Documente Academic
Documente Profesional
Documente Cultură
Allergic Contact Stomatitis Case Report and Review
Încărcat de
Virma PutraTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Allergic Contact Stomatitis Case Report and Review
Încărcat de
Virma PutraDrepturi de autor:
Formate disponibile
458 Indian Journal of Clinical Practice, Vol. 22, No.
9, February 2012
Allergic Contact Stomatitis: A Case Report and
Review of Literature
P LOKESH, T ROOBAN, JOSHUA ELIZABETH, K UMADEVI, K RANGANATHAN
A
llergic contact stomatitis is a rare disorder,
which most clinicians are not familiar with.
A wide variety of substances are known to
elicit adverse oral mucosal reactions. Flavoring agents,
preservatives and dental materials are the most common
causes of allergic/hypersensitivity reactions related to
oral mucosa. Flavoring agents and preservatives have
been used widely in commercially available personal
hygiene products and foods, thereby increasing the risk
hypersensitivity reactions.
Previous exposure with an allergen is essential for
diagnosis of allergic contact stomatitis. Sensitization
usually occurs through contact of allergen with the oral
mucosa. Rarely, sensitization may also occur by contact
of allergen with skin. Memory T cells are activated soon
afer the initial exposure. On re-exposure to the same
allergen, a type IV hypersensitivity reaction occurs. This
reaction may be delayed by at least 48 hours and the
clinical presentation may vary depending on the severity
of the reaction.
CASE REPORT
A 26-year-old dental postgraduate student presented
with a complaint of pain and difuse intraoral
erythematous lesions for the past three days. The patient
frst experienced roughness and discomfort in the lef
Dept. of Oral and Maxillofacial Pathology,
Ragas Dental College and Hospital, Chennai
buccal mucosa four days ago. The following day he
developed erythematous lesions and pain in the lef
buccal mucosa, followed by lesions on the anterior part
of ventral tongue, sof palate, right buccal mucosa and
lower labial mucosa. Difculty in brushing, speech and
burning sensation while eating were experienced, for
which 2% benzocaine gel was applied 3-4 times every
day before food intake.
Intraoral examination revealed carious 26, glass
ionomer cement (GIC) Class I restoration in 46,
buccally inclined 18 and 28. Difuse erythema involving
the whole of sof palate, without extension on to the
hard palate was seen (Fig. 1). Ventral surface of anterior
tongue was bright red in color with few small
whitish plaques, suggestive of necrosis (Fig. 2).
Lower labial mucosa exhibited irregular zones
of erythema. Large oval to irregular bright red
patches surrounded by whitish edematous zones
were seen on buccal mucosa, extending some
distance into the vestibule on both right (Fig. 3) and lef
side (Fig. 4). The keratinized mucosa of the hard palate,
gingiva and dorsum of the tongue was not involved.
Further questioning did not reveal history of any
change or use of oral hygiene products, recent dental
treatment or drug intake. Eventually, patient did recall
an episode of having food at a restaurant 2-3 days
before developing the lesions. Patient also gave a
history of episodes of recurrent minor aphthous ulcers.
One such episode occurred about two years ago and
was characterized by multiple painful oral lesions,
ABSTRACT
Allergic contact stomatitis is a well-recognized entity, which may be easily overlooked by the clinician since its signs and
symptoms are similar to various other oral lesions. Accurate diagnosis warrants adequate treatment that will help in providing
prompt relief and will also prevent further recurrences. We present a case report of a 27-year-old South Indian male student,
who presented with multiple erythematous erosions involving much of the nonkeratinized oral mucosa. History revealed that
there was a previous episode of a similar lesion, associated with intake of food with favoring agents. Based on the history
and clinical features, we arrived at a diagnosis of allergic contact stomatitis and successfully treated the lesions with topical
and systemic antihistamines.
Keywords: Allergic contact stomatitis, oral mucosa, antihistamines
CASE REPORT
CASE REPORT
459 Indian Journal of Clinical Practice, Vol. 22, No. 9, February 2012
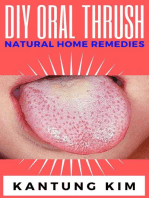
Figure 1. Difuse erythema of sof palate.
Figure 2. Erosive lesions on ventral surface of tongue.
which developed soon afer intake of specifc food,
which the patient has been avoiding since then. Based
on the history and clinical features, a provisional
diagnosis of allergic stomatitis was made.
MANAGEMENT
Patient was advised to avoid foods with preservatives
and favoring agents. Cetirizine hydrochloride 10 mg
tablet hs, 5 ml of diphenhydramine hydrochloride
syrup mixed with equal amount of an antacid
liquid in a swish and swallow method 3-4 times
daily were prescribed to alleviate the symptoms.
During the follow-up visit, four days later, most of
the initial lesions had healed without any scarring
(Figs. 5-8). A mild increase in the pigmentation was
seen on the buccal mucosa. Two new lesions, which
were not present during the initial examination, were
seen on both the lef and right sides of buccal mucosa,
adjacent to the upper canine and premolars (Figs. 9
and 10). These lesions were erythematous areas,
2 1 cm in size with whitish necrotic plaques. Patient
was advised to continue the same medications for three
more days, following which all the oral lesions healed
completely.
DISCUSSION
Contact stomatitis is an infammation of the oral mucosa
caused by external substances. It can be caused by a
Figure 3. Erythematous lesions on right buccal mucosa.
Figure 4. Erythematous lesions on lef buccal mucosa.
CASE REPORT
460 Indian Journal of Clinical Practice, Vol. 22, No. 9, February 2012
Figure 7. Right buccal mucosa - 4 days afer therapy.
Figure 8. Lef buccal mucosa - 4 days afer therapy.
variety of substances, which can either act as irritant
or allergic agents. These substances include dental
materials, preservatives and favoring agents in foods
or oral hygiene products. Oral mucosa is less commonly
prone to contact allergic reactions, when compared to
skin, though the later is exposed to a wide variety of
antigenic stimuli. This can be atributed to the various
biologic and physiologic diferences between the two.
Saliva acts as a solvent that solubilizes, dilutes and
also starts digesting potential allergens and helps
to wash them there by limiting the duration and
number of molecules that contact oral mucosa. Limited
keratinization makes hapten binding more difcult
and the limited number of antigen presenting cells
in the oral mucosa decreases the chance of antigen
recognition. Irritants and allergens that do contact the
oral mucosa are removed more quickly because of
higher vascularity and faster epithelial renewal rates
than in keratinized skin.
Balsam of peru, cinnamon, cinnamic aldehyde,
menthol, peppermint and eugenol are some of the
common oral favoring allergens.
These reactions can be either acute or chronic.
Clinical presentations vary based on the nature of
reaction, type of allergen site and duration of contact.
Patients with acute lesions may present with burning
or redness. Vesicles are rarely seen and if present
rupture in a short while afer formation. Some patients
Figure 5. Sof palate - 4 days afer therapy.
Figure 6. Ventral surface of tongue - 4 days afer therapy.
CASE REPORT
461 Indian Journal of Clinical Practice, Vol. 22, No. 9, February 2012
Figure 9. Lesions on right buccal mucosa, during review
visit.
Figure 10. Lesions on lef labial vestibule, during review
visit.
may experience edema, itching or stinging sensation.
Contact allergy lesions occur directly at the site of
exposure to the causative agent. Acute lesions develop
soon afer antigenic exposure; diagnosis of these may
be straightforward since a cause-and-efect relationship
can be easily established.
Chronic lesions typically present as areas of erythema,
edema, desquamation and occasionally ulceration. In
addition, allergic contact stomatitis can also present
as erosions with rough surface and irregular borders,
ofen surrounded by a red halo. These lesions may
be indistinguishable from aphthous ulcers and other
Table 1. Differential Diagnoses
Pemphigus Lupus erythematosus
Pemphigoid Syphilis
Lichen planus Friction-induced
Drug reactions Contact stomatitis
Erythema multiforme Erythematous candidiasis
lesions during clinical examination. Erosions can also
be caused by trauma arising from friction between
the teeth or irregular dental restorations. Burns from
hot foods, radiation and caustic chemicals also cause
similar erosions.
Hence, it is essential to elicit a thorough history and
exclude other pathosis presenting with similar lesions
clinically (Table 1). Patch testing of oral mucosa is
difcult and may yield false-negative results. Some
common conditions which can present as erosive
lesions in the oral mucosa are listed in Table 1.
Identifcation and elimination of the allergen that
initiated the reaction is essential to treat the condition,
as well as to prevent recurrences. If an association is
not established, cutaneous patch testing may be useful.
Lesions respond well once the antigenic stimulus
is eliminated. Antihistamines, topical anesthetics
and topical corticosteroids are the commonly used
pharmacological agents. Use of antihistamine
suspensions in a swish and swallow method provide
the advantage of both local and systemic action. Some
of these agents may not be tolerable when there is a
mucosal breach. Hence, a well-tolerated, favored
antacid was included in the prescription.
CONCLUSION
Allergic contact stomatitis is a well-recognized entity,
the incidence of which could be far more than that
reported. Clinical presentation and histopathologic
features are not always specifc. Hence, a high-degree
of suspicion and careful history taking to establish
a cause-and-efect relationship is essential. Biopsy
fndings may be confrmatory but not always essential.
Health practitioners should consider contact allergic
stomatitis in the diferential diagnosis of nonspecifc
oral lesions so as to provide proper treatment and
avoid recurrences.
CASE REPORT
462 Indian Journal of Clinical Practice, Vol. 22, No. 9, February 2012
Consent
Writen informed consent was obtained from the
patient for publication of this case report and
accompanying images.
Competing Interests
The authors declare that they have no competing
interests.
Acknowledgments
We thank our Principal, Dr S Ramachandran, for
encouraging the publication of this case report and
Dr Yakob Martin, for the images.
SUGGESTED READING
LeSueur BW, Yiannias JA. Contact stomatitis. Dermatol
Clin 2003;21(1):105-14, vii.
Tosti A, Piraccini BM, Peluso AM. Contact and irritant
stomatitis. Semin Cutan Med Surg 1997;16(4):314-9.
Ophaswongse S, Maibach HI. Allergic contact cheilitis.
Contact Dermatitis 1995;33(6):365-70.
1.
2.
3.
Nevelle B, Damm D, Allen C, Bouquot J. Oral and
Maxillofacial Pathology. 3rd edition.
Ostman PO, Anneroth G, Skoglund A. Amalgam-
associated oral lichenoid reactions. Clinical and histologic
changes afer removal of amalgam fllings. Oral Surg
Oral Med Oral Pathol Oral Radiol Endod 1996;81(4):
459-65.
Kowitz G, Jacobson J, Meng Z, Lucatorto F. The efects of
tartar-control toothpaste on the oral sof tissues. Oral Surg
Oral Med Oral Pathol 1990;70(4):529-36.
Tremblay S, Avon SL. Contact allergy to cinnamon: case
report. J Can Dent Assoc 2008;74(5):445-61.
De Rossi SS, Greenberg MS. Intraoral contact allergy:
a literature review and case reports. J Am Dent Assoc
1998;129(10):1435-41.
Raap U, Stiesch M, Reh H, Kapp A, Werfel T. Investigation
of contact allergy to dental metals in 206 patients.
Contact Dermatitis 2009;60(6):339-43.
Torgerson RR, Davis MD, Bruce AJ, Farmer SA, Rogers
RS 3rd. Contact allergy in oral disease. J Am Acad
Dermatol 2007;57(2):315-21.
4.
5.
6.
7.
8.
9.
10.
S-ar putea să vă placă și
- Allergic Contact Stomatitis: A Case Report and Review of LiteratureDocument5 paginiAllergic Contact Stomatitis: A Case Report and Review of LiteratureFajar RamadhanÎncă nu există evaluări
- Allergicstomatitis 2012Document6 paginiAllergicstomatitis 2012Agustine Hanafi PutriÎncă nu există evaluări
- Stomatitis Allergy ToothpasteDocument3 paginiStomatitis Allergy ToothpastemochbryllianÎncă nu există evaluări
- Treatment of Lingual Traumatic Ulcer Accompanied With Fungal InfectionsDocument5 paginiTreatment of Lingual Traumatic Ulcer Accompanied With Fungal InfectionsYuganya SriÎncă nu există evaluări
- A Review of Drug-Induced Oral ReactionsDocument19 paginiA Review of Drug-Induced Oral ReactionsSri RahayuÎncă nu există evaluări
- Clinical: Contact Allergy To Cinnamon: Case ReportDocument4 paginiClinical: Contact Allergy To Cinnamon: Case ReportGrace Victoria OctavianusÎncă nu există evaluări
- Drug-Induced Erythema Multiforme Case Studies and Literature ReviewDocument5 paginiDrug-Induced Erythema Multiforme Case Studies and Literature ReviewfersaÎncă nu există evaluări
- Oral Erythroplakia - A Case Report: Mahendra Patait, Urvashi Nikate, Kedar Saraf, Priyanka Singh and Vishal JadhavDocument4 paginiOral Erythroplakia - A Case Report: Mahendra Patait, Urvashi Nikate, Kedar Saraf, Priyanka Singh and Vishal JadhavhelmysiswantoÎncă nu există evaluări
- 15 D16 298 Popovska MirjanaDocument5 pagini15 D16 298 Popovska MirjanaVera Radojkova NikolovskaÎncă nu există evaluări
- Stomatitis Venenata: A Rarity: Case ReportDocument2 paginiStomatitis Venenata: A Rarity: Case ReportJoel Nathaniel Richard JosephÎncă nu există evaluări
- Referat 1Document3 paginiReferat 1Tupicica GabrielÎncă nu există evaluări
- A Case Report On Symptomatic Primary Herpetic Gingivostomatitis (New)Document4 paginiA Case Report On Symptomatic Primary Herpetic Gingivostomatitis (New)Annisa MardhatillahÎncă nu există evaluări
- Oral MedicineDocument4 paginiOral MedicineRizki Dwi LestariÎncă nu există evaluări
- Denture Stomatitis CausesDocument4 paginiDenture Stomatitis CausesDentist HereÎncă nu există evaluări
- Desquamative GingivitisDocument6 paginiDesquamative Gingivitissidra malikÎncă nu există evaluări
- 657-Article Text-1074-1-10-20221221Document3 pagini657-Article Text-1074-1-10-20221221putraÎncă nu există evaluări
- Erythema Multiforme: A Case Series and Review of Literature: November 2018Document8 paginiErythema Multiforme: A Case Series and Review of Literature: November 2018Nurlina NurdinÎncă nu există evaluări
- Denture Stomatitis 3Document4 paginiDenture Stomatitis 3Utami MayasariÎncă nu există evaluări
- Oral Pemphigus Vulgaris: A Case Report With Review of The LiteratureDocument4 paginiOral Pemphigus Vulgaris: A Case Report With Review of The LiteratureDhilah Harfadhilah FakhirahÎncă nu există evaluări
- Chem Ical BurnDocument3 paginiChem Ical BurnvasabakaÎncă nu există evaluări
- Tugas Jurnal Blok 12Document7 paginiTugas Jurnal Blok 12Astasia SefiwardaniÎncă nu există evaluări
- Oral Complications of Cancer TreatmentDocument68 paginiOral Complications of Cancer TreatmentFarisha RasheedÎncă nu există evaluări
- Hypersensitivity in DentistryDocument10 paginiHypersensitivity in DentistryCasperock CasperockÎncă nu există evaluări
- 5 курс Тема 12. (English translation)Document8 pagini5 курс Тема 12. (English translation)Viktoriya GorobinskayaÎncă nu există evaluări
- Lichen Planus Article PDFDocument3 paginiLichen Planus Article PDFSuresh KumarÎncă nu există evaluări
- Drug Induced StomatitisDocument4 paginiDrug Induced StomatitisRamadhani P SalichaÎncă nu există evaluări
- Stomatitis Medicamentosa Case Report SummaryDocument5 paginiStomatitis Medicamentosa Case Report Summaryathika yuraseptiÎncă nu există evaluări
- 1752 1947 3 98Document4 pagini1752 1947 3 98Rini RiantiÎncă nu există evaluări
- Over-The-Counter Oral Hygiene Products Misuse: A Case ReportDocument4 paginiOver-The-Counter Oral Hygiene Products Misuse: A Case ReportDr Sharique AliÎncă nu există evaluări
- Pedo 1Document6 paginiPedo 1ايمن جمعة احمدÎncă nu există evaluări
- StomatitisDocument44 paginiStomatitisNessa Layos Morillo100% (1)
- Jurnal Gingivitis Vivian 190631174Document5 paginiJurnal Gingivitis Vivian 190631174VivianÎncă nu există evaluări
- Ok PM BellaDocument25 paginiOk PM Bellapark kinanÎncă nu există evaluări
- Pharmacological Management of Common Soft Tissue Lesions of The Oral CavityDocument16 paginiPharmacological Management of Common Soft Tissue Lesions of The Oral CavityAcisum2Încă nu există evaluări
- A Review and Guide To Drug Associated Oral Adverse Effects-Oral Mucosal and Lichenoid Reactions. Part 2Document10 paginiA Review and Guide To Drug Associated Oral Adverse Effects-Oral Mucosal and Lichenoid Reactions. Part 2Sheila ParreirasÎncă nu există evaluări
- Cinnamon Contact Stomatitis: A Case Report and ReviewDocument2 paginiCinnamon Contact Stomatitis: A Case Report and ReviewDwiÎncă nu există evaluări
- Lip Abscess From Isotretinoin CheilitisDocument2 paginiLip Abscess From Isotretinoin CheilitisSulistya NingsihÎncă nu există evaluări
- Erythema Multiforme Major: Case Report and Review of LiteratureDocument6 paginiErythema Multiforme Major: Case Report and Review of LiteratureSasa AprilaÎncă nu există evaluări
- Acute Ulcerative Stomatitis.Document5 paginiAcute Ulcerative Stomatitis.Manar AlsoltanÎncă nu există evaluări
- Case Report Necrotizing Ulcerative Gingivitis, A Rare Manifestation As A Sequel of Drug-Induced Gingival Overgrowth: A Case ReportDocument7 paginiCase Report Necrotizing Ulcerative Gingivitis, A Rare Manifestation As A Sequel of Drug-Induced Gingival Overgrowth: A Case ReportPutri Dwi AnggrainiÎncă nu există evaluări
- Erythema Multiforme-Oral Variant: Case Report and Review of LiteratureDocument4 paginiErythema Multiforme-Oral Variant: Case Report and Review of LiteratureMarniati JohanÎncă nu există evaluări
- Oral Pemphigus Vulgaris: Corresponding Author: K Subadra, Ksubadra@sriramachandra - Edu.inDocument12 paginiOral Pemphigus Vulgaris: Corresponding Author: K Subadra, Ksubadra@sriramachandra - Edu.inDiva AzariaÎncă nu există evaluări
- A Case Report On Symptomatic Primary Herpetic GingivostomatitisDocument5 paginiA Case Report On Symptomatic Primary Herpetic GingivostomatitisHeinzÎncă nu există evaluări
- Angular Cheilitis Guide: Causes, Symptoms & TreatmentDocument3 paginiAngular Cheilitis Guide: Causes, Symptoms & TreatmentNur Sita DewiÎncă nu există evaluări
- Case Report: Ulcerative Lichen Planus in ChildhoodDocument4 paginiCase Report: Ulcerative Lichen Planus in ChildhoodDeasireeÎncă nu există evaluări
- Oral Ulceration Causes and DiagnosisDocument10 paginiOral Ulceration Causes and Diagnosisمحمد حسنÎncă nu există evaluări
- Guide to diagnosing and managing oral ulcersDocument10 paginiGuide to diagnosing and managing oral ulcersMazaya Haekal IIÎncă nu există evaluări
- Physiotherapy Improves Mouth Opening in OSMFDocument9 paginiPhysiotherapy Improves Mouth Opening in OSMFViral ParekhÎncă nu există evaluări
- Case Report 2 PDFDocument5 paginiCase Report 2 PDFSittiNurQomariahÎncă nu există evaluări
- 01 Pitfalls of Patch Testing With Dental MaterialsDocument2 pagini01 Pitfalls of Patch Testing With Dental MaterialsGddoi SangsueÎncă nu există evaluări
- Lichen Planus of Lip - Report of A Rare Case With Review of LiteratureDocument7 paginiLichen Planus of Lip - Report of A Rare Case With Review of LiteratureDharmapadmi KasilaniÎncă nu există evaluări
- Management of Acute Primary Herpetic Gingivo-Stomatitis in ChildrenDocument3 paginiManagement of Acute Primary Herpetic Gingivo-Stomatitis in ChildrenNindy PutriÎncă nu există evaluări
- Enfermedades InmunologicasDocument14 paginiEnfermedades InmunologicasKarina OjedaÎncă nu există evaluări
- Management of Oral Lichen Plannus: A Clinical Study: Jayachandran S, Koijamsashikumar SDocument4 paginiManagement of Oral Lichen Plannus: A Clinical Study: Jayachandran S, Koijamsashikumar Sranz ibonkÎncă nu există evaluări
- PV 1Document4 paginiPV 1Aing ScribdÎncă nu există evaluări
- The Role of Allergy in Oral Mucosal DiseasesDocument6 paginiThe Role of Allergy in Oral Mucosal Diseasesanissa fitriÎncă nu există evaluări
- Review Article: Oral Ulceration - Aetiopathogenesis, Clinical Diagnosis and Management in The Gastrointestinal ClinicDocument14 paginiReview Article: Oral Ulceration - Aetiopathogenesis, Clinical Diagnosis and Management in The Gastrointestinal ClinicAmira KaddouÎncă nu există evaluări
- Holistic Management For Severe Oral Lichen Planus - A Case ReportDocument8 paginiHolistic Management For Severe Oral Lichen Planus - A Case Reportrahmania alikhlashÎncă nu există evaluări
- Oral Health Bamboo Salt PDFDocument2 paginiOral Health Bamboo Salt PDFVirma PutraÎncă nu există evaluări
- Oral Health Bamboo Salt PDFDocument2 paginiOral Health Bamboo Salt PDFVirma PutraÎncă nu există evaluări
- Wallace Workshop 6490 Wednesdy AMDocument35 paginiWallace Workshop 6490 Wednesdy AMVirma PutraÎncă nu există evaluări
- Oral Cancer and Precancerous Lesions DetectionDocument21 paginiOral Cancer and Precancerous Lesions DetectionVirma PutraÎncă nu există evaluări
- Asian Journal of Pharmaceutical and Clinical ResearchDocument2 paginiAsian Journal of Pharmaceutical and Clinical Researchikeuchi_ogawaÎncă nu există evaluări
- Herpes Assoc EM-2011Document4 paginiHerpes Assoc EM-2011Virma PutraÎncă nu există evaluări
- WHDocument3 paginiWHVirma PutraÎncă nu există evaluări
- PhoneticsDocument5 paginiPhoneticsdorasani99Încă nu există evaluări
- Angiodem-2010 NO PICDocument6 paginiAngiodem-2010 NO PICVirma PutraÎncă nu există evaluări
- Materi Oral Premalignant-2008Document6 paginiMateri Oral Premalignant-2008Virma PutraÎncă nu există evaluări
- 7 Suleyman Aguloglu A Fibre Reinforced Fixed Partial Denture CaseDocument4 pagini7 Suleyman Aguloglu A Fibre Reinforced Fixed Partial Denture CaseVirma PutraÎncă nu există evaluări
- Radio 6 (Anterior Poci) Iv1Document1 paginăRadio 6 (Anterior Poci) Iv1Virma PutraÎncă nu există evaluări
- Comparison of Porcelain Veneers and Crowns For Resolving Esthetic Problems: Two Case ReportsDocument4 paginiComparison of Porcelain Veneers and Crowns For Resolving Esthetic Problems: Two Case ReportsVirma PutraÎncă nu există evaluări
- Esthetic Closure of Diastema by Porcelain Laminate Veneers: A Case ReportDocument4 paginiEsthetic Closure of Diastema by Porcelain Laminate Veneers: A Case ReportVirma PutraÎncă nu există evaluări
- MR Sialography of Iatrogenic Sialocele - Comparison WithDocument7 paginiMR Sialography of Iatrogenic Sialocele - Comparison WithVirma PutraÎncă nu există evaluări
- Class V Preparation and Restoration Open Sandwich Technique EnamelDocument6 paginiClass V Preparation and Restoration Open Sandwich Technique EnamelVirma PutraÎncă nu există evaluări
- Kisi-Kisi SK3 Blok 12Document1 paginăKisi-Kisi SK3 Blok 12Virma PutraÎncă nu există evaluări
- Fixed Drug Eruption, Bolognia DermatologyDocument2 paginiFixed Drug Eruption, Bolognia Dermatologyjacob89Încă nu există evaluări
- LeukoplakiaDocument24 paginiLeukoplakiaAshish SoniÎncă nu există evaluări
- Primary Secondary Skin Lesions 2003Document32 paginiPrimary Secondary Skin Lesions 2003Louisa Abigail D'CruzÎncă nu există evaluări
- Egyptian Fellowship Board LogbookDocument247 paginiEgyptian Fellowship Board LogbookHussein NazzalÎncă nu există evaluări
- PsoriasisDocument11 paginiPsoriasisJeno SigamaniÎncă nu există evaluări
- The Rash That Becomes ErythrodermaDocument71 paginiThe Rash That Becomes ErythrodermacuteÎncă nu există evaluări
- EFFLORESCENCE IN THE SKINDocument31 paginiEFFLORESCENCE IN THE SKINFahri PutraÎncă nu există evaluări
- Original Article Blaschkoian Lichen PlanusDocument6 paginiOriginal Article Blaschkoian Lichen PlanusiwakiwakÎncă nu există evaluări
- Tinea Capitis Diagnosis and TreatmentDocument27 paginiTinea Capitis Diagnosis and TreatmentSyafitri NavisyaÎncă nu există evaluări
- Pemphigus foliaceus Case ReportDocument3 paginiPemphigus foliaceus Case ReportShinichi Ferry RoferdiÎncă nu există evaluări
- Ulkus Dekubitalis CareDocument48 paginiUlkus Dekubitalis CareBefalia AisarahmadaniÎncă nu există evaluări
- Oral PathologyDocument59 paginiOral PathologyJohn Brewster100% (5)
- Examination of The SkinDocument24 paginiExamination of The SkinRay Christoffer GomezÎncă nu există evaluări
- Chapter 17: Nail Disorders & Surgery: Nail Entities Nail Anatomy Surgical Nail ProceduresDocument9 paginiChapter 17: Nail Disorders & Surgery: Nail Entities Nail Anatomy Surgical Nail ProcedurespoddataÎncă nu există evaluări
- Tinea KrusisDocument7 paginiTinea KrusisMahra Elita SiregarÎncă nu există evaluări
- THE PREVALENCE OF ORAL MUCOSAL LESIONS in MORADABAD - UTTAR PRADESH BY - DR. ANAND PRATAP SINGH SPONSERED BY: - RURAL DENTAL SOCIETY FOR ORAL DISEASE PREVENTION AND CURE - LUCKNOWDocument123 paginiTHE PREVALENCE OF ORAL MUCOSAL LESIONS in MORADABAD - UTTAR PRADESH BY - DR. ANAND PRATAP SINGH SPONSERED BY: - RURAL DENTAL SOCIETY FOR ORAL DISEASE PREVENTION AND CURE - LUCKNOWanandsingh001100% (4)
- Oral Ulcers: Acute and ChronicDocument39 paginiOral Ulcers: Acute and Chronicnour almarshadiÎncă nu există evaluări
- Occupational Skin DisordersDocument17 paginiOccupational Skin DisordersDarlah Imma AuraniÎncă nu există evaluări
- Patient Education - Eczema (Atopic Dermatitis) (The Basics) - UpToDateDocument6 paginiPatient Education - Eczema (Atopic Dermatitis) (The Basics) - UpToDateRadu BalanÎncă nu există evaluări
- Fungal Ear Infection & Scalp Ringworm GuideDocument7 paginiFungal Ear Infection & Scalp Ringworm GuideFaiq LÎncă nu există evaluări
- Dermato Venerology ScienceDocument11 paginiDermato Venerology ScienceAQis AQishÎncă nu există evaluări
- Paediatric DermatologyDocument12 paginiPaediatric DermatologyDuranka PereraÎncă nu există evaluări
- Bullous Pemphigoid PosterDocument21 paginiBullous Pemphigoid PosterChe Ainil ZainodinÎncă nu există evaluări
- Subacute PLEVADocument3 paginiSubacute PLEVAArya PratamaÎncă nu există evaluări
- 2 5456181012360856193Document70 pagini2 5456181012360856193Maha KhalidÎncă nu există evaluări
- Mouth Problems - DermNet NZDocument3 paginiMouth Problems - DermNet NZMudassar SattarÎncă nu există evaluări
- SclerodermaDocument20 paginiSclerodermariskaicung100% (1)
- Lumps and Ulcer, Sebaceous Cyst, Lipoma, Dermoid CystDocument88 paginiLumps and Ulcer, Sebaceous Cyst, Lipoma, Dermoid CystAbdulsalam DostÎncă nu există evaluări
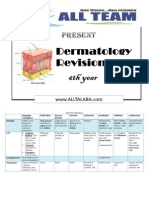
- Dermatology RevisionDocument7 paginiDermatology RevisionmksharmaaÎncă nu există evaluări
- Benign Moles and LesionsDocument2 paginiBenign Moles and LesionsMari MariÎncă nu există evaluări