Pradesh Dental CouncilDocument1 paginăUttar Pradesh Dental CouncilFaizan KassarÎncă nu există evaluări
- World Journal of Surgical Oncology: Abnormal HCG Levels in A Patient With Treated Stage I Seminoma: A Diagnostic DilemmaDocument3 paginiWorld Journal of Surgical Oncology: Abnormal HCG Levels in A Patient With Treated Stage I Seminoma: A Diagnostic DilemmaarakbaeÎncă nu există evaluări
- Superparamagnetic Iron Oxide NanoparticlesDocument21 paginiSuperparamagnetic Iron Oxide NanoparticlesarakbaeÎncă nu există evaluări
- 1471 2490 6 5Document4 pagini1471 2490 6 5arakbaeÎncă nu există evaluări
- 842Document8 pagini842arakbaeÎncă nu există evaluări
- Planning of Electroporation-Based Treatments UsingDocument10 paginiPlanning of Electroporation-Based Treatments UsingarakbaeÎncă nu există evaluări
- Targeting The Dynamic HSP90 Complex in CancerDocument13 paginiTargeting The Dynamic HSP90 Complex in CancerarakbaeÎncă nu există evaluări
- 90 6601867aDocument7 pagini90 6601867aarakbaeÎncă nu există evaluări
- The Role of Radiotherapy in Cancer TreatmentDocument9 paginiThe Role of Radiotherapy in Cancer TreatmentarakbaeÎncă nu există evaluări
- Mosaic JDocument7 paginiMosaic JarakbaeÎncă nu există evaluări
- Van DykDocument31 paginiVan DykarakbaeÎncă nu există evaluări
- Tugas Mata Kuliah Pengolahan CitraDocument5 paginiTugas Mata Kuliah Pengolahan CitraarakbaeÎncă nu există evaluări
- The European Society of Therapeutic Radiology and Oncology–European Institute of Radiotherapy (ESTRO–EIR) Report on 3D CT-based in-room Image Guidance Systems- A Practical and Technical Review and GuideDocument16 paginiThe European Society of Therapeutic Radiology and Oncology–European Institute of Radiotherapy (ESTRO–EIR) Report on 3D CT-based in-room Image Guidance Systems- A Practical and Technical Review and GuidearakbaeÎncă nu există evaluări
- Macro Reference GuideDocument45 paginiMacro Reference GuideMarcos Vinicios Borges GaldinoÎncă nu există evaluări
- Macros Roimanager3dDocument2 paginiMacros Roimanager3darakbaeÎncă nu există evaluări
- Auto-Align Manuscript Supplement FinalDocument9 paginiAuto-Align Manuscript Supplement FinalarakbaeÎncă nu există evaluări
- Ki67 Expression and Docetaxel Efficacy in Patients With Estrogen Receptor-Positive Breast CancerDocument7 paginiKi67 Expression and Docetaxel Efficacy in Patients With Estrogen Receptor-Positive Breast CancerarakbaeÎncă nu există evaluări
- Detection of Patient Setup Errors With A Portal Image - DRR Registration Software ApplicationDocument14 paginiDetection of Patient Setup Errors With A Portal Image - DRR Registration Software ApplicationarakbaeÎncă nu există evaluări
- Intensity-Modulated Radiation Therapy With or Without Chemotherapy For Nasopharyngeal Carcinoma - Radiation Therapy Oncology Group Phase II Trial 0225Document7 paginiIntensity-Modulated Radiation Therapy With or Without Chemotherapy For Nasopharyngeal Carcinoma - Radiation Therapy Oncology Group Phase II Trial 0225arakbaeÎncă nu există evaluări
- Importance of Protocol Target Definition On The Ability To Spare Normal Tissue - An IMRT and 3D-CRT Planning Comparison For Intraorbital TumorsDocument9 paginiImportance of Protocol Target Definition On The Ability To Spare Normal Tissue - An IMRT and 3D-CRT Planning Comparison For Intraorbital TumorsarakbaeÎncă nu există evaluări
- Automatic Localization and Delineation of Collimation Fields in Digital and Film-Based RadiographsDocument9 paginiAutomatic Localization and Delineation of Collimation Fields in Digital and Film-Based RadiographsarakbaeÎncă nu există evaluări
- Control, Correction, and Modeling of Setup Errors and Organ MotionDocument12 paginiControl, Correction, and Modeling of Setup Errors and Organ MotionarakbaeÎncă nu există evaluări
- Equinox BTMB 8003 1 v092009Document4 paginiEquinox BTMB 8003 1 v092009arakbaeÎncă nu există evaluări
- Edge Detection of The Radiation Field in Double Exposure Portal Images Using A Curve Propagation AlgorithmDocument14 paginiEdge Detection of The Radiation Field in Double Exposure Portal Images Using A Curve Propagation AlgorithmarakbaeÎncă nu există evaluări
- Extremely Low-Frequency Magnetic Field Enhances The Therapeutic Efficacy of Low-Dose Cisplatin in The Treatment of Ehrlich CarcinomaDocument8 paginiExtremely Low-Frequency Magnetic Field Enhances The Therapeutic Efficacy of Low-Dose Cisplatin in The Treatment of Ehrlich CarcinomaarakbaeÎncă nu există evaluări
- Effects of Honey and Its Mechanisms of Action On The Development and Progression of CancerDocument26 paginiEffects of Honey and Its Mechanisms of Action On The Development and Progression of CancerNurHidayatÎncă nu există evaluări
- Detection of Patient Setup Errors With A Portal Image - DRR Registration Software ApplicationDocument14 paginiDetection of Patient Setup Errors With A Portal Image - DRR Registration Software ApplicationarakbaeÎncă nu există evaluări
- Honey and Cancer - Sustainable Inverse Relationship Particularly For Developing Nations-A ReviewDocument11 paginiHoney and Cancer - Sustainable Inverse Relationship Particularly For Developing Nations-A ReviewarakbaeÎncă nu există evaluări
- Protective Effect of Yashtimadhu (Glycyrrhiza Glabra) Against Side Effects of Radiation-Chemotherapy in Head and Neck MalignanciesDocument4 paginiProtective Effect of Yashtimadhu (Glycyrrhiza Glabra) Against Side Effects of Radiation-Chemotherapy in Head and Neck MalignanciesNurHidayatÎncă nu există evaluări
- Does Honey Have The Characteristics of Natural Cancer VaccineDocument8 paginiDoes Honey Have The Characteristics of Natural Cancer VaccinearakbaeÎncă nu există evaluări
- MiR-210 As A Marker of Chronic Hypoxia, But Not A Therapeutic Target in Prostate CancerDocument6 paginiMiR-210 As A Marker of Chronic Hypoxia, But Not A Therapeutic Target in Prostate CancerarakbaeÎncă nu există evaluări
- DRTP Uuer ManualDocument10 paginiDRTP Uuer ManualNavin ChandarÎncă nu există evaluări
- InstwiseadmDocument209 paginiInstwiseadmSaiÎncă nu există evaluări
- TB Quiz - 2023Document2 paginiTB Quiz - 2023Sahil KhanÎncă nu există evaluări
- RA-120500 PHYSICIAN Manila 11-2020Document255 paginiRA-120500 PHYSICIAN Manila 11-2020iya gerzonÎncă nu există evaluări
- Medical List Regular 100419Document98 paginiMedical List Regular 100419krishnakumars0% (1)
- Orthopedic Surgery Complete IMG ListDocument153 paginiOrthopedic Surgery Complete IMG ListF AbdullaÎncă nu există evaluări
- Executive Rule For CME - PD - SCFHSDocument14 paginiExecutive Rule For CME - PD - SCFHSsevattapillaiÎncă nu există evaluări
- Doctor ListDocument1 paginăDoctor ListDebankita MandalÎncă nu există evaluări
- AMEE Guide No. 25: The Assessment of Learning Outcomes For The Competent and Reflective PhysicianDocument16 paginiAMEE Guide No. 25: The Assessment of Learning Outcomes For The Competent and Reflective PhysicianAnonymous wGAc8DYl3VÎncă nu există evaluări
- New Ao Trauma PR Acetab Pelvic Szeged 08.22Document16 paginiNew Ao Trauma PR Acetab Pelvic Szeged 08.22Dr.upendra goudÎncă nu există evaluări
- Alloutment 1st Round AIQ DeemedDocument281 paginiAlloutment 1st Round AIQ DeemedMd Ali MajorÎncă nu există evaluări
- 2018 SATS Membership List For The WebsiteDocument9 pagini2018 SATS Membership List For The WebsiteRubilin NitishaÎncă nu există evaluări
- Minilip Gynae DataDocument85 paginiMinilip Gynae DataShweta jainÎncă nu există evaluări
- Ghotki Updated 2023 24Document11 paginiGhotki Updated 2023 24ahmar7698Încă nu există evaluări
- Radiology Log BookDocument51 paginiRadiology Log BookZulqarnain AbidÎncă nu există evaluări
- Uttarakhand Round 2 Revised Allotment Dated 29oct 5pmDocument264 paginiUttarakhand Round 2 Revised Allotment Dated 29oct 5pmPrudhvi MadamanchiÎncă nu există evaluări
- First Allotment List of C.G. State Govt./Pvt. MBBS and BDS Course 2021Document80 paginiFirst Allotment List of C.G. State Govt./Pvt. MBBS and BDS Course 2021arindamÎncă nu există evaluări
- Clinical Skills Coordinator Job DescriptionDocument6 paginiClinical Skills Coordinator Job DescriptionYee Han KwongÎncă nu există evaluări
- SB 3: Medical Marijuana BillDocument26 paginiSB 3: Medical Marijuana BillSteven DoyleÎncă nu există evaluări
- MOP UP Round Allotment Result DME UG 2023Document38 paginiMOP UP Round Allotment Result DME UG 2023shriram8920Încă nu există evaluări
- Teaching The Humanities in Medical EducationDocument1 paginăTeaching The Humanities in Medical EducationCardiff University School of Medicine C21 Curriculum ShowcaseÎncă nu există evaluări
- Philippines - Emilio Aguinaldo CollegeDocument12 paginiPhilippines - Emilio Aguinaldo Collegeimes123Încă nu există evaluări
- Khawaja Ms Sialkot MbbsDocument5 paginiKhawaja Ms Sialkot MbbsRayan ArhamÎncă nu există evaluări
- Allotments PG Med r1 Web 16082023Document65 paginiAllotments PG Med r1 Web 16082023Tanveer MansuriÎncă nu există evaluări
- List of Eligible Candidates MBBS 2019Document7 paginiList of Eligible Candidates MBBS 2019subhamchampÎncă nu există evaluări
- Mecpg2022 Open I ResultDocument155 paginiMecpg2022 Open I ResultJenish LagejuÎncă nu există evaluări
- Anaesthesia Science 10Document1 paginăAnaesthesia Science 10KelompokC IPDÎncă nu există evaluări
- Deemed Stray Vacancy Round Seats PG MD - Ms - DiplomaDocument39 paginiDeemed Stray Vacancy Round Seats PG MD - Ms - DiplomaManoj KashyapÎncă nu există evaluări
- Enhancing UK Core Medical Training Through Simulation-Based Education: An Evidence-Based ApproachDocument36 paginiEnhancing UK Core Medical Training Through Simulation-Based Education: An Evidence-Based ApproachAndxp51Încă nu există evaluări