Documente Academic
Documente Profesional
Documente Cultură
Clinical Governance
Încărcat de
ummuawisyDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Clinical Governance
Încărcat de
ummuawisyDrepturi de autor:
Formate disponibile
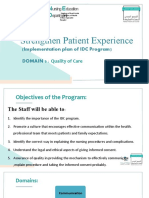
ACHIEVING EXCELLENCE
IN CLINICAL GOVERNANCE
Framework Document and Companion Guide
for the Integrated Management
of Quality, Safety and Risk In
The Malaysian Health Care System
Patient Safety Council of Malaysia & Quality in Medical Care Section
Medical Development Division Ministry of Health Malaysia
02.LayOut 12/3/10 4:55 PM Page 1
2 Achieving Excellence In Clinical Governance
1. Framework Document
for the integrated management of quality, safety and risk in
the Malaysian health care system
2. Companion Guide
to support self-assessment against the Framework
Document
3. Electronic Self Assessment Tool
in the form of a CD
This document
consists of three parts:
02.LayOut 12/3/10 4:55 PM Page 2
Contents
Achieving Excellence In Clinical Governance 3
Section A
1.0 Purpose 8
2.0 Background 8
2.1 The objectives of the Clinical Governance Framework 9
2.2 Related Policy and Regulatory Considerations 9
3.0 A Framework for the Integrated Management of Quality, Safety & Risk 11
3.1 Introduction 11
3.2 6 Essential Underpinning Requirements: 12
3.2.1 Communication and Consultation with Key Stakeholders 12
3.2.2 Clear Accountability Arrangements 12
3.2.3 Adequate Capacity and Capability 13
3.2.4 Standardized Policies, Procedures, Protocols and Guidelines 13
3.2.5 Monitoring and Review Arrangements 13
3.2.6 Assurance Arrangements 13
3.3 Check Questions 13
4.0 Six Core Processes and Programmes 16
4.1 Clinical Effectiveness and Audit 16
4.2 Involvement of Patients/ Service Users and the Public/ Community 16
4.3 Risk Management and Patient Safety 16
4.3.1 Risk Management Process 16
4.3.2 High-Priority Risk 16
4.3.3 Patient Safety 17
4.3.4 Occupational Health and Safety 17
4.3.5 Environmental Safety 17
4.3.6 Incident and Complaints Reporting/ Recording, Analysis and Learning 17
4.4 Staffing and Staff Management 17
4.5 Service Improvement 17
4.6 Learning and Sharing Information 18
4.7 Check Questions 18
5.0 Outcomes 21
5.1 Key Performance Indicators (KPIs) 21
5.2 Check Questions 21
6.0 Conclusion 22
02.LayOut 12/3/10 4:55 PM Page 3
4 Achieving Excellence In Clinical Governance
Section B
1. Introduction 24
1.1 Background 24
1.2 Performing a Self-assessment Against the Framework 25
1.3 Electronic Self-Assessment Tool 26
1.3.1 Running the Tool 26
1.3.2 Entering Data
1.3.3 Recording Good Practice 28
1.3.4 Recording Actions or Quality Improvement Plans (QIPs) 28
1.3.5 Aggregating information Across Departments, etc. 29
1.3.6 Analysing the data 30
1.4 Beyond self-assessment I - Improving Quality, Safety and Risk 33
management using the Plan-Do-Study-Act (PDCA) Improvement Model
1.5 Beyond Self-Assessment II - Improving quality, Safety and Risk 33
Management Using the HSE Change Model
2. Essential underpinning requirements 35
A Communication and Consultation with Key Stakeholders 35
B Clear Accountability Arrangements 37
C Adequate Capacity and Capability 39
D Standardised Policies, Procedures and Guidelines 41
E Monitoring and Review Arrangements 42
F Assurance Arrangements 44
3. Core processes and programmes 45
G Clinical Effectiveness and Audit 45
H Patient and Public Involvement 49
I Risk Management and Patient Safety 50
J Staffing and Staff Management 54
K Service Improvement 55
L Learning and Sharing Information 57
4. Outcomes 59
M Key Performance Indicators (KPIs) 59
5. Glossary of Terms 61
6. Frequently Asked Questions (FAQs) 65
02.LayOut 12/3/10 4:55 PM Page 4
Achieving Excellence In Clinical
Governance
Framework Document and Companion Guide
for the Integrated Management
of Quality, Safety and Risk In
The Malaysian Health Care System
02.LayOut 12/3/10 4:55 PM Page 5
6 Achieving Excellence In Clinical Governance
Foreword
By The Director-General of Health Malaysia
and Chairman of the Patient Safety Council of Malaysia
S
afety is an integral component of quality health care and one which
patients, their families as well as health care professionals value.
Patients and their families expect to receive health care that is safe as
well as effective. Thus, it is indeed apt that the safety of our healthcare
system be given paramount importance in line with the first principle of
medicine, Primum non nocere or Above all, do no harm, which is an
espoused value that all health care professionals subscribe to.
Making the Malaysian health care system safer has always been one of the
key goals of the Ministry of Health and is a core element of its many Quality
improvement activities. Malaysia is also a strong supporter of the WHOs
World Alliance for Patient Safety, to which it became one of the earliest
signatories in the world, in May 2006.
The pursuit of quality and safety requires the concerted efforts of all the
major stakeholders and the building of partnerships. Developing a safe
Malaysian health care system necessitates the institutionalization of a
culture of safety within it and one of the key steps is to do away with the
prevailing blaming and finger-pointing culture, replacing it with a just or
non-punitive, learning culture. This culture is a necessary requirement for
the successful implementation of clinical governance.
I am pleased that the Patient Safety Council of Malaysia and the Quality in
Medical Care Section, Medical Development Division of the Ministry of
Health, through the development of smart partnerships with both the public
and private sectors as well as the WHO, have succeeded in producing this
Achieving Excellence in Clinical Governance: Framework Document and
Companion Guide for the Integrated Management of Quality, Safety and
Risk in the Malaysian Health Care System which are part of the formidable
arsenal to develop and attain good Clinical Governance.
To begin our journey towards a safer health care system, elements of the
Clinical Governance Framework should be studied, discussed and
implemented by all stake-holders. Thus, I would like to wish all of you every
success as you endeavour to develop a world class health care system that
is capable of providing safe, effective, equitably-accessed and patient-
centred services to all who require them.
Tan Sri Dato Seri Dr. Hj. Mohd Ismail Merican
Director-General of Health Malaysia
02.LayOut 12/3/10 4:55 PM Page 6
Achieving Excellence In Clinical Governance 7
Advisors
Tan Sri Dato Seri Dr. Hj. Mohd Ismail Merican
Director-General of Health Malaysia and Chairman of the Patient Safety Council of Malaysia
Datuk Dr. Noor Hisham bin Abdullah
Deputy Director-General of Health (Medical), MOH
Dato Dr. Hassan bin Abdul Rahman
Deputy Director-General of Health (Public Health), MOH
Dato Dr. Maimunah bt. Abdul Hamid
Deputy Director-General of Health (Research and Technical Support), MOH
Dato Dr. Hj. Azmi bin Shapie
Director of Medical Development, Medical Development Division, MOH
Members of the Patient Safety Council of Malaysia
Authors
Dr. Hjh Kalsom bt. Maskon
Public Health Physician, Quality In Medical Care Section, Medical Development Division, MOH
Dr. PAA Mohamed Nazir bin Abdul Rahman
Public Health Physician, Quality In Medical Care Section, Medical Development Division, MOH
Mr. Stuart Emslie
WHO and MOH Consultant on Patient Safety and Clinical Risk Management, United Kingdom
Dr. Nor Aishah bt. Abu Bakar
Public Health Physician (Occupational Health), Quality In Medical Care Section, Medical Development
Division, MOH
Dr. Amin Sah bin Hj. Ahmad
Public Health Physician (Hospital and Health Management), Quality in Medical Care Section, Medical
Development Division, MOH
Secretariat
Sister Rashidah Ngah
Quality In Medical Care Section, Medical Development Division, MOH
Mrs. Roshaidah Othman
Quality In Medical Care Section, Medical Development Division, MOH
02.LayOut 12/3/10 4:55 PM Page 7
8 Achieving Excellence In Clinical Governance
1. Purpose
This document is intended to provide a broad policy direction for the adoption of Clinical Governance as
the over-arching framework for integrating all the Quality, Safety and Risk Management initiatives in the
health and health-related agencies in Malaysia, both public and private.
2. Background
The Ministry of Health Malaysia (MOH), as the lead agency for health in the country, is committed to
driving the health care sector in the provision of safe, high quality services through the implementation
of the Clinical Governance concept. Other health and health-related agencies in the public and private
sectors are actively implementing quality improvement efforts so as to improve the quality and safety of
patient care, in line with international efforts led by the World Alliance for Patient Safety, to which Malaysia
became a signatory in 2006. These activities are also ably supported by the Patient Safety Council of
Malaysia, set up by Cabinet decree in January 2003, and comprising key stake-holders of health in the
Malaysian health care system. The Patient Safety Council of Malaysia has been entrusted to lead national-
level efforts targeted at promoting and enhancing patient safety.
The Clinical Governance concept was first introduced to the National Health Service in England in the
1990s, in its attempt to improve the quality and safety of healthcare, in a systematic, integrated and
organized manner. Clinical Governance is a framework of accountability for quality and excellence in
health care in the National Health Service (NHS) of the United Kingdom. It is defined as a framework
through which NHS organizations are accountable for continually improving the quality of their health
services and safe-guarding high standards of care by creating an environment in which excellence in
clinical care will flourish. The NHS in Scotland defines Clinical Governance as corporate
accountability for clinical performance.
Currently, the many quality improvement initiatives being implemented are conducted by separate groups
of professionals, using their preferred approaches and methods, and are not integrated
1
. The framework
described in this document provides a comprehensive and clear picture of the quality and safety
improvement programmes as well as their linkages. It also defines the roles and responsibilities of the
health care organizations involved.
The MOHs vision of a safe health care system is epitomised by the 1Care for 1Malaysia concept, initiated
by the Malaysian Government, which focuses on people-centred health care services and gives priority to
performance, as embodied in the motto People First, Performance Now.
1Care is a structured national health system that is responsive and provides choice of quality health care, ensuring
universal coverage for the healthcare needs of the Malaysian population, based on solidarity and equity
Dato Dr. Maimunah bt. Abd.Hamid, Deputy Director-General of Health (Research and Technical Support)
To realize this noble vision, there is thus the need for a framework for the improvement of governance in
health care as well as the health care delivery system. The role of the MOH is manifold, one of which is
the development, implementation, monitoring of performance and evaluation of the various Quality
Improvement (QI) activities (which target patient safety) in the Quality Assurance Programme (QAP) in
Government hospitals. The MOH is also actively engaging the private sector, as key stake-holders of
health care, to further strengthen their capacity and capability to improve the quality and safety of health.
Raising and maintaining the quality and safety of health care requires commitment to continuous
improvement from everyone involved in the health care system as epitomised by the motto Quality and
Safety, its Everybodys Business and is expected to achieve the best possible health outcomes and
quality of life for the population within the resources available.
1
Research on Evaluation of Quality Assurance Programme, Institute for Health Systems Research, 2009
02.LayOut 12/3/10 4:55 PM Page 8
Achieving Excellence In Clinical Governance 9
The document is based on a framework that had been developed for, and is currently being implemented
in the public healthcare system in the Republic of Ireland, which is governed by the Health Service
Executive (HSE). It is based on the WHO and MoH Consultants ten year experience in implementing
clinical governance in public healthcare systems in the United Kingdom, Australia and Ireland. The WHO
consultant provided technical assistance in imparting practical knowledge and skills to implement an
integrated framework for the MoH Malaysia in 2009. Since 2006, the MOH has received technical support
from the WHO to develop and implement Clinical Risk Management, Incident Reporting and Root Cause
Analysis as a method of reporting, learning and improving the safety of health care delivered.
2.1 The Objectives of the Clinical Governance Framework are:
To ensure that there is a systematic framework for the healthcare sector (public and private) for
the integration of quality, safety and risk management programmes to support and drive the
provision of safe, effective and high quality services
To drive core programmes for quality, safety and risk management
To ensure that appropriate accountability, leadership and oversight arrangements are in place
to institutionalise and internalise quality and safety
It is hoped that greater synergy will be achieved through the harmonization of quality improvement
initiatives, which will contribute towards the institutionalisation of a culture of quality and professionalism
amongst health personnel at all levels.
Recognizing the multiple approaches and programmes already in place to improve quality, safety and risk
management within the Malaysian health sector, this document is not intended to be highly prescriptive.
Rather, the key requirements are set out as check questions which are provided for consideration by
service managers and clinicians in an attempt to identify any areas for improvement. A Self-Assessment
Tool is available to allow service providers to score themselves in relation to the check questions. The
Companion Guide is provided as an additional guidance to help meet the requirements of the check
questions.
2.2 Related policy and regulatory considerations
The critical importance of patient safety, quality of care and management of risk generally in the
planning, provision and review of health services is increasingly being recognized. The commitment
of the MOH towards quality is emphatically stated in its vision, mission and the core elements of its
corporate culture.
02.LayOut 12/3/10 4:55 PM Page 9
10 Achieving Excellence In Clinical Governance
Vision for Health A nation working together for better health
The Mission of the Ministry of Health is to lead and work in partnership
To facilitate and support the people to
attain fully their potential in health
appreciate health as a valuable asset
take individual responsibility and positive action for their health
To ensure a high quality health system that is
customer-centred
equitable
affordable
efficient
technologically appropriate
environmentally adaptable
innovative
with emphasis on:
professionalism, caring and teamwork
respect for human dignity
community participation
With the launching of the MOHs National Quality Assurance Programme (QAP) in 1985, Quality in health care
became a system-wide issue, from the previously individual professionals concern (through professional
excellence and self-regulation). Thus, Quality became everybodys business. Since then, all the Divisions of
the MOH have implemented Quality Improvement (QI) activities utilising the various relevant approaches, such
as the following:-
Indicator approach National Indicator Approach (NIA)
Key Performance Indicators (KPI)
Hospital Specific Approach (HSA)
Clinical Audit Peri-operative Mortality Review (POMR)
Adult Intensive Care Unit Audit, incorporating Care Bundles
Maternal and Peri-natal Mortality Review
Nursing Audit
External Organisation Audit Hospital Accreditation Programme (MSQH)
ISO
Clinical Risk Management Incident Reporting and Learning Systems
(including RCA and HFMEA)
WHO Global Patient Safety Challenge
Hospital Infection Control
Occupational Safety and Health
Patient-Centred Services Patient Satisfaction Surveys
Complaints Management
Statistical Process Control Cumulative Summation (CUSUM) incorporated in Clinical
Registries
02.LayOut 12/3/10 4:55 PM Page 10
Achieving Excellence In Clinical Governance 11
In May 1998, the Strategic Plan for Quality in Health (MOH/PPAK-15(QAP)
2
) which outlined the goals,
policies and strategies for quality improvement efforts in the MoH, was developed and adopted by the
MOH. It provided:
a framework within which decisions may be made regarding priorities and needs in addressing
quality-related issues
the direction of the various quality improvement strategies and activities; and a strategic framework
which was to be implemented at the various levels by all involved in pursuing quality in health care.
Thus, Quality Improvement (QI) has become the official MoH policy with the establishment of QA
committees at all levels of the organization, from the MOH level (QA Steering committee), Programme (or
Division) level, State level, to the hospital level. In addition, the Private Healthcare Facilities and Services
Act 1998 and Regulations 2006 mandate QI in private healthcare facilities for the following: National
Mortality Assessment, Incident Reporting and QI activities, thus making Quality and Safety a nation-wide
concern. This commitment was further reinforced in May 2006, when the Hon. Minister of Health ratified
Malaysias participation in the World Alliance for Patient Safety, making Malaysia one of the earliest
countries in the world committed to supporting WHOs comprehensive programme for patient safety at
national level.
The Government of Malaysia is committed to the equitable provision of excellent services to the Malaysian
public by promoting and implementing national efforts in quality improvement (QI). Government Circulars
are regularly produced and disseminated for implementation to drive the public sector towards excellence
in service delivery as well as outcomes through the implementation of quality initiatives such as MS ISO,
Total Quality Management (TQM), Key Performance Indicators (KPI), Innovation, The Prime Ministers
Quality Awards, Star Rating, Accreditation and others. The latest drive is towards measuring performance
using Key Performance Indicators for the nation and the Ministries, in line with the achievement of set
targets in priority Key Result Areas (KRAs) for the health sector in this country.
3. A Framework for the Integrated Management of Quality, Safety and Risk
3.1 Introduction
Acknowledgements: This framework is adapted from the Health Service Executive (HSE), Ireland:
Framework Document Version 1, January 2009 Towards Excellence in Clinical Governance A
Framework for Integrated Quality, Safety and Risk Management Across HSE Service Providers, is
based on the HSE Quality and Risk Standard. Questions in Section H are adapted from the Victorian
Health Safety and Quality Framework, Australia.
A training session and testing of the framework for the Malaysian context was conducted by the
WHO Consultant from 19th to 21st August 2009. Participants from various levels included the State
Health Deputy Directors (Medical), Hospital Directors, University Malaya, Universiti Kebangsaan
Malaysia, the Malaysian Society for Quality in Health (MSQH), KPJ group, MOHs Public Health
Division and the Secretariat of the Patient Safety Council of Malaysia, The assessments provided a
forum for introducing the framework and an initial assessment of the status of the health service
organisations in Malaysia, and the framework was well-received by all participants.
There are three key components to the framework
3
:
i. Essential underpinning requirements (equivalent to Donabedians structure)
ii. Core processes and programmes (equivalent to Donabedians process)
iii. Performance indicators (equivalent to Donabedians outcomes)
2
The Strategic Plan for Quality in Health, MOH, 1998
3
An Introduction to Quality Assurance in Health Care. Oxford University Press. 2000. The three components are based on the three components of
Avedis Donabedians Structure, Process, Outcome Model of Quality
02.LayOut 12/3/10 4:55 PM Page 11
12 Achieving Excellence In Clinical Governance
Figure 1: illustrates the framework for the integrated management of quality, safety and risk, adopted and
modified for use.
Figure 1- Framework for Intergrated Quality, Safety and Risk Management
These components form the basis for health care providers, through the process of self-assessment, to
determine the extent to which an integrated quality, safety and risk management system is in place in their
organizations. A total of 69 check questions relating to key aspects of the framework have been developed.
The supporting document, the Companion Guide and the Self-Assessment Tool, modified for the Malaysian
context, can be used by health managers and clinicians to assess the extent to which an integrated framework
for quality, safety and risk management is in place within their hospital or health service. On completion of the
self- assessment process, where there are improvements that are needed, an action plan should be developed.
Regular monitoring and review of the action plans will ensure that actions are being implemented, leading to
better outcomes.
3.2 6 Essential underpinning requirements (Donabedians Structure)
Like the skeletal structure of a human being, the essential underpinning requirements must be in
place, in order to drive safe and effective service. Effective leadership and management are required
to lead the quality, safety and risk management agenda.
3.2.1 Communication and consultation with key stakeholders
Structures and strategies to facilitate effective communication and consultation with key
stakeholders must be in place within and outside the organization. In addition, stakeholder
analysis should be conducted. This is to ensure that all relevant stakeholders are
identified and that appropriate mechanisms for communication and consulting with the
various stakeholders or stakeholder groups are put in place.
3.2.2 Clear accountability arrangements
Accountability arrangements for quality and risk management should be clearly defined
and put in place at all levels, from front-line staff up to the organisations most senior
Assurance Communication
Policies
Capacity &
Capabality
Monitoring &
Review
Patient /
Services Users
Accountability
Learning and Sharing Information
Learning form incident reviews
Learning from patient experience
Risk Management & Patient Safety
Complaints/claims/incident
Health and safety
Risk management process
Staffing & Staff Management
Workplace planning and recruitment
Induction
Continuous professional development
Clinical Effectiveness and Audit
Clinical guidelines
Clinical Audit
Service Improvement
Identifying bottlenecks
Reducing inefficiencies
Reducing variation in key processes e.g
discharge
Patient/Service/User and
Public/Community Involvement
Patient information
Consumer panels
Patient experience surveys
Outcome Outcome
Outcome Outcome
Outcome Outcome
02.LayOut 12/3/10 4:55 PM Page 12
Achieving Excellence In Clinical Governance 13
accountable manager or governing body. Individual responsibilities will be set out in the
job descriptions. Accountability arrangements for committees and /or groups involved in
quality, safety and risk management with terms of reference and robust reporting
arrangements must be set. Independent groups that must work together effectively and
share resources should be linked by hierarchy, information systems, and where relevant,
common memberships.
The organization will establish a committee or group to oversee quality, safety and risk
management performance and report periodically to local senior management. To achieve
comprehensive quality, safety and risk management across all service providers, it is
recommended that, where relevant, the committee comprises members from many
disciplines.
3.2.3 Adequate capacity and capability
Capacity and capability imply adequate numbers of qualified people as well as adequate
physical and financial resources. The organisation should have the capacity and
capability to implement and monitor effective quality, safety and risk management
systems. Managers at all levels should fulfill their responsibility by demonstrating
commitment to the management of quality, safety and risk.
3.2.4 Standardised policies, procedures, protocols and guidelines
The organisation should have a system in place to facilitate the development of
standardized policies, procedures, protocols and guidelines. These guidelines should be
based on best available evidence and should be governed by a formal document control
process that includes processes to support the on-going review and change of policies
and guidelines. Staff should be provided with support and guidance on the sourcing,
appraising, and implementation of evidence-based practice and on implementing any
resulting changes in practice. Where new services are being established, the development
of policies, procedures, protocols and guidelines should be considered at the time of
commissioning.
3.2.5 Monitoring and review arrangements
Senior managers should ensure adequate monitoring and review of the systems that are
in place for quality, safety and risk management. All aspects of the framework should be
regularly monitored and reviewed in order that management can learn from any weakness
in the systems and make improvements where necessary. There is a need to develop
suitable KPIs for quality, safety and risk management and to report on selected KPIs.
3.2.6 Assurance arrangements
Hospital directors/board of directors/top level managers should ensure that they obtain
sufficient assurance on the effectiveness of the systems in place for quality, safety and
risk management to form part of their monitoring and review process. Assurances can
come from a variety of sources either within or outside the orgnisation. The most objective
assurances are derived from independent reviewers such as internal audit or external
accreditation bodies (e.g. MSQH/JCI). These are supplemented from non-independent
sources which include clinical audit, mortality and morbidity reviews and internal
management processes, to name a few.
3.3 Check questions
The table below contains check questions that can be utilised to gain an understanding of their
strengths and areas for improvement in relation to implementation of the underpinning requirements
outlined above. The responses to these questions can be either yes, no, partial, not applicable
or dont know. The partial responses are categorised as low, moderate or high. Where a no
or partial response is provided, an action plan or quality improvement plan (QIP) should be
developed to implement any requirements. Where the question number box is shaded, this denotes
that the response to the question may need input and aggregation of information from a number of
departments, Further information on the assessment process is provided in the Companion Guide
and also with the Self-Assessment Tool.
02.LayOut 12/3/10 4:55 PM Page 13
14 Achieving Excellence In Clinical Governance
Clinical Governance Self-Assessment Tool
ESSENTIAL UNDERPINNING REQUIREMENTS: CHECK QUESTIONS
A. Communication and consultation with key stakeholders with regard to Goals and Objectives
for safety
1. Has a stakeholder analysis been carried out to identify all internal and external
stakeholders relating to quality, safety and risk management?
2. Are arrangements in place to ensure that the stakeholder analysis is maintained up-to-date?
3. Is there effective communication and consultation with internal stakeholders in relation to the
purpose, objectives and working arrangements for quality, safety and risk management?
4. Are internal and, (where appropriate), external stakeholders kept fully informed of progress in
achieving objectives for quality, safety and risk management?
5. Is there effective communication and consultation with external stakeholders in relation to
quality, safety and risk management?
B. Clear accountability arrangements (Roles and Responsibilities)
1. Are clearly documented accountability arrangements in place to support the hospital director to
discharge his/her responsibility for quality, safety and risk management?
2. Do the documented accountability arrangements ensure that that the hospital director is fully
informed in relation to key areas of quality, safety and risk performance?
3. Within the accountability arrangements, are the roles and responsibilities played by any
committees or groups clearly described?
4. Do committee structures and reporting arrangements provide for co-ordination and integration
of quality, safety and risk activities and priorities?
C. Adequate capacity and capability
1. Do managers and clinicians at all levels demonstrate commitment to the management of
quality, safety and risk?
2. Do service planning and other business arrangements take into account the hospitals quality,
safety and risk management Goals and Priorities when developing budget and other financial
strategies?
3. Is a specified portion of the hospitals annual budget committed to achieving defined goals for
quality, safety and risk management?
4. Is there access to appropriate resources to implement effective quality, safety and risk
management systems, e.g. qualified people, physical and financial resources, access to
specialist expertise, etc.?
5. Information and training programmes: Are there structured training programmes to ensure that
all staff are provided with adequate quality, safety and risk management information, instruction
and training appropriate to their role?
02.LayOut 12/3/10 4:55 PM Page 14
Achieving Excellence In Clinical Governance 15
D. Standardised policies, procedures, protocols and guidelines
1. Does the hospital operate a standardized document control process for all policies, procedures,
protocols and guidelines?
2. Are arrangements in place for training staff in appraising and developing policies, procedures,
protocols and guidelines and for identifying evidence-based best practice?
3. Are policies, procedures, protocols and guidelines standardized throughout the hospital and,
where appropriate, are they evidence-based?
4. Are arrangements in place to ensure that, where new services are being established, the
development of policies, procedures, protocols and guidelines is considered at the time of
commissioning?
E. Monitoring and review arrangements
1. Are all aspects of the framework described in this document regularly monitored and reviewed
in order that management can learn from any weaknesses in the systems and make
improvements, where necessary?
2. Are the results of independent and other audits used to improve the hospitals quality, safety
and risk management systems?
3. Are key performance indicators reviewed regularly to identify and correct shortfalls to drive
continuous improvement in quality, safety and risk management?
F. Assurance arrangements
1. Do the hospital director and senior management receive sufficient assurance on the systems in
place for quality, safety and risk management?
2. Do the assurances received by the hospital director and senior management form an integral
part of their on-going monitoring and review processes?
02.LayOut 12/3/10 4:55 PM Page 15
16 Achieving Excellence In Clinical Governance
4. Six Core Processes and Programmes (Donabedians Process)
Where appropriate, healthcare organisations should have in place the following core processes and
programmes:
4.1 Clinical effectiveness and audit
The term clinical effectiveness is used in this document to encompass clinical audit, QA or HSA
studies and evidence-based practice (refer to Companion Guide)
A structured programme, or programmes, should be in place to systematically monitor and improve
the quality of clinical care provided across all services. This should include, systems to monitor
clinical effectiveness activity (including clinical audit);mechanisms to assess and implement relevant
clinical guidelines; systems to disseminate relevant information; and use of supporting information
systems.
The processes and outcomes of care should be regularly audited and should demonstrate that the
delivery of care reflects adopted guidelines and protocols. Audits should be based on agreed
selection criteria such as: high risk, cost, or volume: serious concerns arising from adverse events
or complaints: new guidelines: local or national priorities; or patient focus.
Where appropriate, and whenever possible, clinical effectiveness activities should be patient -
centred, i.e., they should take into account the whole patient journey. This requires multi-
professional working and may require collaboration across organizational boundaries.
Clinical effectiveness activities have a significant cost implication in terms of the resources required
to support projects and the opportunity cost of professionals examining and assessing their
practice. These costs need to be justified and hospitals should be able demonstrate that the clinical
effectiveness activities that they support result in demonstrable improvements in the standards of
care and represent efficient use of resources.
4.2 Involvement of patients /service users and the public/ community
Mechanisms should be in place to involve patients/service users and the public/communities in the
planning, development, delivery and evaluation of health services. These mechanism should be
evaluated and the results of this involvement used to improve the manner in which services are
configured or delivered. This should include a systematic process to ensure that hospitals respond
to, and learn from all forms of feedback.
The involvement of service users and the community should be facilitated at all levels of the
hospitals, including individual care episodes, information development, service planning, staff and
service user education and quality review and improvement.
4.3 Risk management and patient safety
4.3.1 The risk management process
Risks of all kinds should be systematically identified, assessed and managed in order of
priority, in accordance with international standard ISO 31000 Risk management:
Principles and guidelines on implementation. Risk of all kinds means that risks need
to be managed across the board, including risk to the safety and quality of patient care;
occupational health, safety and welfare risk; environmental and fire safety risk; risks to
business continuity; and so on. The principal vehicle for managing and communicating risk
at all levels is the risk register, which allows a repository of risk information to be
maintained.
4.3.2 Knowing high-priority risks
Notwithstanding the need to systematically identify, assess and manage risks of all kinds,
service providers should be able to demonstrate that they have systems in place to manage
known high-priority risk issues such as:
02.LayOut 12/3/10 4:55 PM Page 16
Achieving Excellence In Clinical Governance 17
- Medication management
- Slip, trips and falls
- Violence and aggression
- Infection control
- Haemovigilance
- Utility contingency
- Medical devices
- Waste management
- Moving and handling
- Suicide and deliberate self-harm
- Patient absconsion
- Management of patient information
Pro-active methods such as Healthcare Failure Mode and Effects Analysis (HFMEA) can be
used to identify and control critical areas in the process of health care, to help ensure their
safety. Reactive methods such as Root Cause Analysis (or Systems analysis) can also be
utilized to ensure that future adverse events or near-misses are not repeated.
4.3.3 Patient safety
Internationally, patient safety is now recognized as a major concern which requires a specific
management focus. An on-going programme of patient safety improvement should
therefore be in operation. All risks to patient safety should be identified, assessed and
managed, in line with implementing the risk management process set out above.
4.3.4 Occupational safety, health and welfare
All staff-related occupational safety, health and welfare risks should be identified, assessed
and managed, in line with implementing the risk management process set out for
occupational safety, health and welfare. Occupational Safety and Health Act 1994 and
Regulations have stated clearly the responsibility of employers and employees with regard
to safety, health and welfare of workers and workplace. Health care facilities need to comply
with the Act and Regulations. This includes the establishment and function of a Safety and
Health Committee in an organisation which has forty (40) or more workers.
4.3.5 Environmental and fire safety
All environment and fire safety risks should be identified, assessed and managed, in line
with implementing the risk management process set out above. Appropriate systems and
processes should be in place to ensure that environmental and fire risks are minimised
through meeting legislative and mandatory requirements.
4.3.6 Incidents and complaints reporting/recording, analysis and learning
Reporting, recording, analyzing and learning from incidents and complaints are key
components of a successful reactive approach to risk management. All incidents and
complaints should be properly recorded; reported to management; managed in accordance
with an agreed policy; rated according to impact; reviewed (through RCA) where appropriate
to determine contributory factors, root causes and any actions required. Incidents/
complaints should be subjected to periodic aggregate reviews to identify trends and further
opportunities for learning, risk reduction and quality improvement.
4.4 Staffing and staff management
Systems should be in place to ensure appropriate work-force planning, induction, and training and
development for staff appropriate to their roles and responsibilities. Continuing learning and
development programmes aimed at meeting the development needs of staff and the service needs
of the hospital should be in place.
4.5 Service improvement
Notwithstanding the core processes and programmes outlined above, hospitals should ensure that
there is a structured programme in place to support continuous quality improvement across all
services. This requires the identification of quality priorities for the hospital e.g. through the hospital-
02.LayOut 12/3/10 4:55 PM Page 17
18 Achieving Excellence In Clinical Governance
level QA committees; adopting relevant approaches to Quality Improvement; and utilizing
appropriate quality tools to secure demonstrable benefits for patients.
Hospitals should be participate in relevant external Quality Assurance programmes, such the MSQH
Hospital Accreditation Programme, Joint Commission International, ISO, NATA Australia etc., where
available. This will assist them in implementing a comprehensive quality improvement programme
incorporating externally-recognised standards as well as internally-led initiatives.
4.6 Learning and sharing information
It is essential that all hospitals develop a learning culture and that effective learning and sharing
processes are developed to spread good practice and generally educate/inform others. The pursuit
of continuous improvement in quality, safety and risk management is crucially dependent on
learning from experience and on sharing information about good practice. This requires the
establishment and maintenance of effective processes for learning and for sharing good practice in
relation to quality, safety and risk management.
Examples of good practice can be identified by front-line staff or by independent assessors. In some
healthcare organisations, a library of good practice can be found, for example, on the organisations
intranet and this can be shared with other organizations. Some organisations establish regular
learning and sharing fora where staff can bring examples of good practice for discussion.
Newsletters are also a good means of disseminating information for learning and sharing. In
addition, good practice can be shared through third party organisations, e.g. quality accreditation
bodies such as the Malaysian Society for Quality in Health (MSQH).
4.7 Check questions
The table below contains check questions that can be utilized by hospitals to gain an understanding
of their strengths and areas for improvement in relation to the implementation of the core processes
and programmes outlined above. The responses to these questions can either yes, no, partial,
not applicable or dont know. The partial responses are categorized as low, moderate or high.
Where a no or partial response is provided, an action plan or quality improvement plan (QIP)
should be developed to implement any requirements. Where the question number box is shaded,
this denotes that the response requires the combination of information from a number of
departments, service areas, etc. Further information on the assessment process is provided in the
Companion Guide and also with the Electronic Self Assessment Tool.
CORE PROCESSES AND PROGRAMMES : CHECK QUESTIONS
G Clinical effectiveness and audit
1. Is a structured programme, in place to systematically monitor and improve the quality of clinical
care provided across all services?
2. Are arrangements in place to monitor clinical effectiveness activity, including clinical audit?
3. Is the implementation of evidence-based practice through use of recognized standards,
guidelines and protocols promoted?
4. Are information systems being properly exploited to support clinical effectiveness activity?
5. Are clinical audits based on agreed selection criteria (e.g. high risk, cost or volume; serious
concerns arising from adverse events or complaints; new guidelines; local or national priorities; or
patient focus)?
02.LayOut 12/3/10 4:55 PM Page 18
Achieving Excellence In Clinical Governance 19
6. Is there evidence that clinical effectiveness activities result in changes in clinical practice and
improvements in the standards of care
H Service user and Community Involvement
(**Questions are adapted from the Victorian Health Safety and Quality Framework, Australia
1. Is patient/ service user and public feedback (including feedback on actual patient experience)
regularly sought and integrated into quality, safety and risk management improvement activities?
2. Is sufficient information and opportunity provided for patient /service users to meaningfully
participate in their own care?
3. Are patient /service users and the public involved in the development of patient information?
4. Are arrangements in place to train and support patient /service users, staff and the public involved
in the patient and public involvement process?
5. Are patients/service users and the public invited to assist in planning new services?
I Risk management and patient safety
1. Are risks of all kinds systematically identified and assessed?
2. Are risk of all kinds managed in order of priority?
3. Are risk registers used for the purpose of managing and communicating risk at all levels?
4. Are arrangements in place to manage known high priority risk issues?
5. Are staff-related occupational safety, health and welfare risks identified, assessed and managed?
Are arrangements in place to ensure the management of occupational health, safety and welfare?
6. Are environmental and fire safety risks identified, assessed and managed?
Are arrangements in place to ensure that environmental and fire risks are minimized through
meeting legislative and mandatory requirements?
7. Is an on-going programme of patient safety improvement in operation?
8. Are arrangements in place to ensure that medical device alerts/safety notices are circulated to
all relevant staff and are acted on?
9. Are incidents properly recorded and reported to management?
10 Are incidents managed in accordance with an agreed policy?
11. Are incidents rated according to impact and reviewed, where appropriate, to determine
contributory factors, root causes and any actions required?
12. Are incidents subjected to periodic aggregate reviews to identify trends and further opportunities
for learning, quality and safety improvement, and risk reduction?
13. Are complaints, comments and appeals properly recorded and reported to management?
14. Are complaints managed in accordance with an agreed policy?
02.LayOut 12/3/10 4:55 PM Page 19
20 Achieving Excellence In Clinical Governance
15. Are complaints rated according to impact and reviewed, where appropriate, to determine
contributory factors, root cause and any action required?
16. Are complaints and comments subjected to periodic aggregate reviews to identify trends and
further opportunities for learning, quality and safety improvement, risk reduction?
17. Where appropriate, are all claims recorded and analysed to identify opportunities for learning,
quality and safety improvement, and risk reduction?
J Staffing and staff management
1 Are arrangements in place to ensure appropriate workforce planning?
2. Are arrangements in place to ensure appropriate recruitment, induction and training &
development for staff appropriate to their roles and responsibilities?
3. Do the arrangements set out in Questions 1 & 2 to ensure compliance with related Malaysian
employment registration?
4. Are continuing learning and development programmes in place and aimed at meeting the
development needs of staff and services?
5. Are robust pre-employment checks carried out and the requirement set out in this framework?
6. Are arrangements in place to identify and deal with poor professional performance?
K Service Improvement
1. Are quality, safety and risk management goals clear, communicated effectively throughout the
hospital and reflected in relevant service planning processes?
2. Do local quality, safety and risk management plans take account of identified national /
international priorities?
3. Does the hospital participate in relevant external accreditation programmes?
4. Do quality improvement activities utilize a range of quality improvement tools to assist with
assessing and diagnosing issues, identifying remedies and measuring improvement?
L Learning and sharing information
1. Does the hospital routinely learn from patient experience?
2. Does the hospital routinely learn from incidents occurring within the hospital and elsewhere?
3. Does the hospital regularly communicate to patients, staff and other relevant stake-holders
improvements that have been made as a consequence of learning from patient experience and
incidents?
4. Does the hospital share information and learning about serious incidents with other hospitals, the
State Health Department or the Ministry of Health head quarters?
5. Are arrangements in place for learning and for sharing information on good practice in relation to
quality, safety and risk management?
02.LayOut 12/3/10 4:55 PM Page 20
Achieving Excellence In Clinical Governance 21
5. Outcomes
5.1 Key Performance Indicators (KPIs)
The ultimate test of effective systems for quality, safety and risk management is the extent to which
they achieve improvements in outcomes or results for patients, service users and other
stakeholders. Demonstration of improvements in quality, safety and risk management requires the
definition of relevant key performance indicators (KPIs). Hospitals should take a systematic
approach to identifying a range of KPIs relevant to them.
In addition to locally-developed KPIs, all MOH hospitals should monitor their self-assessed
percentage compliance with the integrated quality, safety and risk management framework. This KPI
can be determined by using the electronic self-assessment tool accompanying this document.
Effective management of quality, safety and risk should result in demonstrable improvements in
KPIs. Further information on KPIs is contained in the Companion Guide.
5.2 Check Questions
The table below contains check questions that can be utilised by hospitals to gain an understanding
of their strengths and areas for improvement in relation to achieving the required outcomes from an
integrated quality, safety and risk management system. The responses to these questions can be
either yes, no, partial, not applicable, or dont know. The partial responses are categorized
as low, moderate or high. Where a no or partial response is provided, an action plan or quality
improvement plan (QIP) should be developed to implement any requirements. Where the question
number box is shaded, this denotes that the response to the question may need input from a number
of departments, service areas, etc. Further information on the assessment process is provided in the
Companion Guide and also with the Electronic Self Assessment Tool.
Outcomes: Check questions
M Key Performance Indicators (KPIs)
1. Have local KPIs been developed for quality, safety and risk management?
2. Are the KPIs monitored as part of on-going quality, safety and risk management
improvement activities?
3. Do the KPIs demonstrate that there is on-going improvement in quality, safety and
risk management?
02.LayOut 12/3/10 4:55 PM Page 21
22 Achieving Excellence In Clinical Governance
6. Conclusion
Every health care organisation is responsible and accountable for improving the quality of care provided
and sustaining high standards of care. Adoption of the Clinical Governance Framework will be a useful
guide for healthcare providers to develop and implement the various quality, safety and risk management
systems in the health sector in Malaysia and hopefully, result in excellence in clinical performance as well
as a culture of safety, making the realization of the noble aim of People First, Performance Now a
realisable goal in the near future.
1
Research on Evaluation of Quality Assurance Programme, Institute for Health Systems
Research, 2009
2
The Strategic Plan for Quality in Health, MOH, 1998
3
An Introduction to Quality Assurance in Health Care. Oxford University Press. 2000. The three
components are based on the three components of Avedis Donabedians Structure, Process, Outcome
Model of Quality
02.LayOut 12/3/10 4:55 PM Page 22
Achieving Excellence In Clinical Governance 23
Excellence In Clinical Governance
COMPANION GUIDE
To support self-assessment against the
Framework Document
02.LayOut 12/3/10 4:55 PM Page 23
24 Achieving Excellence In Clinical Governance
1. Introduction
1.1 Background
This Companion Guide provides managers and health care professionals with additional information
to self-assess the compliance of their organisational units with the various check questions
contained in the Framework Document. There is information contained in the Guide for each check
question, including, where appropriate, brief additional guidance, examples of verification and
pointers to web-based and other resources. Service providers are strongly encouraged to submit
their own examples of guidance, verification and resources for sharing with other providers through
updated versions of this Companion Guide.
This Guide is based, in part, on practical insights gained, and feedback obtained whilst undertaking
2 pilots of the draft Framework document for the Health Services Executive (HSE) of Ireland as well
as the MOH workshops on Clinical Governance in 2008 and 2009. Based on the feedback obtained,
the following comprise potential benefits of implementing the quality, safety and risk management
framework:
structure & standardisation nationally
inefficiencies & adverse events identified & addressed
provides a framework for planning services and prioritising resources
enables clear understanding of accountability & responsibility
provides a structure to share good practice
can help improve patient safety
The feedback also provided a list of potential concerns that need to be addressed, which can
jeopardise the successful implementation of the framework, including:
Will this be just a paper exercise?
Visibility of risk but no resources to correct
Increased workload, with no extra resources
Finger-pointingfear of the blame game
How to ensure buy-in at all levels?
Current climate poor staff morale
How do we get senior medical staff involved?
In the current climate, it is fully appreciated that there will be challenges for some in fully
implementing this framework a journey that may take 3-5 years. Consequently, a key concern
during self-assessment and implementation is that, wherever possible, providers who identify what
they believe to be examples of good practice in quality, safety and risk management within their own
organisations should share these with other provider units for learning and improvement purposes.
As Scally and Donaldson proposed for the National Health Service in England, it should be possible
to spread good practice in order to help others improve and, in so doing, shift the mean of quality
performance across all aspects of service provision (Figure 1).
Figure 1 Spreading good practice and shifting the mean quality performance
02.LayOut 12/3/10 4:55 PM Page 24
Achieving Excellence In Clinical Governance 25
Note that the examples of verification provided in this document should not be considered as THE
check-list for compliance or as an exhaustive list of examples. It is recommended that you draw up
your own check-list (of verification criteria), based on this guidance, to suit your own local context.
It is hoped that verification criteria and other information can be shared, for the benefit of all service
providers. In the spirit of continuous improvement, verification criteria contained within this
Companion Guide will be updated based on feedback received.
It should also be noted that whilst this Guide aims to provide additional information to managers and
clinicians in support of their self-assessment exercise against the Framework Document, it cannot
replace obtaining access to expert advice and assistance on quality, safety and risk management
matters.Just as in medicine, there is much in the field of healthcare quality, safety and risk
management that is necessarily subjective and dependent on local factors. This Companion Guide
should be updated regularly in response to suggestions and identified good practices across
Malaysian providers after they have conducted self-assessment studies against the Framework
Document.
1.2 Performing a self-assessment against the Framework
The Framework Document and the Companion Guide, taken together, are tools to help promote
change and build a culture of quality, safety and risk management across Malaysian health care
providers. With reference to this document and the main Framework Document, managers and
clinicians should undertake a reasonable (but not complete) assessment of the extent to which a
suitable framework is in place within their hospital or service. A total of 69 check questions relating
to key aspects of the framework are contained in this document. They are not exhaustive i.e. there
can be other questions that are relevant but have not beent included in the list of 69 check questions.
Responses to these questions can either be:
YES, NO, PARTIAL (low, moderate or high), NOT APPLICABLE or DONT KNOW.
Where a no, partial or dont know response is provided, either an action plan or Quality
Improvement Plan (QIP) should be developed to address these shortfalls. Proper monitoring and
review of the action plans and/or QIPs will ensure that actions are carried out, leading ultimately to
better outcomes for patients and their significant others.
The initial, or baseline assessment should represent an honest and searching analysis of the provider
organisations strengths and areas for improvement in relation to arrangements in place for quality,
safety and risk management. At all times, when considering the check questions, those doing the
assessment should consider carefully the extent to which arrangements are in place and working
effectively. This Companion Guide can assist in this regard. In addition, an electronic assessment
tool is provided to enable self-assessment to be carried out in relation to the check questions, and
this is outlined below. In preparing the baseline assessment, it is important to bring together all key
individuals who can contribute to the assessment process. They should be familiar with the
Framework Document and have an understanding of the kinds of information that will be required to
complete the assessment. Given the right people and suitable preparation, a reasonable baseline
assessment can be produced within a fairly short space of time.
During this time, the individuals participating in the process will, as a group:
1. Briefly review each check question and provide a consensus view of the level of compliance
across the organisation. Give a Dont know response if they cannot answer the question.
2. Identify any particular strengths in relation to the question which could lead to examples of
good practice that could be shared with others. Detailed information on these can always be
gathered as part of a subsequent exercise.
3. Identify weaknesses that they may have in relation to the question that will lead to an action
plan or Quality Improvement Plan (QIP). Again, detailed information on these can always be
gathered as part of a subsequent exercise.
02.LayOut 12/3/10 4:55 PM Page 25
26 Achieving Excellence In Clinical Governance
The assessment should draw, where appropriate, on the results of independent audits and the
perspectives of a range of stakeholders. It is recognised that there are aspects to the questions
contained in this document that are subjective and depend on managers detailed knowledge of their
local context together with an understanding of quality, safety and risk management.
Note that the issue here is NOT about how much your organisation scores in terms of compliance
to the Framework. What is important is that action is taken to rectify weaknesses in quality, safety
and risk management and, over time, there is improvement in compliance against the framework as
demonstrated by improvements in compliance scores. Healthcare quality, safety and risk
management are in a constant state of flux and standards are improving all the time. Thus, even
when a Yes response is given for any check question, which indicates, essentially, 100%
compliance in relation to the issue addressed by the question, this does not mean that we should be
complacent and not try to improve further. This is because, this years 100% compliance might, next
year, be rather less than 100%. The emphasis is on continual improvement.
1.3 Electronic self-assessment tool
An electronic self-assessment tool containing the check questions is available, which can be used
to determine compliance scores as key indicators of performance against the questions and the
overall framework for quality, safety and risk management.
1.3.1 Running the tool
Double-click on QSRMFrameworkScoring_V1.3_Feb_2009 to run the tool, which is an
Excel spreadsheet. You will see the following introductory screen (Figure 2), which
contains basic instructions on how to operate the tool. Note that there are several
worksheets listed at the bottom covering data entry, good practice, actions or QIPs,
aggregation and analysis. These are outlined in more detail below:
Figure 2 Introductory screen
1.3.2. Entering data
Click on the DATA ENTRY worksheet tab at the bottom of the screen. The following
screen appears:
3
A demonstration version of the spreadsheet tool is also provided, which is pre-populated with responses to the various questions so that you can get a
feel for the analytical capabilities of the tool. The demonstration version is named QSRMFrameworkScoring_V1.3_Feb_2009_DEMO. Some of the
screenshots in this document are taken from the demonstration version of the electronic self-assessment tool.
02.LayOut 12/3/10 4:55 PM Page 26
Achieving Excellence In Clinical Governance 27
Figure 3 Data entry screen
The check questions outlined in the quality, safety and risk management framework document have
been entered for scoring and analysis purposes. Each question is assigned a Level, which is:
1 (whether the question relates to underpinning requirements) or
2 (whether the question relates to core processes) or
3 (whether the question relates to outcomes)
Run your mouse cursor over the Question boxes with a small red triangle in the top right corner to
reveal each question. You can enter a response, in the form of the number 1, against each question.
In terms of scoring, there are five possible question responses : yes, high partial (HP), moderate
partial (MP), low partial (LP) and no. The tool automatically assigns the following scores to your
response: Yes=100%, H=80%, M=50%, L=20% and No=0%.
One way to think about a high partial response is consider it a yes, but.. i.e. you meet many of
the requirements of the question, but are not quite there yet. Similarly, a low partial can be thought
of as a no, but.. i.e. there is little in place but you can point to evidence of some aspects of
compliance.
You must enter ONE response for each question. This can include a not applicable (N/A) or a dont
know (D/K) response.
If the CHECK box is green, then you HAVE entered a response.
If the CHECK box is white, you have NOT entered a response.
If the CHECK box is red, you have entered too many responses. Make sure you enter ONLY ONE
response!
If the ACTION box is coloured red, this flags up that you have not scored 100% on the question
and, therefore, action(s) or a Quality Improvement Plan (QIP) may be needed.
The COUNT line simply counts the number of each type of response and this is then converted to
a Percentage response immediately below. Thus you can immediately get a feel for the response
profile in relation to the questions comprising the element.
02.LayOut 12/3/10 4:55 PM Page 27
28 Achieving Excellence In Clinical Governance
1.3.3 Recording good practice
Click on the GOOD PRACTICE worksheet tab. The following screen appears:
Figure 4 Good practice screen
The GOOD PRACTICE worksheet allows you to build a simple list of what you consider
to be good practices in your organisation. These will be determined from the strengths
you identify as part of your self-assessment against the framework. You can then share
this information, and your scoring information, with other organisations to build a
learning, sharing and benchmarking culture. Over time, this will help you improve quality
and safety and reduce risk.
1.3.4 Recording actions or Quality Improvement Plans (QIPs)
Click on the ACTIONS or QIPs worksheet tab. The following screen appears.
The ELEMENT SCORE (%) gives the overall score for the element, taking account of any not
applicable questions.
Note that scores are based on professional judgment made in relation to responding to the various
questions in the DATA ENTRY worksheet. Scoring is relative and not absolute. The objective is to
provide a profile, not to suggest precision.
Figure 5 Actions or quality improvement plans screen
02.LayOut 12/3/10 4:55 PM Page 28
Achieving Excellence In Clinical Governance 29
You can type in the relevant details under the various headings to build a comprehensive
action plan in relation to compliance with the quality, safety and risk management
framework. Alternatively, you can use your own local action planning approach.
1.3.5 Aggregating data across departments, service areas, etc.
Should you need to aggregate data for individual questions across departments, service
areas, etc. to establish an overall response to a question, click on the AGGREGATION
worksheet. You will see the following screen:
Figure 6 Aggregation matrix screen
The quality, safety and risk management framework set out in the framework document is applicable
at an organisational level. An organisation is defined as a collection of services, departments
and/or functions under the actual or assumed overall direction and control of a senior management
team or governing body. In practical terms, this definition is intended to cover public and private
hospitals and other health care organisations in Malaysia. There are a range of services, departments
and/or functions that aggregate up to provide a picture of the whole organisation. In a hospital you
would have various departments or services such as Accident and Emergency, Cardiology, General
Surgery, Paediatrics, Radiology, and so on. Similarly, in a Public Health Department of the MOH,
you would have various services such as primary care services, family health etc.
Many of the framework check questions may require aggregation across the organisation to
determine the overall question response (i.e. yes, high partial, moderate partial, low partial or no).
With reference to the questions contained within the Framework Document, and reiterated in this
Companion Guide, a SHADED QUESTION NUMBER BOX INDICATES THAT THE QUESTION
REQUIRES POSSIBLE AGGREGATION ACROSS THE ORGANISATION. It is up to senior
organisational managers to collect and collate, where appropriate, sufficient information at lower
levels within the organisation in order that a judgement can be made about the level of
organisational compliance with each framework check question.
As an example, consider question A.3 - Is there effective communication and consultation with
internal stakeholders in relation to the purpose, objectives and working arrangements for quality,
safety and risk management? Here you would ensure that all internal (i.e. within the organisation)
stakeholders had been identified (from question A.1) and that there was documented evidence of
communication and consultation on purpose, objectives and working arrangements for quality,
safety and risk management with each service and other stakeholder groups (e.g. finance
department, infection control, etc.). In looking at the evidence, ask yourself the question Does
02.LayOut 12/3/10 4:55 PM Page 29
30 Achieving Excellence In Clinical Governance
communication and consultation appear to be working effectively? You might have to ask specific
questions of a number of people representing different internal stakeholder groups in order to gain
a better picture of communication and consultation effectiveness. In doing this work, you might
deduce that there appears to be evidence of compliance in around half of all services/ departments,
and limited or no compliance in the remainder. Given the compliance rating options of no, low
partial, moderate partial, high partial and full compliance, you would select moderate partial as your
level of compliance and produce an action plan accordingly.
It is helpful to produce a matrix of relevant questions against various services, departments, etc.
so that you can identify compliance, using the yes, high partial, moderate partial, low partial and
no response approach, for each relevant question against each service. Figure 7 shows a simple
illustrative example using the aggregation matrix contained in the Electronic Self-Assessment Tool.
It can be seen that for each of the departments listed a numerical response has been provided for
each question that identifies the degree of compliance with the question within the department. This
numerical response is based on the Yes=100%, H=80%, M=50%, L=20% and No=0%approach, i.e.
100 is entered for a Yes response, 80 for a high partial response, and so on. When the response data
has been entered for each department/question combination, the overall question response (Yes, HP,
MP, LP, or No) is presented at the bottom of the matrix. This is used to determine the overall
response to the question on the DATA ENTRY worksheet (see section 1.3.2, above).
Figure 7 Specimen aggregation matrix
1.3.6 Analysing the data
Click on the ANALYSIS worksheet tab, a screen similar to Figure 8, overleaf, appears (this
particular screen shows that some data has been entered). This shows a table containing a
summary of responses to the questions in each element of the framework, together with the
element scores.
If you scroll down the worksheet you will find three graphical analysis presentations. Figure 9
overleaf shows a bar chart containing element scores. Figure 10 shows a pie chart containing
a breakdown of responses to self-assessment questions. Figure 11 shows a bar chart
containing a Level analysis depicting summary scores for underpinning requirements (level
1), core processes and programmes (level 2) and outcomes (level 3).
You can highlight and copy any of the above analysis options using standard Windows (TM)
copy facilities and paste them into, for example, a WORD document for reporting purposes.
You can also print them directly from the Electronic Self-Assessment Tool to a printer.
02.LayOut 12/3/10 4:55 PM Page 30
Achieving Excellence In Clinical Governance 31
Figure 8 Analysis: Table of element scores
Figure 9 Analysis: Bar chart showing element scores (%)
02.LayOut 12/3/10 4:55 PM Page 31
32 Achieving Excellence In Clinical Governance
Figure 10 Analysis: Breakdown of responses to self-assessment questions
Figure 11 Analysis: Level analysis depicting score for underpinning requirements (level 1),
core processes and programmes (level 2) and outcomes (level 3)
02.LayOut 12/3/10 4:55 PM Page 32
Achieving Excellence In Clinical Governance 33
1.4 Beyond self-assessment I - Improving quality, safety and risk management using the Plan-Do-
Study-Act (PDSA) improvement model
The PDSA improvement model (Figure 12) is widely used in healthcare internationally and can be
usefully applied in the context of the Quality, Safety and Risk Management Framework to help
identify, implement and evaluate improvements. Further information on the practical application of
the PDSA model in healthcare can be found on the website of the Institute for Healthcare
Improvement (IHI) at www.ihi.org/IHI/Topics/ImprovementMethod/HowToImprove/
Figure 12 The PDSA model
1.5 Beyond self-assessment II - Improving quality, safety and risk management using the HSE
Change Model
A very useful publication titled Improving Our Services A Users Guide to Managing Change in the
Health Service Executive was recently produced by the HSE of Ireland and it sets out a
comprehensive change model for improving services based on extensive research (Figure 13).
A summary of the guide can be downloaded at:
www.hse.ie/eng/Publications/Human_Resources/Improving_Our_Services_Summary.pdf
The full guide can be downloaded at:
www.hse.ie/eng/Publications/Human_Resources/Improving_Our _Services.pdf
02.LayOut 12/3/10 4:55 PM Page 33
34 Achieving Excellence In Clinical Governance
Figure 13 The HSE Change Model
02.LayOut 12/3/10 4:55 PM Page 34
Achieving Excellence In Clinical Governance 35
2. Essential underpinning requirements (Donabedians Structure)
A COMMUNICATION AND CONSULTATION WITH KEY STAKE-HOLDERS with regard to goals
and objectives for safety
NB Shaded number box indicates question requires possible aggregation across the
organisation.
1. Has a stakeholder analysis been carried out to identify all internal and external stakeholders
relating to quality, safety and risk management?
GUIDANCE
A stakeholder analysis should be conducted to ensure that:
all appropriate internal and external stakeholders have been identified and
appropriate mechanisms have been defined for communicating and consulting with the
various stakeholders or stakeholder groups (see questions A4 and A5).
A formal stakeholder analysis may not be necessary if there is sufficient evidence that there is a clear
understanding of who the key stakeholders are. Stakeholders are likely to have been identified in a
range of documentation (See below). However, it is considered good practice to undertake and
properly document a formal stakeholder analysis. A specimen stakeholder analysis (for illustration
only) is given below.
Specimen Stakeholder Analysis (Illustrative only)
EXAMPLES OF VERIFICATION
Stakeholder analysis documentation
Strategic framework document
Risk management strategy
Public engagement strategy
HR strategy
Training needs analysis
Staff survey
Patient survey
Stakeholder
Internal/
External
Communication/ Consultation
Strategies
Frequency
Staff INTERNAL Staff handbook Annually
Annual report Annually
Induction programme Monthly
Newsletter Quarterly
Communications boards Weekly
Staff survey Bi-annually
Internet-based podcast Quarterly
etc. etc.
Patients/ EXTERNAL Annual report Annually
Services Users Focus groups Ad-hoc
Patient/Service User survey Annually
Newspaper/magazine Quarterly
Conferences Annually
etc. Ad hoc
Consumer EXTERNAL Annual report Annually
Association / Focus groups Ad-hoc
Patient Survey Annually
representative Conferences Annually
organisations
02.LayOut 12/3/10 4:55 PM Page 35
36 Achieving Excellence In Clinical Governance
2. Are arrangements in place to ensure that the stakeholder analysis is maintained up-to-date?
GUIDANCE: In the case of a formal stakeholder analysis, there should be a documented policy
outlining arrangements both for conducting the analysis and for ensuring that the analysis is
maintained up-to-date. There may be a committee or group that has responsibility for maintaining
the stakeholder analysis up-to-date. Check that the analysis is indeed maintained up-to-date by
reference to dated updates of the stakeholder analysis.
EXAMPLES OF VERIFICATION:
Relevant policy
3. Is there effective communication and consultation with internal stakeholders in relation to the
purpose, objectives and working arrangements for quality, safety and risk management?
GUIDANCE: The test of an effective communication and consultation mechanism is does it work
and, as such, services should aim to provide clear evidence of effectiveness. Internal stakeholders
will include, for example, staff, committees, groups, departments, etc. Check firstly that there is
communication/ consultation with all internal stakeholders, and secondly that such communication/
consultation can be considered to be effective. Do all internal stakeholders have a clear
understanding of the purpose, objectives and working arrangements for quality, safety and risk
management?
EXAMPLES OF VERIFICATION
Stakeholder surveys
Apparent impact of communication strategies on key performance indicators
4. Are internal and (where appropriate) external stakeholders kept fully informed of progress in
achieving objectives for quality, safety and risk management?
GUIDANCE: Stake-holder engagement in quality, safety and risk management is extremely
important. One means of keeping stakeholders engaged is to keep them informed on progress to
achieve objectives. The means of keeping external stake-holders informed should be as set out in
the stakeholder analysis (see question 1, above). Note that the only requirement here is to
demonstrate that internal and, where appropriate. external stakeholders are kept fully informed of
progress. There is no requirement to test the effectiveness of the communication processes that
keep stakeholders fully informed. It is assumed that if the information is properly communicated,
then stake-holders will be informed. You should check that information on progress to achieve
objectives is being properly communicated to all relevant stakeholders.
EXAMPLES OF VERIFICATION:
Stakeholder communication logs
5. Is there effective communication and consultation with external stakeholders in relation to
quality, safety and risk management?
GUIDANCE: As identified above, the test of an effective communication and consultation
mechanism is does it work and, as such, services should aim to provide clear evidence of
effectiveness. Check firstly that there is communication/ consultation with relevant external
stakeholders, and secondly that such communication/ consultation can be considered to be
effective.
EXAMPLES OF VERIFICATION
Stakeholder surveys
02.LayOut 12/3/10 4:55 PM Page 36
Achieving Excellence In Clinical Governance 37
B CLEAR ACCOUNTABILITY ARRANGEMENTS (Roles & Responsibilities)
NB Shaded number box indicates question requires possible aggregation across the organisation.
1. Are clearly documented accountability arrangements in place to support the hospital director to
discharge his/her responsibility for quality, safety and risk management?
GUIDANCE: There should be an organisation chart or organogram and, possibly, an accountability
framework document that describes the accountability arrangements for quality, safety and risk
management. In most instances the arrangements will be hierarchical with structures in place that
lead up to the senior accountable manager (e.g. hospital director, etc.).
This guide does not presume to know the best arrangements for any particular service provider. The
maxim What matters is what works should be followed. In a hierarchical accountability framework
there will be a hierarchy of job functions and committees or groups leading up to the senior
accountable manager. The organisational chart might identify, for example, and in no particular
order:
Quality/ Occupational Health and Safety Officer/QA nurse/Audit Committee/Radiation
Safety Committee
Quality Assurance Committee/Clinical Audit Committee, etc.
For all job positions, there should be clearly-documented job descriptions and reporting
arrangements. All committees and groups should have clear terms of reference and reporting
arrangements.
EXAMPLES OF VERIFICATION
Organogram/ Job descriptions & Committee/Group terms of reference/ Quality
strategy/KPI
RESOURCES
www.worcestershirehealth.nhs.uk/SWPTC_Library/Policies_and_Procedures/Risk_
Management/Risk%20Management%20strategy.pdf
2. Do the documented accountability arrangements ensure that that the hospital director is fully
informed in relation to key areas of quality, safety and risk performance?
GUIDANCE: The arrangements should cover all areas of quality, safety and risk management deemed
crucial or key by the Organisation/ service provider. For example, if radiation protection is a
consideration for the organisation,then there will most likely be a radiation safety committee
(however named). It is important to be clear about the range of performance information that will be
required by the senior accountable manager to provide assurance that quality, safety and risk
performance is being properly managed. Expert advice from individuals and/or functions with expert
knowledge of quality, safety and risk management is essential. Check that the
accountabilityarrangements cover all key areas and are capable of keeping the senior accountable
manager fully informed in relation to key areas of quality, safety and risk performance.
EXAMPLES OF VERIFICATION: See 1 above
3. Within the accountability arrangements are the roles and responsibilities played by any
committees or groups clearly described ?
GUIDANCE: Check all relevant documentation for clear descriptions of the roles and responsibilities
for committees or groups.
EXAMPLES OF VERIFICATION: See 1 above
02.LayOut 12/3/10 4:55 PM Page 37
38 Achieving Excellence In Clinical Governance
4. Do committee structures and reporting arrangements provide for coordination and integration
of quality, safety and risk activities and priorities?
GUIDANCE: This will most likely involve a judgement call. Quality, safety and risk management
activitie should be co-ordinated and priorities should be set across the board, and not in silos.
How do the structures and reporting arrangements provide for coordination and integration? Is there
evidence that an integrated approach to quality, safety and risk is being taken? Further, is there
evidence that priorities are being set across the board?
EXAMPLES OF VERIFICATION: See 1 above
02.LayOut 12/3/10 4:55 PM Page 38
Achieving Excellence In Clinical Governance 39
C ADEQUATE CAPACITY AND CAPABILITY
1. Do managers and clinicians at all levels demonstrate commitment to the management of quality,
safety and risk?
GUIDANCE: Quality & safety is everybodys business. Managers at all levels must lead by example.
They should demonstrate their commitment by ensuring these matters are considered high priority
in everything the organisation does. Thus, quality, safety and risk management matters might be
standing agenda items at various regular management meetings and senior managers perform
regular quality & safety walk-arounds. Managers who attend relevant education and training events,
get involved in complaints and incidents investigations and set aside specific budget to address
quality, safety and risk management goals (see question 3. below) may also be seen to be
demonstrating commitment.
EXAMPLES OF VERIFICATION: Minutes of relevant committee meetings/ Notes associated with
walkarounds, etc. showing evidence of managerial engagement/ Evidence of managers attendance
at educational and training events, e.g. Root Cause Analysis/ Evidence of managers involvement in
complaints and incident investigations
2. Do service planning and other business planning arrangements take into account the hospitals
quality, safety and risk management goals and priorities when developing budgets and other
financial strategies?
GUIDANCE: Look for documented evidence, in meeting minutes, etc., that service planning and other
business planning arrangements take account of quality, safety and risk management goals when
developing budgets and other financial strategies.
EXAMPLES OF VERIFICATION: Minutes of meetings of relevant committees or groups.
3. Is a specified portion of the organisations annual budget committed to achieving defined goals
for quality, safety and risk management?
GUIDANCE: Often, financial resources need to be allocated for quality & safety goals to be achieved.
Look to see whether senior management has set aside specific financial resources for achieving
defined quality, safety and risk management goals. For example, there may be specific quality, safety
or risk management initiatives that have been allocated funding, including education and training.
EXAMPLES OF VERIFICATION: Minutes of relevant meetings/ Details of budgets, including
education/ training.
4. Is there access to appropriate resources to implement effective quality, safety and risk
management systems, e.g. qualified people, physical and financial resources, access to
specialist expertise, etc.?
GUIDANCE: The resources that are provided to deal with quality and risk management need to be
realistic, i.e. in line with issues such as the organisations risk profile. Financial resources is partly
dealt with in question 3, above, and can be a thorny issue. Service providers need to view
investments in quality, safety and risk management as adding value to service provision, rather than
simply being a drain on financial resources. There is increasing evidence in healthcare that investing
in quality, safety and risk management can save money in the longer term through reduction in waste
and improvements inefficiency.
What is potentially more challenging to assess is the extent to which an organisation has access to
appropriate staffing resources for quality, safety and risk management. Larger hospital organisations
might have an entire department or function dedicated to quality, safety and risk management with
sufficient qualified and trained staff.
02.LayOut 12/3/10 4:55 PM Page 39
40 Achieving Excellence In Clinical Governance
As part of the self-assessment against this question, organisations might identify all staff and other
resources they have available to deal with quality, safety and risk management matters. This might
include qualified quality, safety and/or risk management advisors, front-line leads for quality, safety
and/or risk management, etc. It might also include managers and clinicians who have undertaken
any form of education and training in relation to quality, safety and/or risk management. A resource
matrix can then be produced setting out all resources available at different levels. Guidance should
then be sought from an experienced adviser as to whether overall resources are appropriate to
implement effective quality, safety and risk management systems.
EXAMPLES OF VERIFICATION: Resource matrix
5. Are there structured training programmes to ensure that all staff are provided with adequate
quality, safety and risk management information, instruction and training appropriate to their
role?
GUIDANCE: All staff will need some form of quality, safety and risk management training but only
as appropriate to their role. For some staff, all of their information, instruction and training
requirements will be satisfied in relation to induction and on-going training processes. Other staff
may require additional information, instruction and training. The difference between instruction and
training can sometimes be debatable. For practical purposes, instruction relates to showing
somebody how to carry out a practical activity, whereas training is regarded as a more formal
process that includes theory as well as practice.
One way of assessing compliance with this question is for organisations to conduct an overall
information, instruction and training needs analysis. Many organisations will already be familiar with
conducting a training needs analysis. Such an analysis should be informed by the organisations risk
profile (see Element I, below).
When thinking through provision of instruction and training, as well as considering induction and
on-going training provision, think whether you have other events going on, or have access to e.g.
local quality, safety or risk management workshops; seminars; conferences; specialist in-house
training. Think also about your policies, procedures and guidelines, staff booklets and other
published information in relation to whether staff have adequate information.
EXAMPLES OF VERIFICATION
Documented analysis of information, instruction and training needs
Documented assessment of whether needs have been, or are being met
Training records of staff
Events log (conferences, seminars, etc.)
Information publications for staff.
02.LayOut 12/3/10 4:55 PM Page 40
Achieving Excellence In Clinical Governance 41
D. STANDARDISED POLICIES, PROCEDURES, PROTOCOLS AND GUIDELINES
NB Shaded number box indicates question requires possible aggregation across the organisation.
1. Does the organisation operate a standardised document control process for all policies,
procedures, protocols and guidelines?
GUIDANCE: Health and social care organisations typically have large numbers of policies,
procedures, protocols and guidelines, A medium-sized hospital, for example, can have several
hundred policy documents alone. Likewise, the combined service providers making up a District
could have several hundred policies. Thus, control of these documents in terms of issuing them and
maintaining them up-to-date can pose a major challenge. It is therefore necessary to ensure that the
organisation operates a standardised document control process. The document control process
could be manually implemented or, ideally, will be computer-based.
EXAMPLES OF VERIFICATION: Document control policy/ procedure
2. Are arrangements in place to train staff in appraising and developing policies, procedures,
protocols and guidelines and identifying evidence-based best practice?
GUIDANCE: Specific training should be provided to relevant staff in relation to developing policies,
procedures and guidelines and identifying evidence-based best practice. Such training may be
provided in-house or may be externally sourced e.g. from the Health Technology Assessment Unit
of the MOH.
EXAMPLES OF VERIFICATION: Policy on policies/ Staff training records
RESOURCES:
The following article from New Zealand provides a useful introduction to clinical
guidelines and evidence-based medicine: www.nzgg.org.nz/download/files/Didsbury_Oct03
3. Are policies, procedures, protocols and guidelines standardised throughout the organisation
and, where appropriate, are they evidence-based?
GUIDANCE: This question is a check to ensure all policies are standardised and are evidence-based.
If in doubt, randomly sample policies to confirm.
EXAMPLES OF VERIFICATION: Random sampling of policies to ensure compliance.
4. Are arrangements in place to ensure that where new services are being established, the
development of policies, procedures, protocols and guidelines is considered at the time of
commissioning?
GUIDANCE: This question is a check to ensure that the need for developing policies etc. when
developing new services is not overlooked.
EXAMPLES OF VERIFICATION
Check service development plans and actions taken to develop policies, etc.
02.LayOut 12/3/10 4:55 PM Page 41
42 Achieving Excellence In Clinical Governance
E. MONITORING AND REVIEW ARRANGEMENTS
NB Shaded number box indicates question requires possible aggregation across the organisation.
1. Are all aspects of the framework described in this document regularly monitored and reviewed
in order that management can learn from any weaknesses in the systems and make
improvements where necessary?
GUIDANCE: Each aspect of the quality, safety and risk management system described by the
Framework Document should be periodically monitored and reviewed by local management at least
on an annual basis. This involves monitoring and reviewing, either separately or together, the
following matters relating to effective quality, safety and risk management:
Communication and consultation with key stakeholders
Clear accountability arrangements
Adequate capacity and capability
Standardised policies, procedure and guidelines
Monitoring and review arrangements
Assurance arrangements
Clinical effectiveness and audit
Patient and public involvement
Risk management and patient safety
Staffing and staff management
Service improvement
Learning and sharing information
Key Performance Indicators (KPIs)
As part of the review process, any identified weaknesses in any aspect of the framework should
be rectified.
EXAMPLES OF VERIFICATION: Relevant meeting minutes that highlight reviews carried out and
any actions required/taken; Relevant review reports
2. Are the results of independent and other audits used to improve hospitals quality, safety and
risk management systems?
GUIDANCE: For the purpose of this question, the term audit is widely defined to encompass all
types of review leading to a report on the strengths and weaknesses in the systems in place for
quality, safety and risk management. To be considered independent an audit must be carried out by
an individual, function or organisation that is not directly associated with the service provider. For
example, independent audits might be carried out by the Malaysian Society for Quality in Health
(MSQH), Joint Commission International (JCI) or ISO.
EXAMPLES OF VERIFICATION
Action plans showing improvement actions linked to audits, reports, etc.
Minutes of relevant meetings
KPIs demonstrating performance improvement(s) linked to improvements in the systems
for quality, safety and risk management
3. Are key performance indicators reviewed regularly to identify and correct shortfalls to drive
continuous improvement in quality, safety and risk management?
GUIDANCE: See also guidance associated with questions M.1 M.3, below. KPIs can be tracked
over time to determine anomalies, which can be investigated to determine whether system
improvements need to be made. For example, the figure overleaf shows a trend for adverse events,
i.e. incidents involving harm to patients, for a hospital in the UK for a whole year (1996). The
doubling in the number of reported adverse events around August/ September can be clearly seen.
This anomaly was subjected to a root cause analysis and it was found to be caused by management
02.LayOut 12/3/10 4:55 PM Page 42
Achieving Excellence In Clinical Governance 43
weaknesses around the handling of new junior doctors. The junior doctors would come in to the
hospital at this time while many of the senior staff doctors were on summer holidays. With the lack
of clinical supervision, junior doctors would be allowed to literally do their own thing. The result was
an increase in the number of reported incidents involving harm to patients.
EXAMPLES OF VERIFICATION
Action plans showing improvement actions
Minutes of relevant meetings
Reports from Professional bodies
Reports from external audit
Reports from multi-professional audit
RESOURCES
The Institue for Healthcare Improvement in the USA has an excellent range of resources
available freely to help healthcare organisations improve through tracking key performance
indicators. See www.ihi.org/IHI/Topics/Improvement/
02.LayOut 12/3/10 4:55 PM Page 43
44 Achieving Excellence In Clinical Governance
F. ASSURANCE ARRANGEMENTS
NB Shaded number box indicates question requires possible aggregation across the organisation.
1. Do the hospital director and senior management receive sufficient assurance on the systems in
place for quality, safety and risk management?
GUIDANCE: The determination of what constitutes sufficient is a judgment call by those carrying
out the self-assessment, assisted where necessary by those with specialist quality, safety and/or risk
management knowledge and expertise.
One approach to determining sufficiency of assurance is to construct a matrix of all actual sources
of assurance available from within and outside the organisation and determine, based on the
organisations risk profile, whether it is felt that sufficient assurance exists, or whether there are gaps
in assurance. The table below gives an illustrative matrix. The question that needs to be continually
asked is Given the nature and extent of assurances available to me, do I feel assured that effective
systems are in place for quality, safety and risk management?
SPECIMEN ASSURANCE MATRIX (ILLUSTRATIVE)
KEY RISK (From Risk Register) Source of Assurance
Internal/
External
EXAMPLES OF VERIFICATION
Internal audit reports
Clinical audit reports
Management reports
Minutes of the committee(s) responsible for overseeing quality, safety and risk management
e.g. QA committee of a hospital
2. Do the assurances received by senior management form an integral part of their on-going
monitoring and review processes?
GUIDANCE: See also question E.2, which is related (although it deals with general management
rather than, necessarily, senior management). What evidence is there that senior management
utilise the assurances they are provided with on quality, safety and risk management issues as part
of their own (i.e. senior management) monitoring and review of the overall organiastion?
EXAMPLES OF VERIFICATION
Minutes of relevant meetings
Reports to the MOH
Infection control Policies and Procedures on Infection Internal
Control MOH Malaysia, 2010
Information management Internal Audit report on compliance
with information management standards Internal
02.LayOut 12/3/10 4:55 PM Page 44
Achieving Excellence In Clinical Governance 45
3. Core processes and programmes (Donabedians Process)
G. CLINICAL EFFECTIVENESS AND AUDIT
NB Shaded number box indicates question requires possible aggregation across the organisation.
1. Is a structured programme in place to systematically monitor and improve the quality of clinical
care provided across all services?
GUIDANCE: The Framework Document states A structured programme, or programmes, should be
in place to systematically monitor and improve the quality of clinical care provided across all
services. This should include, systems to monitor clinical effectiveness activity (including clinical
audit); mechanisms to assess and implement relevant clinical guidelines; systems to disseminate
relevant information; and use of supporting information systems.
The clinical effectiveness cycle, which includes clinical audit, is presented in the figure below:
Access to evidence-based
knowledge base
Evidence-based Practice
Critical Appraisal
National Standards and
Guidelines
CUSUM
Clinical Care Pathways
Clinical Guidelines
Quality Improvement
Change Management
Project Management
Care Bundles
Clinical Audit
KPIs
NIA, HSA
02.LayOut 12/3/10 4:55 PM Page 45
Stage 1
Planning for audit
Plan
Do
Check
Act
Stage 2
Criteria/Standard selection
Stage 3
Measuring performance
Stage 4
Making improvements
Stage 5
Sustaining improvements
46 Achieving Excellence In Clinical Governance
G. CLINICAL EFFECTIVENESS AND AUDIT
NB Shaded number box indicates question requires possible aggregation across the organisation.
The clinical audit process is presented below. This figure is reproduced from Building a Culture of
Patient Safety see Resources section, below. The figure is adapted from guidance on Principles for
Best Practice in Clinical Audit published by the National Institute for Health and Clinical Excellence
in the UK (NICE) again, see Resources section, below.
The key requirement under this question is to check whether these is a structured programe, or
programmes, in place to systematically monitor and improve the quality of clinical care provided
across all services. The programme, or programmes, should be based around clinical effectivenesss
and clinical audit approaches, as briefly outlined in the figures above, and set out in detail in the
Resources listed below, The Department of Health & Children publication Building a Culture of
Patient Safety provides a particularly good introduction to clinical effectiveness and clinical audit in
chapter 7. The NICE guidance Principles for Best Practice in Clinical Audit explores clinical audit in
detail.
EXAMPLES OF VERIFICATION
Programme documentation
Relevant policy/ procedure
Minutes of relevant meetings (e.g. clinical effectiveness or clinical audit committee
meetings)
Action/ Improvement plans
RESOURCES
Department of Health & Children (2008). Building a Culture of Patient Safety. Report of
the Commission on Patient Safety and Quality Assurance
NICE (2002). Principles for best practice in clinical audit. Free download at:
www.nice.org.uk/media/796/23/BestPractiseClinicalAudit.pdf
02.LayOut 12/3/10 4:55 PM Page 46
Achieving Excellence In Clinical Governance 47
2. Are arrangements in place to monitor clinical effectiveness activity, including clinical audit?
GUIDANCE: This question provides a check on the monitoring aspect of question G.1, above. Are
arrangements in place to monitor clincial effectiveness activity, including clinical audit? Are they
sufficient? Do they work? Does the programme (or programmes) in place to improve the quality of
clinical care provided across all services actually work? Are demonstrable improvements in clinical
care being made as a consequence?
EXAMPLES OF VERIFICATION
Relevant policy
Minutes of relevant meetings (e.g. clinical effectiveness or clinical audit committee
meetings)
Clinical audit plan(s)
Completed clinical audit reports
Action/ Improvement plans
Management reports outlining evidence of improvements in clinical care
3. Is the implementation of evidence-based practice through use of recognised standards,
guidelines and protocols promoted?
GUIDANCE: The implementation of evidence-based practice through use of recognised standards,
guidelines and protocols should be promoted by the organisation as a matter of policy. All relevant
policy documentation should make reference to this. Evidence-based practice should not be
interpreted as being limited to clinical practice. All practices, including managerial practices, should,
where possible, be evidence-based. Check to ensure that every opportunity is being taken to
promote the implementation of evidence-based practice through use of recognised standards,
guidelines and protocols.
EXAMPLES OF VERIFICATION
Relevant policies, e.g. quality, clinical effectiveness/audit, risk management, etc.
Minutes of relevant meetings, e.g. clinical effectiveness/audit committee
Ask relevant staff
4. Are information systems being properly exploited to support clinical effectiveness activity?
GUIDANCE:The determination of whether information systems are being properly exploited is a
judgment call by those carrying out the self-assessment, assisted where necessary by those with
specialist clinical effectiveness knowledge and expertise. In some cases, the information systems
may not be there to exploit. Where information systems are in place, the key issues here are to check
a) whether the information within the systems is being fully utilised to support clinical effectiveness
activity and b) whether there are any deficiences in the information systems themselves that could
be improved to provide better clinical effectiveness support.
EXAMPLES OF VERIFICATION
Clinical effectiveness policy/ procedures/ Ask staff engaged in clinical effectiveness
activity
5. Are clinical audits based on agreed selection criteria (e.g. high risk, cost, or volume; serious
concerns arising from adverse events or complaints; new guidelines; local or national priorities;
or patient focus)?
GUIDANCE: Given limited resources, it is usually necessary to prioritise clinical audit activity. The
determination of priority in clincal audit selection should be based on agreed criteria. The criteria
should be clearly set in the relevant policy and procedural documentation, and reflected in clinical
audit work plans, etc.
02.LayOut 12/3/10 4:55 PM Page 47
48 Achieving Excellence In Clinical Governance
EXAMPLES OF VERIFICATION
Clincial audit policy/procedure
Documented clinical audit work plan
RESOURCES
NICE (2002). Principles for best practice in clinical audit. Free download at
www.nice.org.uk/media/796/23/BestPracticalClinicalAudit.pdf
6. Is there evidence that clinical effectiveness activities result in changes in clinical practice and
improvements in the standards of care?
GUIDANCE: The outcome of clinical effectiveness activity is to demonstrate improvement in care
through changes in clinical practice and improvement in care standards. What evidence exists to
demonstrate improvement? Can clinical practice change be demonstrated? How have care
standards improved as a consequence of clinical effectiveness activity?
EXAMPLES OF VERIFICATION
Clinical effectiveness/ audit reports
Minutes of relevant meetings e.g. clinical effectiveness/audit committee
Ask staff
02.LayOut 12/3/10 4:55 PM Page 48
Achieving Excellence In Clinical Governance 49
H. PATIENT/ SERVICE USER AND PUBLIC/ COMMUNITY INVOLVEMENT
NB Shaded number box indicates question requires possible aggregation across the organisation.
(**questions are adapted from the Victorian Safety and Quality Improvement Framework, Australia)
1. Is patient/ service user and public feedback, (including feedback on actual patient experience)
regularly sought and integrated into quality, safety and risk management improvement
activities?
GUIDANCE: A range of approaches can be adopted to obtain feedback, including complaints and
suggestions mechanisms, focus groups, surveys, meetings with patient groups, etc. Feedback
should be regularly sought, analysed and the key finding from the feedback incorporated into
ongoing quality, safety and risk improvement activities.
EXAMPLES OF VERIFICATION
Survey report
Focus group reports
Suggestion reports
Minutes of relevant meetings
Action/ improvement plans
RESOURCES
See Victorian Safety and Quality Improvement Framework, Australia.
2. Is sufficient information and opportunity provided for patients/service users to meaningfully
participate in their own care?
GUIDANCE: A professional judgment, backed by meaningful patient/service user feedback, needs to
be made about the sufficiency of information and opportunities for patients to participate in their
own care.
EXAMPLES OF VERIFICATION
Patient surveys
Examination of Care Plans
Check role of clinical nurse specialists
Information guides for patients/service users
3. Are patients/ service users and the public involved in the development of patient information?
EXAMPLES OF VERIFICATION
Check minutes of meetings, relevant reports, etc.
4. Are arrangements in place to train and support patients/ service users, staff and the public involved
in the patient and public involvement process?
GUIDANCE: A tool kit can be produced to assist with training and support.
EXAMPLES OF VERIFICATION
Evidence of completed training using the tool kit
5. Are patients/ service users and the public invited to assist in planning new services?
EXAMPLES OF VERIFICATION
Check arrangements for planning new services
Check attendance at relevant meetings (meeting minutes)
02.LayOut 12/3/10 4:55 PM Page 49
50 Achieving Excellence In Clinical Governance
I. RISK MANAGEMENT AND PATIENT SAFETY
Shaded number box indicates question requires possible aggregation across the organisation.
1. Are risks of all kinds systematically identified and assessed?
GUIDANCE: Refer to Resources, below.
EXAMPLES OF VERIFICATION:
Risk management policy/Risk register(s)/ Evidence of risk identification workshops/ Incident
reviews/ Complaints review
RESOURCES:
AS/NZS 4360:2004 the Australian/New Zealand Risk Management Standard
2. Are risks of all kinds managed in order of priority?
GUIDANCE: Typically, given limited resources and other considerations, risks need to be managed
in some kind of priority order. This usually happens in the context of the risk register where risks are
assessed and evaluated and are ranked in relation to the magnitude of the risk.
EXAMPLES OF VERIFICATION:
Risk register(s) & risk action plan(s)
RESOURCES:
MOH RCA Manual; AS/NZS 4360:2004
3. Are risk registers used for the purpose of managing and communicating risk at all levels?
GUIDANCE: The key requirement of this question is to determine whether risk register are used at
all levels in the organisation. Risk registers are, essentially, communication tools. They help ensure
sufficient information on risks is communicated to the appropriate level in an organisation to allow
the risk to be properly managed.
EXAMPLES OF VERIFICATION:
Evidence of risk registers at all levels in the organisation
RESOURCES:
MOH RCA Manual; AS/NZS 4360:2004
4. Are arrangements in place to manage known high-priority risk issues?
GUIDANCE: Service providers should be able to demonstrate that they have systems in place to
manage known high-priority risk issues such as in the current MOH Incident Reporting System and
the Private Health Care Facilities and Services Act 1998 Regulations 2006 list of mandatory incidents
to be monitored. Examples of priority areas include:
Medication management; Slips, trips and falls; Violence and aggression; Vulnerable adults
and children; Infection control; Haemovigilance; Utility contingency; Medical devices
Waste management; Moving and Handling; Restraint; Suicide and deliberate self-harm; High
priority risk issues will typically have been previously identified from local experience and
national initiatives. The risk register will also contribute to an understanding of local high
priority risk issues.
EXAMPLES OF VERIFICATION:
Dedicated policies covering specific high priority risk issues/ Relevant programmes to address high-
priority risk issues/ Relevant action plans
02.LayOut 12/3/10 4:55 PM Page 50
Achieving Excellence In Clinical Governance 51
5. Are staff-related occupational safety, health and welfare risks identified, assessed and
managed? Are arrangements in place to ensure the management of occupational health, safety
and welfare?
GUIDANCE: All staff-related occupational safety, health and welfare risks should be identified,
assessed and managed in line with implementing the risk management process set out above.
Appropriate systems and processes should be in place to ensure the management of occupational
safety, health and welfare as per the Malaysian Occupational Safety and Health Act 1994 and
Regulations.
EXAMPLES OF VERIFICATION:
Use of OHSA audit tool/ Inclusion of a range of occupational safety, health and welfare risks in risk
register(s)/ Action plans incorporating actions to address occupational safety, health and welfare risk
issues.
6. Are environmental and fire safety risks identified, assessed and managed? Are arrangements in
place to ensure that environmental and fire risks are minimised through meeting legislative and
mandatory requirements?
GUIDANCE: All environmental and fire safety risks should be identified, assessed and managed in
line with implementing the risk management process set out above. Appropriate systems and
processes should be in place to ensure that these risks are minimised through meeting legislative
and mandatory requirements. Seek the advice of competent professionals when determining risks
and actions.
EXAMPLES OF VERIFICATION:
Environmental and fire safety audit and/ or inspection records/ Inclusion of a range of environmental
and fire risks in risk register(s)/ Action plans incorporating actions to address environmental and fire
safety risk issues
7. Is an on-going programme of patient safety improvement in operation?
GUIDANCE: Achieving significant improvements in patient safety is currently seen as a major
imperative for healthcare internationally. This is evidenced by the relatively recent establishment of
the World Health Organisation (WHO) World Alliance for Patient Safety. All risks to patient safety
should be identified, assessed and managed in line with implementing a robust risk management
process defined by the above questions.
EXAMPLES OF VERIFICATION:
Evidence of on-going implementation of a programme on patient safety.
RESOURCES
WHO World Alliance for Patient Safety - www.who.int/patientsafety/en/
HIQA www.hiqa.ie
UK National Patient Safety Agency www.npsa.nhs.uk
USA Joint Commission - www.ccforpatientsafety.org/
ECRI Institute www.ecri.org
Institute for Healthcare Improvement (IHI) - www.ihi.org/IHI/Topics/PatientSafety/
US Department of Veterans Affairs National Center for Patient Safety - www.va.gov/ncps/
US Agency for Healthcare Research and Quality - www.ahrg.gov/qual/
02.LayOut 12/3/10 4:55 PM Page 51
52 Achieving Excellence In Clinical Governance
8. Are arrangements in place to ensure that Medical Device Alerts/Safety Notices are circulated
to all relevant staff and are acted on?
GUIDANCE: A suitable policy and procedure should be in place to ensure that all alerts and safety
notices are circulated to all relevant staff and, most importantly, are acted upon. Various software
systems exist that enable this to be done efficiently.
EXAMPLES OF VERIFICATION:
Policy/ procedure for dealing with medical device alerts and safety notices/ Software system in use
for identifying and circulating alerts and notices, and for monitoring whether they have been acted
upon.
9. Are incidents properly recorded and reported to management?
GUIDANCE: Refer to incident management policy and procedure for detailed guidance.
EXAMPLES OF VERIFICATION:
Random sample of local incident reports
RESOURCES:
Incident Reporting (IR) manual)
10. Are incidents managed in accordance with an agreed policy?
GUIDANCE: There should be a locally-agreed policy for incident management that takes cognisance
of the MOHs overall incident management policy and procedure.
EXAMPLES OF VERIFICATION:
Local incident management policy/ Select a sample of incidents and trace back how they were
managed to establish degree of compliance with policy/ Talk to managers, clinicians and staff
RESOURCES:
MOH 1998 Incident Reporting manual and subsequent versions of this manual
11. Are incidents rated according to impact and reviewed, where appropriate, to determine
contributory factors, root causes and any actions required?
GUIDANCE: All reported incidents should be rated according to impact in order to determine what,
if any, further action is required, The key to learning from incidents is root cause analysis
(sometimes termed systems analysis). Refer to MOH systems analysis/ root cause analysis in the
QA manuals and Clinical Incident Surveillance Systems manual 2010 for further information.
EXAMPLES OF VERIFICATION:
Incident reports/ Risk register information/Incident investigation/ RCA report
RESOURCES:
MOH or local private hospital incident reporting manual/ policy and procedure
12. Are incidents subjected to periodic aggregate reviews to identify trends and further opportunities
for learning, quality and safety improvement, and risk reduction?
GUIDANCE: All reported incident information should be aggregated to identify trends and further
opportunities for learning, etc.
EXAMPLES OF VERIFICATION:
Incident review reports
02.LayOut 12/3/10 4:55 PM Page 52
Achieving Excellence In Clinical Governance 53
RESOURCES:
MOH or local private hospital incident management policy and procedure
13. Are complaints, comments and appeals properly recorded and reported to management?
GUIDANCE: Refer to MOH guidelines on complaints management.
EXAMPLES OF VERIFICATION:
Check a sample of complaints reports
RESOURCES:
MOH guidelines on complaints management
14. Are complaints managed in accordance with an agreed policy?
GUIDANCE: This question relates to the management of the complaint subsequent to its being
reported to management. There should be an agreed local policy for management of complaints that
takes cognisance of MOH guidelines.
EXAMPLES OF VERIFICATION:
Local complaints management policy / Select a sample of complaints and trace back how they were
managed to establish degree of compliance with policy/ Talk to managers, clinicians and staff
RESOURCES:
MOH guidelines on complaints management
15. Are complaints rated according to impact and reviewed, where appropriate, to determine
contributory factors, root causes and any actions required?
GUIDANCE: All reported complaints should be rated according to impact in order to determine what,
if any, further action is required, The key to learning from complaints is root cause analysis
(sometimes termed systems analysis), Refer to MOH guidelines on Root Cause Analysis/ systems
analysis for further information.
EXAMPLES OF VERIFICATION:
Complaints reports/ Risk register information/ Complaints investigation/ RCA report
RESOURCES:
MOH guidelines on complaints management
16. Are complaints and comments subjected to periodic aggregate reviews to identify trends and
further opportunities for learning, quality and safety improvement, and risk reduction?
GUIDANCE: All complaints information should be aggregated to identify trends and further
opportunities for learning, etc.
EXAMPLES OF VERIFICATION:
Complaints review reports/ Action/ improvement plans/ Risk register information
RESOURCES:
MOH guidelines on complaints management
17. Where appropriate, are all claims recorded and analysed to identify opportunities for learning,
quality and safety improvement, and risk reduction?
EXAMPLES OF VERIFICATION:
Claims review reports/ Action/ improvement plans/ Risk register information
02.LayOut 12/3/10 4:55 PM Page 53
54 Achieving Excellence In Clinical Governance
J. STAFFING AND STAFF MANAGEMENT
Shaded number box indicates question requires possible aggregation across the organisation.
1. Are arrangements in place to ensure appropriate workforce planning?
GUIDANCE: Arrangements should reflect workforce planning policies, strategies, etc.
EXAMPLES OF VERIFICATION
Workforce planning policies etc.
Evidence of compliance with workforce planning arrangements
RESOURCES
workforce planning policies, strategies, etc.
2. Are arrangements in place to ensure appropriate recruitment, induction, and training and
development for staff appropriate to their roles and responsibilities?
EXAMPLES OF VERIFICATION
Relevant policies, procedures, etc.
Induction programmes
Training needs analysis reports
Training records
3. Do the arrangements set out in questions 1 and 2 ensure compliance with related Malaysian
employment legislation?
EXAMPLES OF VERIFICATION
Check all relevant arrangement, i.e. policies, procedures, etc.
RESOURCES
Relevant legislation/ Relevant Malaysian policies, codes, guidance, etc.
4. Are continuing learning and development programmes in place and aimed at meeting the
development needs of staff and services?
EXAMPLES OF VERIFICATION
Check learning and development programme details
Training needs analysis
Development needs analysis
5. Are robust pre-employment checks carried out in line with national policy and the requirements
set out in this framework?
EXAMPLES OF VERIFICATION
Evidence of employment checks
RESOURCES
Relevant national policies etc.
6. Are arrangements in place to identify and deal with poor professional performance?
EXAMPLES OF VERIFICATION
Policy on identifying and dealing with poor professional performance.
Evidence of instances where poor performance has been identified and dealt with in
accordance with relevant policy
02.LayOut 12/3/10 4:55 PM Page 54
Achieving Excellence In Clinical Governance 55
K. SERVICE IMPROVEMENT
NB Shaded number box indicates question requires possible aggregation across the organisation.
1. Are quality, safety and risk management goals clear, communicated effectively throughout the
organisation and reflected in relevant service planning processes?
GUIDANCE: The MOHs QA manuals, KPI manuals, Incident reporting manuals, WHO World Alliance
for Patient Safety programmes etc. contain a wealth of guidance relevant to this entire element of
the Framework see Resources, below.
EXAMPLES OF VERIFICATION
Communication arrangements
Check actual communication
Check relevant service and business planning processes
RESOURCES
Improving Our Services A Users Guide to Managing Change in the Health Service
Executive. www.hse.ie/eng/Publications/Human_Resources/Improving_Our_Services.pdf
2. Do local quality, safety and risk management plans take account of identified national priorities?
EXAMPLES OF VERIFICATION
World Alliance for Patient Safety Safe Surgery Saves Lives and WHO Clean Care Is Safer Care
3. Does the organisation participate in relevant external accreditation programmes?
GUIDANCE: A range of accreditation programmes exist, e.g. MSQH, JCI programmes, etc.
Draw up a list of accreditation programmes that your organisation participates in.
EXAMPLES OF VERIFICATION
Evidence of accreditation programme participation
4. Do quality improvement activities utilise a range of quality improvement tools to assist with
assessing and diagnosing issues, identifying remedies and measuring improvement?
GUIDANCE: There are many quality improvement tools available in healthcare that can assist with
diagnosing issues, identifying remedies and measuring improvement. The following are generally-
accepted tools for quality improvement:
Performance measures, including clinical indicators and key performance indicators
Adverse event management
Culture and change management
Team Building
Integrated care pathways
Incident monitoring
Clinical audits
Flow-charts
Cause-and-effect diagrams
Brainstorming
Pareto charts
Histograms
Run charts
Control charts
Scattergrams
CUSUM
02.LayOut 12/3/10 4:55 PM Page 55
56 Achieving Excellence In Clinical Governance
Other tools include failure mode and effects analysis (FMEA), lean techniques, Plan-Do-Check-Act
(PDSA), theory of constraints, CUSUM and six sigma. Six sigma is a particularly powerful tool for
measuring and monitoring quality improvement.
EXAMPLES OF VERIFICATION
Look for evidence of use of a range of quality improvement tools in service improvement
projects and in day-to-day quality improvement activity
RESOURCES
Irish Health Services Accreditation Board. Acute Care Accreditation Scheme A Framework
for Quality and Safety. 2nd Edition.
Department of Health & Children (2008). Building a Culture of Patient Safety. Report of the
Commission on Patient Safety and Quality Assurance.
The US Institute for Healthcare Improvement provides a range of free quality improvement
tools at www.ihi.org/IHI/Topics/ImprovementMethods/Tools/
A compendium of information on six sigma in healthcare can be found at
http:/healthcare.isixsigma.com/spotlight/
02.LayOut 12/3/10 4:55 PM Page 56
Achieving Excellence In Clinical Governance 57
L. LEARNING AND SHARING INFORMATION
NB Shaded number box indicates question requires possible aggregation across the organisation.
1. Does the hospital routinely learn from patient experience?
GUIDANCE: Actively seeking patients, and other service users views about their experience of health
and social care can provide valuable insights and learning that can inform service, quality, safety and
risk management improvement processes. See Resources section, below. What evidence exists that
demonstrates that your organisation routinely learns from patient experience?
EXAMPLES OF VERIFICATION
Learning reports from patient survey information
Relevant policies
Risk register
Improvement action plans
Complaints and suggestions from clients
RESOURCES
Various patient satisfaction guidelines and reports from the Irish Society for Quality &
Safety in Healthcare are available for download at
www.isqsh.ie/docs/default.asp?mnu=8&wgID=&folder=Patient+Participation
2. Does the hospital routinely learn from incidents occurring within the organisation and
elsewhere?
GUIDANCE: Whilst it is unfortunate that incidents should occur in healthcare, particularly in
instances where they result in harm to people, nevertheless it behooves organisations to reflect upon
and learn from what has happened in an effort to avoid, or reduce the likelihood of future similar
incidents. It is important that this learning happens not just within the organisation, but also happens
in relation to incidents occurring elsewhere in another service provider in Malaysia, for example,
or in organisations in other countries. The benefits of learning from incidents occurring elsewhere,
of course, include the fact that it has not happened in your own organisation.
In addition to learning from individual incidents, it is important to learn from incident trends. Plotting
many incidents over time can reveal important issues that need to be addressed. The figure in the
guidance associated with question E3 is a case in point.
What evidence exists to show that your organisation routinely learns from incidents occurring within
your own organisation, and elsewhere?
EXAMPLES OF VERIFICATION
Incident investigation/analysis reports (e.g RCA report)
Action plans resulting from incident review
Risk identification process
Risk register, detailing risks resulting from incident investigation/analysis/review
RESOURCES
Latest MOH guidance on incident management
Department of Health & Children (2008). Building a Culture of Patient Safety.
Report of the Commission on Patient Safety and Quality Assurance
3. Does the organisation regularly communicate to patients, staff and other relevant stakeholders
improvements that have been made as a consequence from learning from patient experience and
incidents?
GUIDANCE: People usually appreciate knowing what improvements have been made in response to
feedback on patient experience and incidents. In essence, this can be thought of as closing the loop.
02.LayOut 12/3/10 4:55 PM Page 57
58 Achieving Excellence In Clinical Governance
Such feedback can be provided in many ways such as making public specialists reports, or
communicating the information in regular newsletters or general annual reports.
EXAMPLES OF VERIFICATION
Patient survey reports
Incident reports
Communications policy
Regular newsletters
Annual reports
Internal communication notice boards
4. Does the hospital share information and learning about serious incidents with other health
providers and agencies?
GUIDANCE: When things go wrong it is important that information and learning is communicated
with others. Learning from elsewhere should be a key component of any organisations risk
identification process.
EXAMPLES OF VERIFICATION
Participation in national incident reporting schemes
Reports to relevant agencies e.g. MADRAC, National Haemovigilance Programme
5. Are arrangements in place for learning and for sharing information on good practice in relation
to quality, safety and risk management?
GUIDANCE: Assuring the safety of patients, staff and visitors is a key priority in the MOH and the
private sector.
This requires a collaborative approach to the analysis of quality and risk information so that the
lessons learnt from this analysis are shared across the service area or organisation and across the
Malaysian health care system a whole. It is essential that service providers develop a learning culture
and that effective learning and sharing processes are developed to spread good practice and
educate/inform others. The electronic self-assessment tool provides a means of capturing
information on goof practice that can be shared with other organisations and services.
EXAMPLES OF VERIFICATION
Seminars.
Briefings.
Workshops.
Education programmes.
Newsletters, journals, publications etc.
Presentation at National/International conferences
Electronic self-assessment tool (Quality, safety and risk management framework)
Hospital web-sites
02.LayOut 12/3/10 4:55 PM Page 58
Achieving Excellence In Clinical Governance 59
4. Outcomes
M. KEY PERFORMANCE INDICATORS (KPIs)
NB Shaded number box indicates question requires possible aggregation across the organisation.
1. Have local KPIs been developed for quality, safety and risk management?
GUIDANCE: The following guidance is adapted from the Audit Commission in England see
Resources, below.
A performance indicator (PI) is a clearly defined measurement of one aspect of performance. It
literally provides an indication of how well you are performing a given activity. A key performance
indicator is one that provides essential organisational level information on the performance of an
activity for accountability and performance management purposes. Examples of local KPIs are given
below.
Performance information on quality, safety and risk management is not an end in itself. It may be
used to:
1. Measure progress towards achieving local or corporate quality, safety and risk management
objectives and targets.
2. Promote the accountability of service providers to patients/service users, the public and
other stakeholders.
3. Compare performance to identify opportunities for improvement.
4. Promote service improvement by publicising performance levels.
KPIs come in all shapes and sizes. It is important that you select the key indicators that reflect
your activities and management needs. Examples of KPIs currently used, or proposed in the MOH
Patient Care Services QAP:
% compliance with Quality, Safety and Risk Management Framework (from the electronic
scoring tool)
Patient reported satisfaction (e.g. very satisfied, satisfied, somewhat satisfied, somewhat
dissatisfied, dissatisfied, very dissatisfied)
Staff satisfaction (composite indicator e.g. very satisfied, satisfied, somewhat satisfied,
somewhat dissatisfied, dissatisfied, very dissatisfied)
Incident reporting rates (injury incidents; ill health incidents; near misses)
% of all reported injury incidents (excluding near misses) categorised as High risk/ severity
STEMI Mortality rate
Specialist Clinic waiting time
Out-patient waiting lists
Elective Operations Cancellation Rates
Hospital MRSA, ESBL rates
Presence of fully operational, up-to-date risk register in place in accordance with MOH risk
management guidance (Yes, No, Partial) by hospital/department
Presence of fully operational, up-to-date risk register in place in accordance with MOH risk
management guidance (Yes, No, Partial) by State
For a comprehensive introduction to the specification and use of performance indicators, refer to the
Audit Commission guidance document specified in the Resources section, below.
Much can be learned from the work of the Government Agency for Research in Healthcare Quality
(AHRQ) in the USA, who have published comprehensive indicator sets for healthcare quality and
patient safety. Refer to the AHRQ indicators specified in the Resources section, below.
The MOH will specify a national KPI set for quality, safety and risk management based, at least in
part, on a review of indicators being used by local service providers.
02.LayOut 12/3/10 4:55 PM Page 59
60 Achieving Excellence In Clinical Governance
EXAMPLES OF VERIFICATION
Local performance indicator list or dashboard.
Indicator specification and use in specific circumstances, e.g. strategic frameworks; patient
safety goals; patient satisfaction reports; medication error reports; risk management
reporting; complaints management; service level reporting; etc.
RESOURCES
Audit Commission (UK - 15 June 2000). On Target. The practice of performance indicators.
This is a highly recommended resource, which is freely downloadable from (Search for the
practice of performance indicators).
Agency for Healthcare Research and Quality (AHRQ, USA March 2008). AHRQ Quality
Indicators Version 3.2: Prevention quality indicators; Inpatient quality indicators; and patient
safety indicators.
2. Are the KPIs monitored as part of on-going quality, safety and risk management improvement
activities?
GUIDANCE: Indicators should be regularly monitored to ensure that performance is on track. Any
significant variances in indicators should be investigated to determine causation. It should be noted
that performance indicators do not provide answers to why differences exist but raise questions and
suggest where problems may exist (i.e. they are flags to denote areas for possible improvements).
EXAMPLES OF VERIFICATION
Performance reports, clearly setting out KPI information
Evidence of consideration of reports by relevant committees and senior managers (e.g. see
relevant minutes).
Evidence that, where necessary, action is taken by management in response to monitoring
(e.g. see relevant minutes).
3. Do the KPIs demonstrate that there is on-going improvement in quality, safety and risk
management?
GUIDANCE: Ultimately, any system of performance measurement exists to demonstrate
improvement. Do the KPIs that you use show, over time, that improvements in the quality and safety
of care, together with improvements in risk management generally, are being realised?
EXAMPLES OF VERIFICATION
Performance reports, clearly setting out improvements in KPIs over time
02.LayOut 12/3/10 4:55 PM Page 60
Achieving Excellence In Clinical Governance 61
5. Glossary of terms
The following glossary of terms is a sub-set of terms principally drawn, verbatim, from the HSEs Quality
and Risk Taxonomy Governance Group Draft Report, June 2008. Each term is listed in alphabetical order
and, for each term, a definition is provided and the source of the definition is referenced. The full report
should be consulted for a full list of references. Note that there are some definitions in italics. These are
taken from a previous draft version of this Framework Document.
Term Definitions And References
Accountability is the obligation to demonstrate and take responsibility for performance in light of
commitments and expected outcomes (Information Management, Government of Canada,
2004)
Accountable Being held responsible (WHO, 2007).
Accreditation Accreditation involves self assessment by a health care organisation to evaluate their level
of performance in relation to established standards. The self assessment is validated by an
external review team which consists of peers and service users (IHSAB 2005)
Actions taken Actions taken to reduce, manage or control the harm, or probability of harm associated with
an incident (WHO, 2007).
Adverse Event Refer to Incident
Attributes Qualities, properties or features of someone or something (WHO, 2007).
Audit Auditing is an independent, objective assurance and consulting activity designed to add
value and improve an organisation's operations. It helps an organisation accomplish its
objectives by bringing a systematic, disciplined approach to evaluate and improve the
effectiveness of risk management, control, and governance processes. (Institute of Internal
Auditors, 2007)
Clinical Audit The systematic, critical analysis of the quality of care, including the procedures used for
diagnosis and treatment, the use of resources and the resulting outcome and quality of life
for the patient (Quality and Fairness: A Health System for You, 2001)
or
A quality improvement process that seeks to improve the patient care and outcomes through
systematic review of care against explicit criteria and implementation of change. Aspects of
the structures, processes and outcomes of care are selected and systematically evaluated
against explicit criteria. Where indicated, changes are implemented at an individual team, or
service level and further monitoring is used to confirm improvement in healthcare delivery
(National Institute for Health and Clinical Excellence)
Clinical The extent to which specific clinical interventions do what they are intended to do, i.e.
Effectiveness maintaining and improve health, securing the greatest possible health gain from the
available resources (NHS Scotland, 2005).
or
The extent to which specific clinical interventions, when deployed in the field for a particular
patient or population, do what they are intended to do i.e. maintain and improve health and
secure the greatest possible health gain from the available resources. (Promoting Clinical
Effectiveness: A framework for action in and through the NHS, NHS Executive, January
1996)
Clinical Guideline Systematically developed statements to assist health care professional and patient decisions
about appropriate health care for specific clinical circumstances. They identify good practice
but contain little operational detail and are not rigid constraints on decisions. (Adapted from
definitions by Institute of Medicine and NHS Executive, England).
Clinical A Framework through which organisations are accountable for continually improving the
Governance quality of their services and safeguarding high standards of care by creating an environment
in which excellence will flourish (adapted Scally and Donaldson, 1998)
02.LayOut 12/3/10 4:55 PM Page 61
62 Achieving Excellence In Clinical Governance
Code of Practice Codes of Practice are general guidelines setting out good practice relating to government
legislation providing guidance and direction in addressing a particular and specific area for
improvement (National Disability Authority, 2001).
Complaint A Complaint means a complaint made about any action of the Executive, or a Service
Provider that, it is claimed, does not accord with fair or sound administrative practice, and
adversely affects the person by whom, or on whose behalf, the complaint is made (Health
Act 2004)
Confidentiality Ensuring that information is accessible only to those authorised to have access
(International Organisation for Standardisation, 2008a).
Continuous Quality Continuous Quality Improvement is a management Improvement (CQI) philosophy and
system which involves management, staff and health professionals in the continuous
improvement of work processes to achieve better outcomes of patient/ client/ resident care
(Health Canada 1993).
Contractor Means any individual, employer or organisation whose employees undertake work for a
fixed or other sum and who supplies the materials and labour (whether their own labour or
that of another) to carry out such work, or supplies the labour only (Health and Safety
Authority, 2006).
Contributing factor Any factor(s) pertaining to an organisation and/or person which can impact positively or
negatively on the organisation and/or person (adapted Information Services NHS Scotland,
2004)
Corporate Corporate governance is the system by which organisations direct and governance control
their functions and relate to their stakeholders in order to manage their business, achieve
their missions and objectives and meet the necessary standards of accountability, integrity
and propriety (Framework for corporate and financial governance of the HSE, 2006).
Culture A set of beliefs, values, attitudes, and norms of behaviour shared by individuals within an
organisation (Davies HTO, Nutley SM, Mannion R. 2000).
Error Failure of a planned action to be completed as intended or use of a wrong plan to achieve
an aim (Institute of Medicine 2000).
Evaluation Assessment/ appraisal of the degree of success in meeting the goals and expected results
(outcomes) of the organisation, service, programme, population or patients/ clients (HIQA
2006).
Evidence-based The conscientious, explicit and judicious use of current best evidence in practice making
decisions about the care of patients/service users (Gardner MJ and Altman DG, 1986)
Framework A framework is a set of components that provide the foundations and organisational
arrangements for designing, implementing, monitoring, reviewing and continually
improving (adapted International Organisation for Standardisation, 2008b).
Goals Broad statements that describe the desired state for the future and provide direction for day-
to-day decisions and activities (HIQA 2006).
Governance Systems, processes and behaviour(s) by which organisations lead, direct and control their
functions in order to achieve organisational objectives, safety and quality of service and in
which they relate to patients and carers, the wider community and partner organisations
(Department of Health, 2006)
Guideline A Guideline is a principle or criterion that guides or directs action (Concise Oxford
Dictionary, 1995)
Harm A detrimental impact on the organisations stated objectives, including physical,
psychological, financial, environmental harm (adapted Leveson 1995)
Term Definitions And References
02.LayOut 12/3/10 4:55 PM Page 62
Achieving Excellence In Clinical Governance 63
Hazard A source of potential harm (AS/NZS 4360:2004)HealthcareServices received by individuals
or communities to promote, maintain, monitor or restore health (WHO, 2007).
Impact The outcome of an event expressed quantitatively and / or qualitatively being a loss, injury,
disadvantage or gain (adapted AS/NZS 4360:2004).
Incident Any event that causes or has the potential to cause harm. (adapted Myatt, V.L. 2002)
Key Performance Key Performance Indicators (KPI) are financial and non-financial Indicators metrics used to
help an organisation define and measure progress towards organisational goals (Parmenter
D, 2007)
Likelihood Describes the probability or frequency of an impact occurring (adapted AS/NZS 4360:2004))
Monitor To check, supervise, observe critically, or record the progress of an activity, action or system
on a regular basis in order to identify change from the performance level required or
expected (AS/NZS 4360:2004))
Near Miss An event that could have resulted in an incident, but did not, either by chance or through
timely intervention (Quality Interagency Co-0peration Task Force, 2000)
Objectives Concrete, measurable steps taken to achieve goals (HIQA 2006).Patient A person who is a
recipient of healthcare (WHO, 2007).
Patient Safety Any event that causes, or has the potential to cause harm to a patient Incident (adapted
WHO, 2007).
Policy Written statement that clearly indicates the position and values of the organisation on a
given subject (HIQA 2006).
Procedure Written set of instructions that describe the approved and recommended steps for a
particular act or sequence of acts (HIQA 2006).
Protocol Operational instructions which regulate and direct activity (NHS Scotland 2005).
Quality Doing the right thing consistently to ensure the best possible outcomes for patients,
satisfaction for all customers, retention of staff and a good financial performance (Leahy and
Wiley 1998).
Record Includes any memorandum, book, report, statement, register, plan, chart, map,
specification, diagram, pictorial or graphic work or other document, any photograph, film or
recording (whether of sound or images or both), and any form in which data (within the
meaning of the Data Protection Act 1988 and 2003) are held, and form (including machine-
readable form) or thing in which information is held or stored manually, mechanically or
electronically, and anything that is a part or copy, in any form, of any of the foregoing or is
any combination of two or more of the foregoing (Freedom of Information Act 1997)
Residual Risk Risk remaining after all reasonable practicable control measures are implemented (adapted
AS/NZS 4360: 2004).
Risk The chance of something happening that will have an impact on the achievement of
organisational stated objectives (AS/NZS 4360:2004)).
Risk Analysis A systematic process to understand the nature of and to deduce the level of risk
(AS/NZS 4360:2004)
Risk Assessment The overall process of risk identification, risk analysis and risk evaluation
(AS/NZS 4360:2004)
Risk Avoidance A decision not to become involved in, or withdraw from a risk situation
(AS/NZS 4360:2004)
Term Definitions And References
02.LayOut 12/3/10 4:55 PM Page 63
64 Achieving Excellence In Clinical Governance
Risk Control An existing process, policy, device, practice or action that acts to minimise negative risk or
enhance positive opportunities (AS/NZS 4360:2004)
Risk Criteria Terms of reference by which the significance of risk is assessed (AS/NZ 4360:2004)
Risk Evaluation Process of comparing the level of risk against risk criteria (AS/NZS 4360:2004)
Risk Management The culture, processes and structures that are directed towards realizing potential
opportunities whilst managing adverse effects (AS/NZS 4360:2004)
Risk management The systematic application of management policies, procedures and process practices to the
tasks of communicating, establishing the context, identifying analysing, evaluating, treating,
monitoring and reviewing (AS/NZS 4360:2004)
Risk Management Set of elements of an organisations management system concerned with Framework
managing risk (AS/NZS 4360:2004)
Risk Matrix Is a form of presentation, a single table, which enables easy comparison of the values placed
on different risks (Health Care Standards Unit and Risk Management Working Group 2004).
Risk Maturity The extent to which a robust risk management approach has been adopted and applied, as
planned, by management across the organisation to identify, assess, decide on responses
to and report on opportunities and threats that affect the achievement of the organisations
objectives (Institute of Internal Auditors UK and Ireland, 2007).
Risk Register A risk register is a management tool that enables an organisation to understand its
comprehensive risk profile. It is simply a repository for risk information (Health Care
Standards Unit and Risk Management Working Group 2004).
Risk Retention Acceptance of the burden of loss, or benefit of gain from a particular risk
(AS/NZS 4360:2004)
Risk Sharing Sharing with another party the burden of loss, or benefit of gain from a particular risk
(AS/NZS 4360:2004)
Risk Treatment Process of selection and implementation of measures to modify risk (AS/NZS 4360:2004).
Root cause A structured investigation that aims to identify the true cause(s) of a problem, analysis and
the actions necessary to eliminate it (Andersen, B. and Fagerhaug, T. 2000). (Note: this is a
reactive process)
Safety Freedom from Hazard (WHO, 2007)
Serious Incident An incident which involved or is likely to cause extreme harm or is likely to become a matter
of significant concern to service users, employees or the public (HSE 2008)
Stake-holder Individuals, organisations or groups that have an interest or share, legal or otherwise, in
services. Stakeholders may include referral sources, service providers, employers,
insurance companies or payers. (HIQA 2006)
Standards Recognised best practice criteria by which the performance, efficiency, achievement etc. of
a person or organisation can be assessed (adapted Collins Dictionary 2001)
System Analysis A structured, systematic study of a system with a view to establishing, either reactively or
proactively the root cause(s) of actual or potential adverse effects and the actions necessary
to prevent or mitigate future adverse effects (Emslie, S. 2004). (Note: this is a reactive and
pro-active process)
Term Definitions And References
02.LayOut 12/3/10 4:55 PM Page 64
Achieving Excellence In Clinical Governance 65
6. Frequently Asked Questions
The following are a selection of key questions that have been asked relating to the Framework for
Integrated Quality, Safety and Risk Management across the Malaysian health care system
What is the fundamental purpose of the Framework?
Fundamentally, the Framework exists to ensure:
1. there is an appropriate framework for quality, safety and risk management in place across
Malaysian providers in health, personal social care to support and drive improvements in the
provision of safe, effective, high quality services;
2. drive core programmes of work in quality, safety and risk management, including: patient safety;
continuous professional development; and service improvement; and
3. ensure that appropriate accountability and oversight arrangements are in place to
monitor quality, safety and risk management performance and to support the provision of
assurances to senior management and the MOH top management
Why do some of the Framework questions seem a bit wooly? Can you not make them more specific?
The Framework is not intended to be highly prescriptive. The MOH recognises that service providers will
want to be innovative in how they address aspects of the Framework. Consequently, rather than pin you
down with highly prescriptive standards, we have produced a more generic quality, safety and risk
management framework that gives you as much latitude as possible to determine how best to meet the
requirements.
Why are staff not represented along with patients and service users at the heart of the Framework
diagram (the diagram containing concentric circles diagram showing patient/service user at the
centre together with underpinning requirements, core processes and programmes and outcomes
see Figure 1 in the Framework Document)?
The Framework relates to the core purpose of our existence, which is about helping patients and service
users live healthier, more fulfilled lives. The MOH does take the issue of staff health, safety and well-being
very seriously and this is reflected in the core processes and progammes aspect of the Framework.
How do risk registers relate to the Framework?
Risk management and, in particular, use of risk registers is an important aspect and is described in the
core processes and programmes component of the Framework. It should be borne in mind that any
assessment made against the Framework can be considered as forming part of a risk identification
exercise, and any weaknesses found can be considered as risks to the service provider and treated within
their local risk management process as such.
Will additional resources be made available to implement the Framework?
There are unlikely to be additional resources made available. It is important that service providers use
some of the techniques espoused by the Framework (e.g. risk management prioritisation methodologies)
to ensure optimal deployment of existing resources to improve the safety and quality of services.
02.LayOut 12/3/10 4:55 PM Page 65
66 Achieving Excellence In Clinical Governance
02.LayOut 12/3/10 4:55 PM Page 66
S-ar putea să vă placă și
- Introduction to Clinical Effectiveness and Audit in HealthcareDe la EverandIntroduction to Clinical Effectiveness and Audit in HealthcareÎncă nu există evaluări
- NHS Framework For Clinical GovernanceDocument12 paginiNHS Framework For Clinical Governancetiara_kusumaningtyas50% (2)
- Clinical Governance in The UK NHSDocument4 paginiClinical Governance in The UK NHSchiefsanjivÎncă nu există evaluări
- Medical Staff BylawsDocument39 paginiMedical Staff BylawsMaria Francesca MapaÎncă nu există evaluări
- Good Governance Practices in A HospitalDocument25 paginiGood Governance Practices in A HospitalSiddhesh KhadeÎncă nu există evaluări
- Quality Control & Quality Improvement: Under SupervisionDocument20 paginiQuality Control & Quality Improvement: Under Supervisionheba abd elazizÎncă nu există evaluări
- Uhmb Quality ImprovementDocument44 paginiUhmb Quality Improvementeloxs100% (1)
- What Is Clinical GovernanceDocument8 paginiWhat Is Clinical GovernanceApollwn100% (1)
- Leadership in Health Care Organizations PDFDocument44 paginiLeadership in Health Care Organizations PDFsyanti puspitasariÎncă nu există evaluări
- Joint Commission International (JCI) Requirements Related To Safe SurgeryDocument16 paginiJoint Commission International (JCI) Requirements Related To Safe Surgeryngurah_wardanaÎncă nu există evaluări
- Jci Booklet EngDocument46 paginiJci Booklet EngKimberly Solis100% (1)
- Quality in HealthcareDocument95 paginiQuality in Healthcarelaxman Bhatt0% (1)
- Health Care Quality ConceptsDocument11 paginiHealth Care Quality Conceptsmike700usÎncă nu există evaluări
- Healthcare Quality ManagementDocument2 paginiHealthcare Quality ManagementGajendra TodakarÎncă nu există evaluări
- International Principles For Healthcare Standards BDocument21 paginiInternational Principles For Healthcare Standards BevaÎncă nu există evaluări
- FMEA10 Sample PagesDocument24 paginiFMEA10 Sample Pageswy1suwirjaÎncă nu există evaluări
- STAN5 JCI AccreditationDocument57 paginiSTAN5 JCI AccreditationYulinur FirdausÎncă nu există evaluări
- مشروع المعايير الوطنية للمستشفيات - الأولويات الصحية الوطنيةDocument251 paginiمشروع المعايير الوطنية للمستشفيات - الأولويات الصحية الوطنيةMMMI-IÎncă nu există evaluări
- @@assessment of Medical Documentation As Per Joint Commission InternationDocument6 pagini@@assessment of Medical Documentation As Per Joint Commission InternationNahari ArifinÎncă nu există evaluări
- IPSG PresentationDocument38 paginiIPSG Presentationmuhammed shamaa100% (1)
- Dimensions of Quality in HealthcareDocument21 paginiDimensions of Quality in HealthcareKaranÎncă nu există evaluări
- Organizational Chart Cbahi ThemeDocument8 paginiOrganizational Chart Cbahi ThemeVelmurugan KumarasamyÎncă nu există evaluări
- Strengthen Patient Experience: (Implementation Plan of IDC Program) Domain 2Document21 paginiStrengthen Patient Experience: (Implementation Plan of IDC Program) Domain 2Rina LestariÎncă nu există evaluări
- High Performance in Hospital ManagementDocument232 paginiHigh Performance in Hospital ManagementTamil Selva100% (1)
- Joint Commission TST Hand Hygiene Data Collection Tool PDFDocument5 paginiJoint Commission TST Hand Hygiene Data Collection Tool PDFJoel Guillen JulianÎncă nu există evaluări
- Allocating Hospital Resources To Improve Patient ExperienceDocument6 paginiAllocating Hospital Resources To Improve Patient ExperienceMichael0% (1)
- JCI Whitepaper Cpgs Closing The GapDocument12 paginiJCI Whitepaper Cpgs Closing The GapMathilda UllyÎncă nu există evaluări
- ACHS Clinical Indicator PDFDocument169 paginiACHS Clinical Indicator PDFTri Hastuti HendrayaniÎncă nu există evaluări
- Strengthen Patient Experience: (Implementation Plan of IDC Program) Domain 3Document17 paginiStrengthen Patient Experience: (Implementation Plan of IDC Program) Domain 3Rina LestariÎncă nu există evaluări
- 7-Healthcare Safety Q Solutions 3rdDocument40 pagini7-Healthcare Safety Q Solutions 3rdn83% (6)
- Quality Management SystemDocument19 paginiQuality Management SystemSaqibKhanÎncă nu există evaluări
- Provider (6.3) ManualDocument44 paginiProvider (6.3) ManualFIAZ MAQBOOL FAZILIÎncă nu există evaluări
- Hospital Operations Excellence in ChinaDocument12 paginiHospital Operations Excellence in ChinaChennawit Yulue100% (1)
- Bench Marking Hospital Performance in HealthDocument48 paginiBench Marking Hospital Performance in Healthakhilaoruvingal100% (1)
- Accreditation Manual 2nd EditionDocument49 paginiAccreditation Manual 2nd EditionjGithinji100% (2)
- Improving Operating Theatre Performance Complete Step Guide Without PicDocument83 paginiImproving Operating Theatre Performance Complete Step Guide Without PicNana AkwaboahÎncă nu există evaluări
- WHO Handbook Heathcare Quality PolicyDocument74 paginiWHO Handbook Heathcare Quality PolicydazzlerofallÎncă nu există evaluări
- Improve Care.: Empower ChangeDocument13 paginiImprove Care.: Empower Changekukun67% (3)
- Total Quality Management ReportDocument37 paginiTotal Quality Management Reportmonir61Încă nu există evaluări
- Practical Clinical Audit Handbook v1 1Document50 paginiPractical Clinical Audit Handbook v1 1chunmun__sÎncă nu există evaluări
- Hospital ManagerDocument3 paginiHospital ManagerOkello George PatrickÎncă nu există evaluări
- Quality in Healthcare and AccreditationDocument25 paginiQuality in Healthcare and AccreditationSooraj ThomasÎncă nu există evaluări
- Patient Satisfaction QuestionnaireDocument4 paginiPatient Satisfaction QuestionnairePrasad KVVÎncă nu există evaluări
- Hospital AdministratorDocument2 paginiHospital AdministratorYogesh MittalÎncă nu există evaluări
- Interior Health Medication Management AuditDocument46 paginiInterior Health Medication Management AuditJoe Fries100% (1)
- 13 Patient Saefty and Quality ImprovementDocument36 pagini13 Patient Saefty and Quality ImprovementShafiq Ur RahmanÎncă nu există evaluări
- Compre Exam Review - Hospital Planning, Infrastructure., Design and MaintenanceDocument2 paginiCompre Exam Review - Hospital Planning, Infrastructure., Design and MaintenancePatricia PagsolinganÎncă nu există evaluări
- JCIADocument100 paginiJCIAKenny JosefÎncă nu există evaluări
- Ambulatory CareDocument2 paginiAmbulatory CareKarla JavierÎncă nu există evaluări
- CPHQ IntroductionDocument34 paginiCPHQ IntroductionDina Baroudi100% (3)
- Look-Alike, Sound-Alike Medication NamesDocument4 paginiLook-Alike, Sound-Alike Medication NamesBenjel AndayaÎncă nu există evaluări
- Healthcare Quality Assurance ManualDocument77 paginiHealthcare Quality Assurance ManualEvonne Tan100% (1)
- CBAHI IndicatorsDocument4 paginiCBAHI IndicatorsJery Js0% (1)
- Managing Healthcare OrganisationsDocument16 paginiManaging Healthcare OrganisationsSamuel Josafat Olam100% (1)
- Q SolnDocument100 paginiQ Solnahmed salah100% (1)
- Your Key To Understanding EC, EM, and LSDocument6 paginiYour Key To Understanding EC, EM, and LSteguh santosoÎncă nu există evaluări
- Protection of Patient ValuablesDocument4 paginiProtection of Patient Valuablesamirrzch100% (3)
- KPI Discussion Paper 3Document22 paginiKPI Discussion Paper 3Manager HR Hijaz Hospital100% (1)
- Buku Panduan Incident ReportingDocument120 paginiBuku Panduan Incident ReportingFaizudin HafifiÎncă nu există evaluări
- Clinical Audit Guideline 2023Document33 paginiClinical Audit Guideline 2023Team DIVAÎncă nu există evaluări
- Prescribing Policy HGMDocument9 paginiPrescribing Policy HGMummuawisyÎncă nu există evaluări
- DMTAC Protocol Tuanku Ampuan Najihah Kuala Pilah Update March 2013Document17 paginiDMTAC Protocol Tuanku Ampuan Najihah Kuala Pilah Update March 2013ummuawisy100% (1)
- Policy For Ambulance ServicesDocument11 paginiPolicy For Ambulance Servicesummuawisy0% (1)
- Manual ESTDocument12 paginiManual ESTummuawisyÎncă nu există evaluări
- Medical Clinic Standards v.1Document13 paginiMedical Clinic Standards v.1ummuawisyÎncă nu există evaluări
- Dilution Guide For HAMDocument128 paginiDilution Guide For HAMummuawisyÎncă nu există evaluări
- Look Alike Sound Alike MedDocument4 paginiLook Alike Sound Alike MedummuawisyÎncă nu există evaluări
- Final-Chronic Dialysis Treatment Standards - Nov 2012Document38 paginiFinal-Chronic Dialysis Treatment Standards - Nov 2012ummuawisyÎncă nu există evaluări
- MSQH Standards - PT Rights - KesedaranDocument33 paginiMSQH Standards - PT Rights - Kesedaranummuawisy100% (2)
- Whole Hospital Policy 011111Document43 paginiWhole Hospital Policy 011111ummuawisy100% (7)
- Accreditation Process - Chronic DialysisDocument1 paginăAccreditation Process - Chronic DialysisummuawisyÎncă nu există evaluări
- A2 Snakebite Management in Asia and AfricaDocument161 paginiA2 Snakebite Management in Asia and Africaummuawisy100% (1)
- Good Governance MedicineDocument27 paginiGood Governance MedicineummuawisyÎncă nu există evaluări
- Activities Patient SafetyDocument13 paginiActivities Patient SafetyummuawisyÎncă nu există evaluări
- 1 - Trial of Antivenom For Local Effects of Green Pit VipersDocument6 pagini1 - Trial of Antivenom For Local Effects of Green Pit VipersummuawisyÎncă nu există evaluări
- ABC Ven Analysis 2009Document59 paginiABC Ven Analysis 2009ummuawisy100% (6)
- A Brief Guide To Snake Envenomations in Malaysia and Antivenom Therapy (Edited)Document18 paginiA Brief Guide To Snake Envenomations in Malaysia and Antivenom Therapy (Edited)ummuawisyÎncă nu există evaluări
- 5 - Cross Neutralization of Neuro AntivenomDocument8 pagini5 - Cross Neutralization of Neuro AntivenomummuawisyÎncă nu există evaluări
- One StreamDocument14 paginiOne StreamAbdulghany Sulehria100% (1)
- ACCA AAA Audit Risk by Alan Biju PalakDocument18 paginiACCA AAA Audit Risk by Alan Biju Palakayush nandaÎncă nu există evaluări
- Testbank AIS - Chapter 1 (Hall) Testbank AIS - Chapter 1 (Hall)Document15 paginiTestbank AIS - Chapter 1 (Hall) Testbank AIS - Chapter 1 (Hall)HANNAH TUBLEÎncă nu există evaluări
- 2020 SHF Operational Manual FINALDocument57 pagini2020 SHF Operational Manual FINALHassan SamiÎncă nu există evaluări
- A (1083) Supplier QualificationDocument7 paginiA (1083) Supplier QualificationDharmesh Patel100% (1)
- Current Developments in Accounting TheoryDocument8 paginiCurrent Developments in Accounting TheorySheirgene NgÎncă nu există evaluări
- Curriculum Vitae: Ehrar-Ul-Haq Qa/Qc-Manager Aramco SAP #70005313Document6 paginiCurriculum Vitae: Ehrar-Ul-Haq Qa/Qc-Manager Aramco SAP #70005313Md ShariqueÎncă nu există evaluări
- ProfileDocument6 paginiProfilenemoo80 nemoo90Încă nu există evaluări
- SGV - E - Accounts Receivables, Trade - October 2015Document3 paginiSGV - E - Accounts Receivables, Trade - October 2015Christian Dela CruzÎncă nu există evaluări
- Professional Resume FormatDocument3 paginiProfessional Resume FormatsankalpadixitÎncă nu există evaluări
- Modul Auditing Ch08 Materiality Decisions and Performing Analytical ProceduresDocument19 paginiModul Auditing Ch08 Materiality Decisions and Performing Analytical ProceduresDanik Astutik PageÎncă nu există evaluări
- Proposal - Training For Bangladesh Government Officials 2Document7 paginiProposal - Training For Bangladesh Government Officials 2Mohd Zaki Mohd YaacobÎncă nu există evaluări
- Integrated Management Systems Assessment A Maturity Model ProposalDocument11 paginiIntegrated Management Systems Assessment A Maturity Model ProposalVíctor Alex OrtizÎncă nu există evaluări
- 16th Annual Report APSPDCLDocument137 pagini16th Annual Report APSPDCLdfÎncă nu există evaluări
- Audit Verification ProformaDocument9 paginiAudit Verification ProformaBilal ZulfiqarÎncă nu există evaluări
- HEC Financial Rules - 2009Document23 paginiHEC Financial Rules - 2009Shahid Malik0% (1)
- My Project Effect of Financial Statement Fraud On Organisational Performance A Case Study of Selected Deposit Money Banks in NigeriaDocument92 paginiMy Project Effect of Financial Statement Fraud On Organisational Performance A Case Study of Selected Deposit Money Banks in NigeriaRock KimÎncă nu există evaluări
- Its Pmo CharterDocument10 paginiIts Pmo CharterRakesh SharmaÎncă nu există evaluări
- Lambers Cpa Review AuditDocument589 paginiLambers Cpa Review AuditZedge100% (4)
- Control GuidanceDocument22 paginiControl GuidanceJonahtanÎncă nu există evaluări
- WTIA Vs WA Department of Labor & IndustriesDocument31 paginiWTIA Vs WA Department of Labor & IndustriesGeekWireÎncă nu există evaluări
- Final of Final Response To NBE's ExaminersDocument108 paginiFinal of Final Response To NBE's Examinersdaniel nugusieÎncă nu există evaluări
- The Impact of XBRL On Financial Reporting: A Conceptual AnalysisDocument8 paginiThe Impact of XBRL On Financial Reporting: A Conceptual AnalysisChima EmmanuelÎncă nu există evaluări
- MODAUD1 UNIT 5 Audit of Biological Assets PDFDocument5 paginiMODAUD1 UNIT 5 Audit of Biological Assets PDFMjoyce A. BruanÎncă nu există evaluări
- Enron ScandalDocument39 paginiEnron ScandalhomsomÎncă nu există evaluări
- Assignment AccountingDocument12 paginiAssignment AccountingAslamJaved68Încă nu există evaluări
- Management Accounting: Made By: Nalin Bba 2 YrDocument12 paginiManagement Accounting: Made By: Nalin Bba 2 YrSahil BeighÎncă nu există evaluări
- Saint Mary's University Financial DisclosureDocument4 paginiSaint Mary's University Financial DisclosureThe Chronicle HeraldÎncă nu există evaluări
- Hap GuideDocument249 paginiHap GuideBaleegh Al-sharabyÎncă nu există evaluări
- Risk Based Approach To ValidationDocument6 paginiRisk Based Approach To ValidationAlex CristiÎncă nu există evaluări