Documente Academic
Documente Profesional
Documente Cultură
Peeters
Încărcat de
lovehope0 evaluări0% au considerat acest document util (0 voturi)
25 vizualizări5 paginipaper
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentpaper
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
25 vizualizări5 paginiPeeters
Încărcat de
lovehopepaper
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 5
349
Address for correspondence:
Marc Hendrikx, MD, PhD, Dept. of Cardiothoracic Surgery,
Jessa Hospital, Campus Virga Jesse, Stadsomvaart 11,
B-3500 Hasselt, Belgium.
E-mail: marc.hendrikx@jessazh.be
Received 21 November 2012; revision accepted for publication
25 June 2013.
INTRODUCTION
The prevalence of thoracic aortic aneurysms has
increased over the last 30 years. Actually, the incidence
Elective reconstruction of the ascending aorta for aneurysmal
disease restores normal life expectancy.
An analysis of risk factors for early and late mortality
Dries VAN DUFFEL
1*
, BSc; Ruben VAN GEMERT
1*
, BSc; Pascal STARINIERI
2
MSc; Jean-Louis PAUWELS
2
, MSc;
Agnes NATUKUNDA
3
, BSc; Trias Wahyuni RAKHMAWATI
3
, BSc; Maxwell Tawanda CHIREHWA
3
, BSc;
James ORWA
3
, BSc; Herbert THYS
3
, PhD; Patrick DEBOOSERE
4
, PhD; Boris ROBIC
1,2
, MD; Urbain MEES
2
, MD;
Marc HENDRIKX
1,2
, MD, PhD
1
Faculty of Medicine and Life Sciences, Hasselt University, Hasselt, Belgium;
2
Dept. of Cardiothoracic Surgery, Jessa Hospital, Hasselt,
Belgium;
3
CENSTAT, Hasselt University, Hasselt, Belgium;
4
Faculty of Sociology, Vrije Universiteit Brussels, Brussels, Belgium.
*Tese authors contributed equally to the paper
Objective We investigated the survival of patients who had undergone elective reconstruction of the ascending aorta for degenerative aneurysms.
The long-term survival was compared to an age- and sex-matched case-control population. An analysis of risk factors, inuencing survival was made.
Methods and results From May 1998 to January 2012, 72 patients underwent elective reconstruction of the ascending aorta for degen-
erative disease at the department of Cardiothoracic Surgery of the Jessa Hospital, Hasselt, Belgium. Sixty patients were treated with Bentall procedures,
whereas 12 received valve-sparing procedures. The average age of the patient group was 65.5 years (range 24-80), with 64% males.
Thirty-day mortality was 9.7% (consistent with calculated Euroscore II: 9.2%). The long-term survival was 80.9% at 3, 5 and 10 years. No deaths occurred
between 3 and 10 years postoperatively. In an age- and sex case-matched Belgian population, 3-, 5- and 10-year survival were 95.7%, 94.7% and 85.2%,
respectively. Long-term survival was not signicantly dierent between both groups. Poor NYHA class at the time of surgery (P = 0.041) and COPD (P = 0.028)
had a signicant impact on global survival. Valve-sparing operations provide similar long-term survival, avoiding thrombo-embolic complications.
Conclusions Reconstruction of the ascending aorta for degenerative aneurysmal disease restores normal life expectancy, compared with an
age- and sex-matched case-control population. Early mortality is consistent with the Euroscore II risk calculation. Whereas late survival progressively
declines in the average population, it remains constant in the treated group after 3 years. COPD and poor functional class signicantly impair survival.
Valve-sparing procedures confer a similar long-term survival as valve replacement.
Keywords: Aorta ascending aneurysm survival risk factor.
in individuals over 65 years is estimated around 3-4%.
The condition negatively impacts on the survival of
patients, mainly due to the occurrence of two dreaded
complications: dissection or rupture, both occurring at
an incidence of approximately 3.5 in 100,000. Elective
reconstruction of the ascending aorta by either the clas-
sical Bentall operation or more recently by valve-sparing
procedures, such as the Yacoub or David procedures,
aims at preventing those complications. Whether this
surgery restores life expectancy to normal, remains a
matter of debate. This paper describes our clinical expe-
rience with these procedures and the long-term out-
come.
Acta Cardiol 2013; 68(4): 349-353 doi: 10.2143/AC.68.4.2988887
[
Original article ]
D. Van Duel et al. 350
Twelve patients underwent valve-sparing procedures:
7 reimplantation or David procedures and 5 remodelling
or Yacoub procedures.
Duration of extracorporeal circulation was 172 73 min
for a clamp time of 113 43 min. In 5 patients, circulatory
arrest had to be carried out in order to reconstruct the
aortic arch during the same procedure. This was carried
out under deep hypothermic circulatory arrest (equaliza-
tion of all temperatures at 18C) combined with selective
antegrade cerebral perfusion. The average duration of
circulatory arrest was 24 8 min.
STATISTICAL ANALYSIS
A Kaplan-Meier curve was constructed to calculate
survival in the treatment group. The common closing
date method was used and the survival status of each
patient was assessed on August 31, 2012. To compare
the survival of those patients with the expected survival
of an average Belgian population, a randomly selected
(age and sex) case-matched population was studied.
The two groups were compared, using the log-rank test.
The Cox proportional hazard models were adapted to
estimate the relative risk of death for covariates in the
dataset. Two-sided P-values of 0.05 were considered
statistically significant. The statistical analysis was car-
ried out using STATA and R-software.
RESULTS
Perioperative and in-hospital mortality and
morbidity
There were seven 30-day or in-hospital deaths (9.7%).
No patient died during surgery. The patients died from
the following causes: two as a consequence of sepsis, two
due to multi-organ failure, one as a consequence of
pneumonia, one because of right ventricular failure and
one following rupture of an abdominal aneurysm.
Postoperative complications can be summarized as
follows: 14 patients (19%) suffered pulmonary compli-
cations, three needed a revision for bleeding or tampon-
ade (4%), 24 patients (33%) presented with one or more
episodes of atrial fibrillation, high grade AV-block devel-
oped in three patients (4%). Transient renal function
impairment (GFR < 60 ml/min) occurred in 18 patients
(25%), none of whom required dialysis.
Time-related survival
Within three months of discharge from the hospital,
another four patients died: one from pneumonia, one as
a consequence of CVA, one patient committed suicide
PATIENTS AND METHODS
From May 1998 to January 2012, 72 patients under-
went elective reconstruction of the ascending aorta. Data
from this patient cohort were analysed, using the data-
base from the department of Cardiothoracic Surgery at
the Jessa hospital. Follow-up information was obtained
using patient files, telephone contact with the patient or
his/her close relatives or through the general practi-
tioner. Follow-up was 100% complete.
Patient characteristics are shown in table I.
The aetiology of the aortic disease was degenerative
in 25 patients (35%). There was annulo-aortic ectasia in
13 patients (18%) and 17 patients presented with a bicus-
pid valve (24%). Less common indications for recon-
struction were aneurysm of the sinus of Valsalva
(4 patients, 6%) and endocarditis (4 patients, 6%). One
patient had a dysfunctional prosthesis and 8 patients
(11%) were treated for chronic dissection of the ascend-
ing aorta. As a rule, a diameter of 5.5 cm was taken as
cut-off for surgery, except for Marfan patients and
patients with bicuspid valves, in which case surgery was
performed at 5 cm or more.
In 44 patients, a Bentall procedure was performed
using a valved conduit with a St. Jude mechanical pros-
thesis. Sixteen patients underwent a modified Bentall
procedure, using a bioprosthesis (8 Carpentier-Edwards
pericardial valves, 2 Medtronic-Mosaic porcine valves,
2 Mitroflow pericardial valves, 1 biovalsalva graft, 2 Free-
style full root prostheses and 1 full root homograft).
Table 1 Patient characteristics and risk prole
Variable (N = 72) Value %
Gender (M/F) 46/26 64/36
Median age (years; Q1-Q3) 65.5 (57;71)
Age distribution (years) 24 - 80
Cardiovascular risk factors
Hypertension 35 48.6
Coronary artery disease 26 36.1
Diabetes mellitus 7 9.7
COPD 15 20.8
Bicuspid valve 15 20.8
NYHA class
I & II 38 52.7
III & IV 34 47.2
Marfan syndrome 2 2.8
Ejection fraction
60% 42 58.3
> 60% 30 41.6
Creatinine (mg/dl; mean SD ) 1.09 0.42
Survival after ascending aortic reconstructive surgery 351
3.39 times higher than that of non-COPD patients.
Patients with a good functional status (NYHA I or II) at
the time of surgery survived better than those with a
poor functional status (NYHA III and IV; P = 0.041).
Other covariates could not be identified to significantly
influence survival after reconstructive surgery. This,
however, could be the consequence of the small sample
size, combined with a limited number of events. No
mortality occurred in the treated group from three years
after surgery onwards.
Six out of 43 patients who received a mechanical
prosthesis, died. In the biological group, 3 out of 17 died
and in the valve-sparing group 4 out of 12. Long-term
survival was not significantly different between patients
with a mechanical or a biological prosthesis (P = 0.62).
Also valve-sparing surgery had a comparable survival
(P = 0.33 vs biological prosthesis).
and one elderly patient died in a nursing home as a con-
sequence of progressive deterioration of his general con-
dition. In the second year after surgery, one patient died
of the consequences of diabetes type II. In year 3 after
surgery, another two patients died, one following a road
traffic accident and one from unknown causes. Three-,
five- and ten-year survival remained constant at 80.9%.
To compare the survival of these patients with the
expected survival of the average Belgian population, a
randomly selected age- and sex-matched case-control
population was studied. The Kaplan-Meier survival
curve of both groups is shown in figure 1. Three-, 5- and
10-year survival of this group was 95.7%, 94.7% and
85.2%, respectively. The case-matched population shows
a better initial survival, due to the expected per operative
mortality in the aortic surgery group. Later on, however,
there is an incremental loss in the case-matched popula-
tion, resulting in a similar long-term survival.
Incremental risk factors for premature death
To assess which covariates influence global survival
of elective aortic reconstructive surgery, a Cox propor-
tional hazard model was applied to the population. As
preoperative variables, age of the patient at surgery,
gender, left ventricular function, hypertension, presence
of a bicuspid aortic valve, associated coronary disease,
diabetes, COPD, renal function impairment and NYHA
class were taken into account.
As perioperative variables, surgeon experience and
type of surgery were built into the model. The data of
the proportional hazard model are shown in table 2.
The presence of COPD at surgery revealed to be an
unfavourable factor for global survival (P = 0.028). The
risk of death for COPD patients in this series was
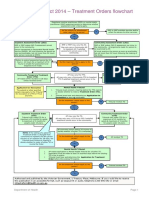
Fig. 1 Kaplan-Meier survival curve in aortic surgery and
case-matched population
Table 2 Proportional hazard model
Characteristic Unadjusted Adjusted
HR (SE) P -value HR (SE) P -value
Age 1.005 (0.026) 0.831 1.006 (0.031) 0.854
Gender 1.760 (0.981) 0.310 2.694 (1.800) 0.138
Hypertension 0.474 (0.285) 0.215 0.410 (0.278) 0.189
Bicuspid valve 0.674 (0.518) 0.608 1.099 (0.968) 0.915
Coronary disease 1.464 (0.707) 0.708 1.464 (0.927) 0.547
Diabetes mellitus 0.745 (0.776) 0.778 0.873 (0.974) 0.903
COPD 3.394 (1.889) 0.028 4.542 (2.875) 0.017
Renal failure 1.012 (0.011) 0.275 1.013 (0.015) 0.382
Surgeon experience (years) 0.911 (0.048) 0.076 0.931 (0.077) 0.390
NYHA (I or II vs III or IV) 0.112 (0.120) 0.041
Ejection fraction 0.634 (0.449) 0.51
D. Van Duel et al. 352
86% and 81.5%, respectively. The 5- and 10-year survival
reported by Maureira
5
et al. is 86.3 2.78% and
73.7 4.23%. Tamura et al.
6
report a survival of 84.2%
at 5 years and 64.3% at 15 years. Verbakel et al.
7
report
a 78% 4% overall survival at 5 years and 66% 10%
at 10 years (with an early mortality of 11.2%). In the
previously mentioned National UK Registry 5 year sur-
vival was 77.1% and 10 year survival 70%
3
.
Because it is difficult to compare absolute survival
data in different series, given the fact that risk factors
may considerably vary between groups, we decided to
compare the survival of the treatment group with the
expected survival of an average Belgian population.
A randomly selected age- and sex-matched case-control
study population was obtained from the national Belgian
census. Due to the expected early mortality, the case-
matched population had a better initial survival. How-
ever, due to a continued attrition rate in the case-matched
population, long-term survival was not significantly
different in both groups. Therefore, this study suggests
that patients with degenerative disease of the ascending
aorta who survive reconstructive surgery, have a low risk
of complications and a normal life expectancy thereafter.
Risk factor analysis
Cox proportional hazard analysis identified COPD
as an independent risk factor for overall mortality with
an adjusted hazard ratio of 4.542 (SE 2.875, P = 0.017).
The risk of premature death for COPD patients was
3.39 times higher than for non-COPD patients.
Due to the limited number of patients and events,
this study may, however, not have the mathematical
power to identify additional variables.
In our study, for example, age could not be identified
to have a predictive value for survival. Although this
observation is confirmed by other authors
8,9
, Prifti et al.
4
and David et al.
10
find a relation between age of the
patient and survival. It should be pointed out, however,
that the average age of this patient group was relatively
high (65.5 years). In younger patients, survival is sig-
nificantly superior. David et al. obtained a 5-year sur-
vival of 94% and a 10-year survival of 88% in a patient
population with an average age of 45 years at surgery
(40% Marfan patients).
The choice of valve for aortic root reconstruction
seems to have no influence on long-term outcome. There
was no difference between long-term survival of patients
with a mechanical or a biological prosthesis (P = 0.62).
This observation confirms previous reports by Etz et
al.
11
and Lehr et al.
12
. However, in the context of aortic
root reconstruction, all biological prostheses may not
perform equally. A recent report on the Hancock bio-
prosthetic porcine conduit for aortic root reconstruction
Morbidity
Forty-four patients were treated with coumadin for
a mechanical prosthesis. In this group, two serious cer-
ebral bleeding events occurred: one resulted in a per-
manent deficit and one in a transient ischaemic attack.
One patient with a biological Bentall procedure devel-
oped an ischaemic CVA (4%). There were no thrombo-
embolic complications in the valve-sparing group.
One patient developed paraparesis following spinal
chord ischaemia as a consequence of circulatory arrest
for an associated replacement of the aortic arch.
There were no reinterventions for failed Bentall pro-
cedure as a consequence of pseudoaneurysma formation
at the level of the coronary buttons. No significant aor-
tic incompetence occurred in the valve-sparing group.
DISCUSSION
Hospital mortality
Hospital mortality in our patient population of elec-
tive ascending aortic surgery reconstruction was 9.7%.
The calculated operative risk according to Euroscore II
for this group was 9.2%. This is comparable to reported
mortality in other papers. In a mixed population of elec-
tive and urgent cases, Pacini et al. report a hospital
mortality of 6.9% with 6.6% acute dissections
1
. Kou-
choukos et al. report 5.2% mortality with 10% acute
dissections
2
. In a recent report from a national cohort
in the United Kingdom, 30-day mortality for non-urgent
composite valved grafts in aortic position is 6.9%
(1,379 patients)
3
. Our single-centre study confirms pre-
vious reports that ascending aortic reconstruction can
be performed with a reasonable operative risk. Neverthe-
less, reconstruction of the ascending aorta remains a
complex procedure and carries a significant early risk
even in elective patients.
Whether this early risk can be reduced, remains a
matter of debate. However, in this study we identified
functional class as a significant predictor of early mortal-
ity (P = 0.041). Therefore we speculate that early outcome
could be improved by earlier referral of patients, par-
ticularly since poor functional class seems associated
with aortic expansion and/or valvular regurgitation,
resulting in left ventricular dysfunction.
Long-term survival
Five-year survival in the treated group was 80.9% and
no further attrition was observed until 15 years after
surgery. Although this is a limited number of patients,
this long-term follow-up is comparable to other series.
Prifti et al.
4
report a 3-, 5- and 10-year survival of 91.8%,
Survival after ascending aortic reconstructive surgery 353
of late aortic incompetence. In this series we preserved
the aortic valve only in patients with tricuspid aortic
valve and normal cusps. With increasing confidence in
this technique, indications have broadened. Several
groups have shown that reconstruction of bicuspid aor-
tic valves in the presence of proximal aortic dilatation
results in a good short-term outcome, regardless whether
the remodelling technique
16
or the reimplantation tech-
nique is used
17
.
In the younger population, valve-sparing surgery
shows distinct advantages: in this patient group, no
thrombo-embolic complications were observed, whereas
in the mechanical prosthesis group one CVA and one
TIA occurred and in the bioprosthesis group one ischae-
mic CVA.
Despite these promising evolutions in aortic recon-
structive surgery, even the surgeons most dedicated to
valve-sparing surgery, will admit that there are a number
of severely diseased aortic valves, in which the Bentall
procedure remains the treatment of choice. It is reassur-
ing to see that this procedure can be carried out with a
good and predictable short- and long-term survival and
that for the hospital survivors we are able to restore life
expectancy to normal.
CONFLICT OF INTEREST: none declared..
reported low actuarial survival rates at 5 (77.0 5.3%)
and 10 (54.0 7.5%) years (excluding operative and in-
hospital deaths 14%). There was a high rate of reinter-
vention in this group for structural valve degeneration
(freedom from reoperation at 10 years 64 10.2%)
13
.
It should be pointed out that in our series no reinterven-
tions for structural degeneration had to be performed.
This series includes 12 aortic valve-sparing proce-
dures, designed to preserve the aortic valve cusps. David
et al.
14
and Yacoub et al.
15
have developed different tech-
niques in which the native valve can be preserved and
lifelong anticoagulation can be avoided or at least post-
poned. Remodelling of the aortic root, as first described
by Yacoub et al.
15
is probably the more physiologic
operation because it recreates the aortic sinuses and
sino-tubular junction allowing for near-physiologic
motion of the cusps and annulus. However, particularly
in patients with annuloaortic ectasia, lack of support of
the aortic annulus may result in progressive dilatation
and subsequent aortic incompetence. Therefore, we did
not use this technique in annuloaortic ectasia and man-
aged to avoid significant aortic incompetence. Reim-
plantation of the aortic valve, as described by David et
al.
14
is a more demanding procedure, since it implies
suturing the entire annulus and subcommissural trian-
gles into a prosthetic graft. However, this technique
stabilizes the annulus and therefore reduces the incidence
1. Pacini D, Ranocchi F, Angeli E, Settepani F,
Pagliaro M, Martin-Suarez S, Di Bartolomeo R,
Pierangeli A. Aortic root replacement with
composite valve graft.
Ann Thorac Surg 2003; 76: 90-8.
2. Kouchoukos NT, Wareing TH, Murphy SF,
Perrillo JB. Sixteen-year experience
with aortic root replacement.
Results of 172 operations.
Ann Surg 1991; 214: 308-18; discussion 18-20.
3. Kalkat MS, Edwards M-B, Taylor KM,
Bonser RS. Composite aortic valve
graft replacement: mortality outcomes
in a national registry.
Circulation 2007; 116: 301-6.
4. Prifti E, Bonacchi M, Frati G, Proietti P,
Giunti G, Babatasi G, Massetti M, Sani G.
Early and long-term outcome in
patients undergoing aortic root
replacement with composite graft
according with composite graft
according to Bentalls technique.
Eur J Cardiothorac Surg 2002; 21: 15-21.
5. Maureira P, Vanhuyse F, Martin C, Lekehal M,
Carteaux JP, Tran N, Villemot JP. Modified
Bentall procedure using two short grafts for
coronary reimplantation: long-term results.
Ann Thorac Surg 2012; 93: 443-9.
6. Tamura K, Arai H, Kawaguchi S, Makita S,
Miyagi N, Watanabe T, Fujiwara T. Long-term
results of modified Bentall procedure using
flanged composite aortic prosthesis.
Ann Thorac Cardiovasc Surg 2013; 19: 126-30.
7. Verbakel KM, Van Straten AH, Hamad MA, Tan ES,
ter Woorst JF. Results of one-hundred and
seventy patients after elective Bentall operation.
Asian Cardiovasc Thorac Ann 2012; 20: 418-25.
8. Svensson L, Crawford S, Hess K, Coselli J,
Safi H. Composite valve graft replacement of
the proximal aorta: comparison of techniques
in 348 patints.
Ann Thorac Surg 1992; 54: 427-37.
9. Tambeur L, Tirone DE, Unger M, Armstrong S,
Ivanov J, Webb G. Results of surgery for aortic
root aneurysm in patients with the Marfan
syndrome.
Eur J Cardiothorac Surg 2000; 17: 415-9.
10. David TE, Feindel CM, Webb GD, Colman JM,
Armstrong S, Maganti M. Long-term results of
aortic valve-sparing operations for aortic root
aneurysm.
J Thorac Cardiovasc Surg 2006; 132: 347-54.
11. Etz CD, Bischoff MS, Bodian C, Roder F,
Brenner R, Griepp RB, Di Luozzo G. The Bentall
procedure: is it the gold standard? A series of
597 consecutive cases.
J Thorac Cardiovasc Surg 2010; 140(6 Suppl):
S64-70; discussion S86-91.
12. Lehr EJ, Wang PZ, Oreopoulos A, Kanji H,
Norris C, Macarthur R. Midterm outcomes and
quality of life of aortic root replacement:
mechanical vs biological conduits.
Can J Cardiol 2011; 27: 262.e15-20.
13. Badiu CC, Bleiziffer S, Eichinger WB,
Hettich I, Krane M, Bauernschmitt R,
Lange R. Long-term performance of
the Hancock bioprosthetic valved
conduit in the aortic root position.
J Heart Valve Dis 2011; 20: 191-8.
14. David TE, Armstrong S, Ivanov J, Webb GD.
Aortic valve sparing operations: an update.
Ann Thorac Surg 1999; 67: 1840-56.
15. Yacoub MH, Gehle P, Chandrasekaran V,
Birks EJ, Child A, Radley-Smith R.
Late results of a valve-sparing
operation in patients with aneurysms
of the ascending aorta and root.
J Thorac Cardiovasc Surg 1998; 115: 1080-90.
16. Schfers HJ, Kunihara T, Fries P, Brittner B,
Aicher DJ. Valve-preserving root
replacement in bicuspid aortic valves.
J Thorac Cardiovasc Surg 2010; 140(6 Suppl):
S36-40; discussion S45-51.
17. de Kerchove L, Boodhwani M, Glineur D,
Vandyck M, Vanoverschelde J-L,
Noirhomme P, El Khoury G. Valve
sparing-root replacement with the
reimplantation technique to increase the
durability of bicuspid aortic valve repair.
J Thorac Cardiovasc Surg 2011; 142: 1430-8
REFERENCES
S-ar putea să vă placă și
- 106720070205Document8 pagini106720070205lovehopeÎncă nu există evaluări
- Obstetric Nursing Sample ChapterDocument14 paginiObstetric Nursing Sample ChapterlovehopeÎncă nu există evaluări
- Bytes October 13-65-88 - FinalDocument24 paginiBytes October 13-65-88 - FinallovehopeÎncă nu există evaluări
- CBSPD 2014 Pharmaceutical Price ListDocument24 paginiCBSPD 2014 Pharmaceutical Price Listlovehope100% (1)
- SolutionsDocument14 paginiSolutionsHazem DiabÎncă nu există evaluări
- Uttar Pradesh Voluntary Action NetworkDocument3 paginiUttar Pradesh Voluntary Action NetworklovehopeÎncă nu există evaluări
- 2014 - 13 - Article 5Document4 pagini2014 - 13 - Article 5lovehopeÎncă nu există evaluări
- Fundamentals of NMR - James PDFDocument31 paginiFundamentals of NMR - James PDFSoundarya ChandramouleeswaranÎncă nu există evaluări
- Developing a bio-relevant dissolution method for EfavirenzDocument4 paginiDeveloping a bio-relevant dissolution method for EfavirenzlovehopeÎncă nu există evaluări
- Chemistry ExpDocument4 paginiChemistry ExplovehopeÎncă nu există evaluări
- Introduction of PharmacologyDocument10 paginiIntroduction of PharmacologylovehopeÎncă nu există evaluări
- Attachment C454ea4cDocument32 paginiAttachment C454ea4clovehopeÎncă nu există evaluări
- A C A D e M I C S C I e N C e SDocument5 paginiA C A D e M I C S C I e N C e SlovehopeÎncă nu există evaluări
- J. Org. Chem., 1962, 27 (9), PP 3236-3239Document4 paginiJ. Org. Chem., 1962, 27 (9), PP 3236-3239lovehopeÎncă nu există evaluări
- J Jep 2005 01 031Document2 paginiJ Jep 2005 01 031lovehopeÎncă nu există evaluări
- Exp't 41: The Reaction of Maleic Anhydride and CycloheptatrieneDocument5 paginiExp't 41: The Reaction of Maleic Anhydride and CycloheptatrienelovehopeÎncă nu există evaluări
- Exp 11Document4 paginiExp 11lovehopeÎncă nu există evaluări
- J Biomaterials 2012 03 046Document18 paginiJ Biomaterials 2012 03 046lovehopeÎncă nu există evaluări
- Drying Evaporation EnglishDocument1 paginăDrying Evaporation EnglishlovehopeÎncă nu există evaluări
- Exp 31Document4 paginiExp 31lovehopeÎncă nu există evaluări
- Exp't 51: Nitration of NitrobenzeneDocument4 paginiExp't 51: Nitration of NitrobenzenelovehopeÎncă nu există evaluări
- Exp't 42: Two Easy Diels-Alder PuzzlesDocument5 paginiExp't 42: Two Easy Diels-Alder Puzzleslovehope0% (1)
- SolubilityDocument10 paginiSolubilityOmar S. SalihÎncă nu există evaluări
- Exp't 61: 1,4-Di-T-Butylbenzene Via Friedel-Crafts AlkylationDocument6 paginiExp't 61: 1,4-Di-T-Butylbenzene Via Friedel-Crafts AlkylationlovehopeÎncă nu există evaluări
- Exp't 42: Two Easy Diels-Alder PuzzlesDocument5 paginiExp't 42: Two Easy Diels-Alder Puzzleslovehope0% (1)
- Exp 11Document4 paginiExp 11lovehopeÎncă nu există evaluări
- Exp 4Document4 paginiExp 4lovehopeÎncă nu există evaluări
- Exp't 13: Phase-Transfer-Catalyzed Alkylation of Diethyl MalonateDocument5 paginiExp't 13: Phase-Transfer-Catalyzed Alkylation of Diethyl MalonatelovehopeÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Policy For Exemption From Assessment and Examination FinalDocument28 paginiPolicy For Exemption From Assessment and Examination FinalGloria JaisonÎncă nu există evaluări
- Health Assessment Project Assignment CultureDocument8 paginiHealth Assessment Project Assignment CultureJennifer PortilloÎncă nu există evaluări
- Panduan Praktik Klinis Ugd PopoolivDocument49 paginiPanduan Praktik Klinis Ugd PopoolivrusliÎncă nu există evaluări
- Central Maine Healthcare Cancer Institute Certificate of Need ApplicationDocument33 paginiCentral Maine Healthcare Cancer Institute Certificate of Need ApplicationMaine Trust For Local NewsÎncă nu există evaluări
- Infection Control: Dr.T.V.Rao MD Professor of MicrobiologyDocument41 paginiInfection Control: Dr.T.V.Rao MD Professor of Microbiologytummalapalli venkateswara rao100% (1)
- Endoscopic Band Ligation Is Safe Despite Low Platelet Count and HighDocument10 paginiEndoscopic Band Ligation Is Safe Despite Low Platelet Count and HighGustavo FernándezÎncă nu există evaluări
- Remembering The Good Old Days: Dr. Naresh TrehanDocument1 paginăRemembering The Good Old Days: Dr. Naresh TrehanLife WatchÎncă nu există evaluări
- THE AUTOPSY PROCESSDocument31 paginiTHE AUTOPSY PROCESSiutkr7ki7r7tkiÎncă nu există evaluări
- Caesarean Section Performing Caesarean SectionDocument13 paginiCaesarean Section Performing Caesarean SectionBlablabla BlablablaÎncă nu există evaluări
- 1 Early Management of Trauma Patient in The HospitalDocument23 pagini1 Early Management of Trauma Patient in The HospitalkgnmatinÎncă nu există evaluări
- Penguins Medicine August-SeptumberDocument215 paginiPenguins Medicine August-SeptumberKhattabÎncă nu există evaluări
- Normothermia Audit Tool: AHRQ Safety Program For SurgeryDocument3 paginiNormothermia Audit Tool: AHRQ Safety Program For SurgeryDewi ListyoriniÎncă nu există evaluări
- A Comprehensive Introduction To Abdominal Acupuncture 1519537480Document5 paginiA Comprehensive Introduction To Abdominal Acupuncture 1519537480Marco GutzÎncă nu există evaluări
- Evaluasi Kelengkapan Rekam Medis Berdasa 1093e2ccDocument9 paginiEvaluasi Kelengkapan Rekam Medis Berdasa 1093e2ccOctavia MaltaÎncă nu există evaluări
- Medical Surgical Nursing Practice Test Part 1Document15 paginiMedical Surgical Nursing Practice Test Part 1cleznielÎncă nu există evaluări
- Pharmacology of LSD Review (Book Review)Document3 paginiPharmacology of LSD Review (Book Review)Matt BaggottÎncă nu există evaluări
- Map Hgs Good HopeDocument1 paginăMap Hgs Good HopeKevin venessÎncă nu există evaluări
- BATHE Journal PDFDocument10 paginiBATHE Journal PDFKAROMAHUL MALAYA JATIÎncă nu există evaluări
- National Cancer Control Program OverviewDocument15 paginiNational Cancer Control Program OverviewAparna Kingini100% (1)
- Flowchart - Mental Health Act Treatment OrderDocument1 paginăFlowchart - Mental Health Act Treatment OrderEdwin100% (1)
- Spotters 1Document10 paginiSpotters 1elavarkuzhali2019Încă nu există evaluări
- Blood Culture Manual MT - SinaiDocument41 paginiBlood Culture Manual MT - SinaiAvi Verma100% (1)
- Section16 - Questions and AnswersDocument62 paginiSection16 - Questions and Answersdivine venturoÎncă nu există evaluări
- Freedom TherapeuticDocument2 paginiFreedom TherapeuticAna WongÎncă nu există evaluări
- FAQs - NBME Comprehensive Clinical Science Self-Assessments - Updated July 28, 2021Document3 paginiFAQs - NBME Comprehensive Clinical Science Self-Assessments - Updated July 28, 2021羅瑞恩Încă nu există evaluări
- Tuberculin Skin Testing (Mantoux Test PPD Test) : Dr. Heda Melinda, DR., Spa (K) .,M.KesDocument2 paginiTuberculin Skin Testing (Mantoux Test PPD Test) : Dr. Heda Melinda, DR., Spa (K) .,M.KesFelix AnthonyÎncă nu există evaluări
- Conservative Management of Cutaneous Sinus Tract of Dental Origin Report of Two CasesDocument4 paginiConservative Management of Cutaneous Sinus Tract of Dental Origin Report of Two CasesInternational Journal of Innovative Science and Research TechnologyÎncă nu există evaluări
- Drugs for Cough, Bronchial Asthma and InflammationDocument47 paginiDrugs for Cough, Bronchial Asthma and InflammationNavlika DuttaÎncă nu există evaluări
- Science 2013 Couzin Frankel 68 9Document2 paginiScience 2013 Couzin Frankel 68 9Ricardo ChavarriaÎncă nu există evaluări
- 16.3 Risks of TobaccoDocument4 pagini16.3 Risks of TobaccoGabriel ParksÎncă nu există evaluări