Documente Academic
Documente Profesional
Documente Cultură
4 - Antimicrobial Efficacy of Chlorhexidine and Calcium Hydroxide Camphorated Paramonochlorophenol On Infected Primary Molars A Split-Mouth Randomized Clinical Trial
Încărcat de
kochikaghochi0 evaluări0% au considerat acest document util (0 voturi)
41 vizualizări10 paginilkbh
Titlu original
4 . Antimicrobial Efficacy of Chlorhexidine and Calcium Hydroxide Camphorated Paramonochlorophenol on Infected Primary Molars a Split-mouth Randomized Clinical Trial
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentlkbh
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
41 vizualizări10 pagini4 - Antimicrobial Efficacy of Chlorhexidine and Calcium Hydroxide Camphorated Paramonochlorophenol On Infected Primary Molars A Split-Mouth Randomized Clinical Trial
Încărcat de
kochikaghochilkbh
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 10
VOLUME 44 NUMBEP 2 FEBPUAPY 2013 113
QUI NTESSENCE I NTERNATI ONAL
ENDODONTONTICS/PEDIATRIC DENTISTY
this therapy does not eliminate all the bac-
teria, and these remaining microorganisms
may increase between appointments.
3-6
Calcium hydroxide [Ca(OH)
2
] has been
advocated for this purpose due to its anti-
resorptive activity,
7
tissue-dissolving
properties
8,9
and repair induction of hard
tissue formation.
10
The antibacterial proper-
ties are attributed to its elevated pH of
12.5,
11
which can lead to protein denatur-
ation and damage of the bacterial cytoplas-
mic membrane.
12
However, the initially high
pH of Ca(OH)
2
is buffered by the dentin,
13
limiting its antibacterial efcacy.
14
Booauso
of this limitation, its association with other
antimicrobial agents, such as camphorated
paramonochlorophenol (CPMC)
12
and
iodine compounds
15
has been proposed.
Phenolic compounds have potent antimi-
crobial activity, and scientic evidence sug-
gests that the Ca(OH)
2
/CPMC association
has a broader spectrum of action and
It has been demonstrated that bacteria and
their byproducts play an essential role in
the pathogenesis of pulpoperiapical dis-
eases,
1
and the success of endodontic
treatment depends on the reduction or
elimination of these bacteria.
2
Chemomechanical preparation has been
reported as an effective therapy in the
reduction of the number of microorganisms
isolated from the root canals
3-5
; however,
1
PhD Candidate, Postgraduate Program in Dentistry, Federal
University of Cear, Fortaleza, Brazil.
2
Associate Professor, Department of Pathology and Legal
Medicine, Federal University of Cear, Fortaleza, Brazil.
3
Associate Professor, Department of Clinical Dentistry, Federal
University of Cear, Fortaleza, Brazil.
Correspondence: Dr Cristiane S Roriz Fonteles, Unidade de
Pesquisas Clnicas/Universidade Federal do Cear, Laboratrio
de Farmacologia, Metablica e Fisiologia Celular, Avenida Jos
Bastos, 3390, sala 106, Caixa Postal 3229, CEP 60.436-160,
Fortaleza-Ce, Brazil. Email: cfontele@ufc.br
Antimicrobial efcacy of chlorhexidine and
calcium hydroxide/camphorated
paramonochlorophenol on infected primary
molars: A split-mouth randomized clinical trial
Ramille Arjo Lima DDS, MS
1
/Cibele Barreto Mano de Carvalho MD,
MS, PhD
2
/Thyciana Rodrigues Ribeiro DDS, MS
1
/Cristiane S Roriz
Fonteles DDS, MS, PhD
3
Objective: To compare via a split-mouth randomized clinical trial the efcacy of 1%
chlorhexidine gel, calcium hydroxide/camphorated paramonochlorophenol (Callen PMCC),
and a one-visit endodontic treatment against mutans streptococci and anaerobic bacteria
found in primary molars with necrotic pulps and to assess clinical success rates after 12
months. Method and Materials: Pre- and posttreatment intracanal samples were collected
from 37 teeth (from 21 children) for analysis of the number of mutans streptococci and
anaerobic bacteria. Clinical and radiographic criteria were analyzed to determine treat-
ment outcome. Results: Chlorhexidine gel signicantly reduced mutans streptococci levels
(P = .010), whereas Callen PMCC signicantly reduced the levels of anaerobic bacteria
(P = .002). No dioronoos in tno roduotion o mutans stroptoooooi (P = .187) and anaer-
obes (P = .564) were observed between groups. The clinical success rates were 85.71%
(Callen PMCC), 78.57% (chlorexidine gel), and 77.77% (one-visit treatment). Conclusion:
Teeth treated with Callen PMCC presented the highest clinical success rate. The 1%
chlorhexidine gel, as well as calcium hydroxide/camphorated paramonochlorophenol, pre-
sented limited efcacy in reducing bacteria from necrotic primary root canals.
(Quintessence Int 2013;44:113122)
Key words: calcium hydroxide, camphorated paramonochlorophenol, chlorhexidine,
primary molars, pulp necrosis
114 VOLUME 44 NUMBEP 2 FEBPUAPY 2013
QUI NTESSENCE I NTERNATI ONAL
Li ma et al
eliminates bacteria faster than mixtures of
Ca(OH)
2
with inert vehicles. Therefore,
CPMC should not be regarded as a vehicle
for the Ca(OH)
2
but an additional medica-
tion.
12
Iodophors are complexes of iodine
and solubilizing agents that act as reser-
voirs of active free iodine. The antimicrobial
action of iodine is rapid even at low concen-
trations.
15
Anotnor substanoo o intorost tnat nas
been extensively studied in endodontics is
chlorhexidine, a bisbiguanide with hydro-
philic and hydrophobic properties, and
antimicrobial activity against streptococci,
actinomyces, Gram-negative rods, yeasts,
total aerobes, and total anaerobes.
16,17
High
concentrations of chlorhexidine have an
immediate bactericidal effect, penetrating
the bacterial cell wall and leading to pre-
cipitation of the cytoplasm, whereas lower
concentrations are bacteriostatic in nature.
Its wide range of activity, in addition to other
favorable properties such as substantivity
18-20
and the ability to inhibit the adherence of
key pathogens,
21
justies the use of
onlornoxidino in dontistry. Altnougn provi-
ous works have studied these intracanal
medicaments in the endodontic treatment
of permanent teeth,
6,22-26
only a limited num-
ber of investigations are found in the litera-
ture regarding the use of these substances
in primary teeth with pulp necrosis.
27,28
Therefore, the aim of this split-mouth ran-
domized clinical trial was to compare the
efcacy of 1% chlorhexidine gel, Ca(OH)
2
/
CPMC (Callon PMCC |SS Wnito Artigos
Dentrios]
), and a one-visit endodontic
treatment (control group) against mutans
streptococci and anaerobic bacteria found
in primary molars with necrotic pulps.
METHOD AND MATERIALS
Subject recruitment
Patients from Pediatric Dental Clinic of the
Federal University of Cear (UFC), Fortaleza,
Brazil, soon botwoon Ootobor 2007 and
Novombor 2008 witn onio oomplaint o
toothache, molars with an associated stula
or abscess, or a specic referral for end-
odontic treatment were considered for this
study. A total o 21 noaltny, 4- to 8 yoar-old
children (37 teeth), with one (control) or two
(test groups) necrotic primary molars were
recruited for this study (from a total of
approximately 200 children screened to
participate in this clinical trial). Teeth were
considered necrotic when at least one of
the following criteria were present, second-
ary to dental caries: presence of an associ-
ated intraoral stula, gingival abscess,
spontaneous pain, radiographic evidence
of furcation involvement or periapical
pathology, or dental mobility associated
with one of the previously mentioned clinical
and/or radiographic signs and symptoms of
pulpal necrosis. Fourteen children (28 teeth)
were enrolled in groups 1 (Ca(OH)
2
/CPMC)
and 2 (chlorhexidine). These children had
at least two necrotic primary molars in dif-
ferent hemiarches with pulp necrosis (split-
moutn study). Nino onildron partioipatod as
a control group, which consisted of a one-
visit endodontic treatment. Two children
presented three primary molars with pulp
necrosis and therefore participated in the
three groups. Patients who received antibi-
otic therapy in the 3 months before study
initiation were excluded from this clinical
trial. No onildron woro romovod rom tno
study once the clinical trial began. This
study had a split-mouth design to reduce
the inuence of individual variables in treat-
mont outoomo (Fig 1). A lottory systom was
used to randomize the rst molar to be
treated in each participant and determine
the choice of treatment for the selected
tootn. Tnus, wnon troatmont A was solootod
for a molar on the right side of the mouth,
troatmont B would bo tno troatmont o
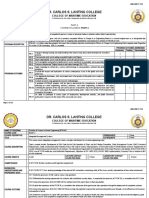
Fig 1 Split-mouth design used in the study.
Ca(OH)
2
/CPMC
CHX
VOLUME 44 NUMBEP 2 FEBPUAPY 2013 115
QUI NTESSENCE I NTERNATI ONAL
Li ma et al
choice for the molar on the left side. The
same researcher performed patient recruit-
ment and endodontic treatment. Study
approval by the Ethics Committee from the
Federal University of Cear Medical School
was obtained. Informed consents were
signed by patients legal guardians before
the children were enrolled in the study. This
study was also registered at www.clinical
trials.gov (idontihor: NCT00624572) as
Efcacy of Chlorhexidine as Intracanal
Medicament in Primary Teeth.
Endodontic treatment and
sampling procedures
Prior to treatment initiation, antisepsis of the
oral cavity was performed, local anesthesia
was administered, carious tissue was
removed, and access to the pulp chamber
was oroatod. Pubbor dam and an asoptio
technique were used throughout the end-
odontio troatmont. Ator oomploting aoooss,
the rst root canal sample (S1) was taken
by consecutively placing two sterile paper
points inside each root canal to a level
approximately 2 mm short of the root apex.
Ator 1 minuto, tno papor points woro
removed and placed in plastic tubes
(Eppendorf safe-lock tubes, Eppendorf)
containing 1 mL of reduced transport uid
(PTF). Subsoquontly, onomomoonanioal
preparation was performed with sequential
K-les (Dentsply Maillefer) and 1% sodium
nypoonlorito (NaOCl) solution. Ono millilitor
of this solution was used to rinse the canals
after each instrument, and canals were
dried with sterile paper points. Teeth select-
ed for the control group had a second root
canal sample (S2) withdrawn by following
the same protocol described for S1, where-
as in the Ca(OH)
2
/CPMC and chlorhexidine
groups, the intracanal medication was
placed as described. Teeth randomly
selected to receive medication 1 were
treated with Callen PMCC, and teeth select-
ed for medication 2 were treated with 1 mL
of 1% chlorhexidine gel (Farmafrmula)
(Table 1). Teeth treated with Ca(OH)
2
/
CPMC and chlorhexidine were provisionally
restored with glass-ionomer cement (Vitro
Fil, DFL ndustria o Comoroio S.A.). Botn
medications remained in the canals for 14
days. Ator tnis poriod, pationts roturnod to
the clinic for removal of the provisional res-
toration and remaining intracanal medica-
tion. The root canals were abundantly
irrigatod witn 1% NaOCl. Poot oanals woro
left empty, and provisional restorations were
roplaood. Ator 2 days, tno pationts roturnod
to the clinic and a second root canal sam-
plo was takon. Poot oanals woro lot ompty
for 2 more days to prevent a possible false
negative in the bacterial count as a result of
immodiato samplo oollootion. Ator S2 was
obtained, 17% ethylenediaminetetraacetic
aoid (EDTA) (Biodinmioa Qu|mioa o
Farmacutica) was left in the canals for 3
minutes for smear layer removal followed by
irrigation witn 3 mL o 1% NaOCl. Tnon, tno
canals were lled with zinc oxideeugenol
Table 1 Substances used as intracanal medications
Ingredients Weight
Callen PMCC
Calcium hydroxide 48.32 g/100mL
Paramonochlorophenol 0.72 g/100mL
Camphor 2.16 g/100mL
Chlorhexidine gel 1%
Chlorhexidine digluconate 20% 5 mL
Methylparaben 0.135 g
Propylparaben 0.015 g
Hydroxyethylcellulose 1.15 g
Stevioside 0.24 g
Glycerol 5 g
Water 100 g
116 VOLUME 44 NUMBEP 2 FEBPUAPY 2013
QUI NTESSENCE I NTERNATI ONAL
Li ma et al
paste. Once endodontic treatment was con-
cluded, all teeth were permanently restored
with stainless steel crowns. To conceal
patients identication from the researcher
responsible for sample collection, each
plastic tube
was identied with a number.
Booauso o dioronoos in tno oonsistonoy,
color, and odor of the two studied treat-
ments, as well as differences in the treat-
ment protocol used for the controls, this
was not a blinded study.
Microbiologic analysis
For microbiologic processing, samples
were transported to the laboratory within 30
minutes. Tubes were agitated for 1 minute,
and 10-fold serial dilutions p to 10
-5
were
made in prereduced anaerobically steril-
izod buorod salt solution (PBS). For tno
analysis of mutans streptococci, aliquots of
100 L from each dilution were spread onto
bacitracin Mitis-salivarius agar plates
(Difco), and they were microaerobically
incubated at 37C for 3 days. For the analy-
sis of anaerobic bacteria, 10 L of each
dilution was sproad onto Bruoolla Agar
platos (BBL Miorobiology Systom) supplo-
mented with 5% debrinated sheep blood
and 1% hemin/menadione in triplicates.
Bruoolla platos woro inoubatod anaorobi-
cally inside anaerobic jars (GasPak System,
BBL Miorobiology Systoms) at 37C or 7
days. Ator tno inoubation poriod, oolony-
forming units (CFUs) were counted, and
actual counts were calculated based on the
known dilution factors. Gram stain assay
was performed for each CFU.
Clinical outcome analysis
The clinical outcome (success or failure) of
endodontic treatment was also analyzed.
Failure of endodontic therapy was consid-
ered when a tooth showed, during the follow-
up period, associated stula, gingival
abscess, and/or mobility. Immediately and
30, 90, 120, 270, and 360 days after the
endodontic therapy, periapical radiography
was performed as a diagnostic adjunt for the
assessment of clinical success. The radio-
graphic criteria used to determine presence
or absence of treatment success were (1)
resolution of any preexistent pathologic
interradicular or periapical radiolucent areas,
(2) absence of newly formed postoperative
pathologic radiolucencies, (3) absence or
arrest of pathologic external root resorption,
(4) absence of internal root resorption, and
(5) normal eruption of the permanent suc-
oossor. Padiograpnio oxamination was por-
formed with the Spectro device (Dabi
Atlanto), oalibratod to oporato at 7 mA, 70
Kvp, and 0.5 seconds of lm exposure time.
Ultraspeed Kodak lms (Eastman Kodak)
and lm positioners (Han-shi) were used to
standardize the radiographs.
Statistical analysis
The Kruskal-Wallis test was used to com-
pare S1 and S2 values between groups and
to compare the reduction levels of anaero-
bic bacteria. Comparisons between S1 and
S2 within each group were made using the
Wilcoxon test. The level of signicance was
set at 5% (P < .05) for all analysis.
RESULTS
Considering 37 teeth included in this study,
64.86% (24 teeth) presented detectable
mutans streptococci levels in initial sam-
ples, whereas 94.59% (35 teeth) presented
detectable levels of anaerobic bacteria.
Comparisons of mutans streptococci counts
in S1 showed no signicant difference
between groups (P = .526). Similar results
were observed when comparing anaerobic
counts (P = .772). Ator troatmont (S2),
71.42%, 71.42%, and 77.77% of the teeth
from groups 1, 2, and control, respectively,
had detectable bacterial levels.
A statistioally signihoant dooroaso in
mutans streptococci counts was observed
in the chlorhexidine group (P = .010).
However, this decrease was not observed
with the Ca(OH)
2
/CPMC (P = .625) or con-
trol groups (P = .500) (Table 2). Treatment
with Ca(OH)
2
/CPMC demonstrated statisti-
cally signicant decrease in anaerobes
(P = .002). Decrease in the anaerobic
counts was also observed following
chlorhexidine (P = .080) and one-visit end-
odontic treatments (P = .156), but these
reductions were not statistically signicant
(Tablo 3). No statistioally signihoant dior-
ence in mutans streptococci reduction was
VOLUME 44 NUMBEP 2 FEBPUAPY 2013 117
QUI NTESSENCE I NTERNATI ONAL
Li ma et al
observed between groups (P = .187).
Comparisons between reduction levels of
anaerobic bacteria did not signicantly dif-
fer among the three groups (P = .564).
Gram-positive cocci were the most com-
monly observed bacterial morphotypes in
S1 (23 samples, 62.16%), followed by
Gram-negative (13 samples, 35.13%) and
Gram-positive (5 samples, 13.51%) bacilli
and Gram-negative cocci (3 samples,
8.10%). Ator troatmont witn Ca(OH)
2
/
CPMC, the presence of Gram-positive cocci
was only observed in 6 samples (42.85%),
followed by Gram-negative bacilli (5 sam-
ples, 35.71%), Gram-negative cocci (2
samples, 14.28%), and Gram-positive
bacilli (2 samples, 14.28%). For the
chlorhexidine group, a predominance of
Gram-negative bacilli was observed in S2
(6 samples, 42.85%), followed by Gram-
positive cocci (4 samples, 28.57%), Gram-
negative cocci (3 samples, 21.42%), and
Gram-positive bacilli (2 samples, 14.28%).
Gram-positive cocci were the most fre-
quently observed morphotypes (6 samples,
66.66%) in the control group (S2), whereas
Gram-negative cocci and Gram-positive
bacilli were each found in only one sample
(11.11%). Gram-negative bacilli were not
observed in the nal samples of this group.
Ator 12 montns o ollow-up, 30 o 37
treated teeth (81.08%) were considered
successful according to the previously
mentioned criteria. In contrast, treatment
failure was identied in 7 teeth (18.91%).
When only clinical criteria were considered,
after 12 months, 4 teeth presented treat-
ment failure, 3 of which were as a result of
the presence of mobility and one was a
result of the presence of pain. The most
commonly observed radiographic evidenc-
es of failure were the presence/persistence
of unresolved interradicular and periapical
radiolucies (n = 6) and pathologic external
root resorption (n = 3). In addition, 85.71%
(12 teeth) of teeth treated with Ca(OH)
2
/
CPMC, 78.57% (11 teeth) of teeth treated
with chlorhexidine, and 77.77% (7 teeth) of
the controls presented a successful out-
come. Of the 7 cases considered treatment
failures, 4 of them presented an increase
and 2 expressed no reduction in the anaer-
obic bacterial levels after treatment with
intracanal medication (Table 4).
Table 2 Mean (standard error) pre- and posttreatment mutans streptococci
counts (CFU/mL) for each group
Pretreatment Posttreatment P value
**
Ca(OH)
2
/CPMC 4.44 10
3
(2.59 10
3
) 5.84 10
4
(5.63 10
4
) .63
Chlorhexidine 3.34 10
5
(2.26 10
5
) 5.31 10
4
(5.28 10
4
) .010
***
Control group 1.40 10
3
(1.09 10
3
) 1.33 10
3
(1.10 10
3
) .5
P value
*
.53 .89
*
Kruskal-Wallis used for comparison,
**
Wilcoxon test used for comparison,
***
statistically signicant difference.
Table 3 Mean (standard error) pre- and posttreatment anaerobic bacterial counts
(CFU/mL) for each group
Pretreatment Posttreatment P value
**
Ca(OH)
2
/CPMC 2.71 10
5
(1.12x10
5
) 1.33 10
4
(9.37 10
3
) .002
***
Chlorhexidine 4.98 10
6
(4.74 10
6
) 9.67 10
4
(5.58 10
4
) .080
Control group 4.61 10
5
(4.42 10
5
) 1.85 10
4
(1.04x10
4
) .156
P value
*
.772 .541
*
Kruskal-Wallis used for comparison,
**
Wilcoxon test used for comparison,
***
statistically signicant difference.
118 VOLUME 44 NUMBEP 2 FEBPUAPY 2013
QUI NTESSENCE I NTERNATI ONAL
Li ma et al
DISCUSSION
To the authors knowledge, no previous
studies have identied an acceptable
threshold of intracanal microbial levels for
the establishment of a successful clinical
outcome in pulpectomized primary molars.
However, a signicantly higher success
rate has been observed in permanent teeth
with undetectable microbial levels prior to
root canal obturation, in comparison with
root canals with detectable concentrations
of bacteria.
29
Though undetectable bacteri-
al levels cannot always be translated as a
total absence of bacteria, nor can they
guarantee the lack of intracanal recoloniza-
tion, a negative culture prior to root canal
obturation should be the ultimate goal in
primary endodontics. Thus, intracanal med-
ication may act as a valuable aid in canal
disinfection.
3
In the present study, the pres-
ence of bacteria (mutans streptococci or
anaerobic bacteria) was observed in almost
all the S1 samples. In agreement with our
ndings, others have veried bacterial pres-
ence in 9299% of the samples.
23,30-32
Nogativo oulturos in tno initial or hnal sam-
ples do not imply sterility. This can be a
result of limitations of the experimental pro-
tocol, since the samples are collected from
only the main canal. Thus, other regions in
the root canal system that also have bacte-
ria may not be reached by sampling proce-
dures.
25
To minimize this limitation, in our
study, nal samples were obtained 48 hours
after intracanal medication removal.
Detectable mutans streptococci levels
were identied in several initial samples.
Cohen et al,
33
in a pioneer study, had veri-
ed the presence of Streptococcus salivari-
us in 70% of the samples. Marsh and
Largent
34
verified the presence of
Streptococcus in 82% of the specimens.
We believe that these ndings are justied
by the nonexistence, at that time, of correct
techniques for strict anaerobic culturing.
Poot oanal inootions aro polymiorobial in
nature, with prevalence of anaerobic micro-
organisms.
35
In recent studies of bacterial
prevalence in primary root canals with pulp
necrosis, mutans streptococci was found in
48.4%
30
and 30%
36
of the cases. Gomes et
al,
35
in a study using permanent teeth, veri-
fied the prevalence of 53.3% of
Streptococcus species, but mutans strepto-
cocci was observed in only 3.33% of their
study samples. Primary teeth have large
and ample pulp chambers that provide
more contact with saliva and the oral envi-
ronment after pulp exposure due to caries,
which differs from the permanent dentition.
Table 4 Clinical, radiographic, and microbiologic features associated with treat-
ment failures
Cases
of failure Group
Clinical
aspect Radiographic aspect
Anaerobic
reduction
S mutans
reduction
Bacterial morpho-
type at fnal sample
1 2 Mobility Pathologic root resorption/
periapical radiolucencies
0 12000 Gram-positive cocci
2 2 Mobility Periapical radiolucencies -267000 2460000 Gram-negative bacilli
3 1 Pain - -2300 -50 Gram-negative cocci/
Gram-negative bacilli/
Gram-positive cocci
4 1 - Pathologic root resorption/
periapical radiolucencies
1230000 137000 Gram-negative cocci
5 2 - Periapical radiolucencies -533000 0 Gram-negative cocci
6 3 Mobility Pathologic root resorption
Periapical radiolucencies
-12000 0 Gram-positive cocci/
Gram-positive bacilli
7 3 - Periapical radiolucencies 0 0 Gram-negative cocci
Group 1, Ca(OH)
2
/CPMC; Group 2, chlorhexidine; Group 3, control.
VOLUME 44 NUMBEP 2 FEBPUAPY 2013 119
QUI NTESSENCE I NTERNATI ONAL
Li ma et al
These anatomic characteristics may explain
the higher prevalence of mutans strepto-
cocci in primary root canals.
Ca(OH)
2
has been used worldwide as
intracanal medication. However, different
studies have attested to the inefcacy of
this medication in reducing microorganisms
from root canals, especially Enterococcus
faecalis, suggesting a possible benet from
the addition of substances that could
improve its antibacterial activity
.
6,14,37
Despite the excellent results previously
described with the combination of Ca(OH)
2
/
iodoform paste (Vitapex) as lling material
for endodontic treatment in primary teeth,
38
our choice of Ca(OH)
2
/CPMC was a result
of its superior antibacterial action
39
and
because previous evidence suggested that
this association may not render additional
antimicrobial action to what has already
been observed with Ca(OH)
2
alone.
40
In the
present study, Ca(OH)
2
/CPMC, associated
with chemomechanical procedures, signi-
cantly reduced anaerobic bacterial counts,
in agreement with previous works.
25,41,42
However, this association did not demon-
strate efcacy in mutans streptococci
reduction. The inefcacy of this intracanal
medication against mutans streptococci
may be attributed to factors such as neu-
tralization of Callen PMCC byproducts of
bacterial metabolism,
43
intrinsic bacterial
resistance, or alteration of the bacterial
expression of genes, allowing survival to
environment changes promoted by
Ca(OH)
2
.
12
Chlorhexidine gel at a 1% concentration
was tested because its viscous condition
allows good adaptation to the root canal
walls and it promotes a better disinfection
than the solution form.
44
We veried a
reduction in mutans streptococci counts
with the use of chlorhexidine as intracanal
medication and a trend toward a reduction
in the levels of anaerobic bacteria, in con-
trast with the results previously described
by other authors.
24,26,28
In the studies of
Wang et al
26
and Manzur et al,
24
chlorhexi-
dine was used in permanent teeth with a 2%
oonoontration. Ator intraoanal modioation
[Ca(OH)
2
/CPMC or chlorhexidine], 71.42%
of the root canals still presented anaerobic
bacteria, in contrast with other studies that
observed the presence of bacteria in
26.7%
22
and 26%
45
of root canals from per-
manent teeth.
The control group consisted of primary
molars that received one-visit endodontic
treatment, without intracanal medication. In
contrast to our ndings, Manzur et al
24
reported elimination of 66% of bacteria with
only chemomechanical preparation. Their
sample consisted of multi- and single-root-
ed permanent teeth and the use of a 1%
NaOCl solution or irrigation. Siquoira Junior
et al
25
veried 45.5% of bacterial elimination
after instrumentation and irrigation with
2.5% NaOCl in a samplo oonsisting o sin-
gle-rooted permanent teeth. Wang et al
26
observed bacterial elimination in 90.5% of
teeth after instrumentation and irrigation
with 2% chlorhexidine gel, using single- and
multirooted permanent teeth. Faria et al
27
veried microorganism elimination in 20%
of cases after instrumentation and irrigation
witn 2.5% NaOCl solution in primary inoi-
sors and molars. In the present study, 1%
NaOCl was usod as an irrigant solution and
the sample consisted solely of primary
molars. Peters et al
6
afrmed that the differ-
ences observed between the studies in the
reduced numbers of microorganisms may
be associated with the different concentra-
tions o NaOCl usod or irrigation. Divorsity
between samples (primary vs permanent
dentition, single- vs multirooted teeth) may
also explain these different outcomes. In the
present study, we did not observe a signi-
cant reduction in mutans streptococci or
anaerobe counts in the control group. Some
factors can explain the inefcacy of the
chemomechanical procedures in the elimi-
nation of microorganisms from root canals,
such as complex morphology (the solution
does not reach all parts of the canals) and
the presence of blood, exudates, and
remaining tissue.
46
In agreement with previous studies,
Gram-positive cocci were predominant
before and after treatment.
23,32,35,47
Aooording to Do Paz,
48
Gram-positive bac-
teria have the ability to change their nutri-
tional demands during periods of starvation
by limiting the amount of nutrient intake and
storing the energy used in metabolism,
allowing them to survive for long periods.
Some species, such as E faecalis, are
alkaline-resistant and can survive inside the
120 VOLUME 44 NUMBEP 2 FEBPUAPY 2013
QUI NTESSENCE I NTERNATI ONAL
Li ma et al
root canals, even after the use of Ca(OH)
2
as an intracanal medication. In addition,
species can adapt to alkaline environments
by maintaining homeostasis between intra-
and extracellular pH, and others can also
form biolms, protecting each other.
However, the observed predominance of
Gram-negative bacilli after chlorhexidine
treatment demonstrates its enhanced activ-
ity against Gram-positive bacteria.
49
Presently, ve cases considered clinical
failures showed the presence of Gram-
negative microorganisms in their nal sam-
ples. It is known that these microorganisms
generate toxic products that affect the api-
cal and periapical tissues, and their cell
walls contain endotoxins that consist of
lipopolysaccharides (LPS) that are of funda-
mental clinical importance because when
released either during bacterial growth, or
after cell death, they may activate the
release of bradykinin, a potent mediator of
pain and inammatory response, leading to
bone resorption at the apical region.
50
Aooording to Goorig and Camp,
50
for
endodontic treatment of primary teeth to be
considered successful, the treated tooth
should remain asymptomatic, with no mobil-
ity and free of any pathology. In the present
study, these factors were analyzed to
assess treatment outcome (success or fail-
ure), and radiographic characteristics such
as the appearance or progression of inter-
radicular and periapical pathological radio-
lucencies, and internal or external root
resorptions were also evaluated. Pulpectomy
success rates remained high throughout a
12-month follow-up period. Moskovitz et al
51
reported a success rate of 82% during a
6-month follow-up of 174 primary teeth end-
odontically treated in one visit. Similarly,
Trairatvorakul and Chunlasikaiwan
52
found
success in 85% of cases in one-visit end-
odontic treatments using zinc oxideeuge-
nol paste as lling material. Mortazavi and
Mesbahi
53
found 78.5% clinical/radiograph-
ic success rate using zinc oxideeugenol
paste, concurring with our ndings (77.7%).
Imura et al
54
found a 91.45% total success
rate (all types of treatments included) in a
study sample consisting of permanent teeth
treated in one or more sessions. The authors
also included cases of retreatment. Unlike
our study, a higher success rate in one-visit
treatments (94.75%) was observed, than
that performed in two or more sessions
(89.5%). Weiger et al
55
also found higher
success rates in permanent teeth treated in
one session (83.3%) compared to those
treated in two sessions (70.9%). The authors
used Ca(OH)
2
for 7 days, as intracanal
medication, differing from our study in which
chlorhexidine and Ca(OH)
2
associated with
CPMC were the treatment of choice.
CONCLUSION
In the present study, while chlorhexidine
demonstrated efcacy in mutans strepto-
cocci reduction, the Ca(OH)
2
/CPMC asso-
ciation was only effective in reducing
anaerobic bacteria, but presented the best
clinical results after a 12-month follow-up. In
spite of being predominantly anaerobic in
nature, the intracanal microbiota of the pri-
mary dentition has a mixed ora that must
be eliminated to assure successful end-
odontic therapy. Thus, 1% chlorhexidine
gel, as well as Ca(OH)
2
/CPMC demonstrat-
ed limited efcacy in the reduction of bacte-
ria from primary infected root canals. The
present results suggest that a possible
association between these two medications
in future studies may eliminate more ef-
ciently these bacteria.
ACKNOWLEDGMENT
The authors acknowledge the fnancial support of the
Fundao Cearense de Apoio ao Desenvolvimento
Cientfco e Tecnolgico (FUNCAP, Brazil) in the develop-
ment of this study.
REFERENCES
1. Kakehashi S, Stanley HR, Fitzgerard RJ. The efects of
surgical exposures of dental pups in germ-free and
conventional laboratory rats. Oral Surg 1965;20:
340-349.
VOLUME 44 NUMBEP 2 FEBPUAPY 2013 121
QUI NTESSENCE I NTERNATI ONAL
Li ma et al
2. Sjgren U, Figdor D, Persson S, Sundqvist G.
Infuence of infection at the time of root flling on
the outcome of endodontic treatment of teeth with
apical periodontitis. Int Endod J 1997;30:297-306.
3. Bystrm, A, Sundqvist G. Bacteriological evaluation
of the efcacy of mechanical root canal instrumen-
tation in endodontic therapy. Scand J Dent Res
1981;89:321-328.
4. Bystrm, A, Sundqvist G. Bacteriologic evaluation of
the efect of 0.5 percent sodium hypochlorite in
endodontic therapy. Oral Surg 1983;55:307-312.
5. Bystrm, A, Sundqvist G. The antibacterial action of
sodium hypoclorite and EDTA in 60 cases of end-
odontic therapy. Int Endod J 1985;18:35-40.
6. Peters LB, Van Winkelhof AJ, Buijs JF, Wesselink PR.
Efects of instrumentation, irrigation and dressing
with calcium hydroxide on infection in pulpless
teeth with peripical bone lesions. Int Endod J
2002;35:13-21.
7. Tronstad L. Root reabsortion etiology, terminology
and clinical manifestations. Endod Dental Traumatol
1988;4:241-252.
8. Hasselgren, G, Olsson B, Cvek M. Efects of calcium
hydroxide and sodium hypoclorite on the dissolu-
tion of necrotic porcine muscle tissue. J Endod
1988;14:125-127.
9. Andersen M, Lund A, Andreasen JO, Andreasen FM.
In vitro solubility of human pulp tissue in calcium
hydroxide and sodium hypochlorite. Endod Dent
Traumatol 1992;8:104-108.
10. Foreman PC, Barnes F. A review of calcium hydrox-
ide. Int Endod J 1990;23:283-297.
11. Heithersay GS. Calcium hydroxide in the treatment
of pulpless teeth with associated pathology. J Brit
Endod Soc 1975;8:74-92.
12. Siqueira Jnior JF, Lopes HP. Mechanisms of antimi-
crobial activity of calcium hydroxide: A critical
review. Int Endod J 1999;32:361-369.
13. Nerwich A, Fiqdor D, Messer HH. pH changes in root
dentine over a 4-weeks period following root canal
dressing with calcium hydroxide. J Endod 1993;19:
302-306.
14. Sathorn C, Parashos P, Messer H. Antibacterial ef-
cacy of calcium hydroxide intracanal dressing: A
systematic review and meta-analysis. Int Endod J
2007;40:2-10.
15. Athaniassiadis B, Abbott PV, Walsh, LJ. The use of
calcium hydroxide, antibiotics and biocides as anti-
microbial medicaments in endodontics. Aust Dent J
2007;52:64-82.
16. Russell AD. Chlorhexidine: Antibacterial action and
bacterial resistance. Infect 1986;14:212-215.
17. Mohammadi Z, Abbott, PV. The properties and
applications of chlorexidine in endodontics. Int
Endod J 2009;42:288-302.
18. Komorowski R, Grag H, Wu XY. Antimicrobial sub-
stantivity of chlorhexidine-treated bovine root den-
tin. J Endod 2000;26:315-317.
19. Basrani B, Santos JM, Tjrderhane L, et al. Substantive
antimicrobial activity in chlorhexidine-treated
human root dentin. Oral Surg Oral Med Oral Pathol
Oral Radiol Endod 2002;94:240-245.
20. Khademi, AA, Mohammadi Z, Havaee A. Evaluation
of the antibacterial substantivity of several intra-
canal agents. Aust Endod J 2006;32:112-115.
21. Grenier D. Efect of chlorhexidine on the adherence
properties of Porphyromonas gingivalis. J Clin
Periodontol 1996;23:140-142.
22. Barbosa CAM, Gonalves RB, Siqueira Jnior JF,
Uzeda M. Evaluation of the antibacterial activities of
calcium hydroxide, chlorhexidine, and camphorat-
ed paramonochlorophenol as intracanal medica-
ment--A clinical and laboratory study. J Endod
1997;23:297-300.
23. Chu FCF, Leung WK, Tsang PCS, Chow TW,
Samaranayake LP. Identifcation of cultivable micro-
organisms from root canals with apical periodonti-
tis following two-visit endodontic treatment with
antibiotics/steroid or calcium hydroxide dressings. J
Endod 2006;32:17-23.
24. Manzur A, Gonzales AM, Pozos, A, Herzog DS,
Friedman S. Bacterial quantifcation in teeth with
apical periodontitis related to instrumentation and
diferent intracanal medications: A randomized
clinical trial. J Endod 2007;33:114-118.
25. Siqueira Jnior JF, Magalhes KM, Ras IN. Bacterial
reduction in infected root canals treated with 2.5%
NaOCl as irrigant and calcium hydroxide/camphor-
ated paramonochlorophenol paste as an intracanal
dressing. J Endod 2007;33:667-672.
26. Wang CS, Arnold RR, Trope M, Teixeira FB. Clinical
efciency of 2% chlorhexidine gel in reducing intra-
canal bacteria. J Endod 2007;33:1283-1289.
27. Faria G, Nelson-Filho P, Freitas AC, Assed S, Ito IY.
Antibacterial efect of root canal preparation and
calcium hydroxide paste (calen) intracanal dressing
in primary teeth with apical periodontitis. J Appl
Oral Sci 2005;13:351-355.
28. na , Goculu D, Uzel A. Efcacy of various intra-
canal medicaments against Enterococcus faecalis in
primary teeth: An in vivo study. J Clin Pediatric Dent
2006;30: 233-236.
29. Sjgren U, Figdor D, Persson S, Sundqvist G.
Infuence of infection at the time of root flling on
the outcome of endodontic treatment of teeth with
apical periodontitis. Int Endod J 1997; 30:297-306.
30. Pazelli LC, Freitas AC, Ito IY, Souza-Gulgemin MCM,
Medeiros AS, Nelson-Filho P. Prevalence of microor-
ganisms in root canals on human deciduous teeth
with necrotic pulp and chronic periapical lesions.
Pesquisa Odontolgica Brasileira 2003;17:367-371.
31. Kvist T, Molander A, Dahln G, Reit C. Microbiological
evaluation of one- and two visit endodontic treat-
ment of teeth with apical periodontitis: A random-
ized, clinical trial. J Endod 2004;30:572-576.
122 VOLUME 44 NUMBEP 2 FEBPUAPY 2013
QUI NTESSENCE I NTERNATI ONAL
Li ma et al
32. Ferrari PHP, Cai S, Bombana AC. Efect of endodon-
tic procedures on enterococci, enteric bacteria and
yeasts in primary endodontic infections. Int Endod J
2005;38:372-380.
33. Cohen MM., Joress SM, Calisti LP. Bacteriologic
study of infected deciduous molars. Oral Surg
1960;13:1382-1386.
34. Marsh SJ, Largent MD. A bacteriological study of the
pulp canals of infected primary molars. J Dent Child
1967;34:460-470.
35. Gomes BPFA, Pinheiro ET, Gad-Neto CR, et al.
Microbiological examination of infected dental root
canals. Oral Microbiol Immunol 2004;19:71-76.
36. Silva LAB, Nelson-Filho P, Faria G, Souza-Gulgemin
MCM, Ito IY. Bacterial profle in primary teeth with
necrotic pulp and periapical lesions. Braz Dent J
2006;17:144-148.
37. Heling I, Steinberg D, Kenig S, Gavrilovich I, Sela MN,
Friedman M. Efcacy of a sustained-release device
containing chlorexidine and Ca(OH)
2
in preventing
secondary infection of dentinal tubules. Int Endod J
1992;25:20-24.
38. Nakornchai S, Banditsing P, Visetratana N. Clinical
evaluation of 3Mix and Vitapex as treatment
options for pulpally involved primary molars. Int J
Paediatr Dent 2010;20:214221.
39. Tchaou WS, Turng BF, Minah GE, Coll JA. In vitro
inhibition of bacteria from root canals of primary
teeth by various dental materials. Pediatr Dent
1995;17:351-355.
40. Estrela C, Estrela CRA, Hollanda ACB, Decurcio DA,
Pcora JD. Infuence of iodoform on antimicrobial
potential of calcium hydroxide. J Appl Oral Sci
2006;14:33-37.
41. Siqueira Jnior JF, Uzeda, M. Desinfection by calci-
um hydroxide pastes of dentinal tubules infected
with two obligate and one facultative anaerobic
bacteria. J Endod 1996;22:674-676.
42. Siqueira Jnior JF, Uzeda M. Intracanal Medicaments:
Evaluation of the antibacterial efects of chlorhexi-
dine, metronidazole, and calcium hydroxide associ-
ated with three vehicles. J Endod 1997;23:16-19.
43. Nakajo K, Nakazawa F, Iwaku M, Hoshino E. Alkali-
resistant bacteria in root canal systems. Oral
Microbiol Immunol 2004;19:390-394.
44. Ferraz CC, Gomes BP, Zaia AA, Teixeira FB, Souza-
Filho FJ. In vitro assessment of the antimicrobial
action and the mechanical ability of chlorhexidine gel
as an endodontic irrigant. J Endod 2001;32:452-455.
45. Reit C, Dahln G. Decision making analysis of end-
odontic treatment strategies in teeth with apical
periodontitis. Int Endod J 1988;21:291-299.
46. Soares JA. Microbiota dos canais radiculares asso-
ciados s leses periapicais crnicas e sua sig-
nifcncia clnica. JBE 2002;3:106-117.
47. Sundqvist G. Taxonomy, ecology, and pathogenici-
ty of the root canal fora. Oral Surg Oral Med Oral
Pathol 1994;78:522-530.
48. De Paz LC. Gram-positive organisms in endodontic
infections. Endod Topics 2004;9:79-96.
49. Gomes BPFA, Lilley JD, Drucker DB. Clinical signif-
cance of dental root canal microfora. J Dent
1996;24:47-55.
50. Goerig AC, Camp JH. Root canal treatment in pri-
mary teeth: A review. Pediatr Dent 1983;5:33-37.
51. Moskovitz M, Sammara E, Holan G. Success rate of
root canal treatment in primary molars. J Dent
2005;33:41-47.
52. Trairatvorakul C, Chunlasikaiwan S. Success of pulp-
ectomy with zinc oxide-eugenol vs calcium hydrox-
ide/iodoform paste in primary molars: A clinical
study. Pediatr Dent 2008;30:303-308.
53. Mortazavi M, Mesbahi M. Comparison of zinc oxide
and eugenol, and Vitapex for root canal treatment
of necrotic primary teeth. Int J Paediatr Dent
2004;14:417-424.
54. Imura N, Pinheiro ET, Gomes BP, Zaia AA, Ferraz CC,
Souza-Filho FJ. The outcome of endodontic treat-
ment: A retrospective study of 2000 cases perfomed
by a specialist. J Endod 2007;33:1278-1282.
55. Weiger R, Rosendahl R, Lst C. Infuence of calcium
hydroxide intracanal dressings on the prognosis of
teeth with endodontically induced periapical
lesions. Int Endod J 2000;33:219-226.
S-ar putea să vă placă și
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Shotcreting in Australia 2010Document84 paginiShotcreting in Australia 2010Vedad TerzicÎncă nu există evaluări
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Specimen 1 ValuationDocument17 paginiSpecimen 1 ValuationLight BearerÎncă nu există evaluări
- Preparation and Evaluation of Orthodontic Setup PDFDocument20 paginiPreparation and Evaluation of Orthodontic Setup PDFLiezty VioLen'sÎncă nu există evaluări
- Modeling of Soil-Structure Interaction as Finite Element Using SAP2000Document5 paginiModeling of Soil-Structure Interaction as Finite Element Using SAP2000Tariq MahmoodÎncă nu există evaluări
- Antigen-Presentation and The Role of Dendritic Cells in PeriodontitisDocument23 paginiAntigen-Presentation and The Role of Dendritic Cells in PeriodontitiskochikaghochiÎncă nu există evaluări
- Peri-Implant Bone Loss As A Function of Tooth-Implant DistanceDocument7 paginiPeri-Implant Bone Loss As A Function of Tooth-Implant DistancekochikaghochiÎncă nu există evaluări
- Per I Tons IllerDocument25 paginiPer I Tons IllerkochikaghochiÎncă nu există evaluări
- 3mespe Cements v5Document12 pagini3mespe Cements v5kochikaghochiÎncă nu există evaluări
- 11Document16 pagini11kochikaghochiÎncă nu există evaluări
- Ijp 18 5 Elmowafy 13Document2 paginiIjp 18 5 Elmowafy 13kochikaghochiÎncă nu există evaluări
- 14Document13 pagini14kochikaghochiÎncă nu există evaluări
- Cytokine Gene Polymorphism and Immunoregulation in Periodontal DiseaseDocument25 paginiCytokine Gene Polymorphism and Immunoregulation in Periodontal DiseasekochikaghochiÎncă nu există evaluări
- 15Document9 pagini15kochikaghochiÎncă nu există evaluări
- Ijp 18 5 Editorial 1Document3 paginiIjp 18 5 Editorial 1kochikaghochiÎncă nu există evaluări
- Ijp 18 5 Hassel 11Document5 paginiIjp 18 5 Hassel 11kochikaghochiÎncă nu există evaluări
- 10Document10 pagini10kochikaghochiÎncă nu există evaluări
- Ijp 18 5 Mack 9Document6 paginiIjp 18 5 Mack 9kochikaghochiÎncă nu există evaluări
- Ijp 18 5 Grandini 7Document6 paginiIjp 18 5 Grandini 7kochikaghochiÎncă nu există evaluări
- Ijp 18 5 Coward 8Document9 paginiIjp 18 5 Coward 8kochikaghochiÎncă nu există evaluări
- Effect of Original Water Content in Acrylic Resin On Processing ShrinkageDocument2 paginiEffect of Original Water Content in Acrylic Resin On Processing ShrinkagekochikaghochiÎncă nu există evaluări
- 6Document15 pagini6kochikaghochi100% (1)
- Ijp 18 5 Botelho 2Document6 paginiIjp 18 5 Botelho 2kochikaghochiÎncă nu există evaluări
- 4Document18 pagini4kochikaghochiÎncă nu există evaluări
- 5Document13 pagini5kochikaghochiÎncă nu există evaluări
- 8Document15 pagini8kochikaghochiÎncă nu există evaluări
- 9Document14 pagini9kochikaghochiÎncă nu există evaluări
- 7Document8 pagini7kochikaghochiÎncă nu există evaluări
- 3Document10 pagini3kochikaghochiÎncă nu există evaluări
- The Use of Oral Implants in Compromised Patients: Daniel Van SteenbergheDocument3 paginiThe Use of Oral Implants in Compromised Patients: Daniel Van SteenberghekochikaghochiÎncă nu există evaluări
- Preoperative Radiologic Planning of Implant Surgery in Compromised PatientsDocument14 paginiPreoperative Radiologic Planning of Implant Surgery in Compromised PatientskochikaghochiÎncă nu există evaluări
- 14Document10 pagini14kochikaghochiÎncă nu există evaluări
- 12Document13 pagini12kochikaghochiÎncă nu există evaluări
- Diagnosis of Periodontal Manifestations of Systemic DiseasesDocument13 paginiDiagnosis of Periodontal Manifestations of Systemic DiseaseskochikaghochiÎncă nu există evaluări
- 11Document39 pagini11kochikaghochiÎncă nu există evaluări
- ASSIGNMENTDocument10 paginiASSIGNMENTKoleen Lopez ÜÎncă nu există evaluări
- Psychoacoustics: Art Medium SoundDocument3 paginiPsychoacoustics: Art Medium SoundTheodora CristinaÎncă nu există evaluări
- Ego7 Manual enDocument76 paginiEgo7 Manual ensullivanj69Încă nu există evaluări
- Misamis Occidental Plans to Protect Aquamarine ResourceDocument8 paginiMisamis Occidental Plans to Protect Aquamarine ResourcejelosalisaliÎncă nu există evaluări
- A7670 Series Hardware Design v1.03Document69 paginiA7670 Series Hardware Design v1.03Phạm NamÎncă nu există evaluări
- 800-40 Suspencion ChalmersDocument7 pagini800-40 Suspencion ChalmersJhonatan Velasquez CastellanosÎncă nu există evaluări
- Water System BOQ 16.12.2023 R0Document144 paginiWater System BOQ 16.12.2023 R0moinu85Încă nu există evaluări
- Railway Electrification Projects Budget 2019-20Document9 paginiRailway Electrification Projects Budget 2019-20Muhammad Meraj AlamÎncă nu există evaluări
- ArtsDocument5 paginiArtsRhovi Christine AbandoÎncă nu există evaluări
- AkzoNobel-Trigonox 239Document6 paginiAkzoNobel-Trigonox 239Wafa AjiliÎncă nu există evaluări
- P198 Software and Atlases For Evaluating Thermal Bridges 0Document10 paginiP198 Software and Atlases For Evaluating Thermal Bridges 0cm08909Încă nu există evaluări
- TacoDocument12 paginiTaconguyennhan2190Încă nu există evaluări
- Briefing Paper No 4 CV Electrification 30 11 17 PDFDocument5 paginiBriefing Paper No 4 CV Electrification 30 11 17 PDFAlex WoodrowÎncă nu există evaluări
- Colistimethate Sodium 1 Million I.U. Powder For Solution For Injection - Colistin - (Emc)Document8 paginiColistimethate Sodium 1 Million I.U. Powder For Solution For Injection - Colistin - (Emc)hakim shaikhÎncă nu există evaluări
- March 17, 2016 Strathmore TimesDocument24 paginiMarch 17, 2016 Strathmore TimesStrathmore TimesÎncă nu există evaluări
- Unit 5 Project ManagementDocument19 paginiUnit 5 Project ManagementYashu RajÎncă nu există evaluări
- Medulla Oblongata Nucleus (Final)Document7 paginiMedulla Oblongata Nucleus (Final)Hassan.shehri100% (3)
- Torn MeniscusDocument10 paginiTorn MeniscusKrystal Veverka100% (3)
- Boston Acoustic PDFDocument12 paginiBoston Acoustic PDFAdam StarkÎncă nu există evaluări
- TRUKE C20-33(35)L CLARK ENGINE PARTS LISTDocument2 paginiTRUKE C20-33(35)L CLARK ENGINE PARTS LISTРоман ПетровÎncă nu există evaluări
- Answer Sheet FINAL LipidDocument3 paginiAnswer Sheet FINAL LipidFaridah MagumparaÎncă nu există evaluări
- Dr. Carlos S. Lanting College: College of Maritime EducationDocument14 paginiDr. Carlos S. Lanting College: College of Maritime EducationJeynard Moler J. TanÎncă nu există evaluări
- National Leprosy Control Program For CHNDocument18 paginiNational Leprosy Control Program For CHNNaomi Cyden YapÎncă nu există evaluări
- Kinematics Problem SetDocument1 paginăKinematics Problem SetMohammad JubranÎncă nu există evaluări
- October 14, 2011 Strathmore TimesDocument28 paginiOctober 14, 2011 Strathmore TimesStrathmore TimesÎncă nu există evaluări
- Advanced Technologies of CDQ Plant Advanced Technologies of CDQ PlantDocument12 paginiAdvanced Technologies of CDQ Plant Advanced Technologies of CDQ Plant조기현Încă nu există evaluări