Documente Academic
Documente Profesional
Documente Cultură
Jurnal Entamoeba
Încărcat de
Enggartika MaharaniDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Jurnal Entamoeba
Încărcat de
Enggartika MaharaniDrepturi de autor:
Formate disponibile
Fadeyi et al Antigen Detection of E.
histolytica
Int J Health Res, June 2009; 2(2): 169
Reprinted from
International Journal
of of of of
Health Research
Peer-reviewed Online Journal
http://www.ijhr.org
Abstracting/Indexing
African Index Medicus, Open-J-Gate, Directory of Open Access Journals (DOAJ), Socolar,
EBSCO, Index Corpenicus, Embase
Fadeyi et al Antigen Detection of E. histolytica
Int J Health Res, June 2009; 2(2): 170
International Journal of Health Research
The International Journal of Health Research is an online international journal allowing free unlimited access to
abstract and full-text of published articles. The journal is devoted to the promotion of health sciences and related
disciplines (including medicine, pharmacy, nursing, biotechnology, cell and molecular biology, and related
engineering fields). It seeks particularly (but not exclusively) to encourage multidisciplinary research and
collaboration among scientists, the industry and the healthcare professionals. It will also provide an international
forum for the communication and evaluation of data, methods and findings in health sciences and related
disciplines. The journal welcomes original research papers, reviews and case reports on current topics of special
interest and relevance. All manuscripts will be subject to rapid peer review. Those of high quality (not previously
published and not under consideration for publication) will be published without delay. The maximum length of
manuscripts should normally be 10,000 words (20 single-spaced typewritten pages) for review, 6,000 words for
research articles, 3,000 for technical notes, case reports, commentaries and short communications.
Submission of Manuscript: The International Journal of Health Research uses a journal management
software to allow authors track the changes to their submission. All manuscripts must be in MS Word and in
English and should be submitted online at http://www.ijhr.org. Authors who do not want to submit online or
cannot submit online should send their manuscript by e-mail attachment (in single file) to the editorial office
below. Submission of a manuscript is an indication that the content has not been published or under consideration for
publication elsewhere. Authors may submit the names of expert reviewers or those they do not want to review their papers.
Enquiries: Enquiries: Enquiries: Enquiries:
The Editorial Office
International Journal of Health Research
Deans Office, College of Medicine
Madonna University, Elele Campus, Rivers State
E-mail: editor_ijhr@yahoo.com or editor@ijhr.org
PORACOM
Academic Publishers
Fadeyi et al Antigen Detection of E. histolytica
Int J Health Res, June 2009; 2(2): 171
International Journal of Health Research, June 2009; 2(2): 171-175 (e229p67-71)
Poracom Academic Publishers. All rights reserved.
Available at http://www.ijhr.org
Original Research Article
Antigen Detection of Entamoeba Histolytica Intestinal
Infection: Cost-Associated Challenge in a Resource
Poor Country
Received: 02-Mar-09 Revised: 17-Mar-09 Accepted: 21-Mar-09
Abstract
Purpose: Laboratory diagnosis of Entamoeba
histolytica infection is still being made through
compound light microscopy in resource limited
countries despite the associated flaws. This study is
aimed at applying and determining the usefulness of
ELISA antigen detection technique for E. histolytica
intestinal infection diagnosis in a resource poor nation.
Methods: A total of 150 subjects with acute and
persistent diarrhoea had their stool specimens
examined by compound light microscopy for E.
histolytica/dispar and other intestinal parasites. Ninety-
four of them (62.67%) had their stool specimens
examined with ELISA antigen detection for E.
histolytica
Results: Two (1.33%) of the subjects were positive for
E. histolytica/ dispar on microscopy but none was
positive for E. histolytica by ELISA antigen detection.
Subjects positive by microscopy were identified as E.
dispar (1.33%) carriers.
Conclusion: ELISA antigen detection technique is a
preferred method of detection of parasites even in
resource poor settings to avoid confusing results. At
present, the best use of E. histolytica II kit in resource
poor nations should be limited to screening of E.
histolytic/dispar microscopically positive stool samples
for E. histolytica infection.
Keywords: Amoebasis; Antigen detection; ELISA;
Entamoeba histolytica; Laboratory diagnosis; Nigeria.
Abayomi Fadeyi *
Charles Nwabuisi
Boaz Adegboro
Department of Medical Microbiology and
Parasitology, Faculty of Basic Medical
Sciences, College of Medicine, University of
Ilorin, PMB 1515, Ilorin, Nigeria.
*For Correspondence:
Email: abayomifadeyi@yahoo.com
Open Access
Online Journal
e229p67
Fadeyi et al Antigen Detection of E. histolytica
Int J Health Res, June 2009; 2(2): 172
Introduction
Entamoeba histolytica, the causative agent
of amoebaisis, is believed to infect more than
10% of the worlds population with majority of
infection occurring in the developing world
[1,2]. The parasite has been reported as the
third major cause of death attributable to
parasitic infections globally, after malaria and
schistosomiasis [2,3]. However, the
diagnosis of intestinal amoebiasis, the first
stage of multi-systemic disease caused by E.
histolytica, is plagued with many challenges.
In Nigeria, laboratory diagnosis of intestinal
amoebiasis is often based on compound
microscopy which does not accurately detect
the amoeba species [4]. As of 1997, it was
officially accepted by the World Health
Organization
(WHO) that E. histolytica sensu
lato is composed of two
morphologically
identical species: the pathogenic E.
histolytica
sensu stricto and the non-
pathogenic (but very common) Entamoeba
dispar [5]. These
two parasites cannot be
correctly distinguished under compound
microscopy
alone unless the trophozoites of
E. histolytica are seen engulfing
red blood
cells (heamatophagous trophozoites) [4].
Even though, the identification of
heamatophagous trophozoite on compound
microscopy is considered diagnostic, it is
practically a rare finding and occurs mainly in
acute dysentery [4,5].
Alternative diagnostic and specific
approaches for amoebiasis had since been
developed and these include enzyme linked
immunosorbent assay (ELISA) antigen
detection technique; culture followed by
isoenzyme analysis on electrophoresis and
polymerase chain reaction (PCR) based
techniques [4]. None of these new
approaches is currently being used in
Nigeria. The aim of this work therefore is to
apply and determine the usefulness of ELISA
antigen detection technique for E. histolytica
intestinal infection diagnosis among patients
with diarrhoea in a resource poor nation like
Nigeria.
Patients and Methods
Patients
This study was conducted at the University
of Ilorin Teaching hospital (UITH), Ilorin,
Nigeria between December 2005 and May
2007. The study was approved by the Ethical
review committee of UITH, Ilorin. All
consenting patients presenting to the various
hospitals within the Ilorin metropolis with
acute and persistent diarrhoea or dysentery
within the period of study were enlisted.
Patients with chronic diarrhoea and those on
antimicrobials, antacids, laxative, soap and
water enema within a two week period from
the sampling or those who have just
completed investigation with barium
meal/enema were excluded from the study.
Stool samples reaching the laboratory after
two hours of collection were also not
processed. The age and sex of patients were
noted at the time of recruitment.
Single stool specimen was collected in a
clean, dry, wide neck, sterile bottle from each
of the participant and was divided into two
parts. One part of the specimen for diagnosis
by ELISA antigen detection was preserved at
-20
o
C until analysis, while the one for
microscopy was processed immediately.
Methods
To a drop of normal saline on a microscope
slide, was suspended a small amount of the
stool specimen and was covered with cover
slip. This was examined under a compound
light microscope first under x10 objective
lens and then under x 40 objective whose
stage had been warmed with a 60 watt bulb
for at least one min.
The stool sample was concentrated by the
sedimentation technique using formol-ethyl
acetate method [7]. A drop of the sediment
obtained was examined in a drop of 2%
iodine for cysts of E. histolytica. Cysts, ova
and larvae of other intestinal parasites were
also sought for and identified using diagrams
in the image library of DPDx CD on
e229p68
Fadeyi et al Antigen Detection of E. histolytica
Int J Health Res, June 2009; 2(2): 173
Laboratory Diagnosis of Parasitic Diseases
by Centre for Disease Control and
Prevention, USA [8].
The E. histolytica enzyme linked immuno-
sorbent assay (ELISA) based antigen
detection kit (E. histolytica II) made by
TechLab (USA) was used according to
manufacturers instructions. The kit is based
on monoclonal antibody-peroxidase
conjugate specific for E. histolytica adhesin.
According to the manufacturer, a positive
result is recorded if optical density of >0.05 is
obtained after subtracting the negative
control optical density.
A total of 150 specimens were collected and
all examined microscopically, while 94
randomly selected stool specimens,
including the ones positive for E. histolytica/
dispar on microscopy, were examined with
ELISA antigen detection method obtained
from USA. Only 62.67% of the patients had
their stool screened for E. histolytica with
ELISA antigen detection kit due to cost
associated factor as it takes about N2,000.00
(approximately $14.00) to process a single
stool. The cost of obtaining in Nigeria an
ELISA antigen detection kit is about
N146,000 (approximately US$1000.00).
The data collected were presented using
descriptive statistics.
Results
By microscopy, only 2 (1.33%) of the
patients were positive for E. histolytica/
dispar. None of the patients was positive for
E. histolytica by ELISA antigen detection
technique implying that the prevalence of E.
dispar was 1.33%.
Other intestinal parasites seen in the stool of
some patients are presented in Table 1. The
overall level of intestinal parasitic infection
was 9.33%. Ascaris lumbricoides (5.33%)
was the most predominant intestinal parasite
seen. Schistosoma mansoni and hookworm
were seen in 0.67% and 1.33% of the
patients, respectively. Mixed infections were
found in 0.67% with A. lumbricoides and
hookworm being responsible for the co-
infection. Intestinal parasitosis among the
male and female patients with diarrhoea
were found mainly among those aged 10
years and below (Table 2).
Discussion
In developing countries, diagnosis of E.
histolytica infections remains unsatisfactory
largely because of the inadequacies of the
laboratory methods readily available. The
most commonly used method is microscopy
which had resulted in various prevalence
rates in different localities and even within
the same region over time [9-11]. In this
study, only 1.33% of the patients were
positive for E. histolytica/dispar using
microscopy. The use ELISA antigen based
diagnostic method has made it possible to
detect that the microscopy result was indeed
inaccurate as none of the patients was
positive for E. histolytica. This result is an
indication that the frequent reliance on
microscopy for diagnosis of amoebiasis in
resource poor settings like the situation in
Nigeria could often lead to wrong diagnosis.
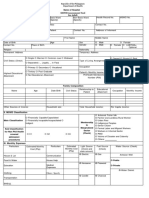
Table 1: Intestinal parasites seen in the stool specimens of patients with diarrhoea in Ilorin, Nigeria
Parasite type Number positive Rate (%)
Ascaris lumbricoides
Hookworm
Schistosoma mansoni
Ascaris lumbricoides + Hookworm
Entamoeba hisolytica/dispar
8
2
1
1
2
5.33
1.33
0.67
0.67
1.33
Total 14 9.33
n=150
e229p69
Fadeyi et al Antigen Detection of E. histolytica
Int J Health Res, June 2009; 2(2): 174
Table 2: Age and sex related occurrence of intestinal parasites in the
stool specimens of patients with diarrhoea in Ilorin, Nigeria
Male Diarrhoea Patients Female Diarrhoea Patients
Age range
(years)
Number
examined
Number infected with
parasites (%)
Number
examined
Number infected with
parasites (%)
<1 8 2 (3.03) 9 3 (3.57)
1-5 54 1 (1.52) 26 2 (2.38)
6-10 47 2 (3.03) 25 1 (1.19)
11-15 16 0 (0.00) 34 1 (1.19)
16-20 15 0 (0.00) 42 1 (1.19)
>20 10 0 (0.00) 14 1 (1.19)
Total 66 5 (7.58) 84 9 (10.71)
The inaccurate diagnosis of amoebiasis
based on microscopy results has been
documented in different studies. In a study
conducted in North Eastern
Brazil, 4.1% of
patients were positive for E. histolytica/dispar
with microscopy but with both PCR and
antigen immunoenzymatic
assay, none (0%)
was positive for E. histolytica [12]. In another
study conducted in Bangladesh, out of 98
patients with diarrhoea, 88 were diagnosed
to be infected with E. histolytica by
microscopy but only 53 were positive by
isoenzyme analysis and 45 (85%) out of
these were positive by the ELISA antigen
detection method [13]. Another study in
Bangladesh also showed that, out of 202
diarrhoea patients whose stool samples were
examined by microscopy, 69 were positive
for E. histolytica while 106 were negative.
However, of the 69 positive stool specimens
by microscopy for E. histolytica, only 56 were
positive with ELISA antigen detection
method [14]. Similarly, 2 out of 106 negative
stool samples for E. histolytica by
microscopy were positive with ELISA antigen
detection method with the results of ELISA
correlating well with the gold standard
(culture followed by isoenzyme analysis).
To the best of our knowledge, there are no
reported studies in Nigeria yet where ELISA
antigen detection method or other molecular
techniques had been used to diagnose
amoebiasis for comparison. Nonetheless,
from the present study and others cited
above, more patients are often positive by
microscopy than with ELISA and other
methods adjudged more precise than
microscopy for E. histolytica. This is probably
because of the wrong identification of other
Entamoeba species and white blood cells as
E. histolytica with microscopic method [4].
This result therefore shows that most
patients treated for amoebiasis based on
microscopic diagnosis actually required no
treatment hence, the need to shift to the use
of ELISA antigen detection method and
probably, PCR for diagnosis of E. histolytica
by developing countries who already do not
do so.
The high cost however of using ELISA
antigen based technique for diagnosis of E.
histolytica is a major challenge in resource
poor countries. To buy and ship a tray of
ELISA antigen detection kit used in this study
to Nigeria cost about N146,000 (approx-
imately $1,000.00) and by extension, an
already impoverished patient may need to
pay about N3000 (approximately $21.00) for
a single stool examination. The cost of this
procedure probably also explain the reason
why this type of study has never been
reported in this country. Therefore the
support of government and non-
governmental agencies in reducing the cost
of ELISA antigen detection kit is highly
advocated as a cheap and readily available
kit would result in routine specimen testing
thereby enhancing the quality of medical
care and indirectly, the quality of life of the
citizenry. Until this is done, the best use of E.
e229p70
Fadeyi et al Antigen Detection of E. histolytica
Int J Health Res, June 2009; 2(2): 175
histolytica II kit in resource poor nations
should be limited to screening of E.
histolytic/dispar microscopically positive stool
samples for E. histolytica infection among
patients that can afford the cost of this test.
Conclusion
The use of microscopy in the diagnosis of
amoebiasis in resource poor settings often
leads to wrong diagnosis and hence wrong
treatment. ELISA antigen detection
technique correctly diagnoses amoebiasis
and prevents the confusing result from
microscopy that cannot specifically
differentiate E. histolytica from E. dispar.
However, the cost of each test is too
expensive for most patients in Nigeria.
It is recommended that at present, the best
use of E. histolytica II kit in resource poor
nations should be limited to screening of E.
histolytic/dispar microscopically positive stool
samples for E. histolytica infection.
References
1. Stanley, S. L., Jr. Amoebiasis. Lancet. 2003;
361:10251034.
2. Radvin JI, Petri WA. Entamoeba histolytica
(Amebiasis). In: Mandel GL, Bennett JE, Dolin R.
Principles & Practice of infectious diseases (4
th
Edition) CLS. 1995; 2395 - 2408.
3. Smith LA. Diagnostic parasitology In: Textbook of
diagnostic microbiology edited by Connie RM,
George M Jr., W. B. Saunders Company. 1995;
733-793
4. Tanyuksel M, Petri WA, Jr. Laboratory Diagnosis
of Amebiasis. Clin. Micro. Rev. 2003; 16: 713729.
5. World Health Organization. Amoebiasis. Wkly.
Epidemiol. Rec. 1997; 72:97-100.
6. Kebede, A., J. J. Verweij, B. Petros, and T.
Polderman. Misleading microscopy in amoebiasis.
Trop. Med. Int. Health. 2004; 9:651-652.
7. Monica Cheesbrough. Distric laboratory practice in
tropical coutries. Cambridge University press.1998;
196-198.
8. Center for Disease Control and Prevention,
National Center for Infectious Diseases, Division of
Parasitic Diseases. Amoebiasis. In DPDx CD for
Laboratory Diagnosis of Parasitic Diseases
Emphasizing Intestinal and Food borne Parasite:
2001.
9. Alakpa GE, Fagbenro-Beyioku AF. Cyclospora
cayetanensis and intestinal parasitic profile in stool
samples in Lagos, Nigeria. Acta Protozool. 2002;
41: 221 227.
10. Agi IA. Pattern of intestinal infection in Sagbama
community of Niger Delta, Nigeria. W. Afric. J.
Med. 1995;14 (1): 39-42.
11. Ozumba UC, Ozumba NA, Anya S. Helminthiasis
in pregnancy in Enugu, Nigeria. J. Health Sc. 2005;
51 (3): 291-293.
12. Sandra MB, Pinheiro RM, Carneiro IS, Aca JI,
Irmo MAM Jr, Maria RMC, Luiz BC Jr.
Determination of the prevalence of Entamoeba
histolytica and E. dispar in the Pernambuco State
of Northeastern Brazil by a polymerase chain
reaction. Am J Trop Med Hyg. 2004; 70(2): 221-
224.
13. Haque R, Ali IKM, Akther S, Petri WA Jr.
Comparisom of PCR, Isoenzyme analysis and
antigen detection for diagnosis of Entamoeba
histolytica infection J. Clin. Microbiol: 1998; 36:
449 - 452.
14. Blessmann J, Buss H, Ton Nu PA, Dinh BT, Viet
Ngo QT, Van AL, Abd Alla MD, Jackson TFHG,
Ravdin JI, Tannich
E. Real -Time PCR for detection
and differentiation of Entamoeba histolytica and
Entamoeba dispar in fecal samples. J. Clin. Micro.
2000; 40:12: 4413 -4417.
e229p71
Fadeyi et al Antigen Detection of E. histolytica
Int J Health Res, June 2009; 2(2): 176
e229p72
S-ar putea să vă placă și
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Pencarrow Lighthouse Conservation PlanDocument98 paginiPencarrow Lighthouse Conservation PlanClarice Futuro MuhlbauerÎncă nu există evaluări
- Calculation in ApheresisDocument5 paginiCalculation in Apheresismilica cucuzÎncă nu există evaluări
- Unit4 Planning For A Health CareerDocument76 paginiUnit4 Planning For A Health CareerkitcathÎncă nu există evaluări
- Rule 11: OR Exactly How Crazy Do I Need To Act To Get Out of Here?Document56 paginiRule 11: OR Exactly How Crazy Do I Need To Act To Get Out of Here?Joshua Ling100% (2)
- The 2030 Agenda For Sustainable Development and The "Five PS"Document2 paginiThe 2030 Agenda For Sustainable Development and The "Five PS"Laraib ShahidÎncă nu există evaluări
- Hbsag Form New 2021Document1 paginăHbsag Form New 2021GCMDHÎncă nu există evaluări
- Manual For Doctors To Evaluate Permanent Physical ImpairmentDocument33 paginiManual For Doctors To Evaluate Permanent Physical Impairmentyuvrajavi100% (1)
- KKP Mpu3022Document4 paginiKKP Mpu3022Zulbasim ZiyadÎncă nu există evaluări
- ICCD Power Point 2015Document16 paginiICCD Power Point 2015OhioOhioÎncă nu există evaluări
- How To Write Clinical Learning ObjectivesDocument1 paginăHow To Write Clinical Learning ObjectivesNick MacaballugÎncă nu există evaluări
- (1998) Chronic Disease Management What Will It Take To Improve Care For Chronic IllnessDocument3 pagini(1998) Chronic Disease Management What Will It Take To Improve Care For Chronic IllnessDaniel MeloÎncă nu există evaluări
- REFERAT Koass Neurologi - Carpal Tunnel SyndromeDocument34 paginiREFERAT Koass Neurologi - Carpal Tunnel SyndromeVindhita RatiputriÎncă nu există evaluări
- A Practical Approach To Nutrition, Protein-Energy Wasting, Sarcopenia, and Cachexia in Patients With Chronic Kidney DiseaseDocument10 paginiA Practical Approach To Nutrition, Protein-Energy Wasting, Sarcopenia, and Cachexia in Patients With Chronic Kidney DiseasevhnswrÎncă nu există evaluări
- Analysis and Design of Concrete StructuresDocument614 paginiAnalysis and Design of Concrete StructuresLinda MadlalaÎncă nu există evaluări
- Medium ComDocument6 paginiMedium ComrsadÎncă nu există evaluări
- Missed ABMP Exam Questions With Correct AnswersDocument37 paginiMissed ABMP Exam Questions With Correct Answersgkim58646Încă nu există evaluări
- EpilepsyDocument24 paginiEpilepsysalmanhabeebek100% (2)
- Lab1ESR 08Document11 paginiLab1ESR 08Muhamad AfidinÎncă nu există evaluări
- Adult Mswd-ToolDocument3 paginiAdult Mswd-Toolclaverialc10Încă nu există evaluări
- TZ Dairy Industry FAODocument46 paginiTZ Dairy Industry FAOKai GwalandaÎncă nu există evaluări
- Circles of SupportDocument1 paginăCircles of Supportapi-276867030Încă nu există evaluări
- Own: ICARUS Training Services Safety Briefing/ Attendance FormDocument2 paginiOwn: ICARUS Training Services Safety Briefing/ Attendance FormTim Brown0% (1)
- English 10 Questionnaire 3rd QuarterDocument7 paginiEnglish 10 Questionnaire 3rd QuarterklimbaroÎncă nu există evaluări
- Jones, Julia - Basic Yoga For Busy People - 3 Books in 1 - Illustrated Yoga Poses + Easy Yoga Classes To Reduce Body Fat and Eliminate Stress + Yoga Fitness Journal (2021)Document110 paginiJones, Julia - Basic Yoga For Busy People - 3 Books in 1 - Illustrated Yoga Poses + Easy Yoga Classes To Reduce Body Fat and Eliminate Stress + Yoga Fitness Journal (2021)dilaylaÎncă nu există evaluări
- CYD DUPONT CASE - Motion For Class Certification Chemours 05182022Document58 paginiCYD DUPONT CASE - Motion For Class Certification Chemours 05182022zblackx2023Încă nu există evaluări
- Diagnostic Centers MOU FormDocument5 paginiDiagnostic Centers MOU FormMuhammad Usman Ghani100% (1)
- Mental HealthDocument31 paginiMental HealthGelo Angeles100% (1)
- Drug Presentation AtropineDocument6 paginiDrug Presentation AtropineShivam Malik100% (1)
- 10 Simulation Exercises As A Patient Safety Strategy PDFDocument9 pagini10 Simulation Exercises As A Patient Safety Strategy PDFAmanda DavisÎncă nu există evaluări
- The Merciad, April 14, 1988Document8 paginiThe Merciad, April 14, 1988TheMerciadÎncă nu există evaluări