Documente Academic
Documente Profesional
Documente Cultură
1 Imunitate Innascuta
Încărcat de
Gabriela SitaruTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
1 Imunitate Innascuta
Încărcat de
Gabriela SitaruDrepturi de autor:
Formate disponibile
1
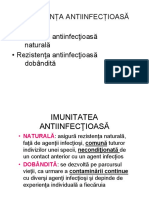
IMUNITATEA = APRARE
Toi ne mbolnvim uneori..., apoi ne
nsntoim
Ce se ntmpl n organism n timpul unei
infecii / afeciuni ?
De ce ne nsntoim ?
SISTEMUL IMUN
Colecie de CELULE i MOLECULE care
protejeaz organismul mpotriva infeciilor,
transformrilor maligne i celulelor proprii
transformate non-self
IMUNITATE
raspuns independent de antigen
receptori pt. patogeni:
codificati in genom
specificitate joasa
raspuns imediat
lipsa memorie
prezenta la toate organismele
pluricelulare
raspuns dependent de antigen
receptori pt. patogeni:
generati (rearanjare genica)
specificitate inalta
raspuns lent
memorie imunologica
(expansiune clonala Ly)
prezenta doar la vertebrate
SISTEM INTEGRAT
INNASCUTA / nespecifica
(innate immunity)
DOBINDITA / specifica
(adaptive immunity)
Rspunsuri imune
Skin & Mucous membranes
rapidly regenerating surfaces,
peristaltic movement, mucociliary
escalator, vomiting, flow of urine/tears,
coughing
Cellular and humoral defences
lysosyme, sebaceous/mucous secretions,
stomach acid, commensal
organisms,complement proteins,
phagocytosis, NK cells
Invasion
& infection
Barriers
Innate immunity
Adaptive immunity
+
+
Inflammation
Cellular and humoral defences
Antibodies, cytokines, T helper cells,
cytotoxic T cells
2
Innate immune response
Inbuilt immunity to resist infection
Native, natural immunity
Present from birth
Not specific for any particular microbial substance
Not enhanced by second exposure
Has no memory
Uses cellular and humoral components
Is poorly effective without adaptive immunity
Also involved in the triggering and amplification of
adaptive immune responses
Factori fizici / mecanici
1. Bariere anatomice
- piele
- mucoase
Functia de prevenire a intrarii
microorganismelor patogene
Factori chimici
Factori biologici
motilitate: muco-ciliara, peristaltica
mucus
fluxul fluidelor prin organism
pH
molecule antimicrobiene
limfocite T intraepiteliale ()
celule B-1
Imunitatea
innscut
2. Componente moleculare
- receptori
- molecule secretate
Imunitatea
innscut
Functia de recunoastere
Functii efectorii
Mol. anorganice: HCl, NO, H
2
O
2
Peptide antibacteriene: defensine, cathelicidine, histatine
Proteine antibacteriene: lizozim, lactoferina, transferina
Lectine: colectine, ficoline, receptori pentru Manoza
Complement
Citokine: IFN-/, IL-1, TNF-, CSF
Chemokine: IL-8, MIP, MCP
Receptori: TLR
3. Componente celulare
Functia de eliminare a
microorganismelor patogene
celule NK
Fagocitoza
Inflamatie
Citotoxicitate
neutrofile
monocite/macrofage
celule dendritice
bazofile
mastocite
eozinofile
Imunitatea
innscut
3
Functions within seconds of contacting a
pathogen
A mechanical, selectively permeable
barrier between the outside and inside:
Produce natural antibiotics - cationic
antibacterial peptides - defensins and
cathelicidins
May possess motile cilia
Rapidly renewable
Produce cytokines - proteins that alter
the behaviour of other cells
Produce chemokines - proteins that
attract other cells
May produce mucins
Transport antibodies from inside to
outside
First line of defence - Epithelial cells
Outside
Inside
Primary role is to block
the entry of
microorganisms
Immune responses
Skin & Mucous membranes
rapidly regenerating surfaces,
peristaltic movement, mucociliary
escalator, vomiting, flow of urine/tears,
coughing
Cellular and humoral defences
lysosyme, sebaceous/mucous secretions,
stomach acid, commensal
organisms,complement proteins,
phagocytosis, NK cells
Invasion
& infection
Barriers
Innate immunity
Adaptive immunity
+
+
Inflammation
Cellular and humoral defences
Antibodies, cytokines, T helper cells,
cytotoxic T cells
Epithelial cells activated upon
contact with microorganism
Chemokines and cytokines are made
by activated epithelial cells
General scheme of an immune response
Pathogen with non-self proteins
damages the epithelium to break
through the epithelial barrier
Cytokines and Chemokines
A diverse collection of soluble proteins and peptides that modulate the
behaviour of cells at nM to pM concentrations
Conceptually similar to hormones
However cytokines and chemokines are not exclusively produced
by organised cells located in glandular tissue
Act both locally and systemically
Have highly pleiotropic effects (show many biological activities)
Chemokines largely associated with chemoattraction of other cells
The activities of cytokines and chemokines often overlap with other
cytokines and chemokines
4
Post capillary endothelial
cells are impermeable to
cells and plasma
Inflammation
Cytokines - tumour necrosis factor (TNF)
and interleukin 1 (IL-1) change the morphology,
adhesive properties and permeability of
endothelial cells
Inflammation
Heat - Swelling - Redness - Pain - Loss of Function
Rspunsul inflamator celular (1)
- Neutrofilele si
monocitele circulante
au o mobilitate foarte
mare.
PMN si Mo au capacitatea sa
se strecoare prin spatiile
inguste interendoteliale,
recrutate chemotactic
(chemokine) la locul
infectiei
Daca infectia se
raspandeste, fagocite
noi din torentul
circulator sunt atrase
la locul infectiei
- Fagocitele ingurgiteaza
particulele straine
similar cu amoebele
Mechanism of Cell Migration
Tethering and rolling
Cells normally roll past resting endothelial cells
Cytokine activated endothelial cells express adhesion molecules
Tethering
Rolling
Tethering and rolling are mediated
by SELECTINS
Rolling
Neutrophil
is activated by
chemokines
Selectin is shed
Cytokines from epithelium activate expression of
Intracellular adhesion molecules (ICAMs)
INTEGRIN
(adhesion molecule)
has low affinity for
ICAM
Cell activation
changes integrin
to high affinity
format
Activation dependent adhesion & arrest
5
Leukocyte Adhesion
Phagocytic
neutrophils
respond to an
epithelial
chemokine IL-8
Cells migrate
from the blood
into the tissue
underlying the
infection
Migration and diapedesis
Firm adhesion causes the neutrophil
to flatten and migrate between the
endothelial cells
Neutrophil migrates towards site of
infection by detecting and following a
gradient of chemokine.
Neutrophils migrate readily to IL-8
made by epithelilal cells that have
encountered microorganisms
Diapedesis
Inflammation
Heat - Swelling - Redness - Pain - Loss of Function
6
Fagocite profesionale - PMN, MQ (1)
- Leucocite Polimorfonucleare (PMN)
Granulocite:
o Neutrofile, eozinofile, basofile, mastocite
Sunt fagocite cu via scurt, continnd lizozomi
Produc ap oxigenat i radicali superoxid
Proteine bactericide lactoferina
PMNs joac un rol major in protectia mpotriva infectiilor
Defecte genetice/dobndite infectii cronice sau recurente
- Macrofagele fagocite tisulare derivate din monocitele ciculante,
migreaza din sange in tesuturi se diferentiaza:
o celule Kupffer in ficat
o macrofage alveolare in plaman
o celule mezangiale in rinichi
o macrofage splenice (sinusale) in pulpa alba - Sistemul Reticuloendotelial
(SRE) / Reticulohistiocitar (SRH)
o macrofage peritoneale plutind liber in fluidul peritoneal (seroase)
o celule microgliale in SNC
o celule Langerhans in piele
Neutrophil
Neutrophil
Neutrophils
Also called polymorphonucelar
leukocytes
4 to 10 million per ml of blood
Infection activates cytokines that
stimulate the bone marrow to produce
up to 20 million neutrophils per ml of
blood.
Main role is to get to site of infection
rapidly and ingest microorganisms.
After taking up microorganisms the
neutrophil will die.
Neutrophil Chemotaxis
Neutrophils chasing yeast
Tissue macrophage
Blood monocyte
Monocytes
0.5 to 1 million monocytes per ml of
blood
Migrate into the tissues and
differentiate into Macrophages
Phagocytose microorganisms
Present antigens to T cells
The name of monocyte-derived cells
depends upon the tissue they reside in:
Liver - Kupffer cells
Lung - Alveolar macrophages
CNS - Microglial cells
Bone - Osteoclasts
Human Macrophage ingesting yeast
Fagocite (2)
- Initial, in spatiul interstitial trec
PMN:
se acumuleaza in 30-60 minute de la
aparitia agentului declansator
fagociteaza intrusul si tesuturile
lezate
elibereaza enzime lizozomale
- Daca inflamatia persista:
dupa 12-18 ore interstitiul este
infiltrat cu mononucleare
(macrofage si limfocite)
Macrofagele
o suplimenteaza activitatea PMN
o prezinta Ag, Ly T
- Daca inflamatia continua, raspunsul
inflamator este suplimentat si
accentuat cu elemente ale
imunitatii dobandite Ac si LyT
(Ac activeaza si sistemul
complementului) Vindecare
7
Fagocite (3)
- Celulele seriei macrofagice au doua functii majore:
Ingereaza si digera microorganisme si particule
straine
Prezinta Antigene (Ag) - componenta imunogena
o Preia Ag, il proceseaza si il prezinta Ly T
* Alte celule prezentatoare de Ag (APC) (precursori
hematopoietici, fagocite mai putin eficiente)
Celule dendritice in splina si ganglioni
Celule interdigitate in timus
Celule Langerhans in piele
Proces activ, initiat de
legarea fagocitului la
patogen prin
intermediul unor
receptori
Agentul patogen este
inconjurat de
pseudopode
membranare si apoi
internalizat:
- Fagozom
- Fagolizozom
- Vacuola digestiva
- Corp rezidual
Fagocitoza (cont)
- Proces activ, initiat de legarea la patogen prin intermediul unor
receptori
- Agentul patogen este inconjurat de pseudopode membranare si apoi
internalizat
Fagocitoza Fagocitoza
- Caracteristici
Definitie: preluarea unor particule de dimensiune mare (in
principal microorganisme), datorita capacitatii de a distinge
intre tipurile de carbohidrati produsi de mamifere si bacterii
(self - nonself)
o Pathogen-associated molecular patterns (PAMPs): LPS,
peptidoglicani, lipoarabinomanani, dsRNA - substante
prezente relativ constant (fara variabilitate antigenica) la
un grup mare de patogeni
Actin-dependenta, chlatrin-independenta
Rata & eficienta mare de internalizare
- Receptori fagocitari - pattern recognition receptors (PRRs) or
molecules (PRMs)
o Externi
FcR (CD16, CD64), CR3 (CD11b), Scavenger receptor
(CD36), Mannose receptor
o Interni
TLRs - Toll like receptors
8
Fagocitoza
(cont)
opsonin
dependenta, fiind
mediata de:
Ac sau
C3b
Fagocitoza
independent de oxigen dependent de oxigen
Mecanism
- defensine
- cathepsina B
- lizozim
- lactoferina
- enzime proteolitice
O
2
H
2
O
2
1
O
2
OCl
OH
Rol
eliminare a microorganismelor patogene
prelucrare Atg pt. prezentare
Mecanismele uciderii bacteriilor - cont.
-Explozia oxidativa
Activata in urma fagocitozei
Stimulata de PRRs
Consum crescut de O2
Produce substante care sunt toxice directe pentru
bacterii:
o Produsi derivati ai Oxigenului
o Produsi derivati ai Nitrogenului
NO (monoxidul de azot)
Produs de NO sintetaza inductibila (iNOS)
Enzima este indusa de cytokine, LT, TNF
Explozia oxidativa-speciile reactive ale O
2
Speciile reactive ale oxigenului se formeaza prin
Explozia oxidativa, care presupune:
Cresterea consumului de O
2
Glicogenoliza - cresterea oxidarii glucozei
Formarea anionului superoxid, apei oxigenate si a acidului
percloric:
o 2O
2
+ NADPH 2O
2
-
+ NADP
+
+ H
+
(NADPH oxidaza)
o O
2
-
+ 2H
+
H
2
O
2
HO
(SOD superoxid dismutaza) (Fe
2+
)
o H
2
O
2
+ Cl
2
2HOCl
(MPO mieloperoxidaza - granulele azurofile,
doar in PMN nu si in MQ)
Radicalii derivati de O
2
sunt detoxifiati de ceruloplasmina,
transferina, superoxid dismutaza (SOD), catalaza & glutation
peroxidaza (H
2
O
2
)
9
General scheme of an immune response
Both humans and pathogens are made of
proteins carbohydrates & lipids
Most microorganisms do not cause disease in humans
How does the human immune system distinguish
pathogens from human tissues and harmless
microorganisms?
Pathogens
Disease - causing organisms
Protozoa, Bacteria, Viruses, Fungi, Worms etc
Receptori (self vs. non-self microbian):
PRR Pattern Recognition Receptor
PAMP Pathogen Associated Molecular Pattern
(Medzhitov & J aneway, 1997)
Recunoastere imuna
Ipoteze
self
non-
self
origine antigen / context biologic
Pattern Recognition Receptors - PRR
Endocytic PRRs
glycosylphosphatidylinositol
(gpi)-linked receptor
Scavenger receptors (SR)
C-type lectin receptors
(CLR)
LPS
oxLDL; microbes
Microbes; microbial
moieties
Signaling PRRs
Toll-like receptors (TLR)
NOD-like receptors (NLR)
RIG1-like helicases (RLH)
Microbial moieties
Bacterial lipoproteins
Nucleic acids
Bridging molecules
Collectins
Ficolins
Pentraxins
Sugars
Glycoproteins
Microbes; microbial
moieties
(adaptat dupa Jeannin et al. Pattern recognition receptors in the immune response against
dying cells, Current Opinion in Immunology 2008, 20:18)
10
PAMP
invariabile
inalt conservate
specifice microbilor
(patogeni + non-patogeni)
comune pentru o clasa de microbi
vitale pentru microorganisme
lipopolizaharid
peptidoglican
acid lipoteichoic
lipoproteine
manoza
ADN
ARN dc
flagelina
pilina
zimozan
Gram-negative Gram-positive
a) ENDOCITOZA - Endocytic PRRs
proteina bact.
receptori manoza
(lectina C)
FAGOCIT
receptori scavenger
(CD36, CD68, SRB-1)
C3b
glicoproteina
bact.
receptori opsonine
(CR1)
Bacterie
LPS, LTA
man
Receptori fagocitari de suprafa - PRR:
leag ali compui bacterieni
-3. Scavenger Receptor - CD36
Recunoaste liganzi:
o polianionici (ds-RNA, LPS)
o carbohidrati
o Lp cu densitate mica (LDL) acetilate
Se gasesc pe toate fagocitele
Specific MQ, leaga peretele celulei bacteriene &
LPS
Fagociteaza celule apoptotice
o factor nou MFG-E8 (eliberat din MQ activate se
leaga la celulele apoptotice via fosfatidilserina)
b) TRANSMITERE SEMNAL - Signaling PRRs
TLR
Toll-like receptors
NOD
nucleotide-binding
oligomerization domain
RIG-1
retinoic acid-inducible gene-1
11
+ TLRs sunt proteine transmembranare
+ Toll - molecula identificata ca fiind esentiala pentru patern-ul
embrionic de Drosophila
+ Conservat pe parcursul evolutiei la insecte & oameni
+ TLRs la mamifere este omolog cu domeniul citoplasmatic al receptorului
IL-1 si IL-18 (Toll-IL1-R sau TIR domain)
+Domeniul extracelular este diferit
+ Au fost raportati 10 TLRs (1-10)
+Exprimati diferentiat pe celulele imune (nivel scazut)
+Expresia este modulata (inductibila) ca raspuns la anumiti
stimuli
+Exprimati si pe alte tipuri celulare (e.g., celule endoteliale)
Receptorii fagocitari interni
Toll-like (TLRs)
Toll-like receptors (TLR)
proteine transmembranare tip I
conservate filogenetic (Drosophila om)
domeniu extracelular bogat in leucina
domeniu intracelular TIR (similar IL-1R)
TLR mamifere (11-om, 13-soarece):
recunoastere PAMPs
asociere cu alti TLR sau alte proteine (MD2,CD14)
Lipoproteins, lipopeptides
Peptidoglycan
Zymosan
LPS Leptospira interrogans
LPS P.gingivalis
GPI (T.cruzi)
Lipoarabinomannan
Phosphatidylinositol dimannoside
(M. tuberculosis)
TLR2
+(TLR1/TLR6)
LPS
Taxol
HSP60
Fibronectin
F Protein (RSV)
Flagellin CpG DNA
TLR4 TLR5 TLR9
Danger hypothesis
Danger
signal
Naive
T cells
APC
Normal
cell
Damaged
cell
Signal 1
Signal 2 (co-
stimulation)
- infection
- tissue damage
- stress cells
- hypoxia
- temperature shifts
- hsp
Celula
NK
Celula
tinta
Celula
NK
Celula
tinta
Absenta
citotoxicitatii
Citotoxicitate
NKR
NCR Ligand
activator
MHC
cls I
NKR
NCR
Ligand
activator
Missing self
12
Functiile imunitatii innascute
PAMP
Stimulare PRR stimuleaza fagocitoza
induce activitate microbicida
induce citokine inflamatorii:
IL-1, IL-6, TNF- (NF-kB)
activeaza imunitatea dobindita
^ expresia molec. co-stim.
(MHC cls.II, CD80/CD86)
Citokine Macrofag activat
IL-1
- activeaza
endoteliul vascular
- activeaza Ly
- ^ acces cel. efect.
- activeaza
endoteliul vascular
- creste
permeab. vasculara
- ^ acces cel. efect.
- activeaza Ly
- ^ producere Atc.
- activeaza NK
- induce dif. Th1
TNF- IL-6
IL-12
EFECTE LOCALE
EFECTE SISTEMICE
- febra
- producere de IL-6
- febra
- mobilizare metaboliti
- soc
- febra
- inducere proteine
faza acuta
Mediatorii specifici
- Citokinele
Produsi celulari de natura proteica cu rol de mesaj pentru alte
celule, carora le spun cum sa se comporte
IL-1, TNF- si -, IFN- sunt importante in mod special in inflamatii.
Cresc expresia endoteliala a moleculelor de adeziune, activarea si
agregarea PMNs, etc.
- Interferonii
- Produsi de celulele infectate cu virusuri, actioneaza ca si mesageri de
scurta durata care protejeaza celulele invecinate de infectia virala.
interferon:
o Inhiba replicarea virala, creste numarul NK si induce antigenele MHC-I
interferon:
o Inhiba replicarea virala, creste numarul NK si induce antigenele MHC-I
interferon:
o Activeaza macrofagele si induce antigenele MHC-II
o Apararea imuna impotriva infectiilor si proliferarilor maligne.
Interferonii
Proprietati IFN- IFN- IFN-
NOMENCLATURA Type I,
Leukocyte
Type I,
Fibroblast
Type II, Immune
Inductori MAJORI Virus Virus, LPS Antigens,
mitogens, TNF-
+ IL-12
Nr de GENE 26 1 1
SURSA CELULARA T cells, B cells
Macrophages
Fibroblasts,
epithelial cells
T cells, natural
killer cells
Dupa expunere corespunzatoare cele mai multe celule sunt apte sa produca cel putin un tip de IFN I.
Tipul I de IFN poate fi indus de asemenea de LPS (endotoxina bacteriana), IL-1 si TNF.
Sinteza IFN- este inalt reglata numai in anumite tipuri de celule si este indusa de stimuli specifici
IFN- factorul major de activare macrofagica; rol crucial intre mecanismele de aparare ne-
specifica a gazdei impotriva a numerosi patogeni.
13
Functii efectorii: Rolul interferonului
IFN-/
Celula infectata viral Celula neinfectata
IFN receptor
2-5 (A)
Sintetaza
PKR
Inhibare sinteza proteica
degradare mRNA
+ translatie mRNA
Pathogens Epithelial barrier Activated epithelial cells
Epithelial cytokines Permeabilised endothelium Cell & fluid migration
Opsonisation
Phagocytosis
Interaction with
other cells of the
innate and adaptive
immune systems
Barriers -
Seconds
Epithelial activation -
Minutes Cytokines/chemokines -
Minutes to days
Neutrophils -
Hours
Monocytes/macrophages -
Hours to days NK cells -
Hours to days
Timing of innate immunity after infection
Short-
lived
Long-lived & connect with
adaptive immune system
Complement -
Minutes
Other Cells Involved in Innate Immunity
Macrophage
Monocyte
Neutrophil
PMN
Eosinophil
Basophil
Mast cell
Phagocytosis
Presentation to
lymphocytes
Phagocytic
Anti-bacterial
Anti-parasite
Immunity - Allergy
?Protection of
mucosal surfaces? - Allergy
Protection of
mucosal surfaces - Allergy
14
Eosinophil Basophil
Neutrophil
Monocyte
Lymphocyt
e
Neutrophil
Basophil
Eosinophil
Eosinophil
Eosinophils attacking a schistosome larva in the presence of serum (IgE)
from an infected patient.
Degranulated mast cell
Resting Mast cell
Mast Cells
Mediators released include:
Leukotriene C
4
& D
4
, Prostaglandin D
2
Platelet Activating Factor,
Chymase, Tryptase, Heparin, Histamine IL-4, IL-5, IL-6, IL-8, TNF-
Causing:
Vasodilation, increased vasopermeability, contraction of smooth muscle,
bronchoconstriction, increase neutrophil chemotaxis, increase eosinophil,
neutrophil and monocyte chemotaxis, anticoagulation, increased
fibroblast proliferation & platelet activation
Cells Of The
Immune System
Pluripotent
haemopoietic
stem cell
Common
lymphoid
progenitor
Myeloid
progenitor
Lymphocyte Adaptive
immunity
Macrophage
Monocyte
Neutrophil
PMN
Eosinophil
Basophil
Mast cell
Phagocytosis
Ag presentation
Phagocytic
Anti-bacterial
Anti-parasite
Immunity - Allergy
?Protection of
mucosal surfaces?
- Allergy
Protection of
mucosal surfaces
- Allergy
15
Non-T, non-B cells
No classical antigen receptors
Part of the innate immune system
Recognise and kill abnormal cells such
as tumour cells
Directly induce apoptosis in virus
infected cells by pumping proteases
through pores that they make in
target cells
Similar cytolytic mechanisms to
cytotoxic T lymphocytes (CTL)
Involved in antibody-dependent
cellular cytotoxicity (ADCC)
Natural Killer (NK) cells
Interferon
(IFN) receptor
Activated macrophage
Growth factors, angiogenic
factors, proteinases -
REPAIR & REMODELLING
NK
Cytokines TNF, IL-12
IFN
Interactions between phagocytes and other innate
immune components: Natural Killer cells
Sistemul proteinelor plasmatice -
raspunsul imun nespecific umoral
Secreted Pattern Recognition
Molecules (sPRM)
Proteine de faza acuta
Produse mai ales de ficat, dar si de fagocite, cu rol in:
Activarea Complementului
Opsonizarea celulelor microbiene
16
Cascada coagularii
- Nonspecific defense system
The combination of antibodies with antigens does not cause destruction of
the antigens or pathogen.
- Antibodies serve to identify the targets for immunological attack. Antibody-
induced activation of the complement.
- The complement proteins are designated C-1 to C-9.
These proteins are in an inactive state. Become activated by the
attachment of antibodies to antigens.
- Complement proteins can be subdivided into 3 components:
C1q, r, s: recognization.
C4, C2, C3: activation.
C5-C9: attack (complement fixation).
- Activated via classic (C1) or alternative (C3) pathways to generate MAC (C5
C9) that punch holes in microbe membranes
- In acute inflammation
o Vasodilation, vascular permeability, mast cell degranulation (C3a, C5a)
o Leukocyte chemotaxin, increases integrin avidity (C5a)
o As an opsonin, increases phagocytosis (C3b, C3bi)
Complement System
17
b
C4b
+
C2b
C3b
+
Bb
Activation of C System - cont.
Imunitatea Innscut - faze
Inflamaia
- Component major a rspunsului imun nespecific/
specific
- Rspuns protectiv la injurie, montat s restabileasc
statusul normal
- Iniiat de lezarea esuturilor:
mecanic/fizic (ex. arsuri)
chimic ( ex. expunere la ageni corozivi)
biologic (ex. microorganisme)
imunologic (ex. hipersenzitivitate)
- Implic fagocite i mediatorii secretai de fagocite,
precum i excretai de celulele secretorii
Inflamatia - Functii
- Distrugerea si indeprtarea substantelor
/ particulelor duntoare / strine
- Izolarea zonei infectate/inflamate
- Stimularea rspunsului imun specific
- Vindecare
18
Caracteristicile Inflamaiei
- Edemaierea zonei (tumor)
- Eritem (rubor)
- Creterea temperaturii
(calor)
- Durere (dolor)
- Pierderea funcionalitii
(functio lesa)
- Reacii / interferene
inflamatorii locale:
Activarea coagulrii
Cile formatoare ale
Kininelor
Fibrinoliza
Eliberarea de histamin i prostaglandine determin
vasodilataie local nsoit de:
o increased blood flow redness and warmth
o increased capillary permeability
o edema (swelling) due to fluids seeping from
capillaries
o more WBCs to site
o phagocytes move out of vessels into
extracellular fluid (ECF)
o phagocytes engulf and destroy bacteria
Rspunsul inflamator local
Inflamatia locala
- In tesutul interstitial
exista o populatie
rezidenta de
leucocite.
- Mastocitul:
elibereaza amine
biogene (histamina,
serotonina)
secreta
prostaglandine,
leukotriene, citokine
si TNF-a.
- PMN:
fagociteaza
agresorul
Rspunsul inflamator sistemic (1)
- Induction of fever
Caused by many bacterial products (endotoxins
from G(-) bacteria)
Endogenous pyrogens from monocytes and
macrophages (IL-1 and certain interferons)
- Increased WBC production / releasing
- Increased synthesis of hydrocortisone and
adrenocorticotropic hormone (ACTH)
- Production of acute phase proteins C-reactive
protein binds to membranes of certain
microorganisms to activate the complement
system
19
Rspunsul inflamator sistemic (2)
POSITIVE
- indicate a reaction to
infection
- stimulate phagocytosis
- slow bacterial growth
increases body temperature
beyond the tolerance of some
bacteria
decreases blood iron levels
NEGATIVE
- extreme heat enzyme
denaturation and interruption
of normal biochemical
reactions
> 39 C (103F) is dangerous
> 41C (105F) could be fatal and
requires medical attention
Febra are efecte pozitive i negative asupra infeciei i
funciei organismului
Rspunsul inflamator sistemic (3)
Nu este doar un sistem de aparare simplu,
menit sa tina in loc infectia pina la
interventia imunitatii dobindite
Instruieste sistemul imunitatii dobindite
pentru a raspunde la infectii
Decizia majora de a raspunde
sau nu unui antigen este luata de
imunitatea innascuta, prin
receptorii codificati in genom !
Imunitate innascuta
Immune responses
Skin & Mucous membranes
rapidly regenerating surfaces,
peristaltic movement, mucociliary
escalator, vomiting, flow of urine/tears,
coughing
Cellular and humoral defences
lysosyme, sebaceous/mucous secretions,
stomach acid, commensal
organisms,complement proteins,
phagocytosis, NK cells
Invasion
& infection
Barriers
Innate immunity
Adaptive immunity
+
+
Inflammation
Cellular and humoral defences
Antibodies, cytokines, T helper cells,
cytotoxic T cells
20
ROL i FUNCTII
Recunoastere
Functii efectoare
prevenire intrare
eliminare
Rol instructiv asupra imunitatii specifice
microorganisme
patogene
initierea si tipul raspunsului
originea si contextul
Ag
Imunitatea
innscut
PAMP
TLR
pathogen
Endocytic
PRR
Naive
T cells
CD80/86
Th1
IFN-
CD28
MHC-II
TCR
IL-12
DC
(adapted after Medzhitov R,
Nature Reviews Immunology, 1,
2001, 135-145)
Th1
IFN-
INNATE
IMMUNITY
ADAPTIVE IMMUNITY
cellular immune response
S-ar putea să vă placă și
- Superintestinul: Un plan de patru săptămâni pentru reprogramarea microbiomului, refacerea sănătății și pierderea în greutateDe la EverandSuperintestinul: Un plan de patru săptămâni pentru reprogramarea microbiomului, refacerea sănătății și pierderea în greutateÎncă nu există evaluări
- Imuno MergedDocument347 paginiImuno MergedGigiEnergieÎncă nu există evaluări
- Întărirea sistemului imunitar în funcție de grupa sanguină.: O metodă inedită de a vă proteja de virusuriDe la EverandÎntărirea sistemului imunitar în funcție de grupa sanguină.: O metodă inedită de a vă proteja de virusuriEvaluare: 5 din 5 stele5/5 (2)
- Curs 3Document49 paginiCurs 3Ioana CucosÎncă nu există evaluări
- Dieta pentru zile senine II: De la durere la echilibru spiritual, psihologic, nutritivDe la EverandDieta pentru zile senine II: De la durere la echilibru spiritual, psihologic, nutritivEvaluare: 5 din 5 stele5/5 (1)
- Imunologie LPDocument9 paginiImunologie LPLUÎncă nu există evaluări
- Curs 4 - Rezistenta Antiinfectioasa NaturalaDocument30 paginiCurs 4 - Rezistenta Antiinfectioasa NaturalaSorina SmarandoiuÎncă nu există evaluări
- ImunologieDocument263 paginiImunologieIlinca RizeaÎncă nu există evaluări
- Introducere in ImunologieDocument20 paginiIntroducere in ImunologieAndrea Dea100% (1)
- Curs 3 Apărarea Celulară. Reacţia Inflamatorie.Document90 paginiCurs 3 Apărarea Celulară. Reacţia Inflamatorie.Football Fan JFT96Încă nu există evaluări
- LeucociteDocument33 paginiLeucociteGeorge PetreaÎncă nu există evaluări
- Curs 2 Concepte Referitoare La Apararea AntiinfectioasaDocument51 paginiCurs 2 Concepte Referitoare La Apararea AntiinfectioasatimcarasÎncă nu există evaluări
- Imunologie Si AlergologieDocument19 paginiImunologie Si AlergologieamgdanielaÎncă nu există evaluări
- 3.fiziologia LeucocitelorDocument28 pagini3.fiziologia LeucocitelorSchuster Stephan100% (2)
- InflamatiaDocument44 paginiInflamatiaAndra-Elena SpiridonÎncă nu există evaluări
- Curs 1 - Org Sist ImunDocument44 paginiCurs 1 - Org Sist ImunDaniel Ciprian50% (2)
- Cursul 1. InflamatiaDocument44 paginiCursul 1. InflamatiaSulea RaduÎncă nu există evaluări
- Curs LeucociteDocument5 paginiCurs LeucociteAdrian ABÎncă nu există evaluări
- Imunitatea InnascutaDocument5 paginiImunitatea InnascutaMaria CloșcăÎncă nu există evaluări
- Curs 3 Medicamente BiologiceDocument38 paginiCurs 3 Medicamente BiologiceDeaconu ElenaÎncă nu există evaluări
- c2 - Modalitati de Aparare A OrganismuluiDocument8 paginic2 - Modalitati de Aparare A OrganismuluialiceinwinterÎncă nu există evaluări
- ImunologieDocument10 paginiImunologiexsmileÎncă nu există evaluări
- Imunitatea. Sistemul Imun. Imunitatea Înnăscută A MacroorganismuluiDocument83 paginiImunitatea. Sistemul Imun. Imunitatea Înnăscută A MacroorganismuluiDiana ColtunÎncă nu există evaluări
- Curs 2Document54 paginiCurs 2Bianca Gabriela ZanfirÎncă nu există evaluări
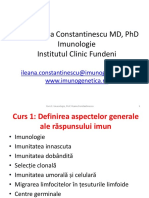
- Curs 1 - Imunologie - MD - RomDocument31 paginiCurs 1 - Imunologie - MD - RomSendre CarmenÎncă nu există evaluări
- FizioDocument17 paginiFizioStom StomÎncă nu există evaluări
- V4. Imunitatea Şi Alergiile. Bolile InfectioaseDocument68 paginiV4. Imunitatea Şi Alergiile. Bolile InfectioaseMarin Gh Ciobanu100% (3)
- Cursul 10 Fiziologia LeucocitelorDocument63 paginiCursul 10 Fiziologia LeucocitelorMocanu BiancaÎncă nu există evaluări
- Curs 2 - Organele Sistemului ImunDocument39 paginiCurs 2 - Organele Sistemului ImunTeodora PapucÎncă nu există evaluări
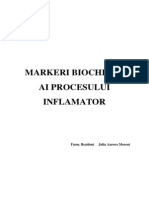
- Aspecte Biochimice Ale Procesului InflamatorDocument17 paginiAspecte Biochimice Ale Procesului InflamatorJulia HangaÎncă nu există evaluări
- Organe LimfoideDocument45 paginiOrgane LimfoideYoana PanteaÎncă nu există evaluări
- Curs 2-3 Leucocite Si Hemostaza NDocument57 paginiCurs 2-3 Leucocite Si Hemostaza NAnaMariaBobesÎncă nu există evaluări
- Curs 4 - Sange (2) - Fim 2022Document30 paginiCurs 4 - Sange (2) - Fim 2022Alexia TanaseÎncă nu există evaluări
- Imunopat Curs 3Document14 paginiImunopat Curs 3Ioana VoinescuÎncă nu există evaluări
- INFLAMATIADocument12 paginiINFLAMATIAAndreea BurlacuÎncă nu există evaluări
- Imuno CursDocument89 paginiImuno Cursioana_cretuuÎncă nu există evaluări
- Curs NR 2Document40 paginiCurs NR 2Tiberiu BalanÎncă nu există evaluări
- Inflamatii Curs PDFDocument200 paginiInflamatii Curs PDFAnonymous sOlmzOsG6FÎncă nu există evaluări
- Apararea AntiinfectioasaDocument62 paginiApararea AntiinfectioasaLuana-Maria GherasieÎncă nu există evaluări
- Curs 2 - 2022Document42 paginiCurs 2 - 2022Larisa CatanescuÎncă nu există evaluări
- InflamatiiDocument43 paginiInflamatiiW205 SamÎncă nu există evaluări
- Imunologie. Curs1-15Document369 paginiImunologie. Curs1-15Marta DumitracheÎncă nu există evaluări
- FIZIOLOGIE Sangele2Document63 paginiFIZIOLOGIE Sangele2Mihaela VadanaÎncă nu există evaluări
- Prelegere Nr.67. InflamatiaDocument126 paginiPrelegere Nr.67. InflamatiaElena CataragaÎncă nu există evaluări
- Curs Imunitatea InnascutaDocument30 paginiCurs Imunitatea InnascutaAndreea MireaÎncă nu există evaluări
- Prelegere InflamatiaDocument128 paginiPrelegere InflamatiaCorinaÎncă nu există evaluări
- Curs 9 PDFDocument49 paginiCurs 9 PDFAlex MirceaÎncă nu există evaluări
- Rezistenta NaturalaDocument32 paginiRezistenta NaturalaAnamaria Facalet100% (2)
- 03.raspuns Imun La Nivelul Aparatului Respirator...Document4 pagini03.raspuns Imun La Nivelul Aparatului Respirator...Lily OzunuÎncă nu există evaluări
- Leucocite Si TrombociteDocument113 paginiLeucocite Si TrombociteDana Chitoi100% (1)
- Inflamatia MorfopatologieDocument84 paginiInflamatia MorfopatologieRusu NicolaeÎncă nu există evaluări
- InflamatiaDocument104 paginiInflamatiaTudor OstopoviciÎncă nu există evaluări
- Inflamatia (Anatomie Patologica)Document44 paginiInflamatia (Anatomie Patologica)Justin Wooten100% (1)
- Curs Fiziologie MD IDocument89 paginiCurs Fiziologie MD IChristina HurstÎncă nu există evaluări
- ImunologieDocument40 paginiImunologieVasilescu Anca Daniela100% (1)
- Cursuri InflamatiiDocument131 paginiCursuri InflamatiiOana Andreea Ursică100% (1)
- Cursul 4 IMUNO CEPA ModificatDocument33 paginiCursul 4 IMUNO CEPA Modificatbianca111519Încă nu există evaluări
- Celulele Sistemului Imun. Citokine - AlbDocument73 paginiCelulele Sistemului Imun. Citokine - AlbLaura DianaÎncă nu există evaluări
- Img 0063Document1 paginăImg 0063Gabriela SitaruÎncă nu există evaluări
- Img 0032Document1 paginăImg 0032Gabriela SitaruÎncă nu există evaluări
- Img 0066Document1 paginăImg 0066Gabriela SitaruÎncă nu există evaluări
- Img 0060Document1 paginăImg 0060Gabriela SitaruÎncă nu există evaluări
- Img 0028Document1 paginăImg 0028Gabriela SitaruÎncă nu există evaluări
- Img 0050Document1 paginăImg 0050Gabriela SitaruÎncă nu există evaluări
- Img 0052Document1 paginăImg 0052Gabriela SitaruÎncă nu există evaluări
- Img 0053Document1 paginăImg 0053Gabriela SitaruÎncă nu există evaluări
- Img 0051Document1 paginăImg 0051Gabriela SitaruÎncă nu există evaluări
- Img 0037Document1 paginăImg 0037Gabriela SitaruÎncă nu există evaluări
- Img 0049Document1 paginăImg 0049Gabriela SitaruÎncă nu există evaluări
- Img 0011Document1 paginăImg 0011Gabriela SitaruÎncă nu există evaluări
- Img 0026Document1 paginăImg 0026Gabriela SitaruÎncă nu există evaluări
- Img 0021Document1 paginăImg 0021Gabriela SitaruÎncă nu există evaluări
- Img 0020Document1 paginăImg 0020Gabriela SitaruÎncă nu există evaluări
- Img 0017Document1 paginăImg 0017Gabriela SitaruÎncă nu există evaluări
- Img 0006Document1 paginăImg 0006Gabriela SitaruÎncă nu există evaluări
- Img 0012Document1 paginăImg 0012Gabriela SitaruÎncă nu există evaluări
- Img 0002Document1 paginăImg 0002Gabriela SitaruÎncă nu există evaluări