Documente Academic
Documente Profesional
Documente Cultură
Approach To Hospital Patient Severe Insulin Resistance JCEM 2011
Încărcat de
IffatNaeem0 evaluări0% au considerat acest document util (0 voturi)
48 vizualizări11 paginiIv insulin is the standard of care for initial treatment of significant hyperglycemia. Illness, medications, the endocrine and inflammatory response to stress can contribute to insulin resistance. Achieving glucose treatment goals can be more challenging in the presence of severe insulin resistance.
Descriere originală:
Titlu original
Approach to Hospital Patient Severe Insulin Resistance JCEM 2011
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentIv insulin is the standard of care for initial treatment of significant hyperglycemia. Illness, medications, the endocrine and inflammatory response to stress can contribute to insulin resistance. Achieving glucose treatment goals can be more challenging in the presence of severe insulin resistance.
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
48 vizualizări11 paginiApproach To Hospital Patient Severe Insulin Resistance JCEM 2011
Încărcat de
IffatNaeemIv insulin is the standard of care for initial treatment of significant hyperglycemia. Illness, medications, the endocrine and inflammatory response to stress can contribute to insulin resistance. Achieving glucose treatment goals can be more challenging in the presence of severe insulin resistance.
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 11
Approach to the Hospitalized Patient with
Severe Insulin Resistance
Jennifer Larsen and Whitney Goldner
University of Nebraska Medical Center, Department of Internal Medicine, Division of
Diabetes, Endocrinology, and Metabolism, Omaha, Nebraska 68198-3020
Glucose control improves outcomes inthe hospitalizedpatient, particularly patients
onprolongedventilator support, after acutemyocardial infarctionor after coronary
artery bypass surgery. An iv insulin algorithmis the standard of care for initial treat-
ment of significant hyperglycemia in the hospitalized patient, and it can be transi-
tioned to periodic sc insulin once the patient is more stable. However, illness, med-
ications, the endocrine and inflammatory response to stress, and pain can all
contribute to insulin resistance and further aggravate preexisting insulin resistance
causedbyobesity. Glucosetreatment goals havebeenestablishedtoguidethe
1
rapy,
but achieving those goals can be more challenging in the presence of severe insulin
resistance. When target glucose values are not achieved with established insulin
algorithms, thepractitioner shouldevaluatefor potential causes of insulinresistance
from technical factors that cause pseudo-insulin resistance as well as other mod-
ifiablefactors, suchas electrolytedisorders, parenteral andenteral nutrition, or other
medications. Publishedglucoseguidelines provideglucosegoalstoguidechanges
inthe insulinalgorithm, but these goals may be difficult toachieve inall individuals.
Weproposeastepwiseapproachtoevaluateandtreat severeinsulinresistanceinthe
hospitalized patient in order to achieve glucose goals in a timely fashion. (J Clin
Endocrinol Metab 96: 26522662, 2011)
A
48-yr-old female was admitted for fever and possible
sepsis secondary to a perirectal abscess. She was
unconscious, intubated, andhypotensiveonacatecholamine
infusion in the intensive care unit when consultation for glu-
cose management was initiated. She was last seen at the ad-
mittinghospital 4yr before admission, at whichtime she was
reported to have borderline diabetes. Outpatient medica-
tions were unknown at the time of admission. Blood sugar
was 692 mg/dl on admission laboratory, temperature was
38.5C, bloodpressurewas 60/40mmHg, andpulsewas 105
beats per minute. Body mass index calculated from previ-
ously recorded height was 45 kg/cm
2
. On examination, she
was noted to have acanthosis nigricans around her neck and
in both axillae, considerable abdominal obesity, and lower
extremity venous stasis changes with 1pitting edema. On
the standard iv insulin algorithm, she was receiving 32 U of
regular insulinper hour, andher bedside capillary bloodglu-
ISSN Print 0021-972X ISSN Online 1945-7197
Printed in U.S.A.
Copyright 2011 by The Endocrine Society
doi: 10.1210/jc.2011-0255 Received January 27, 2011. Accepted May 31, 2011.
Abbreviation: TPN, Total parenteral nutrition.
Accreditation and Credit Designation Statements
The Endocrine Society is accredited by the Accreditation
Council for Continuing Medical Education to provide con-
tinuing medical educationfor physicians. The Endocrine So-
ciety has achieved Accreditation with Commendation.
The Endocrine Society designates this Journal-based
CME activity for a maximum of 1 AMA PRA Category 1
Credit
TM
. Physicians should claim only the credit commen-
surate with the extent of their participation in the activity.
Learning Objectives
Upon completion of this educational activity, participants
should be able to:
Evaluate potential causes of significant insulin resistance
that can impair the ability to achieve glucose target values
Develop potential strategies for addressing insulin resis-
tance in the hospital
Convert from intravenous to subcutaneous insulin injec-
tions in the hospitalized patient
Apply current guidelines for glucose target values in the
hospitalized patient
Target Audience
This Journal-based CME activity should be of substantial
interest to endocrinologists and other clinicians caring for
hospitalized patients with insulin resistance.
Disclosure Policy
Authors, editors, and Endocrine Society staff involved in
planning this CME activity are required to disclose to learn-
ers any relevant financial relationship(s) that have occurred
within the last 12 months with any commercial interest(s)
whose products or services are discussed in the CME con-
tent. The Endocrine Society has reviewed all disclosures and
resolved or managed all identified conflicts of interest, as
applicable.
Disclosures for JCEM Editors are found at http://www.
endo-society.org/journals/Other/faculty_jcem.cfm.
The following individuals reported NO relevant financial
relationships:
Jennifer Larsen, M.D., Whitney Goldner, M.D., and Leon-
ard Wartofsky, M.D., reported no relevant financial
relationships.
Endocrine Society staff associated with the development of
content for this activity reported no relevant financial
relationships.
Acknowledgement of Commercial Support
This activity is not supported by grants, other funds, or in-
kind contributions from commercial supporters.
Privacy and Confidentiality Statement
The Endocrine Society will record learners personal infor-
mation as provided on CME evaluations to allow for issu-
ance and tracking of CME certificates. No individual per-
formance data or any other personal information collected
from evaluations will be shared with third parties.
Method of Participation
This Journal-based CME activity is available in print and
online as full text HTML and as a PDF that can be viewed
and/or printed using Adobe Acrobat Reader. To receive
CME credit, participants should review the learning objec-
tives and disclosure information; read the article and reflect
on its content; then go to http://jcem.endojournals.org and
find the article, click on CME for Readers, and follow the
instructions to access and complete the post-activity test
questions and evaluation. The estimated time to complete
this activity, including review of material, is 1 hour. If you
have questions about this CME activity, please direct them
to education@endo-society.org.
Activity release date: September 2011
Activity expiration date: September 2012
S P E C I A L F E A T U R E
A p p r o a c h t o t h e P a t i e n t
2652 jcem.endojournals.org J Clin Endocrinol Metab, September 2011, 96(9):26522662
cose remained over 400 mg/dl, despite increasing the insulin
per protocol for the previous 4 h.
Background
Importance of glucose control to outcomes
Glucose control improves outcomes in the hospital-
ized patient, particularly in the patient with acute myo-
cardial infarction, the intensive care unit patient req-
uiring prolonged ventilator support, and the patient
undergoing coronary artery bypass surgery (15). En-
thusiasmfor very tight glucose control in the outpatient
setting has been tempered by recent large, multicenter
trials. In ACCORD (6), VA-Diabetes Trial (7), and
ADVANCE(8), intensifying diabetes therapy to achieve
a lower glucose goal did not reduce cardiovascular
events or overall mortality. In fact, intensification of
diabetes therapy came with a price, an increased fre-
quency of hypoglycemia (911).
The NICE SUGAR Study, the largest inpatient glucose
control study to date, was designed to confirm whether
intensive control (glucose, 81108 mg/dl) improves out-
comes in the intensive care unit compared with usual care
(180 mg/dl). In this study, intensive glucose control in-
creased incidence of severe hypoglycemia as well as 90-d
mortality (11). This study prompted the modification of
the current consensus guideline by the American Diabetes
Association and the American Association of Clinical En-
docrinologists, whichnowrecommends atarget glucose of
140180 mg/dl for the majority of critically ill patients
and premeal and randomblood glucose targets below140
and 180 mg/dl, respectively, in all other hospitalized pa-
tients (12). What the consensus guideline did not discuss,
and has not yet been established, is the optimal strategy by
which to achieve these guidelines, particularly in those
with extreme insulin resistance or difficult to control hy-
perglycemia. In the end, the risk of hypoglycemia must be
weighedagainst the potential benefits of glucose control in
each individual patient. The glucose goals and treatment
algorithm should be adjusted based on that assessment.
Causes and mechanisms of severe insulin
resistance
Insulin resistance in the hospitalized patient is often
multifactorial (Table 1). First, hyperglycemia and insulin
resistance can result from the endocrine response to
stress. Activation of the sympathetic nervous system
along with the up-regulation of proinflammatory cyto-
kines (13, 14), particularly TNF and nuclear factor-
(15), causes a cascade of events, including lipolysis, with
increased free fatty acids (16), activation of the hypotha-
lamic-pituitary-adrenal axis and increased cortisol secre-
tion, altered insulin signal transduction, and increased
glucose production. The increasing prevalence of obesity
in the general population has also increased the frequency
and severity of insulin resistance in and outside the hos-
pital, including in the very young (15, 1719). Body mass
index also predicts insulin resistance and total insulin re-
quirements in the hospitalized patient (20, 21). Many ther-
apeutic agents administered to the hospitalized patient, par-
ticularly catecholamines, corticosteroids, and enteral and
total parenteral nutrition (TPN), also contribute to insulin
resistance and hyperglycemia. TPN is more likely to cause
hyperglycemia than enteral nutrition because it bypasses in-
cretin-stimulated insulin release (2224). Fat emulsion,
whether administered as a source of calories with TPN(e.g.
Intralipid) or used as a diluent (e.g. as with propofol, an
anesthetic agent used for sedation in the intensive care unit),
can also temporarily exacerbate insulin resistance (25). Cor-
ticosteroids (26), independent of the route of administration,
and other immunosuppressant medications, such as tacroli-
mus and sirolimus (27, 28), are also well established to con-
tributetohyperglycemia. Other hormoneproducts cancause
hyperglycemia by reducing insulin secretion [e.g. octreotide
(29)] or inhibiting insulin action [e.g. megestrol acetate (30)
usedtostimulateappetiteinlong-termhospitalizedpatients].
TABLE 1. Causes of insulin resistance in the hospitalized patient
Agent Refs.
Stress hormones 13, 14
Obesity 1521
Electrolyte disorders: hypokalemia, hypocalcemia, hypercalcemia, and hypomagnesemia 4446
TPN and enteral nutrition 2224
Fatty emulsion (e.g. Intralipid), including medications that are administered in fatty emulsion such as propofol 25
Corticosteroids and other immune suppressants (tacrolimus and sirolimus) 2628
Anesthetic agents: isoflurane, sevoflurane 4749
Hormone products: megestrol acetate (Megace), octreotide, leuprolide (Lupron), bicalutamide 29, 30, 50
Hormone disorders: Cushings syndrome, hormone-secreting tumors (e.g. glucagonoma or somatostatinoma),
acromegaly, hyperaldosteronism, hyperthyroidism, hypothyroidism, and pheochromocytoma
44, 5154
Other medical illnesses known to contribute to hyperglycemia: pancreatitis, hepatitis C, cystic fibrosis 5558
Miscellaneous genetic or other acquired rare causes of insulin resistance: Rabson-Mendenhall syndrome, familial
partial lipodystrophy, congenital generalized lipodystrophy, type A or B insulin resistance syndrome
5961
J Clin Endocrinol Metab, September 2011, 96(9):26522662 jcem.endojournals.org 2653
Rarely, evaluation of severe insulin resistance can uncover
previously unrecognized hormone disorders. In our experi-
ence, these factors are additive: obese patients under stress
who require treatment with agents known to exacerbate in-
sulin resistance have the most severe insulin resistance and
highest insulin requirements.
Strategies to Identify and Address Causes
of Insulin Resistance
If hyperglycemia is severe or persists despite marked in-
tensification of the insulin regimen, the clinician should
investigate for potential cause(s) of insulin resistance (Ta-
ble 1). A stepwise approach to the severely insulin-resis-
tant individual is often required. If a patient is receiving sc
insulin and is persistently hyperglycemic despite insulin
dose escalation and repeated administration of supple-
mental insulin, then sc insulin should be discontinued for
an iv insulin algorithm. In our experience, sc insulin may
be poorly or variably absorbed in critically ill patients and
in those with edema or impaired circulation that results in
poor perfusion of sc tissues. Treatment of all patients with
significant hyperglycemia should begin with a validated iv
infusion protocol (12). If hyperglycemia persists despite ap-
propriate treatment with iv insulin, then an evaluation for
causesof pseudo-insulinresistanceshouldbeinitiated(Ta-
ble 2). Insome cases, the patient canappear tobe resistant to
insulin when the prescribed insulin has not actually reached
the patient. This can occur when the iv is disconnected,
plugged, or intermittently obstructed or the insulin infusion
is connected into the maintenance iv far from the patient.
Rarely, the insulin resistance occurs suddenly after a new
bag or syringe of insulin is placed, suggesting that the insulin
was not added. Observedadministrationof sc insulinas well
as inspectionof theivinsulinsetupcanuncover someof these
technical causes of insulin resistance.
Simultaneously, the practitioner should evaluate the
patient for other underlying disorders or medications that
could contribute to the hyperglycemia and insulin resis-
tance (Table 1). In our experience, intermittent hypergly-
cemia can occur when a patient is receiving unpredictable
nutrition or is intermittently administered a medication
known to cause or exacerbate hyperglycemia. By evalu-
ating the timing of hyperglycemia and comparing it to the
timing of other administered medications or solutions, in-
cluding those being administered in glucose or fat emul-
sion, one can usually uncover the cause. Glucose swings
caused by intermittent medications can be reduced by set-
ting specific administration times for these medications,
such as corticosteroids, along with prescribed fixed doses
of sc insulin to prevent large glucose swings.
Occasionally, significant hyperglycemia (180 mg/dl)
may persist, despite increasing insulin doses, until the se-
verity of illness decreases or contributing medications are
reduced. In some of these cases, exacerbating factors can
be modified, eliminated, or treated to improve glucose
concentration or improve insulin resistance (Table 2). Al-
though it may not be possible to reduce or withhold all
agents known to exacerbate hyperglycemia, understand-
ing the potential causes can make it easier to troubleshoot
and develop appropriate treatment strategies.
Several strategies can be used to improve glucose control
during TPN administration. First, adding regular insulin to
the TPN itself can decrease the iv insulin infusion require-
TABLE 2. Approach to the severely insulin-resistant patient
Potential cause Proposed action
Exclude causes of pseudo-insulin resistance. Check to see when the hyperglycemia occurred relative to last
initiated bag or syringe of insulin, look at where the insulin
infusion is connected to other iv tubing, establish that the iv port
has a good blood return and all connections are tight.
Review current medication list to identify potential
medications contributing to insulin resistance
that could be modified if appropriate.
For example, if on corticosteroids for presumed adrenal insufficiency,
evaluate whether the dose is excessive and could be reduced.
Look for other contributing diseases or electrolyte
disorders that should be treated.
Evaluate current electrolytes and review chart for indications of other
disease (e.g. pancreatitis or other hormone disorders).
Evaluate the number and volume of medications
being given in glucose solution to determine
whether alternative infusions can be
considered.
Discuss with pharmacy which medications could be administered in
a non-glucose solution.
TPN Consider switching to enteral tube feeding if indicated; consider
decreasing glucose concentration or rate of administration;
consider adding insulin to TPN solution to reduce amount needed
in iv insulin algorithm to reduce risk if TPN suddenly or
unexpectedly discontinued.
Intralipid Consider holding for 24 h until severity of illness has improved, other
conditions have been assessed, and treatment initiated.
2654 Larsen and Goldner Severe Insulin Resistance J Clin Endocrinol Metab, September 2011, 96(9):26522662
ments, as well as decreasetheriskof hypoglycemiaif theTPN
issuddenlystopped. However, wedonot recommendadding
more than half of the total daily insulin requirements to the
TPN solution to prevent hypoglycemia if renal function or
insulinrequirements rapidly change. Changing fromTPNto
enteral tube feeding as soon as it can be accomplished can
reduce insulin requirements (31). Decreasing the iv dextrose
concentration or rate in the TPN or withholding Intralipid
canalsoimprove insulinresistance inthe short term. Chang-
ingfromafreefattyacidinfusion(e.g. Intralipid) toasoybean
fat supplement has also been described to improve hyper-
glycemia, while maintaining desired calories (32). If the pa-
tient is already prescribed enteral nutrition, switching to a
lower carbohydrate or diabetes-specific enteral formula or a
monounsaturated fatty acid enteral formula (3335) can re-
duce hyperglycemia. However, adding fiber to the enteral
formula has not beenshowntoimprove glycemic control (36).
It is just as important to decrease insulin infusion rates
or sc insulin doses as insulin requirements decline. Sudden
decreases in insulin requirements can occur with the onset
of acute renal failure, discontinuationof TPN, or changing
from TPN to enteral tube feeding. In some cases, the al-
gorithm should be adjusted down multiple steps rather
than waiting for multiple episodes of hypoglycemia.
Using the Intravenous Insulin Infusion
Protocol
Once the decision has been made to initiate iv insulin, it is
important to know where iv insulin can be administered in
each hospital. In many hospitals, iv insulin can only be ad-
ministeredoncertainfloors or intensive care units, sopatient
transfer may be required. It is also recommended that a val-
idated iv insulin protocol be used (12). The Nebraska Med-
ical Center iv insulin algorithm was adapted from and with
the permission of Hirsch and colleagues (37). The Nebraska
Medical Center insulin algorithm and sc insulin order sets
shown are in Fig. 1, AC, the latter recently recognized by
The Joint Commission as a best practice model program.
Even with preexisting insulin resistance, we recommend
initiating iv insulin therapy with the lowest algorithm, des-
ignated algorithmAin our protocol (Fig. 1). However, with
severe insulin resistance, greater amounts of insulin are re-
quired. The protocol has beenextendedtocover the needs of
these individuals as shown in Fig. 1B. The nursing staff
should be educated on howto initiate and adjust the insulin
algorithmfor glucoseconcentrations that arehigher or lower
thanthe statedglucose target range. It is just as important for
the hospital teamto knowhowto run the iv insulin protocol
and to discuss in advance and anticipate what to do in situ-
ations where insulin requirements might be expected to
change. For example, with interruption of enteral nutrition
or new-onset renal failure, the prescribing health care pro-
vider should be alerted and a plan initiated to temporarily
decrease or hold the insulin, depending on the specific cir-
cumstances and prior glucose concentration.
Titrating the insulin rate more rapidly than recom-
mendedby the order set increases the riskof hypoglycemia
by overshooting the glucose target, but it will not speedthe
time to achieve the glucose target. Periodic glucose mon-
itoring is essentialwith hourly testing considered opti-
mal until a stable insulin infusion rate and glucose con-
centration are achieved. Testing should be performed no
less frequentlythanevery2hfor the durationof the insulin
infusion to minimize wide swings in blood glucose. The
concept of a glucose target is meant to guide changes in
insulin rates, not that all glucose values have to absolutely
fall inthat target range. Progress towardthe target glucose
is more important than achieving a glucose target in some
patients, such as those with hyperosmolar coma. Correct-
ing the glucose and hyperosmolarity too quickly can in-
crease the risk of central pontine myelinolysis (38, 39).
The insulin infusion rate algorithmshould be adjusted,
not stopped, when glucose values consistently fall below
the glucose target range but above hypoglycemia (70139
mg/dl) to avoid large swings in glucose concentration.
Recognizing and treating hyperglycemia in hospitalized
patients will occur more quickly with a mandatory glucose
surveillance program. We implemented a mandatory nurse-
initiatedglucose surveillance programonall newly admitted
patients to designated floors. This programidentified signif-
icant hyperglycemia (180 mg/dl) in 3% of all admitted
patients without a history of diabetes andidentifiedthe need
for patient education with more rapid initiation of insulin
treatment, as recommended by current guidelines.
Transitioning to Subcutaneous Insulin
Once hyperglycemia has improved and stabilized on iv
insulin, transitioning to sc insulin should be the next step.
At our institution, we consider transition to sc insulin
when the majority of the blood sugars are within goal and
the insulin infusion rate or pattern is within one or two
steps using the same iv insulin algorithm for at least the
preceding8h, but preferably24h(Table 3). It is preferable
to wait until after any change in medications or planned
intervention that would dramatically change insulin re-
quirements, such as discontinuation of TPN. The daily
insulinrequirement canbe calculateddirectlyfromthe last
24 h iv insulin infusion.
We have described three scenarios in Table 3: the pa-
tient whois remaining oncontinuous calories (scenario1),
J Clin Endocrinol Metab, September 2011, 96(9):26522662 jcem.endojournals.org 2655
the patient who is being changed fromcontinuous calories
to an intermittent oral diet (scenario 2), and the patient
who will be changed from continuous to intermittent or
overnight enteral tube feeding or TPN (scenario 3). Most
hospitalized patients and all severely insulin-resistant pa-
tients will require both a long-acting basal insulin (NPH,
detemir, or glargine) andfast-actingbolus insulin(regular,
aspart, lispro, or glulisine). Supplemental scale insulin
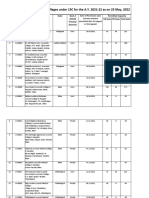
FIG. 1. Intravenous and sc insulin order forms. The order sets are shown for iv insulin algorithms for initiation (A; levels A to C); for more resistant
individuals (B; levels D to I); and for transition from iv infusion to sc insulin (C).
2656 Larsen and Goldner Severe Insulin Resistance J Clin Endocrinol Metab, September 2011, 96(9):26522662
alone, without a basal insulin, should not be a primary
strategy for glucose control (12). When evaluating which
basal insulin is preferred, NPHand the long-acting analog
glargine were considered equivalent when used in combina-
tion with short-acting supplemental insulin for treatment of
patients on continuous enteral feedings (40). Another con-
sideration is that an Intralipid infusion may require a higher
dose of long-acting insulin during the 810 h of its admin-
istration, requiring coordination with the primary or nu-
trition support team. Glucose should be monitored us-
ing point of care bedside testing at intervals that
correspond to the type of nutrition being given, either
every 4 h with continuous nutrition or before meals and
bedtime for those receiving bolus feeds or meals.
If the patient has been on no nutrition but will be rap-
idly transitioning to meals, such as after a recent surgery,
FIG. 1. (Continued).
J Clin Endocrinol Metab, September 2011, 96(9):26522662 jcem.endojournals.org 2657
the calculated requirements while on the insulin infusion
can be used to calculate the basal insulin dose. Bolus
insulin can be added for meals when the patient begins to
eat (see scenario 2). In patients eating regular meals, sim-
ilar rates of glycemic control andhypoglycemiaoccur with
daily long-acting (detemir or glargine) plus short-acting
insulin with meals (aspart, lispro, or glulisine) as occur
with split mixed-dose insulin (NPH plus regular) (41).
However, we and others prefer short-acting analog in-
sulins (aspart, lispro, or glulisine) for meals and sup-
FIG. 1. (Continued).
2658 Larsen and Goldner Severe Insulin Resistance J Clin Endocrinol Metab, September 2011, 96(9):26522662
plemental insulin in the hospital (42) because their
quicker onset and shorter action allow them to be ad-
ministered as an insulin:carbohydrate ratio (carb ratio)
based on what the patient actually eats to reduce epi-
sodes of hypoglycemia in the patient with inconsistent
intake or decreased renal function.
In most cases, the insulin dose needed to cover meals is
roughly equal to that calculated for the basal insulin re-
quirements. There are several ways the meal or bolus in-
sulin can be estimated and administered. First, an amount
equal to the estimated daily basal rate can be divided into
three equal doses for breakfast, lunch, and supper, assum-
ingthree equal-sizedmeals. Asecondmethodis toestimate
meal requirements from the iv insulin infusion if the pa-
tient was eating during that infusion, as suggestedinTable
3, scenario2. Inthis case, the insulinrequiredover the 34
h after a meal, minus the basal insulin rate over the same
time period, is given as a fixed dose or used to calculate a
carb ratio. In some cases, the carb ratio used for meals
before admissioncanbe applied. Aconservative methodis
to assume a carb ratio, where someone assumed to be
insulin sensitive would be given 1 U insulin/15 g carbo-
hydrate, whereas an insulin-resistant individual would be
assumed to require at least 23 U insulin/15 g carbohy-
drate. However, with severe insulin resistance, the ratio
can be much higher, 510 U insulin/15 g carbohydrate.
TABLE 3. Algorithms for transition from iv to sc insulin
Scenario 1 Patient currently on and staying on continuous calories (enteral or parenteral nutrition). Needs basal and
supplemental scale insulin.
Step 1 Estimate 24-h basal insulin requirements from last 24 h of iv insulin or from the number of hours
available (e.g. total from last 8 h 3 for estimated 24-h requirement).
Step 2 Choose one of the following options:
Option 1 Give one third dose as NPH every 8 h, or
Option 2 Give one half dose as glargine or detemir insulin every 12 h, or
Option 3 Give full dose as single glargine or determir insulin daily.
Step 3 Continue iv insulin infusion for 3 h after first dose of sc insulin, or less if glucose falls to 100 mg/dl.
Step 4 Change from hourly glucose testing to every 4 h glucose testing after iv insulin discontinued to be timed with
the first dose of scheduled long-acting insulin.
Step 5 Add a fast-acting analog or regular insulin supplemental scale every 4h (see Fig. 1B order set).
Step 6 Adjust scheduled long-acting insulin based on glucose values or consistent need for supplemental insulin as indicated.
Scenario 2 Currently on continuous calories with plans to discontinue and advance to diet as tolerated. Needs basal,
bolus (for meals), and supplemental scale insulin.
Step 1 Estimate 24-h basal insulin requirements from new basal requirements after continuous calories have stopped
and before meals have started. A minimum of 45 h may be required (e.g. new insulin rate 3 U/h on
average for last 3 h to 24 h insulin requirement 3 24 72 U).
Step 2 Choose one of the following options to administer basal insulin:
Option 1 Give the entire calculated basal insulin as glargine or detemir as a single daily dose or half in morning and half
at bedtime, or
Option 2 Divide calculated basal insulin as NPH twice daily (either two thirds in morning and one third in evening or one
half in morning and one half in evening, depending on pattern suggested during iv insulin).
Step 3 Estimate insulin required for meals, or
Option 1 Give fast-acting analog or regular insulin at every meal (snacks) using an insulin:carbohydrate ratio (carb ratio) with
meals. If previous carb ratio is unknown, start with 1 U/15 g, or 23 U/15 g carbohydrate if more insulin resistant, or
Option 2 Give fixed dose fast-acting analog or regular insulin with meals. Calculate dose based on insulin required
during meals eaten while on iv insulin, or dose equal to one half calculated morning NPH dose at each meal,
assuming a consistent carbohydrate intake at each meal.
Step 4 Continue iv insulin infusion for 3 h after first dose of sc insulin, or less if glucose falls to 100 mg/dl.
Step 5 Change from hourly glucose testing to before meal and bedtime glucose testing as soon as iv insulin stopped.
Step 6 Add a fast-acting analog or regular insulin supplemental scale at meals (see Fig. 1B order set). Glucose is often checked at
0200 to 0300 h, the first one or two nights after transition to moni to r for nocturnal hypoglycemia, as well.
Step 7 Adjust scheduled long- and short-acting insulins based on glucose values or consistent need for supplemental
insulin as indicated.
Scenario 3 Currently on continuous calories and plans to change to intermittent or overnight enteral tube feeding or TPN.
Step 1 Estimate 24-h basal insulin requirements as with scenario 1 or 2 above.
Step 2 Choose one of the following options:
Option 1 Bolus tube feedings. Add bolus fast-acting insulin at the time of planned tube feeding based on the
carbohydrate content and volume of formula, and a calculated carb ratio to be determined as described
under scenario 2, option 1; or
Option 2 Scheduled overnight tube feeding. Administer an additional dose of NPH, which can be incorporated into the
scheduled evening dose if appropriate, with an additional 510 U of fast-acting analog or regular insulin at
the start of the scheduled tube feed. Measure glucose at the start, at 0300 h, and at the conclusion of the
tube feed and adjust insulin accordingly. If the patient is eating during the day, as well, cover that food with
additional fast-acting regular or analog insulin based on the carb ratio.
A stepwise approach is provided for the most common clinical scenarios.
J Clin Endocrinol Metab, September 2011, 96(9):26522662 jcem.endojournals.org 2659
Some hospitals provide the carbohydrate content of foods
on the meal ticket, allowing the patient or the nurse to
assess carbohydrate intake of the meal and dose insulin
according to a prescribed carb ratio. This is particularly
useful for patients who are eating inconsistently.
Insulin requirements can change rapidly with changing
renal function, stress, activity, food consumption, or med-
ications, particularly in the severely insulin-resistant pa-
tient. New-onset hypoglycemia should prompt an assess-
ment of renal function or change in iv or enteral nutrition
rate or carbohydrate content. Likewise, intermittent epi-
sodes of hyperglycemia should prompt questions about
medications being infused, inconsistent eating, or addi-
tional uncovered food or snacks being purchased or
brought in by family or friends. On demand meal or-
dering, available in many hospitals, also allows continu-
ous eating behavior that may be more difficult to assess
and cover with bolus insulin, increasing the risk for
stacking insulin doses, and later hypoglycemia.
Intermittent corticosteroid doses can be covered with
additional timed sc insulin. We often use sc NPHtimed to
a daily or every other day iv or oral dose of corticosteroids.
In this way, the NPH dose can be tapered with the corti-
costeroid dose, independent of other scheduled insulin
doses. However, meal-time insulin doses may also need to
be increased for the 48 h after a very high dose of cor-
ticosteroid, then tapered as the steroids taper.
Controversies and Areas of Uncertainty
In general, oral hypoglycemic agents are discontinued if
previously prescribed and are not recommended for treat-
ment of newhyperglycemia in the hospitalized patient be-
cause of the many contraindications encountered in this
setting. However, once the patient is stable and particu-
larly in preparation for discharge, oral insulin-sensitizing
agents (i.e. thiazolidinedione or metformin) in particular
canhave a significant impact ontotal insulinrequirements
in the severely insulin-resistant patient. However, a thor-
ough evaluation for potential contraindications (e.g. plan
for iv contrast, fluctuating renal or cardiac status) should
be completed before initiation of therapy.
U500 regular insulin has been used in patients with
severe insulin resistance and daily insulin requirements of
at least 200 U of U100 insulin per day (43). However,
because U500insulinis doseddifferently thanU100, there
is considerable concern about greater risk of serious in-
sulin errors without proper nursing, patient, and physi-
cian education if used in the hospital. For this reason, we
dont recommend routine use of U500 insulin in the hos-
pitalized patient at this time, even if it is being prescribed
before admission, at least until the daily requirements can
be confirmed using U100 insulin.
Use of sc insulin pumps in the hospital is another area
of uncertainty. When the patient is unable to make deci-
sions about their pump themselves, we discontinue sc in-
sulinpumptherapyandinitiate either ivinsulininfusionor
sc long-acting basal insulin with short-acting bolus insulin
at meals until the patient is deemed capable of managing
their pump again without aid. Settings where this should
be consideredinclude anyone withsevere illness (e.g. inthe
intensive care unit), undergoing or immediately after an-
esthesia, with evidence of confusion or disorientation, or
receiving treatment with a medication known to impair
judgment such as narcotics.
Returning to the Patient
Blood cultures grew out gram-negative organisms. The pa-
tient was given iv antibiotics, was taken to surgery for inci-
sion and drainage of the abscess, and received fluid resusci-
tation. Within 24 h, she was weaned off iv catecholamines.
Despite clinical improvement, her insulin requirements re-
mainedgreaterthan20U/h, andglucoseremainedabove200
mg/dl. Theivinfusionwas beingadministeredappropriately,
and no additional electrolyte or contributing medical ill-
nesses were identified. The only other prescribedmedication
was continuous TPN. We added 50 Uto the next 24-h TPN
infusion bag and continued her iv insulin infusion. With this
additional insulin and improved infection, her iv insulin re-
quirements and blood glucose improved dramatically. Be-
fore extubation, she required 10 Uregular insulin/h iv, with
a glucose range of 130170 mg /dl. Once extubated, she
informedus that she hadpreviously beentaking detemir 120
Utwicedailyandaspart 25U/15gcarbohydrateserving. Her
high insulin requirements before admission are consistent
with and would predict that she may require even higher
doses of insulin during her hospital course, even with tran-
sition back to sc insulin. When a diet was ordered, we added
aspart insulinat 25U/15gcarbohydrateservingandchanged
her long-acting sc insulin to detemir 120 U twice daily, cal-
culated from her iv insulin requirements. Three hours after
the first dose of detemir, the iv infusion was discontinued,
andwe addeda supplemental scale of aspart insulinat meals
inadditiontoher carbratio. Bloodglucose values were 120
130 mg/dl in the morning and 150200 mg/dl at bedtime.
Insulin was adjusted based on glucose values through the
remainder of the hospitalization. Because edema had in-
creased during the hospitalization, thiazolidinediones were
not added, and metformin was not restarted until she was
stable after hospital discharge.
2660 Larsen and Goldner Severe Insulin Resistance J Clin Endocrinol Metab, September 2011, 96(9):26522662
Conclusions
Achieving glucose control in the patient with severe insulin
resistance requires a strategic approach. The optimal dosing
strategy and insulin requirements will vary with changing
acuity, nutrition, activity, and medications (type, dose, and
timing). Education of all health care staff is needed to safely
use an iv insulin algorithm to achieve glucose targets in the
hospital setting. Just as important, all providers and consul-
tants needtocommunicatewitheachother andact as ateam,
alerting other team members when changes are anticipated
(e.g. going to the operating room, discontinuing TPN or
other nutrition). There are significant risks of both hyper-
glycemia and hypoglycemia in the hospitalized patient, par-
ticularly in the severely insulin-resistant patient who is more
likely to experience sudden changes in insulin requirements.
Patient safety must be considered before any other stated or
published consensus statement or goal. If the health care
team feels a lower glucose goal can be achieved safely and
would be beneficial to that patients outcome or if frequent
hypoglycemia results fromthe current algorithmand goals,
the algorithm and goals should be adjusted accordingly.
Acknowledgments
Address all correspondence and requests for reprints to: Jennifer
Larsen, M.D., Department of Internal Medicine, 983020 Ne-
braska Medical Center, Omaha, Nebraska 68198-3020. E-mail:
jlarsen@unmc.edu.
Disclosure Summary: The authors have nothing to declare.
References
1. Van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx
F, Schetz M, Vlasselaers D, Ferdinande P, Lauwers P, Bouillon R
2001 Intensive insulin therapy in the critically ill patients. N Engl
J Med 345:13591367
2. Van den Berghe G, Wilmer A, Milants I, Wouters PJ, Bouckaert B,
Bruyninckx F, Bouillon R, Schetz M2006 Intensive insulin therapy
in mixed medical/surgical intensive care units: benefit versus harm.
Diabetes 55:31513159
3. MalmbergK1997Prospectiverandomisedstudyof intensiveinsulintreat-
ment on long term survival after acute myocardial infarction in patients
withdiabetes mellitus. DIGAMI (Diabetes Mellitus, InsulinGlucose Infu-
sion in Acute Myocardial Infarction) Study Group. BMJ 314:15121515
4. MalmbergK, RydenL, Wedel H, BirkelandK, BootsmaA, Dickstein
K, Efendic S, Fisher M, Hamsten A, Herlitz J, Hildebrandt P,
MacLeod K, Laakso M, Torp-Pedersen C, Waldenstro m A 2005
Intense metabolic control by means of insulin in patients with dia-
betes mellitus and acute myocardial infarction (DIGAMI 2): effects
on mortality and morbidity. Eur Heart J 26:650661
5. Furnary AP, Gao G, Grunkemeier GL, Wu Y, Zerr KJ, Bookin SO,
Floten HS, Starr A 2003 Continuous insulin infusion reduces mor-
tality in patients with diabetes undergoing coronary artery bypass
grafting. J Thorac Cardiovasc Surg 125:10071021
6. Gerstein HC, Miller ME, Byington RP, Goff Jr DC, Bigger JT, Buse
JB, Cushman WC, Genuth S, Ismail-Beigi F, Grimm Jr RH, Probst-
field JL, Simons-Morton DG, Friedewald WT2008 Effects of intensive
glucose lowering in type 2 diabetes. NEngl J Med 358:25452559
7. Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven
PD, Zieve FJ, Marks J, Davis SN, Hayward R, Warren SR, Goldman
S, McCarren M, Vitek ME, Henderson WG, Huang GD 2009 Glu-
cose control and vascular complications in veterans with type 2
diabetes. N Engl J Med 360:129139
8. Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M,
Marre M, Cooper M, Glasziou P, Grobbee D, Hamet P, Harrap S,
Heller S, LiuL, Mancia G, MogensenCE, PanC, Poulter N, Rodgers
A, Williams B, Bompoint S, de Galan BE, Joshi R, Travert F 2008
Intensive blood glucose control and vascular outcomes in patients
with type 2 diabetes. N Engl J Med 358:25602572
9. Turchin A, Matheny ME, Shubina M, Scanlon JV, Greenwood B, Pend-
ergrass ML 2009 Hypoglycemia and clinical outcomes in patients with
diabetes hospitalized in the general ward. Diabetes Care 32:11531157
10. Egi M, Bellomo R, Stachowski E, French CJ, Hart GK, Taori G,
Hegarty C, Bailey M2010 Hypoglycemia and outcome in critically
ill patients. Mayo Clin Proc 85:217224
11. Finfer S, Chittock DR, Su SY, Blair D, Foster D, Dhingra V, Bellomo R,
Cook D, Dodek P, Henderson WR, Hebert PC, Heritier S, Heyland DK,
McArthur C, McDonald E, Mitchell I, Myburgh JA, Norton R, Potter J,
Robinson BG, Ronco JJ 2009 Intensive versus conventional glucose con-
trol in critically ill patients. NEngl J Med 360:12831297
12. Moghissi ES, Korytkowski MT, DiNardo M, Einhorn D, Hellman
R, Hirsch IB, Inzucchi SE, Ismail-Beigi F, Kirkman MS, Umpierrez
GE 2009 American Association of Clinical Endocrinologists and
American Diabetes Association consensus statement on inpatient
glycemic control. Diabetes Care 32:11191131
13. Wang YY, Lin SY, Chuang YH, Chen CJ, Tung KC, Sheu WH2011
Adipose proinflammatory cytokine expression through sympathetic sys-
temisassociatedwithhyperglycemiaandinsulinresistanceinaratischemic
stroke model. AmJ Physiol Endocrinol Metab 300:E155E163
14. ONeill PA, Davies I, Fullerton KJ, Bennett D1991 Stress hormone
and blood glucose response following acute stroke in the elderly.
Stroke 22:842847
15. Hotamisligil GS 2006 Inflammation and metabolic disorders. Na-
ture 444:860867
16. Lewis GF, Carpentier A, Adeli K, Giacca A 2002 Disordered fat
storage and mobilization in the pathogenesis of insulin resistance
and type 2 diabetes. Endocr Rev 23:201229
17. Carvalho GQ, Pereira PF, Serrano HM, do Carmo Castro France-
schini S, Oliveira de Paula S, Priore SE, do Carmo Gouveia Peluzio
M 2010 Peripheral expression of inflammatory markers in over-
weight female adolescents and eutrophic female adolescents with a
high percentage of body fat. Appl Physiol Nutr Metab 35:464470
18. XuH, Barnes GT, Yang Q, TanG, Yang D, ChouCJ, Sole J, Nichols
A, Ross JS, Tartaglia LA, Chen H2003 Chronic inflammation in fat
plays a crucial role in the development of obesity-related insulin
resistance. J Clin Invest 112:18211830
19. Huang RC, Mori TA, Burke V, NewnhamJ, Stanley FJ, Landau LI,
Kendall GE, Oddy WH, Beilin LJ 2009 Synergy between adiposity,
insulin resistance, metabolic risk factors, and inflammation in ad-
olescents. Diabetes Care 32:695701
20. Pieracci F, Hydo L, Eachempati S, Pomp A, Shou J, Barie PS 2008
Higher body mass index predicts need for insulin but not hypergly-
cemia, nosocomial infection, or death in critically ill surgical pa-
tients. Surg Infect (Larchmt) 9:121130
21. Cammu G, Lecomte P, Casselman F, Demeyer I, Coddens J, Morias
K, Deloof T, Nobels F, Van Crombrugge P, Foubert L 2007 Prein-
duction glycemia and body mass index are important predictors of
perioperative insulin management in patients undergoing cardiac
surgery. J Clin Anesth 19:3743
22. Pasquel FJ, Spiegelman R, McCauley M, Smiley D, Umpierrez D,
Johnson R, Rhee M, Gatcliffe C, Lin E, Umpierrez E, Peng L, Umpi-
errez GE 2010 Hyperglycemia during total parenteral nutrition: an
important marker of poor outcome and mortality in hospitalized
patients. Diabetes Care 33:739741
J Clin Endocrinol Metab, September 2011, 96(9):26522662 jcem.endojournals.org 2661
23. OKeefe SJ 2006Physiological response of the humanpancreas toenteral
and parenteral feeding. Curr Opin Clin Nutr Metab Care 9:622628
24. Sarkisian S, Fenton TR, Shaheen AA, Raman M 2010 Parenteral
nutrition-associated hyperglycemia in noncritically ill inpatients is
associated with higher mortality. Can J Gastroenterol 24:453457
25. Carpentier AC, Bourbonnais A, Frisch F, Giacca A, Lewis GF 2010
Plasma nonesterified fatty acid intolerance and hyperglycemia are associ-
ated with intravenous lipid-induced impairment of insulin sensitivity and
disposition index. J Clin Endocrinol Metab 95:12561264
26. PrettyC, Chase JG, LinJ, ShawGM, Le Compte A, RazakN, Parente
JD 2011 Impact of glucocorticoids on insulin resistance in the crit-
ically ill. Comput Methods Programs Biomed 102:172180
27. Shivaswamy V, McClure M, Passer J, FrahmC, Ochsner L, Erickson
J, Bennett RG, Hamel FG, Larsen JL 2010 Hyperglycemia induced
by tacrolimus and sirolimus is reversible in normal Sprague-Dawley
rats. Endocrine 37:489496
28. Larsen JL, Bennett RG, Burkman T, Ramirez AL, Yamamoto S, Gulizia
J, Radio S, Hamel FG2006 Tacrolimus and sirolimus cause insulin resis-
tance in normal Sprague Dawley rats. Transplantation 82:466470
29. Torella R, Giugliano D, Improta L, Scognamiglio G, Sgambato S,
DOnofrio F 1980 Somatostatin and insulin secretion in man. IV.
The role of calcium. J Clin Endocrinol Metab 51:12981302
30. Wagner JD, Thomas MJ, Williams JK, ZhangL, Greaves KA, Cefalu
WT1998Insulinsensitivity andcardiovascular riskfactors inovari-
ectomized monkeys with estradiol alone or combined with no-
megestrol acetate. J Clin Endocrinol Metab 83:896901
31. Lidder P, Flanagan D, Fleming S, Russell M, Morgan N, Wheatley
T, Rahamin J, Shaw S, Lewis S 2010 Combining enteral with par-
enteral nutritiontoimprove postoperative glucose control. Br J Nutr
103:16351641
32. Ohkawa H, Fukuwa C, Matsuzawa-Nagata N, Yokogawa K,
Omura K, Miyamoto K2008 Soybean fat supplementation controls
insulin resistance caused by fat-free total parenteral nutrition.
J Pharm Pharmacol 60:461465
33. YokoyamaJ, SomeyaY, YoshiharaR, Ishii H2008Effects of high-mono-
unsaturated fatty acid enteral formula versus high-carbohydrate enteral
formula on plasma glucose concentration and insulin secretion in healthy
individuals and diabetic patients. J Int Med Res 36:137146
34. Pohl M, Mayr P, Mertl-Roetzer M, Lauster F, Lerch M, Eriksen J,
Haslbeck M, Rahlfs VW2005 Glycaemic control in type II diabetic
tube-fed patients with a new enteral formula low in carbohydrates
and high in monounsaturated fatty acids: a randomised controlled
trial. Eur J Clin Nutr 59:12211232
35. Alish CJ, Garvey WT, Maki KC, Sacks GS, Hustead DS, Hegazi RA,
Mustad VA 2010 A diabetes-specific enteral formula improves gly-
cemic variability in patients with type 2 diabetes. Diabetes Technol
Ther 12:419425
36. Visek J, Zourek M, Lacigova S, Rusavy Z2007 Influence of fiber on gly-
cemicindexofenteralnutrition.JPENJParenterEnteralNutr31:491495
37. Trence DL, Kelly JL, HirschIB2003The rationale andmanagement
of hyperglycemia for in-patients with cardiovascular disease: time
for change. J Clin Endocrinol Metab 88:24302437
38. Burns JD, Kosa SC, Wijdicks EF 2009 Central pontine myelinolysis
in a patient with hyperosmolar hyperglycemia and consistently nor-
mal serum sodium. Neurocrit Care 11:251254
39. OMalley G, Moran C, Draman MS, King T, Smith D, Thompson CJ,
Agha A2008 Central pontine myelinolysis complicating treatment of the
hyperglycaemic hyperosmolar state. Ann Clin Biochem45:440443
40. Korytkowski MT, Salata RJ, Koerbel GL, Selzer F, Karslioglu E,
Idriss AM, Lee KK, Moser AJ, Toledo FG2009 Insulin therapy and
glycemic control in hospitalized patients with diabetes during en-
teral nutrition therapy: a randomized controlled clinical trial. Dia-
betes Care 32:594596
41. Umpierrez GE, Hor T, Smiley D, Temponi A, Umpierrez D, Ceron
M, Munoz C, Newton C, Peng L, Baldwin D 2009 Comparison of
inpatient insulin regimens with detemir plus aspart versus neutral
protamine hagedorn plus regular in medical patients with type 2
diabetes. J Clin Endocrinol Metab 94:564569
42. Moghissi ES 2010 Addressing hyperglycemia from hospital admis-
sion to discharge. Curr Med Res Opin 26:589598
43. Lane WS, Cochran EK, Jackson JA, Scism-Bacon JL, Corey IB,
Hirsch IB, Skyler JS 2009 High-dose insulin therapy: is it time for
U-500 insulin? Endocr Pract 15:7179
44. Fallo F, Della Mea P, Sonino N, Bertello C, Ermani M, Vettor R,
Veglio F, Mulatero P 2007 Adiponectin and insulin sensitivity in
primary aldosteronism. Am J Hypertens 20:855861
45. Amend Jr WJ, Steinberg SM, Lowrie EG, Lazarus JM, Soeldner JS,
Hampers CL, Merrill JP 1975 The influence of serum calcium and
parathyroid hormone upon glucose metabolism in uremia. J Lab
Clin Med 86:435444
46. Lima Mde L, Cruz T, Rodrigues LE, BomfimO, Melo J, Correia R,
Porto M, Cedro A, Vicente E 2009 Serum and intracellular magne-
siumdeficiency inpatients withmetabolic syndromeevidences for
its relationtoinsulinresistance. Diabetes Res ClinPract 83:257262
47. Tanaka K, Kawano T, Tomino T, Kawano H, Okada T, Oshita S,
Takahashi A, Nakaya Y 2009 Mechanisms of impaired glucose
tolerance and insulin secretion during isoflurane anesthesia. Anes-
thesiology 111:10441051
48. TanakaK, KawanoT, Tsutsumi YM, KinoshitaM, KakutaN, Hirose K,
KimuraM, OshitaS2011Differential effectsofpropofol andisofluraneon
glucose utilization and insulin secretion. Life Sci 88:96103
49. Kitamura T, Ogawa M, Kawamura G, Sato K, Yamada Y2009 The
effects of sevoflurane and propofol on glucose metabolism under
aerobic conditions in fed rats. Anesth Analg 109:14791485
50. Paniagua MA, Hirsch IB2005 Insulin resistance as an adverse effect
of leuprolide and bicalutamide treatment. J Gerontol ABiol Sci Med
Sci 60:12831284
51. Mitrou P, Boutati E, Lambadiari V, Tsegka A, Raptis AE, Tountas
N, Economopoulos T, Raptis SA, Dimitriadis G 2010 Insulin resis-
tance in hyperthyroidism: the role of IL6 and TNF . Eur J Endo-
crinol 162:121126
52. Resmini E, Minuto F, Colao A, Ferone D 2009 Secondary diabetes
associated with principal endocrinopathies: the impact of newtreat-
ment modalities. Acta Diabetol 46:8595
53. Adlan MA, Bondugulapati LN, Premawardhana LD 2010 Glucose
intolerance and diabetes mellitus in endocrine disorderstwo case
reports and a review. Curr Diabetes Rev 6:266273
54. Maratou E, Hadjidakis DJ, Peppa M, Alevizaki M, Tsegka K, Lam-
badiari V, MitrouP, Boutati E, Kollias A, Economopoulos T, Raptis SA,
DimitriadisG2010Studiesofinsulinresistanceinpatientswithclinical and
subclinical hyperthyroidism. Eur J Endocrinol 163:625630
55. Arrese M, Riquelme A, Soza A 2010 Insulin resistance, hepatic ste-
atosis and hepatitis C: a complex relationship with relevant clinical
implications. Ann Hepatol 9 Suppl:112118
56. Raman VS, Loar RW, Renukuntla VS, Hassan KV, Fishman DS,
Gilger MA, Heptulla RA2011 Hyperglycemia and diabetes mellitus
in children with pancreatitis. J Pediatr 158:612616.e1
57. ItoT, Kawabe K, Arita Y, HisanoT, Igarashi H, Funakoshi A, Sumii
T, Yamanaka T, Takayanagi R 2007 Evaluation of pancreatic en-
docrine and exocrine function in patients with autoimmune pan-
creatitis. Pancreas 34:254259
58. Sterescu AE, Rhodes B, Jackson R, Dupuis A, Hanna A, Wilson DC,
Tullis E, Pencharz PB2010 Natural history of glucose intolerance in
patients with cystic fibrosis: ten-year prospective observation pro-
gram. J Pediatr 156:613617
59. Tuthill A, Semple RK, Day R, Soos MA, Sweeney E, Seymour PJ,
Didi M, Orahilly S 2007 Functional characterization of a novel
insulin receptor mutation contributing to Rabson-Mendenhall syn-
drome. Clin Endocrinol (Oxf) 66:2126
60. Hegele RA 2003 Monogenic forms of insulin resistance: apertures that
expose the common metabolic syndrome. Trends Endocrinol Metab 14:
371377
61. Musso C, Cochran E, Moran SA, Skarulis MC, Oral EA, Taylor S,
Gorden P 2004 Clinical course of genetic diseases of the insulin
receptor (type A and Rabson-Mendenhall syndromes): a 30-year
prospective. Medicine (Baltimore) 83:209222
2662 Larsen and Goldner Severe Insulin Resistance J Clin Endocrinol Metab, September 2011, 96(9):26522662
S-ar putea să vă placă și
- Allah (SWT) Is The Best of Those Who PlotDocument4 paginiAllah (SWT) Is The Best of Those Who PlotIffatNaeemÎncă nu există evaluări
- Hypothyroidism AIM 2009Document16 paginiHypothyroidism AIM 2009IffatNaeem100% (1)
- Non-Thyroidal Illness Endo Clin NA 2007Document16 paginiNon-Thyroidal Illness Endo Clin NA 2007IffatNaeemÎncă nu există evaluări
- MGMT Subclinical HypothyroidismDocument4 paginiMGMT Subclinical HypothyroidismIffatNaeemÎncă nu există evaluări
- Approach To NTMNG Jcem 2011Document11 paginiApproach To NTMNG Jcem 2011IffatNaeemÎncă nu există evaluări
- Amiodarone & Thyroid Disease JCEM 2010Document8 paginiAmiodarone & Thyroid Disease JCEM 2010IffatNaeemÎncă nu există evaluări
- Yale Insulin Infusion ProtocolDocument2 paginiYale Insulin Infusion ProtocolIffatNaeemÎncă nu există evaluări
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- SOAP FormatDocument2 paginiSOAP FormatFarooq ShahÎncă nu există evaluări
- Plant Usage in Protecting The Farm Animal Health - V. Davidović, M. Joksimović Todorović, B. Stojanović, R. RelićDocument12 paginiPlant Usage in Protecting The Farm Animal Health - V. Davidović, M. Joksimović Todorović, B. Stojanović, R. RelićCk_psihÎncă nu există evaluări
- List of Books To Be Used For Rasashastra Data CollectionDocument1 paginăList of Books To Be Used For Rasashastra Data CollectionMikel MillerÎncă nu există evaluări
- Work Work - Life Balance Life Balance ƛ ƛ Understanding The Complex World Understanding The Complex WorldDocument22 paginiWork Work - Life Balance Life Balance ƛ ƛ Understanding The Complex World Understanding The Complex WorldKrishan SainiÎncă nu există evaluări
- Bells That Ring - Proctor, K. (1997)Document4 paginiBells That Ring - Proctor, K. (1997)elaineÎncă nu există evaluări
- Scorpion Envenomation Causing Neuromuscular Toxicity (United States, Mexico, Central America, and Southern Africa) - UpToDateDocument28 paginiScorpion Envenomation Causing Neuromuscular Toxicity (United States, Mexico, Central America, and Southern Africa) - UpToDatejoaoalmeida_1955100% (1)
- Brand Name - Generic NameDocument6 paginiBrand Name - Generic Namejonette carataoÎncă nu există evaluări
- Cardiogenic ShockDocument27 paginiCardiogenic ShockMuhammad Ikbar100% (1)
- List of Permitted Ayurveda Colleges For The A.Y. 2021-22 Till 06.05.2022Document52 paginiList of Permitted Ayurveda Colleges For The A.Y. 2021-22 Till 06.05.2022Re Ed EstÎncă nu există evaluări
- Bereavement and Autism: A Universal Experience With Unique ChallengesDocument11 paginiBereavement and Autism: A Universal Experience With Unique ChallengesBrian A. Wong100% (1)
- CGHS Rates 2014 - AhmadabadDocument72 paginiCGHS Rates 2014 - AhmadabadJayakrishna ReddyÎncă nu există evaluări
- CHN HandiesDocument10 paginiCHN HandiesFreeNursingNotesÎncă nu există evaluări
- The Use of Hypnosis and Systematic Desensitisation in The Management of Dental Phobia A Case ReportDocument6 paginiThe Use of Hypnosis and Systematic Desensitisation in The Management of Dental Phobia A Case ReportAnissa Citra UtamiÎncă nu există evaluări
- Drug Design Metabolism 3Document19 paginiDrug Design Metabolism 3Hanaa HashemÎncă nu există evaluări
- Management of PreeclampsiaDocument11 paginiManagement of PreeclampsiaDanÎncă nu există evaluări
- Mood Disorders Lesson PlanDocument17 paginiMood Disorders Lesson Planapi-2841042060% (1)
- Homeopathy and DentistryDocument3 paginiHomeopathy and DentistrynadiidaÎncă nu există evaluări
- 필라테스 논문Document6 pagini필라테스 논문Kang Hoon KimÎncă nu există evaluări
- Blood Gas Analysis: Zulkifli. DR., Span., Mkes Department of Anesthesiology and Reanimation FK Unsri/ RSMHDocument20 paginiBlood Gas Analysis: Zulkifli. DR., Span., Mkes Department of Anesthesiology and Reanimation FK Unsri/ RSMHIvanRaykaÎncă nu există evaluări
- Approved Practice Setting With Facility License Number and Contact Oct 2023Document30 paginiApproved Practice Setting With Facility License Number and Contact Oct 2023ns5qp4t26dÎncă nu există evaluări
- Critical Care Nursing Diagnosis and Management UrdenDocument8 paginiCritical Care Nursing Diagnosis and Management UrdenMonet0% (1)
- Iliotibial Band Syndrome - FannyDocument13 paginiIliotibial Band Syndrome - FannyAlfiani Rosyida Arisanti Syafi'iÎncă nu există evaluări
- 1-Prirodno Okruzenje I Mentalno ZdravljeDocument8 pagini1-Prirodno Okruzenje I Mentalno ZdravljeUvoBubaÎncă nu există evaluări
- Case Study PresentationDocument21 paginiCase Study Presentationmaeumi3008100% (1)
- A New Neurofeedback Protocol For DepressionDocument12 paginiA New Neurofeedback Protocol For DepressionVezér RóbertÎncă nu există evaluări
- Project Isr - JascapDocument42 paginiProject Isr - JascapPrakrutiShahÎncă nu există evaluări
- Modul 06 PDFDocument16 paginiModul 06 PDFL TereÎncă nu există evaluări
- Application of Orems Theory To NSG PracticeDocument26 paginiApplication of Orems Theory To NSG PracticeLorde Sungcad Ricafrente100% (3)
- Ictus Ortesis MmiiDocument10 paginiIctus Ortesis MmiiCeto Ust Puerto MonttÎncă nu există evaluări
- TB Case Finding (Slide)Document15 paginiTB Case Finding (Slide)Emman Acosta DomingcilÎncă nu există evaluări