Documente Academic
Documente Profesional
Documente Cultură
Terapi British Seks
Încărcat de
RakaArdiansyah0 evaluări0% au considerat acest document util (0 voturi)
59 vizualizări5 paginiadf
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentadf
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
59 vizualizări5 paginiTerapi British Seks
Încărcat de
RakaArdiansyahadf
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 5
Final 15/02/08
United Kingdom National Guideline on the Management of Molluscum
Contagiosum (2007)
Clinical Effectiveness Group (British Association of Sexual Health and HIV)
Introduction and methodology
Scope and purpose
Molluscum contagiosum (MC) is a benign viral skin infection most commonly seen in
children. However sexual contact in adults may lead to the appearance of lesions in the
genital area. The main objective of this guideline is to enable the healthcare practitioner
to reassure a patient with genital MC that their condition is harmless and to offer an
appropriate plan of management.
Specifically:
This guideline highlights the key clinical features that should allow the diagnosis of
genital MC to be made with confidence and outlines the treatment options. Reference will
also be made to the interaction between MC and HIV infection.
It is aimed primarily at people aged 16 or older presenting to health care professionals
working in departments offering level 3 care in STI management in England and Wales,
tier 5 in Scotland (1,2). However the recommendations are appropriate in all health care
settings.
Stakeholder involvement
This guideline has been produced by medical specialists from relevant disciplines.
Successive drafts have been reviewed by the clinical effectiveness group of BASHH. It
was posted for comment for 3 months on the BASHH website.
Rigour of development
A Medline search was undertaken using search terms molluscum contagiosum, genital
and randomised controlled trial (RCT). The Cochrane database was also searched under
molluscum contagiosum. Trials restricted to children aged <16 years only were excluded.
One systemic review of treatment of MC in the Cochrane database was also excluded as
it did not consider the treatment of sexually transmitted MC. Two studies involving the
use of podophyllotoxin and imiquimod were considered. The study on imiquimod used a
1% cream whereas the 5% preparation is available in the UK.
What is new in the guideline
No new evidence
Minor rewording
Audit standardsadded
Final 15/02/08
Aetiology
Molluscum contagiosum is caused by a pox virus
The virus is probably passed on by direct skin-to-skin contact, and may affect any
part of the body
Sexual contact may lead to the appearance of lesions in the genital area
There is anecdotal evidence associating facial lesions with HIV-related
immunodeficiency (3-5)
Clinical features
Symptoms and signs
After an incubation period of three to twelve weeks, discrete, pearly,
papular, smooth or umbilicated lesions appear (6)
In immunocompetent individuals the size of the lesions seldom exceeds
five millimetres, and if untreated there is usually spontaneous regression
after several months
Complications
Secondary bacterial infection may result if lesions are scratched
In the immunocompromised eg in HIV infection, lesions may become
large and exuberant, and secondary infection may be problematic.
Diagnosis
This is usually based on characteristic clinical appearance
The main differential diagnosis is with genital warts, which are neither
smooth nor umbilicated
The core of lesions can be examined by electron microscopy, under which
typical poxvirus-like particles will be seen.
Management
General advice
As the natural history is of spontaneous regression of lesions, treatment is
offered for cosmetic reasons only
Further investigation
As other STIs may co-exist, a full screen for these should be undertaken
(level of evidence III, grade of recommendation B) (7)
Final 15/02/08
HIV testing is recommended in patients presenting with facial lesions
(level of evidence III, grade of recommendation B)
Treatment
The aim is tissue destruction with viral demise accompanying this. There are no
medicines licensed for the treatment of MC in the UK.
Recommended regimes
Cryotherapy apply liquid nitrogen until a halo of ice surrounds the
lesion. Repeat applications may be necessary (level of evidence 4, grade
of recommendation C)
Expression of the pearly core, either manually or using forceps (level of
evidence 4, grade of recommendation C)
Piercing with an orange stick , with or without the application of tincture
of iodine or phenol (level of evidence 4, grade of recommendation C)
Curettage or diathermy may be carried out under local anaesthesia (level
of evidence 4, grade of recommendation C)
Podophyllotoxin cream (0.5%) can be self-applied in men (level of
evidence 1b, grade of recommendation A). (8)
Imiquimod 5% cream can be self-applied in men (level of evidence 1b,
grade of recommendation A).(9)
In patients with HIV infection, the introduction of highly active
antiretroviral therapy may lead to resolution of lesions (level of evidence
III, grade of recommendation B) (10,11)
Allergy
Treatments to which there is known hypersensitivity should be
avoided
Pregnancy and breastfeeding
Cryotherapy and other purely destructive methods are safe
Podophyllotoxin is contraindicated. The British National
Formulary advises that Imiquimod should be used with caution
Sexual partners
Contact tracing of partners is unnecessary
Final 15/02/08
Auditable outcomes
Percentage of patients with MC offered STI screen : Target 100%
Conflict of interest
None
The recommendations in this guideline may not be appropriate for use in all clinical
situations. Decisions to follow these recommendations must be based on the professional
judgement of the clinician and consideration of individual patient circumstances.
All possible care has been undertaken to ensure the publication of the correct dosage of
medication and route of administration. However, it remains the responsibility of the
prescribing physician to ensure the accuracy and appropriateness of the medication they
prescribe.
This guideline was commissioned and edited by the CEG of the BASHH, without
external funding being sought or obtained
Author and centre
Gordon Scott, Lauriston Building, Edinburgh
Membership of the CEG
Dr Keith Radcliffe, Whittal Street Clinic, Birmingham (BASHH); Dr Imtyaz Ahmed-
J usuf, Nottingham City Hospital (BASHH); Dr David Daniels, West Middlesex Hospital
(Chair NAG); Dr Mark FitzGerald, Taunton and Somerset (BASHH); Dr Neil Lazaro
(RCGP); Dr Guy Rooney, Swindon and Oxford (RCP); Dr Gill McCarthy, Kingston
Hospital (BASHH)
References
1. The national strategy for sexual health and HIV; J uly 2001: www.doh.gov.uk
2. Scottish Executive 2005. Respect and Responsibility. Strategy and action plan for
improving sexual health. Edinburgh, Scottish Executive
3. Schwartz J J , Myskowski PL. Molluscum contagiosum in patients with human
immunodeficiency virus infection. J Am Acad Dermatol 1992;27:583-8
4. Goldstein B, Berman B, Dukenik E. Correlation of skin disorders with CD4
lymphocyte counts in patients with HIV/AIDS. J Am Acad Dermatol
1997;36:262-4.
Final 15/02/08
5. Kolokotronis A, Antoniades D, Katsoulidis E, Kioses V. Facial and perioral
molluscum contagiosum as a manifestation of HIV infection. Aust Dent J
2000;45:49-52
6. Gottlieb SL, Myskowski PL. Molluscum contagiosum. Int J Dermatol
1994;33:453-61
7. Radcliffe KW, Daniels D, Evans BA. Molluscum contagiosum: a neglected
sentinel infection. Int J STD AIDS 1999;2:416-8.
8. Syed TA, Lundin S, Ahmad M. Topical 0.3% and 0.5% podophyllotoxin cream
for self-treatment of molluscum contagiosum in males. A placebo-controlled,
double-blind study. Dermatology. 1994;189:65-8.
9. Syed TA, Goswami J , Ahmadpour OA, Ahmad SA. Treatment of molluscum
contagiosum in males with an analog of imiquimod 1% in cream: a placebo-
controlled, double-blind study. J Dermatol 1998;25:309-13
10. Hicks CB, Myers SA, Giner J . Resolution of intractable molluscum contagiosum
in a human immunodeficiency virus infected patient after institution of
antiretroviral therapy with ritonavir. Clin Inf Dis 1997;24:1023-5.
11. Calista D, Boschini A, Landi G. Resolution of disseminated molluscum
contagiosum with highly active antiretroviral therapy (HAART) in patients with
AIDS. Eur J Dermatol 1999;9:211-3.
S-ar putea să vă placă și
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Predominant Bacteria Detected From The Middle Ear Fluid of Children Experiencing Otitis Media: A Systematic ReviewDocument3 paginiPredominant Bacteria Detected From The Middle Ear Fluid of Children Experiencing Otitis Media: A Systematic ReviewbosÎncă nu există evaluări
- Systemic Infections From GiDocument10 paginiSystemic Infections From GiJake MillerÎncă nu există evaluări
- Complications of FracturesDocument29 paginiComplications of FracturesAlina Panciuc100% (1)
- Clinical Bacteriology Lecture (W01)Document3 paginiClinical Bacteriology Lecture (W01)nicholehernandez05Încă nu există evaluări
- Cytotoxic and Antimicrobial Activity of The Crude Extract of Abutilon IndicumDocument4 paginiCytotoxic and Antimicrobial Activity of The Crude Extract of Abutilon IndicumApurba Sarker ApuÎncă nu există evaluări
- 3rd Periodic Exam-Health Care ServiceDocument6 pagini3rd Periodic Exam-Health Care ServiceCrystal Ann Monsale Tadiamon100% (1)
- Publications SEA HLM 419Document101 paginiPublications SEA HLM 419Devendra NiranjanÎncă nu există evaluări
- The Physical and Sexual SelfDocument49 paginiThe Physical and Sexual SelfFuransuhito100% (1)
- Mls 044: Clinical Bacteriology Session 9: Antimicrobial Agents - Mechanisms of Action and ResistanceDocument5 paginiMls 044: Clinical Bacteriology Session 9: Antimicrobial Agents - Mechanisms of Action and ResistanceJJ AngÎncă nu există evaluări
- Unit 4Document86 paginiUnit 4vanitapanda14959Încă nu există evaluări
- Microbiology: Section IiDocument40 paginiMicrobiology: Section Iiparthibanb88100% (78)
- To Know The Importance of Food Microbiology in Commercial Kitchens: A Study of Cruise Lines and HotelsDocument17 paginiTo Know The Importance of Food Microbiology in Commercial Kitchens: A Study of Cruise Lines and HotelsAnonymous CwJeBCAXpÎncă nu există evaluări
- 3.skin PathologyDocument38 pagini3.skin PathologyFaisal MehboobÎncă nu există evaluări
- LevofloxacinDocument3 paginiLevofloxacinkezia_reyes67% (3)
- Adult Living Donor Liver Transplant: Questions and AnswersDocument36 paginiAdult Living Donor Liver Transplant: Questions and Answersjsus22Încă nu există evaluări
- GlossitisDocument7 paginiGlossitisLjubomirErdoglija100% (3)
- Krammer2018 PDFDocument21 paginiKrammer2018 PDFJulio Martinez RodriguezÎncă nu există evaluări
- Subject PredicateDocument69 paginiSubject PredicateyuldaÎncă nu există evaluări
- Classical Swine FeverDocument143 paginiClassical Swine FeverAgus SuwarnoÎncă nu există evaluări
- Reflection Paper About Covid-19Document1 paginăReflection Paper About Covid-19sei gosa100% (1)
- Sand Fly PDFDocument4 paginiSand Fly PDFSneha SahaÎncă nu există evaluări
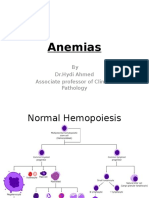
- Anemias (1) by DR - Hydi 3rd MBBS-2016Document63 paginiAnemias (1) by DR - Hydi 3rd MBBS-2016Suban GouseÎncă nu există evaluări
- Caroli Disease and CholangiocarcinomaDocument10 paginiCaroli Disease and CholangiocarcinomaDanielle Foster100% (1)
- HealthsafetyDocument32 paginiHealthsafetyapi-346614972Încă nu există evaluări
- Candidosis A New ChallengeDocument7 paginiCandidosis A New ChallengeSalvador contreras huertaÎncă nu există evaluări
- Health 3rd Quarter LessonDocument26 paginiHealth 3rd Quarter LessonJason LaroaÎncă nu există evaluări
- البلهارسيا PDFDocument5 paginiالبلهارسيا PDFbdalftahasamh20Încă nu există evaluări
- 1.endo PerioLesionPartIThePathogenesisDocument8 pagini1.endo PerioLesionPartIThePathogenesisMaulida SyafarinaÎncă nu există evaluări
- Immunization InstructionsDocument2 paginiImmunization InstructionsAli SadeqiÎncă nu există evaluări
- Economics Final Project PDFDocument13 paginiEconomics Final Project PDFMd Zahidul IslamÎncă nu există evaluări