Documente Academic
Documente Profesional
Documente Cultură
Clostridium Difficile
Încărcat de
Rita della Valentini0 evaluări0% au considerat acest document util (0 voturi)
81 vizualizări9 paginiC. Difficile colitis is a cause of infectious diarrhea due to a type of sporeforming bacteria. Symptoms include bloating and diarrhea, with abdominal pain, which may become severe. Relapses of CDI have been reported in up to 20% of cases.
Descriere originală:
Drepturi de autor
© © All Rights Reserved
Formate disponibile
DOCX, PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentC. Difficile colitis is a cause of infectious diarrhea due to a type of sporeforming bacteria. Symptoms include bloating and diarrhea, with abdominal pain, which may become severe. Relapses of CDI have been reported in up to 20% of cases.
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca DOCX, PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
81 vizualizări9 paginiClostridium Difficile
Încărcat de
Rita della ValentiniC. Difficile colitis is a cause of infectious diarrhea due to a type of sporeforming bacteria. Symptoms include bloating and diarrhea, with abdominal pain, which may become severe. Relapses of CDI have been reported in up to 20% of cases.
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca DOCX, PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 9
Clostridium difficile colitis (also known as C.
diff diarrhea, Clostridium difficile infection [CDI]
and pseudomembranous colitis) is a cause of infectious diarrhea due to a type of spore-
forming bacteria
[1]
Latent symptoms of CDI often mimic some flu-like symptomsand can mimic
disease flare in people with inflammatory bowel disease-associated colitis.
[2]
C diff release toxins that
can causebloating and diarrhea, with abdominal pain, which may become severe.
The colitis is thought to occur when this bacteria replaces normal gut flora that has been
compromised, usually following antibiotic treatment for unrelated infection. The disturbance of
normal healthy bacteria may provide C. difficile an opportunity to overrun the
intestinal microbiome.
[3]
It is a type of antibiotic-associated diarrhea.
Mild cases of CDI can often be treated by discontinuing the antibiotics. More serious cases require
specific antibiotic treatment. Relapses of CDI have been reported in up to 20% of cases.
[4]
C.
difficile infection is a growing problem in health care facilities, killing some 14,000 people a year in
the United States.
Signs and symptoms[edit]
Symptoms range from mild diarrhea to severe life-threatening inflammation of the colon.
[6]
In adults, a clinical prediction rule found the best signs to be: significant diarrhea ("new onset of
more than three partially formed or watery stools per 24-hour period"), recent antibiotic exposure,
abdominal pain, fever (up to 40.5 C or 105 F), and a distinctive foul stool odour. In a population of
hospitalized patients, prior antibiotic treatment plus diarrhea or abdominal pain had a sensitivity of
86% and a specificity of 45%.
[7]
In this study with a prevalence of positive cytotoxin assays of 14%,
the positive predictive value was 18% and the negative predictive value was 94%.
In children, the most prevalent symptom of a CDI is watery diarrhea with at least three bowel
movements a day for two or more days, which may contain fever, loss of appetite, nausea, and/or
abdominal pain.
[1]
Those with a severe infection may also develop serious inflammation of the colon
and have little or no diarrhea.
Cause[edit]
Main article: Clostridium difficile (bacteria)
C. difficile diarrhea is caused by an infection by the C. difficile bacteria. Primary risk factors are
exposure to antibiotics, exposure to a healthcare environment, and acid-suppressing medications. C.
difficile spores are resistant to most routine surface cleaning methods, except for diluted bleach.
[citation
needed]
Spores can remain viable in the environment for long periods.
[citation needed]
In small numbers, C.
difficile does not result in significant disease.
C. difficile[edit]
Individual, drumstick-shaped C. difficile bacilli seen through scanning electron microscopy
Clostridia are motile bacteria, ubiquitous in nature and especially prevalent in soil. Under the
microscope, they appear as long, irregular (often drumstick- or spindle-shaped) cells with a bulge at
their terminal ends. Under Gram staining, C. difficile cells are Gram-positive and show optimum
growth on blood agar at human body temperatures in the absence of oxygen. When stressed, the
bacteria produce sporesthat can tolerate extreme conditions that the active bacteria cannot
tolerate.
[4]
C. difficile can become established in the human colon; it is present in 25% of the adult
population.
[4]
How C. difficile spreads
Pathogenic C. difficile strains produce multiple toxins. The most well-characterized
are enterotoxin (Clostridium difficile toxin A) and cytotoxin(Clostridium difficile toxin B), both of which
can produce diarrhea and inflammation in infected patients, although their relative contributions have
been debated.
[4]
Toxins A and B are glucosyltransferases that target and inactivate the Rho family of
GTPases. Toxin B (cytotoxin) induces actin depolymerization by a mechanism correlated with a
decrease in the ADP-ribosylation of the low molecular mass GTP-binding Rho proteins.
[8]
Another
toxin, binary toxin, has also been described, but its role in disease is not fully understood.
[9]
Antibiotic treatment of CDIs can be difficult, due both to antibiotic resistance and physiological
factors of the bacteria (spore formation, protective effects of the pseudomembrane).
[4]
The
emergence of a new, highly toxic strain of C. difficile, resistant to fluoroquinoloneantibiotics, such
as ciprofloxacin and levofloxacin, said to be causing geographically dispersed outbreaks in North
America was reported in 2005.
[10]
The U.S. Centers for Disease Control in Atlanta warned of the
emergence of an epidemic strain with increased virulence, antibiotic resistance, or both.
[11]
C. difficile is transmitted from person to person by the fecal-oral route. However, the organism forms
heat-resistant spores that are not killed by alcohol-based hand cleansers or routine surface cleaning.
Thus, these spores survive in clinical environments for long periods. Because of this, the bacteria
can be cultured from almost any surface. Once spores are ingested, their acid-resistance allows
them to pass through the stomach unscathed. They germinate and multiply into vegetative cells in
the colon upon exposure to bile acids.
In 2005, molecular analysis led to the identification of the C. difficile strain type characterized as
group BI by restriction endonucleaseanalysis , as North American pulse-field-type NAP1 by pulsed-
field gel electrophoresis and as ribotype 027; the differing terminology reflects the predominant
techniques used for epidemiological typing. This strain is referred to as C. difficile BI/NAP1/027.
[12]
Risk factors[edit]
Antibiotics[edit]
C. difficile colitis is most strongly associated with fluoroquinolones, cephalosporins, carbapenems,
and clindamycin.
[13][14][15]
The European Center for Disease Prevention and Control recommend that
fluoroquinolones and the antibiotic clindamycin be avoided in clinical practice due to their high
association with CDI.
[citation needed]
Some research suggests the overuse of antibiotics in the raising of livestock is contributing to
outbreaks of bacterial infections such as C. difficile.
[16]
Antibiotics, especially those with a broad activity spectrum (such as clindamycin) disrupt
normal intestinal flora. This can lead to an overgrowth of C. difficile, which flourishes under these
conditions. Pseudomembranous colitis can follow, creating generalized inflammation of the colon
and the development of "pseudomembrane", a viscous collection of inflammatory cells, fibrin, and
necrotic cells.
[4]
Healthcare environment[edit]
People are most often nosocomially infected in hospitals, nursing homes, or other medical
institutions, although infection outside medical settings is increasing. The rate of C.
difficileacquisition is estimated to be 13% in patients with hospital stays of up to two weeks, and 50%
with stays longer than four weeks.
[17]
Long-term hospitalization or residence in a nursing home within the previous year are independent
risk factors for increased colonization.
[18]
Acid suppression medication[edit]
Increasing rates of community-acquired CDI are associated with the use of medication to
suppress gastric acid production: H2-receptor antagonists increased the risk 1.5-fold, andproton
pump inhibitors by 1.7 with once-daily use and 2.4 with more than once-daily use.
Pathophysiology[edit]
The use of systemic antibiotics, including (but not limited to) any penicillin-based antibiotic such
as ampicillin, cephalosporins, and clindamycin, causes the normal bacterial flora of the bowel to be
altered. In particular, when the antibiotic kills off other competing bacteria in the intestine, any
bacteria remaining will have less competition for space and nutrients. The net effect is to permit
more extensive growth than normal of certain bacteria. Clostridium difficile is one such type of
bacterium. In addition to proliferating in the bowel, C. difficilealso produces toxins. Without either
toxin A or toxin B, C. difficile may colonize the gut, but is unlikely to cause pseudomembranous
colitis.
[21]
Diagnosis[edit]
Micrograph of a colonic pseudomembrane in C. difficile colitis, a type of pseudomembranous colitis,H&E stain
Endoscopic image of pseudomembranous colitis, with yellow pseudomembranes seen on the wall of the sigmoid
colon
Pathological specimen showing pseudomembranous colitis
Pseudomembranous colitis on computertomography
Prior to the advent of tests to detect C. difficile toxins, the diagnosis was most often made
by colonoscopy or sigmoidoscopy. The appearance of "pseudomembranes" on the mucosa of
the colon or rectum is highly suggestive, but not diagnostic of the condition.
[22]
The
pseudomembranes are composed of an exudate made of inflammatory debris, white blood cells.
Although colonoscopy and sigmoidoscopy are still employed, stool testing for the presence of C.
difficile toxins is now often the first-line diagnostic approach. Usually, only two toxins are tested for -
toxin A and toxin B - but the organism produces several others. This test is not 100% accurate, with
a considerable false-negative rate even with repeat testing.
revention[edit]
Antibiotics[edit]
The most effective method for preventing CDI is proper antimicrobial prescribing. In the hospital
setting, where CDI is most common, nearly all patients who develop CDI are exposed to
antimicrobials. Although proper antimicrobial prescribing sounds easy to do, about 50% of
antimicrobial use is considered inappropriate. This is consistent whether in the hospital, clinic,
community, or academic setting. A decrease in CDI by limiting antibiotics or by limiting unnecessary
antimicrobial prescriptions in general, both in outbreak and non-outbreak settings has been
demonstrated to be most strongly associated with reduced CDI. Further, reactions to medication
may be severe: CDI infections were the most common contributor to adverse drug events seen in
U.S. hospitals in 2011.
[29]
Probiotics[edit]
Some evidence indicates probiotics may be useful to prevent infection and
recurrence.
[30][31]
Treatment with Saccharomyces boulardii in those who are not immunocompromised
with C. difficile may also be useful.
[32][33]
In 2010, the Infectious Diseases Society of
Americarecommended against their use due to the risk of complications.
[30][32]
Subsequent reviews,
however, did not find an increase in adverse effects with treatment.
[31]
and overall treatment appears
safe.
[34]
Infection control[edit]
Rigorous infection protocols are required to minimize this risk of transmission.
[35]
Infection control
measures, such as wearing gloves when caring for people with CDI, are effective at
prevention.
[36]
This works by limiting the spread of C. difficile in the hospital setting. In addition,
washing with soap and water will eliminate the spores from contaminated hands, but alcohol-based
hand rubs are ineffective.
[37]
Bleach wipes containing 0.55% sodium hypochlorite have been shown
to kill the spores and prevent transmission between patients.
[38]
Installing lidded toilets and closing
the lid prior to flushing also reduces the risk of contamination.
[39]
Those who have CDIs should be in rooms with other people with CDIs or by themselves when in
hospital.
[36]
Common hospital disinfectants are ineffective against C. difficile spores and may actually promote
spore formation. However, disinfectants containing a 10:1 ratio of water to bleacheffectively kill the
spores.
[40]
Hydrogen peroxide vapor (HPV) systems used to sterilize a patient room post discharge
has been shown to reduce infection rates and to reduce risk of infection to subsequent patients. The
incidence of CDI was reduced by 53%
[41]
or 42%
[42]
though use of HPV. Ultraviolet cleaning devices
and dedicated housekeeping staff to disinfect the rooms of patients infected with C. difficile after
discharge may be effective.
[43]
Treatment[edit]
Carrying C. difficile without symptoms is common. Treatment in those without symptoms is
controversial. In general, mild cases do not require specific treatment.
[4][44]
Oral rehydration therapy is
useful in treating dehydration associated with the diarrhea.
Medications[edit]
A number of different antibiotics are used for C. difficile, with the available agents being more or less
equally effective.
[45]
Metronidazole is typically the initial drug of choice, because of lower price.
[32]
Oral vancomycin is second-line for mild to moderate cases and is recommended first-line for
severe disease.
[32]
Vancomycin and metronidazole, however, appear to be equally effective.
[44]
Fidaxomicin has been found to be equally effective as vancomycin in those with mild to
moderate disease.
[46]
It is tolerated as well as vancomycin
[47]
and may have a lower risk of
recurrence.
[45]
It may be used in those who have recurrent infections and have not responded to
the other antibiotics.
[46]
Drugs used to slow or stop diarrhea such as loperamide may worsen C. difficile disease, so are not
recommended.
[48]
Cholestyramine, an ion exchange resin, is effective in binding both toxin A and B,
slowing bowel motility and helping prevent dehydration.
[49]
Cholestyramine is not recommended with
vancomycin. A last-resort treatment in those who are immunosuppressed is intravenous
immunoglobulin (IVIG).
[49]
Probiotics[edit]
Evidence to support the use of probiotics in the treatment of active disease is insufficient.
[32][50]
thus in
this situation they are neither recommended as an add-on to standard therapy nor for use alone.
[51]
Stool transplant[edit]
Fecal bacteriotherapy, known as a stool transplant, is about 90% effective in those in whom
antibiotics have not worked.
[52]
It involves infusion of bacterial flora acquired from the feces of a
healthy donor to reverse the bacterial imbalance responsible for the recurring nature of the
infection.
[53]
The procedure replaces normal, healthy colonic flora that had been wiped out by
antibiotics, and reestablishes resistance to colonization by Clostridium difficile.
[54]
Due to the epidemic in North America and Europe, FMT has gained increasing prominence, with
some experts calling for it to become first-line therapy for CDI
Klasifikasi anemia akibat Gangguan Eritropoiesis[sunting | sunting sumber]
1. Anemia defisiensi Besi :
Tidak cukupnya suplai besi mengakibatkan defek pada sintesis Hb, mengakibatkan
timbulnya sel darah merah yang hipokrom dan mikrositer.
2. Anemia Megaloblastik
Defisiensi folat atau vitamin B12 mengakibatkan gangguan pada sintesis timidin dan defek
pada replikasi DNA, efek yang timbul adalah pembesaran prekursor sel darah (megaloblas)
di sumsum tulang, hematopoiesis yang tidak efektif, dan pansitopenia.
3. Anemia Aplastik
Sumsum tulang gagal memproduksi sel darah akibat hiposelularitas. Hiposelularitas ini dapat
terjadi akibat paparan racun, radiasi, reaksi terhadap obat atau virus, dan defek pada
perbaikan DNA serta gen.
4. Anemia Mieloptisik
Anemia yang terjadi akibat penggantian sumsum tulang oleh infiltrate sel-sel tumor,
kelainan granuloma, yang menyebabkan pelepasan eritroid pada tahap awal.
[2]
Klasifikasi anemia berdasarkan ukuran sel[sunting | sunting sumber]
1. Anemia mikrositik : penyebab utamanya yaitu defisiensi besi dan talasemia (gangguan Hb)
2. Anemia normositik : contohnya yaitu anemia akibat penyakit kronis seperti gangguan ginjal.
3. Anemia makrositik : penyebab utama yaitu anemia pernisiosa, anemia akibat konsumsi
alcohol, dan anemia megaloblastik.
[3]
Etiologi[sunting | sunting sumber]
Secara garis besar, anemia dapat disebabkan karena :
1. Peningkatan destruksi eritrosit, contohnya pada penyakit gangguan sistem imun, talasemia.
2. Penurunan produksi eritrosit, contohnya pada penyakit anemia aplastik, kekurangan nutrisi.
3. Kehilangan darah dalam jumlah besar, contohnya akibat perdarahan akut, perdarahan
kronis, menstruasi, ulser kronis, dan trauma.
[4]
Diagnosa
Pemeriksaan darah sederhana bisa menentukan adanya anemia. Persentase sel darah merah
dalam volume darah total (hematokrit) dan jumlah hemoglobin dalam suatu contoh darah bisa
ditentukan. Pemeriksaan tersebut merupakan bagian dari hitung jenis darah komplit (CBC).
Manajemen terapi[sunting | sunting sumber]
Terapi langsung ditujukan pada penyebab anemia, dapat berupa :
1. Transfusi darah
2. Pemberian kortikosteroid atau obat-obatan lain yang dapat menekan sistem imun.
3. Pemberian eritropoietin, hormon yang berperan pada proses hematopoiesis, berfungsi untuk
membantuk sumsum tulang pada proses hematopoiesis.
4. Pemberian suplemen besi, vitamin B12, vitamin-vitamin, dan mineral lain yang dibutuhkan.
[5]
S-ar putea să vă placă și
- Peac Hiv-2Document31 paginiPeac Hiv-2SdÎncă nu există evaluări
- The Musculoskeletal System...Document24 paginiThe Musculoskeletal System...Charity Grace Magno67% (3)
- PA 514 Intro To Infectious Disease SyllabusDocument11 paginiPA 514 Intro To Infectious Disease Syllabuslu100% (1)
- Serotonin Syndrome 06.24.2015Document18 paginiSerotonin Syndrome 06.24.2015Emily EresumaÎncă nu există evaluări
- Clinical Handbook of Infectious Diseases in Farm AnimalsDocument146 paginiClinical Handbook of Infectious Diseases in Farm Animalsigorgalopp100% (1)
- 5.thyroid Gland LectureDocument96 pagini5.thyroid Gland Lecturesdsher100% (3)
- Introduction and Overview of Community Health Nursing: Mary Ann Rosa MSN, RN, CS, GNPDocument66 paginiIntroduction and Overview of Community Health Nursing: Mary Ann Rosa MSN, RN, CS, GNPphoenix18075% (4)
- Infectious Diseases in Pregnancy - 2005 Vol.32 Issues 3Document290 paginiInfectious Diseases in Pregnancy - 2005 Vol.32 Issues 3Rickky Kurniawan,MDÎncă nu există evaluări
- Hemolytic Uremic Syndrome - Case Report: MædicaDocument3 paginiHemolytic Uremic Syndrome - Case Report: MædicaEstellaÎncă nu există evaluări
- Venous Thromboembolism (VTE) Pathophysiology September 2016Document46 paginiVenous Thromboembolism (VTE) Pathophysiology September 2016Nick GouvatsosÎncă nu există evaluări
- 2018 Fall Geriatrics SyllabusDocument41 pagini2018 Fall Geriatrics SyllabusSen SioÎncă nu există evaluări
- Community-Acquired Pneumonia 1Document15 paginiCommunity-Acquired Pneumonia 1Jaime BarraganÎncă nu există evaluări
- Chronic Hepatitis B Infection A ReviewDocument12 paginiChronic Hepatitis B Infection A ReviewMr. LÎncă nu există evaluări
- Apasl HBV Guideline 2016 PDFDocument98 paginiApasl HBV Guideline 2016 PDFDewanggaWahyuPrajaÎncă nu există evaluări
- Chronic Leukemia: Rahmawati Minhajat A. Fachruddin BenyaminDocument24 paginiChronic Leukemia: Rahmawati Minhajat A. Fachruddin BenyaminMJ Putra100% (1)
- Pediatrics in Review 2013 SalmonelosisDocument11 paginiPediatrics in Review 2013 SalmonelosisCarlos Elio Polo VargasÎncă nu există evaluări
- NatureDP 2020 DeliriumDocument26 paginiNatureDP 2020 DeliriumPaloma GBÎncă nu există evaluări
- Anti Retro Viral Drugs ClassificationDocument19 paginiAnti Retro Viral Drugs Classification王慧媚100% (1)
- Pharmacokinetics and Pharmacodynamics PDFDocument166 paginiPharmacokinetics and Pharmacodynamics PDFCarolina PosadaÎncă nu există evaluări
- Acute Kidney InjuryDocument15 paginiAcute Kidney InjuryManish VijayÎncă nu există evaluări
- Hemolytic AnemiaDocument18 paginiHemolytic AnemiaAdisurya NugrahaÎncă nu există evaluări
- Predanalitika KoagulacijaDocument10 paginiPredanalitika KoagulacijaAnonymous w4qodCJÎncă nu există evaluări
- Infectious Diseases - Infective EndocarditisDocument41 paginiInfectious Diseases - Infective Endocarditisfire_n_iceÎncă nu există evaluări
- Megaloblastic AnaemiaDocument11 paginiMegaloblastic AnaemiaJesmin_36Încă nu există evaluări
- Drug-Induced QT Interval ProlongationDocument13 paginiDrug-Induced QT Interval ProlongationgeoaislaÎncă nu există evaluări
- NHL Nandu CopasDocument95 paginiNHL Nandu CopaswihelminaÎncă nu există evaluări
- Micro GramNegCocci MD2021Document5 paginiMicro GramNegCocci MD2021Patricia Mae de JesusÎncă nu există evaluări
- Guidelines For Sedation and Anesthesia in GI Endos PDFDocument11 paginiGuidelines For Sedation and Anesthesia in GI Endos PDFHernan RuedaÎncă nu există evaluări
- Approach To The Child With Anemia - UpToDateDocument41 paginiApproach To The Child With Anemia - UpToDateDaniel Enrique CardenasÎncă nu există evaluări
- Evidence-Based Infectious DiseasesDe la EverandEvidence-Based Infectious DiseasesDominik MertzÎncă nu există evaluări
- A. Inflammation and Repair: I. Disease Process (6 Questions)Document17 paginiA. Inflammation and Repair: I. Disease Process (6 Questions)Anonymous Sw4Pk9fÎncă nu există evaluări
- 10 - Infectious Diseases (9700 AS Biology)Document33 pagini10 - Infectious Diseases (9700 AS Biology)ho100% (1)
- Stigma and Discrimination-HIV and Aids Context: (A Case Study of University CommunityDocument9 paginiStigma and Discrimination-HIV and Aids Context: (A Case Study of University CommunityJASH MATHEWÎncă nu există evaluări
- Hemolytic Uremic SyndromeDocument10 paginiHemolytic Uremic SyndromeYonz LedesmaÎncă nu există evaluări
- Textbook of Medical Parasitology Protozoology HelmDocument2 paginiTextbook of Medical Parasitology Protozoology HelmAnge OuedraogoÎncă nu există evaluări
- 2011 - Metformin - Multi-Faceted Protection Against CancerDocument22 pagini2011 - Metformin - Multi-Faceted Protection Against CancerVladDaculÎncă nu există evaluări
- Epidemiology EpidemiologyDocument13 paginiEpidemiology EpidemiologyBiratNagarÎncă nu există evaluări
- Stem Cell TransplantationDocument13 paginiStem Cell TransplantationMylls MondejarÎncă nu există evaluări
- Syphilis SlidesDocument85 paginiSyphilis SlidesSamuel Sebastian Sirapanji100% (1)
- Opioids A ReviewDocument19 paginiOpioids A ReviewAlan padilla sesma100% (1)
- Vasopressors and Inotropes in ShockDocument8 paginiVasopressors and Inotropes in ShockRiska PashaÎncă nu există evaluări
- Anti Infective AgentsDocument13 paginiAnti Infective AgentsEricka AbellaÎncă nu există evaluări
- Background: Alpha ThalassemiaDocument24 paginiBackground: Alpha ThalassemiacristieristiieÎncă nu există evaluări
- Chapter-49 - Non-Tubercular MycobacteriaDocument14 paginiChapter-49 - Non-Tubercular MycobacteriamanaÎncă nu există evaluări
- Viral Hepatitis PDFDocument4 paginiViral Hepatitis PDFNina BracyÎncă nu există evaluări
- Hepatitis Serology Cheat SheetDocument4 paginiHepatitis Serology Cheat SheetNi Putu YPÎncă nu există evaluări
- Blood and Immunity Study GuideDocument4 paginiBlood and Immunity Study GuideKimberly PollyÎncă nu există evaluări
- Lymphocytosis 2017Document3 paginiLymphocytosis 2017HafsahMalik100% (1)
- RCT Appraisal Sheets 2005 English-2Document4 paginiRCT Appraisal Sheets 2005 English-2Mahardhika AcintyaÎncă nu există evaluări
- Problems in Bone Marrow PathologyDocument29 paginiProblems in Bone Marrow PathologymaurocznÎncă nu există evaluări
- Management of Common Infections With Antimicrobials Guidance Clinical Practice Guidelines (2019) PDFDocument4 paginiManagement of Common Infections With Antimicrobials Guidance Clinical Practice Guidelines (2019) PDFveerrajuÎncă nu există evaluări
- Systemic Lupus Erythematosus (SLE)Document39 paginiSystemic Lupus Erythematosus (SLE)Nadya SabrinaÎncă nu există evaluări
- Drug-Resistant TB TreatmentDocument120 paginiDrug-Resistant TB TreatmentNadzhin15Încă nu există evaluări
- RAAS CKD ProgressionDocument86 paginiRAAS CKD ProgressionNikesh DoshiÎncă nu există evaluări
- Hiv Treatment: IC2 Haemato-Lymphoid and Tropical Medicine HLTM Dr. Eoghan de Barra 2014Document55 paginiHiv Treatment: IC2 Haemato-Lymphoid and Tropical Medicine HLTM Dr. Eoghan de Barra 2014Faiq Syukri Bin SaparudinÎncă nu există evaluări
- 5 HypertensionDocument219 pagini5 HypertensionRaul GascueñaÎncă nu există evaluări
- Off-The-Shelf' Allogeneic CAR T CellsDocument15 paginiOff-The-Shelf' Allogeneic CAR T Cellsalex portilloÎncă nu există evaluări
- Malaria Treatment TableDocument9 paginiMalaria Treatment Tableاحمد عرفاتÎncă nu există evaluări
- IDSA Guideline PDFDocument80 paginiIDSA Guideline PDFArifHidayatÎncă nu există evaluări
- Hematological Disorders in Geriatric PatientsDocument18 paginiHematological Disorders in Geriatric PatientsAndre HawkÎncă nu există evaluări
- Oncologic EmergenciesDocument32 paginiOncologic EmergenciesColleen BernilÎncă nu există evaluări
- Pharmacovigilance: FROMDocument46 paginiPharmacovigilance: FROMmeyhal17Încă nu există evaluări
- Anaerobic Infections in HumansDe la EverandAnaerobic Infections in HumansSydney FinegoldEvaluare: 5 din 5 stele5/5 (1)
- Hemodialysis - Different AspectsDocument321 paginiHemodialysis - Different AspectsIndera VyasÎncă nu există evaluări
- BiodiversityDocument3 paginiBiodiversityNaresh KumarÎncă nu există evaluări
- Contingency Plan For Covid - 19Document12 paginiContingency Plan For Covid - 19anneÎncă nu există evaluări
- Antibiotika AminoglikosidaDocument12 paginiAntibiotika AminoglikosidaEVY INDRIYANIÎncă nu există evaluări
- Post Dural Puncture HeadacheDocument3 paginiPost Dural Puncture HeadachecignalÎncă nu există evaluări
- Agility & TestLine SmartKits - AN - 210x210mm - 3Document5 paginiAgility & TestLine SmartKits - AN - 210x210mm - 3Abdalazeez AlsayedÎncă nu există evaluări
- Chapter 1: Diphtheria: I. Disease DescriptionDocument10 paginiChapter 1: Diphtheria: I. Disease DescriptionTina MorleyÎncă nu există evaluări
- Foreskin Hygiene Fact Sheet Healthy Male 2019Document4 paginiForeskin Hygiene Fact Sheet Healthy Male 2019MADAGASCAR IDÎncă nu există evaluări
- Emerging Infectious Diseases Vol1no4Document56 paginiEmerging Infectious Diseases Vol1no4Jorge RodriguezÎncă nu există evaluări
- 02 Biological Classification Ncert Master For Neet-UgDocument5 pagini02 Biological Classification Ncert Master For Neet-UgRiya VermaÎncă nu există evaluări
- PH and Amine (Whiff) TESTDocument3 paginiPH and Amine (Whiff) TESTNovy Sylvia WardanaÎncă nu există evaluări
- 6th Grade Science Chapter 2 Viruses and BacteriaDocument42 pagini6th Grade Science Chapter 2 Viruses and Bacteriagurdeep singhÎncă nu există evaluări
- Widal TestDocument11 paginiWidal TestlialestariÎncă nu există evaluări
- FilariaDocument65 paginiFilarialunaghilvin2026Încă nu există evaluări
- Chapter 12 Micropara TransesDocument6 paginiChapter 12 Micropara TransesmarilexdomagsangÎncă nu există evaluări
- Pharmacy-Immunology 19: Primary & Acquired Immunodeficiency Saber HusseinDocument18 paginiPharmacy-Immunology 19: Primary & Acquired Immunodeficiency Saber Husseinmmoney1Încă nu există evaluări
- MCQs of Pharmacology Unit-2 (D) Anti-Viral DrugsDocument4 paginiMCQs of Pharmacology Unit-2 (D) Anti-Viral DrugsShayan ShayanÎncă nu există evaluări
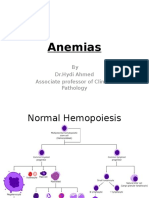
- Anemias (1) by DR - Hydi 3rd MBBS-2016Document63 paginiAnemias (1) by DR - Hydi 3rd MBBS-2016Suban GouseÎncă nu există evaluări
- Update On Environmental and Host Factors Impacting The RiskDocument10 paginiUpdate On Environmental and Host Factors Impacting The RiskNur SyahiraÎncă nu există evaluări
- Swine FluDocument22 paginiSwine FluNurhidayahÎncă nu există evaluări
- Reflection Paper About Covid-19Document1 paginăReflection Paper About Covid-19sei gosa100% (1)
- Neuromyelitis OpticaDocument1 paginăNeuromyelitis OpticaArun PonnaÎncă nu există evaluări
- Types of MicroorganismsDocument69 paginiTypes of MicroorganismshyvasÎncă nu există evaluări
- Predominant Bacteria Detected From The Middle Ear Fluid of Children Experiencing Otitis Media: A Systematic ReviewDocument3 paginiPredominant Bacteria Detected From The Middle Ear Fluid of Children Experiencing Otitis Media: A Systematic ReviewbosÎncă nu există evaluări
- Tropics - Infectious DiseasesDocument1.194 paginiTropics - Infectious DiseasesSabera KapasiÎncă nu există evaluări
- Cefazolin and Dextrose USPDocument3 paginiCefazolin and Dextrose USPYaleswari Hayu PertiwiÎncă nu există evaluări
- Soalan Pathology 3Document425 paginiSoalan Pathology 3muhammadridhwanÎncă nu există evaluări