Documente Academic
Documente Profesional
Documente Cultură
Nres1dm-Chapter I and II
Încărcat de
mlmmandap0 evaluări0% au considerat acest document util (0 voturi)
89 vizualizări35 paginikjlkl
Titlu original
Nres1dm-Chapter i and II
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentkjlkl
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
89 vizualizări35 paginiNres1dm-Chapter I and II
Încărcat de
mlmmandapkjlkl
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 35
1 | P a g e
THE GREATEST FACTORS
AFFECTING THE LENGTH OF CONFINEMENT
AMONGST DIABETIC PATIENTS IN THE PHILIPPINES
A thesis presented to the faculty of the College of Nursing at Dr. Carlos S. Lanting College
In partial fulfillment requirements for Bachelor of Science in Nursing
Nursing Research Class
By:
Level III Nursing Students
Cabie, Marielle
Culala, John Christopher
Dychinco, Franklin Gerard
Gaspar, Ryan James
Javier, Raquel
Pulido, Blite Khirsteen
Saleumpatchay, Mona Lee
Saygo, Maria Vienna Rose
Valenzuela, Jennifer
2 | P a g e
Submitted to:
Sir Leonilo M. Cruz R.N., M.A.N.
CHAPTER I- INTRODUCTION:
Perhaps there are still many Filipinos, who, until now are still not fully aware what
Diabetes is all about. Maybe for some they still associate it with just poor diet like eating too
many sweets, drinking large amounts of soft drinks or too much consumption of rice during meal
time or just because their grandmother, mother or uncle had it thats why they have it too.
Diabetes is a kind of sickness that affects any person from different walks of life. A wealthy and
educated individual can and may have it just as the same with someone poor and uneducated. Its
a disease known to many but does everyone really know about it? Does everyone affected by it
or family members or caregivers of patients with diabetes really know how to deal with it?
The Philippines ranks 10th among countries with the highest diabetes incidence
worldwide*. (According to the website charantia.com, Diabetes Crisis in the Philippines)
An estimated 6 Million Filipinos know they have diabetes. Another 6 Million Filipinos have
diabetes but do not know they have it. Health experts believe many more have impaired glucose
tolerance (IGT) and are prone to diabetes. According to the website of DOH, Diabetes is ranked
8 in the leading causes of mortality from Year 2004-2009. On the global picture, About 347
million people worldwide have diabetes (According to WHO, as of October, 2013). With all
these facts in mind, one can say, it really is prevalent and so, something must be done to deter the
continuous spread of such a disease or at least, improve the diabetic patients state of health,
amidst illness because, Unless we act now to change our lifestyle of too much sweet and fatty
foods and too little exercise, our path will lead us to the gaping mouth of a diabetes epidemic. (*
Source: US Centers for Disease Control and Prevention 2004 press statement)
3 | P a g e
As nursing students here at the Dr. Carlos Lanting College, it is now our goal to not only
educate ourselves with this type of disease but on how we can partake in educating our clients
and their families regarding their condition. One of the most common problems our diabetic
clients are facing is the prolonged confinement in various hospitals where they are admitted.
Clearly there are several contributing factors as to why they stay longer than expected and we
wish to find out the underlying reasons why and how we can potentially offer a solution. As
nurses, we believe that the key to a patients immediate recovery or healing does not always
depend and rely on medications, it is our invaluable care, touch and comfort that sometimes,
more often than not, makes the difference.
THEORETICAL FRAMEWORK:
Sister Callista Roys Adaptation Model of Nursing
In 1976, Sister Callista Roy developed the Adaptation Model of Nursing, a prominent nursing
theory. Nursing theories frame, explain or define the provision of nursing care. Roy's model sees
the individual as a set of interrelated systems (biological, psychological and social). The
individual strives to maintain a balance between these systems and the outside world, but there is
no absolute level of balance. Individuals strive to live within a unique band in which he or she
can cope adequately. The paradigm below shows how the interrelated systems of human being
contributes to the coping process and adaptation.
4 | P a g e
The concept of a system as applied to an individual. Roy conceptualizes the person in a holistic
perspective. Individual aspects of parts act together to form a unified being. Additionally, as
living systems, persons are in constant interaction with their environments. Between the system
and the environment occurs an exchange of information, matter, and energy. Characteristics of a
system include inputs, outputs, controls, and feedback.
Major concepts
Environment - Conditions, circumstances and influences that affect the development and
behavior of humans as adaptive systems.
Health - A state and process of being and becoming integrated and whole.
Person - The human adaptive system and defined as a whole with parts that function as a unity
for some purpose. Human systems include people groups organizations, communities, and
5 | P a g e
society as a whole. (Roy & Andrews, 1999)
Goal of nursing
The promotion of adaptation in each of the four modes..
Adaptation - The process and outcome whereby thinking and feeling persons as individuals or
in groups use conscious awareness and choice to create human and environmental integration.
Four Adaptive Modes
1. Physiologic-physical mode: physical and chemical processes involved in the function and
activities of living organisms; the underlying need is physiologic integrity as seen in the degree
of wholeness achieved through adaptation to changes in needs. In groups, this is the manner in
which human systems manifest adaptation relative to basic operating resources. The basic
need of this mode is composed of the needs associated with oxygenation, nutrition, elimination,
activity and rest, and protection. The complex processes of this mode are associated with the
senses, fluid and electrolytes, neurologic function, and endocrine function.
2. Self-concept-group identity mode: focuses on psychological and spiritual integrity and a
sense of unity, meaning, purposefulness in the universe.
3. Role function mode: refers to the roles that individuals occupy in society fulfilling the need
for social integrity; it is knowing who one is, in relation to others.
4. Interdependence mode: the close relationships of people and their purpose, structure and
development individually and in groups and the adaptation potential of these relationships.
6 | P a g e
Adaptive responses are those that promote the integrity of the person. The persons integrity, or
wholeness, is behaviorally demonstrated when the person is able to meet the goals in terms of
survival, growth, reproduction and mastery. Ineffective responses do not support these goals.
(Roy & Andrews, 1991)
Coping mechanisms describe the control processes of the person as an adaptive system. Some
coping mechanisms are inherited or genetic, such as white blood cell defense mechanism against
bacteria that seek to invade the body. Other mechanisms are learned, such as the use of
antiseptics to cleanse a wound.
Two Coping Subsytems
A. Cognator subsystem - A major coping process involving four cognitive-emotive
channels: perceptual and information processing, learning, judgment, and emotion.
B. Regulator subsystem - A basic type of adaptive process that responds automatically
through neural, chemical, and endocrine coping channels.
Focal stimuli - Those stimuli that are the proximate causes of the situation.
7 | P a g e
Contextual stimuli - All other stimuli in the internal or external environment, which may or
may not affect the situation.
Residual stimuli - Those immeasurable and unknowable stimuli that also exist and may
affect the situation.
When using Roys model as a theoretical framework, the following can serve as a guide for the
assessment of Diabetic patients.
I. Adaptation Modes
A. Physiologic Mode
1. To what extent is the patient able to meet his/her basic survival needs?
2. Is there any difficulty in meeting such basic survival needs?
B. Self-Concept Mode
1. How does the clients view themselves in terms of their ability to meet goals? To
what extent do they see themselves as self-directed? Other directed?
2. What are the values of the patient?
C. Role Function Mode
1. Describe the roles assumed by the patient.
2. To what extent are the roles supportive, in conflict, reflective of role overload?
3. How are the decisions reached?
D. Interdependence Mode
1. To what extent are family members, health care team and subsystems within the
environment allowed the patient to be independent in goal identification and
achievement?
8 | P a g e
2. To what extent are the members supportive of one another?
3. What are the familys support systems? Significant others?
4. To what extent is the patient open to information and assistance from others
5. Describe the interaction patterns the patient engage with his/her support systems
and multidisciplinary team, during the period of confinement.
9 | P a g e
CONCEPTUAL FRAMEWORK: THE SELF CARE AND ADAPTATION CONTINUUM
Upon conceptualizing our perspective and theoretical framework in this study, we arrived
at the major governing assumption which states that the length of confinement among
patients with Diabetes mellitus is greatly affected by the patients ability and will to
achieve self-care, that is to say that the length of confinement is inversely proportional
to self care continuum. We define self-care continuum as the state of the awareness of
and understanding the multidimensionality of the self and varying factors affecting
adaptation. The multidimensionality of the self utilizes Sister Callista Roys human
subsystems as its component parts, which includes; the physiological system, self
concept, interdependence and role function. The following are our 14-fold major
concepts:
1. The supporting premise that justifies the major governing assumption mentioned above is
that the patients, in the first place, will not be spending long period of hospital stay if
there are no aggravating factors, which, per se, are as complex as the multidimensionality
of the self and the mileu.
2. The consummation of self care continuum is measured by the progress of the patients
coping mechanisms ( the subsystems according to Roy), through the adaptation
continuum.
3. The adaptation continuum, which is represented by the X-axis in the paradigm, implies
the vague process of withstanding a crisis (or illness state), so as to achieve recovery and
ideal health or if not, at least, a relative state of health. It is affected by the
multidimensionality of internal and external factors. The internal factors include the
10 | P a g e
patients physiologic system, self concept, knowledge, cognition of the problem, beliefs,
perceptions and values. External factors include the rest of the affecting variables that are
beyond patients control. (Ex. Environment, support system, medical management,
nursing care quality, financial aspect etc..). Such factors, be it internal or external, can
either be a barrier against or synergistic with self care continuum.
4. The Multi-Factor Variables are group of multi-dimensional variables pertaining to the
internal and external factors affecting the patients Self-care continuum, coping
mechanisms, adaptation, multi-factor health barrier continuum/ health synergistic
continuum and length of hospital confinement.
5. The Relative state of Health, is the patients health state that is relative to condition (or
pathological condition or disease process). It means that any person can be considered
healthy according to their own conditions, as long as majority of the Multi-factor
Variables in the y-axis will purposively work towards pushing the patients self-care
continuum to the zone of good adaptation.
6. Multi-factor health barrier continuum is the measure of how much the factors become
antagonistic with the self care-continuum, adaptation and coping mechanisms. It pulls the
patient back to the zone of poor adaptation.
7. Multi-factor health synergistic continuum is the measure of how much the factors are
purposively working well towards the patients good adaptation. It pushes the patient
away from the zone of poor adaptation.
8. The nurses, with the multidisciplinary care team, have the unique role in therapeutically
manipulating the external factors, towards the betterment of clients adaptation. As for
example, convincing the client to increase his/her will to achieve self-care, via educating
the client and the support system in assisting the latter. The ultimate goal of Nursing is to
move the patients adaptation, self-care and coping mechanism continuum towards the
nearest zone of Good adaptation.
11 | P a g e
9. The length of hospital confinement pertains to the period which begins at the patients
admission and ends as soon as the patient was discharged.
10. There are three different goals of the self- care and adaptation continuum, namely; The
5.1. Ideal health, which is the state of not merely the absence of disease or infirmity but
wellness in all aspects (as defined by the WHO), 5.2. Recovery, the state of the resolution
of pathological condition and 5.3. is the Relative state of health. The 3
rd
goal is the more
realistic version of the ideal health, and therefore, the practicable goal of this conceptual
model in the context of diabetic patients, because, it is a fact that it is almost impossible
for them to totally eliminate such infirmity from their body.
11. The adaptation continuum is composed of two different levels, 6.1. Zone of Good
adaptation and 6.2. Zone of Poor Adaptation. Good adaptation, is when coping
mechanisms are being used purposively, and thus, adaptive, while poor adaptation, on the
contrary, is maladaptive.
12. The zone of good adaptation starts at the point of equilibrium between the graph of the
length of confinement and self-care continuum graph. It pertains to the point at which the
patient has the ability for self-care, or at least, manifests the will for self-care.
13. The efficiency of the methods that will be implemented in achieving the self-care
continuum goals can attain its optimum levels by focusing on the greatest factors that
affect the patients length of hospital confinement.
14. Self-care is equal to the manifestation of adaptive behaviors..
12 | P a g e
THE PARADIGM: Self care and Adaptation Continuum
The figure below represents the paradigm that depicts the conceptual framework.
13 | P a g e
STATEMENT OF THE PROBLEM:
Zone of Poor Adaptation
Adaptation Boundary
Length of Hospital Confinement
Multi-factor Health Barrier
Continuum
Self Care Continuum
Multi-factor Health Synergistic
continuum
M
u
l
t
i
-
F
a
c
t
o
r
V
a
r
i
b
l
e
s
(
I
n
t
e
r
n
a
l
/
E
x
t
e
r
n
a
l
)
Equilibrium
14 | P a g e
The study will explore the possible factors among diabetic patients at QMMC regarding
the length of confinement/stay at the hospital. Specifically, it sought to answer the following
questions:
1. What is the personal profile of the diabetic patients as to:
1. Age
2. Gender
3. Occupation
4. Civil Status
5. Monthly Income of the Family (below 3000 above 50000)
6. Date of Confinement/ Admission
7. Length of Confinement (upon survey)
8. Educational attainment
2. What are the common complications causing confinement for diabetic patients?
3. What are some factors that affect the length of their stay at the hospital?
4. Does the length of their confinement affect their family members? How does diabetic patients
affect the family members? (Financial, social, emotional, physical)
5. What are their coping mechanisms during the period of their stay? Is it effective?
15 | P a g e
ASSUMPTIONS:
1. A diabetic patient may have blurry visions. Or worse, diabetic retinopathy.
2. A patient with diabetes might have difficulties in wound healing process. And might
have complaints of foul smelling odor from the wound.
3. A diabetic patient who is being confined in a long period of time might have some
financial issues and might not be able to meet his daily hospital bills and medications.
4. The negligence and carelessness of a health care team member, may lead to
complications that should not suppose to happen to the patients. For example: Bed
sores, pulmonary embolism, infections, etc.
5. Environmental status of the hospital delays the healing process of the patients wound
and brings more infections to the patient.
6. Multi-organ dysfunction is one of the leading causes of being confined in the hospital in
diabetic patients.
7. The patients family and primary care giver/s, shoulders the burden of care.
8. The goal of the health care team, especially the nurses, is to assist the patient for better
adaptation.
16 | P a g e
HYPOTHESES:
1. There is a significant correlation between the diabetic patients length of
hospital confinement and compliance with medical regimen.
2. There is a significant difference between the length of diabetic patients length
of hospital confinement and presence of co-morbid conditions.
3. There is no difference between the diabetic patients educational attainment
and degree of compliance with medical regimen.
4. There is no significant correlation between the diabetic patients socioeconomic
status and degree of compliance with medical regimen.
5. There is a significant relationship between a diabetic patients adaptation and
quality of health care.
17 | P a g e
SIGNIFICANCE OF THE STUDY
OBJECTIVES:
1. To identify the factors that greatly affects the length of hospital confinement among patients
with diabetes.
2. To explain how such factors contributes to the length of hospital confinement.
3. To identify the most effective nursing management in terms of discharge plan and health
teaching towards minimizing the length of confinement and alleviating unwanted effects of the
disease process.
This study will help, in providing careful planning and knowledge on how to teach patients about
diabetes, helping them create a diet plan that caters to there personal needs and the demands of
there particular disease, instruct them to maintain a healthy weight, exercise regularly, go
through each aspect of her medical needs and how to take care of them: this includes insulin
shots, measuring glucose levels and monitoring her intake of sodium and sugar.
The aim of patient education especially for people with diabetes is to improve their knowledge,
skills and confidence, enabling them to take increasing control of their own condition and
integrate effective self-management into their daily lives. High-quality structured education can
have a profound effect on health outcomes and can significantly improve quality of life by
follow a consistent meal plan and schedule, eat the right amount of carbohydrate foods for good
blood sugar control, choose lower fat options and limit saturated fats, drink plenty of water.
18 | P a g e
At the end of the study this will benefit the nursing students, clinical nurses, people, diabetic
patients and researchers.
A. The nursing students and clinical nurses will benefit through acquiring new knowledge
about more therapeutic nursing management and care of patients with diabetes.
B. This study serves as an aid in providing a significant amount of information to the people
who are not aware of Diabetes and the factors affecting the length of confinement and its
damaging effects to a person as a whole, thereby possessing the necessary knowledge to
handle and make decisions on this situation.
C. Diabetic patient will benefit by increasing their awareness about diabetes and promoting
healthy coping techniques, as manifested for example, by fully understanding the
importance of healthy eating strategies, and reducing risk for complications.
D. The Researcher will benefit through awareness why the confinement of diabetic patient
prolonged, and they will improve better the quality of care.
19 | P a g e
DEFINITION OF TERMS
Adaptation - The process and outcome whereby thinking and feeling persons as individuals or in
groups use conscious awareness and choice to create human and environmental integration.
Amputation - is the removal of a body extremity by trauma, prolonged constriction, or surgery.
Bed sores - are localized injuries to the skin and/or underlying tissue that usually occur over a
bony prominence as a result of pressure, or pressure in combination with shear and/or friction.
Blood Sugar - is the amount of glucose (sugar) present in the blood of a human or animal.
20 | P a g e
Blindness is the condition of lacking visual perception due to physiological or neurological
factors.
Blood Pressure - is the pressure exerted by circulating blood upon the walls of blood vessels, and
is one of the principal vital signs.
Contextual stimuli - All other stimuli in the internal or external environment, which may or may
not affect the situation.
Cognator subsystem - A major coping process involving four cognitive-emotive channels:
perceptual and information processing, learning, judgment, and emotion.
Carbohydrates - means any food that is particularly rich in the complex carbohydrate starch
(such as cereals, bread, and pasta) or simple carbohydrates, such as sugar (found in candy, jams,
and desserts).
Cholesterol - A fat-like substance that is made by the human body and eaten in animal products.
Cholesterol is used to form cell membranes and process hormones and vitamin D.
Community-acquired Infection - an infection contracted outside of a health care setting or an
infection present on admission.
21 | P a g e
Cardiovascular Disease - is a class of diseases that involve the heart, the blood vessels (arteries,
capillaries, and veins) or both.
Calories - A unit of heat measurement used in nutrition to measure the energy value of foods. A
calorie is the amount of heat energy needed to raise the temperature of 1 kilogram of water 1C.
Coping Mechanism - any effort directed to stress management, including task-oriented and ego
defense mechanisms, the factors that enable an individual to regain emotional equilibrium after a
stressful experience. It may be an unconscious process.
Diabetes mellitus - Diabetes mellitus is a condition in which the pancreas no longer produces
enough insulin or cells stop responding to the insulin that is produced, so that glucose in the
blood cannot be absorbed into the cells of the body.
End-stage Renal Disease is a chronic irreversible renal failure.
Environment - The totality of circumstances surrounding an organism or group of organisms,
especially the combination of external physical conditions that affect and influence the growth,
development, and survival of organisms.
22 | P a g e
Equilibrium - A condition in which all influences acting upon it are canceled by others, resulting
in a stable, balanced, or unchanging system.
Focal stimuli - Those stimuli that are the proximate causes of the situation.
Gestational Diabetes - Gestational diabetes is a condition that occurs during pregnancy. Like
other forms of diabetes, gestational diabetes involves a defect in the way the body processes and
uses sugars (glucose) in the diet.
Health - a condition of physical, mental, and social well-being and the absence of disease or
other abnormal condition.
Hyperglycemia - Condition characterized by excessively high levels of glucose in the blood, and
occurs when the body does not have enough insulin or cannot use the insulin it does have to turn
glucose into energy.
Healthy Diet - provides the body with essential nutrition: fluid, adequate essential amino acids
from protein, essential fatty acids, vitamins, minerals, and adequate calories.
Insulin - A hormone secreted by the pancreas in response to high blood sugar levels that induces
hypoglycemia. Insulin regulates the body's use of glucose and the levels of glucose in the blood
by acting to open the cells so that they can intake glucose.
23 | P a g e
Infection - invasion and multiplication of microorganisms in body tissues, especially that causing
local cellular injury due to competitive metabolism, toxins, intracellular replication, or antigen-
antibody response.
Length of confinement is the duration of stay of a patient in a hospital.
Mental stress - A general term encompassing mental arousal and/or emotional stress.
Multi-factor health barrier continuum - is the measure of how much the factors become
antagonistic with the self care-continuum, adaptation and coping mechanisms. It pulls the patient
back to the zone of poor adaptation.
Multi-factor health synergistic continuum - is the measure of how much the factors are
purposively working well towards the patients good adaptation. It pushes the patient away from
the zone of poor adaptation.
Multi-Factor Variables- are group of multi-dimensional variables pertaining to the internal and
external factors affecting the patients Self-care continuum, coping mechanisms, adaptation,
multi-factor health barrier continuum/ health synergistic continuum and length of hospital
confinement.
24 | P a g e
Multiple organ dysfunction - is the presence of altered organ function in acutely ill patients such
that homeostasis cannot be maintained without intervention. It usually involves two or more
organ systems.
Mortality - the ratio of the total number of deaths to the total number of the population during a
specified time period.
Obesity - is an abnormal accumulation of body fat, usually 20% or more over an individual's
ideal body weight.
Overweight - more than normal in body weight after adjustment for height, body build, and age,
or 10% to 20% above the person's "desirable" body weight.
Omega-3 Fatty Acids - Any of various polyunsaturated fatty acids that are found primarily in
fish, fish oils, vegetable oils, and leafy green vegetables, and that seem to reduce the risk of
stroke and heart attack.
Proteins - the principal constituents of the protoplasm of all cells, are of high molecular weight
and consist of -amino acids joined by peptide linkages
25 | P a g e
Pulmonary embolism - is an obstruction of a blood vessel in the lungs, usually due to a blood
clot, which blocks a coronary artery.
Self-care Continuum is a sequence of care of oneself without medical, professional, or other
assistance or oversight.
Self-Concept - the composite of ideas, feelings, and attitudes that a person has about his or her
own identity, worth, capabilities, and limitations.
Type 1 Diabetes Mellitus - is a form of diabetes mellitus that results from the autoimmune
destruction of the insulin-producing beta cells in the pancreas.
Type 2 Diabetes Mellitus - is a metabolic disorder that is characterized by high blood sugar in
the context of insulin resistance and relative lack of insulin.
26 | P a g e
SCOPE AND DELIMITATTION
Research Problem: This research seeks to determine the factors affecting the length of
confinement among diabetic patients.
General Purpose: This study aims to focus on the identified factors as the determinant/s on
the formulation of better care plan, more effective health teaching and implementation of
necessary interventions in the care of diabetic patients in the hospital.
Topic studied: The demographic profile of the selected diabetic patients, their coping
mechanism, the effect of their condition on their primary care giver, and how all such
factors and variables affects their coping and adaptation.
Population: 15 selected Diabetic patients confined on the medical-surgical wards of Quirino
Memorial Medical Center.
Locale of the study: Quirino Memorial Medical Center- Project 4, Cubao, Quezon City.
Period of Study: Second semester of the School Year 2013-2014 to the end of the first
semester of the School year 2014-2015.
27 | P a g e
CHAPTER II- REVIEW OF THE RELATED
LITERATURES
The burden of diabetes is increasing globally, particularly in developing countries. The causes
are a complex, but are in large part due to rapid increases in overweight, obesity and physical
inactivity.
Although there is good evidence that a large proportion of cases of diabetes and its complications
can be prevented by a healthy diet, regular physical activity, maintaining a normal body weight
and avoiding tobacco, this evidence is not widely implemented. Coordinated action is needed
from the level of international and national policy to reduce exposure to the known risk factors
for diabetes and to improve access to and quality of care.
However, despite of the knowledge of these prevention efforts, still, there are about 347 million
people worldwide have diabetes and, in the local scenario, Diabetes Mellitus still ranks the 8
th
leading cause of mortality from 2004- 2009.
According to the website of DOH, Diabetes is ranked 8 in the leading causes of mortality from Year
2004-2009
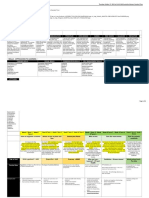
MORTALITY: TEN (10) LEADING CAUSES
NUMBER AND RATE/100,000 POPULATION
Philippines
5-Year Average (2004-2008) & 2009
28 | P a g e
CAUSES
5-Year Average
(2004-2008)
2009*
Number Rate Number Rate
1. Diseases of the Heart 82,290 94.5 100,908 109.4
2. Diseases of the Vascular System 55,999 64.3 65,489 71.0
3. Malignant Neoplasms 43,185 49.6 47,732 51.8
4. Pneumonia 35,756 41.1 42,642 46.2
5. Accidents** 34,704 39.9 35,990 39.0
6. Tuberculosis, all forms 25,376 29.2 25,470 27.6
7. Chronic lower respiratory diseases 20,830 24.0 22,755 24.7
8. Diabetes Mellitus 19,805 22.7 22,345 24.2
9.Nephritis, nephrotic syndrome and nephrosis 11,612 13.4 13,799 15.0
10. Certain conditions originating in the perinatal
period
12,590 14.5 11,514 12.5
Note: Excludes ill-defined and unknown causes of mortality
* reference year
** External causes of Mortality
REFERENCE: http://www.doh.gov.ph/node/198.html
10 facts about diabetes
(Reviewed October 2013 W.H.O.) (from: http://www.who.int/features/factfiles/diabetes/en/)
29 | P a g e
1. There is an emerging global epidemic of diabetes that can be traced back to rapid
increases in overweight, obesity and physical inactivity.
2. Diabetes is predicted to become the seventh leading cause of death in the world by the
year 2030.Total deaths from diabetes are projected to rise by more than 50% in the next
10 years.
3. There are two major forms of diabetes: Type 1 diabetes is characterized by a lack of
insulin production and type 2 diabetes results from the body's ineffective use of insulin.
4. A third type of diabetes is gestational diabetes. This type is characterized by
hyperglycaemia, or raised blood sugar, which has first appeared or been recognized
during pregnancy.
5. Type 2 diabetes is much more common than type 1 diabetes. Type 2 accounts for around
90% of all diabetes worldwide. Reports of type 2 diabetes in children previously rare
have increased worldwide. In some countries, it accounts for almost half of newly
diagnosed cases in children and adolescents.
6. Cardiovascular disease is responsible for between 50% and 80% of deaths in people with
diabetes. Diabetes has become one of the major causes of premature illness and death in
most countries, mainly through the increased risk of cardiovascular disease (CVD).
7. In 2004, an estimated 3.4 million people died from consequences of high fasting blood
sugar.
8. 80% of diabetes deaths occur in low- and middle-income countries. In developed
countries most people with diabetes are above the age of retirement, whereas in
developing countries those most frequently affected are aged between 35 and 64.
9. Diabetes is a leading cause of blindness, amputation and kidney failure.Lack of
awareness about diabetes, combined with insufficient access to health services and
essential medicines, can lead to complications such as blindness, amputation and kidney
failure.
30 | P a g e
10. Type 2 diabetes can be prevented. Thirty minutes of moderate-intensity physical activity
on most days and a healthy diet can drastically reduce the risk of developing type 2
diabetes. Type 1 diabetes cannot be prevented.
The above mentioned facts stated by the World Health Organization, suggests that, because co-
morbid conditions are very common, hospitalization will always be at hand.
When a person with diabetes is hospitalized, many factors can contribute to variations in blood
sugar or glucose levels. Stress, a different meal plan, various drugs, treatments and the illness for
which the person is being hospitalized for itself can all come into play for a patient with
diabetes.It's well known that excessive glucose levels can slow healing and boost infection risk.
The average length of stay was 5.4 days (4). Diabetes was the principal diagnosis in only 8% of
these hospitalizations. In addition to having a medical history of diabetes, patients presenting to
hospitals may have unrecognized diabetes or hospital-related hyperglycemia. Based on hospital
chart review, 64% of patients with hyperglycemia had preexisting diabetes or were recognized as
having new-onset diabetes during hospitalization. Thirty-six percent of the hyperglycemic
patients remained unrecognized as having diabetes in the discharge summary, although diabetes
or hyperglycemia was documented in the progress notes for one-third of these patients.
(http://care.diabetesjournals.org/content/27/2/553.long)
Patients with type 1 or type 2 diabetes mellitus are frequently admitted to a hospital, usually for
treatment of conditions other than the diabetes. In one study, 25 percent of patients with type 1
diabetes and 30 percent with type 2 diabetes had a hospital admission during one year; patients
with higher values for hemoglobin A1C (A1C) were at highest risk for admission. The
prevalence of diabetes rises with increasing age, as does the prevalence of other diseases; both
factors increase the likelihood that an older person admitted to a hospital will have diabetes.
31 | P a g e
Much of what was formerly done in hospital, including many surgical procedures, complex
diagnostic testing, or treatment of community-acquired infections, is now done in a clinic or at
home. However, the presence of diabetes might precipitate admission of a patient who would
otherwise be treated as an outpatient. Whether in hospital or not, glycemic control is likely to
become unstable in these patients because of the stress of the illness or procedure, the
concomitant changes in dietary intake and physical activity, and the frequent interruption of the
patient's usual antihyperglycemic regimen.
Once in the hospital, the length of stay and cost are greater for patients with diabetes than for
those without it. Efficient treatment of diabetes in hospital may be an important factor in limiting
the costs of care. .
http://www.uptodate.com/contents/management-of-diabetes-mellitus-in-hospitalized-patients
There are many factors that contribute in the confinement of diabetes patient, one of this factor is
the high level of blood glucose (hyperglycemia). Mental stress causes the body to produce
especially high levels of stress hormone, which drive to high level of glucose. There are some
ways to reduce mental health stress, first, teach your self to relax when under stress using deep-
breathing exercises or techniques you learn in a stress-management, second evaluate your
schedule and determine if you can make changes to relieve stress, third exercise regularly. The
length of confinement is depend on the severity of the disease, because diabetes would be treated
as outpatient. If you are diabetic patient either you confined in the hospital or outpatient, the
most important thing to do is monitoring and controlling your blood glucose.
DIABETES AND THE FILIPINO DIET
Published Friday, 12 April 2013 Written by Jeffrey O. Valisno
32 | P a g e
DIABETES is a chronic disease manifested through elevated blood sugar levels. A person with
diabetes does not have a normal production of insulin, which is a protein hormone that helps
sugar leave the blood and enter the cells of the body.
Here are some disturbing facts about diabetes in the Philippines:
Diabetes was the ninth leading cause of death from 1999 to 2002 in the Philippines. As of
2005, diabetes affected one in every 25 Filipinos.
Of every 100 deaths, five died of diabetes in 2005, from just two in 1999 says a report of the
National Epidemiology Center of the Department of Health (DoH). The number of deaths due to
diabetes grew the fastest among all diseases between 1999 and 2005 said the report -- from 9,749
reported diabetes cases in 1999, the number grew by 11.2% to 18,441 cases in 2005.
As of 2012, diabetes affects the lives of 9.7% of the adult population in the Philippines, said
Dr. Danilo F. Baldemor, diabetologist and immediate past president of the Philippine
Association of Diabetes Educators (PADE), Inc., during a press conference last month.
This number tends to double if we add the 12.5% of Filipinos who are at-risk of diabetes with
impaired glucose tolerance (IGT). Combined, one out of every five Filipino adults or
approximately 11 million has either prediabetes or diabetes, Mr. Baldemor explained.
DIET CHANGE
The doctor said the problem of diabetes could be attributed to the rising weight challenge of
Filipinos.
Obesity is one of the risk factors for diabetes. In 2008, obesity has ballooned to 25% in 2008
33 | P a g e
from 1987 statistics of only 13.5%, he said.
Mr. Baldemor said the reason Filipinos are becoming heavier could be linked to changing dietary
habits as revealed in the 2008 Food Consumption Survey done by the Food & Nutrition Research
Institute.
The survey showed that 40% of Filipino households are taking their meals and snacks outside of
home, and approximately 30% of the caloric intake in a day was derived from animal sources in
2008 as compared to 20% in 1978.
Rice, sugar and cooking oil are the top three food items commonly consumed by Filipinos. And
there was a significant increase in the intake of rice, he said.
Recognizing the importance of nutrition in the total diabetes management, PADE conducted a
study among Filipinos with diabetes about their typical breakfast.
The study revealed that compared to the expert macronutrient guidelines of the American
Diabetes Association (ADA) and European Association for the Study of Diabetes (EASD), the
typical Filipino breakfast is 30% protein, more than the 20% limit in the ADA and EASD
guidelines.
Mr. Baldemor said the excess protein makes Filipinos more prone to diabetes. And for those who
already have diabetes, the excess protein may lead to complications like end-stage renal disease
and other kidney problems. He explained that kidney damage makes it more difficult for
individuals to process sugar, thus complicating the case of most diabetics.
NUTRITION FOR HEALTH
34 | P a g e
Mr. Baldemor said there is a need for complete diabetes management that integrates medication,
a healthy diet, physical activity and exercise, and medical nutrition therapy.
In the Philippines, diabetes experts composed of health care professionals from seven medical
societies and institutions developed the Philippine Diabetes Nutrition Algorithm (PhilDNA).
PhilDNA provides recommendations on diabetes-specific nutrition to support the goals of weight
loss, lowering blood sugar, blood pressure and cholesterol for prevention of complications and
longevity.
Included in the PhilDNA recommendation is the use of diabetes-specific formula like Glucerna
Triple Care, which is a specialized drink manufactured by global health care company Abbott.
Abbott Nutrition International (Philippines) medical director Jose Rodolfo V. Dimaano, Jr. said
Glucerna Triple Care has been clinically shown to help manage weight and reduce
cardiovascular risk factors in conjunction with an overall diabetes management plan, including
diet and exercise.
He said the product provides an advanced, slowly digested carbohydrate system to manage blood
sugar response. It also has a unique heart-friendly lipid blend rich in Omega-3 fatty acids to
support heart health, and a combination of key ingredients to help reduce weight and the
patients waistline.
He added that Glucerna Triple Care has 32 vitamins and minerals and is 225 calories per serving.
It is available in vanilla and chocolate flavors..
(source: Business World
) http://www.bworldonline.com/weekender/content.php?id=68524
35 | P a g e
Having the article written by Valisno (2013), the principles of food management for people with
diabetes can then, be summarized as follows:
- Eat regular meals with carbohydrate making up approximately 50% of meals
- Limit intake of foods high in fat, salt and sugar
- Try to increase fruit and vegetable intake
- Nothing is banned, but some foods may need to be eaten less regularly than others.
A dietitian can help to explain these principles to both ward staff and people with diabetes -
particularly those who are newly diagnosed during their hospital stay.
Summary:
Every nurse in every hospital department will have some contact with people with diabetes.
Illness and stress can interact with the condition and cause blood glucose control to deteriorate.
This in turn can delay recovery and may produce complications such as infection. Attention to
maintaining good diabetes control is thus essential. Nurses can play a significant role in
promoting this by providing up-to-date and evidence-based care and support.
S-ar putea să vă placă și
- Nutritional Counselling. How To Motivate People To Correct Their Eating HabitsDe la EverandNutritional Counselling. How To Motivate People To Correct Their Eating HabitsÎncă nu există evaluări
- Summary of Theoretical Foundations of NursingDocument6 paginiSummary of Theoretical Foundations of Nursinghans_manalo100% (5)
- An Evolutionary Approach to Understanding and Treating Anorexia Nervosa and Other Eating ProblemsDe la EverandAn Evolutionary Approach to Understanding and Treating Anorexia Nervosa and Other Eating ProblemsÎncă nu există evaluări
- Update Checked by Maam V Sep 10Document83 paginiUpdate Checked by Maam V Sep 10ashamy acolÎncă nu există evaluări
- NCM 107 1Document5 paginiNCM 107 1Clint Mikael EulatrizÎncă nu există evaluări
- Summary, Analysis & Review of Sylvia Tara’s The Secret Life of FatDe la EverandSummary, Analysis & Review of Sylvia Tara’s The Secret Life of FatÎncă nu există evaluări
- Nursing Conceptual ModelDocument16 paginiNursing Conceptual Modelmedallarodriguez241Încă nu există evaluări
- Food Counselling. How To Motivate People To Change Eating HabitsDe la EverandFood Counselling. How To Motivate People To Change Eating HabitsÎncă nu există evaluări
- In Partial Fulfillment of The Requirement in NCM 201 Health AssessmentDocument11 paginiIn Partial Fulfillment of The Requirement in NCM 201 Health AssessmentKathHinlogÎncă nu există evaluări
- Changing for Good: A Revolutionary Six-Stage Program for Overcoming Bad Habits and Moving Your Life Positively ForwardDe la EverandChanging for Good: A Revolutionary Six-Stage Program for Overcoming Bad Habits and Moving Your Life Positively ForwardEvaluare: 4 din 5 stele4/5 (29)
- Dorothea OremDocument9 paginiDorothea OremZialmare Romulo CruzÎncă nu există evaluări
- Assignment - Nursing Models RAMDocument14 paginiAssignment - Nursing Models RAMinoka sandamali AriyarathneÎncă nu există evaluări
- Breaking Free: Overcoming Anorexia and Body Image DistortionDe la EverandBreaking Free: Overcoming Anorexia and Body Image DistortionÎncă nu există evaluări
- Betty Neuman: Health Care System ModelDocument4 paginiBetty Neuman: Health Care System ModelMchll EspnzÎncă nu există evaluări
- Bioregulatory Medicine: An Innovative Holistic Approach to Self-HealingDe la EverandBioregulatory Medicine: An Innovative Holistic Approach to Self-HealingEvaluare: 5 din 5 stele5/5 (1)
- Orem's Self-Care Deficit PDFDocument28 paginiOrem's Self-Care Deficit PDFCarl Philip PerezÎncă nu există evaluări
- Dual Diagnosis Recovery Workbook: A Holistic Guide to Mental & Substance RecoveryDe la EverandDual Diagnosis Recovery Workbook: A Holistic Guide to Mental & Substance RecoveryÎncă nu există evaluări
- Autonomous Decision MakingDocument17 paginiAutonomous Decision MakingJoYCe100% (1)
- Multimodal Treatment of Acute Psychiatric Illness: A Guide for Hospital DiversionDe la EverandMultimodal Treatment of Acute Psychiatric Illness: A Guide for Hospital DiversionÎncă nu există evaluări
- Week 1 - Part A MID 100Document4 paginiWeek 1 - Part A MID 100Ram AugustÎncă nu există evaluări
- Summary of Max Lugavere with Paul Grewal's Genius FoodsDe la EverandSummary of Max Lugavere with Paul Grewal's Genius FoodsÎncă nu există evaluări
- NURSING CONCEPTS Exam GuideDocument24 paginiNURSING CONCEPTS Exam Guide2016114427Încă nu există evaluări
- PrintedFundamentals of NursingDocument23 paginiPrintedFundamentals of NursingAaron EspirituÎncă nu există evaluări
- Prelim NotesDocument13 paginiPrelim Notesjohncarlo ramosÎncă nu există evaluări
- SISTER CALLISTA ROY-Adaptation Theory-1Document17 paginiSISTER CALLISTA ROY-Adaptation Theory-1Louis Gabriel AdayaÎncă nu există evaluări
- CHRONICITYDocument5 paginiCHRONICITYvavafo7699Încă nu există evaluări
- Adaptation Model Theorist: Sister Callista Roy Name of Model: Adaptation ModelDocument6 paginiAdaptation Model Theorist: Sister Callista Roy Name of Model: Adaptation ModelErynhÎncă nu există evaluări
- Nursing Theory and TheoristsDocument12 paginiNursing Theory and TheoristsSundaraBharathiÎncă nu există evaluări
- Assingement of Psychology and SociologyDocument7 paginiAssingement of Psychology and SociologySurkhali BipanaÎncă nu există evaluări
- The Problem and Its SettingDocument20 paginiThe Problem and Its Settingimee15Încă nu există evaluări
- Community Health NursingDocument14 paginiCommunity Health NursingKira100% (13)
- Orem's TheoryDocument27 paginiOrem's TheoryREVATHI H K100% (3)
- Chapter 7Document6 paginiChapter 7ceciliaÎncă nu există evaluări
- Chapter 3Document4 paginiChapter 3Sera SazleenÎncă nu există evaluări
- Dorothea Orem-Self Care TheoryDocument10 paginiDorothea Orem-Self Care TheoryNikhil MohanÎncă nu există evaluări
- Nursing TheoryDocument12 paginiNursing TheoryMandy JameroÎncă nu există evaluări
- MS Review EdgeworthDocument89 paginiMS Review EdgeworthRichard Ines Valino100% (7)
- Nursing Theory Unit III - Inam 2024Document37 paginiNursing Theory Unit III - Inam 2024Safi UllahÎncă nu există evaluări
- CHN Mod 1Document5 paginiCHN Mod 1Monlexter MewagÎncă nu există evaluări
- LA1 Assignment ContentDocument4 paginiLA1 Assignment ContentbibsÎncă nu există evaluări
- AppendectomyDocument39 paginiAppendectomyBella IsananÎncă nu există evaluări
- Nursing TheoryDocument11 paginiNursing TheoryJenny SembranoÎncă nu există evaluări
- Thesis Statement Examples For Eating DisordersDocument6 paginiThesis Statement Examples For Eating Disordersjenniferontiveroskansascity100% (2)
- Lesson 1 The Stuart Stress Adaptation ModelDocument50 paginiLesson 1 The Stuart Stress Adaptation ModelMaria Victoria A. PraxidesÎncă nu există evaluări
- High Sweet Heart: NSTEMI Secondary To Hypertension, DMDocument46 paginiHigh Sweet Heart: NSTEMI Secondary To Hypertension, DMCharmmaine Yu-AcmanÎncă nu există evaluări
- Principles of GerontologyDocument7 paginiPrinciples of Gerontologyprokuno100% (12)
- Models of PreventionDocument80 paginiModels of Preventionsunielgowda88% (8)
- 500 Medical Surgical Sample QuestionDocument323 pagini500 Medical Surgical Sample QuestionElizabella Henrietta TanaquilÎncă nu există evaluări
- Health Promotion, Prevention ModelDocument20 paginiHealth Promotion, Prevention ModelRana Vandana67% (3)
- Nursing TheoristsDocument21 paginiNursing TheoristsMiss AÎncă nu există evaluări
- Knowledge Deficit Theory: Submitted By: Alex Kate Dela BSN 1 STEM A Submitted To: Ms. Rubilyn SumayloDocument4 paginiKnowledge Deficit Theory: Submitted By: Alex Kate Dela BSN 1 STEM A Submitted To: Ms. Rubilyn Sumaylokassy yeonÎncă nu există evaluări
- Community Health NursingDocument18 paginiCommunity Health NursingCharmagne Joci EpantoÎncă nu există evaluări
- Dorothea Orem's Self-Care Theory: Practice in 1971, Second in 1980, in 1995, and 2001Document9 paginiDorothea Orem's Self-Care Theory: Practice in 1971, Second in 1980, in 1995, and 2001Aulia Dwi RahmawatiÎncă nu există evaluări
- Republic of The Philippines Tamag, Vigan City 2700 Ilocos SurDocument16 paginiRepublic of The Philippines Tamag, Vigan City 2700 Ilocos SurJewel Ramos GalinatoÎncă nu există evaluări
- Group 2: Peptic Ulcer: Zoleta, Dayla Shaine May de Leon, Alexandra Caparros, Clea Balino, Iris JoyDocument120 paginiGroup 2: Peptic Ulcer: Zoleta, Dayla Shaine May de Leon, Alexandra Caparros, Clea Balino, Iris JoyDayan CabrigaÎncă nu există evaluări
- A Case Presentation of Diabetes Mellitus Type 2 Uncontrolled Non-Healing WoundDocument47 paginiA Case Presentation of Diabetes Mellitus Type 2 Uncontrolled Non-Healing Woundashamy acolÎncă nu există evaluări
- NCM114 - Learn Mat 1 2021Document32 paginiNCM114 - Learn Mat 1 2021jjÎncă nu există evaluări
- Lecture 2 Health Beliefs by WindaDocument20 paginiLecture 2 Health Beliefs by Windawinda lestariÎncă nu există evaluări
- SynopsisDocument11 paginiSynopsisnandhu0% (1)
- Transition Theory Applications - "Wishes": ArticleDocument6 paginiTransition Theory Applications - "Wishes": ArticleBo SanÎncă nu există evaluări
- Sports DrinksDocument2 paginiSports DrinksWeronika PÎncă nu există evaluări
- About Canada: Health and IllnessDocument14 paginiAbout Canada: Health and IllnessFernwood Publishing0% (1)
- Objectiv ES Rationa LE: Evaluatio NDocument3 paginiObjectiv ES Rationa LE: Evaluatio NAnonymous FgT04krgym100% (1)
- Physical Education and Health 12Document9 paginiPhysical Education and Health 12Rona Mae BetitaÎncă nu există evaluări
- CompilationDocument14 paginiCompilationSylph AngeliqueÎncă nu există evaluări
- The Healthy Lifestyle and Personal Control QuestionnaireDocument23 paginiThe Healthy Lifestyle and Personal Control QuestionnaireDon Chiaw ManongdoÎncă nu există evaluări
- Unfuck Your Program: 10 Weeks of Periodization, Intermediate Program Read The Instructions First!Document19 paginiUnfuck Your Program: 10 Weeks of Periodization, Intermediate Program Read The Instructions First!olafÎncă nu există evaluări
- Aerobic and Anaerobic Excercises SummaryDocument7 paginiAerobic and Anaerobic Excercises SummaryThermus AquaticusÎncă nu există evaluări
- Pe8 q1 Mod3 Planprepareactitout v2Document29 paginiPe8 q1 Mod3 Planprepareactitout v2Teacher 5Încă nu există evaluări
- Efficacy of Teaching Self-Management Strategies On Auditory Hallucinations Among Schizophrenic PatientsDocument11 paginiEfficacy of Teaching Self-Management Strategies On Auditory Hallucinations Among Schizophrenic PatientsFrandi CahyaÎncă nu există evaluări
- Dorothea Orems Theory of Self Care DeficitDocument35 paginiDorothea Orems Theory of Self Care DeficitDiah Permata SariÎncă nu există evaluări
- Employability Skills (Weightage 10) : Deep Narayan Singh PGT (Computer Science), KV CHHDocument20 paginiEmployability Skills (Weightage 10) : Deep Narayan Singh PGT (Computer Science), KV CHHNCDRC SSFÎncă nu există evaluări
- NP1 Family Nursing 3Document2 paginiNP1 Family Nursing 3Jonas Marvin AnaqueÎncă nu există evaluări
- Fitness Training Program: Program Start Date Client's Information Warm-UpDocument2 paginiFitness Training Program: Program Start Date Client's Information Warm-UpMohamed AtefÎncă nu există evaluări
- 2019 Planning OverviewDocument7 pagini2019 Planning Overviewapi-323922022Încă nu există evaluări
- The Russian Approach To Planning A Weightlifting ProgramDocument7 paginiThe Russian Approach To Planning A Weightlifting ProgramStefan Hedengren100% (3)
- Proofed - Final - Clinical Evaluation 4020-21-22 - 1Document11 paginiProofed - Final - Clinical Evaluation 4020-21-22 - 1api-313199824Încă nu există evaluări
- M&F Training GuideDocument19 paginiM&F Training Guidecnico403Încă nu există evaluări
- Face SerumDocument10 paginiFace SerumLiliana CojocaruÎncă nu există evaluări
- Week 1Document11 paginiWeek 1Hanna Clarisse BangayanÎncă nu există evaluări
- By Sayyed Nadar ShahDocument9 paginiBy Sayyed Nadar ShahShayan ShayanÎncă nu există evaluări
- Resistance TrainingDocument4 paginiResistance TrainingRuchelle Denice Demaisip IIÎncă nu există evaluări
- Introduction To Food Additives: A. Larry Branen and R. J. HaggertyDocument9 paginiIntroduction To Food Additives: A. Larry Branen and R. J. HaggertytintfenÎncă nu există evaluări
- Healthy Lifestyle DramaDocument2 paginiHealthy Lifestyle DramaJoseph Hayes100% (1)
- Marathon Half: 12-Week Training PlanDocument10 paginiMarathon Half: 12-Week Training PlanJames RetkuÎncă nu există evaluări
- Delta Training Plan OverviewDocument3 paginiDelta Training Plan Overviewhierophant241160% (5)
- DNHS SHS Exam in PE and Health 11 (Midterm Exam SY 2017-2018) Answer SheetDocument2 paginiDNHS SHS Exam in PE and Health 11 (Midterm Exam SY 2017-2018) Answer SheetArangote Glenn92% (91)
- Williams Essentials of Nutrition and Diet Therapy 10th Edition Roth Test BankDocument11 paginiWilliams Essentials of Nutrition and Diet Therapy 10th Edition Roth Test BankSamanthaRamospfozx100% (18)
- Love Yourself, Heal Your Life Workbook (Insight Guide)De la EverandLove Yourself, Heal Your Life Workbook (Insight Guide)Evaluare: 5 din 5 stele5/5 (40)
- Summary of Mary Claire Haver's The Galveston DietDe la EverandSummary of Mary Claire Haver's The Galveston DietEvaluare: 5 din 5 stele5/5 (1)
- Gut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)De la EverandGut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Evaluare: 4 din 5 stele4/5 (378)
- The Obesity Code: Unlocking the Secrets of Weight LossDe la EverandThe Obesity Code: Unlocking the Secrets of Weight LossEvaluare: 4 din 5 stele4/5 (5)
- Forever Strong: A New, Science-Based Strategy for Aging WellDe la EverandForever Strong: A New, Science-Based Strategy for Aging WellÎncă nu există evaluări
- Instant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookDe la EverandInstant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookEvaluare: 3.5 din 5 stele3.5/5 (2)
- How Not to Die by Michael Greger MD, Gene Stone - Book Summary: Discover the Foods Scientifically Proven to Prevent and Reverse DiseaseDe la EverandHow Not to Die by Michael Greger MD, Gene Stone - Book Summary: Discover the Foods Scientifically Proven to Prevent and Reverse DiseaseEvaluare: 4.5 din 5 stele4.5/5 (83)
- Metabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeDe la EverandMetabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeÎncă nu există evaluări
- Summary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisDe la EverandSummary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisEvaluare: 3 din 5 stele3/5 (2)
- Sugar Crush: How to Reduce Inflammation, Reverse Nerve Damage, and Reclaim Good HealthDe la EverandSugar Crush: How to Reduce Inflammation, Reverse Nerve Damage, and Reclaim Good HealthEvaluare: 4 din 5 stele4/5 (6)
- Eat & Run: My Unlikely Journey to Ultramarathon GreatnessDe la EverandEat & Run: My Unlikely Journey to Ultramarathon GreatnessÎncă nu există evaluări
- The Body Book: The Law of Hunger, the Science of Strength, and Other Ways to Love Your Amazing BodyDe la EverandThe Body Book: The Law of Hunger, the Science of Strength, and Other Ways to Love Your Amazing BodyÎncă nu există evaluări
- The Food Lover's Cleanse: 140 Delicious, Nourishing Recipes That Will Tempt You Back into Healthful EatingDe la EverandThe Food Lover's Cleanse: 140 Delicious, Nourishing Recipes That Will Tempt You Back into Healthful EatingEvaluare: 4 din 5 stele4/5 (3)
- The Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonDe la EverandThe Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonEvaluare: 3.5 din 5 stele3.5/5 (33)
- Eat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouDe la EverandEat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouÎncă nu există evaluări
- The Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyDe la EverandThe Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyEvaluare: 4.5 din 5 stele4.5/5 (2)
- Eat Complete: The 21 Nutrients That Fuel Brainpower, Boost Weight Loss, and Transform Your HealthDe la EverandEat Complete: The 21 Nutrients That Fuel Brainpower, Boost Weight Loss, and Transform Your HealthEvaluare: 2 din 5 stele2/5 (1)
- The Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsDe la EverandThe Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsEvaluare: 4 din 5 stele4/5 (49)
- The Stark Naked 21-Day Metabolic Reset: Effortless Weight Loss, Rejuvenating Sleep, Limitless Energy, More MojoDe la EverandThe Stark Naked 21-Day Metabolic Reset: Effortless Weight Loss, Rejuvenating Sleep, Limitless Energy, More MojoÎncă nu există evaluări
- Secrets From the Eating Lab: The Science of Weight Loss, the Myth of Willpower, and Why You Should Never Diet AgainDe la EverandSecrets From the Eating Lab: The Science of Weight Loss, the Myth of Willpower, and Why You Should Never Diet AgainEvaluare: 3.5 din 5 stele3.5/5 (38)
- Keto Friendly Recipes: Easy Keto For Busy PeopleDe la EverandKeto Friendly Recipes: Easy Keto For Busy PeopleEvaluare: 3.5 din 5 stele3.5/5 (2)
- Body Love Every Day: Choose Your Life-Changing 21-Day Path to Food FreedomDe la EverandBody Love Every Day: Choose Your Life-Changing 21-Day Path to Food FreedomEvaluare: 4 din 5 stele4/5 (1)
- The Diet Trap Solution: Train Your Brain to Lose Weight and Keep It Off for GoodDe la EverandThe Diet Trap Solution: Train Your Brain to Lose Weight and Keep It Off for GoodÎncă nu există evaluări
- Find Your Path: Honor Your Body, Fuel Your Soul, and Get Strong with the Fit52 LifeDe la EverandFind Your Path: Honor Your Body, Fuel Your Soul, and Get Strong with the Fit52 LifeEvaluare: 4 din 5 stele4/5 (3)
- The Complete Guide to Fasting: Heal Your Body Through Intermittent, Alternate-Day, and Extended FastingDe la EverandThe Complete Guide to Fasting: Heal Your Body Through Intermittent, Alternate-Day, and Extended FastingÎncă nu există evaluări
- The Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthDe la EverandThe Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthÎncă nu există evaluări
- How to Be Well: The 6 Keys to a Happy and Healthy LifeDe la EverandHow to Be Well: The 6 Keys to a Happy and Healthy LifeEvaluare: 5 din 5 stele5/5 (1)
- The Volumetrics Eating Plan: Techniques and Recipes for Feeling Full on Fewer CaloriesDe la EverandThe Volumetrics Eating Plan: Techniques and Recipes for Feeling Full on Fewer CaloriesÎncă nu există evaluări