Documente Academic
Documente Profesional
Documente Cultură
Adaptive Ability PDF
Încărcat de
Luis Torres Ossandon0 evaluări0% au considerat acest document util (0 voturi)
48 vizualizări10 paginiTrauma brain injury (TBI) is a common, acquired childhood disability. Few studies have attempted to measure the impact of preinjury functions on postinjury behavior. More severe injury is associated with a decrease in functional ability at 6 months post-TBI.
Descriere originală:
Titlu original
adaptive ability.pdf
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentTrauma brain injury (TBI) is a common, acquired childhood disability. Few studies have attempted to measure the impact of preinjury functions on postinjury behavior. More severe injury is associated with a decrease in functional ability at 6 months post-TBI.
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
48 vizualizări10 paginiAdaptive Ability PDF
Încărcat de
Luis Torres OssandonTrauma brain injury (TBI) is a common, acquired childhood disability. Few studies have attempted to measure the impact of preinjury functions on postinjury behavior. More severe injury is associated with a decrease in functional ability at 6 months post-TBI.
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 10
1639
Disability & Rehabilitation
2012
34
19
1639
1647
2012 Informa UK, Ltd.
10.3109/09638288.2012.656789
0963-8288
1464-5165
Disability & Rehabilitation, 2012; 34(19): 16391647
2012 Informa UK, Ltd.
ISSN 0963-8288 print/ISSN 1464-5165 online
DOI: 10.3109/09638288.2012.656789
14 June 2011
03 January 2012
09 January 2012
Context: Traumatic brain injury (TBI) is a common, acquired
childhood disability, which has been shown to have a
signicant impact on childrens cognitive and educational
function. While behavioral problems are also noted, there is
ongoing debate about the contribution of preinjury factors
in this domain. Few studies have attempted to measure the
impact of these preinjury functions on postinjury behavior.
Objective: To compare pre and postinjury adaptive ability,
behavior, executive function and quality of life (QOL) and
to identify factors that contribute to outcomes in these
domains including injury severity, socio-demographic and
preinjury characteristics. Design: Consecutive recruitments to
a prospective, longitudinal study, utilizing a between factor
design, with injury severity as the independent variable.
Participants and methods: Children admitted to hospital with
a diagnosis of TBI aged between 6 and 14 years (n=205)
were divided according to injury severity (mild, moderate
and severe). Adaptive behavior (Vineland Adaptive Behavior
Scales), child behavior (Child Behavior Checklist), everyday
executive functions (Behavior Rating Inventory of Executive
Function) and QOL (Child Health Questionnaire) assessed at
6 months post-TBI. Results and conclusions: Severity by time
interactions were identied across a range of outcome domains
demonstrating that more severe injury is associated with a
decrease in functional ability at 6 months post-TBI. This eect
was most pronounced for everyday executive skills, social
function and internalizing aspects of child behavior. Preinjury
function was a consistent predictor of postinjury status. Injury
severity contributed little to the prediction of functional
outcomes once preinjury functioning was accounted for in
the model. Age at injury and family cohesion were relevant
to specic outcome domains only. Socio-economic status did
not contribute signicantly to outcome at 6 months. Preinjury
functioning as reported by parents in the acute phase may be a
useful predictive tool for identifying children who may be at risk
of functioning diculties 6 months post-TBI.
Keywords: Adaptive behavior, behavior, child, executive
function, quality of life, traumatic brain injury
Introduction
Childhood traumatic brain injury (TBI) is the most frequent
cause of interruption to normal development, with as many
as 500:100,000 children experiencing a TBI in any 1 year,
and with 1/30 newborns sustaining a TBI by age 16[1]. With
advances in medical treatment, mortality rates are low and
RESEARCH PAPER
Adaptive ability, behavior and quality of life pre and posttraumatic brain
injury in childhood
Vicki Anderson
1,2,3
, Robyne Le Brocque
4
, Greg Iselin
4
, Senem Eren
1,3
, Rian Dob
5
, Timothy J. Davern
6
,
Lynne McKinlay
7
& Justin Kenardy
4
1
Critical Care & Neuroscience, Murdoch Childrens Research Institute, Melbourne, Australia,
2
Department of Psychology,
Royal Childrens Hospital, Melbourne, Australia,
3
Psychological Science, University of Melbourne, Melbourne Australia,
4
Centre for National Research on Disability and Rehabilitation Medicine, The School of Medicine,
5
School of Psychology,
University of Queensland, Brisbane, Australia,
6
Psychological Medicine, Monash University, Melbourne, Australia, and
7
Queensland Paediatric Rehabilitation Service, Royal Childrens Hospital, Brisbane, Australia
Correspondence: Vicki Anderson, PhD, Department of Psychology, Royal Childrens Hospital, Parkville, Victoria 3052, Australia.
E-mail: vicki.anderson@rch.org.au
Childhood traumatic brain injury
Priorities for intervention: (i) more severe injury; (ii)
presence of pre-injury impairment; (iii) younger age
at injury and (iv) evidence of family dysfunction.
Level of functional impairment postinjury rarely meets
criteria for a frank diagnosis (e.g. intellectual impair-
ment and psychiatric disorder) and thus children are
frequently ineligible for routine community supports.
Reduced executive skills and social competence and
elevated behavioral disturbances indicate that evi-
dence-based interventions addressing these domains
are a priority.
Implications for Rehabilitation
(Accepted January 2012)
1640 V. Anderson etal.
Disability & Rehabilitation
there are ever-increasing numbers of survivors. Te acute and
lasting efects of severe TBI are recognized by the National
Institutes of Health Consensus Development Panel on reha-
bilitation of persons with TBI, which has highlighted the
dramatic change in the individuals life course, profound
disruption of the family and costly lifetime expenses [2].
In school-aged survivors, residual impairments are reported
in a range of areas including cognition, educational achieve-
ment, behavior and quality of life (QOL) [39]. Tese defcits
may impact on a childs capacity to interact with the environ-
ment, causing lags in skill acquisition and peer interaction,
and resulting in increasing gaps between injured children and
their age-matched peers. Follow-up of survivors of childhood
TBI demonstrates that, even with access to rehabilitation, sig-
nifcant problems may persist [4,7,10,11].
Injury or biological factors appear to explain a propor-
tion of the variance in outcomes post-TBI. Te best estab-
lished of these is injury severity, where a dose-response
relationship is frequently identifed [3,12,13], with more
severe injury associated with greater impairment. However,
this relationship alone has been insufcient to account for
the wide variability in outcomes, particularly within the
pediatric population [9] and for domains other than physical
and intellectual abilities. Other potential predictors include
the childs age at injury, and social context, including socio-
economic status (SES) and family environment [1422]. A
further consideration that is frequently noted, but infre-
quently evaluated, is the contribution of premorbid factors,
in particular, preinjury child adaptive functions and behavior
and preinjury environment.
In the TBI literature it is commonly argued that individuals
who have sustained are likely to be diferent to the general
population. Previous studies have reported that, within the
child TBI population, there is a high incidence of behavioral
difculties, including learning problems, attentional defcits
and impulsivity [2325]. It has also been documented that TBI
is more common in families where parents are socially dis-
advantaged, unemployed or emotionally disturbed [3,26,27],
and where parental neglect and poor supervision are evident
[28]. If these characteristics are present in children with TBI,
it may be difcult to diferentiate TBI-specifc sequelae from
those present premorbidly.
Te present study aimed to address early outcome from
TBI, within the context of functional abilities including adap-
tive skills, behavior, everyday executive function and QOL,
using a prospective, longitudinal design and with attention
to the infuences of multiple potential predictors of outcome.
Based on previous fndings, it was predicted that:
1. Tere would be a signifcant diference between pre and
postinjury function across the following domains: adap-
tive skills, behavior, everyday executive function and
QOL.
2. More severe TBI would be associated with poorer func-
tion in these domains at 6 months postinjury.
3. Injury severity and preinjury function would be the best
predictors of postinjury function, with age at injury, fam-
ily and socio-demographic factors less critical.
Method
Participants
Tis article reports on data relating to both preinjury function
and function assessed at 6 months postinjury from a larger
prospective, longitudinal study. Participants represented
consecutive admissions to the Mater Childrens Hospital in
Brisbane and the Royal Childrens Hospitals in Brisbane and
Melbourne. Following admission, the research team was
notifed of family details via hospital staf in either the emer-
gency department or the neurosurgery ward of each hospital.
Inclusion criteria were: (i) 614 years at time of injury; (ii)
admission to hospital for TBI; and (iii) a documented period
of altered consciousness. Exclusion criteria included: (i) par-
ents level of English unsatisfactory for completion of ques-
tionnaires; (ii) previous documented neurological, psychiatric
or developmental disorder; (iii) TBI was a result of suspected
child abuse. In total, 514 families were eligible for participa-
tion in the study. However, 309 failed to respond to invitations
to participate within the study timeframe, were unable to be
contacted or declined participation due to time pressures. Te
resultant sample comprised 205 families with children who
had sustained a TBI. Children had a mean age of 10.75 years
[standard deviation (SD)=2.51] at the time of their accident.
Of the sample, 92 (45%) children were from Brisbane and 113
(55%) from Melbourne and 142 (69%) were male.
Demographic and injury details were collected on recruit-
ment to the study, and are presented in Tables I and II. Federal
privacy regulations prevented the collection of these data for
nonparticipating families. Medical records were accessed to
determine injury severity. Using the method described by
Anderson etal. (1997), injury severity was classifed based on
the childs lowest Glasgow Coma Scale score (GCS) [29] in the
frst 24 hours and the presence/absence of neurological or radio-
logical abnormalities. Injury severity was classifed as follows:
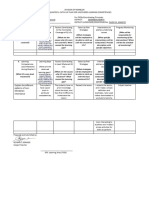
Table I. Demographics characteristics of sample.
Mild TBI Moderate TBI Severe TBI
No. participants, n (%) 130 (63.4) 55 (26.9) 20 (9.70)
Gender (males), n (%) 94 (72.3) 34 (61.8) 14 (70.0)
Age at injury, M (SD) 10.80 (2.42) 10.48 (2.60) 11.12 (2.93)
Recruitment location
Melbourne, n (%) 72 (55.4) 33 (60.0) 8 (40.0)
Brisbane, n (%) 58 (44.6) 22 (40.0) 12 (60.0)
Socio-economic status
High 62 (64) 24 (25) 11 (11)
Medium 52 (65) 23 (29) 5 (6)
Low 9 (53) 6 (35) 2 (12)
Preinjury function
VABS: TOT M(SD) 96.56 (15.87) 96.67 (17.67) 100.06 (16.42)
CBCL:TOT M (SD) 50.86 (9.56) 51.49 (10.18) 50.80 (9.66)
BRIEF: GEC M (SD) 50.86 (10.04) 50.68 (8.70) 54.05 (12.55)
CHQ:PHYS* M (SD) 47.64 (11.80) 42.70 (16.51) 34.93 (24.87)
FSIQ: 3 months* M (SD) 104.77 (11.84) 99.36 (13.82) 91.78 (10.39)
*p<0.001.
VAB:TOT, Vineland Adaptive Behavior Scale: Composite Score; CBCL:TOT, Child
Behavior Checklist: Total Behavior Problems; BRIEF:GEC, Behavior Rating Invento-
ry of Executive Function: Global Executive Composite; FSIQ, Full Scale Intelligence
Quotient; CHQ:PHYS, physical subscale; CHQ:PSYCHOL, psychosocial subscale;
TBI, traumatic brain injury; SD, standard deviation.
Pre- and post-TBI adaptive ability, behavior and QOL 1641
2012 Informa UK, Ltd.
(i) mild TBI (n = 130, 63%): lowest GCS between 1315 and
an absence of neurological and radiological abnormalities; (ii)
moderate TBI (n = 55, 27%): lowest GCS between 912 and/
or presence of intracranial lesions or neurological abnormality
and (ii) severe TBI (n=20, 10%): lowest GCS between 38 and/
or presence of intracranial lesions or neurological abnormality.
Measures
Demographic-medical interview
Preinjury medical, developmental, social and educational
history of each participant was documented through inter-
views with the primary caregiver. Information regarding
parental occupation, education level and family constella-
tion was also collected. A modifed version of the Australian
Standard Classifcation of Occupations [30] was used to
determine SES. Tis information was collected during
the initial interview with families and SES rankings were
based on the higher ranking occupation of the mother and
father. Injury data were collected from medical records.
Baseline data on child adaptive function, behavior, execu-
tive function and QOL were collected from parent ratings
of their childs function before their injury using the instru-
ments described below. Te degree of limitations in fam-
ily activities (due to child ill health) and family cohesion
were obtained from parent preinjury ratings from the Child
Health Questionnaire (CHQ) [31].
Child function
Intellectual ability
Te Wechsler Abbreviated Scale of Intelligence [32] was
administered to all children in the study at 3 months
postinjury. Full Scale Intelligence Quotient (IQ) (M = 100,
SD=15) was calculated and used as a sample descriptor.
Adaptive functioning, behavior, executive functioning
and QOL
Parents completed a number of questionnaires, rating their
childs function across several domains. Preinjury ratings
were provided on recruitment to the study, and subsequent
ratings were collected at 6 months postinjury, on the follow-
ing measures:
1. Adaptive functioning: Te Vineland Adaptive Behavior
Scale (VABS) [33] has a questionnaire format, which
provides information on a childs level of adaptive
function in the following domains: Communication
(VABS:COMM), Daily Living Skills (VABS:DL), and
Socialization (VABS:SOC). A Total Adaptive Behavior
score (VABS:TOT) is also derived. For each of these areas
standard scores were calculated (M=100, SD=15).
2. Behavior: Childrens pre and postinjury behavior was
assessed via the Child Behavior Checklist (CBCL) [34].
Te three summary scales (internalizing: CBCL:INT;
externalizing: CBCL:EXT; and total problems: CBCL:
TOT; M=50, SD=10) were examined.
3. Executive function: Te Behavior Rating Inventory of
Executive Function (BRIEF) [35] measures executive
functioning in children in day-to-day settings. Te 86
items are scored on a 3-point scale (never, sometimes
and ofen), yielding eight clinical scales and two validity
scales (inconsistency and negativity). Inhibition, shif
and emotional control scales comprise the Behavioural
Regulation Index (BRI), and initiation, working mem-
ory, planning, organization of materials and monitor-
ing clinical scales comprise the Metacognition Index
(MCI). Te BRI and MCI combine to yield an overall
score: Global Executive Composite (GEC). T scores
(M=50, SD=10) are calculated for each, with higher T
scores indicating that the child is experiencing greater
difculties.
4. Quality of life: Te Australian adaptation of the CHQ
[31] assesses functional health status and well-being in
children including physical (CHQ:PHYS) and psycho-
social (CHQ:PSYCHOL) functioning and the impact of
the childs functioning on the parent (CHQ:FC). T scores
for Physical and Psychosocial subscales were computed
(M = 50, SD = 10) acutely and at 6 months post-TBI.
Ten standardized scores were also considered, relating to
child behavior and mental health, child self-esteem, child
functioning and the impact of the childs psychosocial
health on the parent.
Procedure
Te study was approved by the Human Research Ethics
Committees of the Mater Childrens Hospital in Brisbane
and the Royal Childrens Hospitals in Brisbane and
Melbourne and was conducted in compliance with national
legislation and the Code of Ethical Principles for Medical
Research Involving Human Subjects of the World Medical
Table II. Injury and medical characteristics of sample.
Mild TBI Moderate TBI Severe TBI
Age at injury: years, M (SD) 10.80 (2.42) 10.48 (2.60) 11.12 (2.93)
Glasgow coma scores
GCS: admission* M (SD) 14.66 (0.57) 13.41 (2.14) 8.85 (4.10)
GCS: lowest in 24 hrs* M (SD) 14.44 (0.68) 12.69 (2.36) 6.75 (3.18)
Duration of coma *
None, n (%) 52 (40.0) 21 (38.2) 2 (10.0)
05 mins, n (%) 49 (37.7) 18 (32.7) 9 (45.0)
5 min1 day, n (%) 1 (0.8) 3 (5.50) 3 (15.0)
17 days, n (%) - - 3 (15.0)
Not recorded, n (%) 28 (21.50) 13 (23.60) 3 (15.0)
Cause of injury*
MVA passenger, n (%) 9 (6.9) 10 (18.20) 6 (30.0)
MVA pedestrian, n (%) 3 (2.3) 8 (14.50) 5 (25.0)
Fall, n (%) 80 (61.6) 23 (41.90) 8 (40.0)
Blow/knock, n (%) 16 (12.30) 7 (12.70) 1 (5.0)
Sport, n (%) 22 (16.90) 7 (12.70) -
Neurological signs* n (%) 18 (34.0) 23 (43.40) 12 (22.6)
CT/MRI pathology*
None, n (%) 128 (100.00) 27 (49.10) 5 (25.0)
Frontal, n (%) - 5 (9.10) 1 (5.0)
Extrafrontal, n (%) - 6 (10.90) 2 (10.0)
Multifocal/difuse, n (%) - 17 (30.9) 12 (60.0)
*p<0.05.
GCS, Glasgow Coma Score; MVA, motor vehicle accident;TBI, traumatic brain injury;
SD, standard deviation; CT/MRI, computed tomography/magnetic resonance imaging.
1642 V. Anderson etal.
Disability & Rehabilitation
Association (Declaration of Helsinki). Children who met
the selection criteria were identifed during hospital admis-
sion or shortly afer discharge. Parents and primary caregiv-
ers were approached, either in person or through written
correspondence, to take part in the study. Consistent with
ethical guidelines, participants were entered into the study
once informed written consent was obtained. Within the
frst 2 months postinjury, parents completed the demo-
graphic interview and the assessments of child function-
ing with respect to their childs preinjury functioning. At
3 months post-TBI children completed the IQ assessment.
At 6 months postinjury, the parent/caregiver completed
questionnaires relating to the childs current level of func-
tioning and the child was assessed for neuropsychological
functioning.
Statistical analysis
Quantitative analyses were conducted using SPSS (version
14.0). Item level missing data were treated according to
standard scoring rules for each variable or mean substituted.
Missing data due to noncompletion of questionnaires were
deleted from analyses on a case by case basis. Analysis of data
lost to attrition showed no signifcant diference between
those who remained in the study and those who were lost
to follow-up for the independent variables of injury severity,
gender, age and socio-economic status.
Initially the three injury severity groups were compared
[analysis of variance (ANOVA)] to identify any demographic
or injury-related diferences. To address hypotheses 1 and 2,
that there would be a signifcant diference between pre and
postinjury function, with more severe injury leading to greater
impairment, ANOVA (severity by time) was conducted for each
outcome domain (adaptive function, behavior, executive function
and QOL). We were particularly interested in severity by time
interaction efects which would indicate deterioration in parent
ratings of child function for children with more severe injuries.
Tukeys honestly signifcant diference analyses were conducted
to identify group diferences. For Hypothesis 3, that injury
severity and preinjury function would be the best predictors of
postinjury function, hierachical regressions were employed for
each outcome domain. Baseline variables, child variables (age
at injury, gender and SES) CHQ:FC and injury severity (mild,
moderate and severe) were included in each analysis.
Results
Demographic and injury characteristics of sample
Analysis indicated no group diferences across TBI severity
groups with respect to age at injury, gender, SES, preinjury
adaptive abilities, behavior or executive function. For QOL,
signifcant diferences were observed for the childs physical
functioning at time 1 with children with severe TBI having
signifcantly lower physical functioning compared to mild
and moderate TBI. Not unexpectedly, intellectual ability at 3
months postinjury was signifcantly lower for children with
more severe insults. Tere were also no systematic difer-
ences identifed across the three recruitment sites (Table I).
As illustrated in Table II, diferences were found for all
measures of injury severity: GCS on admission, lowest GCS
in the frst 24 hours, duration of coma, cause of injury, neuro-
logical signs and computed tomography/magnetic resonance
imaging (CT/MRI) pathology. Of the 205 children included
in the study, 25 (12%) sustained injury as a motor vehicle pas-
senger, 17 (8%) as a motor vehicle pedestrian, 111 (54%) from
falls, 24 (12%) from knocks/blows, and 28 (14%) from sport-
ing accidents. Presence of neurological signs (e.g., seizures,
dysarthria, ataxia, blurred vision) was observed in 53 (26%)
participants. CT/MRI was available on 124 (60%) participants.
Abnormalities were detected on 44 (22%) of scans. Tere were
44 (22%) children who sustained skulls fractures and 20 (10%)
of children required neurosurgical intervention.
Pre and postinjury (6 months) outcomes across severity
groups
Adaptive function
Analysis of pre and postinjury parent ratings of adaptive
function revealed surprisingly few signifcant fndings
(Table III). No signifcant time efects were evident for
overall adaptive function, daily living skills or communica-
tion skills. For socialization, a signifcant severity by time
efect was found, F(2,106) = 6.31, p = 0.003, with children
with severe TBI demonstrating signifcantly lower social-
ization skills at 6 months postinjury compared with their
preinjury functioning (p = 0.01). Children with mild and
moderate TBI did not show signifcant changes over time
in this domain.
Child behavior
No signifcant diference was observed for time efects for
parent ratings of child behavior on the CBCL, however there
was a signifcant severity by time interaction for CBCL:TOT,
F(2,151) = 4.59, p = 0.01, and CBCL:INT, F(2,149) = 2.99,
p = 0.05 (Table III). Post hoc analyses showed that parents
rated their child as having signifcantly more total behavior
problems at 6 months post severe TBI (p=0.01). Tere was
no signifcant diference over time for total behavior problems
for children with mild or moderate injuries. For internalizing
behavior, children with mild TBI were found to have some
improvement in their symptoms (p = 0.01). Tere were no
signifcant group diferences for externalizing behavior.
Executive skills
Parent ratings of everyday executive skills on the BRIEF showed
a consistent pattern of group diferences, both for time and
for severity by time interaction (Table III). Diferences were
observed for the BRIEF:GEC for both time, F(1,154)=25.88,
p< 0.001, and interaction efects, F(2,154)=9.73, p<0.001.
Children with moderate (p=0.03) and severe TBI (p<0.001)
had signifcantly higher levels of dysfunction at 6 months
postinjury compared to their preinjury functioning. A similar
pattern was observed for both moderate and severe TBI groups
for performance on the BRIEF:MCI [time: F(1,154)=23.69,
p < 0.001; severity by time: F(2,154) = 8.23, p < 0.001].
Signifcant time and severity by time efects were also observed
Pre- and post-TBI adaptive ability, behavior and QOL 1643
2012 Informa UK, Ltd.
for the BRIEF:BRI [time: F(1,154)=18.45, p<0.001; severity
by time: F(2,154)=7.55, p=0.001]. Post hoc analyses showed
signifcantly poorer functioning for children with severe TBI
(p<0.001), but no signifcant changes over time for children
with mild and moderate TBI.
Quality of life
Signifcant main efects for time were observed for
CHQ:PHYS, with poorer physical function acutely postin-
jury, F(1,146)=7.04, p=0.01. No severity by time efect was
observed. In contrast, no signifcant time efect was observed
for CHQ:PSYCHOL, however a signifcant severity by time
interaction was detected, F(2,146)=3.45, p=0.03. Although
the overall model was signifcant, group level diferences just
failed to meet signifcance. Children with mild TBI performed
marginally better at 6 months TBI (p=0.06) while those with
severe TBI had lower psychological performance at 6 months
postinjury than at injury (p=0.06).
Predictors of postinjury abilities
Outcomes of regression analyses are presented for each of the
four functional domains under investigation: adaptive func-
tioning, child behavior, executive skills and QOL (TableIV).
Variables entered into the regression models included the
relevant preinjury baseline variable, child variables including
child gender, age at injury and socio-economic status; family
functioning and cohesion and injury severity.
Adaptive functioning
A signifcant regression model was found for adaptive behavior
[VABS:TOT: F(7,71) = 7.58; p < 0.001]. Signifcant variables
included preinjury VABS:TOT, and child age at injury. Te
model accounted for 37% of the variance in adaptive behavior
functioning. A signifcant model was also found for childrens
communication skills at 6 months postinjury [VABS:COMM:
F(7,113) = 10.50; p < 0.001]. Signifcant variables included
preinjury VABS:COMM and child age at injury. Te model
accounted for 36% of the variance in childs communication
functioning at 6 months postinjury. A similar model was also
found for the childs functioning in terms of daily living skills
[VABS:DL: F(7,98) = 11.64; p < 0.001]. Again, signifcant
variables included preinjury VABS:DL and child age at injury
and accounted for 42% of the variance in functioning in daily
living skills at 6 months. A signifcant model was also found
for socialization skills at 6 months postinjury [VABS:SOC:
F(7,88) = 9.68; p < 0.001]. For this model both preinjury
VABS:SOC and injury severity contributed signifcantly to
predicting VABS:SOC at 6 months. Te model accounted
for 39% of the variance in childs socialization at 6 months
postinjury. In summary, preinjury adaptive functioning pre-
dicted postinjury functioning across each of the domains.
Child age at injury was also signifcant in the models for total
functioning, communication skills and daily living but not for
socialization. Injury severity was not signifcant in the models
except for predicting postinjury socialization, where children
with more severe injury had poorer functioning. Child gen-
der, SES and family cohesion were nonsignifcant in predict-
ing adaptive functioning at 6 months.
Child behavior
Signifcant models were also obtained for child behavior
problems at 6 months post TBI injury. For CBCL:TOT,
[F(7,137) = 22.41, p < 0.001], preinjury CBCL:TOT and
injury severity were signifcant and accounted for 51% of the
Table III. Pre and postinjury (6 months) parent ratings of childrens adaptive function, behavior, executive functioning and quality of life by TBI severity.
Mild TBI Moderate TBI Severe TBI
Pre Post Pre Post Pre Post
Adaptive function
VABS:TOT M (SD) 95.70 (14.01) 97.87 (14.47) 98.58 (20.71) 97.2 (13.07) 99.38 (16.54) 93.08 (16.97)
VABS:COMM M (SD) 97.63 (14.85) 98.77 (14.16) 93.84 (18.00) 95.56 (15.28) 95.13 (17.72) 91.06 (15.05)
VABS: DL M (SD) 92.70 (12.44) 92.76 (13.01) 95.39 (19.54) 98.26 (10.69) 95.12 (12.34) 93.94 (16.50)
VABS:SOC M (SD)*
a
101.30 (13.10) 103.82 (13.00) 100.38 (13.00) 100.48 (10.60) 105.23 (12.25) 95.85 (18.16)
Behavior
CBCL:TOT M (SD)*
b
50.85 (9.52) 50.03 (9.94) 51.87 (10.07) 50.74 (12.54) 51.16 (9.79) 55.89 (10.74)
CBCL:INT M (SD)***
c
51.37 (10.16) 49.24 (10.57) 51.00 (8.70) 52.19 (10.96) 53.00 (10.04) 51.26 (10.43)
CBCL:EXT M (SD) 50.57 (9.75) 51.02 (10.47) 53.65 (9.79) 52.15 (11.08) 52.50 (10.51) 55.74 (11.65)
Executive function
BRIEF:GEC M (SD)**
c,
**
b
50.75 (9.96) 51.04 (10.39) 50.63 (8.90) 53.92 (11.97) 54.89 (12.30) 63.63 (12.43)
BRIEF:BRI M (SD)**
c,
**
b
49.42 (9.56) 49.78 (10.33) 50.08 (10.25) 51.89 (11.79) 53.32 (12.42) 61.58 (12.89)
BRIEF:MCI M (SD)**
c,
**
b
51.43 (10.07) 51.70 (10.58) 50.87 (8.30) 53.92 (11.97) 55.26 (11.38) 62.84 (11.41)
Quality of Life
CHQ:PHY M (SD)***
c
47.65 (11.81) 50.77 (9.46) 42.70 (16.51) 48.06 (12.55) 34.93 (24.87) 39.81 (14.23)
CHQ:PSYCHOL M (SD) 47.76 (10.38) 49.86 (9.62) 46.77 (9.70) 46.39 (11.90) 43.45 (13.07) 38.54 (14.38)
*p<0.01; **p<0.001; ***p<0.05.
a
Severity efect.
b
Severity by time interaction.
c
Time efect.
VABS:TOT, Adaptive Composite Score; VABS:COMM, communication domain; VABS:DL, daily living domain; VABS:SOC, socialization domain; CBCL:TOT, total behav-
ior problems; CBCL:INT, internalizing problems; CBCL:EXT, externalizing problems; BRIEF:GEC, Global Executive Composite; BRIEF:BRI, Behavioral Regulation Index;
BRIEF:MCI, Metacognitive Index; CHQ:PHYS, physical Subscale; CHQ:PSYCHOL, psychosocial subscale; TBI, traumatic brain injury; SD, standard deviation.
1644 V. Anderson etal.
Disability & Rehabilitation
variance in child total behavior problems at 6 months. A sig-
nifcant model was also obtained for internalizing behavior at
6 months postinjury [CBCL:INT: F(7,136)=17.59; p<0.001].
Preinjury CBCL:INT was the only signifcant variable in the
model which accounted for 45% of the variance in internal-
izing behavior scores at 6 months postinjury. A similar model
was found for externalizing scores at 6 months (CBCL:EXT:
F(7,134) = 0 21.78; p < 0.001. Once again, the only variable
signifcant in the fnal model was preinjury CBCL:EXT. Te
fnal accounted for 51% of the variance in externalizing
behavior at 6 months.
Executive functioning
A signifcant model was also found for global executive func-
tioning [BRIEF:GEC: F(7,138)=29.71; p<0.001]. Signifcant
variables in the model included preinjury BRIEF:GEC,
CHQ:FC and injury severity. Te model accounted for 58% of
the variance in outcomes. For behavioral regulation, analyses
resulted in a signifcant model [BRIEF:BRI: F(7,138)=25.40;
p < 0.001] with signifcant variables including preinjury
BRIEF:BRI and injury severity. Te model accounted for 54%
of the variance in behavioral regulation at 6 months. A sig-
nifcant model was also obtained predicting metacognition
at 6 months [BRIEF:MCI: F(7,138)=31.40; p<0.001]. Once
again, preinjury BRIEF:MCI, CHQ:FC, and injury severity
were signifcant. Te model accounted for 60% of the variance
in metacognitive outcome at 6 months postinjury. In sum-
mary, preinjury executive functioning predicted functioning
at 6 months post injury. Injury severity was also signifcant in
predicting outcomes. Child age at injury, gender and SES were
nonsignifcant. Family cohesion also signifcantly predicted
GEC scores and metacognition at 6 months postinjury.
Quality of life
Regression analysis predicting physical functioning at
6 months was signifcant [CHQ:PHYS: F(7,133) = 4.28,
p<0.001], however accounted for only 14% of the variance.
Preinjury CHQ:PHYS and injury severity were the only
variables that signifcantly predicted physical functioning at
6 months. For psychosocial functioning the model was also
signifcant [CHQ:PSYCHOL: F(7,133)=11.01, p<0.001] and
accounted for 33% of the variance in functioning at 6 months
postinjury. Preinjury CHQ:PSYCHOL and injury severity
were both signifcant variables in the model. In summary,
only preinjury QOL and injury severity predicted QOL at
6 months postinjury.
Table IV. Regression analyses predicting functioning outcomes at 6 months post-TBI injury.
Outcome (postinjury ratings) Adjusted R
2
Test statistic Signifcant variables B SE B Beta p value
Adaptive function
VABS:TOT 0.37 F(7,71)=7.58; p<0.001 VABS:TOT Pre- 0.36 0.09 0.39 <0.001
Age 2.25 0.57 0.38 <0.001
VABS:COMM 0.36 F(7,113)=10.50; p<0.001 VABS:COMM Pre- 0.30 0.07 0.33 <0.001
Age 1.98 0.45 0.35 <0.001
CHQ:FA 0.11 0.05 0.17 0.03
VABS:DL 0.42 F(7,98)=11.64; p<0.001 VABS:DL: Pre- 0.32 0.07 0.34 <0.001
Age 2.54 0.45 0.45 <0.001
VABS:SOC 0.39 F(7,88)=9.68; p<0.001 VABS:SOC Pre- 0.64 0.09 0.58 <0.001
GCS 4.71 1.65 0.24 0.005
Behavior
CBCL:TOT 0.51 F(7,137)=22.41; p<0.001 CBCL:TOT Pre- 0.76 0.08 0.68 <0.001
GCS 2.36 0.93 0.15 0.012
CBCL:INT 0.45 F(7,136)=17.59; p<0.001 CBCL:INT Pre- 0.70 0.77 0.66 <0.001
CBCL:EXT 0.51 F(7,134)=21.78; p<0.001 CBCL:EXT Pre- 0.73 0.08 0.66 <0.001
Executive function
BRIEF:GEC 0.58 F(7,138)=29.71; p<0.001 BRIEF:GEC Pre- 0.73 0.07 0.62 <0.001
CHQ:FC 0.10 0.04 0.14 0.014
GCS 3.55 0.92 0.21 <0.001
BRIEF:BRI 0.54 F(7,138)=25.40; p<0.001 BRIEF:BRI Pre- 0.68 0.07 0.60 <0.001
Injury severity 3.13 0.95 0.19 0.001
BRIEF:MCI 0.60 F(7,138)=31.40; p<0.001 BRIEF:MCI Pre- 0.78 0.07 0.66 <0.001
CHQ:FC 0.11 0.04 0.15 0.007
Injury severity 3.19 0.89 0.19 000
Quality of life
CHQ:PHYS 0.14 F(7,133)=4.28; p=0.000 CHQ:PHYS Pre- 0.16 0.08 21 0.049
injury severity 4.08 1.36 0.24 0.003
CHQ:PSYCHOL 0.33 F(7,133)=11.01; p=0.000 CHQ:PSYCHOL Pre- 0.40 0.09 0.37 0.000
injury severity 4.34 1.17 .26 0.000
VABS:TOT, Adaptive Composite Score; VABS:COMM, communication domain; VABS:DL, daily living domain; VABS:SOC, socialization domain; CBCL:TOT, total behav-
ior problems; CBCL:INT, internalizing problems; CBCL:EXT, externalizing problems; BRIEF:GEC, Global Executive Composite; BRIEF:BRI, Behavioral Regulation Index;
BRIEF:MCI, Metacognitive Index; CHQ:PHYS, physical subscale; CHQ:PSYCHOL, psychosocial subscale; CHQ:FC, family cohesion; VHQ:FA, family activities; Pre, preinjury
scores; TBI, traumatic brain injury.
Pre- and post-TBI adaptive ability, behavior and QOL 1645
2012 Informa UK, Ltd.
Discussion
Te present study examined sub-acute functional outcomes
(adaptive ability, child behavior, everyday executive function
and QOL) in school-aged children who had sustained a mild,
moderate or severe TBI 6 months previously. Preinjury status
and injury severity were explored to determine their contribu-
tion to these outcomes. To assist in diferentiating postinjury
problems specifc to TBI, we excluded children from this study
with preexisting neurological, psychiatric or developmental
disorders, previous TBI or nonaccidental injuries. We also
established that there were no severity group diferences for
demographic factors, which might confound outcomes (e.g.
gender, SES and age at injury).
Contrary to predictions, few changes were noted for adap-
tive abilities from preinjury to 6 months postinjury, with little
impact of injury severity. Of note, these fndings are in keep-
ing with those reported by Anderson and colleagues [10,12]
who found few diferences at 6 months postinjury, but with
impairments in adaptive function emerging by 12 months
and persisting to 30 months. Te exception to this pattern was
for socialization, where the severe TBI group showed a sub-
stantial decrease in social skills from preinjury to 6 months
postinjury, possibly due to extended hospitalization and con-
valescence and associated restrictions in social interactions.
Child behavior problems were seen to increase postinjury,
consistent with the work of others [6,36], although, group
mean ratings remained well within the normal range for all
TBI groups. Children with severe TBI were found to have
greater overall behavior problems at 6 months following TBI
than children with milder insults. No group or time diferences
were identifed for externalizing behaviors. For internalizing
behaviors, a small, but signifcant decrease in problems was
detected specifc to children with mild TBI.
By far the most dramatic results for the study were seen
for everyday ratings of executive function. On the BRIEF, all
summary measures indicated poorer function by 6 months
post-TBI and this was also associated with more severe injury.
Tese fndings suggest that executive dysfunction is present
relatively early postinjury.
As might be expected, in the physical domain, children
with TBI showed signifcant improvement in the physical
domain from the acute phase to 6 months post-TBI. Further,
children with severe TBI demonstrated poorer function both
acutely and 6 months postinjury, suggesting that physical
defcits associated with TBI persist in this group. Consistent
with the small literature on postinjury QOL [8], children with
severe injury appeared to be most vulnerable to experience
poorer QOL in the psychosocial domain. Parent ratings sug-
gested poorer psychosocial QOL at 6 months for children
with severe TBI. Taken together with poorer social adaptive
outcomes, these results suggest specifc and increasing psy-
chosocial problems post-TBI in the context of severe injury.
Tese results, taken together with fndings from regres-
sion analyses, highlight the importance of injury severity
for sub-acute functional outcomes afer child TBI, a fnding
that has been well established in the literature [11,13]. More
severe injury, as measured by depth of coma in the 24 hours
postinjury and abnormalities identifed by CT and MRI, con-
tributed signifcantly to social skills, overall behavioral func-
tion, executive abilities and QOL. In contrast, age at injury
was less infuential, impacting only postinjury total adaptive
function, communication and daily living skills. Tis lack of
relationship may be explained by the age range under study,
with previous research identifying greatest risk for children
injures prior to age 5 years [13,14]. As expected, preinjury
function also had a major impact on postinjury function
for all domains under study. Investigation of environmental
factors indicated that SES was not infuential at six months
postinjury. While this fnding is in direct contradiction to
those reported by other groups [22], it may be that, in this
relatively early stage postinjury, the impact of psychosocial
factors is yet to emerge. Further follow-up of this sample is
needed to determine whether this is the case. Of note, the
more proximal infuence of family cohesion did emerge as a
predictor for parent ratings of everyday executive abilities.
Study limitations
Several methodological issues need to be considered when
interpreting these fndings. Firstly, the study design does not
include a noninjured control group. To minimize any con-
founds associated with our design, we employed only mea-
sures with robust psychometric properties with standardized
scores. Secondly, preinjury evaluations have been criticized as
potentially biased, with the possibility of a halo efect emerg-
ing, where parents idealize their injured child. In response
to this concern, we note that the total group and severity
group preinjury means for all measures included in the study
protocol indicate distributions similar to population expecta-
tions. Further, as severity groups did not difer on any of these
measures there is little evidence that such factors have had a
signifcant impact on our fndings. Finally, our ratings of both
pre and postinjury child function are primarily based on a
single source parent-ratings. Tis may result in a reporting
bias, and future studies should include multiple informants to
reduce the possibility of this occurring.
Clinical implications
Study fndings have important implications for management
and intervention, particularly as the timeframe for follow-up
of this sample (that is to 6 months postinjury) is in keeping
with the timing of intensive acute rehabilitation following
childhood TBI. Te most consistent fnding was the critical
importance of preinjury function in predicting abilities at 6
months postinjury. Tis suggests that allocation of manage-
ment and intervention resources, as well as decisions relating
to compensation payments, need to consider not only injury
severity, but also preinjury risk factors. Specifcally, children
with preinjury vulnerabilities may be at particular risk, with
such impairments exacerbated following TBI.
With respect to the relevance of injury severity, our results
indicate the expected dose-response relationship between
injury severity and outcome. Specifcally, where no preexist-
ing problems were present, mild TBI was associated with few
functional consequences at 6 months postinjury, and thus of
lowest priority for intervention services. Similarly, children
1646 V. Anderson etal.
Disability & Rehabilitation
with moderate TBI were also at relatively low risk for functional
impairments, with the exception of executive difculties, such
as poor planning, problem solving and working memory. In
contrast, more severe insult was associated with greatest risk
of functional difculties across all domains assessed, and it
follows that these children should be considered to have the
highest priority for rehabilitation services. Other risk factors
for poor outcome were earlier age at injury and lower levels
of family cohesion. Taken together, these fndings suggest
that the priorities for access to interventions focused on func-
tional abilities should be: (i) more severe injury; (ii) presence
of preinjury impairment; (iii) younger age at injury and (iv)
evidence of family dysfunction.
Study fndings also suggest some direction in terms of the
nature and focus of intervention services for children post-
TBI. Of note, our results, and those of others previously, indi-
cate that the level of functional impairment present postinjury
rarely meets criteria for a frank diagnosis (e.g. intellectual
impairment and psychiatric disorder) and thus children are
frequently ineligible for routine community supports. Despite
this, the degree of functional impairment clearly impacts on
QOL and community participation. Reduced executive skills
and social competence and elevated risk of behavioral distur-
bance would suggest that interventions that focus on these
domains should be a priority. Recently, the availability of
evidence-based interventions for these abilities has improved,
both for child-directed and family-based approaches [3742],
and a focus on such approaches should be considered as an
addition to traditional physical and cognitive techniques.
Conclusions
In conclusion, reporting on a large and well character-
ized sample of child survivors of TBI, our study has found
evidence to support the deterioration of everyday executive
skills, social function, and aspects of child behavior postinjury
in association with signifcant TBI sustained in childhood.
Preinjury functioning was the strongest predictor of function-
ing at 6 months post TBI. Injury severity was also signifcant
in the models tested and contributed to the prediction of dete-
rioration in child behavior, executive ability and QOL. Other
factors such as age at injury and family cohesion are relevant
to specifc outcome domains only, and SES was not identi-
fed as contributing signifcantly to outcome at this stage of
recovery. Tis study contributes to our understanding of the
changes observed in multiple functioning domains following
TBI in children. Results suggest that preinjury functioning as
reported by parents, considered in conjunction with injury
severity, may provide a powerful tool for identifying children
at high risk for subsequent difculties following TBI.
Declaration of Interest: NHMRC project grant (Kenardy,
Anderson, Bellamy & McKinlay).
References
1. Mitra B, Cameron P, Butt W. Population-based study of paediatric
head injury. J Paediatr Child Health 2007;43:154159.
2. National Institute of Health. NIH consensus development panel
on rehabilitation of persons with traumatic brain injury. JAMA
1999;282:974983.
3. Chadwick O, Rutter M, Brown G, Shafer D, Traub MU. A prospective
study of children with head injuries: II. Cognitive sequelae. Psychol
Med 1981;11:4961.
4. Jafe KM, Fay GC, Polissar NL, Martin KM, Shurtlef H, Rivara JB,
Winn HR. Severity of pediatric traumatic brain injury and early
neurobehavioral outcome: a cohort study. Arch Phys Med Rehabil
1992;73:540547.
5. Jafe KM, Fay GC, Polissar NL, Martin KM, Shurtlef HA, Rivara JM,
Winn HR. Severity of pediatric traumatic brain injury and neurobe-
havioral recovery at one year a cohort study. Arch Phys Med Rehabil
1993;74:587595.
6. Fletcher JM, Ewing-Cobbs L, Miner ME, Levin HS, Eisenberg HM.
Behavioral changes afer closed head injury in children. J Consult Clin
Psychol 1990;58:9398.
7. Kinsella GJ, Prior M, Sawyer M, Ong B, Murtagh D, Eisenmajer R,
Bryan D, etal. Predictors and indicators of academic outcome in chil-
dren 2 years following traumatic brain injury. J Int Neuropsychol Soc
1997;3:608616.
8. McCarthy ML, MacKenzie EJ, Durbin DR, Aitken ME, Jafe KM,
Paidas CN, Slomine BS, et al.; Childrens Health Afer Trauma
Study Group. Health-related quality of life during the frst year
afer traumatic brain injury. Arch Pediatr Adolesc Med 2006;160:
252260.
9. Taylor HG, Drotar D, Wade S, Yeates K, Stancin T, Klein S. Recovery
from traumatic brain injury in children: the importance of the family.
In: Broman SH, Michel ME, editors. Traumatic brain injury in chil-
dren. New York: Oxford University Press; 1995. pp 188218.
10. Anderson VA, Morse SA, Catroppa C, Haritou F, Rosenfeld JV. Tirty
month outcome from early childhood head injury: a prospective anal-
ysis of neurobehavioural recovery. Brain 2004;127:26082620.
11. Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Minich N. A
prospective study of short- and long-term outcomes afer traumatic
brain injury in children: behavior and achievement. Neuropsychology
2002;16:1527.
12. Anderson VA, Morse SA, Klug G, Catroppa C, Haritou F, Rosenfeld J,
Pentland L. Predicting recovery from head injury in young children: a
prospective analysis. J Int Neuropsychol Soc 1997;3:568580.
13. Anderson VA, Catroppa C, Haritou F, Morse S, Rosenfeld JV.
Identifying factors contributing to child and family outcome 30
months afer traumatic brain injury in children. J Neurol Neurosurg
Psychiatr 2005;76:401408.
14. Anderson V, Moore C. Age at injury as a predictor of outcome follow-
ing pediatric head injury. Child Neuropsychol 1995;1:187202.
15. Catroppa C, Anderson VA, Morse SA, Haritou F, Rosenfeld JV. Outcome
and predictors of functional recovery 5 years following pediatric trau-
matic brain injury (TBI). J Pediatr Psychol 2008;33:707718.
16. Ducrocq SC, Meyer PG, Orliaguet GA, Blanot S, Laurent-Vannier
A, Renier D, Carli PA. Epidemiology and early predictive factors of
mortality and outcome in children with traumatic severe brain injury:
experience of a French pediatric trauma center. Pediatr Crit Care Med
2006;7:461467.
17. Johnson AR, DeMatt E, Salorio CF. Predictors of outcome fol-
lowing acquired brain injury in children. Dev Disabil Res Rev
2009;15:124132.
18. Keenan HT, Bratton SL. Epidemiology and outcomes of pediatric
traumatic brain injury. Dev Neurosci 2006;28:256263.
19. McKinlay A, Kyonka EG, Grace RC, Horwood LJ, Fergusson DM,
MacFarlane MR. An investigation of the pre-injury risk factors asso-
ciated with children who experience traumatic brain injury. Inj Prev
2010;16:3135.
20. Tompkins CA, Holland AL, Ratclif G, Costello A, Leahy LF, Cowell V.
Predicting cognitive recovery from closed head-injury in children and
adolescents. Brain Cogn 1990;13:8697.
21. Rutter M, Chadwick O, Shafer D. Head injury. In: Rutter M, editor.
Developmental neuropsychiatry. New York: Guilford Press; 1983. pp
83111.
22. Yeates KO, Taylor HG, Drotar D, Wade SL, Klein S, Stancin T,
Schatschneider C. Preinjury family environment as a determinant of
recovery from traumatic brain injuries in school-age children. J Int
Neuropsychol Soc 1997;3:617630.
23. Asarnow F, Satz P, Light R, Zaucha K, Lewis R, McCleary C. Te
UCLA study of mild closed head injury in children and adolescents.
In: Broman SH, Michel ME, editors. Traumatic brain injury in chil-
dren. New York: Oxford University Press; 1995. pp 117146.
Pre- and post-TBI adaptive ability, behavior and QOL 1647
2012 Informa UK, Ltd.
24. Craf AW, Shaw DA, Cartlidge NE. Head injuries in children. Br Med
J 1972;4:200203.
25. Rutter M. Psychological sequelae of brain damage in children. Am J
Psychiatry 1981;138:15331544.
26. Dalby PR, Obrzut JE. Epidemiologic characteristics and seque-
lae of closed head-injured children and adolescents: a review Dev
Neuropsychol 1991;7:3568
27. Klonof H. Head injuries in children: predisposing factors accident
conditions, accident proneness and sequelae. Am J Public Health
1971;61:24052417.
28. Moyes CD. Epidemiology of serious head injuries in childhood. Child
Care Health Dev 1980;6:19.
29. Teasdale G, Jennett B. Assessment of coma and impaired conscious-
ness. A practical scale. Lancet 1974;2:8184.
30 McLennan W. Australian Standard Classifcation of Occupations. 2nd
ed. Canberra Australian Government Publishing Service; 1997.
31. Landgraf JM, Abetz L, Ware JE. Te CHQ Users Manual. 1st ed.
Boston, MA: Te Health Institute, New England Medical Center;
1996.
32. Wechsler D. Wechsler abbreviated scale of intelligence. San Antonio,
TX: Te Psychological Corporation; 1999.
33. Sparrow S, Balla DA, Cicchetti DV. Vineland Adaptive Behavior Scales:
Interview Edition, Survey Form Manual. Circle Pines, Minnesota:
American Guidance Services; 1984.
34. Achenbach TM. Manual for the Child Behavior Checklist/ 4-18 and
1991 profle. Burlington, VT: University of Vermont, Department of
Psychiatry; 1991.
35. Gioia GA, Isquith PK, Guy SC, Kenworthy L. Behavior Rating
Inventory of Executive Function. Odessa, FL: Psychological
Assessment Resources; 2000.
36. Schwartz L, Taylor HG, Drotar D, Yeates KO, Wade SL, Stancin T.
Long-term behavior problems following pediatric traumatic brain
injury: prevalence, predictors, and correlates. J Pediatr Psychol
2003;28:251263.
37. Hoof IV, Andersson K, Bergman B, Sejersen T, Von Wendt L, Bartfai
A. Benefcial efect from a cognitive training programme on children
with acquired brain injuries demonstrated in a controlled study. Brain
Inj 2005;19:511518.
38. vant Hoof I, Andersson, K, Bergman B, Sejersen T, von Wendt L,
Bartfai A. A randomized controlled trial on children with acquired
brain injuries reveals sustained favorable efects of cognitive training.
Neurorehabilitation 2007:22:109116.
39. Ylvisaker M, Feeney T. Executive functions, self-regulation, and
learned optimism in paediatric rehabilitation: a review and implica-
tions for intervention. Pediatr Rehabil 2002;5:5170.
40. Braga L. Rehabilitation and the role of the family. Brain Injury
2000:17:19.
41. Butler RW, Copeland DR. Attentional processes and their remediation
in children treated for cancer: a literature review and the development
of a therapeutic approach. J Int Neuropsychol Soc 2002;8:115124.
42. Wade SL, Michaud L, Brown TM. Putting the pieces together: pre-
liminary efcacy of a family problem-solving intervention for chil-
dren with traumatic brain injury. J Head Trauma Rehabil 2006;21:
5767.
Copyright of Disability & Rehabilitation is the property of Taylor & Francis Ltd and its content may not be
copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written
permission. However, users may print, download, or email articles for individual use.
S-ar putea să vă placă și
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5795)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- National Building Code 2005Document17 paginiNational Building Code 2005Shivraj ThakareÎncă nu există evaluări
- Program Assessment Tool Kit:: A Guide To Conducting Interviews and Surveys A Guide To Conducting Interviews and SurveysDocument74 paginiProgram Assessment Tool Kit:: A Guide To Conducting Interviews and Surveys A Guide To Conducting Interviews and Surveyswinter55Încă nu există evaluări
- Report 3 - WACSDocument64 paginiReport 3 - WACSiking balonÎncă nu există evaluări
- CEX 6331 - Construction Engineering and Management Submit Answers ToDocument2 paginiCEX 6331 - Construction Engineering and Management Submit Answers ToNero PereraÎncă nu există evaluări
- Beliefs, Practices, and Reflection: Exploring A Science Teacher's Classroom Assessment Through The Assessment Triangle ModelDocument19 paginiBeliefs, Practices, and Reflection: Exploring A Science Teacher's Classroom Assessment Through The Assessment Triangle ModelNguyễn Hoàng DiệpÎncă nu există evaluări
- Study Guide For Pipher Intro Chapter 1 Chapter 2Document2 paginiStudy Guide For Pipher Intro Chapter 1 Chapter 2api-253671419Încă nu există evaluări
- Michigan School Funding: Crisis and OpportunityDocument52 paginiMichigan School Funding: Crisis and OpportunityThe Education Trust MidwestÎncă nu există evaluări
- Kolej Vokasional Jabatan PerniagaanDocument9 paginiKolej Vokasional Jabatan PerniagaanMeister PrabaÎncă nu există evaluări
- Progress Test Files 1-6 Answer Key A Grammar, Vocabulary, and PronunciationDocument8 paginiProgress Test Files 1-6 Answer Key A Grammar, Vocabulary, and PronunciationEva Barrales0% (1)
- Anchor Chart PaperDocument2 paginiAnchor Chart Paperapi-595567391Încă nu există evaluări
- The Discipline of Social WorkDocument29 paginiThe Discipline of Social WorkRachel Valenzuela54% (13)
- 0405Document38 pagini0405chuviethung1997Încă nu există evaluări
- 2022 Book PrimaryAndSecondaryEducationDuDocument467 pagini2022 Book PrimaryAndSecondaryEducationDuFRANCISCA INDIRA CABRERA ARAYAÎncă nu există evaluări
- CorrectionsDocument337 paginiCorrectionsUnited States Militia100% (2)
- Republic of The Gambia: Ministry of Basic and Secondary Education (Mobse)Document43 paginiRepublic of The Gambia: Ministry of Basic and Secondary Education (Mobse)Mj pinedaÎncă nu există evaluări
- 7 Strategies To Ignite Your Team's CreativityDocument8 pagini7 Strategies To Ignite Your Team's CreativityvarunbsbÎncă nu există evaluări
- The Educational Value of Crossword PuzzlesDocument1 paginăThe Educational Value of Crossword PuzzlesbangyansygÎncă nu există evaluări
- IGCSE Science (Double Award) TSM Issue 2Document52 paginiIGCSE Science (Double Award) TSM Issue 2frogfloydÎncă nu există evaluări
- One Size Fit AllDocument8 paginiOne Size Fit AllneelsafdarÎncă nu există evaluări
- CV - Hendro FujionoDocument2 paginiCV - Hendro FujionoRobert ShieldsÎncă nu există evaluări
- UTS Character StrengthsDocument3 paginiUTS Character StrengthsangelaaaxÎncă nu există evaluări
- Shs Class RecordDocument62 paginiShs Class RecordMae Sheilou Conserva PateroÎncă nu există evaluări
- Department of Education: Weekly Learning Activity PlanDocument2 paginiDepartment of Education: Weekly Learning Activity PlanSaz RobÎncă nu există evaluări
- Reyes Tag Ppt-PrefinalsDocument11 paginiReyes Tag Ppt-PrefinalsRaphaella Mae Alegre ReyesÎncă nu există evaluări
- Ya'qūb Ibn Is Āq Al-Kindī, Alfred L. Ivry-Al-Kindi's Metaphysics - A Translation of Ya'qūb Ibn Is Āq Al-Kindī's Treatise On First Philosophy (Fī Al-Falsafah Al-Ūlā) - SUNY (1974) PDFDocument215 paginiYa'qūb Ibn Is Āq Al-Kindī, Alfred L. Ivry-Al-Kindi's Metaphysics - A Translation of Ya'qūb Ibn Is Āq Al-Kindī's Treatise On First Philosophy (Fī Al-Falsafah Al-Ūlā) - SUNY (1974) PDFDwi Afrianti50% (2)
- Registration As An Apec ArchitectDocument6 paginiRegistration As An Apec ArchitectTonyDingleÎncă nu există evaluări
- Teaching Arts in The Elementary Grades: OgdimalantaDocument12 paginiTeaching Arts in The Elementary Grades: OgdimalantaDiana Rose SimbulanÎncă nu există evaluări
- Loyola International School, Doha, Qatar. Academic Session 2020 - 2021 Home-School Weekly Plan (05-04-2020 To 09-04-2020) Class - KG-IIDocument3 paginiLoyola International School, Doha, Qatar. Academic Session 2020 - 2021 Home-School Weekly Plan (05-04-2020 To 09-04-2020) Class - KG-IIAvik KunduÎncă nu există evaluări
- CV Main EnglishDocument2 paginiCV Main EnglishArie KelmachterÎncă nu există evaluări
- Catch Up Plan Template Division of Romblon1Document12 paginiCatch Up Plan Template Division of Romblon1MICHELLE RAFAELÎncă nu există evaluări