Documente Academic
Documente Profesional
Documente Cultură
Alara PDF
Încărcat de
Wafa ApriliaDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Alara PDF
Încărcat de
Wafa ApriliaDrepturi de autor:
Formate disponibile
Recognizing New Procedures for
Patient Protection
The concept of
ALARA
As Low As Reasonably Achievable
November 2004
FDA accepted updated guidelines for
dental radiography to achieve ALARA as
presented by ADA representing many
dental professional organizations.
What does it mean?
Very simply stated, treat each patient as an
individual
Selection criteria-Dentist must examine their
patients before ordering radiographs
Try to stay as far below dose limits as possible
Be consistent with the purpose for which the
activity is undertaken
Use procedures that require the least amount of
radiation exposure possible to produce the
greatest amount of data
Determine risk factors prior to exposing.
Protective Devices
Lead apron-not required if all other
guidelines in 2004 report are followed
rigorously
Thyroid Collars-provide for all children and
for adults when it wont interfere with
examination
Protective Devices
Cephalometric imaging-filters for imaging
the soft tissues of the facial profile
together with the skeleton should be
placed at the x-ray source rather than at
the image receptor, the x-ray beam should
be collimated to the area of clinical interest
Image receptor (film speed)-use no speed
slower than E speed
Collimation-
Rectangular
collimation should be
used for periapical
radiography and
when feasible for
bitewing radiography
Another note on collimation.
Round cones can be adapted rather than
replaced
Risk in relation to age
based upon a relative risk of 1 at age 30
Age Group (years) Multiplication factor for risk
<10 x 3
10-20 x 2
20-30 x 1.5
30-50 x 0.5
50-80 x 0.3
80+ Negligible risk
It assumes the multiplicative risk projection model, averaged for the two sexes. In fact,
risk for females is always relatively higher than for males.
Radiation Effects to Gonads
Embryo/Fetus Radiation Effects
Radiation Effects to Thyroid
Radiation Bone Marrow Effects
Radiation Bone Marrow Effects
Risk to marrow is induction of leukemia
< 1% bodys total marrow exposed to dental x-rays
(mandibular marrow spaces)
FMXR with round collimation is 0.142 mSv
FMXR with rectangular collimation is 0.06mSv.
Total Mean Active Bone Marrow Dosage 0.01 mSv for
Pano
The mean active bone marrow dose from one chest film is
0.03 mSv
Threshold leukemia induction estimated whole-body
exposure of 50 mSv
Radiation Effects to Thyroid
100 mSv reported for thyroid carcinoma
induction
FMXR thyroid exposure < 0.3 mSv
Panoramic thyroid dose 0.04 mSv
Effects may be more significant in
children because of more active
metabolic rates
50% reduction in exposure by using
thyroid collar on apron
Radiation Effects to Gonads
Gonadal dental x-ray exposure result of
secondary (scatter) radiation
Gonadal scatter exposure from FMXR is
approximately 0.002 mSv
DOSE IS REDUCED 98% BY LEADED
APRON!!
FMXR gonadal exposure with leaded apron
is 10 times less than average background
daily exposure!
Embryo/Fetus Radiation
Effects
Pregnant patients should have radiographs
taken if needed for diagnosis
Congenital defects negligible from gonadal
exposures < 200 mSv (Hiroshima survivor study)
Single x-ray exposure < 0.001 mSv with leaded
apron
Probability of 1
st
generation defect from
dental x-rays is 9 in one billion
Time
Distance
Shielding
Dose Equivalents for Dental Films
Full-mouth series
D Speed Film .084 mSv
F Speed Film <.033 mSv
BWXR (4 films)
D Speed Film .017 mSv
F Speed Film <.007 mSv
Panoramic radiograph .007 mSv
Average natural background radiation
3 mSv / yr (.01 mSv / day)
Compared to Other X-ray Exams
Chest x-ray 0.01 0.05 mSv
Skull x-ray 0.1 0.2 mSv
Abdomen x-ray 0.6 1.7 mSv
Barium exam 3 8 mSv
Head CT 2 4 mSv
Body CT 5 15 mSv
Estimates of Life Expectancy Loss
Health Risk Time Lost
Smoking 20 cigs/day 6 years
Overweight (15%) 2 years
Alcohol (US Average) 1 year
All accidents 207 days
All natural hazards 7 days
Rad dose of 3 mSv/yr 15 days
Cohen, Health Physics, 1991
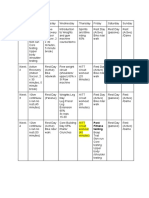
New Patients
Child with primary dentition
BW only if interproximal spaces cannot be viewed or
probed
Child with transitional dentition
Add periapicals or panoramic to evaluate
development
Adolescents
Because of increase in possibility of periodontal
disease panoramic is recommended
Adult
Posterior bitewings, and selected periapicals
or panoramic, a full-mouth series is preferred
when the patient has evidence of disease or
history of extensive treatment
Adult edentulous
Individualized exam based on clinical signs
and symptoms
Recall Patients
Recall patients with increased risk
for caries
Child or adolescent
Every 6-12 months
Adult dentate or partially edentulous
Caries risk assessment should determine
frequency
Every 6-18 months
Adult edentulous
Radiographs should not be performed without
evidence of pathology
Recall patients with no increased
risk for caries
Children with primary or transitional
dentition
BW every 12-24 months
If proximal surfaces cannot be examined
visually or with a probe
Adolescents
BW every 18-36 months
Adult
BW every 24-36 months
Recall patient with periodontal
disease
Clinical judgment as to the need for and
type of radiographic images for the
evaluation of periodontal disease.
May include BW and or periapical images
of selected areas where periodontal
disease can be identified clinically.
Clinical situations for which
radiographs may be indicated
1. Positive clinical findings
Previous treatment
History of pain or trauma
Familial history of dental anomalies
Etc.
2. Positive clinical signs and symptoms
Clinical evidence of periodontal disease
Large or deep restorations
Deep carious lesions
Malposed or impacted teeth
Swelling
Etc
Factors increasing risk for caries
may include
High level of caries experience or
demineralization
History of recurrent caries
High number of cariogenic bacteria
Poor quality of existing restorations
And the list goes on.
Improving Patient Care with
ALARA
Patient A
22 year old female
Recall patient-every 6 months
Negative medical history
Lives in a community with fluoridated
water
Has had no previous dental restorations in
permanent teeth
When should BW radiographs
be made?
A. Every 6 months
B. Every year
C. Every 2 years
D. None of the above
Answer
C. Every two years
Sources
Perry, D.A., Beemsterboer, P.L., & Taggart, E.J.(2001).
Periodontology for the dental hygienist. Philadelphia, PA:
W.B. Saunders Company.
Iannucci-Haring, J. & Jansen, L. (2000). Dental
radiography: Principles and techniques. Philadelphia,
PA: W.B. Saunders Company.
DiGangi, P. (2006) ALARA: What does it mean?
Contemporary Oral Hygiene, March 2006, 22-28.
Thompson, E.M. (2006) Radiation safety update.
Contemporary Oral Hygiene, March 2006, 10-17.
Sources
FDA website
http://www.fda.gov/cdrh/radhlth/adaxray-1.html
Radiation Health in Dentistry
Procter & Gamble Website for
Professionals
Continuing Education Section
www.dentalcare.com
Thanks for your attention!
S-ar putea să vă placă și
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Physical Education Cambridge Progression Test P1 - ST3 (2022)Document12 paginiPhysical Education Cambridge Progression Test P1 - ST3 (2022)Givemore MuromboÎncă nu există evaluări
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- MyonecrosisDocument5 paginiMyonecrosisJennifer ArangoÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5795)
- Rex ResearchDocument43 paginiRex ResearchGrigoriadis GeorgiosÎncă nu există evaluări
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- A Case of Aspartate Aminotransferase MacroenzymeDocument3 paginiA Case of Aspartate Aminotransferase MacroenzymeOlfiany Laurenzia PongohÎncă nu există evaluări
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Beck - Depresyon.olcegi - Ref .Mak .FtronlineDocument24 paginiBeck - Depresyon.olcegi - Ref .Mak .FtronlinekinetiklurÎncă nu există evaluări
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- Hysterectomy ReportDocument18 paginiHysterectomy ReportMa. Louise Lovely RosalesÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- SLR Fitness ProgramDocument5 paginiSLR Fitness ProgramKevin ZuddÎncă nu există evaluări
- ACLSDocument275 paginiACLSShajahan SideequeÎncă nu există evaluări
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Hematology Reference RangesDocument9 paginiHematology Reference Rangesdrafq2000Încă nu există evaluări
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- ThyrotoxicosisDocument16 paginiThyrotoxicosisFiorella Peña MoraÎncă nu există evaluări
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- State of The Art IPDocument13 paginiState of The Art IPSam SamiÎncă nu există evaluări
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- Small For Gestational AgeDocument14 paginiSmall For Gestational AgeMaria Delia Salvado100% (2)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Stress Management Objectives Stree Illness and Adaptaion OriginalDocument49 paginiStress Management Objectives Stree Illness and Adaptaion OriginalKhizar AliÎncă nu există evaluări
- Jinoob KCDocument6 paginiJinoob KCAshok NarayananÎncă nu există evaluări
- Asthma Control Test 4 To 11 YearsDocument2 paginiAsthma Control Test 4 To 11 YearsIsiakpona AdaÎncă nu există evaluări
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- How To Get Electives at AKU (Experience)Document15 paginiHow To Get Electives at AKU (Experience)FarazÎncă nu există evaluări
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Camh Suicide Prevention HandbookDocument96 paginiCamh Suicide Prevention Handbook873810skah100% (3)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- FLG 212 Study GuideDocument19 paginiFLG 212 Study GuidecynthiaÎncă nu există evaluări
- Biochemistry-Module 10 (Electrolytes)Document11 paginiBiochemistry-Module 10 (Electrolytes)Rommel BaraquielÎncă nu există evaluări
- Hyperbaric Oxygen Therapy: ReferenceDocument5 paginiHyperbaric Oxygen Therapy: ReferenceFariz NurÎncă nu există evaluări
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- Home Health Documentation Example 2021Document15 paginiHome Health Documentation Example 2021Deidra Adam100% (1)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1091)
- Hemodynamic Disorders Thromboembolic Disease and ShockDocument13 paginiHemodynamic Disorders Thromboembolic Disease and ShockAbu HuraraÎncă nu există evaluări
- Diagnosis and TreatmentDocument6 paginiDiagnosis and TreatmentVadim BulbakÎncă nu există evaluări
- 11 Anti-Coagulants & FibrinolyticsDocument52 pagini11 Anti-Coagulants & FibrinolyticsUmmuShefaÎncă nu există evaluări
- Reading A Head CT, What Every EP Should Know PDFDocument62 paginiReading A Head CT, What Every EP Should Know PDFAdistya Sari100% (1)
- ElectrotherapyDocument2 paginiElectrotherapyroxer07Încă nu există evaluări
- 10.blood Vessels & HeartDocument4 pagini10.blood Vessels & Heartharips motupalliÎncă nu există evaluări
- Objective Type Question (Fill in The Blanks)Document12 paginiObjective Type Question (Fill in The Blanks)Dr. Jayesh Patidar67% (3)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Assisting in Intravenous Infusion NewDocument52 paginiAssisting in Intravenous Infusion NewDianne LabisÎncă nu există evaluări
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)