Documente Academic
Documente Profesional
Documente Cultură
Clinical Prediction Rule To Identify Patients Likely To Responde To Lumbar Spine Stabilization Exercisess: A Randomized Controlled Validation Study
Încărcat de
SamSchroetkeTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Clinical Prediction Rule To Identify Patients Likely To Responde To Lumbar Spine Stabilization Exercisess: A Randomized Controlled Validation Study
Încărcat de
SamSchroetkeDrepturi de autor:
Formate disponibile
6 | january 2014 | volume 44 | number 1 | journal of orthopaedic & sports physical therapy
L
ow back pain (LBP) is
common among the general
population, with a lifetime
prevalence and point pre-
valence estimated to be greater
than 80% and 28%, respectively.
12
Although short-term outcomes are gen-
erally favorable, some patients go on to
experience long-term pain and disabil-
ity,
32,40,78
and recurrence rates are high.
17,78
Systematic reviews of various physi-
cal therapy interventions for LBP do not
provide strong support for any particu-
lar treatment approach.
2,50,51,77
One pos-
sible reason is the use of heterogeneous
samples of patients in many clinical trials
for LBP. Patients with LBP demonstrate
both etiologic and prognostic hetero-
geneity,
7,40,45
which makes it unlikely for
any single intervention to have a signi-
cant advantage over another in a general
population with LBP. Classifying patients
into more homogeneous subgroups has
been previously identied as a top re-
TSTUDY DESIGN: Randomized controlled trial.
TOBJECTIVE: To determine the validity of a
previously suggested clinical prediction rule (CPR)
for identifying patients most likely to experience
short-term success following lumbar stabilization
exercise (LSE).
TBACKGROUND: Although LSE is commonly
used by physical therapists in the management
of low back pain, it does not seem to be more
efective than other interventions. A 4-item CPR
for identifying patients most likely to benet from
LSE has been previously suggested but has yet to
be validated.
TMETHODS: One hundred ve patients with
low back pain underwent a baseline examination
to determine their status on the CPR (positive or
negative). Patients were stratied by CPR status
and then randomized to receive an LSE program
or an intervention consisting of manual therapy
(MT) and range-of-motion/exibility exercises.
Both interventions included 11 treatment sessions
delivered over 8 weeks. Low back painrelated
disability was measured by the modied version of
the Oswestry Disability Index at baseline and upon
completion of treatment.
TRESULTS: The statistical signicance for the
2-way interaction between treatment group and
CPR status for the level of disability at the end
of the intervention was P = .17. However, among
patients receiving LSE, those with a positive CPR
status experienced less disability by the end of
treatment compared with those with a nega-
tive CPR status (P = .02). Also, among patients
with a positive CPR status, those receiving LSE
experienced less disability by the end of treatment
compared with those receiving MT (P = .03). In
addition, there were main efects for treatment and
CPR status. Patients receiving LSE experienced
less disability by the end of treatment compared to
patients receiving MT (P = .05), and patients with
a positive CPR status experienced less disability
by the end of treatment compared to patients with
a negative CPR status, regardless of the treatment
received (P = .04). When a modied version of
the CPR (mCPR) containing only the presence of
aberrant movement and a positive prone instability
test was used, a signicant interaction with treat-
ment was found for nal disability (P = .02). Of the
patients who received LSE, those with a positive
mCPR status experienced less disability by the end
of treatment compared to those with a negative
mCPR status (P = .02), and among patients with
a positive mCPR status, those who received LSE
experienced less disability by the end of treatment
compared to those who received MT (P = .005).
TCONCLUSION: The previously suggested CPR
for identifying patients likely to benet from LSE
could not be validated in this study. However, due
to its relatively low level of power, this study could
not invalidate the CPR, either. A modied version
of the CPR that contains only 2 items may possess
a better predictive validity to identify those most
likely to succeed with an LSE program. Because
this modied version was established through post
hoc testing, an additional study is recommended
to prospectively test its predictive validity.
TLEVEL OF EVIDENCE: Prognosis, level 1b. J
Orthop Sports Phys Ther 2014;44(1):6-18. Epub 21
November 2013. doi:10.2519/jospt.2014.4888
TKEY WORDS: lumbar spine, manual therapy
1
Department of Physiotherapy, Ariel University, Ariel, Israel.
2
Bat-Yamon Physical Therapy Clinic, Clalit Health Services, Israel.
3
Giora Physical Therapy Clinic, Clalit Health
Services, Israel.
4
Department of Physical Therapy, Faculty of Social Welfare and Health Sciences, University of Haifa, Haifa, Israel. This study was approved by the Helsinki
Committee of Clalit Health Services. The authors certify that they have no afliations with or nancial involvement in any organization or entity with a direct nancial interest
in the subject matter or materials discussed in the article. Address correspondence to Dr Alon Rabin, Ariel University, Department of Physiotherapy, Kiryat Hamada, PO Box 3,
Ariel, Israel. E-mail: alonrabin@gmail.com T Copyright 2014 Journal of Orthopaedic & Sports Physical Therapy
ALON RABIN, DPT, PhD
1
ANAT SHASHUA, BPT, MS
2
KOBY PIZEM, BPT
3
RUTHY DICKSTEIN, PT, DSc
4
GALI DAR, PT, PhD
4
A Clinical Prediction Rule to Identify
Patients With Low Back Pain Who Are
Likely to Experience Short-Term Success
Following Lumbar Stabilization Exercises:
A Randomized Controlled Validation Study
[ RESEARCH REPORT ]
44-01 Rabin.indd 6 12/17/2013 5:18:33 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
journal of orthopaedic & sports physical therapy | volume 44 | number 1 | january 2014 | 7
search priority,
6
and, in fact, more recent
research has suggested that matching pa-
tients with interventions based on their
specic clinical presentation may yield
improved clinical outcomes.
8,10,15,27,47
Structural as well as functional
impairments, such as decreased and
delayed activation of the transversus ab-
dominis and atrophy of the lumbar mul-
tidus,
25,34,37,48,69,80
have been identied
among patients with LBP. These impair-
ments may result in a reduction in spinal
stifness
82
and possibly render the spine
more vulnerable to excessive deforma-
tion and pain. Lumbar stabilization ex-
ercises (LSE) attempt to address these
impairments by retraining the proper
activation and coordination of trunk
musculature.
58,64
Stabilization exercises
are widely used by physical therapists in
the management of LBP.
8,11,22,24,35,44,49,50,62,65
Although some evidence exists to support
the remediating efects of LSE on some
of the muscle impairments identied in
patients with LBP,
36,73,74
the clinical ef-
cacy of this intervention seems to vary.
When compared to sham or no interven-
tion, LSE appears to be advantageous
22,65
;
however, when compared to other exer-
cise interventions or to manual therapy
(MT), no denitive advantage has been
ascertained.
11,24,35,44,49,50,62,75
In light of the variable clinical suc-
cess of LSE and in accordance with the
aforementioned need to classify patients
who have LBP into more homogeneous
subgroups, Hicks et al
33
suggested a clini-
cal prediction rule (CPR) to specically
identify patients with LBP who are likely
to exhibit short-term improvement with
LSE. Four variables were found to pos-
sess the greatest predictive power for
treatment success: (1) age less than 40
years, (2) average straight leg raise (SLR)
of 91 or greater, (3) the presence of aber-
rant lumbar movement, and (4) a positive
prone instability test.
33
When at least 3
of the 4 variables were present, the posi-
tive likelihood ratio for achieving a suc-
cessful outcome was 4.0, increasing the
probability of success from 33% to 67%.
33
The study by Hicks et al
33
comprises the
rst stage in establishing a CPR, the deri-
vation stage.
4,14,55
Following derivation, a
CPR must be validated, that is, shown to
consistently predict the outcome of inter-
est in a separate and preferably prospec-
tive investigation.
26
Given its preliminary
nature, and because CPRs do not typi-
cally perform as well on new samples of
patients,
21,30,67,68
modication of the CPR
may also be necessary to achieve satisfac-
tory predictive validity. Once validated,
CPRs can move into the nal stage of
their determination, which includes an
investigation into their impact on clini-
cal practice (impact analysis).
4,14,55
Validation of the CPR for LSE re-
quires a randomized controlled trial in
which patients with a diferent status on
the CPR (positive or negative) undergo
an LSE program, as well as a comparison
intervention.
4
The use of a comparison
intervention is important to determine
whether the CPR can truly identify pa-
tients who will benet specically from
LSE, as opposed to patients who have a
favorable prognosis irrespective of the
treatment received.
66
Finally, to validate
the CPR in the most clinically meaning-
ful manner, we believe that the compari-
son intervention should be considered a
viable alternative to LSE, rather than a
sham or an inert intervention.
Manual therapy is an intervention fre-
quently used by physical therapists in the
management of patients with LBP
39,46,56
and is recommended by several clinical
practice guidelines and systematic reviews
for the management of acute, subacute,
and chronic LBP.
1,9,19,76
These factors, com-
bined with the fact that LSE programs
have previously demonstrated varied
levels of success compared to MT,
11,24,50,62
suggest that MT may be a suitable com-
parison intervention for testing the validi-
ty of the CPR. In contrast to its use among
heterogeneous samples,
11,24,50,62
LSE
should demonstrate a clearer advantage
among patients with LBP who also satisfy
the CPR, if the CPR accurately identies
the correct target patient population.
The purpose of this investigation was
to determine the validity of, or to possibly
modify, the previously suggested CPR for
identifying patients most likely to benet
from LSE. We hypothesized that among
patients receiving LSE, those with a posi-
tive CPR status would exhibit a better
outcome compared to those with a nega-
tive CPR status. We also hypothesized
that among patients with a positive CPR
status, those who received LSE would ex-
hibit a better outcome compared to those
who received MT.
METHODS
Patients
O
ne hundred ve patients diag-
nosed with LBP and referred to
physical therapy at 1 of 5 outpa-
tient clinics of Clalit Health Services in
the Tel-Aviv metropolitan area, Israel,
were recruited for this study. Subjects
were included if they were 18 to 60 years
of age, had a primary complaint of LBP
with or without associated leg symptoms
(pain, paresthesia), and had a minimum
score of 24% on the Hebrew version of
the modied Oswestry Disability Index
(MODI) outcome measure. Patients
were excluded if they presented with a
history suggesting any red ags (eg, ma-
lignancy, infection, spine fracture, cauda
equina syndrome); 2 or more signs sug-
gesting lumbar nerve root compression,
such as decreased deep tendon reexes,
myotomal weakness, decreased sensation
in a dermatomal distribution, or a posi-
tive SLR, crossed SLR, or femoral nerve
stretch test; or a history of corticosteroid
use, osteoporosis, or rheumatoid arthri-
tis. Patients were also excluded if they
were pregnant, received chiropractic
or physical therapy care for LBP in the
preceding 6 months, could not read or
write in the Hebrew language, or had a
pending legal proceeding associated with
their LBP. Prior to participation, all pa-
tients signed an informed consent form
approved by the Helsinki Committee of
Clalit Health Services.
Therapists
Sixteen physical therapists were involved
44-01 Rabin.indd 7 12/17/2013 5:18:35 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
8 | january 2014 | volume 44 | number 1 | journal of orthopaedic & sports physical therapy
[ RESEARCH REPORT ]
in the study. Eleven therapists, with be-
tween 4 and 12 years of experience in
outpatient physical therapy patient care,
provided treatment, and 5 therapists,
with between 13 to 25 years of experi-
ence, performed baseline and follow-
up evaluations. Prior to beginning the
study, all participating therapists under-
went two 4-hour sessions in which the
rationale and protocol of the study were
presented and the examination and treat-
ment procedures were demonstrated and
practiced. Therapists had to pass a writ-
ten examination of the study procedures
prior to data collection. Finally, each
therapist received a manual describing
treatment and evaluation procedures,
based on the therapists role in the study
(treatment or evaluation). Therapists in-
volved in treating patients were unaware
of the concept of the CPR throughout the
study, to avoid bias from this knowledge
during treatment. All treating therapists
provided both treatments of the study
(LSE and MT).
Procedure
After giving consent, patients completed
a baseline examination that included de-
mographic information, an 11-point (0-
10) numeric pain rating scale (NPRS),
on which 0 was no pain and 10 was
the worst imaginable pain, the Hebrew
version of the MODI,
3,28
and the Hebrew
version of the Fear-Avoidance Beliefs
Questionnaire.
38,79
In addition, the his-
tory of the present and any past LBP
was documented, followed by a physical
examination.
The physical examination included a
neurological screen to rule out lumbar
nerve root compression; lumbar active
motion, during which the presence of ab-
errant movement, as dened by Hicks et
al,
33
was determined; bilateral SLR range
of motion; segmental mobility of the lum-
bar spine; and the prone instability test.
The patients status on the CPR (positive
or negative) was established based on the
ndings of the physical examination.
Examiners who performed the base-
line examinations, as well as examiners
who screened patients for eligibility to
participate in the study, were blinded to
the intervention allocation of the patients.
Reliability
The reliability of the individual physical
examination items comprising the CPR,
as well as that of the entire CPR, has been
reported previously.
60
In that study,
60
the
interrater reliability for determining CPR
status was excellent ( = 0.86), and the
interrater reliability of each of the items
comprising the CPR ranged from moder-
ate to substantial ( = 0.64-0.73).
60
Randomization
At the conclusion of the physical exami-
nation, each patient was randomized to
receive LSE or MT. Randomization was
based on a computer-generated list of
random numbers, stratied by CPR status
to ensure that adequate numbers of pa-
tients with a positive and a negative CPR
status would be included in each interven-
tion group. The list was kept by a research
assistant who was not involved in patient
recruitment, examination, or treatment.
Intervention
Patients in both groups received 11 treat-
ment sessions over an 8-week period.
Each patient was seen twice a week dur-
ing the rst 4 weeks, then once a week
for 3 additional weeks. A 12th session
(usually on the eighth week) consisted
of a nal evaluation. The total number
of sessions (12) matched the maximum
number of physical therapy visits allowed
annually per condition under the policy
of the Clalit Health Services health main-
tenance organization, which covered all
patients participating in the study. Pa-
tients in both groups were prescribed a
home exercise program consistent with
their treatment group; however, no at-
tempt was made to monitor patients
compliance with the home exercise
program.
Lumbar Stabilization Exercises
The LSE program was largely based on
the program described by Hicks et al,
33
with a few minor changes in the order of
the exercises and a few additional levels
of difculty for some of the exercises. Pa-
tients were initially educated about the
structure and function of the trunk mus-
culature, as well as common impairments
in these muscles among patients with
LBP. Patients were then taught to per-
form an isolated contraction of the trans-
versus abdominis and lumbar multidus
through an abdominal drawing-in ma-
neuver (ADIM) in the quadruped, stand-
ing, and supine positions.
63,64,69,71,73
Once
a proper ADIM was achieved (most likely
by the second or third visit), additional
loads were placed on the spine through
various upper extremity, lower extremity,
and trunk movement patterns. Exercises
were performed in the quadruped, sidely-
ing, supine, and standing positions, with
the goal of recruiting a variety of trunk
muscles.
18,53,54
In each position, exercises
were ordered by their level of difculty,
and patients progressed from one exer-
cise to the next after satisfying specic
predetermined criteria. In the seventh
treatment session, functional movement
patterns were incorporated into the
training program while performing an
ADIM and maintaining a neutral lumbar
spine. This stage, which was not includ-
ed in the derivation study, was added to
the program because it has been recom-
mended by others.
22,58,62
The exercises in
each stage of the LSE program, as well as
the specic criteria for progression from
one exercise to the next, are outlined in
APPENDIX A (available at www.jospt.org).
Manual Therapy
The MT intervention included several
thrust and nonthrust manipulative tech-
niques directed at the lumbar spine that
have been used previously with some
degree of success in various groups with
LBP.
10,15,20,59
In addition, manual stretch-
ing of several hip and thigh muscles was
performed, as exibility of the lower ex-
tremity is purported to protect the spine
from excessive strain.
54
Finally, active
range-of-motion and stretching exercis-
es were added to the program, as these
44-01 Rabin.indd 8 12/17/2013 5:18:36 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
journal of orthopaedic & sports physical therapy | volume 44 | number 1 | january 2014 | 9
are commonly prescribed in combina-
tion with MT to maintain or improve the
mobility gains resulting from the manual
procedures.
10,15,20,47
The exercises included
were selected to minimize trunk muscle
activation and to avoid duplication be-
tween the 2 interventions.
All manual procedures and exercises
were prescribed based on the clinical
judgment of the treating therapist; how-
ever, each session could include up to 3
manual techniques, 1 of which had to be
a thrust manipulative technique directed
at the lumbar spine, and an additional
technique that had to include a manual
stretch of a lower extremity muscle. The
third technique, as well as the comple-
mentary range-of-motion/exibility ex-
ercises, was given at the discretion of the
treating therapist. The MT techniques, as
well as all exercises used in the MT proto-
col, are described in APPENDIX B (available
at www.jospt.org).
Evaluation
The MODI served as the primary out-
come measure in this investigation. The
MODI is scored from 0 to 100 and has a
minimal clinically important diference
(MCID) of 10 points among patients with
LBP.
57
The secondary outcome measure
was the NPRS, which has an MCID of 2
points among patients with LBP.
16
Both
measures were administered before the
beginning of treatment and immediately
after the last treatment session by an in-
vestigator not involved in patient care.
Sample Size
Sample size was calculated to detect a be-
tween-group diference of 12 points in the
nal score of the MODI, based on the in-
teraction between treatment group (LSE
versus MT) and CPR status (positive ver-
sus negative), with an alpha level of .05
and a power of 70%. Based on a 16-point
standard deviation, it was determined
that 20 patients were needed in each cell.
Pilot data suggested that the prevalence
of patients with a positive status on the
CPR was approximately 33%. Therefore,
it was estimated that 120 patients would
be necessary to include 40 patients with
a positive CPR status; however, 40 such
patients were included after 105 patients
were recruited, and recruitment was
stopped at that point.
Statistical Analysis
Descriptive statistics, including frequen-
cy counts for categorical variables and
measures of central tendency and dis-
persion for continuous variables, were
used to summarize the data. All baseline
variables were assessed for normal distri-
bution using the Shapiro-Wilk test. Base-
line variables were compared between
treatment groups (LSE versus MT), CPR
status (positive versus negative), and
the resulting 4 subgroups using a 2-way
analysis of variance and chi-square tests
for continuous and categorical variables,
respectively.
The primary aim of the study was
tested using 2 separate analyses of cova-
riance (ANCOVAs), with the nal MODI
score serving as the dependent variable in
1 model and the nal NPRS score serving
as the dependent variable in the second
model. In both models, treatment group
and CPR status served as independent
variables, and the baseline MODI score
(or baseline NPRS score) was used as
a covariate. The residuals of all models
were tested for violations of the ANCOVA
assumptions and for outliers. The main
efects of treatment group and CPR sta-
tus, as well as the 2-way interaction be-
tween these factors on the nal MODI
and NPRS scores, were evaluated. The a
priori level of signicance for these analy-
ses was P.05. Two pairwise comparisons
were planned following the ANCOVA: (1)
a comparison of diferences between pa-
tients with a positive CPR receiving LSE
and those with a negative CPR receiving
LSE, and (2) a comparison of diferences
between patients with a positive CPR
receiving LSE and those with a positive
CPR receiving MT. These 2 comparisons
were deemed the most relevant for the
purpose of validating the CPR, as both
included a comparison between patients
receiving a matched intervention (CPR-
positive patients receiving LSE) and
patients receiving an unmatched inter-
vention (either CPR-negative patients
receiving LSE or CPR-positive patients
receiving MT).
The individual items of the CPR, as
well as diferent combinations of these
items, were similarly tested to identify
whether any such combination would
enhance the predictive validity of the
original version. Finally, the outcome was
also dichotomized as successful or unsuc-
cessful based on a previously established
cutof threshold of 50% reduction in the
baseline score of the MODI.
33
The pro-
portion of patients achieving a success-
ful outcome was compared among the
resulting subgroups (LSE CPR+, LSE
CPR, MT CPR+, and MT CPR) using
chi-square analysis.
An intention-to-treat approach was
performed for all analyses by using mul-
tiple imputations for any missing val-
ues of the 2 outcome measures (MODI,
NPRS). First, Littles missing completely
at random test was performed to test the
hypothesis that missing values were ran-
domly distributed. If this hypothesis could
not be rejected, expectation maximization
was used to predict missing values. A per-
protocol analysis was performed as well.
All statistical analyses were performed us-
ing the JMP Version 10 statistical package
(SAS Institute Inc, Cary, NC), as well as
the SPSS Version 19 statistical package
(SPSS Inc, Chicago, IL).
RESULTS
F
ive hundred thirty-one poten-
tial candidates were screened for
eligibility between March 2010 and
April 2012. Two hundred ninety-seven pa-
tients did not meet the inclusion criteria,
and another 129 declined participation.
The remaining 105 patients were admit-
ted into the study. Forty patients had a
positive CPR status, whereas 65 had a
negative status. Forty-eight patients were
randomized to the LSE group, whereas 57
patients were randomized to receive MT.
All patients underwent treatment accord-
44-01 Rabin.indd 9 12/17/2013 5:18:37 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
10 | january 2014 | volume 44 | number 1 | journal of orthopaedic & sports physical therapy
[ RESEARCH REPORT ]
ing to their allocated treatment group.
Sixteen patients did not complete the
LSE intervention, and 8 patients did not
complete the MT intervention (P = .02).
FIGURE 1 presents patient recruitment and
retention throughout the study.
TABLE 1 presents baseline demographic,
history, and self-reported variables for all
groups and subgroups. All baseline vari-
ables were normally distributed, with the
exception of body mass index and dura-
tion of LBP. Log transformations were
thus performed on body mass index and
duration of LBP, resulting in a better dis-
tribution pattern. As a result, the geomet-
ric mean with 95% condence interval is
reported for these variables, as opposed
to mean SD for all other baseline vari-
ables (TABLE 1). No baseline diferences
were noted between the diferent groups
and subgroups other than for age. Pa-
tients with a positive CPR status were
younger than patients with a negative
CPR status (P = .0006). This diference
was expected, as 1 of the items comprising
the CPR is being less than 40 years of age.
Therefore, we did not correct our model
to account for this expected diference.
Littles "missing completely at ran-
dom" test indicated that the hypothesis
that nal MODI and NPRS scores were
randomly missing could not be rejected
(P = .76 for the MODI and P = .52 for the
NPRS). Therefore, expectation maximi-
zation was used to replace missing values.
Completers Versus Noncompleters
All baseline demographic, history, and
self-reported variables were compared
between patients who completed the
intervention (completers, n = 81) and
patients who dropped out prior to com-
pleting the intervention (noncompleters,
n = 24) using Wilcoxon and Fisher ex-
act tests for continuous and categorical
variables, respectively. Noncompleters
exhibited a higher baseline score on
the Fear-Avoidance Beliefs Question-
naire physical activity subscale versus
completers (17.2 versus 15.1, P = .04).
Noncompleters also had a lower level
of education compared to completers
(P = .03). No other diferences were
detected between the completers and
noncompleters.
Analysis by Intention to Treat
The baseline and nal MODI and NPRS
scores for each treatment group and sub-
group are summarized in TABLE 2. When
assessing nal disability level, the statisti-
cal level of signicance for the 2-way in-
teraction between treatment group and
CPR status was P = .17. A main efect was
detected for treatment (P = .05), which
indicated that patients receiving LSE
experienced less disability by the end
of treatment compared to the patients
who received MT. A main efect was also
detected for CPR status (P = .04), indi-
cating that patients with a positive CPR
status experienced less disability by the
end of treatment compared to those with
a negative CPR status, regardless of the
treatment received. The 2 preplanned
pairwise comparisons indicated that (1)
among patients receiving LSE, those with
a positive CPR status experienced less dis-
ability at the end of the intervention com-
pared to those with a negative CPR status
(P = .02); and (2) among patients with a
positive CPR status, those receiving LSE
experienced less disability by the end
of treatment compared to those receiv-
ing MT (P = .03). The change in MODI
between baseline and the end of treat-
ment for the 4 subgroups is represented
in FIGURE 2. No interactions or main ef-
fects were noted for pain (P>.26). TABLE 3
pre sents the adjusted nal disability and
pain scores for all groups and subgroups,
and TABLE 4 presents the diferences in -
nal disability and pain among the difer-
ent groups and subgroups.
Screened for eligibility, n = 531
Randomized, n = 105
Lumbar stabilization exercises,
n = 48
Excluded, n = 297:
MODI <24%, n = 151
Prior physical therapy, n = 28
Nerve root compression, n = 26
Pending legal proceeding, n = 24
Did not meet other inclusion
criteria, n = 68
Declined participation, n = 129
Manual therapy, n = 57
8-wk follow-up, n = 32
16 dropped out
8-wk follow-up, n = 49
8 dropped out
Analyzed, n = 48
CPR+, n = 18
Analyzed, n = 57
CPR, n = 30 CPR+, n = 22 CPR, n = 35
FIGURE 1. Flow diagram of participant recruitment and retention. Abbreviations: CPR, clinical prediction rule;
MODI, modied Oswestry Disability Index.
44-01 Rabin.indd 10 12/17/2013 5:18:38 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
journal of orthopaedic & sports physical therapy | volume 44 | number 1 | january 2014 | 11
The proportion of patients who
achieved a successful outcome, dened
as a reduction of at least 50% in disability
as measured by the MODI, did not difer
among the 4 subgroups (P = .31) (FIGURE 3).
When examining the interaction of
treatment group with each of the indi-
vidual items comprising the CPR on -
nal disability, no signicant efects were
noted (aberrant movement, P = .07; prone
instability test, P = .16; age less than 40
years, P = .72; SLR of 91 or greater, P =
.79). However, when combining the pres-
ence of aberrant movement and a positive
prone instability test (n = 44), a signi-
cant 2-way interaction between treatment
group and the modied version of the CPR
(mCPR) was found for nal disability (P
= .02). When the 2 pairwise comparisons
were repeated using the mCPR, ndings
indicated that (1) among patients receiv-
ing LSE, those with a positive mCPR sta-
tus (n = 20) experienced less disability by
the end of treatment compared to those
with a negative mCPR status (n = 28, P =
.02); and (2) among patients with a posi-
tive mCPR status, those receiving LSE (n
= 20) experienced less disability by the
end of treatment compared to those re-
ceiving MT (n = 24, P = .005). Unlike the
original version of the CPR, the mCPR
did not demonstrate a main efect for -
nal disability (P = .27). No 2-way interac-
tion or main efects were noted for nal
pain level when using the mCPR (P>.09).
TABLE 5 presents the adjusted nal disabil-
ity and pain scores of the diferent groups
and subgroups based on the mCPR, and
TABLE 6 presents the diferences in nal
disability and pain among the groups and
subgroups based on the mCPR.
Finally, the proportion of patients
achieving a successful outcome did not
difer between the subgroups based on
mCPR status (P = .30) (FIGURE 4).
Per-Protocol Analysis
Similar to analysis by intention to treat,
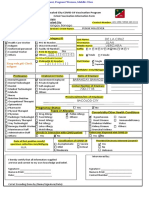
TABLE 1 Baseline Demographic, History, and Self-Report Variables for All Groups
Abbreviations: BMI, body mass index; CPR, patients with a negative status on the clinical prediction rule; CPR+, patients with a positive status on the clini-
cal prediction rule; FABQ-PA, Fear-Avoidance Beliefs Questionnaire physical activity subscale; FABQ-W, Fear-Avoidance Beliefs Questionnaire work subscale;
LBP, low back pain; LSE, patients treated with lumbar stabilization exercises; MODI, modied Oswestry Disability Index; MT, patients treated with manual
therapy; NPRS, numeric pain rating scale.
*Values are mean SD.
CPR greater than CPR+ (P = .0006).
Values are mean (95% condence interval).
Numbers provided when data not available on all patients.
Characteristic LSE (n = 48) MT (n = 57) CPR+ (n = 40) CPR (n = 65)
LSE CPR+
(n = 18)
LSE CPR
(n = 30)
MT CPR+
(n = 22)
MT CPR
(n = 35)
Sex (female), n (%) 25 (52.1) 31 (54.4) 22 (55.0) 34 (52.3) 10 (55.6) 15 (50.0) 12 (54.5) 19 (54.3)
Age, y*
38.3 10.5 35.5 9.1 32.8 7.5 39.2 10.3 32.7 7.4 41.6 10.7 32.8 7.7 37.2 9.6
BMI, kg/m
2
24.4 (22.9, 25.9) 25.8 (24.3, 27.3) 24.2 (22.6, 25.9) 25.9 (24.7, 27.3) 22.9 (20.7, 25.4) 25.9 (24.0, 27.9) 25.6 (23.3, 28.1) 26.0 (24.3, 27.8)
Education, n (%)
Less than high school 2 (4.2) 0 (0) 0 (0) 2 (3.1) 0 (0) 2 (6.7) 0 (0) 0 (0)
High school 21 (43.7) 15 (26.3) 9 (22.5) 27 (41.5) 5 (27.8) 16 (53.3) 4 (18.2) 11 (31.4)
Some postsecondary 8 (16.7) 15 (26.3) 9 (22.5) 14 (21.5) 3 (16.7) 5 (16.7) 6 (27.3) 9 (25.7)
Bachelor 13 (27.1) 17 (29.8) 18 (45.0) 12 (18.5) 8 (44.4) 5 (16.7) 10 (45.5) 7 (20.0)
Master 3 (6.2) 9 (15.8) 4 (10.0) 8 (12.3) 2 (11.1) 1 (3.3) 2 (9.0) 7 (20.0)
Doctorate 1 (2.1) 1 (1.8) 0 (0) 2 (3.1) 0 (0) 1 (3.3) 0 (0) 1 (2.8)
Work status (employed
),
n (%)
38/43 (88.4) 41/53 (77.4) 28/36 (77.8) 51/60 (85.0) 13/16 (81.3) 25/27 (92.6) 15/20 (75.0) 26/33 (78.8)
Smoker, n (%)
16/44 (36.4) 11/53 (20.8) 14/36 (38.9) 13/61 (21.3) 8/16 (50.0) 8/28 (28.6) 6/20 (30.0) 5/33 (15.2)
Duration (days since
onset)
58.7 (41.8, 82.4) 67.4 (48.9, 92.9) 63.8 (44.2, 92.2) 62.0 (46.5, 82.7) 52.0 (30.5, 88.6) 66.3 (43.6, 101.0) 78.4 (47.3, 130.0) 57.9 (39.1, 85.9)
Use of analgesics, n (%)
22/42 (52.4) 32/53 (60.4) 23/36 (63.9) 31/59 (52.5) 9/16 (56.3) 13/26 (50.0) 14/20 (70.0) 18/33 (54.6)
Past LBP, n (%)
34/48 (70.8) 35/56 (62.5) 27/39 (69.2) 42/65 (64.6) 13/18 (72.2) 21/30 (70.0) 14/21 (66.7) 21/35 (60.0)
Symptoms below knee,
n (%)
14 (29.2) 16 (28.1) 8 (20.0) 22 (33.8) 2 (11.1) 12 (40.0) 6 (27.3) 10 (28.6)
NPRS (0-10)* 4.9 1.7 5.3 1.7 4.9 1.7 5.3 1.7 4.4 1.7 5.2 1.6 5.2 1.6 5.4 1.8
MODI (0-100)* 37.8 10.6 37.6 12.5 40.0 12.8 36.3 10.6 37.8 9.4 37.7 11.4 41.8 15.0 35.0 9.9
FABQ-PA (0-24)* 16.2 4.4 15.1 4.9 14.9 5.3 16.0 4.3 15.9 4.3 16.3 4.6 14.1 5.8 15.7 4.2
FABQ-W (0-42)* 18.1 9.9 19.4 10.3 19.9 10.5 18.1 9.9 18.9 11.0 17.6 9.4 20.7 10.3 18.6 10.4
44-01 Rabin.indd 11 12/17/2013 5:18:39 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
12 | january 2014 | volume 44 | number 1 | journal of orthopaedic & sports physical therapy
[ RESEARCH REPORT ]
there was no 2-way interaction between
CPR status and treatment on nal disabil-
ity (P = .14). In addition, a main efect was
retained for CPR status on nal disability
(P = .04), indicating that patients with a
positive CPR status experienced less dis-
ability by the end of treatment compared
to patients with a negative CPR status,
regardless of the treatment received. No
main efect was noted for treatment (P =
.06). The preplanned pairwise compari-
sons indicated that (1) among all patients
receiving LSE, those with a positive CPR
status experienced less disability by the
end of treatment compared to those with
a negative CPR status (P = .02); and (2)
among patients with a positive CPR sta-
tus, those receiving LSE experienced less
disability by the end of treatment com-
pared to those receiving MT (P = .03).
No 2-way interaction or main efect was
noted for pain (P>.21). Chi-square analy-
sis indicated that the proportion of pa-
tients achieving a successful outcome was
greater among patients with a positive
CPR status compared to patients with
a negative CPR status, regardless of the
treatment received (P = .04).
The 2-way interaction between treat-
ment group and the mCPR on nal dis-
ability was retained in the per-protocol
analysis (P = .02). The preplanned pair-
wise comparisons indicated that (1)
among patients receiving LSE, those
with a positive mCPR status experienced
less disability at the conclusion of the
intervention compared to those with a
negative mCPR status (P = .03); and (2)
among patients with a positive mCPR sta-
tus, those receiving LSE experienced less
disability at the conclusion of the inter-
vention compared to those receiving MT
(P = .006). No 2-way interaction or main
efect was noted for pain level when us-
ing the mCPR (P>.13). Finally, although a
greater proportion of patients with a posi-
tive mCPR receiving LSE achieved a suc-
cessful outcome compared to the other 3
subgroups, this diference was not signi-
cant (P = .17).
DISCUSSION
T
he previously suggested CPR
for predicting a successful outcome
following LSE
33
could not be vali-
TABLE 2
Baseline and Final Disability (MODI) and Pain
(NPRS) Scores for All Groups and Subgroups*
Abbreviations: CPR, patients with a negative status on the clinical prediction rule; CPR+, patients
with a positive status on the clinical prediction rule; LSE, patients treated with lumbar stabilization
exercises; MODI, modied Oswestry Disability Index; MT, patients treated with manual therapy;
NPRS, numeric pain rating scale.
*Values are mean SD and are based on intention-to-treat analysis.
Group Baseline MODI (0-100) Final MODI (0-100) Baseline NPRS (0-10) Final NPRS (0-10)
LSE (n = 48) 37.8 10.6 16.1 11.2 4.9 1.7 2.4 1.8
MT (n = 57) 37.6 12.5 20.2 16.0 5.3 1.7 3.1 2.5
CPR+ (n = 40) 40.0 12.8 16.6 17.5 4.9 1.7 2.6 2.4
CPR (n = 65) 36.3 10.6 19.4 11.5 5.3 1.7 2.9 2.2
LSE CPR+ (n = 18) 37.8 9.4 10.7 9.8 4.4 1.7 1.9 1.6
LSE CPR (n = 30) 37.7 11.4 19.4 10.8 5.2 1.6 2.7 1.9
MT CPR+ (n = 22) 41.8 15.0 21.5 20.9 5.2 1.6 3.1 2.8
MT CPR (n = 35) 35.0 9.9 19.4 12.3 5.4 1.8 3.1 2.4
TABLE 3
Baseline Adjusted Final Disability
(MODI) and Pain (NPRS) Among the
Different Groups and Subgroups*
Abbreviations: CPR, patients with a negative status on the clinical prediction rule; CPR+, patients
with a positive status on the clinical prediction rule; LSE, patients treated with lumbar stabilization
exercises; MODI, modied Oswestry Disability Index; MT, patients treated with manual therapy;
NPRS, numeric pain rating scale.
*Values are mean (95% condence interval) and are provided based on intention-to-treat analysis.
Group MODI (0-100) NPRS (0-10)
LSE (n = 48) 15.0 (11.4, 18.6) 2.5 (1.9, 3.1)
MT (n = 57) 20.0 (16.7, 23.3) 3.0 (2.4, 3.5)
CPR+ (n = 40) 14.9 (11.0, 18.8) 2.7 (2.1, 3.4)
CPR (n = 65) 20.1 (17.1, 23.1) 2.8 (2.3, 3.3)
LSE CPR+ (n = 18) 10.7 (4.9, 16.4) 2.4 (1.4, 3.3)
LSE CPR (n = 30) 19.3 (14.9, 23.8) 2.6 (1.9, 3.4)
MT CPR+ (n = 22) 19.1 (13.9, 24.4) 3.0 (2.2, 3.9)
MT CPR (n = 35) 20.9 (16.7, 25.0) 2.9 (2.2, 3.6)
0
5
10
Baseline
LSE CPR+ LSE CPR
M
O
D
I
S
c
o
r
e
,
%
Final
15
20
25
30
35
40
45
MT CPR+ MT CPR
FIGURE 2. Change in disability from baseline to the
end of treatment for the 4 subgroups. Abbreviations:
LSE CPR, patients with a negative status on
the clinical prediction rule treated with lumbar
stabilization exercises; LSE CPR+, patients with a
positive status on the clinical prediction rule treated
with lumbar stabilization exercises; MODI, modied
Oswestry Disability Index; MT CPR, patients with a
negative status on the clinical prediction rule treated
with manual therapy; MT CPR+, patients with a
positive status on the clinical prediction rule treated
with manual therapy.
44-01 Rabin.indd 12 12/17/2013 5:18:41 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
journal of orthopaedic & sports physical therapy | volume 44 | number 1 | january 2014 | 13
dated in our investigation. Nevertheless,
we believe the CPR may hold promise in
identifying patients most likely to experi-
ence success following LSE. Despite the
absence of a CPR-by-treatment interac-
tion, the 2 pairwise comparisons most
relevant for validating the CPR indicated
that, by the end of treatment, patients
with a positive CPR status who received
LSE (a matched intervention) experi-
enced less disability compared to those
with a negative CPR status receiving
LSE or to patients with a positive CPR
status receiving MT (an unmatched in-
tervention). Furthermore, efect sizes for
both of these comparisons were very close
to the MCID of the MODI (10 points),
and the lower bounds of the 95% con-
dence intervals were above zero (TABLE 4).
The extra noise created by the multiple
computations of the ANCOVA might
have prevented a signicant CPR-by-
treatment interaction efect, despite the
consistent advantage for patients with a
positive CPR treated with LSE.
It seems, therefore, that the inability
to validate the CPR in this study is most
likely related to its level of power. Our
a priori sample-size calculation was de-
signed to detect a 12-point diference in
the MODI, with = .05 and a power of
70%. Therefore, it could be argued that
our study was somewhat underpowered.
However, based on our ndings, 314
patients would have been required to
achieve 80% power for detecting an in-
teraction between treatment group and
CPR status, a sample size that was un-
realistic under the circumstances of the
present study. We therefore believe that,
although our results cannot validate the
CPR, they do not invalidate it but, in fact,
seem to imply its potential. It is not un-
reasonable to assume that the CPR in its
current form may still be able to indicate
which patients would most likely succeed
with LSE.
Among other potential reasons for
the inability to validate a CPR are dif-
ferences in sample characteristics, in the
application of the CPR itself, in the ad-
ministration of the intervention, and in
the denition of the outcome between the
derivation and validation studies. With
regard to sample characteristics, the in-
clusion/exclusion criteria in the current
study were fairly similar to those of the
derivation study,
33
which resulted in rela-
tively similar samples. However, patients
in the current study demonstrated a high-
er level of disability at baseline (MODI
score, 37% versus 29% in the derivation
study
33
) and a somewhat longer duration
of symptoms (68 versus 40 days). The
longer duration of LBP in the current
sample could have had a negative efect
on the overall prognosis
32,40,72
; however,
this efect was not expected to difer be-
tween the treatment groups or subgroups.
As for the application of the CPR it-
self, the sample of the current study in-
cluded a higher proportion of patients
with a positive CPR status compared to
the derivation study (38% versus 28%).
33
A likely reason for this diference is the
younger age of our sample (37 versus 42
years). Another possible reason is the
higher prevalence of a positive prone
instability test in our study (71% versus
52% in the derivation study
33
). Because
we used the same testing technique and
rating criteria as outlined by Hicks et al,
33
we cannot explain the diference in prev-
alence rates of a positive prone instability
test. In any event, we do not believe that
the higher rate of a positive CPR status in
our study was likely to hinder the ability
to validate the CPR.
The LSE program used in the current
study was very similar to that used in the
derivation study. In addition, the criteria
for dichotomizing the outcomes as suc-
cess or failure were identical to those
used in the derivation study.
33
Therefore,
we do not believe these factors would
likely explain the inability to validate the
CPR, either.
Finally, the inability to validate the
CPR may be related to the comparison
intervention used in the current study.
TABLE 4
Baseline Adjusted Mean Differences in Final
Disability (MODI) and Pain (NPRS) Between
the Different Groups and Subgroups
Abbreviations: CPR, patients with a negative status on the clinical prediction rule; CPR+, patients
with a positive status on the clinical prediction rule; LSE, patients treated with lumbar stabilization
exercises; MODI, modied Oswestry Disability Index; MT, patients treated with manual therapy;
NPRS, numeric pain rating scale.
*Values are mean diference (95% condence interval).
Positive values indicate an advantage to LSE.
Positive values indicate an advantage to CPR+.
Positive values indicate an advantage to LSE CPR+.
Comparison MODI (0-100)* P Value NPRS (0-10)* P Value
LSE versus MT
5.0 (0.1, 9.9) .05 0.5 (0.3, 1.3) .26
CPR+ versus CPR
5.2 (0.2, 10.2) .04 0.1 (0.7, 0.9) .88
LSE CPR+ versus LSE CPR
8.7 (1.4, 15.9) .02 0.3 (0.9, 1.5) .67
LSE CPR+ versus MT CPR+
8.5 (0.7, 16.3) .03 0.7 (0.6, 1.9) .31
0
10
LSE CPR+ LSE CPR MT CPR+ MT CPR
20
30
40
50
60
70
80
90
S
u
c
c
e
s
s
R
a
t
e
,
%
FIGURE 3. Rate of success (%) among the 4
subgroups based on the original clinical prediction
rule and a cutof threshold of 50% decrease in
baseline modied Oswestry Disability Index score.
Abbreviations: LSE CPR, patients with a negative
status on the clinical prediction rule treated with
lumbar stabilization exercises; LSE CPR+, patients
with a positive status on the clinical prediction rule
treated with lumbar stabilization exercises; MT
CPR, patients with a negative status on the clinical
prediction rule treated with manual therapy; MT
CPR+, patients with a positive status on the clinical
prediction rule treated with manual therapy.
44-01 Rabin.indd 13 12/17/2013 5:18:42 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
14 | january 2014 | volume 44 | number 1 | journal of orthopaedic & sports physical therapy
[ RESEARCH REPORT ]
Manual therapy seemed to be a suitable
comparison intervention because it is fre-
quently used in the management of LBP,
it is advocated by several clinical practice
guidelines,
1,19,76
and it has previously been
shown to have a varied level of success
when compared to LSE in heterogeneous
samples of patients with LBP.
11,24,50,62
Despite this rationale, recent evidence
suggests that spinal manipulation may
result in remediation of some muscle im-
pairments that are the focus of LSE pro-
grams, such as increased activation of the
transversus abdominis and lumbar mul-
tidi.
42,61
It is possible, therefore, that the
manipulation techniques included in the
MT intervention contributed to facilita-
tion of the deep spinal musculature and,
consequently, exerted an efect similar to
that attributed to LSE. Be that as it may,
when spinal manipulation has been pre-
viously performed specically on patients
who meet the stabilization CPR,
41
no ef-
fects were observed on the activation of
the transversus abdominis or internal
oblique, and the clinical efects (pain and
disability) did not exceed the minimal
clinically important threshold.
41
Further-
more, another study indicated that none
of the variables comprising the stabiliza-
tion CPR was associated with increased
activation of the lumbar multidus fol-
lowing spinal manipulation.
43
Finally,
any changes in activation of the lumbar
multidus that were observed immedi-
ately after manipulation did not seem to
be consistently sustained 3 to 4 days after
the application of the technique.
42
There-
fore, we do not believe the manipulation
techniques in our study were likely to
produce long-lasting or clinically signi-
cant changes in recruitment of the spinal
musculature of our patients.
During the process of CPR validation,
it is not unusual to attempt to modify
an original version of a CPR by adding,
omitting, or combining several of its
items.
67,68,81
Our ndings indicate that a
modied version of the CPR (mCPR),
containing only 2 of the original 4 items,
yielded a better predictive validity. The
mCPR did result in a signicant inter-
action efect with treatment, and the 2
corresponding pairwise comparisons
indicated a better outcome for patients
with a positive mCPR status treated with
TABLE 5
Baseline Adjusted Final Disability (MODI)
and Pain (NPRS) Among the Different Groups
and Subgroups Based on the mCPR*
Abbreviations: LSE, patients treated with lumbar stabilization exercises; mCPR, patients with a
negative status on the modied clinical prediction rule; mCPR+, patients with a positive status on the
modied clinical prediction rule; MODI, modied Oswestry Disability Index; MT, patients treated
with manual therapy; NPRS, numeric pain rating scale.
*Values are mean (95% condence interval) and are provided based on intention-to-treat analysis.
Group MODI (0-100) NPRS (0-10)
LSE (n = 48) 15.4 (11.8, 18.9) 2.5 (1.9, 3.0)
MT (n = 57) 20.4 (17.2, 23.7) 3.0 (2.5, 3.5)
mCPR+ (n = 44) 16.5 (12.8, 20.3) 2.7 (2.1, 3.3)
mCPR (n = 61) 19.3 (16.1, 22.4) 2.8 (2.3, 3.3)
LSE mCPR+ (n = 20) 11.2 (5.7, 16.6) 2.0 (1.1, 2.9)
LSE mCPR (n = 28) 19.6 (15.0, 24.2) 2.9 (2.1, 3.6)
MT mCPR+ (n = 24) 21.9 (16.9, 26.9) 3.3 (2.5, 4.1)
MT mCPR (n = 33) 19.0 (14.7, 23.2) 2.8 (2.1, 3.4)
TABLE 6
Baseline Adjusted Mean Differences
in Final Disability (MODI) and Pain
(NPRS) Between the Different Groups
and Subgroups Based on the mCPR
Abbreviations: LSE, patients treated with lumbar stabilization exercises; mCPR, patients with a
negative status on the modied clinical prediction rule; mCPR+, patients with a positive status on the
modied clinical prediction rule; MODI, modied Oswestry Disability Index; MT, patients treated
with manual therapy; NPRS, numeric pain rating scale.
*Values are mean diference (95% condence interval) and are provided based on intention-to-treat
analysis.
Positive values indicate an advantage to LSE.
Positive values indicate an advantage to mCPR+.
Positive values indicate an advantage to LSE (mCPR+).
Comparison MODI (0-100)* P Value NPRS (0-10)* P Value
LSE versus MT
5.0 (0.2, 9.9) .04 0.5 (0.2, 1.3) .18
mCPR+ versus mCPR
2.7 (2.2, 7.7) .27 0.2 (0.6, 1.0) .67
LSE mCPR+ versus LSE mCPR
8.4 (1.3, 15.5) .02 0.8 (0.3, 2.0) .16
LSE mCPR+ versus MT mCPR+
10.7 (3.4, 18.1) .005 1.2 (0.0, 2.4) .05
0
10
LSE mCPR+ LSE mCPR MT mCPR+ MT mCPR
20
30
40
50
60
70
80
90
S
u
c
c
e
s
s
R
a
t
e
,
%
FIGURE 4. Rate of success (%) among the 4
subgroups based on the mCPR and a cutof
threshold of 50% decrease in baseline modied
Oswestry Disability Index score. Abbreviations:
LSE mCPR, patients with a negative status on the
modied clinical prediction rule treated with lumbar
stabilization exercises; LSE mCPR+, patients with
a positive status on the modied clinical prediction
rule treated with lumbar stabilization exercises;
mCPR, modied clinical prediction rule; MT mCPR,
patients with a negative status on the modied
clinical prediction rule treated with manual therapy;
MT mCPR+, patients with a positive status on the
modied clinical prediction rule treated with manual
therapy.
44-01 Rabin.indd 14 12/17/2013 5:18:43 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
journal of orthopaedic & sports physical therapy | volume 44 | number 1 | january 2014 | 15
LSE compared to patients treated with
unmatched interventions. Efect sizes
for these comparisons were either above
or slightly below the MCID of the MODI
(TABLE 6). These ndings seem to suggest
that the mCPR may be a more accurate
predictor of success following LSE.
It is acknowledged that because the
mCPR was derived retrospectively, its
efect on nal disability could have oc-
curred by chance alone. We believe, how-
ever, that several factors point against
this possibility. First, the mCPR is still
composed of items that have been previ-
ously linked to success following LSE in
the derivation study.
33
Second, no other
combination of items from the original
CPR produced similar ndings. Third,
we believe this 2-item version may even
possess a clearer biomechanical plau-
sibility compared to the original CPR.
The mCPR status is considered positive
when both aberrant lumbar movement
and a positive prone instability test are
present. Teyhen et al
70
demonstrated
that, compared to healthy individuals,
patients with LBP, aberrant movements,
and a positive prone instability test dem-
onstrate decreased control of lumbar
segmental mobility during midrange
lumbar motion.
This diference may rep-
resent an altered motor control strategy,
which suggests that an LSE program may
be most benecial under those circum-
stances. Furthermore, Hebert et al
31
dem-
onstrated that individuals with LBP and
a positive prone instability test displayed
decreased automatic activation of their
lumbar multidi compared to healthy
controls. Given the remediating efects
of LSE on muscle activation patterns,
73,74
it seems reasonable that LSE would be
most benecial for patients presenting
with such activation decits. In contrast,
it seems much less clear why patients
under the age of 40 would preferentially
benet from LSE as opposed to MT or
any other intervention. In fact, a younger
age has been previously associated with
a generally favorable prognosis following
an episode of LBP.
5,13,29,52,72
This nding
may help to explain why the CPR in its
original version seemed to be consistently
associated with a better outcome, regard-
less of the treatment received. Likewise,
it seems less intuitive why a greater SLR
range of motion would predict a better
outcome specically following LSE.
Finally, our entire sample included 40
patients with a positive CPR status ac-
cording to the original (4-item) version
and 44 patients with a positive mCPR
status. It could therefore be argued that
the slightly larger number of patients
with a positive mCPR might have simply
increased the power to detect an inter-
action with treatment group. However,
as only 31 patients had a positive status
according to both versions of the CPR, it
seems that the better predictive power of
the mCPR may not simply be a matter of
sample size but may be inherent in pa-
tients presenting with the 2 specic items
comprising the mCPR.
In summary, we believe that, in addi-
tion to its stronger statistical association
with success specically following LSE,
the mCPR carries a stronger biomechani-
cal plausibility as a predictor of success
following this intervention. Nevertheless,
due to its retrospective nature, an addi-
tional investigation is recommended to
prospectively establish the predictive va-
lidity of the mCPR.
Study Limitations
In addition to the aforementioned issues
of power and the retrospective nature of
some of the ndings, the current study
has several additional limitations. First,
the dropout rate was fairly high, in par-
ticular among the LSE group. Overall,
24 patients (22.8%) did not complete
the study. The dropout rate was greater
among patients receiving LSE (33%
versus 14%). We believe that the overall
dropout rate of the current study may
partly reect the dropout rate (31%)
among Israeli patients receiving outpa-
tient physical therapy for common mus-
culoskeletal conditions.
23
The greater
dropout rate among the LSE group also
suggests that patients receiving this in-
tervention may not have perceived it to
be as valuable as MT. The manual contact
included in the MT intervention could
have created an attention efect in favor
of this intervention, which, in turn, might
have contributed to better compliance.
Because this was suspected, the treating
clinicians were encouraged to provide
patients receiving LSE with continuous
verbal as well as manual cuing for main-
taining a neutral lumbar posture and an
ADIM. It seems, however, that this ap-
proach still failed to produce a similar
level of compliance among the 2 groups.
An intention-to-treat analysis was used
in an attempt to minimize the efect of
the dropout rate on our ndings.
Longer-term outcomes should be as-
sessed to determine whether the CPR
in its original or modied version has
any long-term efects on patients in the
various subgroups. In addition, the ex-
ternal validity of our ndings needs to
be considered, as only 105 patients were
recruited after screening 531 potential
participants. Most participants were ex-
cluded for not meeting the minimal level
of disability required for inclusion (FIGURE
1). Therefore, ndings are limited to pa-
tients with LBP with at least a moderate
level of disability.
CONCLUSION
T
he previously suggested CPR
for identifying patients most likely
to succeed following LSE could not
be validated in this study. However, be-
cause the subgroup comparisons most
relevant for the validity of the CPR in-
dicated an advantage for patients with
a positive CPR treated by LSE, and be-
cause of a relatively low level of power,
our ndings suggest that the current CPR
still has the potential to predict success
following LSE. Furthermore, a modied
version of the original CPR that included
only 2 of its items (aberrant movement
and positive prone instability test) was
able to predict a successful outcome spe-
cically following LSE and may serve as
a valid alternative. Future study is rec-
ommended to prospectively validate the
44-01 Rabin.indd 15 12/17/2013 5:18:44 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
16 | january 2014 | volume 44 | number 1 | journal of orthopaedic & sports physical therapy
[ RESEARCH REPORT ]
mCPR as a predictor of success with LSE
in individuals with LBP. Alternatively, to
validate the original version of the CPR, a
larger, replication study is recommended
in an attempt to overcome the insufcient
power of the current study. The ndings
of this study are further limited by a rela-
tively large dropout rate (22.8%) and lack
of a long-term follow-up.
t
KEY POINTS
FINDINGS: Although not validated, the
previously suggested CPR for identifying
patients most likely to succeed follow-
ing LSE shows promise. Furthermore, a
modified version of the CPR containing
only 2 of its original 4 items (presence of
aberrant movement and a positive prone
instability test) demonstrated a better
predictive validity in identifying those
most likely to succeed with LSE.
IMPLICATIONS: Patients with LBP present-
ing with aberrant lumbar movement as
well as a positive prone instability test
may benefit most from an LSE program.
CAUTION: Findings are limited by a
relatively small sample size, a relatively
large dropout rate, and the lack of a
long-term follow-up.
ACKNOWLEDGEMENTS: The authors thank Dr
Gregory Hicks, Arnon Ravid, Ori Firsteter,
Shai Grinberg, Efrat Laor, Dikla Taif, Alon
Ben-Moshe, Mossa Hugirat, Meira Lugasi,
Lena Oifman, Liron Laposhner, Beni Mazoz,
Fadi Knuati, Lena Kin, Ruthy Bachar, Chen
Tel-Avivi, Irit Fridman, Yana Avner, Naomi
Sivan, Rafi Cohen, and Yigal Levran for their
contribution and support of this work.
REFERENCES
1. Airaksinen O, Brox JI, Cedraschi C, et al. Chapter
4. European guidelines for the management of
chronic nonspecic low back pain. Eur Spine
J. 2006;15 suppl 2:S192-S300. http://dx.doi.
org/10.1007/s00586-006-1072-1
2. Assendelft WJ, Morton SC, Yu EI, Suttorp MJ,
Shekelle PG. Spinal manipulative therapy for
low back pain. A meta-analysis of efectiveness
relative to other therapies. Ann Intern Med.
2003;138:871-881.
3. Baron G, Alter R, Halevi-Heitner H, Yasin S, Ofer
Y, Zory H. Modied Oswestry Low Back Pain
Disability Questionnaire: checking reliability and
validity of the questionnaire in Hebrew. Gerontol-
ogy (Israel). 2005;32:147-163.
4. Beattie P, Nelson R. Clinical prediction rules:
what are they and what do they tell us? Aust J
Physiother. 2006;52:157-163.
5. Bekkering GE, Hendriks HJ, van Tulder MW, et al.
Prognostic factors for low back pain in patients
referred for physiotherapy: comparing outcomes
and varying modeling techniques. Spine (Phila
Pa 1976). 2005;30:1881-1886.
6. Borkan JM, Koes B, Reis S, Cherkin DC. A
report from the Second International Forum
for Primary Care Research on Low Back Pain.
Reexamining priorities. Spine (Phila Pa 1976).
1998;23:1992-1996.
7. Bouter LM, van Tulder MW, Koes BW. Methodo-
logic issues in low back pain research in primary
care. Spine (Phila Pa 1976). 1998;23:2014-2020.
8. Brennan GP, Fritz JM, Hunter SJ, Thackeray A,
Delitto A, Erhard RE. Identifying subgroups of
patients with acute/subacute nonspecic low
back pain: results of a randomized clinical trial.
Spine (Phila Pa 1976). 2006;31:623-631. http://
dx.doi.org/10.1097/01.brs.0000202807.72292.a8
9. Bronfort G, Haas M, Evans R, Leininger B, Triano
J. Efectiveness of manual therapies: the UK
evidence report. Chiropr Osteopat. 2010;18:3.
http://dx.doi.org/10.1186/1746-1340-18-3
10. Browder DA, Childs JD, Cleland JA, Fritz JM. Ef-
fectiveness of an extension-oriented treatment
approach in a subgroup of subjects with low
back pain: a randomized clinical trial. Phys Ther.
2007;87:1608-1618. http://dx.doi.org/10.2522/
ptj.20060297
11. Cairns MC, Foster NE, Wright C. Randomized
controlled trial of specic spinal stabilization
exercises and conventional physiotherapy
for recurrent low back pain. Spine (Phila Pa
1976). 2006;31:E670-E681. http://dx.doi.
org/10.1097/01.brs.0000232787.71938.5d
12. Cassidy JD, Carroll LJ, Ct P. The Saskatch-
ewan Health and Back Pain Survey: the preva-
lence of low back pain and related disability in
Saskatchewan adults. Spine (Phila Pa 1976).
1998;23:1860-1866; discussion 1867.
13. Cassidy JD, Ct P, Carroll LJ, Kristman V. Inci-
dence and course of low back pain episodes in
the general population. Spine (Phila Pa 1976).
2005;30:2817-2823.
14. Childs JD, Cleland JA. Development and applica-
tion of clinical prediction rules to improve deci-
sion making in physical therapist practice. Phys
Ther. 2006;86:122-131.
15. Childs JD, Fritz JM, Flynn TW, et al. A clinical
prediction rule to identify patients with low
back pain most likely to benet from spinal ma-
nipulation: a validation study. Ann Intern Med.
2004;141:920-928.
16. Childs JD, Piva SR, Fritz JM. Responsiveness
of the numeric pain rating scale in patients
with low back pain. Spine (Phila Pa 1976).
2005;30:1331-1334.
17. Choi BK, Verbeek JH, Tam WW, Jiang JY.
Exercises for prevention of recurrences of
low-back pain. Cochrane Database Syst
Rev. 2010:CD006555. http://dx.doi.
org/10.1002/14651858.CD006555.pub2
18. Cholewicki J, VanVliet JJ, 4th. Relative contri-
bution of trunk muscles to the stability of the
lumbar spine during isometric exertions. Clin
Biomech (Bristol, Avon). 2002;17:99-105.
19. Chou R, Qaseem A, Snow V, et al. Diagnosis
and treatment of low back pain: a joint clinical
practice guideline from the American College of
Physicians and the American Pain Society. Ann
Intern Med. 2007;147:478-491.
20. Cleland JA, Fritz JM, Kulig K, et al. Comparison
of the efectiveness of three manual physical
therapy techniques in a subgroup of patients
with low back pain who satisfy a clinical pre-
diction rule: a randomized clinical trial. Spine
(Phila Pa 1976). 2009;34:2720-2729. http://
dx.doi.org/10.1097/BRS.0b013e3181b48809
21. Cleland JA, Mintken PE, Carpenter K, et al.
Examination of a clinical prediction rule to
identify patients with neck pain likely to benet
from thoracic spine thrust manipulation and
a general cervical range of motion exercise:
multi-center randomized clinical trial. Phys Ther.
2010;90:1239-1250. http://dx.doi.org/10.2522/
ptj.20100123
22. Costa LO, Maher CG, Latimer J, et al. Motor
control exercise for chronic low back pain: a
randomized placebo-controlled trial. Phys Ther.
2009;89:1275-1286. http://dx.doi.org/10.2522/
ptj.20090218
23. Deutscher D, Horn SD, Dickstein R, et al. As-
sociations between treatment processes, patient
characteristics, and outcomes in outpatient
physical therapy practice. Arch Phys Med
Rehabil. 2009;90:1349-1363. http://dx.doi.
org/10.1016/j.apmr.2009.02.005
24. Ferreira ML, Ferreira PH, Latimer J, et al.
Comparison of general exercise, motor control
exercise and spinal manipulative therapy for
chronic low back pain: a randomized trial. Pain.
2007;131:31-37. http://dx.doi.org/10.1016/j.
pain.2006.12.008
25. Ferreira PH, Ferreira ML, Hodges PW. Changes
in recruitment of the abdominal muscles in
people with low back pain: ultrasound measure-
ment of muscle activity. Spine (Phila Pa 1976).
2004;29:2560-2566.
26. Fritz JM. Clinical prediction rules in physi-
cal therapy: coming of age? J Orthop Sports
Phys Ther. 2009;39:159-161. http://dx.doi.
org/10.2519/jospt.2009.0110
27. Fritz JM, Delitto A, Erhard RE. Comparison
of classication-based physical therapy with
therapy based on clinical practice guidelines
for patients with acute low back pain: a ran-
domized clinical trial. Spine (Phila Pa 1976).
2003;28:1363-1371; discussion 1372. http://
dx.doi.org/10.1097/01.BRS.0000067115.61673.
FF
28. Fritz JM, Irrgang JJ. A comparison of a modied
44-01 Rabin.indd 16 12/17/2013 5:18:45 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
journal of orthopaedic & sports physical therapy | volume 44 | number 1 | january 2014 | 17
MORE INFORMATION
WWW.JOSPT.ORG
@
REFERENCES
Oswestry Low Back Pain Disability Question-
naire and the Quebec Back Pain Disability Scale.
Phys Ther. 2001;81:776-788.
29. Grotle M, Brox JI, Veierd MB, Glomsrd B, Lnn
JH, Vllestad NK. Clinical course and prognostic
factors in acute low back pain: patients consult-
ing primary care for the rst time. Spine (Phila
Pa 1976). 2005;30:976-982.
30. Hancock M, Herbert RD, Maher CG. A guide to
interpretation of studies investigating subgroups
of responders to physical therapy interventions.
Phys Ther. 2009;89:698-704. http://dx.doi.
org/10.2522/ptj.20080351
31. Hebert JJ, Koppenhaver SL, Magel JS, Fritz JM.
The relationship of transversus abdominis and
lumbar multidus activation and prognostic
factors for clinical success with a stabilization
exercise program: a cross-sectional study. Arch
Phys Med Rehabil. 2010;91:78-85. http://dx.doi.
org/10.1016/j.apmr.2009.08.146
32. Henschke N, Maher CG, Refshauge KM, et al.
Prognosis in patients with recent onset low back
pain in Australian primary care: inception cohort
study. BMJ. 2008;337:a171.
33. Hicks GE, Fritz JM, Delitto A, McGill SM. Prelimi-
nary development of a clinical prediction rule for
determining which patients with low back pain
will respond to a stabilization exercise program.
Arch Phys Med Rehabil. 2005;86:1753-1762.
http://dx.doi.org/10.1016/j.apmr.2005.03.033
34. Hides J, Gilmore C, Stanton W, Bohlscheid E.
Multidus size and symmetry among chronic
LBP and healthy asymptomatic subjects.
Man Ther. 2008;13:43-49. http://dx.doi.
org/10.1016/j.math.2006.07.017
35. Hides JA, Jull GA, Richardson CA. Long-term
efects of specic stabilizing exercises for rst-
episode low back pain. Spine (Phila Pa 1976).
2001;26:E243-E248.
36. Hides JA, Stanton WR, McMahon S, Sims K,
Richardson CA. Efect of stabilization training on
multidus muscle cross-sectional area among
young elite cricketers with low back pain. J Or-
thop Sports Phys Ther. 2008;38:101-108. http://
dx.doi.org/10.2519/jospt.2008.2658
37. Hodges PW, Richardson CA. Altered trunk
muscle recruitment in people with low back pain
with upper limb movement at diferent speeds.
Arch Phys Med Rehabil. 1999;80:1005-1012.
38. Jacob T, Baras M, Zeev A, Epstein L. Low back
pain: reliability of a set of pain measurement
tools. Arch Phys Med Rehabil. 2001;82:735-742.
http://dx.doi.org/10.1053/apmr.2001.22623
39. Jette DU, Jette AM. Physical therapy and
health outcomes in patients with spinal impair-
ments. Phys Ther. 1996;76:930-941; discussion
942-945.
40. Jones GT, Johnson RE, Wiles NJ, et al. Predicting
persistent disabling low back pain in general
practice: a prospective cohort study. Br J Gen
Pract. 2006;56:334-341.
41. Konitzer LN, Gill NW, Koppenhaver SL. Investiga-
tion of abdominal muscle thickness changes
after spinal manipulation in patients who meet
a clinical prediction rule for lumbar stabilization.
J Orthop Sports Phys Ther. 2011;41:666-674.
http://dx.doi.org/10.2519/jospt.2011.3685
42. Koppenhaver SL, Fritz JM, Hebert JJ, et al. As-
sociation between changes in abdominal and
lumbar multidus muscle thickness and clinical
improvement after spinal manipulation. J Or-
thop Sports Phys Ther. 2011;41:389-399. http://
dx.doi.org/10.2519/jospt.2011.3632
43. Koppenhaver SL, Fritz JM, Hebert JJ, et al. As-
sociation between history and physical examina-
tion factors and change in lumbar multidus
muscle thickness after spinal manipulation in
patients with low back pain. J Electromyogr
Kinesiol. 2012;22:724-731. http://dx.doi.
org/10.1016/j.jelekin.2012.03.004
44. Koumantakis GA, Watson PJ, Oldham JA. Trunk
muscle stabilization training plus general exer-
cise versus general exercise only: randomized
controlled trial of patients with recurrent low
back pain. Phys Ther. 2005;85:209-225.
45. Leboeuf-Yde C, Lauritsen JM, Lauritzen T. Why
has the search for causes of low back pain
largely been nonconclusive? Spine (Phila Pa
1976). 1997;22:877-881.
46. Li LC, Bombardier C. Physical therapy man-
agement of low back pain: an exploratory
survey of therapist approaches. Phys Ther.
2001;81:1018-1028.
47. Long A, Donelson R, Fung T. Does it matter
which exercise? A randomized control trial of ex-
ercise for low back pain. Spine (Phila Pa 1976).
2004;29:2593-2602.
48. MacDonald D, Moseley GL, Hodges PW. Why
do some patients keep hurting their back?
Evidence of ongoing back muscle dysfunction
during remission from recurrent back pain. Pain.
2009;142:183-188. http://dx.doi.org/10.1016/j.
pain.2008.12.002
49. Macedo LG, Latimer J, Maher CG, et al. Efect of
motor control exercises versus graded activity
in patients with chronic nonspecic low back
pain: a randomized controlled trial. Phys Ther.
2012;92:363-377. http://dx.doi.org/10.2522/
ptj.20110290
50. Macedo LG, Maher CG, Latimer J, McAuley JH.
Motor control exercise for persistent, nonspe-
cic low back pain: a systematic review. Phys
Ther. 2009;89:9-25. http://dx.doi.org/10.2522/
ptj.20080103
51. Machado LA, de Souza M, Ferreira PH, Fer-
reira ML. The McKenzie method for low back
pain: a systematic review of the literature
with a meta-analysis approach. Spine (Phila
Pa 1976). 2006;31:E254-E262. http://dx.doi.
org/10.1097/01.brs.0000214884.18502.93
52. Mallen CD, Peat G, Thomas E, Dunn KM, Croft
PR. Prognostic factors for musculoskeletal pain
in primary care: a systematic review. Br J Gen
Pract. 2007;57:655-661.
53. McGill S. Low Back Disorders: Evidence-based
Prevention and Rehabilitation. Champaign, IL:
Human Kinetics; 2002.
54. McGill SM. Low back exercises: evidence
for improving exercise regimens. Phys Ther.
1998;78:754-765.
55. McGinn TG, Guyatt GH, Wyer PC, Naylor CD, Sti-
ell IG, Richardson WS. Users guides to the med-
ical literature: XXII: how to use articles about
clinical decision rules. Evidence-Based Medicine
Working Group. JAMA. 2000;284:79-84.
56. Mikhail C, Korner-Bitensky N, Rossignol M,
Dumas JP. Physical therapists use of inter-
ventions with high evidence of efectiveness
in the management of a hypothetical typical
patient with acute low back pain. Phys Ther.
2005;85:1151-1167.
57. Ostelo RW, Deyo RA, Stratford P, et al. Interpret-
ing change scores for pain and functional status
in low back pain: towards international consen-
sus regarding minimal important change. Spine
(Phila Pa 1976). 2008;33:90-94. http://dx.doi.
org/10.1097/BRS.0b013e31815e3a10
58. OSullivan PB. Lumbar segmental instability:
clinical presentation and specic stabilizing
exercise management. Man Ther. 2000;5:2-12.
http://dx.doi.org/10.1054/math.1999.0213
59. Powers CM, Beneck GJ, Kulig K, Landel RF,
Fredericson M. Efects of a single session of
posterior-to-anterior spinal mobilization and
press-up exercise on pain response and lumbar
spine extension in people with nonspecic low
back pain. Phys Ther. 2008;88:485-493. http://
dx.doi.org/10.2522/ptj.20070069
60. Rabin A, Shashua A, Pizem K, Dar G. The inter-
rater reliability of physical examination tests
that may predict the outcome or suggest the
need for lumbar stabilization exercises. J Orthop
Sports Phys Ther. 2013;43:83-90. http://dx.doi.
org/10.2519/jospt.2013.4310
61. Raney NH, Teyhen DS, Childs JD. Observed
changes in lateral abdominal muscle thickness
after spinal manipulation: a case series using re-
habilitative ultrasound imaging. J Orthop Sports
Phys Ther. 2007;37:472-479. http://dx.doi.
org/10.2519/jospt.2007.2523
62. Rasmussen-Barr E, Nilsson-Wikmar L, Arvidsson
I. Stabilizing training compared with manual
treatment in sub-acute and chronic low-back
pain. Man Ther. 2003;8:233-241. http://dx.doi.
org/10.1016/S1356-689X(03)00053-5
63. Richardson C, Hodges P, Hides J. Therapeutic
Exercise for Lumbopelvic Stabilization: A Motor
Control Approach for the Treatment and Preven-
tion of Low Back Pain. 2nd ed. Edinburgh, UK:
Churchill Livingstone; 2004.
64. Richardson CA, Jull GA. Muscle controlpain
control. What exercises would you pre-
scribe? Man Ther. 1995;1:2-10. http://dx.doi.
org/10.1054/math.1995.0243
65. Shaughnessy M, Cauleld B. A pilot study to
investigate the efect of lumbar stabilisation
exercise training on functional ability and quality
of life in patients with chronic low back pain. Int
J Rehabil Res. 2004;27:297-301.
66. Stanton TR, Hancock MJ, Maher CG, Koes BW.
Critical appraisal of clinical prediction rules that
aim to optimize treatment selection for muscu-
44-01 Rabin.indd 17 12/17/2013 5:18:46 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
18 | january 2014 | volume 44 | number 1 | journal of orthopaedic & sports physical therapy
[ RESEARCH REPORT ]
MORE INFORMATION
WWW.JOSPT.ORG
@
loskeletal conditions. Phys Ther. 2010;90:843-
854. http://dx.doi.org/10.2522/ptj.20090233
67. Stiell IG, Greenberg GH, McKnight RD, et al.
Decision rules for the use of radiography in
acute ankle injuries. Renement and prospective
validation. JAMA. 1993;269:1127-1132.
68. Stiell IG, Greenberg GH, Wells GA, et al. Pro-
spective validation of a decision rule for the use
of radiography in acute knee injuries. JAMA.
1996;275:611-615.
69. Teyhen DS, Bluemle LN, Dolbeer JA, et al.
Changes in lateral abdominal muscle thickness
during the abdominal drawing-in maneuver in
those with lumbopelvic pain. J Orthop Sports
Phys Ther. 2009;39:791-798. http://dx.doi.
org/10.2519/jospt.2009.3128
70. Teyhen DS, Flynn TW, Childs JD, Abraham LD.
Arthrokinematics in a subgroup of patients likely
to benet from a lumbar stabilization exercise
program. Phys Ther. 2007;87:313-325. http://
dx.doi.org/10.2522/ptj.20060253
71. Teyhen DS, Miltenberger CE, Deiters HM,
et al. The use of ultrasound imaging of the
abdominal drawing-in maneuver in subjects
with low back pain. J Orthop Sports Phys Ther.
2005;35:346-355. http://dx.doi.org/10.2519/
jospt.2005.35.6.346
72. Thomas E, Silman AJ, Croft PR, Papageorgiou
AC, Jayson MI, Macfarlane GJ. Predicting who
develops chronic low back pain in primary care:
a prospective study. BMJ. 1999;318:1662-1667.
73. Tsao H, Druitt TR, Schollum TM, Hodges PW. Mo-
tor training of the lumbar paraspinal muscles in-
duces immediate changes in motor coordination
in patients with recurrent low back pain. J Pain.
2010;11:1120-1128. http://dx.doi.org/10.1016/j.
jpain.2010.02.004
74. Tsao H, Hodges PW. Immediate changes in
feedforward postural adjustments follow-
ing voluntary motor training. Exp Brain Res.
2007;181:537-546. http://dx.doi.org/10.1007/
s00221-007-0950-z
75. Unsgaard-Tndel M, Fladmark AM, Salvesen
O, Vasseljen O. Motor control exercises, sling
exercises, and general exercises for patients
with chronic low back pain: a randomized
controlled trial with 1-year follow-up. Phys Ther.
2010;90:1426-1440. http://dx.doi.org/10.2522/
ptj.20090421
76. van Tulder M, Becker A, Bekkering T, et al. Chap-
ter 3. European guidelines for the management
of acute nonspecic low back pain in primary
care. Eur Spine J. 2006;15 suppl 2:S169-S191.
http://dx.doi.org/10.1007/s00586-006-1071-2
77. van Tulder M, Malmivaara A, Esmail R, Koes B.
Exercise therapy for low back pain: a systematic
review within the framework of the Cochrane
Collaboration back review group. Spine (Phila Pa
1976). 2000;25:2784-2796.
78. Von Korf M, Saunders K. The course of back
pain in primary care. Spine (Phila Pa 1976).
1996;21:2833-2837; discussion 2838-2839.
79. Waddell G, Newton M, Henderson I, Somerville
D, Main CJ. A Fear-Avoidance Beliefs Question-
naire (FABQ) and the role of fear-avoidance
beliefs in chronic low back pain and disability.
Pain. 1993;52:157-168.
80. Wallwork TL, Stanton WR, Freke M, Hides JA.
The efect of chronic low back pain on size and
contraction of the lumbar multidus muscle.
Man Ther. 2009;14:496-500. http://dx.doi.
org/10.1016/j.math.2008.09.006
81. Wells PS, Hirsh J, Anderson DR, et al. A simple
clinical model for the diagnosis of deep-vein
thrombosis combined with impedance
plethysmography: potential for an improve-
ment in the diagnostic process. J Intern Med.
1998;243:15-23.
82. Wilke HJ, Wolf S, Claes LE, Arand M, Wiesend A.
Stability increase of the lumbar spine with dif-
ferent muscle groups. A biomechanical in vitro
study. Spine (Phila Pa 1976). 1995;20:192-198.
PUBLISH Your Manuscript in a Journal With International Reach
JOSPT ofers authors of accepted papers an international audience. The
Journal is currently distributed to the members of APTAs Orthopaedic
and Sports Physical Therapy Sections and 31 orthopaedics, manual therapy,
and sports groups in 25 countries who provide online access either as a
member benet or at a discount. As a result, the Journal is now distrib-
uted monthly to more than 28 500 individuals around the world who special-
ize in musculoskeletal and sports-related rehabilitation, health, and
wellness. In addition, JOSPT reaches students and faculty, physical
therapists and physicians at more than 1,250 institutions in 57 countries.
Please review our Information for and Instructions to Authors at
www.jospt.org in the Info Center for Authors and submit your manuscript for
peer review at http://mc.manuscriptcentral.com/jospt.
44-01 Rabin.indd 18 12/17/2013 5:18:46 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
journal of orthopaedic & sports physical therapy | volume 44 | number 1 | january 2014 | B1
LUMBAR STABILIZATION EXERCISE PROGRAM
Exercise or Activity/Criteria
for Progression Description
Stage 1
ADIM in quadruped; 30 repetitions Following exhalation, the patient tightens the ab-
dominal muscles and draws the belly button up
toward the spine, while maintaining a neutral
lumbar spine position. The contraction is held for
8 seconds.
ADIM in standing; 30 repetitions Following exhalation, the patient tightens the ab-
dominal muscles and draws the belly button in
toward the spine, while maintaining a neutral
lumbar spine position. The contraction is held for
8 seconds.
ADIM in supine; 30 repetitions Following exhalation, the patient tightens the ab-
dominal muscles and draws the belly button in
toward the spine, while maintaining a neutral
lumbar spine position. The contraction is held for
8 seconds.
APPENDIX A
44-01 Rabin.indd 1 12/18/2013 6:15:49 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
B2 | january 2014 | volume 44 | number 1 | journal of orthopaedic & sports physical therapy
[ RESEARCH REPORT ]
Exercise or Activity/Criteria
for Progression Description
Stage 2 During stage 2, the patient progresses from one
exercise to the next in 4 diferent positions: supine
lying, sidelying, quadruped, and standing.
Supine ADIM with heel slide;
20 repetitions with each leg
Starting in a hook-lying position, feet at on the sup-
porting surface, the patient performs an ADIM and
slides 1 heel on the supporting surface until the
knee is straight. The position is held for 4 seconds,
and the leg is returned to the starting position. The
movement is repeated, alternating between legs.
Supine ADIM with leg lift;
20 repetitions with each leg
The patient performs an ADIM and raises 1 foot 10
cm of the supporting surface. The position is held
for 4 seconds, and the leg is returned to the start-
ing position.
Supine ADIM with bridging (2 legs);
30 repetitions
The patient performs an ADIM and raises the but-
tocks of the supporting surface. The position is
held for 8 seconds, and the patient returns to the
starting position.
Supine ADIM with single-leg bridge;
30 repetitions with each leg
Starting in a hook-lying position, the patient per-
forms an ADIM and straightens 1 knee. The patient
then raises the buttocks of the table using the op-
posite leg. The position is held for 8 seconds, and
the patient returns to the starting position.
APPENDIX A
44-01 Rabin.indd 2 12/18/2013 6:15:49 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
journal of orthopaedic & sports physical therapy | volume 44 | number 1 | january 2014 | B3
Exercise or Activity/Criteria
for Progression Description
Stage 2 (continued)
Supine ADIM with curl-up: 1 (elbows
on the table); 30 repetitions
The patient assumes a supine position, with one leg
straight and the other leg bent at the knee and hip
to maintain a neutral pelvic position (no need to
alternate legs). Patient places both hands under
the lumbar spine (this also helps to maintain a
neutral pelvic and lumbar position). Patient per-
forms an ADIM and raises the head and shoulders
of the table. The position is held for 8 seconds,
and the patient returns to the starting position.
Supine ADIM with curl-up: 2 (elbows
of the table); 30 repetitions
The patient assumes a supine position, with one leg
straight and the other leg bent at the knee and hip
to maintain a neutral pelvic position (no need to
alternate legs). Patient places both hands under
the lumbar spine (this also helps to maintain a
neutral pelvic and lumbar position). Patient per-
forms an ADIM and raises the head and shoulders
of the table. The position is held for 8 seconds,
and the patient returns to the starting position.
Supine ADIM with curl-up: 3 (hands
over forehead); 30 repetitions
The patient assumes a supine position, with one leg
straight and the other leg bent at the knee and
hip to maintain a neutral pelvic position (no need
to alternate legs). Patient places both hands over
his/her forehead, performs an ADIM, and raises
the head and shoulders of the table. The position
is held for 8 seconds, and the patient returns to
the starting position.
Horizontal side support, knees bent;
30 repetitions on each side
The patient performs an ADIM and raises the hips
and trunk of the supporting surface. The position
is held for 8 seconds, and the patient returns to
the starting position.
APPENDIX A
44-01 Rabin.indd 3 12/18/2013 6:15:50 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
B4 | january 2014 | volume 44 | number 1 | journal of orthopaedic & sports physical therapy
[ RESEARCH REPORT ]
Exercise or Activity/Criteria
for Progression Description
Stage 2 (continued)
Horizontal side support, knees
straight; 30 repetitions on each side
The patient performs an ADIM and raises the hips
and trunk of the table. The position is held for
8 seconds, and the patient returns to the starting
position.
Horizontal side support, advanced 1;
30 repetitions on each side
The patient performs an ADIM and raises the hips
and trunk of the table. The patient then rotates
the trunk backward and forward (4 times in
each direction), and then returns to the starting
position.
Sidelying horizontal side support,
advanced 2; 30 repetitions
The patient performs an ADIM and raises the hips
and trunk of the table. The patient then rolls
over onto the opposite elbow while maintaining
a neutral spine. The patient then rolls back to the
starting position.
Quadruped with leg raise;
30 repetitions with each leg
The patient performs an ADIM and then straightens
1 leg backward, while maintaining a neutral lumbar
spine position. The position is held for 8 seconds
before returning to the starting position.
APPENDIX A
44-01 Rabin.indd 4 12/18/2013 6:15:50 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
journal of orthopaedic & sports physical therapy | volume 44 | number 1 | january 2014 | B5
Exercise or Activity/Criteria
for Progression Description
Stage 2 (continued)
Quadruped with contralateral arm and
leg raise; 30 repetitions with each
arm and leg
The patient performs an ADIM and then straightens 1
leg backward, along with a contralateral arm raise,
while maintaining a neutral lumbar position. The
position is held for 8 seconds before returning to
the starting position.
Quadruped, advanced; 30 repetitions
with each arm and leg
The patient performs an ADIM and then straightens
1 leg back, along with a contralateral arm raise,
while maintaining a neutral lumbar position. The
position is held for 8 seconds. The patient then
lowers the arm and leg without replacing them
back on the supporting surface and then straight-
ens the arm and leg back to a horizontal position.
Standing rowing; 30 repetitions
with each arm
The patient performs an ADIM and then pulls a 1- to
1.5-kg weight in a rowing motion until the weight is
at chest level. The position is held for 6 seconds,
and the patient then returns the weight to the
starting position.
APPENDIX A
44-01 Rabin.indd 5 12/18/2013 6:15:50 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
B6 | january 2014 | volume 44 | number 1 | journal of orthopaedic & sports physical therapy
[ RESEARCH REPORT ]
Exercise or Activity/Criteria
for Progression Description
Stage 2 (continued)
Walking; patient progresses
to 10 minutes
The patient alternates between performing an ADIM
for 8 seconds and relaxing for 10 seconds, while
walking.
Stage 3 The patient continues with the exercises from stage
2 and begins to practice the following functional
activities.
Sit-to-stand transfer; 30 repetitions The patient sits on a standard chair and performs an
ADIM while keeping the spine in a neutral position.
The patient then rises to a standing position and
then sits back down, while maintaining the lumbar
spine in a neutral position.
Rolling from side to side;
30 repetitions
The patient is in a sidelying position. The patient
performs an ADIM and then rolls from one side to
the other, while maintaining a neutral position of
the lumbar spine. The patient then returns to the
starting position.
Squatting; 30 repetitions The patient leans against a wall and performs an
ADIM. The patient then slides down along the wall
until the knees are at a 45 angle, while maintain-
ing a neutral spine position. The position is held
for 5 seconds, and the patient returns to the start-
ing position.
Lifting; 30 repetitions The patient stands in front of a standard chair. The
patient performs an ADIM and then picks up a 2-
to 3-kg weight placed on the chair and lifts it to a
shelf at shoulder level. The weight is then returned
to the chair, and the patient returns to the starting
position. The patient maintains a neutral position
of the lumbar spine throughout the performance
of the activity.
APPENDIX A
44-01 Rabin.indd 6 12/18/2013 6:15:50 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
journal of orthopaedic & sports physical therapy | volume 44 | number 1 | january 2014 | B7
Exercise or Activity/Criteria
for Progression Description
Stage 3 (continued)
Vacuuming, swiping; patient
progresses to 3 minutes of
continuous activity
The patient performs a vacuuming/swiping motion
while performing an ADIM and maintaining a neu-
tral position of the lumbar spine.
Abbreviation: ADIM, abdominal drawing-in maneuver.
APPENDIX A
MANUAL THERAPY PROGRAM
Manual Techniques
Technique or Stretch/Dosage Description
Lumbosacral thrust manipulation;
up to 2 thrusts on each side
The therapist sidebends the patient toward the
side to be manipulated and rotates the trunk in
an opposite direction until the pelvis lifts of the
table. The therapist then places his/her hand on
the anterior superior iliac spine on the side to be
manipulated, takes up the slack, and applies a
high-velocity, low-amplitude thrust in the direction
of the table.
Lumbar thrust manipulation;
up to 2 thrusts on each side
The therapist exes the hip until motion is detected
at the L4-5 segment. The therapist then rotates
the upper trunk backward until motion is detected
at the L4-5 segment. The therapist then rolls the
patient toward him/her and stretches the segment
to its end range. The therapist then applies a high-
velocity, low-amplitude thrust.
APPENDIX B
44-01 Rabin.indd 7 12/18/2013 6:15:51 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
B8 | january 2014 | volume 44 | number 1 | journal of orthopaedic & sports physical therapy
[ RESEARCH REPORT ]
Technique or Stretch/Dosage Description
Upper lumbar thrust manipulation;
up to 2 thrusts on each side
The patient places both arms on top of the therapists
shoulder. The therapist places the hypothenar
eminence of 1 hand over the transverse process of
the segment to be manipulated. The therapist then
rotates the patient toward him/her and sidebends
away. The therapist then applies a high-velocity,
low-amplitude thrust in a forward direction (rotat-
ing the patient toward him/her).
Posterior/anterior nonthrust mobilization;
40 seconds, 3 repetitions over each
segment at the highest grade tolerated
The therapist places the thenar eminence of 1 hand
(mobilizing hand) over the spinous process of the
segment to be mobilized. The therapist places the
opposite hand over the dorsum of the mobilizing
hand and locks his/her elbows. The therapist then
applies a posterior/anterior force over the segment
in an oscillatory fashion with 1 to 2 oscillations per
second.
Hamstring stretch; 30 seconds,
3 repetitions on each leg
The therapist exes the hip to 90 and then extends
the knee until the patient reports a stretching sen-
sation behind his/her knee.
APPENDIX B
44-01 Rabin.indd 8 12/18/2013 6:15:51 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
journal of orthopaedic & sports physical therapy | volume 44 | number 1 | january 2014 | B9
Technique or Stretch/Dosage Description
Iliopsoas stretch; 30 seconds,
3 repetitions on each leg
The patient maintains 1 knee close to his/her chest.
The therapist lowers the opposite leg over the
edge of the table into hip extension (while keeping
the knee straight) until a stretching sensation is
reported by the patient.
Quadriceps stretch; 30 seconds,
3 repetitions on each leg
The patient maintains 1 knee close to his/her chest.
The therapist lowers the opposite leg over the edge
of the table into hip extension and knee exion
until a stretching sensation is experienced by the
patient.
Tensor fascia lata stretch; 30 seconds,
3 repetitions on each leg
The patient maintains 1 knee close to his/her chest.
The therapist lowers the opposite leg over the edge
of the table into hip extension and knee exion.
The therapist then uses his/her leg to externally
rotate and adduct the patients hip until a stretch-
ing sensation is reported.
APPENDIX B
44-01 Rabin.indd 9 12/18/2013 6:15:51 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
B10 | january 2014 | volume 44 | number 1 | journal of orthopaedic & sports physical therapy
[ RESEARCH REPORT ]
Technique or Stretch/Dosage Description
Piriformis stretch; 30 seconds,
3 repetitions on each leg
The therapist exes the patients hip and knee to 90
and then fully externally rotates the patients hip.
The therapist then stretches the hip into further
exion and adduction (pointing the knee toward
the opposite shoulder of the patient). The motion
continues until the patient reports a stretching
sensation over the ipsilateral buttock.
Range-of-Motion and Flexibility Exercises
Exercise or Stretch/Dosage Description
Cat horse; 30 repetitions, 4 sets The patient curls his/her back up and down in a
comfortable, pain-free range.
Prone press-up; 10 seconds,
10 repetitions
The patient presses up on both hands, extending
his/her spine in a pain-free range. The patient
holds this position for 10 seconds and returns to
the starting position.
APPENDIX B
44-01 Rabin.indd 10 12/18/2013 6:15:52 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
journal of orthopaedic & sports physical therapy | volume 44 | number 1 | january 2014 | B11
Exercise or Stretch/Dosage Description
Standing lumbar extension; 3 seconds,
10 repetitions
The patient leans back and extends the lumbar spine
in a pain-free range. The patient holds the position
for 3 seconds and returns to the starting position.
Quadruped exion; 10 seconds,
10 repetitions
From a quadruped position, the patient brings his/
her buttocks toward the heels to create exion of
the lumbar spine. The patient holds the position
for 10 seconds and returns to the starting position.
Sidelying trunk rotation; 10 seconds,
10 repetitions on each side
The patient presses the upper knee down to rotate
the pelvis toward the table, while rotating the
shoulders up (toward the ceiling) to create maxi-
mal trunk rotation. The patient holds the position
for 10 seconds and returns to the starting position.
APPENDIX B
44-01 Rabin.indd 11 12/18/2013 6:15:52 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
B12 | january 2014 | volume 44 | number 1 | journal of orthopaedic & sports physical therapy
[ RESEARCH REPORT ]
Exercise or Stretch/Dosage Description
Hip exor stretch; 30 seconds,
3 repetitions on each leg
From a half-kneeling position, the patient performs
a posterior pelvic tilt and then leans forward until
a stretch is felt in the front of the hip. The patient
holds the position for 30 seconds and returns to
the starting position.
Quadriceps stretch; 30 seconds,
3 repetitions on each leg
The patient uses a towel/belt to pull the foot up to-
ward his/her buttock (knee exion) until a stretch
is felt in the anterior thigh. The patient holds the
position for 30 seconds and returns to the starting
position.
APPENDIX B
44-01 Rabin.indd 12 12/18/2013 6:15:52 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
journal of orthopaedic & sports physical therapy | volume 44 | number 1 | january 2014 | B13
Exercise or Stretch/Dosage Description
Hamstring stretch; 30 seconds,
3 repetitions on each leg
The patient extends the knee until a stretch is felt in
the posterior aspect of the knee/thigh. The patient
holds the position for 30 seconds and returns to
the starting position.
Piriformis stretch; 30 seconds,
3 repetitions on each leg
The patient crosses 1 leg over the opposite exed
knee. The patient uses a towel to pull the bottom
knee toward his/her shoulder until a stretch is
felt in the opposite buttock. The patient holds the
position for 30 seconds and returns to the starting
position.
APPENDIX B
44-01 Rabin.indd 13 12/18/2013 6:15:52 PM
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
This article has been cited by:
1. John D. Childs, Timothy W. Flynn. 2014. Clinical Decision Making for Low Back Pain: A Step in the Right Direction.
Journal of Orthopaedic & Sports Physical Therapy 44:1, 1-2. [Abstract] [Full Text] [PDF] [PDF Plus]
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
D
o
w
n
l
o
a
d
e
d
f
r
o
m
w
w
w
.
j
o
s
p
t
.
o
r
g
a
t
o
n
A
u
g
u
s
t
9
,
2
0
1
4
.
F
o
r
p
e
r
s
o
n
a
l
u
s
e
o
n
l
y
.
N
o
o
t
h
e
r
u
s
e
s
w
i
t
h
o
u
t
p
e
r
m
i
s
s
i
o
n
.
C
o
p
y
r
i
g
h
t
2
0
1
4
J
o
u
r
n
a
l
o
f
O
r
t
h
o
p
a
e
d
i
c
&
S
p
o
r
t
s
P
h
y
s
i
c
a
l
T
h
e
r
a
p
y
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Focus On Adult Health Medical Surgical Nursing Pellico Edition Test BankDocument8 paginiFocus On Adult Health Medical Surgical Nursing Pellico Edition Test BankCarolineAndersoneacmg100% (33)
- Lumbar Facet Syndrome - BogdukDocument8 paginiLumbar Facet Syndrome - BogdukSamSchroetkeÎncă nu există evaluări
- Jurnal Low Back Pain PDFDocument5 paginiJurnal Low Back Pain PDFFikar AxlrosesÎncă nu există evaluări
- Pain Definitions - On The Definitions and Physiology of Back Pain, Referred Pain, and Radicular PainbogdukDocument3 paginiPain Definitions - On The Definitions and Physiology of Back Pain, Referred Pain, and Radicular PainbogdukSamSchroetkeÎncă nu există evaluări
- Pain Definitions - On The Definitions and Physiology of Back Pain, Referred Pain, and Radicular PainbogdukDocument3 paginiPain Definitions - On The Definitions and Physiology of Back Pain, Referred Pain, and Radicular PainbogdukSamSchroetkeÎncă nu există evaluări
- Ebook Comprehensive Dermatologic Drug Therapy PDF Full Chapter PDFDocument64 paginiEbook Comprehensive Dermatologic Drug Therapy PDF Full Chapter PDFvictor.vega375100% (28)
- UntitledDocument8 paginiUntitledapi-271638639Încă nu există evaluări
- DNB Questions Year WiseDocument104 paginiDNB Questions Year Wiseakish4uÎncă nu există evaluări
- New York Imaging Specialists Announces Grand Opening in Port Jefferson StationDocument2 paginiNew York Imaging Specialists Announces Grand Opening in Port Jefferson StationPR.comÎncă nu există evaluări
- Transverse MyelitisDocument7 paginiTransverse MyelitisAmr BashaÎncă nu există evaluări
- D10W (Anything D5W) - 3% Normal Saline ( 0.9% Hypertonic) - Mannitol - Parenteral NutritionDocument6 paginiD10W (Anything D5W) - 3% Normal Saline ( 0.9% Hypertonic) - Mannitol - Parenteral NutritionAlec Anon100% (1)
- Jurnal Porio 1Document3 paginiJurnal Porio 1Neo YustindraÎncă nu există evaluări
- Annotated BibliographyDocument5 paginiAnnotated Bibliographyapi-286443025Încă nu există evaluări
- Ministry Health Medicines Formulary 1 2015Document371 paginiMinistry Health Medicines Formulary 1 2015David Lim Su ShenÎncă nu există evaluări
- D5LRDocument2 paginiD5LRLouiseville Ann Arcilla PilÎncă nu există evaluări
- Ake Quick Action If Someone Is Choking On A Swallowed ObjectDocument29 paginiAke Quick Action If Someone Is Choking On A Swallowed ObjectYAMINIPRIYANÎncă nu există evaluări
- Acts Reinforcement Mar2020 PDFDocument8 paginiActs Reinforcement Mar2020 PDFErika Kate MedadoÎncă nu există evaluări
- Immunology: 'S CompanionsDocument74 paginiImmunology: 'S CompanionsRoahit RajanÎncă nu există evaluări
- Kebutuhsn Implan Urologi Desember 2021 - November 2022 - 3Document32 paginiKebutuhsn Implan Urologi Desember 2021 - November 2022 - 3Ilham ApriansyahÎncă nu există evaluări
- Importance of Mental HealthDocument2 paginiImportance of Mental HealthCp CsÎncă nu există evaluări
- 5 Patcharee Komvilaisak - Approaching To Pancytopenia 24112017Document43 pagini5 Patcharee Komvilaisak - Approaching To Pancytopenia 24112017Satvik BansalÎncă nu există evaluări
- TRS 987Document286 paginiTRS 987NGOTTAÎncă nu există evaluări
- Male InfertilityDocument38 paginiMale InfertilityPrincessMagnoliaFranciscoLlantoÎncă nu există evaluări
- Hepatic Dysfunction in Dengue Fever - A ProspectiveDocument20 paginiHepatic Dysfunction in Dengue Fever - A ProspectiveSanjay RaoÎncă nu există evaluări
- Pocket-Book MCH Emergencies - English PDFDocument286 paginiPocket-Book MCH Emergencies - English PDFAbigail Kusi-Amponsah100% (1)
- Baxter Revaclear - Datasheet - 2020 - A4 - GBU-RC38-200001 - Low - 0Document2 paginiBaxter Revaclear - Datasheet - 2020 - A4 - GBU-RC38-200001 - Low - 0Black MonkeyÎncă nu există evaluări
- Drug Study - Vitamin B ComplexDocument1 paginăDrug Study - Vitamin B ComplexmikErlh0% (1)
- Breast Cancer Diagnostic Imaging in Dharmais Cancer HospitalDocument32 paginiBreast Cancer Diagnostic Imaging in Dharmais Cancer HospitalIndonesian Journal of CancerÎncă nu există evaluări
- Spotting Signs of AutismDocument23 paginiSpotting Signs of AutismAutism Parenting100% (3)
- Vaccination Form (Sample)Document1 paginăVaccination Form (Sample)Godfrey Loth Sales Alcansare Jr.Încă nu există evaluări
- 7 Chapter 3 Goals of Prevention Methods of PreventionDocument4 pagini7 Chapter 3 Goals of Prevention Methods of Preventionaryam aliÎncă nu există evaluări
- DISCHARGE PLANNING - AnemiaDocument2 paginiDISCHARGE PLANNING - AnemiaJOEY MEAD ARUGAY0% (1)
- Lecture 6 - AnxietyDocument32 paginiLecture 6 - AnxietyPatrick McClairÎncă nu există evaluări
- Antihypnotics and AnxiolyticsDocument12 paginiAntihypnotics and AnxiolyticsSabreena NordinÎncă nu există evaluări