Documente Academic
Documente Profesional
Documente Cultură
Ebp Project Paper
Încărcat de
api-2593197000 evaluări0% au considerat acest document util (0 voturi)
62 vizualizări9 paginiTitlu original
ebp project paper
Drepturi de autor
© © All Rights Reserved
Formate disponibile
DOCX, PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca DOCX, PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
62 vizualizări9 paginiEbp Project Paper
Încărcat de
api-259319700Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca DOCX, PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 9
Running head: IMPLEMENTING A PRACTICE CHANGE 1
Implementation of a Practice Change:
Educating about Co-sleeping as a SIDS Risk
Jordan Dillmore
University of South Florida
IMPLEMENTING A PRACTICE CHANGE 2
Implementation of a Practice Change: Educating about Co-sleeping as a SIDS Risk
In neonatal intensive care units (NICU) across the country, many twins and
other multiple gestation infants are co-bedded by NICU staff, which leads to a
misunderstanding in parents of new infants. New parents have been lead to believe
that that it is safe for their infants to share beds once they are home whether it is
with a parent or a sibling. According to the Centers for Disease Control and
Prevention (2013), SIDS is the leading cause of death of infants 1-12 months of age.
In NICUs, bed sharing is an accepted practice only because the infants are never out
of anyones sight, which ensures that the infants are not suffering from SIDS.
Although, post-discharge it is no longer promoted because parents are not able to
watch their newborns full time and sudden infant death syndrome is permitted to
occur.
PICOT
In parents being discharged home with their newborn child, does the
inclusion of specific co-sleeping education before discharge versus usual care
decrease the rates of SIDS during the first 6 months of life?
Infrastructure of Change
Sarasota Memorial Hospital has a group of nursing professionals in an
evidence-based practice council. An RN from every unit of the hospital, multiple
ARNPs, and a DNP make up the council that is led by Jen Rheingans, PhD. To get help
performing the research, this team would be available for help as well as helping to
get the practice change accepted. The next person contacted would be Dana Peco
who is the Clinical Educator for the delivery unit, mother and baby unit, and the
IMPLEMENTING A PRACTICE CHANGE 3
NICU. Dana Peco can help with the teaching being presented to the staff in these
units.
Synthesized Literature Review
Literature Search
PubMed and CINAHL were searched employing the keywords co-bedding, co-
sleeping, SIDS, and NICU. Limits were set for English language, human subjects, RCT,
peer reviewed, articles in the past 5 years, and articles in the past 10 years. Three
peer-reviewed studies were selected for evaluation and synthesis from these
searches.
Synthesis
Current research is exposing the need to further educate parents against co-
sleeping their infants because there is a direct link between it and infants dying
from SIDS. Kemp and his fellow researchers (2000) found that 43 of the 56 infants
that died of SIDS in their trials were sharing a bed. According to McCoy and fellow
researchers (2008), a SIDS risk is evident in many situations of co-sleeping infants
such as sharing couches, sofas, daybeds, waterbeds, or adult beds and whether it is
with parents, children, or younger siblings. They suggest that parental counseling
about infant sleep environments is needed so the parents can make an informed
decision (McCoy et al., 2008). Kemp and colleagues proved that 84.0% of infant
deaths are preventable and epidemiologic studies and public health campaigns that
identify risk factors and educate have been trailed by large reductions in sudden
infant death syndrome rates (2000). For example, Trachtenberg and colleagues
(2012) provide supporting data with the indication of a 50% decline of infant sleep-
IMPLEMENTING A PRACTICE CHANGE 4
related deaths since the 1990s via the promotion of the Back-to-Sleep campaign
(2012). Research completed to date has proven that co-sleeping an infant with a
parent or sibling has a direct link to SIDS as shown by the 54% of SIDS infants that
died while co-sleeping in the study by Blair and fellow researchers (2009).
Proposed Practice Change
Kemp and colleagues (2000) found that 43 of the 56 infants that died of SIDS
in their trials were sharing a bed and according to the Centers for Disease Control
and Prevention (2013), SIDS is the leading cause of death of infants 1-12 months of
age. It is imperative that parents be educated against co-sleeping their infants to
decrease the rate of SIDS post discharge from a postpartum or NICU unit in the first
six months of life. This is a very low risk intervention and Trachtenberg and fellow
researchers (2012) found a 50% decline in infant deaths after the education related
to the Back-to Sleep campaign proving that parents are listening to medical
professional opinions on lowering risks of infant deaths. Educating NICU and
postpartum unit staff is imperative so they can educate the parents appropriately
against co-bedding their infants in the fist six months of life in order to lower the
risk for SIDS.
To change this knowledge deficit, I plan to educate the staff in the NICU, labor
and delivery unit, and mother and baby unit at Sarasota Memorial Hospital about
the SIDS risk in co-bedding infants post-discharge so they can educate the parents.
Nurses in the postpartum unit and NICU will provide 1:1 education to all parents on
the dangers of co-bedding and the relationship to SIDS. Verbal and written
education will be provided prior to discharge from each unit and documented in the
IMPLEMENTING A PRACTICE CHANGE 5
patients chart. The education will be measured with a pre and post education
knowledge survey completed by the parents.
Change Strategy
Promoting Engagement
All stakeholders including staff and physicians impacted by the practice
change will be encouraged to participate in the education and all nurses will be
mandated in the discharge packet to administer both the pre and post education
knowledge surveys. No one will be allowed out of this practice change as it will be a
mandate before the infant is discharged but if someone would like to make
suggestions on the questions asked or on education delivery plans, they will be
welcome to voice it and everything will be considered.
Iowa Model for Evidence-Based Practice Change
Sarasota Memorial Hospital uses the Iowa model of evidence-based practice
to promote quality care. According to the National Nursing Practice Network
(2013), the physicians, staff, and the evidence-based practice council must
acknowledge that there is a problem with SIDS rates related to co-sleeping or there
is new evidence that is amenable to an evidence-based practice change. Secondly, a
team of stakeholders is formed to develop, implement, and evaluate the practice
change. The team pilots the feasibility and effectiveness of the possible change and if
it is positive, roll out and integration of the practice is facilitated.
Roll Out Plan
Is this topic a priority for the organization?
o Step 1- Assess the need for a practice change
IMPLEMENTING A PRACTICE CHANGE 6
December 2013
o Step 2- Form a team
January 2014
o Assemble relevant research and related literature
February 2014
o Critique and synthesize research for use in practice
February 2014
Is there sufficient research base?
o Select outcome to be achieved
March 2014
o Collect baseline data
March 2014
o Design evidence-based practice guidelines
March 2014
o Implement the project on pilot units
April 2014
o Evaluate process and outcomes
May 2014
o Modify the practice guideline
May 2014
Is change appropriate for adoption in practice?
o Institute the Change in Practice
June 2014
IMPLEMENTING A PRACTICE CHANGE 7
o Continue to evaluate quality of car and new knowledge
July 2014
o Disseminate results
August 2014
Project Evaluation
Beginning in December, nurses will administer a knowledge survey to the
parents before and after the education upon discharge. This will show the efficacy
of the teachings and alert the team in charge of the change of which nurses are doing
well and which arent. The nurses with bad post-education scores can be retaught
the information so it is assured that they are teaching to the expected caliber. Any
improvement from the pre to post knowledge survey will be celebrated as a success.
The effectiveness will also be measured by monitoring the SIDS rate post-discharge
from Sarasota Memorial Hospital within the first six months post-discharge. The
knowledge survey results will be compared to the rate of SIDS to measure the
effectiveness of the change overall. Success will be the verdict when the Sarasota
Memorial Hospital SIDS rate post discharge rate is lower in the most recent quarter
than the last. Any decrease will be a success.
Dissemination
Encouraging implementation of this practice change can be done in several
ways. One of which is by having the stakeholders speak about it at unit meetings
before every shift to promote adoption. Regionally, Sarasota Memorial Hospital can
share their project with some completed cases with other hospitals in hopes that
they will adopt it too. The success information and an updated notification of the
IMPLEMENTING A PRACTICE CHANGE 8
current step in the process can be posted on the Sarasota Memorial Hospital website
and emailed to all staff to initiate excitement and pride in the project which will lead
to more adherence both locally and regionally. The information can be posted in a
nursing journal for the whole country and world to see. A stakeholder on the
nursing evidence-based practice council can take the project to NICU and
postpartum conferences globally to present and share the new evidence.
IMPLEMENTING A PRACTICE CHANGE 9
References
Blair, P. S., Sidebotham, P., Evason- Coombe, C., Edmonds, M., Heckstall-Smith, E. M.
A., & Fleming, P. (2009). Hazardous co-sleeping environments and risk
factors amenable to change. British Medical Journal, 339-b3666. doi:
10.1136/bmj.b3666
Centers for Disease Control and Prevention (2013). Sudden Unexpected Infant Death
and Sudden Infant Death Syndrome. Retrieved from:
http://www.cdc.gov/sids/index.htm
Kemp, J. S., Unger, B., Wilkins, D., Psara, R. M., Ledbetter, T. L., Graham, M. A. &
Thach, B. T. (2000). Unsafe sleep practices and an analysis of bed-sharing
among infants dying suddenly and unexpectedly. Pediatrics, 106(3), e41. doi:
10.1542/peds.106.3.e41
McCoy, R., McKenna, J. J., & Gartner, L. (2008). Guideline on Co-Sleeping and
Breastfeeding. Academy of Breastfeeding Medicine. 3(1), 38-43.
National Nursing Practice Network (2013). Iowa Model. Retrieved from:
http://www.nnpnetwork.org/ebp-resources/iowa-model
Trachtenberg, F. L., Haas, E. A., Kinney, H. C., Stanley, C., & Krous, H. F. (2012). Risk
factor changes for sudden infant death syndrome after initiation of back-to-sleep
campaign Pediatrics, 29(4), 630-638. doi: 10.1542/peds.2011-1419
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Jordan D. Dillmore: CertificationsDocument2 paginiJordan D. Dillmore: Certificationsapi-259319700Încă nu există evaluări
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Multimodal Stimulation in The NicuDocument19 paginiMultimodal Stimulation in The Nicuapi-259319700Încă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- PamphletDocument2 paginiPamphletapi-25931970033% (3)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- SarasotaebpDocument14 paginiSarasotaebpapi-259319700Încă nu există evaluări
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- History of LaparosDocument27 paginiHistory of LaparosDr. Sanjay KolteÎncă nu există evaluări
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Dose and IntervalDocument37 paginiDose and IntervalRosel Ann BontiaÎncă nu există evaluări
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Major Internship DTR SeptoctoberDocument1 paginăMajor Internship DTR SeptoctoberGeraldineMoletaGabutinÎncă nu există evaluări
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Practice Guidelines For Central Venous Access PDFDocument35 paginiPractice Guidelines For Central Venous Access PDFJulio AltamiranoÎncă nu există evaluări
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Basic Principles of Food SafetyDocument2 paginiThe Basic Principles of Food SafetySergio Leonel CardonaÎncă nu există evaluări
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Care Study OsteomyelitisDocument23 paginiCare Study OsteomyelitisJake Pitos100% (1)
- BW Health-5Document2 paginiBW Health-5Michael JaballasÎncă nu există evaluări
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- ARTIKEL ILMIAH SkripsiDocument7 paginiARTIKEL ILMIAH SkripsiSri LestariÎncă nu există evaluări
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Magno 2018Document25 paginiMagno 2018baridinoÎncă nu există evaluări
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- English 2am18 Rattr1Document2 paginiEnglish 2am18 Rattr1Sara AliÎncă nu există evaluări
- Prevalence and Recurrence Rate of Perianal Abscess - A Population-Based Study, Sweden 1997 - 2009Document5 paginiPrevalence and Recurrence Rate of Perianal Abscess - A Population-Based Study, Sweden 1997 - 2009Ridha Aswina DalimuntheÎncă nu există evaluări
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Peds EORDocument29 paginiPeds EORAndrew BowmanÎncă nu există evaluări
- AQUALIPODocument16 paginiAQUALIPOAvalavenia Molina AbadÎncă nu există evaluări
- Health Teaching PlanDocument6 paginiHealth Teaching PlanCharissa Magistrado De Leon100% (1)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- Dr. Bot: Angeles University Foundation Integrated SchoolDocument9 paginiDr. Bot: Angeles University Foundation Integrated SchoolFRANCINE JANE PATI�OÎncă nu există evaluări
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- ATI Week 15Document4 paginiATI Week 15Tee WoodÎncă nu există evaluări
- Diabetic Retinopathy Screening ModuleDocument96 paginiDiabetic Retinopathy Screening ModuleSehaRizaÎncă nu există evaluări
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
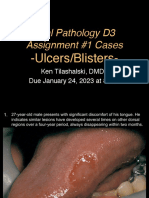
- D3 Ulcers Blisters Cases Due01242023 8amDocument13 paginiD3 Ulcers Blisters Cases Due01242023 8amLinh PhanÎncă nu există evaluări
- MalpresentationDocument16 paginiMalpresentationAnghel CruzÎncă nu există evaluări
- Week 4 Hand Washing and Ppe - CincoDocument3 paginiWeek 4 Hand Washing and Ppe - CincoShecana Rose CincoÎncă nu există evaluări
- Organic Mental Disorder: Presented By: Priyanka Kumari M.Sc. NursingDocument50 paginiOrganic Mental Disorder: Presented By: Priyanka Kumari M.Sc. NursingHardeep KaurÎncă nu există evaluări
- 02 - Quiz - 1 ArgDocument1 pagină02 - Quiz - 1 ArgNatasha NicoleÎncă nu există evaluări
- DNR Education For The PublicDocument37 paginiDNR Education For The PublicJ doeÎncă nu există evaluări
- Dependent Functions of A NurseDocument2 paginiDependent Functions of A NurseJalene AdanÎncă nu există evaluări
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Chapter 23 HomeworkDocument10 paginiChapter 23 HomeworkKvn4N6Încă nu există evaluări
- ABCDE Assessment Exam: Eunice QuijanoDocument3 paginiABCDE Assessment Exam: Eunice QuijanoQuijano GpokskieÎncă nu există evaluări
- Dci Journal PointsDocument1 paginăDci Journal PointsRajesh Rathod0% (1)
- Covid-19 Instructions QuarantineDocument4 paginiCovid-19 Instructions QuarantineFrançois MartinsÎncă nu există evaluări
- General Surgical Emergencies - Devaji, Rao SDocument333 paginiGeneral Surgical Emergencies - Devaji, Rao SVladVizitiu100% (2)
- SIP 2016 Abstract & Background Booklet V.6 PDFDocument187 paginiSIP 2016 Abstract & Background Booklet V.6 PDFJimboreanu György PaulaÎncă nu există evaluări
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)