Documente Academic
Documente Profesional
Documente Cultură
Jugular Foramen
Încărcat de
Indra HadianditeDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Jugular Foramen
Încărcat de
Indra HadianditeDrepturi de autor:
Formate disponibile
CHAPTER 9
Jugular Foramen
Albert L. Rhoton, Jr., M.D.
Department of Neurological Surgery, University of Florida, Gainesville, Florida
Key words: Cranial base, Cranial nerves, Jugular foramen, Microsurgical anatomy, Occipital bone, Skull base, Temporal bone, Venous sinuses
T
he jugular foramen is difficult to understand and to
access surgically (3, 11, 15, 19, 24, 28). It is difficult to
conceptualize because it varies in size and shape in
different crania, from side to side in the same cranium, and
from its intracranial to extracranial end in the same foramen,
and because of its complex irregular shape, its curved course,
its formation by two bones, and the numerous nerves and
venous channels that pass through it (Fig. 9.1). The difficulties
in exposing this foramen are created by its deep location and
the surrounding structures, such as the carotid artery anteri-
orly, the facial nerve laterally, the hypoglossal nerve medially,
and the vertebral artery inferiorly, all of which block access to
the foramen and require careful management.
The jugular foramen is divided into three compartments:
two venous and a neural or intrajugular compartment. The
venous compartments consist of a larger posterolateral ve-
nous channel, the sigmoid part, which receives the flow of the
sigmoid sinus, and a smaller anteromedial venous channel,
the petrosal part, which receives the drainage of the inferior
petrosal sinus. The petrosal part forms a characteristic venous
confluens by also receiving tributaries from the hypoglossal
canal, petroclival fissure, and vertebral venous plexus. The
petrosal part empties into the sigmoid part through an open-
ing in the medial wall of the jugular bulb between the glos-
sopharyngeal nerve anteriorly and the vagus and accessory
nerves posteriorly. The intrajugular or neural part, through
which the glossopharyngeal, vagus, and accessory nerves
course, is located between the sigmoid and petrosal parts at
the site of the intrajugular processes of the temporal and
occipital bones, which are joined by a fibrous or osseous
bridge. The glossopharyngeal, vagus, and accessory nerves
penetrate the dura on the medial margin of the intrajugular
process of the temporal bone to reach the medial wall of the
internal jugular vein. The operative approaches that access
various aspects of the foramen and adjacent areas are the
postauricular transtemporal, retrosigmoid, extreme lateral
transcondylar, and preauricular subtemporal-infratemporal
approaches.
OSSEOUS RELATIONSHIPS
The jugular foramen is located between the temporal bone
and the occipital bone (Figs. 9.1 and 9.2). The right foramen is
usually larger than the left. In a previous study, we observed
that the right foramen was larger than the left in 68% of the
cases, equal to the left in 12%, and smaller than the left in 20%
(24). The foramen is configured around the sigmoid and in-
ferior petrosal sinuses. It can be regarded as a hiatus between
the temporal and the occipital bones. The structures that
traverse the jugular foramen are the sigmoid sinus and jugu-
lar bulb, the inferior petrosal sinus, meningeal branches of the
ascending pharyngeal and occipital arteries, the glossopharyn-
geal, vagus, and accessory nerves with their ganglia, the tym-
panic branch of the glossopharyngeal nerve (Jacobsons nerve),
the auricular branch of the vagus nerve (Arnolds nerve), and the
cochlear aqueduct.
The foramen is situated so that its long axis is directed from
posterolateral to anteromedial, giving it an anterolateral mar-
gin formed by the temporal bone and a posteromedial margin
formed by the occipital bone. From the intracranial end, it is
directed forward, medially, and downward. One cannot see
through the foramen when viewing the skull from directly
above or below because of its roof, formed by the lower
surface of the petrous part of the temporal bone. The foramen,
when viewed from the intracranial side in a posterior to
anterior direction, has a large oval lateral component, referred
to as the sigmoid part, because it receives the drainage of the
sigmoid sinus, and a small medial part, called the petrosal
part, because it receives the drainage of the inferior petro-
sal sinus. The view through the foramen from directly below
reveals the part of the temporal bone forming the dome of the
jugular bulb, rather than a clear opening.
The junction of the sigmoid and petrosal parts is the site of
bony prominences on the opposing surfaces of the temporal
and occipital bones, called the intrajugular processes, which
are joined by a fibrous, or less commonly, and osseous bridge,
the intrajugular septum, separating the sigmoid and petrosal
part of the foramen.
Although the margins of the jugular foramen are formed by
the petrosal part of the temporal bone and the condylar part
of the occipital bone, the other parts of these bones also have
important relationships to the jugular foramen. The petro-
clival fissure, the fissure between the lateral edge of the clival
part of the occipital bone and the petrous part of the temporal
bone, intersects the anteromedial edge of the foramen, and the
occipitomastoid suture, the suture between the mastoid por-
S267 Neurosurgery, Vol. 47, No. 3, September 2000 Supplement
tion of the temporal bone and the condylar part of the occip-
ital bone, intersects its posterolateral edge.
The intrajugular processes of the temporal and occipital
bones divide the anterior and posterior edges of the foramen
between the sigmoid and petrosal parts. The intrajugular
process of the temporal bone protrudes farther into the jugu-
lar foramen than the opposite process from the occipital bone,
and may infrequently reach the smaller intrajugular process
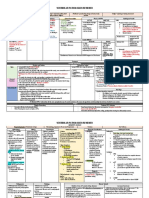
FIGURE 9.1. AD. Osseous relationships. A, the jugular foramen is located between the temporal and occipital bones. One can-
not see directly through the foramen from above, as shown, because it is directed forward under the temporal bone. The sigmoid
groove descends along the mastoid and crosses the occipitomastoid suture where it turns forward on the upper surface of the jugu-
lar process of the occipital bone and enters the foramen by passing under the posterior part of the petrous temporal bone. B, the
view directed from posterior and superior shows the shape of the foramen, which is not seen on the direct superior view. The fora-
men has a larger lateral sigmoid part through which the sigmoid sinus empties and a smaller anteromedial petrosal part through
which the inferior petrosal sinus empties. The two parts are separated by the intrajugular processes of the occipital and temporal
bones. The glossopharyngeal, vagus, and accessory nerves pass through the intrajugular portion of the foramen located between
the sigmoid and petrosal parts. The foramen is asymmetric from side to side with the right side often being larger as shown. The
cochlear aqueduct opens just above the anterior edge of the petrosal part. The vestibular aqueduct opens into the endolymphatic
sac, which sits on the back of the temporal bone superolateral to the sigmoid part of the jugular foramen. C, jugular foramen
viewed from directly below. One cannot see directly through the foramen from below because the foramen is covered above by
the part of the petrous temporal bone forming the jugular fossa, which houses the jugular bulb. The entrance into the carotid canal
is located directly in front of the medial half of the jugular foramen. The stylomastoid foramen is located lateral and the anterior
half of the occipital condyle medial to the jugular foramen. The posterior condylar foramen is transversed by an emissary vein,
which joins the sigmoid sinus. The hypoglossal canal passes above the middle third of the occipital condyle and opens laterally into
the interval between the jugular foramen and carotid canal. D, the view directed from anterior and backward reveals the shape of
the jugular foramen. The roof over the foramen formed by the jugular fossa of the temporal bone is shaped to accommodate the
jugular bulb. The posterior margin of the foramen is formed by the jugular process of the occipital bone, which connects the basal
(clival) part of the occipital bone to the squamosal part. The petroclival fissure intersects the anteromedial margin of the petrosal
part of the foramen. Ac., acoustic; Car., carotid; Coch., cochlear; Cond., condyle; Fiss., fissure; For., foramen; Hypogl., hypoglossal;
Int., internal; Intrajug., intrajugular; Jug., jugular; Mast., mastoid; Occip., occipital; Pet., petrous; Petrocliv., petroclival; Post., poste-
rior; Proc., process; Sig., sigmoid; Squam., squamosal; Stylomast., stylomastoid; Temp., temporal; Vest., vestibular.
S268 Rhoton
Neurosurgery, Vol. 47, No. 3, September 2000 Supplement
of the occipital bone, dividing the jugular foramen into two
bony foramina. A ridge, the intrajugular ridge, extends for-
ward from the intrajugular process of the temporal bone
along the medial edge of the jugular bulb (Fig. 9.1). The
glossopharyngeal nerve courses along its medial edge. Occa-
sionally, the edge of this ridge extends medially toward the
adjacent part of the temporal bone to create a deep groove in
which the nerve courses or it may reach the temporal bone to
form a canal, which surrounds the glossopharyngeal nerve as
it passes through the jugular foramen.
The drainage of the sigmoid sinus is directed forward into the
sigmoid portion of the foramen, where a high domed recess,
the jugular fossa, forms a roof over the top of the jugular bulb
(Figs. 9.1 and 9.3). This recess, which has its summit slightly
lateral to the entrance of the sigmoid sinus, is usually larger on
the right side of the skull, reflecting the larger sigmoid sinus on
FIGURE 9.1. EH. E and F, another jugular foramen. Left side: E, the sutures have been forced open to show the relationship
of the foramen to the petroclival and occipitomastoid sutures. The jugular foramen has a larger lateral part, the sigmoid part,
which receives the drainage of the sigmoid sinus, and a smaller medial part, the petrosal part, which receives the drainage of
the inferior petrosal sinus. The intrajugular process of the occipital bone is somewhat more prominent than shown in C and
projects forward toward the intrajugular process of the temporal bone. The hamate process normally extends along the
medial edge of the petrosal part of the foramen to the adjacent part of the temporal bone, but in this case the sutures were
forced open, leaving an interval between the hamate process and the temporal bone. F, enlarged view. G and H, another jug-
ular foramen. G, the intrajugular process of the temporal bone projects into the interval between the sigmoid and petrosal
parts of the foramen. A ridge, the intrajugular ridge, extends forward from the intrajugular process along the medial side of
the jugular bulb. The glossopharyngeal nerve passes forward along the medial side of the intrajugular process and ridge. The
vagus and accessory nerves enter the dura on the medial side of the process, but quickly descend and do not pass forward
along the medial edge of the ridge as does the glossopharyngeal nerve. The jugular process of the occipital bone often has a
small prominence on its surface that projects toward the intrajugular process of the temporal bone, and in some foramina,
the intrajugular processes of the two bones are joined by an osseous bridge that converts the foramen into two osseous
foramina. In this case, the intrajugular process of the occipital bone is absent. H, enlarged view. The cochlear aqueduct
opens above the petrosal part of the foramen and the site where the glossopharyngeal nerve enters the intrajugular part of
the foramen on the medial side of the intrajugular process. The vestibular aqueduct opens onto the posterior surface of the
temporal bone superolateral to the jugular foramen.
Jugular Foramen S269
Neurosurgery, Vol. 47, No. 3, September 2000 Supplement
that side. The dome of the recess is usually smooth as it conforms
to the jugular bulb, but the summit may also be ridged and
irregular. A small triangular recess, the pyramidal fossa, extends
forward on the medial side of the intrajugular process of the
temporal bone along the anterior wall of the petrosal part of the
foramen. The external aperture of the cochlear canaliculus,
which houses the perilymphatic duct and a tubular prolongation
of the dura mater, opens into the anterior apex of the pyramidal
fossa. The glossopharyngeal nerve enters this fossa below the
point at which the cochlear aqueduct joins its apex.
FIGURE 9.2. Osseous relationships. A, lateral view.
The styloid process projects downward and the facial
nerve exits the stylomastoid foramen on the lateral
side, and both block lateral access to the jugular
foramen. The mandibular condyle blocks access to
the foramen from anteriorly and the vertebral artery
ascending through the C1 transverse process limits
access from behind. The transverse process of C1 sits
behind and often indents the posterior wall of the
internal jugular vein. B, inferior view of the jugular
foramen. The jugular foramen is located lateral to the
anterior half of the occipital condyle. The temporal
bone forms the dome over the jugular bulb. The
jugular process of the occipital bone forms the
posterior margin of the jugular foramen. The jugular
foramen and carotid canal are separated by a narrow bony ridge, which is penetrated medially by the tympanic
canaliculus through which passes the tympanic branch of the glossopharyngeal nerve (Jacobsons nerve). This branch
of the nerve passes forward across the promontory in the medial part of the tympanic cavity, then crosses the floor of
the middle fossa as the lesser petrosal nerve, and eventually reaches the otic ganglion, providing parasympathetic
innervation to the parotid gland. The anterior wall of the sigmoid part of the foramen is the site of a shallow groove across
which the auricular branch of the vagus nerve (Arnolds nerve) passes to enter the mastoid canaliculus. It exits the mastoid
through the tympanomastoid suture. C, lateral view of the left temporal bone. A small fiber (arrow) placed in the tympanic
canaliculus, shown in B, exits the canaliculus in the middle ear where the fibers of the tympanic branch of the glossopharyngeal
nerve cross the promontory, and then regroup to cross the floor of the middle fossa as the lesser petrosal nerve. The styloid
process projects downward lateral to the jugular foramen. Aur., auricular; Br., branch; Canalic., canaliculus; Car., carotid; CN,
cranial nerve; Cond., condyle; Ext., external; Fiss., fissure; For., foramen; Jug., jugular; Mandib., mandibular; Occip., occipital;
Petrotymp., petrotympanic; Proc., process; Trans., transverse; Tymp., tympanic.
S270 Rhoton
Neurosurgery, Vol. 47, No. 3, September 2000 Supplement
The jugular process of the condylar portion of the occipital
bone, which extends behind the jugular foramen and connects
the clival and squamosal parts of the occipital bone, forms the
posteromedial wall of the foramen. This process extends lat-
erally from the area above the posterior half of the occipital
condyle and is penetrated by the hypoglossal canal. The upper
surface of the jugular process of the occipital bone in the area
superomedial to the foramen presents an oval prominence, the
jugular tubercle, which is located above the hypoglossal canal.
The jugular tubercle often has a shallow furrow marking the site
of passage of the glossopharyngeal, vagus, and accessory nerves
across its surface. The terminal end of the sigmoid sinus courses
forward on the superior surface of the jugular process in a deep
hook-like groove, the sigmoid sulcus, which is directed medially
into the sigmoid portion of the jugular foramen.
On the lateral wall of the jugular foramen, a few millimeters
inside the external edge, just behind the point at which the
occipitomastoid suture crosses the lateral edge of the foramen,
is a small foramen, the mastoid canaliculus, and a shallow
groove leading from medial to lateral across the anterior wall of
the sigmoid part to the mastoid canaliculus (Figs. 9.2 and 9.3).
The auricular branch of the vagus nerve (Arnolds nerve)
courses along the groove and enters the canaliculus. The nerve
passes through the mastoid and exits the bone in the inferolateral
part of the tympanomastoid suture. At the site where the intra-
jugular ridge of the temporal bone meets the carotid ridge, a
small canal, the tympanic canaliculus, is directed upward, lead-
ing the tympanic branch arising from the inferior glossopharyn-
geal ganglion (Jacobsons nerve) to the tympanic cavity (Figs.
9.2). Looking from below at the extracranial orifice of the jugular
foramen, it can be recognized that the glossopharyngeal nerve
courses along the medial side of the intrajugular process and
ridge to reach the area below the tympanic canaliculus.
ADJACENT BONY STRUCTURES
On the intracranial side, the petrosal part of the foramen is
located approximately 5 mm below the porus of the internal
canal and 5 mm above the intracranial orifice of the hypoglos-
sal canal (Figs. 9.2 and 9.4). The lateral edge of the foramen is
located below and in approximately the sagittal plane
through the lateral end of the internal acoustic meatus. The
jugular tubercle, a rounded prominence located at the junction
of the basal and condylar parts of the occipital bone, is situated
approximately 8 mm medial to the medial edge of the jugular
foramen. The otic capsule, which is situated in the petrous part
of the temporal bone and which contains the semicircular canals
and cochlea, is located superior to the dome of the jugular bulb.
The occipital condyle is located along the lateral margin of
the anterior half of the foramen magnum in the area below
and medial to the jugular foramen.
The hypoglossal canals, which pass through the condylar
part of the occipital bone in the area above the occipital
condyles, are located medial to the jugular foramina (Figs. 9.1
and 9.3). The intracranial end of the hypoglossal canal is
situated below the jugular tubercle approximately 5 mm in-
feromedial to the petrosal part of the jugular foramen and
several millimeters below the lower part of the petroclival
fissure. A more detailed review is included in the chapter on
the far-lateral approach.
The anterior margin of the jugular foramen, when viewed
extracranially, is formed by the narrow ridge of temporal
bone, the carotid ridge, which separates the foramen and the
carotid canal (Figs. 9.1 and 9.2). The tympanic canaliculus opens
on or near the medial part of the carotid ridge. The styloid
process and the stylomastoid foramen are located lateral to the
outer orifice of the jugular foramen, with the styloid process
being located slightly anteromedial to the stylomastoid foramen.
The facial nerve exits the stylomastoid foramen approximately 5
mm lateral to the lateral edge of the jugular foramen. The ante-
rior margin of the jugular foramen is located just behind the part
of the tympanic bone that forms the posterior wall of the tem-
poromandibular joint and the anterior and inferior wall of the
external auditory canal. The vaginal process of the tympanic
bone, which separates both the carotid canal and sigmoid part of
the foramen from the glenoid fossa, is the site of attachment
of the styloid process to the skull base. The styloid process
projects downward from the vaginal process of the tympanic
bone, lateral to the foramen. The digastric groove is directed
posteriorly from the styloid process along the medial margin of
the mastoid process. Access to the jugular foramen is blocked
laterally by mastoid and styloid processes, the transverse process
of the atlas, and the mandibular ramus (Figs. 9.3 and 9.4).
The tympanic cavity, which is located medial to the tym-
panic membrane, is situated above and lateral to the jugular
bulb and the sharp right-angled curve, called the lateral bend, at
the junction of the vertical and horizontal segments of the pe-
trous carotid artery (Fig. 9.4). Several structures that may be
exposed during surgery for lesions in the jugular foramen are
the vertical and horizontal segments of the petrous portion of the
internal carotid artery, the eustachian tube, and the tensor tym-
pani muscle. Both the cochlea and semicircular canals are located
in the petrous part of the temporal bone above the dome of the
jugular bulb (Fig. 9.4). The facial nerve in the temporal bone,
which often blocks access to lesions in the jugular foramen,
descends through the mastoid lateral to the jugular bulb. The
endolymphatic sac is situated on the posterior surface of the pe-
trous bone between the two layers of the dura in the corner at
which the sigmoid sinus changes its course from a vertical
direction to a horizontal one (Figs. 9.3 and 9.5).
Dural architecture
At the intracranial orifice, the jugular foramen is divided
into three compartments by the dura mater: the petrosal com-
partment situated anteromedially, the sigmoid compartment
situated posterolaterally, and the intrajugular or neural com-
partment situated between the petrosal and sigmoid parts at
the site of the intrajugular processes of the temporal and
occipital bones, the intrajugular septum, and the glossopha-
ryngeal, vagus, and accessory nerves (Figs. 9.3 and 9.5). The
dura over the intrajugular part of the foramen, which is
located anteromedial to the sigmoid part, has two character-
istic perforations, a glossopharyngeal meatus, through which
the glossopharyngeal nerve passes, and a vagal meatus,
through which the vagus and accessory nerves pass (Figs. 9.5
Jugular Foramen S271
Neurosurgery, Vol. 47, No. 3, September 2000 Supplement
FIGURE 9.3. A, posterior superior view of the jugular foramen. The sigmoid sulcus makes a sharp turn just before emptying
into the sigmoid portion of the jugular foramen. The inferior petrosal sinus extends along the petroclival fissure and enters
the petrosal part of the foramen. The nerves enter the intrajugular part of the foramen located between the sigmoid and
petrosal parts. The outlined area shows the approximate site from which B to F were taken. B, the sigmoid sinus descends in
the sigmoid sulcus and makes a sharp anterior turn to enter the jugular foramen. The jugular bulb extends upward under the
petrous temporal bone toward the internal acoustic meatus. The endolymphatic sac is located above the lower portion of the
sigmoid sinus on the back of the temporal bone and opens above through the vestibular aqueduct into the vestibule. The
glossopharyngeal, vagus and accessory nerves penetrate the dura on the medial side of the intrajugular process. C, the dura
covering the jugular foramen and the jugular bulb have been removed. The nerves penetrate the dura on the medial side of
the intrajugular process of the temporal bone. The intrajugular ridge extends forward along the medial side of the jugular
bulb. D, enlarged view. The glossopharyngeal nerve passes forward along the medial side of the intrajugular ridge, but the
vagus and accessory nerves, although entering the dura on the medial side of the intrajugular process, almost immediately
turn downward and do not course along the medial edge of the intrajugular ridge in the medial wall of the jugular bulb, as
S272 Rhoton
Neurosurgery, Vol. 47, No. 3, September 2000 Supplement
and 9.6) (24). Both meatus are located on the medial side of the
intrajugular processes and septum. The glossopharyngeal and
vagal meatus are consistently separated by a dural septum
ranging in width from 0.5 to 4.9 mm (13). The only intradural
site at which the glossopharyngeal nerve is consistently dis-
tinguishable from the vagus nerve is just proximal to this
dural septum. The close origins of the glossopharyngeal and
vagus nerves at the brainstem, and the arachnoidal adhesions
between the two in their course through the subarachnoid
space may make separation difficult except in the area just
proximal to the dural septum. The superior glossopharyngeal
ganglion is easily visible intracranially in about one-third of
nerves. The superior ganglion of the vagus can be seen in-
tracranially in only one-sixth of nerves. Although the cranial
and spinal portions of the accessory nerve most frequently
enter the vagal meatus together, a dural septum may separate
them.
The upper and lateral margins of the intrajugular part of the
foramen are the site of a characteristic thick dural fold that
forms a roof or lip that projects inferiorly and medially to
partially cover the glossopharyngeal and vagal meatus (Figs.
9.5 and 9.6). This structure, called the jugular dural fold, was
ossified on both sides in one specimen (13, 16, 17, 24, 31). The
lip projects most prominently over the glossopharyngeal me-
atus and is comparable to, but smaller than, the posterior lip
of the internal acoustic meatus. It is either predominantly
bony or fibrous and may project a maximum of 2.5 mm over
the margin of the glossopharyngeal meatus. The vagal lip is
less prominent, projecting a maximum of 1 mm over the
lateral margin of the vagal meatus.
Neural relationships
The glossopharyngeal, vagus, and accessory nerves arise
from the medulla as a line of rootlets situated along the
posterior edge of the inferior olive in the postolivary sulcus
(Figs. 9.3 and 9.5). The hypoglossal nerve arises as a line of
rootlets that exit the brainstem along the anterior margin of
the lower two-thirds of the olive in the preolivary sulcus, a
groove between the olive and medullary pyramid.
The glossopharyngeal nerve, at the point at which it pene-
trates the dural glossopharyngeal meatus, turns abruptly for-
ward and then downward and courses through the jugular
foramen in the groove leading from the pyramidal fossa be-
low the opening of the cochlear aqueduct and along the
medial side of the intrajugular ridge. After the nerve exits the
jugular foramen, it turns forward, crossing the lateral surface
of the internal carotid artery deep to the styloid process. As the
nerve transverses the jugular foramen, it expands at the site of its
superior and inferior ganglia (Fig. 9.5). At the external orifice
of the jugular foramen, it gives rise to the tympanic branch
(Jacobsons nerve), which traverses the tympanic canaliculus to
enter the tympanic cavity where it gives rise to the tympanic
plexus, the fibers of which course in shallow grooves on the
promontory and regroup to form the lesser petrosal nerve, pro-
viding parasympathetic innervation by way of the otic ganglion
to the parotid gland.
The vagal rootlets enter the dural subcompartment, called
the vagal meatus, inferior to the glossopharyngeal meatus
from which it is separated by a dural septum (Figs. 9.5 and
9.6). It is joined by the accessory nerve as it enters the dura.
After its rootlets gather in the intracranial orifice of the fora-
men, the vagus nerve expands at the superior ganglion, which
is about 2.5 mm in length, and ends below the extracranial
orifice of the foramen. It sits on the dura, covering the jugular
foramen, and there, along the medial side of the intrajugu-
lar process of the temporal bone, it turns downward. At the
superior ganglion, the vagus nerve communicates with the ac-
cessory nerve, a portion of which blends into the ganglion.
The auricular branch (Arnolds nerve) arises at the level of the
superior vagal ganglion and is joined by a branch from the in-
ferior glossopharyngeal ganglion (Fig. 9.3). The auricular
branch passes laterally in a shallow groove on the anterior
wall of the jugular bulb to reach the lateral wall of the jugular
fossa, where it enters the mastoid canaliculus and ascends
toward the vertical (mastoid) segment of the facial canal,
giving off an ascending branch to the facial nerve as it crosses
lateral to it before turning downward to exit the temporal
bone through the tympanomastoid fissure.
The main trunk of the vagus nerve (or, more accurately, the
superior ganglion) courses anterior and inferior as it crosses
below the midportion of the intrajugular process of the tem-
poral bone (Figs. 9.3 and 9.5). At the intracranial orifice of the
foramen, the intrajugular process of the temporal bone sepa-
rates the ganglion from the sigmoid sinus. In most cases, in
the area immediately below the dura at the level of the intra-
jugular processes, there are no fibrous bands between the
glossopharyngeal nerve and the vagal ganglion.
does the glossopharyngeal nerve. The auricular branch of the vagus nerve (Arnolds Nerve) arises from the vagus nerve,
passes along the groove in the anterior wall of the jugular fossa, and penetrates the mastoid canaliculus in the lateral wall of
the fossa. E, the nerves entering the jugular foramen have been displaced downward. The intrajugular process of the temporal
bone projects backward to join the intrajugular process of the occipital bone, thus forming an osseous bridge that divides the
foramen into two parts. The vagus and accessory nerves pass lateral to the osseous bridge and the inferior petrosal sinus
descends below the bridge to open into the internal jugular vein. F, the hypoglossal nerve has been exposed on the lateral
side of the occipital condyle. It exits the hypoglossal canal and joins the glossopharyngeal, vagus, and accessory nerves below
the jugular foramen in the interval between the internal carotid artery and internal jugular vein. A., artery; Ac., acoustic;
Aur., auricular; Br., branch; Car., carotid; CN, cranial nerve; Cond., condyle; Endolymph., endolymphatic; Gang., ganglion;
Inf., inferior; Intrajug., intrajugular; Jug., jugular; Occip., occipital; Pet., petrosal, petrous; Petrocliv., petroclival; Proc., pro-
cess; Sig., sigmoid; Sup., superior; Temp., temporal; Vert., vertebral; Vestib., vestibular.
Jugular Foramen S273
Neurosurgery, Vol. 47, No. 3, September 2000 Supplement
FIGURE 9.4. AD. Stepwise dissection
of the structures superficial to and
surrounding the jugular foramen. A,
the skin and scalp around the ear have
been reflected to expose the area
lateral to the jugular foramen. The
sternocleidomastoid is exposed behind
and the parotid gland in front of the
ear. The greater occipital nerve and
occipital artery reach the subcutaneous
tissues by passing between the
attachment of the trapezius and
sternocleidomastoid muscles to the
superior nuchal line. The external
acoustic meatus is located a little
forward of the deep site of the jugular
bulb. B, removal of the superficial
muscles and parotid gland exposes the
facial nerve, temporalis and masseter
muscles, posterior belly of the
digastric, and the internal jugular vein.
The sternocleidomastoid muscle has
been reflected backward to expose the
accessory nerve entering its deep
surface. C, the mandibular ramus and
condyle, medial and lateral pterygoid
muscles, and posterior belly of the
digastric have been removed to expose
the styloid process, which is located
lateral to the jugular foramen. The
internal carotid artery ascends to enter
the carotid canal in front of the jugular
foramen. Both the jugular foramen and
carotid canal are situated behind the
tympanic part of the temporal bone,
which forms the posterior wall of the
condylar fossa. The tensor and levator
vela palatini muscles are attached to
the eustachian tube in the area below
the horizontal segment of the petrous
carotid. The infratemporal fossa is
located below the greater wing of the
sphenoid. The mandibular nerve passes through the foramen ovale to enter the upper part of the infratemporal fossa. Branches of the
ascending pharyngeal artery pass through the jugular foramen to supply the surrounding dura. The hypoglossal nerve passes forward
across the external and internal carotid artery. D, the styloid process has been removed to expose the glossopharyngeal, vagus, accessory,
and hypoglossal nerves descending between the internal carotid artery and the internal jugular vein in the area immediately below the
jugular foramen. The glossopharyngeal nerve descends along the lateral side of the internal carotid artery. The accessory nerve passes
backward across the lateral surface of the internal jugular vein. The hypoglossal nerve passes through the hypoglossal canal, which is
located below and medial to the jugular foramen, and descends with the nerves exiting the jugular foramen. The occipital artery gives
rise to a meningeal branch, which passes through the jugular foramen to supply the surrounding dura, and to the stylomastoid artery,
which passes through the stylomastoid foramen with the facial nerve. A., artery; Asc., ascending; Aur., auricular; Br., branch; Cap.,
capitis; Car., carotid; Chor. Tymp., chorda tympani; CN, cranial nerve; Cond., condylar; Dors., dorsal; Eust., eustachian; Ext., external;
Fiss., fissure; Gl., gland; Gr., greater; Inf., inferior; Int., internal; Jug., jugular; Laryn., laryngeal; Lat., lateral, lateralis; Lev., levator; Long.,
longus; M., muscle; Mast., mastoid; Men., meningeal; N., nerve; Obl., oblique; Occip., occipital; Pal., palatini; Pet., petrosal, petrous;
Pharyn., pharyngeal; Post., posterior; Proc., process; Pteryg., pterygoid; Rec., rectus; Retromandib., retromandibular; Scap., scapulae; Seg.,
segment; Semicirc., semicircular; Sig., sigmoid; Squamotymp., squamotympanic; Sternocleidomast., sternocleidomastoid; Stylogloss.,
styloglossus; Stylomast., stylomastoid; Stylophar., stylopharyngeus; Submandib., submandibular; Sup., superior; Temp., temporal; Tens.,
tensor; TM., temporomandibular; Trans., transverse; Tymp., tympanic, tympany; V., vein; Vel., veli; Vent., ventral; Vert., vertebral.
S274 Rhoton
Neurosurgery, Vol. 47, No. 3, September 2000 Supplement
The vagus nerve exits the jugular foramen vertically, retain-
ing an intimate relationship to the accessory nerve (Figs. 9.3
9.5). At the level the two nerves exit the jugular foramen, they
are located behind the glossopharyngeal nerve on the pos-
teromedial wall of the internal jugular vein. As the vagus
nerve passes lateral to the outer orifice of the hypoglossal
canal, it is joined by the hypoglossal nerve medially. The
vagus nerve begins to expand at the site of the inferior vagal
FIGURE 9.4. EH. E, the superior
and inferior oblique have been
exposed by reflecting the more
superficial muscles. The C1
transverse process and rectus
capitis lateralis rest against the
posterior surface of the internal
jugular vein. The rectus capitis
lateralis attaches to the jugular
process of the occipital bone at the
posterior margin of the jugular
foramen. Retracting the levator
scapulae exposes the segment of
the vertebral artery ascending
through the C2 transverse foramen
in front of the ventral ramus of the
C2 nerve root. The vertebral artery,
as it passes medially along the
upper surface of the posterior arch
of the atlas, is situated in the floor
of the suboccipital triangle located
between the superior and inferior
oblique and rectus capitis posterior
major. F, the internal carotid artery
has been displaced posteriorly to
expose the branches of the
ascending pharyngeal, which pass
through the foramen lacerum,
jugular foramen, and hypoglossal
canal to supply the surrounding
dura. The chorda tympani exits the
skull in the medial part of the
condylar fossa by first passing
through the petrotympanic and
then along the squamotympanic
sutures. G, the tympanic bone
forming the lower and anterior
margin of the external meatus has
been removed, but the tympanic
sulcus to which the tympanic mem-
brane attaches has been preserved.
The surface of the temporal and occipital bones surrounding the jugular foramen and carotid canal have an irregular surface that
serves as the attachment of the upper end of the carotid sheath. The mastoid segment of the facial nerve and the stylomastoid fora-
men are situated lateral to the jugular bulb. The chorda tympani arises from the mastoid segment of the facial nerve and courses
along the deep side of the tympanic membrane crossing the neck of the malleus. It exits the skull by passing through the petrotym-
panic and squamotympanic sutures and joins the lingual branch of the mandibular nerve distally. The carotid ridge separates the
carotid canal and jugular foramen. Meningeal branches of the ascending pharyngeal and occipital arteries enter the jugular fora-
men. The glossopharyngeal, vagus, and accessory nerves pass through the jugular foramen on the medial side of the jugular bulb.
H, the tympanic ring and bone lateral to the tympanic cavity have been removed. The internal carotid artery has been displaced
forward out of the carotid canal to expose the carotid sympathetic nerves that ascend with the artery. The glossopharyngeal, vagus,
accessory, and hypoglossal nerves exit the skull on the medial side of the internal carotid artery and jugular vein. The glossopha-
ryngeal and hypoglossal nerves pass forward along the lateral surface of the internal carotid artery, and the accessory nerve de-
scends posteriorly across the lateral surface of the internal jugular vein. The vagus nerve descends in the carotid sheath.
Jugular Foramen S275
Neurosurgery, Vol. 47, No. 3, September 2000 Supplement
FIGURE 9.4. IN. I, lateral view of mastoid and tympanic cavity before removing the tympanic ring. The tympanic segment of the facial
nerve passes below the lateral semicircular canal and turns downward as the mastoid segment to exit the stylomastoid foramen. The
stylomastoid foramen and the mastoid segment are located lateral to the jugular bulb. The semicircular canals are located above the jugu-
lar bulb. J, a probe has been placed in the eustachian tube, which passes downward, forward, and medially from the tympanic cavity and
across the front of the petrous carotid. The third trigeminal division passes through the foramen ovale on the lateral side of the eustachian
tube. K, enlarged view of the tympanic ring with the tympanic membrane removed. The tensor tympany muscle passes backward above
the eustachian tube and gives rise to a tendon that turns sharply lateral around the trochleiform process to attach to the malleus. The
chorda tympani crosses the inner surface of the tympanic membrane and neck of the malleus. The round window opens into the vesti-
bule. The stapes sit in the oval window. The promontory is located lateral to the basal turn of the cochlea. L, the floor of the middle fossa
and the tympanic sulcus have been removed to expose the jugular bulb and petrous carotid. The greater petrosal nerve courses along the
floor of the middle fossa on the upper surface of the petrous carotid. The deep petrosal nerve arises from the sympathetic bundles on the
internal carotid artery. The deep and greater petrosal nerves join to form the vidian nerve, which passes forward through the vidian canal
to join the maxillary nerve and pterygopalatine ganglion in the pterygopalatine fossa. The pharyngobasilar fascia and upper part of the
S276 Rhoton
Neurosurgery, Vol. 47, No. 3, September 2000 Supplement
ganglion just below the foramen and is approximately 2.5 cm
in length.
Accessory nerve
Although the cranial and spinal portions of the accessory
nerve most frequently enter the vagal meatus together, they
may infrequently be separated by a dural septum. The spinal
portion ascends toward the foramen magnum by crawling
along the surface of the dura and may even be buried in the
dura below the foramen magnum (Figs. 9.3, 9.5, and 9.6). At
the dural orifice of the jugular foramen, the nerve is often
indistinguishable from the vagus nerve. The accessory nerve
usually enters the same dural subcompartment as the vagus
nerve and often adheres and blends into the vagus nerve at
the level of the superior vagal ganglion. The accessory nerve
departs the vagal ganglion after it exits the jugular foramen
and descends obliquely laterally between the internal carotid
artery and internal jugular vein and then backward across the
lateral surface of the vein to reach its muscles. Approximately
30% of nerves descend along the medial, rather than the
lateral, surface of the internal jugular vein (8).
Hypoglossal nerve
The hypoglossal nerve does not traverse the jugular fora-
men (Figs. 9.39.5). However, it joins the nerves exiting the
jugular foramen just below the skull and runs with them in
the carotid sheath. The nerve exits the inferolateral part of the
hypoglossal canal and passes adjacent to the vagus nerve,
descends between the internal carotid artery and the internal
jugular vein to the level of the transverse process of the atlas,
where it turns abruptly forward along the lateral surface of
the internal carotid artery toward the tongue, leaving only the
ansa cervicalis to descend with the major vessels.
ARTERIAL RELATIONSHIPS
The arteries that may be involved in pathological abnor-
malities at the jugular foramen include the upper cervical and
petrous portions of the internal carotid artery, the posteriorly
directed branches of the external carotid artery, and the upper
portion of the vertebral artery (Fig. 9.4).
Internal carotid artery
The internal carotid artery passes, almost straightly up-
ward, posterior to the external carotid artery and anterome-
dial to the internal jugular vein, to reach the carotid canal (Fig.
9.4). At the level of the skull base, the internal jugular vein
courses just posterior to the internal carotid artery, being
separated from it by the carotid ridge. Between them, the
glossopharyngeal nerve is located laterally and the vagus,
accessory, and hypoglossal nerves medially.
After the internal carotid artery enters the carotid canal
with the carotid sympathetic nerves and surrounding venous
plexus, it ascends a short distance (the vertical segment),
reaching the area below and slightly behind the cochlea,
where it turns anteromedially at a right angle (the site of the
lateral bend) and courses horizontally (the horizontal seg-
ment) toward the petrous apex (Fig. 9.4). At the medial edge
of the foramen lacerum, it turns sharply upward at the site of
the medial bend to enter the posterior part of the cavernous
sinus.
External carotid artery
The external carotid artery ascends anterior to the internal
carotid artery. Proximal to its terminal bifurcation into the
maxillary and the superficial temporal arteries, it gives rise to
six branches, which can be divided into anterior and posterior
groups according to their directions. The latter group is re-
lated to the jugular foramen.
The ascending pharyngeal artery, the first branch of the
posterior group, often provides the most prominent supply to
the meninges around the jugular foramen (Fig. 9.4) (18). It
arises either at the bifurcation or from the lowest part of the
external or internal carotid arteries. Rarely it arises from the
origin of the occipital artery. It courses upward between the
internal and the external carotid arteries, giving rise to nu-
merous branches to neighboring muscles, nerves, and lymph
nodes. Its meningeal branches pass through the foramen
lacerum to be distributed to the dura lining the middle fossa
and through the jugular foramen or the hypoglossal canal to
supply the surrounding dura of the posterior cranial fossa.
The ascending pharyngeal artery also gives rise to the inferior
tympanic artery, which reaches the tympanic cavity by way of
the tympanic canaliculus along with the tympanic branch of
the glossopharyngeal nerve.
The occipital artery, the second and largest branch of the
posterior group, arises from the posterior surface of the ex-
ternal carotid artery and courses obliquely upward between
the posterior belly of the digastric muscle and the internal
jugular vein (Fig. 9.4). Its meningeal branches, which enter the
posterior fossa through the jugular foramen or the condylar
canal, may make a significant contribution to tumors of the
jugular foramen.
The posterior auricular artery, the last branch in the poste-
rior group, arises above the posterior belly of the digastric
muscle and travels between the parotid gland and the styloid
process. At the anterior margin of the mastoid process, it
divides into auricular and occipital branches, which are dis-
longus capitis have been reflected downward to expose the lower margin of the clivus. M, the jugular bulb has been removed from the
jugular fossa located below the vestibule and semicircular canals. The vertical segment of the petrous carotid has been removed. The
cochlea, which has been opened, is located above the lateral genu of the petrous carotid. The tympanic segment of the facial nerve
passes posteriorly below the lateral semicircular canal. N, the retrosigmoid and presigmoid dura have been opened. The lateral wall of
the vestibule and cochlea have been removed. The vestibule, semicircular canals, and cochlea are exposed above the jugular bulb and
lateral genu of the petrous carotid.
Jugular Foramen S277
Neurosurgery, Vol. 47, No. 3, September 2000 Supplement
tributed to the postauricular and the occipital regions respec-
tively. The stylomastoid branch, which arises below the stylo-
mastoid foramen, enters the stylomastoid foramen to supply
the facial nerve. Its loss can lead to a facial palsy even though
it anastomoses with the petrosal branch of the middle men-
ingeal artery. The posterior auricular branch may share a
common trunk with the occipital artery, or sometimes it is
absent, in which case, the occipital artery gives rise to the
FIGURE 9.5. A, posterior view of the intracranial aspect of the left jugular foramen. The glossopharyngeal, vagus, and accessory nerves
pierce the dural roof of the jugular foramen. The glossopharyngeal nerve is separated from the vagus nerve by a narrow dural septum.
The jugular dural fold projects downward and medially from the lateral and upper margin of the jugular foramen over the site at which
the nerves enter the dura roof of the foramen. The facial and vestibulocochlear nerves and labyrinthine artery enter the internal acoustic
meatus. The subarcuate branch of the anteroinferior cerebellar artery enters the subarcuate fossa. The endolymphatic sac is located
between the dural layers lateral to the jugular foramen. A bridging vein from the medulla joins the inferior petrosal sinus on the medial
side of the jugular bulb. B, the dura has been removed from the posterior surface of the temporal bone. The intrajugular processes of the
temporal and occipital bones, which are connected by a fibrous bridge, the intrajugular septum, separates the sigmoid and petrosal parts
of the foramen. The glossopharyngeal, vagus, and accessory nerves enter the intrajugular part of the foramen by penetrating the dura on
the medial side of the intrajugular process of the temporal bone. C, the glossopharyngeal nerve enters the jugular foramen below the
cochlear aqueduct. The vagus nerve enters the jugular foramen behind the glossopharyngeal nerve. The auricular branch of the vagus
nerve (Arnolds nerve) arises at the level of the superior ganglion and passes around the anterior wall of the jugular bulb. The acces-
sory nerve is formed by multiple rootlets, which arise from the medulla and spinal cord. The accessory rootlets collect together to form a
bundle that blends into the lower margin of the vagus nerve at the level of the jugular foramen. The lower vagal and accessory roots pass
across the surface of the jugular tubercle. D, enlarged view. The glossopharyngeal nerve expands at the site of the superior and inferior
ganglia. The superior ganglion of the vagus nerve is located at the level of or just below the dural roof of the foramen, and the infe-
rior ganglion is located below the foramen at the level of the atlanto-occipital joint. A., artery; Atl., atlanto-; Aur., auricular; Br., branch;
Bridg., bridging; Car., carotid; CN, cranial nerve; Coch., cochlear; Cond., condyle; Endolymph., endolymphatic; Gang., ganglion; Glosso-
phar., glossopharyngeal; Hypogl., hypoglossal; Inf., inferior; Int., internal; Intrajug., intrajugular; Jug., jugular; Labyr., labyrinthine; Lat.,
lateral; Occip., occipital; Pet., petrosal; Proc., process; Sig., sigmoid; Subarc., subarcuate; Sup., superior; Temp., temporal; Vert., vertebral.
S278 Rhoton
Neurosurgery, Vol. 47, No. 3, September 2000 Supplement
stylomastoid artery. Members of the anterior group, whose
origins may be visualized in exposing lesions of the jugular
foramen, include the superior thyroid, lingual, and facial
arteries.
Vertebral artery
The vertebral artery, as it ascends to reach and pass
through the transverse foramen of the atlas, is located below
and behind the jugular foramen (Fig. 9.4). Branches encoun-
tered in approaches to lesions of the jugular foramen include
the meningeal, posterior spinal, and posteroinferior cerebellar
artery.
VENOUS RELATIONSHIPS
The jugular bulb and adjacent part of the internal jugular
vein receives drainage from both intracranial and extracranial
sources, which include the sigmoid and inferior petrosal si-
nuses, the vertebral venous plexus, the venous plexus of the
hypoglossal canal, the posterior condylar emissary vein, and
FIGURE 9.6. Retrosigmoid approach to jugular foramen. A, the detail shows the site of the vertical scalp incision and right
retrosigmoid craniotomy. The cerebellum has been elevated to expose the nerves in the right cerebellopontine angle. The
glossopharyngeal and vagal nerves are separated by the dural septum at the level of the dural roof of the jugular foramen.
The glossopharyngeal nerve enters the glossopharyngeal meatus and the vagus nerve enters the vagal meatus with the
branches of the accessory nerve. Both meatus are very shallow compared with the internal acoustic meatus. The superior and
lateral margins of both meatus project downward and medially over the nerves entering the meatus. The vertebral artery dis-
places the hypoglossal rootlets of Cranial Nerve XII posteriorly so that they intermingle with the rootlets of the accessory
nerve. B, another specimen showing the relationship of the rhomboid lip and choroid plexus protruding from the foramen of
Luschka to the glossopharyngeal and vagus nerves. The choroid plexus protrudes laterally behind the glossopharyngeal nerves.
The rhomboid lip is a thin layer of neural tissue that forms the ventral margin of the foramen of Luschka at the outer end of
the lateral recess. C and D, enlarged view of two jugular foramina. The glossopharyngeal and vagus nerves are consistently
separated by a dural septum at the level of the roof over the jugular foramen. The jugular dural fold projects downward and
medially over the lateral edge of the glossopharyngeal and vagal meatus and over the site at which the nerves penetrate the
dura. A., artery; A.I.C.A., anteroinferior cerebellar artery; Chor., choroid; CN, cranial nerve; Glossophar., glossopharyngeal;
Jug., jugular; Plex., plexus; Vert., vertebral.
Jugular Foramen S279
Neurosurgery, Vol. 47, No. 3, September 2000 Supplement
the vein coursing along the inferior aspect of the petroclival
fissure (Figs. 9.4 and 9.5).
Sigmoid sinus and jugular bulb
The sigmoid sinus is the largest channel emptying into the
jugular foramen (Figs. 9.1 and 9.39.5). After coursing down
the sigmoid sulcus, the sinus turns anteriorly toward the
jugular foramen, crossing the occipitomastoid suture imme-
diately proximal to the foramen. From there, the sinus is
directed forward below the petrous temporal bone at the site
of the jugular bulb. The upward bulging of the superior
margin of the jugular bulb creates a rounded fossa in the
lower surface of the temporal bone below the internal audi-
tory canal. The dome of the jugular bulb may extend upward
in the posterior wall of the internal auditory canal to the level
of the upper margin of the canal. The bulb is usually larger on
the right side, reflecting the larger diameter of the sigmoid
sinus on that side. From the level of the jugular bulb, flow is
directed downward behind the tympanic bone and the carotid
canal into the internal jugular vein.
Inferior petrosal sinus and venous confluens
The foramen also receives the inflow from the inferior
petrosal sinus and the venous confluens in the petrosal part of
the foramen. The inferior petrosal sinus, which courses on the
intracranial surface of the petroclival fissure, communicates
the cavernous sinus and basilar venous plexus at its upper
end and with the jugular bulb at its lower end (Figs. 9.3 and
9.5). The inferior petrosal sinus, as it enters the petrosal part of
the jugular foramen, forms a plexiform confluens with the
venous plexus of the hypoglossal canal, the inferior petro-
clival vein, and tributaries from the vertebral venous plexus
and posterior condylar emissary vein. This confluens, which
fills the petrosal part of the foramen, usually consists of a
main channel, 2 to 3 mm in diameter, and several smaller
channels, less than 1 mm in diameter. It empties into the
medial aspect of the jugular bulb through one or two open-
ings in the venous walls between the glossopharyngeal and
vagus nerves or into the internal jugular vein below the
extracranial orifice.
The inferior petroclival vein courses along the extracranial
surface of the petroclival fissure and is a mirror image of the
inferior petrosal sinus, which courses along the intracranial
surface of the fissure (Fig. 9.5). It empties into the venous
confluens at the lower end of the inferior petrosal sinus at or
just below the extracranial orifice of the jugular foramen or
even above it, through bony clefts between the temporal and
occipital bones.
Bridging veins
A bridging vein, which courses posterior to the glossopha-
ryngeal, vagus, and accessory nerves from the dorsolateral
medulla to the lower end of the sigmoid sinus, is present in
about one-third of cerebellopontine angles (Fig. 9.5, also see
Fig. 3.12). Infrequently, a bridging vein extends from the
ventral medulla to the lower margin of the inferior petrosal
sinus in front of the nerves.
MUSCULAR RELATIONSHIPS
Several muscles that are encountered in the surgical ap-
proaches to the jugular foramen and that provide important
landmarks in the approach are reviewed in detail in the
chapters on the foramen magnum and temporal bone (Fig.
9.4). These include the sternocleidomastoid, situated superfi-
cially in the lateral neck, and the splenius capitis, longissimus
capitis, levator scapulae, and scalenus medius muscles in a
deeper muscular layer.
More anteriorly is the posterior belly of the digastric mus-
cle, which arises in the digastric groove located medial to the
mastoid process and the longissimus capitis. The styloid pro-
cess and its attached muscles appear in the triangular zone
bounded by the posterior belly of the digastric, the external
auditory canal, and the mandibular ramus. Reflecting the
digastric muscle exposes the transverse process of the atlas,
which is covered by the attachments of numerous muscles,
including the superior and inferior obliques, which form the
upper and lower margin of the suboccipital triangle. The
rectus capitis lateralis muscle is the muscle most intimately
related to the jugular foramen. It extends vertically behind the
internal jugular vein from the transverse process of the atlas
to the jugular process of the occipital bone.
On the posterior neck are the trapezius muscle, splenius
capitis, and semispinalis capitis. Beneath the semispinalis ca-
pitis muscle, three muscles arise between the inferior nuchal
line and the margin of the foramen magnum: the rectus capitis
posterior major and minor and the superior oblique muscle.
The suboccipital triangle, an area defined by the opposing
margins of the rectus capitis posterior major and the superior
and inferior oblique muscles, is the site at which the vertebral
artery courses along the upper posterior surface of the atlas.
SURGICAL APPROACHES
Postauricular transtemporal approach
The postauricular transtemporal approach accesses the re-
gion from laterally, through the mastoid, and from below,
through the neck (Fig. 9.7) (2, 4, 5). A C-shaped postauricular
skin incision provides the exposure for a mastoidectomy and
the neck dissection. The external auditory canal is either pre-
served or transected, depending on the anterior extent of the
pathological abnormality. The neck dissection is completed
initially to gain control of the major vessels and the branches
supplying the tumor. The internal carotid artery, branches of
the external carotid artery, internal jugular vein, and lower
cranial nerves are exposed in the carotid sheath. A mastoid-
ectomy with extensive drilling of the infralabyrinthine region
accesses the jugular bulb. A limited mastoidectomy confined
to the area behind the stylomastoid foramen and mastoid
segment of the facial nerve, combined with removal of the
adjacent part of the jugular process of the temporal bone, will
provide access to the posterior and posterolateral aspect of the
jugular foramen. Three obstacles to exposure of the full lateral
half of the jugular foramen, the facial nerve, styloid process,
and rectus capitis lateralis muscle are dealt with by transpos-
ing the facial nerve, removing the styloid process, and divid-
S280 Rhoton
Neurosurgery, Vol. 47, No. 3, September 2000 Supplement
ing the rectus capitis lateralis muscle. Anterior extensions of
the pathological abnormality are reached by sacrificing the
external and the middle ear structures. Sensorineural hearing
can be preserved by maintaining the foot plate of the stapes in
the oval window to avoid opening the labyrinth. Intracranial
extensions of the lesion are reached by the retrosigmoid or
presigmoid approaches after adding a suboccipital craniec-
tomy. The lesion can be removed by a transtemporal infral-
abyrinthine approach directed through the temporal bone
below the labyrinth without the neck dissection, if the ex-
tracranial extension of the lesion is not prominent. The expo-
sure can be extended by opening the otic capsule (translaby-
rinthine approach).
Retrosigmoid approach
A pathological abnormality located predominantly intra-
durally can be resected by the retrosigmoid approach (Fig.
9.6). A lateral suboccipital craniectomy exposes the dura be-
hind the sigmoid sinus. The dura is opened, and the cerebel-
lum is gently elevated away from the posterior surface of the
temporal bone to expose the cisterns in the cerebellopontine
FIGURE 9.7. AD. Postauricular exposure of the jugular foramen. A, the detail shows the site of the scalp incision. The
C-shaped retroauricular incision provides access for the mastoidectomy, neck dissection, and parotid gland displacement. The
scalp flap has been reflected forward to expose the sternocleidomastoid and the posterior part of the parotid gland. B, the
more superficial muscles and the posterior belly of the digastric have been reflected to expose the internal jugular vein and
the attachment of the superior and inferior oblique to the transverse process of C1. A mastoidectomy has been completed to
expose the facial nerve, sigmoid sinus, and capsule of the semicircular canals. C, enlarged view of the mastoidectomy. The
jugular bulb is exposed below the semicircular canals. The chorda tympani arises from the mastoid segment of the facial
nerve and passes upward and forward. The tympanic segment of the facial nerve courses below the lateral canal. D, enlarged
view of the caudal part of the exposure shown in C. The facial nerve and styloid process cover the extracranial orifice of the
jugular foramen. The facial nerve crosses the lateral surface of the styloid process. The stylomastoid artery arises from the
postauricular artery. The rectus capitis lateralis attaches to the jugular process of the occipital bone behind the jugular fora-
men. A., artery; Aur., auricular; Cap., capitis; Car., carotid; Chor. Tymp., chorda tympani; CN, cranial nerve; Coch., cochlear;
Gl., gland; Gr., greater; Inf., inferior; Int., internal; Intrajug., intrajugular; Jug., jugular; Laryn., laryngeal; Lat., lateral, latera-
lis; M., muscle; Med., medial; Mid., middle; N., nerve; Obl., oblique; Occip., occipital; Pet., petrosal, petrous; Post., posterior;
Proc., process; Rec., rectus; Semicirc., semicircular; Sig., sigmoid; Sternocleidomast., sternocleidomastoid; Stylomast., stylo-
mastoid; Sup., superior; Symp., sympathetic; Tr., trunk; Trans., transverse; V., vein.
Jugular Foramen S281
Neurosurgery, Vol. 47, No. 3, September 2000 Supplement
angle and the intracranial aspect of the cranial nerves entering
the jugular foramen, hypoglossal canal, and internal acoustic
meatus.
Far-lateral approach
An extended modification of the retrosigmoid approach, the
far-lateral approach, the subject of another chapter in this issue,
may be selected if the tumor extends down to the foramen
magnum in front of or lateral to the lower brainstem (10, 30, 32,
33). In this approach, the jugular foramen is opened from be-
hind. The dura is opened and the cerebellum elevated to expose
the intracranial extension of the pathological abnormality at the
lower clivus and at the foramen magnum. Several variations,
depending on the location and extent of the pathological abnor-
mality, include drilling the jugular tubercle extradurally and
removing bone above without disturbing the condyle (21, 33).
The extradural reduction of the jugular tubercle aids in minimiz-
FIGURE 9.7. EH. E, the external auditory canal has been transected and the middle ear structures have been removed,
except the stapes, which has been left in the oval window. The lateral edge of the jugular foramen has been exposed by com-
pleting the mastoidectomy, transposing the facial nerve anteriorly, and fracturing the styloid process across its base and
reflecting it caudally. The rectus capitis lateralis has been detached from the jugular process of the occipital bone. The
petrous carotid is surrounded in the carotid canal by a venous plexus. F, a segment of the sigmoid sinus, jugular bulb, and
internal jugular vein have been removed. The lateral wall of the jugular bulb has been removed while preserving the medial
wall and exposing the opening of the inferior petrosal sinus into the jugular bulb. Removing the venous wall exposes the glos-
sopharyngeal, vagus, accessory, and hypoglossal nerves, which are hidden deep to the vein. The main inflow from the petro-
sal confluens is directed between the glossopharyngeal and vagus nerves. G, the medial venous wall of the jugular bulb has
been removed. The intrajugular ridge extends forward from the intrajugular process, which divides the jugular foramen
between the sigmoid and petrosal parts. The glossopharyngeal, vagus, and accessory nerves enter the dura on the medial side
of the intrajugular process, but only the glossopharyngeal nerve courses through the foramen entirely on the medial side of the
intrajugular ridge. The vagus nerve also enters the dura on the medial side of the intrajugular process, but does not course along
the medial side of the intrajugular ridge. H, the intrajugular process and ridge have been removed to expose the passage of the
glossopharyngeal, vagus, and accessory nerves through the jugular foramen. The tip of a right-angle probe identifies the junction of
the cochlear aqueduct with the pyramidal fossa, just above where the glossopharyngeal nerve penetrates the dura.
S282 Rhoton
Neurosurgery, Vol. 47, No. 3, September 2000 Supplement
ing the retraction of the brainstem needed to reach the area
anterior to the medulla and pontomedullary junction.
Preauricular subtemporal-infratemporal approach
The preauricular subtemporal-infratemporal approach, re-
viewed in detail in the chapter on the temporal bone (see Figs.
8.10 and 8.18), exposes the jugular foramen anteriorly. It may
be selected for tumors that extend along the petrous portion of
the internal carotid artery, through the eustachian tube, or
through the cancellous portion of the petrous apex (29). A
preauricular hemicoronal scalp incision is extended down to
at least the level of the tragus and possibly into the cervical
region, depending on the extent of the pathological finding
and whether a neck dissection is needed. The zygomatic arch
is removed or reflected downward with the temporalis mus-
cle, taking care to preserve the frontal branch of the facial
nerve. A frontotemporal bone flap, which may include the
superior or lateral orbital rim, is elevated, and the glenoid
fossa and the mandibular condyle with the joint capsule are
either dislocated inferiorly or removed. The dura is elevated,
and the bone of the middle fossa medial to the glenoid fossa
is removed until the carotid canal is opened. The eustachian
tube and the tensor tympani muscle, which course anterior to
the carotid canal, are sacrificed during this procedure, taking
care to protect the lower cranial nerves as they exit the jugular
foramen. The styloid process is divided at its base, and the
internal carotid artery is reflected anteriorly to gain access to
the clivus and anterior aspect of the jugular foramen. Drilling
can be extended to the posterior fossa through Kawases
triangle or through the clivus to the contralateral internal
carotid artery (14).
DISCUSSION
Pathologies
Tumors are the most common lesions to affect the jugular
foramen; the majority are chemodectomas (glomus jugulare
tumor), neurinomas, and meningiomas, with a small percent-
age of other tumors, such as chondrosarcomas and chordo-
mas (12, 25). The glomus jugulare tumor arises either in the
adventitia of the jugular dome or from the intumescences
along the tympanic branch of the glossopharyngeal nerve or
the auricular branch of the vagus nerve in the jugular foramen
(9). Tumors of the same nature that arise in the tympanic
cavity or in the mastoid on branches of these nerves are
referred to as glomus tympanicum tumors. Small glomus
jugulare tumors remain confined within the jugular foramen.
However, the tumor can extend as follows: 1) along the eu-
stachian tube into the nasopharynx and through the foramina
at the base of the skull, 2) along the carotid artery to the
middle fossa, 3) through the intracranial orifice of the jugular
foramen or along the hypoglossal canal to the posterior fossa,
4) through the tegmen tympani to the floor of the middle
fossa, 5) through the round window and the internal acoustic
meatus to the cerebellopontine angle, and 6) through the
extracranial orifice of the jugular foramen to the upper cervi-
cal region.
Neuromas arise either from the glossopharyngeal, vagus, or
the accessory nerves, and meningiomas from arachnoid gran-
ulations in the jugular bulb or venous sinuses. Although each
tumor has characteristic patterns of invasion and destruction,
the basic anatomic environment is similar to that of the glo-
mus jugulare tumor.
Selection of surgical approach
The approaches to the jugular foramen can be categorized
into three groups: 1) a lateral group directed through the
mastoid bone, 2) a posterior group directed through the pos-
terior cranial fossa, and 3) an anterior group directed through
the tympanic bone. This categorization is based on the ana-
tomic fact that the block of the temporal bone, excluding the
squamous part, is regarded as an irregular pyramid, having
its base on the mastoid surface. In addition, the middle fossa
approaches could be categorized as in the superior group
and the neck dissection upward to the jugular foramen as in
the inferior group. However, the latter approaches are usu-
ally not suitable when used alone for pathological abnormal-
ities of the jugular foramen.
Lateral approach
The lateral approach directed through a mastoidectomy,
used alone or in combination with other approaches, is the
route most commonly selected for lesions extending through
the jugular foramen (7, 12, 22). Because the jugular foramen is
situated under the otic capsule, the approach basic to this
group is called the infralabyrinthine approach. The facial
nerve is frequently transposed anteriorly to drill the bone
inferior to the labyrinth. Avoiding injury to the facial nerve is
one of the key points in the lateral approaches (1). Even with
special care, some degree of transient facial palsy is common,
possibly because of disturbance to the nerves vasculature.
The surgical field can be widened anteriorly by sacrificing the
external auditory canal and middle ear structures or medially
by drilling away the otic capsule (translabyrinthine approach)
or cochlea (transcochlear approach).
The postauricular transtemporal approach, when combined
with a neck dissection, provides satisfactory exposure of the
jugular foramen, mastoid air cells, tympanic cavity, and the
extracranial structures in and around the carotid sheath. Re-
moval of the styloid process along with transposition of the
facial nerve facilitates wide opening of the extracranial orifice
of the jugular foramen and provides access to the lower part
of the petrous portion of the internal carotid artery. A wider
exposure for the extracranial tumor can be obtained by re-
moving the transverse process of the atlas or dislocating or
resecting the mandibular condyle. The intracranial extension
of the tumor is approached either retrosigmoidally or presig-
moidally after adding a lateral suboccipital craniectomy or
craniotomy (4, 6, 10, 26, 27).
Posterior approach
This group includes the retrosigmoid approach and its
more extensive far-lateral and transcondylar variants. These
approaches are suited to the intracranial portion of the tu-
Jugular Foramen S283
Neurosurgery, Vol. 47, No. 3, September 2000 Supplement
mors. The conventional retrosigmoid approach provides access
to the cerebellopontine angle and the intracranial orifice of the
jugular foramen. However, extensions of the tumor through
the foramen magnum or medially into the clivus are beyond the
reach of this approach. The far-lateral and transcondylar modi-
fications access these areas, providing an upward view from
below by opening the posterolateral quarter of the foramen
magnum and removing the posterior part of the occipital con-
dyle. The posterior and posterolateral margin of the jugular
foramen can be accessed by removing the part of the jugu-
lar process of the occipital bone located behind the jugular
foramen and the portion of the mastoid located behind the
mastoid segment of the facial nerve and stylomastoid fora-
men. A flatter view toward the midline clivus is obtained by
additional extradural drilling of the jugular tubercle, although
drilling in front of these nerves risks damaging the nerves as
they cross the jugular tubercle (21, 23).
Anterior approach
The preauricular subtemporal-infratemporal approach is a
major variant of this group of approaches. It uses the pathway
anterior to the external auditory canal and through the tym-
panic bone, which are exposed by removal or displacement of
the glenoid fossa and the temporomandibular joint. The ap-
proach alone can access the anterior part of the jugular fora-
men after reflecting the petrous portion of the internal carotid
artery anteriorly. Further extensive drilling will expose the
middle to upper clivus anteriorly. However, this approach is
most often combined with a lateral approach to access an
anterior extension of the pathology (22). Fisch et al. call this
combined approach the infratemporal fossa approach, Type B
or C according to the anterior extension of the exposure (4).
The selection of the optimal approach requires an under-
standing of the nature and the extension of the lesion. The
combination of two or three approaches may be needed either
in stages or in combination in one operative procedure (4, 25).
Preoperative embolization will often reduce the blood loss
with a vascular tumor. Intraoperative electrophysiological
monitoring is of great help in avoiding nerve injury, in locat-
ing the neural trajectory in and around the tumor, or in
predicting postoperative neural function (3, 20). Carefully
planned reconstruction is required to reduce postoperative
complications, especially leakage of cerebrospinal fluid, and
to achieve a satisfactory cosmetic result.
Reprint requests: Albert L. Rhoton, Jr., M.D., Department of Neuro-
logical Surgery, University of Florida Brain Institute, P.O. Box 100265,
100 S. Newell Drive, Building 59, L2100, Gainesville, FL 32610-0265.
REFERENCES
1. Brackmann DE: The facial nerve in the infratemporal approach.
Otolaryngol Head Neck Surg 97:1517, 1987.
2. Brackmann DE, Arriaga MA: Surgery for glomus tumors,
in Brackmann DE (ed): Otologic Surgery. Philadelphia, W.B.
Saunders Co., 1994, pp 579593.
3. DiChiro G, Fischer RL, Nelson KB: The jugular foramen. J Neuro-
surg 21:447460, 1964.
4. Fisch U, Fagan P, Valavanis A: The infratemporal fossa approach for
the lateral skull base. Otolaryngol Clin N Am 17:513552, 1984.
5. Gardner G, Cocke EW, Robertson JT, Trumbull ML, Palmer RE:
Combined approach surgery for removal of glomus jugulare tu-
mors. Laryngoscope 87:665688, 1977.
6. Gardner G, Robertson JT, Robertson JH, Cocke EW, Clark WC:
Glomus jugulare tumors: Skull base surgery, in Schmidek HH,
Sweet WH (eds): Operative Neurological Techniques. Philadelphia,
W.B. Saunders Co., 1988, ed 2, pp 739752.
7. Goldenberg RA, Gardner G: Tumors of the jugular foramen:
Surgical preservation of neural function. Otolaryngol Head Neck
Surg 104:129, 1991.
8. Grant JCB: An Atlas of Anatomy. Baltimore, Williams &Wilkins, 1951.
9. Guild SR: Glomus jugulare in man. Ann Otol Rhinol Laryngol
62:10451071, 1953.
10. Hakuba A, Hashi K, Fujitani K, Ikuno H, Nakamura T, Inoue Y:
Jugular foramen neurinomas. Surg Neurol 11:8394, 1979.
11. Hovelacque A: Osteologie. Paris, G Doin and Cie, 1967, vol 2, pp
155156.
12. Jackson CG, Cueva RA, Thedinger BA, Glasscock ME III: Cranial
nerve preservation in lesions of the jugular fossa. Otolaryngol
Head Neck Surg 105:687693, 1991.
13. Katsuta T, Rhoton AL Jr, Matsushima T: The jugular foramen:
Microsurgical anatomy and operative approaches. Neurosurgery
41:149202, 1997.
14. Kawase T, Toya S, Shiobara R, Mine S: Transpetrosal approach for
aneurysms of the lower basilar artery. J Neurosurg 63:857867, 1985.
15. Kveton JF, Cooper MH: Microsurgical anatomy of the jugular
foramen region. Am J Otol 9:109112, 1988.
16. Lang J: Anatomy in and on the jugular foramen, in Frowein RA,
Brock M, Klinger M (eds): Advances in Neurosurgery. Berlin,
Springer-Verlag, 1989, vol 17, pp 125132.
17. Lang J: Clinical Anatomy of the Posterior Cranial Fossa and its Foram-
ina. New York, Thieme Medical Publishers, 1991, pp 9295.
18. Lang J: Anatomy of the posterior cranial fossa, in Sekhar LN,
Janecka IP (eds): Surgery of Cranial Base Tumors. New York, Raven
Press, 1993, pp 131146.
19. Lang J, Weigel M: Nerve-vessel relations in the region of the
jugular foramen. Anat Clin 5:4156, 1983.
20. Leonetti JP, Brackmann DE, Prass RL: Improved preservation of
facial nerve function in the infratemporal approach to the skull
base. Otolaryngol Head Neck Surg 101:7478, 1989.
21. Matsushima, T, Ikezaki K, Nagata S, Inoue T, Natori Y, Fukui M,
Rhoton AL Jr: Microsurgical anatomy for lateral approaches to the
foramen magnum: With special reference to the far-lateral ap-
proach and the transcondylar approach, in Nakagawa H (ed):
Surgical Anatomy for Microneurosurgery VII. Tokyo, SciMed Publi-
cations, 1995, pp 8189.
22. Patel SJ, Sekhar LN, Cass SP, Hirsch BE: Combined approaches
for resection of extensive glomus jugulare tumors: A review of 12
cases. J Neurosurg 80:10261038, 1994.
23. Perneczky A: The posterolateral approach to the foramen mag-
num, in Samii M (ed): Surgery in and around the Brain Stem and the
Third Ventricle. Berlin, Springer-Verlag, 1986, pp 460466.
24. Rhoton AL Jr, Buza R: Microsurgical anatomy of the jugular
foramen. J Neurosurg 42:541550, 1975.
25. Samii M, Bini W: Surgical strategy for jugular foramen tumors, in
Sekhar LN, Janecka IP (eds): Surgery of Cranial Base Tumors. New
York, Raven Press, 1993, pp 379387.
26. Samii M, Draf W: Surgery of the middle skull base, in Samii M,
Dwarf W (eds): Surgery of the Skull Base: An Interdisciplinary Ap-
proach. New York, Springer-Verlag, 1989, pp 234359.
S284 Rhoton
Neurosurgery, Vol. 47, No. 3, September 2000 Supplement
27. Samii M, Babu RP, Tatagiba M, Sepehrnia A: Surgical treatment of
jugular foramen schwannomas. J Neurosurg 82:924932, 1995.
28. Schwaber MK, Netterville JL, Maciunas R: Microsurgical anatomy of
the skull base: A morphometric analysis. Am J Otol 11:401405, 1990.
29. Sekhar LN, Schramm VL Jr, Jones NF: Subtemporal-preauricular
infratemporal fossa approach to large lateral and posterior cranial
base neoplasms. J Neurosurg 67:488499, 1987.
30. Sen CN, Sekhar LN: An extreme lateral approach to intradural
lesions of the cervical spine and foramen magnum. Neurosurgery
27:197204, 1990.
31. Silverstein H, Willcox TO, Rosenberg SI, Seidman MD: The jug-
ular dural fold: A helpful base landmark to the cranial nerves.
Skull Base Surg 5:5761, 1995.
32. Spetzler RF, Grahm TW: The far-lateral approach to the inferior
clivus and the upper cervical region: Technical note. Barrow
Neurol Inst Q 6:3538, 1990.
33. Wen HT, Rhoton AL Jr, Katsuta T, de Oliveira E: Microsurgical
anatomy of the transcondylar, supracondylar, and paracondylar
extensions of the far-lateral approach. J Neurosurg 87:555585,
1997.
Cranial cavity with posterior fossa structures, including cerebellum and cranial nerves, from, Andreas Vesalius, De
Humani Corporis Fabrica. Basel, Ex officina Ioannis Oporini, 1543. Courtesy, Rare Book Room, Norris Medical Library,
Keck School of Medicine, Los Angeles, California. (Also see pages S27, S68, and S209.)
Jugular Foramen S285
Neurosurgery, Vol. 47, No. 3, September 2000 Supplement
S-ar putea să vă placă și
- Surgical Approaches To The Skull BaseDocument2 paginiSurgical Approaches To The Skull Baseİbrahim ErkutluÎncă nu există evaluări
- Anatomy and Surgical Approaches of TheDocument2 paginiAnatomy and Surgical Approaches of TheGabriela MacoveanuÎncă nu există evaluări
- Factsheet Acoustic NeuromaDocument12 paginiFactsheet Acoustic NeuromaAhmad ApriansahÎncă nu există evaluări
- Acoustic NeuromaDocument12 paginiAcoustic Neuromasusheel yeshala0% (1)
- Hair Transplant Surgery and Platelet Rich Plasma: Evidence-Based EssentialsDe la EverandHair Transplant Surgery and Platelet Rich Plasma: Evidence-Based EssentialsLinda N. LeeÎncă nu există evaluări
- Manual of Surgery Volume Second: Extremities—Head—Neck. Sixth Edition.De la EverandManual of Surgery Volume Second: Extremities—Head—Neck. Sixth Edition.Încă nu există evaluări
- Essentials of Diseases of the Skin: Including the Syphilodermata Arranged in the Form of Questions and Answers Prepared Especially for Students of MedicineDe la EverandEssentials of Diseases of the Skin: Including the Syphilodermata Arranged in the Form of Questions and Answers Prepared Especially for Students of MedicineÎncă nu există evaluări
- Handbook of Genetic Communicative DisordersDe la EverandHandbook of Genetic Communicative DisordersSanford E. GerberÎncă nu există evaluări
- Spontaneous Size Regression of Vestibular Schwannoma LXGKDocument2 paginiSpontaneous Size Regression of Vestibular Schwannoma LXGKIsmail Ali Syahbana100% (1)
- Through the Eyes of a Survivor - Traumatic Brain InjuryDe la EverandThrough the Eyes of a Survivor - Traumatic Brain InjuryÎncă nu există evaluări
- Venous-Preserving Sylvian DissectionDocument10 paginiVenous-Preserving Sylvian DissectionMorteza Mazloom Farsi BafÎncă nu există evaluări
- The Posterior Fossa Cisterns: Albert L. Rhoton, JR., M.DDocument12 paginiThe Posterior Fossa Cisterns: Albert L. Rhoton, JR., M.DIndra HadianditeÎncă nu există evaluări
- Acoustic NeuromaDocument14 paginiAcoustic NeuromaNeshanth SurendranÎncă nu există evaluări
- Carotid Cavernoid FistulaDocument18 paginiCarotid Cavernoid FistulaRishi SelvamÎncă nu există evaluări
- Brain CisternsDocument42 paginiBrain CisternsLepaca KliffothÎncă nu există evaluări
- 70.CHist TarlovDocument6 pagini70.CHist TarlovIoana BartokÎncă nu există evaluări
- Tentorial IncisuraDocument23 paginiTentorial Incisurabodeadumitru9261100% (1)
- DOD Letter To National Toxicity Panel On TCEDocument9 paginiDOD Letter To National Toxicity Panel On TCEChildren Of Vietnam Veterans Health AllianceÎncă nu există evaluări
- The Posterior Fossa VeinsDocument24 paginiThe Posterior Fossa Veinsbodeadumitru9261100% (2)
- Presenter: DR - Imran Qazi Ent-A Tmo KTHDocument15 paginiPresenter: DR - Imran Qazi Ent-A Tmo KTHimran qaziÎncă nu există evaluări
- Anatomy of The Callosomarginal Artery Applications To Microsurgery and Endovascular SurgeryDocument9 paginiAnatomy of The Callosomarginal Artery Applications To Microsurgery and Endovascular SurgeryvovaatanasovÎncă nu există evaluări
- The Cerebellopontine Angle and Posterior Fossa Cranial Nerves by TheDocument37 paginiThe Cerebellopontine Angle and Posterior Fossa Cranial Nerves by Thebodeadumitru9261100% (2)
- Systemc Lupus EritematousDocument41 paginiSystemc Lupus EritematousCanis MajorisÎncă nu există evaluări
- Explicative Cases of Controversial Issues in NeurosurgeryDocument544 paginiExplicative Cases of Controversial Issues in NeurosurgeryJosé Ramírez100% (2)
- Surgical Anatomy 1Document12 paginiSurgical Anatomy 1Donya Gholami100% (1)
- Acoustic NeuromaDocument52 paginiAcoustic NeuromaAnirudh V. BhatÎncă nu există evaluări
- LLLT in Hair GrowthDocument13 paginiLLLT in Hair GrowthCarlos SilvaÎncă nu există evaluări
- Functional Neuroanatomy Text and Atlas 2nd Edition by Adel AfifiDocument1.079 paginiFunctional Neuroanatomy Text and Atlas 2nd Edition by Adel AfifiPaola Andrea Martínez PérezÎncă nu există evaluări
- 1.5 DermatomesDocument2 pagini1.5 DermatomesAngela CaguitlaÎncă nu există evaluări
- Abdominal WallDocument75 paginiAbdominal WallJojo RyelciusÎncă nu există evaluări
- Analyzing and Defining Medical TermsDocument7 paginiAnalyzing and Defining Medical Termsmarcus colgroveÎncă nu există evaluări
- Anatomical Basis of Cranial Neurosurgery (PDFDrive)Document463 paginiAnatomical Basis of Cranial Neurosurgery (PDFDrive)Alkawthar M. AbdulsadaÎncă nu există evaluări
- Chapter 42 - Dizziness: Key Facts and CheckpointsDocument12 paginiChapter 42 - Dizziness: Key Facts and Checkpointsprofarmah6150Încă nu există evaluări
- CVA and TIADocument104 paginiCVA and TIADocRN100% (1)
- Trigeminal and Facial NerveDocument121 paginiTrigeminal and Facial NerveFadilaÎncă nu există evaluări
- Disorders of Upper and Lower Motor NeuronsDocument38 paginiDisorders of Upper and Lower Motor NeuronsDavid ParraÎncă nu există evaluări
- Hippocampus AnatomyDocument6 paginiHippocampus AnatomyravnoorÎncă nu există evaluări
- Nerve Suply To Head and NeckDocument22 paginiNerve Suply To Head and NeckrajtanniruÎncă nu există evaluări
- 104 Skull, Mandible & The Facial BonesDocument68 pagini104 Skull, Mandible & The Facial BonesSam Tagarda100% (1)
- REV Vestibular Disorders PDFDocument9 paginiREV Vestibular Disorders PDFDennis GasconÎncă nu există evaluări
- Arterial Suppply of Head&NeckDocument89 paginiArterial Suppply of Head&NeckPiyusha SharmaÎncă nu există evaluări
- Trigeminal Nerve: Presented by DR Harees Shabir JR I Departmant of PedodonticsDocument77 paginiTrigeminal Nerve: Presented by DR Harees Shabir JR I Departmant of PedodonticsHarees ShabirÎncă nu există evaluări
- Vascular Sonography TermsDocument4 paginiVascular Sonography TermsawansurfÎncă nu există evaluări
- Ultrasound Cavitation System 3in1 Beautyrelax Br-720 User GuideDocument15 paginiUltrasound Cavitation System 3in1 Beautyrelax Br-720 User GuideJohn Alexis Cofre CofreÎncă nu există evaluări
- What Is The Glycemic Index of Food?Document2 paginiWhat Is The Glycemic Index of Food?Robert StevenÎncă nu există evaluări
- Skull Base Tumors PDFDocument20 paginiSkull Base Tumors PDFhimadriÎncă nu există evaluări
- The EarDocument68 paginiThe EarSatyawira Aryawan Deng100% (1)
- Degeneration and Regenration of Nerve Fibers by Dr. RoomiDocument11 paginiDegeneration and Regenration of Nerve Fibers by Dr. RoomiMudassar RoomiÎncă nu există evaluări
- Middle EarDocument38 paginiMiddle EarJ NÎncă nu există evaluări
- The Intracranial Arachnoid MaterDocument17 paginiThe Intracranial Arachnoid MaterI'Jaz Farritz MuhammadÎncă nu există evaluări
- NIOSH Skin Notation ProfilesDocument24 paginiNIOSH Skin Notation ProfilesJesús Rafael Méndez NateraÎncă nu există evaluări
- Normal Mri Brain - Dr. Piyush OjhaDocument111 paginiNormal Mri Brain - Dr. Piyush OjhaAndrada CatrinoiuÎncă nu există evaluări
- FA NeurologyDocument179 paginiFA Neurologymanoj baniwalÎncă nu există evaluări
- 3.trigeminal NerveDocument81 pagini3.trigeminal NerverajaniÎncă nu există evaluări
- Word XPDocument6 paginiWord XPAVE100% (1)
- Revised International Table of Glycemic Index (Gi) and Glycemic Load (GL) Values - 2002Document47 paginiRevised International Table of Glycemic Index (Gi) and Glycemic Load (GL) Values - 2002fromhamilton5221Încă nu există evaluări
- Sudil Paudyal: 11/01/12 Abdomen Presentation by Sudil 1Document58 paginiSudil Paudyal: 11/01/12 Abdomen Presentation by Sudil 1Haba CristianÎncă nu există evaluări
- Frolich, Human Anatomy, Lower LimbDocument35 paginiFrolich, Human Anatomy, Lower LimbAzwarmuslimHasballahAminÎncă nu există evaluări
- LBP WhoDocument6 paginiLBP WhoMudsa Iing IletoÎncă nu există evaluări
- Vertigo BPPVDocument2 paginiVertigo BPPVleonjunchan_66965707Încă nu există evaluări
- Low Back PainDocument2 paginiLow Back PainBojan KrdžićÎncă nu există evaluări
- Tentorium IncisuraDocument24 paginiTentorium IncisuraIndra Hadiandite100% (1)
- The Posterior Fossa Cisterns: Albert L. Rhoton, JR., M.DDocument12 paginiThe Posterior Fossa Cisterns: Albert L. Rhoton, JR., M.DIndra HadianditeÎncă nu există evaluări
- The Cerebellar ArteriesDocument40 paginiThe Cerebellar Arteriesbodeadumitru9261100% (1)
- Acls Aha 2010Document67 paginiAcls Aha 2010heraaaaÎncă nu există evaluări
- An Invitro Antimicrobial Activity and Bioactivities of Protein Isolated From Marine Sponge - Callyspongia Sp.Document6 paginiAn Invitro Antimicrobial Activity and Bioactivities of Protein Isolated From Marine Sponge - Callyspongia Sp.Indra HadianditeÎncă nu există evaluări
- Bakteri Simbion SponsDocument6 paginiBakteri Simbion SponsIndra HadianditeÎncă nu există evaluări
- Streptococcus PneumoniaeDocument8 paginiStreptococcus PneumoniaeIndra HadianditeÎncă nu există evaluări
- Chart Boys Z 5 10yearsDocument1 paginăChart Boys Z 5 10yearsIndra HadianditeÎncă nu există evaluări
- Isolasi Dan Karakterisasi Aktinomisetes PenghasilDocument9 paginiIsolasi Dan Karakterisasi Aktinomisetes PenghasilIndra HadianditeÎncă nu există evaluări
- Discovery of Novel Metabolites From Marine ActinomycetesDocument7 paginiDiscovery of Novel Metabolites From Marine ActinomycetesAsep Awaludin PrihantoÎncă nu există evaluări
- Higher Algebra - Hall & KnightDocument593 paginiHigher Algebra - Hall & KnightRam Gollamudi100% (2)
- Theories of Counseling and Psychotherapy An Integrative Approach 2Nd Edition Jones Smith Test Bank Full Chapter PDFDocument32 paginiTheories of Counseling and Psychotherapy An Integrative Approach 2Nd Edition Jones Smith Test Bank Full Chapter PDFkatrina.green809100% (11)
- The History of Animals - by AristotleDocument17 paginiThe History of Animals - by Aristotledenunciaambev2023Încă nu există evaluări
- Omm Gurepro Test 2Document7 paginiOmm Gurepro Test 2eugevortÎncă nu există evaluări
- Cranial Base Dan Emergency CaseDocument34 paginiCranial Base Dan Emergency Caserahmad wahyuÎncă nu există evaluări
- Fetal SkullDocument4 paginiFetal Skullsubashik0% (1)
- Posterior Cranial Fossa Anesthetic ManagementDocument48 paginiPosterior Cranial Fossa Anesthetic ManagementDivya Rekha KolliÎncă nu există evaluări
- Cephalometric Evaluation and Measurement of The Upper Airway PDFDocument13 paginiCephalometric Evaluation and Measurement of The Upper Airway PDFSoe San KyawÎncă nu există evaluări
- Races of Britain PDFDocument350 paginiRaces of Britain PDFLuis Otavio Canevazzi de Freitas100% (1)
- 1.04 - The Skeletal SystemDocument7 pagini1.04 - The Skeletal Systemelio pascualÎncă nu există evaluări
- Lossing BerylArbucklesCranial PDFDocument67 paginiLossing BerylArbucklesCranial PDFdeemoney3100% (1)
- The Gross Anatomy of The Head and NeckDocument70 paginiThe Gross Anatomy of The Head and NeckYel YuriÎncă nu există evaluări
- Chapter 11 - SkullDocument10 paginiChapter 11 - Skullwamaithamargaret257Încă nu există evaluări
- Temporal BoneDocument104 paginiTemporal Bonekatnev100% (1)
- Anterior and Posterior Petrosectomy Seminar 13 Jan 2021 DR Abhinav 2Document76 paginiAnterior and Posterior Petrosectomy Seminar 13 Jan 2021 DR Abhinav 2Tamajyoti GhoshÎncă nu există evaluări
- 2 Introduction To Embryology and FetalDocument55 pagini2 Introduction To Embryology and Fetaldemeke andebetÎncă nu există evaluări
- Daftar Nama Anatomi Inggris-LatinDocument58 paginiDaftar Nama Anatomi Inggris-LatinFelicia NikeÎncă nu există evaluări
- John Rolland - Inside MotionDocument154 paginiJohn Rolland - Inside MotionAnisoara Cismasu100% (3)
- Lec 39 - Osteology of The SkullDocument25 paginiLec 39 - Osteology of The Skullleahbay100% (1)
- MCQs For Netters Head and Neck Anatomy For DentistryDocument211 paginiMCQs For Netters Head and Neck Anatomy For DentistryDR. ISHITA SINGHAL88% (8)
- Zoo 113 Selected SlidesDocument29 paginiZoo 113 Selected SlidesSheila Marie CuananÎncă nu există evaluări
- On of D.SC., F.R.S., C.M.Z.S., ofDocument10 paginiOn of D.SC., F.R.S., C.M.Z.S., ofАлександр ПономарёвÎncă nu există evaluări
- Blair Upper CervicalDocument4 paginiBlair Upper Cervicallopezhectora100% (1)
- Endoskeleton of The ChickenDocument20 paginiEndoskeleton of The ChickenJoachimÎncă nu există evaluări
- Antiquityofman 00 KeituoftDocument552 paginiAntiquityofman 00 Keituoftgamersgene100% (1)
- Anteroposterior CephalometricsDocument40 paginiAnteroposterior CephalometricsNingombam Robinson100% (2)
- Skeletal System: I. General CharacteristicsDocument34 paginiSkeletal System: I. General CharacteristicsMason BruceÎncă nu există evaluări
- Bpes2 SemDocument95 paginiBpes2 Semnishthabanga1525Încă nu există evaluări
- Mosby's Orthodontic Review (2nd Edition) Pages 92 - 96Document5 paginiMosby's Orthodontic Review (2nd Edition) Pages 92 - 96sillyazianÎncă nu există evaluări
- Skull ProjectionsDocument66 paginiSkull Projectionsron reteracionÎncă nu există evaluări
- Autopsy: Forensic Medicine & Toxicology, NMCDocument106 paginiAutopsy: Forensic Medicine & Toxicology, NMCAiman sadiq shahÎncă nu există evaluări