Documente Academic
Documente Profesional
Documente Cultură
Mother To Child Transmition of HIV
Încărcat de
Genoveva Maditias Dwi PertiwiDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Mother To Child Transmition of HIV
Încărcat de
Genoveva Maditias Dwi PertiwiDrepturi de autor:
Formate disponibile
Women and Health Learning Package: MTCT of HIV/AIDS
www.the-networktufh.org
1
MOTHER-TO-CHILD TRANSMISSION (MTCT) OF HIV/AIDS
Women and Health Learning Package
Developed by The Network: TUFH Women and Health Taskforce
Second edition, September 2006
Support for the production of the Women and Health Learning Package (WHLP) has been provided
by The Network: Towards Unity for Health (The Network: TUFH), Global Health through Education,
Training and Service (GHETS), and the Global Knowledge Partnership. Copies of this and other
WHLP modules and related materials are available on The Network: TUFH website at
http://www.the-networktufh.org/publications_resources/trainingmodules.asp or by contacting GHETS
by email at info@ghets.org, or by fax at +1 (508) 448-8346.
About the author
Rosebella O. Onyango, BEd, MSc, (Community Health), PhD (Childhood Nutrition)
Senior Lecturer and Director, School of Public Health and Community Development
Maseno University
Maseno, Kenya
Dr Onyango is a public health nutritionist and a trained teacher and researcher, with many
years of teaching, administrative, and research experience at various educational levels.
Eighteen years of that experience have been in teacher training institutions and universities.
She is also an external examiner for nutrition exams in Egerton and Moi Universities, Kenya.
She supervises postgraduate students on a variety of nutrition and public health research
projects.
Dr Onyango has carried out studies on infant feeding in the HIV/AIDS era, nutritional status
and health of children, and related family socioeconomic and environmental factors. Her
research focus is on both pre-school children and women. She has worked with womens
groups in slums and rural settings to improve of maternal and child health and nutrition. She
is a member of Kenya Coalition for Action in Nutrition (K-CAN) and Regional Centre of
Quality Health Care (RCQHC). She is also a member of The Network: TUFH Women and
Health Taskforce.
Her current research interests are in infant feeding in the HIV/AIDS era and home-based
health care for people living with HIV/AIDS (PLWHA). Dr Onyango is a trainer of trainers
for nurses and other health workers in prevention of mother-to-child transmission (PMTCT)
of HIV.
Women and Health Learning Package: MTCT of HIV/AIDS
www.the-networktufh.org
2
MOTHER-TO-CHILD TRANSMISSION (MTCT) OF HIV/AIDS
Global Overview
The HIV/AIDS epidemic has become a major problem in many countries globally and
continues to have a devastating effect on sub-Saharan Africa. The overwhelming majority of
HIV-infected peoplemore than 90%live in developing countries. Adults living in sub-
Saharan Africa are 10 times more likely to be infected with HIV than adults living in North
America, and 20 times more likely than adults living in Western Europe. Eighty percent of
women currently living with HIV are in sub-Saharan Africa, and out of all the children born
with HIV globally, 90% are in this same region.
Prevention of mother-to-child transmission (MTCT) of HIValso known as vertical,
perinatal or parent-to-child transmission (PTCT) to reflect the role of men in the overall chain
of transmission has become a priority for many developing country governments and
agencies. This priority is consistent not only with the broader goals of HIV/AIDS prevention,
but also with commitments to improving child health and survival.
Infants and children in Africa are infected by HIV/AIDS in multiple ways. Those who are
most directly affected are children who acquire HIV/AIDS through MTCT. They face severe
morbidity and near-certain death where sophisticated and costly treatments are nonexistent
and even the availability of basic medicines to treat opportunistic infections is likely to be
erratic. Infant mortality rates, although reduced between 1981 and 1986, have now risen
dramatically, largely due to AIDS. Almost all AIDS deaths in Africa in young children can
be traced back to MTCT.
In developed countries, MTCT rates have fallen to as low as 2% of births among HIV-
infected mothers in recent years with the introduction of HIV counselling and testing, short-
course zidovudine (ZDV) or azidothymadine (AZT) prophylaxis, elective Caesarean delivery
and safe use of infant formula instead of breastfeeding. In Africa, however, where prolonged
breastfeeding is the norm, about 25-35% of HIV-infected mothers pass on the disease to their
infants.
The severity of the MTCT problem in sub-Saharan Africa is due to a number of factors,
including high rates of HIV infection in women of reproductive age, a large total population
of women of reproductive age, high birth rates, and a lack of effective MTCT prevention
interventions. Rates of infections in women are high in sub-Saharan Africa and are growing
rapidly.
Transmission of HIV through breast milk is of concern in many developing countries where
HIV infection in women is common and breastfeeding is universally practiced. In Africa, 30-
40% of children born to HIV-infected women acquire HIV, and 30-50% of infected infants
acquire the disease through breastfeeding. This has reversed previous gains made in child
survival and has eroded health worker confidence in recommending breastfeeding as the best
and safest form of infant feeding.
Promotion of exclusive breastfeeding as the best possible nutrition for infants has been the
cornerstone of child health and survival strategies for the past 20 years, and has played a
major part in lowering infant mortality in many regions of the world. Therefore, the evidence
that has accrued over recent years that breast milk is a significant source of HIV infection has
Women and Health Learning Package: MTCT of HIV/AIDS
www.the-networktufh.org
3
caused a real dilemma for mothers, health personnel, and policymakers. Today, decisions
about infant feeding in settings of high HIV prevalence require a careful balancing of risks,
with the risk of transmitting HIV on one side and the risk of morbidity, mortality and
stigmatisation that can result from not breastfeeding on the other. Breastfeeding is nearly
universal in Africa, making balancing the risks especially challenging.
Malnutrition has been endemic in Africa for decades, complicated by a combination of
factors and more recently by the impact of AIDS. It is estimated that one-third of all children
under five in sub-Saharan Africa are stunted, and more than half suffer from some form of
micronutrient malnutrition. Malnutrition is also common among adults in most parts of
Africa, where more than half of all pregnant women suffer from anaemia.
HIV/AIDS and malnutrition are inextricably interrelated. Studies show that malnutrition
increases both the risk of HIV transmission from mothers to babies and the progression of the
HIV infection. In turn, HIV infection exacerbates malnutrition through its attacks on the
immune system and its impact on nutrient intake, absorption, and utilisation. This puts the
lives of HIV-infected infants at risk from both malnutrition and AIDS-related infections.
The severity of the MTCT problem in sub-Saharan Africa is due to high rates of HIV
infection in women of reproductive age, a large total population of women of reproductive
age, high birth rates, and the lack of effective MTCT prevention intervention.
An estimated 330,000 children younger than five died in the sub-Saharan Africa in 1999 from
HIV infections. Four countries (Botswana, Namibia, Swaziland, and Zimbabwe) have rates of
HIV-attributable under-five mortality of above 30 per 1000, and an additional 16 countries
have rates between 10 and 25 per 1000.
Regional Overview: Kenya
Women and Health Learning Package: MTCT of HIV/AIDS
www.the-networktufh.org
4
Population Profile: Kenya
Total Population 31.3 million
Annual Population growth Rate (%) 1.53
Rate of annual increase in population 3.5%
Total Fertility Rates (TFR) (15-49 years) 5.0
Infant Mortality Rate (IMR)(Per 1000) 78
Under-five Mortality Rate 114
Crude birth rate (per 1000 live births) 29.35
Crude death rate (per 1000 live births) 14.8
Life expectancy (women) 49 years
HIV-infected 1.4 million
AIDS deaths 140,000 adults in 2003
AIDS orphans 890,000
HIV Prevalence (women 15-49) in Urban 12.3%
HIV Prevalence (women 15-49) in Rural 7.5%
HIV Prevalence (men 15-49) In Urban 7.6%
HIV Prevalence (men 15-49) In Rural 3.5%
HIV Prevalence (women 15-49) Total 8.7%
HIV Prevalence (men 15-49) Total 4.5%
HIV Prevalence Total 6.7%
It is estimated that 2.2 million Kenyans are now living with HIV, but few of them know that
they are infected or show symptoms of the disease, and only about 200,000 have AIDS
(Government of Kenya, 2001). Results of the Kenya Demographic and Health Survey
(KDHS) in 2003 indicated that the national prevalence rate derived from women participating
in a 2003 sentinel surveillance program was 9.4%. Gender differences were most striking in
young people. In the 15-19 age group, 3.5% of women and only 0.5% of men were infected,
while in the 20-24 year age group, 8.7% of women and 2.4% of men were infected (KDHS,
2003). It is projected that AIDS will increase the death rate at all ages. However, the impact
will be most severe among young adults and children under the age of five. This rapid
increase in young adult deaths will have serious consequences for economic and social
development.
Kenya has a severe, generalized HIV epidemic, with approximately 1.25 million adults and
over 100,000 children infected. The KDHS 2003 found a prevalence of 9% in adult women
and 5% in adult men. Surveillance of HIV in pregnant women has been conducted annually
since 1990, with prevalence rising to 16% in urban areas and 8% in rural areas in the late
1990s, but now showing signs of decline in some regions. Only 14% of Kenyan adults know
their HIV status, limiting their access to care.
The seroprevalence rate of HIV among pregnant women in Africa exceeds 20% in many
areas. In Kenya, the HIV prevalence in urban areas was reported to range between 4-10% in
low seroprevalence sites and 35% in high seroprevalence sites.
With the observed trends, the percentage of pregnant women who are HIV-infected is
increasing at an alarming rate. Up to 90% of HIV infections in pregnant women are due to
heterosexual contact.
Women and Health Learning Package: MTCT of HIV/AIDS
www.the-networktufh.org
5
More than five million children worldwide have been infected with HIV, almost all through
mother-to-child transmission. The figures are sobering: in 2002 alone, for example, more
than 800,000 children became infected with HIV. Ninety percent of these infections occur in
sub-Saharan Africa, where AIDS has increased infant mortality in the most severely affected
countries. Kenya is counted among one of the countries that are most severely affected by
HIV/AIDS pandemic in Africa.
There was an increase in both the infant mortality rate and under-five mortality rates between
the KDHS of 1989 and 2003. For example, the infant mortality rate increased by 30%, from
60 deaths per 1000 live births in 1989, to 78 in 2003. Similarly, the under-five mortality rate
showed an increase of 30% during the same period. The trend depicts continued deterioration
in the quality of life amongst the Kenyan population over the last 20 years. Some of these
deaths can be attributed to HIV-related infections. This same trend is likely to be found in
poor African countries with similar burdens of HIV/AIDS infections.
Five Key Gains in Breastfeeding and PMTCT in Kenya
The Global AIDS Program has initiated the following:
1. Provision of financial and technical support for the development of a 5-year (2001-
2005) national PMTCT strategy that provides guidelines and a framework for
coordinated program implementation
2. Support for PMTCT services in 18 facilities (including one offering PMTCT+)
3. Integration of voluntary counselling and testing (VCT) and PMTCT into maternal and
child clinics in most hospitals and rural health centres.
4. Campaigns on breastfeeding promotion
5. Provision of mobile VCT services by the Ministry of Health for hard-to-reach
populations.
Five Key Challenges to Infant feeding and MTCT
1. Culturally, every mother is expected to breastfeed her baby, and any deviation from
this practice raises many questions in the family, subjecting the mother to stigma.
2. Lack of appropriate and nutritionally adequate complementary foods for infants.
3. Lack of safe water and poor hygienic practices making the preparation of
complementary foods unsafe.
4. Poor infrastructure at health facilities hindering accessibility to most areas where
there is need for VCT and PMTCT initiatives.
5. Lack of knowledge of HIV status by pregnant women (many women, even when
tested, are afraid to check the test results).
Five Key Factors Increasing MTCT
1. Widespread poverty
2. Low literacy among rural women
3. Home deliveries by traditional birth attendants (TBAs)
4. High rate of HIV infection among women
5. Religious groups that discourage the use of contraceptives, especially condoms
Women and Health Learning Package: MTCT of HIV/AIDS
www.the-networktufh.org
6
Infant Feeding Patterns among Kenyan Women
Breastfeeding and the introduction of supplemental foods are important determinants of the
nutritional status of children, especially those under two years.
Supplementation of breast milk starts quite early in Kenya. Exclusive breastfeeding (breast
milk only) is not common, as only 29% of children under two months and 9% of those under
four months of age are exclusively breastfed. Most of the supplements given are plain water,
water-based liquids, juice, or other milks.
Fifteen percent of babies under two months and 45% of those aged 2-3 months are given
complementary food, presumably mushy or semi-solid food. By the age of 4-5 months, two-
thirds of the children are given complementary foods (KDHS).
Since most mothers in the rural areas are poor and lack safe drinking water and adequate
nutritious complementary foods for the infants, such infants are often fed with nutritionally
inadequate complementary foods prepared in unhygienic conditions. This predisposes such
infants to diarrhoeal illnesses and other infections, increasing both their morbidity and their
mortality.
In 1999, 10% of reported AIDS cases in children were in those under 5 years of age, out of
which 90% of the HIV infections were due to MTCT. It is estimated that the number of
infants infected with HIV per year in Kenya is 100,000. Transmission of HIV from infected
mothers to their babies can occur during the antenatal period (10-20%), labour and delivery
(35-50%), and breastfeeding (14-22%). In order to reduce MTCT, these key HIV
transmission areas must be targeted.
MTCT Prevention Components
Efforts to prevent MTCT should relate to and be considered within the entire spectrum of
HIV/AIDS primary prevention, care and support activities as shown in Table 1.
Table 1: MTCT and the Prevention to Care Continuum
Primary Prevention of
HIV/AIDS in Adults
Core interventions for the
Prevention of MTCT
Care and support
Promotion and provision of
condoms
Behaviour change
communication (including
education and involvement
of partners, families and
communities; life skills and
other programs targeted to
youths)
Prevention and treatment of
sexually transmitted
diseases
Voluntary counselling and
Testing (VCT)
Comprehensive MCH
services (antennal,
postnatal, and child health).
VCT
Improved breastfeeding and
alternative infant feeding
counselling and practices
Optimal Obstetric care
Short-course antiretroviral
(ARV) prophylaxis
Family planning
Postpartum care for
mothers (including family
planning)
Postpartum care for infants
(including identification,
treatment of and palliative
care for AIDS-related
conditions)
Social support for families
and communities affected
by HIV/AIDS, especially
orphans and vulnerable
children
Support to carry out infant
feeding decisions
Women and Health Learning Package: MTCT of HIV/AIDS
www.the-networktufh.org
7
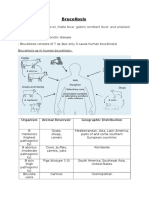
Mechanisms, Timing and Risk Factors of MTCT
MTCT in Africa is the tragic result of a chain of events that most often involves an HIV-
positive man infecting his female partner through unprotected sexual activity, and the partner
infecting her next baby, and potentially several more babies, during the remainder of her
reproductive life. To reflect the important role that men play in this chain of transmission,
some organisations have replaced the biologically precise terminology of mother-to-child
transmission with the behaviourally-sensitive term parent-to-child-transmission.
Infants who acquire HIV infection from their mothers do so during pregnancy (5-10%),
during labour and delivery (10-20%), or after birth through breastfeeding (10-20%). Infection
can also occur after birth through contact with infected blood, blood products, or unsterile
medical equipment, though this is extremely rare even in Africa. Efforts to improve the safety
of the blood supply, to avoid unnecessary delivery-related blood transfusions, and to improve
infection control practices have probably further reduced the incidence of non-MTCT
transmission in infants.
HIV Transmission during pregnancy
In most HIV-infected women, HIV does not cross the placenta from mother to the foetus, and
the placenta actually shields the foetus from HIV. This protection from the placenta may
break down if:
The mother has a viral, bacterial, or parasitic placental infection
The mother becomes infected with HIV during the pregnancy, and hence develops a
high level of HIV for a short time
The mother has severe immune deficiency associated with AIDS
Thus, maternal conditions including untreated placental infections (particularly malaria),
recent HIV infection, and advanced HIV disease have all been cited as risk factors for
MTCT. In addition, malnutrition during pregnancy may directly contribute to MTCT.
HIV transmission during labour and delivery
Infants of infected mothers are at great risk of becoming infected with HIV during childbirth.
During this event, 10-20% of such infants will become infected if no steps are taken to
prevent transmission. Most infants who acquire HIV during labour and delivery do so by
sucking, imbibing or aspirating maternal blood or cervical secretions that contain HIV. The
duration of membrane rupture (deliberately performed to augment or induce labour), acute
chorioamnionitis (resulting from untreated sexually transmitted infections (STIs) or other
infections) and invasive delivery techniques that increase the babys contact with the
mothers blood have been associated with higher risks of MTCT during labour and delivery.
HIV Transmission through breastfeeding
HIV is present in breast milk, although the viral concentrations in breast milk are
significantly lower than those found in blood. On average about 15% of babies born to HIV-
positive mothers will become infected through sustained breastfeeding (24 months or more).
Women and Health Learning Package: MTCT of HIV/AIDS
www.the-networktufh.org
8
Transmission of HIV during breastfeeding is a multi-factorial process. Studies suggest that
the risk of MTCT through breastfeeding depends on a number of factors:
Pattern of breastfeeding (babies who are exclusively breastfed may have lower risk of
becoming infected than those who also consume other liquids, milks, or solid foods in
the first months of life)
Breast health (mastitis, cracked and bloody nipples, and other indications of breast
inflammations are associated with higher risks of transmission)
Breastfeeding duration
Maternal viral load (which is higher with recent infections or advanced disease of the
mother)
Maternal immune status
Maternal nutritional status
The risk of MTCT is believed to double (to about 30%) if the mother becomes infected with
the virus while still breastfeeding. This highlights the importance of primary prevention of
HIV in lactating women.
The risk of HIV transmission through breastfeeding is higher if infants are given both breast
milk and formula (mixed feeding). According to WHO recommendations, HIV- positive
women should be encouraged either to exclusively breastfeed or exclusively formula feed,
but not both.
Primary prevention of HIV infection in infants
Strengthening and scaling up primary prevention of HIV/AIDS to keep men and women of
productive age from becoming HIV-infected themselves must be a priority strategy for
preventing MTCT worldwide. Primary prevention efforts have shown success in stabilising
or reducing HIV infection rates in countries such as Senegal, Uganda, and Thailand, where
they were introduced early in the epidemic and there was strong political commitment,
funding and broad coverage. Considerably more is known now about lessons learnt and best
practices related to achieving primary prevention than in early years of the epidemic.
Primary prevention at the community level traditionally relies on three major components,
each of which can include prevention of mother-to-child transmission.
Promotion and provision of free, subsidised, and/or commercially marketed condoms
Condoms are effective against HIV transmission when used correctly and consistently, but
this is not always understood or accepted by people at risk. Condoms are not always available
at high-risk sites such as brothels and discos (youth dancing places). Hence, both promotion
and provision are important. Programs that promote condom use for HIV prevention should
emphasise their role in prevention of MTCT as well as prevention of disease in sexually
active adults.
Behaviour change communication (BCC) efforts
BCC aims at reducing behaviours that place individuals at risk of becoming HIV-infected or
spreading the virus to uninfected partners by providing accurate information about individual
Women and Health Learning Package: MTCT of HIV/AIDS
www.the-networktufh.org
9
risks, modes of transmission of HIV, and effective means to avoid transmission. It also seeks
to motivate individuals to use information consistently and appropriately. BCC programs
need to include information about MTCT in their strategies. These messages should include
information about risks of MTCT during pregnancy and delivery and through breastfeeding,
and should encourage people to see VCT counsellors or health providers for more
information on how to prevent HIV/AIDS among infants and young children.
Prevention, diagnosis and treatment of STIs
STI prevention and treatment programs are important because the presence of untreated STIs
is now known to increase the risk of transmitting and acquiring HIV. Men and women who
are at risk or have contracted an STI are sexually active and are therefore an appropriate
target audience for information on MTCT risks and prevention. STI services should include
information on the risk of MTCT, modes of transmission, and encouragement to see a VCT
counsellor or health provider for more information on how to prevent HIV/AIDS among
infants and young children.
In addition to the three components described above, MTCT messages should be integrated
into all HIV/AIDS education including life skills curricula, adolescent outreach programs,
programs to reach men and school- and faith-based AIDS education programs.
Activities for primary prevention of MTCT
Develop social marketing programs for condoms and provide free, subsidised and/or
commercially marketed condoms
Condom quality assurance
Promote condom use during pregnancy to prevent infection with HIV and other STIs
Provide training and technical assistance in BCC best practices
Use BCC for primary prevention, including messages and materials development that
target pregnant women and couples.
Identify and promote effective sex negotiation skills
Empower women to negotiate for safer sex with their partners
Support educational printing, radio or TV program development and air time
Provide training in STI prevention, diagnosis and treatment
Provide STI medications
Develop STI syndromic management guidelines
Secure funding for surveys of community knowledge, attitudes and practices related
to HIV/AIDS
Conduct activities to promote political will and support by community leaders
Implement educational and outreach efforts aimed at community members, especially
related to MTCT
Support community-based voluntary counselling and testing (VCT) services
Promote VCT before marriage and before pregnancy
Conduct research in factors influencing mother-to-child transmission of HIV
Prevent vertical transmission through screening, family planning, and health
education
Women and Health Learning Package: MTCT of HIV/AIDS
www.the-networktufh.org
10
Intensify efforts to prevent HIV infection in young women
Ensure that HIV-positive women have access to family planning counselling and
services
Activities to promote safe infant feeding
Review and update national breastfeeding and related infant feeding practices
Review status of the national code for marketing of breast milk substitutes and
support efforts to enforce it.
Support and expand Baby Friendly Hospital Initiatives (BFHI) and ensure that all
infant feeding training include updated information on MTCT
Conduct formative research to adapt United Nations guidelines on infant feeding and
HIV at local settings and ascertain locally available replacement feeding options
Adapt Integrated Management of Childhood Illness (IMCI) and other feeding
guidelines to local settings as needed
Support training on counselling about HIV and infant feeding options (using or
adapting the WHO/UNICEF training package)
Strengthen training in lactation management
Strengthen efforts to promote and support exclusive breastfeeding for six months for
all breastfeeding mothers, including mother-to-mother support in the first months of
life
Strengthen nutrition and health support for mothers, especially HIV-infected mothers
who choose replacement feeding
Explore ways to make replacement feeding safer for HIV-infected mothers, including
clean water, food hygiene and sanitation improvement
Review and update pre-service training curricula for nurses, midwives, nutritionists,
social workers and all other medical/health personnel regarding MTCT issues and
breastfeeding
Strengthen growth monitoring and promotion programs for early identification of
growth faltering
Monitor breastfeeding/infant feeding trends in areas of high HIV prevalence
Monitor media reporting on HIV, MTCT and breastfeeding issues and disseminate
appropriate information
Ways to prevent breast milk transmission of HIV
Provide breastfeeding assistance and counselling, including information on HIV and
breastfeeding in areas with high HIV prevalence.
Avoid breastfeeding completely, or if the woman opts to breastfeed:
Encourage exclusive breastfeeding with abrupt weaning, and avoid mixed feeding
Reduce the duration of breastfeeding to six months, and ensure that this
breastfeeding is exclusive
Avoid breastfeeding when the mother has a breast disease such as mastitis or
cracked nipples
Aggressively treat oral thrush or ulcers in the baby
Women and Health Learning Package: MTCT of HIV/AIDS
www.the-networktufh.org
11
The Essential Package for Preventing MTCT
Prevent HIV infection in young women
Provide family planning counselling for HIV-positive women
Improve maternal health and nutritional status during pregnancy
Screen for STIs in pregnant women and treat them
Reduce maternal viral load using currently recommended regimens of antiretroviral
(ARV) drugs both in antenatal and postnatal periods
Administer the recommended ARV, such as Nevirapine, to the mother (200 mg
orally) during labour
Administer the recommended ARV, such as Nevirapine, to the infant within 72 hours
after birth (2mg/kg body weight syrup)
Use malaria chemoprophylaxis in malaria-endemic areas
Avoid invasive procedures during labour and delivery
Counsel mothers to immediately and exclusively breastfeed, and provide information
on HIV and breastfeeding in areas with high HIV prevalence
Benefits of Reduction of Mother-to-Child Transmission of HIV
Decreases numbers of HIV-infected children
Increases child health and survival
Decreases the load on the health system
Gives an opportunity to improve and expand health services and strengthen the health
infrastructure
Maternal and Infant Risk factors for MTCT of HIV
1. Maternal nutritional status has been found to play a role in MTCT of HIV. Vitamin A
deficiencies in HIV-infected women increases the likelihood that they will transmit
the virus to their infants.
2. Infections of the placenta and the umbilical cord are associated with increased MTCT
of HIV. Infections such as STIs and malaria reduce the effectiveness of the placental
barrier against foetal infections.
3. Premature delivery increases the risk of MTCT of HIV. Prematurity may be a
consequence of infections such as STIs and malaria, or may be due to poor maternal
nutrition.
The Effects of HIV/AIDS on Infant Feeding
Studies have shown that about 15-16% of infants born to HIV-positive mothers are at risk of
HIV transmission through breastfeeding, in addition to the risk during pregnancy and
childbirth.
If the mother becomes infected during pregnancy or lactation, the risk of transmission is
estimated to be as high as 29%. Out of the 3.6 million HIV-infected children globally,
approximately 1.2-1.8 million have been affected through breastfeeding. HIV-positive
Women and Health Learning Package: MTCT of HIV/AIDS
www.the-networktufh.org
12
women therefore need to be educated about HIV transmission through breast milk and about
options to protect their children.
Promotion of exclusive breastfeeding as the best possible nutrition for infants has been the
cornerstone of child health and survival strategies for the past two decades, and has played a
major part in lowering infant mortality in many regions of the world.
It has been reported that the risk of HIV transmission may be lower when exclusive
breastfeeding is practised. This is because HIV is more likely to pass through the infants gut
wall when the wall is disturbed (as happens when solids are introduced prematurely or when
pathogens are introduced through unhygienic preparation of formula or other foods).
Exclusive breastfeeding of infants is generally recommended for the first six months of their
lives, and breastfeeding with complementary foods thereafter, preferably up to twenty-four
months. Breastfeeding has many physical and psychological benefits for infants and mothers,
as well as economic benefits to households and communities.
Benefits of breastfeeding to the infant
Provides a nutritionally complete food
Strengthens the infants immune system, thus preventing many infections
Reduces the infants exposure to infections
Safely rehydrates and provides essential nutrients to a sick child, especially those
suffering from diarrhoeal diseases
Contributes to birth spacing and thus increases the childs chances of survival
Benefits of breastfeeding to the mother
Reduces the womans risk of excessive blood loss after delivery
Provides natural method of delaying pregnancy through the lactational amenorrhea
method (LAM)
Reduces the risk of ovarian cancer, breast cancer, and osteoporosis (bone disease)
Benefits to the household and community
Conserves the funds that otherwise would have been spent on breast milk substitutes,
supplies, and fuel to prepare the substitutes
Saves medical costs to families and governments by preventing illness and by
providing postpartum contraception
The emergence of HIV/AIDS has negatively affected the gains made by breastfeeding
campaigns in the 1990s. This valuable infant food and nutrient source and its many benefits
are now threatened by the HIV/AIDS pandemic. When alternative complementary feeds are
given to infants, all the benefits of breast milk are compromised or lost.
The World Health Organisation (WHO) recommends that Voluntary Counselling and Testing
(VCT) be provided to all pregnant women to allow for informed decision-making about
breastfeeding. For women who are HIV positive, the WHO in 1999 outlined breastfeeding
guidelines, giving four options:
Women and Health Learning Package: MTCT of HIV/AIDS
www.the-networktufh.org
13
1. Give suitable a replacement for breast milk, provided it is affordable for six months
and can be prepared accurately and hygienically. The risk of HIV infection by breast
milk is thereby eliminated.
2. Where suitable replacement feeding is not possible, exclusively breastfeed for 3-6
months followed by abrupt cessation, thus largely reducing the risk of HIV
transmission.
3. Manually express and heat-treat breast milk, or use a breast milk bank.
4. Use a wet nurse who is documented HIV-negative and accepts the risk of being
infected by the baby.
Infant Feeding Practices
The WHO/UNIAIDS/UNICEF guidelines on HIV and infant feeding (WHO 1998)
recommend that HIV-positive mothers should be counselled on the advantages and
disadvantages of different infant feeding options and should be assisted to select the best
option given their specific circumstances. It is the mother who makes the final choice on how
to feed her child, and she should be supported in whatever method she chooses.
In resource-limited settings, HIV-positive mothers have been faced with a dilemma over
feeding options, given that they cannot afford formula feeding, and moreover lack safe water,
adequate fuel, and good sanitation with which to prepare the formula.
Their situation is made worse by cultural child feeding practices and the stigma associated
with HIV/AIDS.
Studies from the south Saharan region indicate that although breastfeeding is the most
prevalent form of infant feeding, exclusive breastfeeding rates are extremely low. A study on
infant feeding practices in Tanzania and Uganda showed that the average breastfeeding
periods were 24.0 and 18.3 months respectively. But in Tanzania, half the study participants
had introduced liquids by 4 months while Uganda participants reported introducing liquids by
6 months. Water and other liquids are given to infants very early in life by most sub-Saharan
African mothers.
Women and Health Learning Package: MTCT of HIV/AIDS
www.the-networktufh.org
14
REFERENCES
Anderson VA (1997). The placental barrier to maternal HIV infection. Obstetrics and
Gynaecology Clinical North America 24 (2): 797-820.
Dabis F, Newell ML, Fransen L, et al. (2000). Preventing mother-to-child transmission of
HIV in Developing countries: Recommended Practice. Health Policy Plan 15 (1): 39-42.
Central Bureau of Statistics (2003). Kenya Demographic and Health Survey (KDHS).
Coutsoudis A, Pillay K, Kuhn L, Spooner E, Coovadia HM (1999). Influence of infant
feeding pattern on early mother-to-child transmission of HIV-1 in Durban, South Africa: a
prospective cohort study. South African vitamin A study group. Lancet 354 (9177): 471-6.
Coutsoudis A, Pillay K, Kuhn L, Spooner E, Coovadia HM (2001). Method of infant-feeding
and transmission of HIV=1 from mothers to children by 15 months of age: A prospective
cohort study from Durban, South Africa. AIDS 15:379-87
deCock K, Fowler MG, Mercier E, et al. (2000b). Prevention of mother-to-child HIV
transmission in resource-poor countries. Journal of American Medical Association. 283:
1175-82.
Dunn DT, Newell ML, Ades AE, et al. (1992). Risk of human immunodeficiency virus type 1
transmission through breastfeeding. Lancet 340:585-88.
Government of Kenya (2004) Ministry of Health, CDC and UNAIDS, Published in UNAIDS
Report, J uly 2004.
Latham MC, Preble EA (2000). Appropriate Feeding Methods for Infants of HIV-Infected
Mothers in Sub-Saharan Africa. British Medical Journal 320: 1656-1660.
Linkages (2001). Breastfeeding and HIV/AIDS: Frequently asked Questions
Linkages (2000). Facts for Feeding; Recommended Practices to Improve Infant Nutrition
during the First Six Months. Washington DC.
Linkages (2000). Facts for Feeding; guidelines for Appropriate Complementary Feeding of
Breastfed Children 6-24 Months of Age. Washington DC..
Mofenson LM, Mcintyre J A (2000). Advances and research directions in the prevention of
mother-to-child HIV-1 transmission. Lancet 355:2237-44.
National Council for Population and Development (NCPD) (2005). Kenpop News: Improving
the Quality of our Population ICPD +10 Lessons Learnt. Vol 1 No. 2
Preble EA, Piwoz EG (2001). Prevention of Mother-To-Child Transmission of HIV in Africa.
A Practical Guidance for Programs.
Poggensee Gabriele, K.Schuidze, I. Moneta, P. Mbezi, C. Baryomunsi and Harma.G. (2004).
Infant feeding practices in western Tanzania and Uganda: implication for infant feeding
Women and Health Learning Package: MTCT of HIV/AIDS
www.the-networktufh.org
15
recommendation for HIV-infected mothers. Tropical medicine and international health. Vol.
9 no.4. 477-485.
Population Reference Bureau Measure Communications (1999). Breastfeeding Patterns in
the Developing World (With Selected Maternal & Child Health Indicators)
Regional Centre for Quality of Health Care (RCQHC) (2000). Health Sector Strategy for
Maternal and Young Child Nutrition: Key actions to improve the nutrition for pregnant and
lactating women and children under two years of age.
Republic of Kenya, Ministry of Health (2002): National Guidelines: Prevention of Mother-to-
Child HIV/AIDS Transmission (PMCT)..
UNAIDS (1998). Best Practice Series: Mother-to- Child Transmission of HIV-Geneva
World Health Organisation Collaborative Study Team (1999). Effect of breastfeeding on
infant and child mortality due to infectious diseases in less developed countries. A pooled
analysis. Lancet 355:451-55.
World Health Organisation (1996). Global Data on Breastfeeding. Geneva
World Health Organisation (1998). HIV and Infant Feeding: Guidelines for Decision Makers.
Geneva.
World Health Organisation (1998). HIV and Infant feeding: A Review of HIV transmission
through Breastfeeding. Geneva.
World Health Organisation (1999). HIV in Pregnancy A review. WHO/CHS/RHR/99 15;
UNAIDS/99.35.
World Health Organisation (2000). Basic Support for Institutionalised Child Survival
(BASICS), United Nations Childrens Fund (UNICEF), Nutrition Essentials: A Guide for
Health Workers. Geneva
World Health Organisation (2000). Use of nevirapine to reduce mother-to-child-transmission
of HIV (MTCT). WHO Review of Reporting Drug Resistance, Geneva, March 24.
WHO/UNICEF (2000). Report of Technical Consultation on Infant and Young Child
Feeding, Geneva
SUGGESTED READING
Dabis F, Leroy V, Castebon K et al. (2000): Preventing mother-to-child transmission of HIV-
1 in Africa in the year 2000. AIDS 14: 1017-26
Kenyan Ministry of Health (2004): Aids in Kenya: background, projections, impact and
Policy, 6th ed. Nairobi, Kenya: National AIDS and STI control.
Women and Health Learning Package: MTCT of HIV/AIDS
www.the-networktufh.org
16
Nyblade L, Field ML (2000). Women, Communities, and the Prevention of Mother-to-
Child Transmission of HIV: Issues and Findings from Community Research in Botswana
and Zambia. International Center for Research on Women. Available at:
http://www.icrw.org/docs/finalsynthesis.doc
Saba J (1999); The results of the PETRA intervention trial to prevent perinatal transmission
in sub-Saharan Africa. Abstract S6. Paper presented at the 6
th
Conference on Retroviruses
and opportunistic infections, Chicago, February.
Semba RD (1997); Overview of the potential role of vitamin A in mother-to-child-
transmission of HIV-1. Acta Paediatrics Supplement 421: 107-12.
South Africa Department of Health (2000). Prevention of. mother-to-child HIV transmission
and management of HIV positive pregnant women. HIV/AIDS and STD Directorate,
Department of Health, South Africa. Available at:
http://www.cadre.org.za/BAC/BACpdf/search='MTCT'
Witkor SZ, Leroy V, Ekpini ER. (2000): 24-month efficacy of short course maternal
zidovudine for the prevention of mother-to-child HIV-1 transmission in a breastfeeding
population: A pooled analysis of two randomised clinical trials in West Africa. Abstract
TuOrB354. A Paper presented at XIII International AIDS Conference, Durban, South Africa.
WHO/UNICEF (2000). Children with HIV/AIDS. In Management of the Child with a Serious
infection or severe malnutrition.
RECOMMENDED WEBSITES
The MTCT-Plus Initiative
www.mtctplus.org
Avert.org Preventing Mother-to-Child Transmission of HIV
http://www.avert.org/motherchild.htm
World Health Organization Mother-to-Child Transmission of HIV (MTCT)
http://www.who.int/reproductive-health/stis/mtct/index.htm
World Health Organization MTCT Nevirapine
http://www.who.int/reproductive-health/publications/archive/nevirapine.htm
Women and Health Learning Package: MTCT of HIV/AIDS Case Studies Student Guide
www.the-networktufh.org
Case Studies Student Guide
Dear students,
These tutorial problems will be done in two sessions led by a tutor. Your tutor will provide
your group with ample opportunities to be self-directing and active in your own quest for
knowledge and reflection by working through the case study in a discussion session. This
means that you will need to participate actively in the discussion and queries on the case
study presented.
The stories of Rukia, Auma and J ennifer were specifically selected to introduce the breadth
and scope of womens health from sociocultural, geopolitical, educational, and human
relations perspectives. The three case studies given in this module highlight the plight of
women as people and as mothers, and explore the factors which adversely affect their
physical, social, emotional, and mental well-being (the WHO definition of health).
Breastfeeding is the lifeline of an infants health. This great source of nutrition and health for
infants has been adversely affected by the onset of HIV/AIDS. Most societies expect mothers
to breastfeed their newborns, and deviant behaviour can be treated harshly, especially in the
developing world. This has left mothers in a dilemma over whether or not to feed their
newborns. In resource-limited situations, it is even more difficult for mothers to practice safe
infant feeding due to their inability to provide adequate supplementary or replacement
feedings. Stigma for PLWHA is yet another compounding factor affecting infant feeding in
this era of HIV/AIDS.
The case studies are purposely designed to be brief and poignant. The objective of each
discussion is not to concentrate on a solution (diagnosis) to the problem. Rather, the focus is
to understand and reflect on the underlying issues and mechanisms involved, and their
relationship to the symptoms and signs which are presented.
You are thus encouraged to explore the wider meaning of womens health outside the scope
of diagnosis and management of disease states specific to women. As such, an open-ended,
less structured approach to the discussion is proposed.
Questions related to the case studies are included as a guideline and not as a compulsory or
strict protocol for the group discussion. Ideally, these questions should be raised by students
themselves in the course of working through the case study.
Each tutorial problem will be carried out in two sessions as described below:
Session 1: Raising Objectives
The students should do the following before handling each case study:
The group consisting of 6-8 students will elect a chairman and a secretary.
The chairman will lead the group and request one of the members to read the case
study aloud.
After this, each member will read the case study quietly and comprehend it well.
The chairman will lead the group and ask members to list all the important terms, new
words/terms and give the theme and learning objectives of the case study. The
secretary will record all points during each session.
The group will be given time within one week to carry out the assignment.
Women and Health Learning Package: MTCT of HIV/AIDS Case Studies Student Guide
www.the-networktufh.org
Session 2: Discussion
This session will follow self-study by each member of the group.
The group will convene and report their findings on the assignment:
The group will give definitions of the new terms/words, explain the important points
in the case study, and give the appropriate theme and learning objectives of the case
study.
The tutor will then discuss with the group members any points they missed about
learning objectives and theme of the case study.
Women and Health Learning Package: MTCT of HIV/AIDS Case Study: Rukia
www.the-networktufh.org
Case Study: Rukia
Rukia is a semi-illiterate 17-year-old married woman living with her mother-in-law in
Malindi, Kenya. Her husband, Baraza, has been ill for some time and has lost a lot of weight.
When Baraza visited voluntary counselling and testing (VCT), he was found to be HIV-
positive. He has not disclosed his HIV status to his wife Rukia.
Rukia is expecting her first baby and is in her seventh month of pregnancy. She is sickly and
malnourished. This has made her feel very weak.
Whenever she complains of any pain, her mother-in-law boils some herbs (roots and leaves)
and gives them to her to drink. Rukia has no money to pay hospital bills, or to go to the
antenatal clinic. Consequently, her mother-in-law has made arrangements with the traditional
birth attendant to help her during delivery. Rukia does not know her HIV status since she has
not been to any VCT.
Questions for students
1. What are the risks that Rukia is most likely to expose the foetus to?
2. Suppose that Rukia is HIV- infected, and she is delivered by the traditional birth
attendant. What steps should she take to protect her infant from an HIV infection?
3. What advice would you give Rukia to improve her nutritional status and health?
Women and Health Learning Package: MTCT of HIV/AIDS Case Study: Auma
www.the-networktufh.org
Case Study: Auma
Auma is a 28-year-old woman who last year lost her first husband and two children, aged 6
and 20 months respectively. She thought the children died as a result of protein-energy
malnutrition (PEM). Both children had long diarrhoeal illnesses, fever, and severe wasting.
Auma has frequent fever and diarrhoea that has resulted in weight loss.
Auma has recently remarried and had another baby. She experiences a lot pain while
breastfeeding due to her cracked nipples. She also says that she doesnt have sufficient breast
milk to satisfy the baby, and she is already considering introducing complementary foods as
she continues to breastfeed.
The community health worker who visited her recently advised her go to the nearby health
centre for a medical examination. She went and was referred to the VCT section. When tested
she was found to be HIV-positive.
She was advised on options of safe breastfeeding. She is not willing to follow the instructions
given to her on safe infant feeding because that may make her husband suspect her of being
HIV-positive.
Questions for students
1. What disease conditions can cause cracked nipples?
2. What are the risks of breastfeeding when the nipples are cracked?
3. What options of safe breastfeeding would you advise Auma to follow?
Women and Health Learning Package: MTCT of HIV/AIDS Case Study: Jennifer
www.the-networktufh.org
Case Study: Jennifer
J ennifer is a 30-year-old woman with a three-month-old infant. Her boyfriend died from
AIDS-related infections before she had the baby. She then left Nairobi and is now living in
Kisumu. She has married another man. Her husband doesnt know about her late boyfriends
cause of death. J ennifer has gone for VCT and knows her HIV status.
She is HIV-positive. She has not disclosed her HIV status to her husband or any member of
her family. She was counselled on proper breastfeeding practices at the postnatal clinic, and
was advised to practice exclusive breastfeeding and avoid mixed feeding.
But she insisted that she would breastfeed her baby like everyone else to avoid arousing any
suspicions about her health. Now she has started feeding the baby on diluted porridge
because she does not have sufficient breast milk. The baby has had a few bouts of diarrhoea
and does not seem to gain weight.
Questions for students
1. Outline the reasons that would make J ennifer hide her HIV status from her husband.
2. What are the dangers of mixed feeding to infants?
3. What are the possible causes of weight loss in J ennifers infant?
Women and Health Learning Package: MTCT of HIV/AIDS Case Studies Tutors Notes
www.the-networktufh.org
Case Studies Tutors Notes
As a tutor you should provide ample opportunities for students to be self-directing and active
in their own quest for knowledge and reflection by working through this case study in a
discussion session. This means that you will need to be patient and refrain as much as
possible from providing all the necessary answers to the students. It also means that you will
need to draw out the quiet and shy members of the small group to share their views and
queries on the case study presented.
The stories in this module were specifically selected to introduce the breadth and scope of
womens health from sociocultural, geopolitical, educational, and human relations
perspectives. The case studies highlight the plight of women, the reality of domestic violence,
and other factors which adversely affect womens physical, social, emotional, and mental
well-being (the WHO definition for health).
The case studies were purposely designed to be brief and poignant. The objective of the
discussion session is not to concentrate on a solution (diagnosis) to the problem. Rather the
focus is to understand and reflect on the underlying issues and mechanisms which are
involved and their relationship to the symptoms and signs which are presented.
The tutor is thus encouraged to invite students to explore the wider meaning of womens
health outside the scope of diagnosis and management of disease states specific to women.
As such, an open-ended, less structured approach to the discussion is encouraged.
Questions related to the case studies are included as a guideline and not as a compulsory or
strict protocol for the group discussion. Ideally, these questions should be raised by students
themselves in the course of working through the case study in the discussion. You are thus
requested to hold on to the question sheets and distribute them at the end of the discussion
session.
To assist you in preparing for your tutor role (and not as a resource expert), a number of
reading materials on the topic of women and health and the specific passages which relate to
the case studies and questions are provided. Please do not at any time pass these materials to
the students in your group.
Case Study: Rukia Tutors Notes
Rukias story is a typical case of ignorance and poverty among many young women.
She cannot attend antenatal clinic, and she will therefore miss out on VCT and any remedial
measurers and advice on breastfeeding. She relies on her mother-in-law for financial support
and medication. She may need ARVs, and she lacks knowledge of opportunistic infections in
AIDS.
Points for discussion
Rukias lack of knowledge of her HIV status
She will have her baby with a traditional birth attendant
Her husband could be HIV-positive
She has missed counselling on infant feeding
Infant will not be given any ARVs such as nevirapine syrup
Women and Health Learning Package: MTCT of HIV/AIDS Case Studies Tutors Notes
www.the-networktufh.org
Rukia may not be able to afford complementary or replacement baby foods
Womens economic empowerment
Case Study: Auma Tutors Notes
Aumas case can be seen to represent many widows who lose their husbands and children to
causes they do not understand and do not associate with HIV/AIDS. They also often become
infected with HIV.
Such women often remarry and have more children who get infected with HIV.
Even if they know their HIV status, they practice risky infant feeding practices due to fear of
stigma, and in Aumas case loss of marriage should the husband suspect her. She at least has
had exposure to the health facilities where VCT and advice on infant feeding are offered.
Auma may have mastitis, which will predispose her infant to HIV infection as she continues
to breastfeed.
Points for Discussion
Lack of knowledge of causes of breast infections and their dangers in lactation
Practice of mixed feeding and its dangers to the baby
Safe breastfeeding options
Similarities between AIDS and PEM
Case Study: Jennifer Tutors Notes
J ennifer has done what most women do when they have lost their partners to AIDS:
they often move to new places where people dont know their past and remarry. They cannot
stop breastfeeding because this raises suspicions about their health. J ennifer cannot declare
her status due to stigma of people with HIV/AIDS and fear of losing her marriage. As a result
the infants health and growth are affected.
Points for Discussion
Stigma when one is known to be HIV-positive
Cultures that stress breastfeeding by all women
Practice of mixed feeding against advice of proper infant feeding
Use of inadequate and non-nutritious feeds for babies
Effect of poor feeding on infants health and growth
S-ar putea să vă placă și
- Global Cancer Transitions According To The Human Development Index (2008-2030) A Population-Based StudyDocument12 paginiGlobal Cancer Transitions According To The Human Development Index (2008-2030) A Population-Based StudyCristian Gutiérrez VeraÎncă nu există evaluări
- Mycobacterium Leprae: Arif Talpur PhysiotherapistDocument11 paginiMycobacterium Leprae: Arif Talpur PhysiotherapistMir Arif HussainÎncă nu există evaluări
- Botswana NnyepiDocument19 paginiBotswana NnyepiBang BojesÎncă nu există evaluări
- Dandruff PDFDocument8 paginiDandruff PDFArthur ChietraÎncă nu există evaluări
- IEN FORMS RPT EmploymentFormDocument3 paginiIEN FORMS RPT EmploymentFormGuru Ramdas Hospital0% (2)
- Pediatric EmergenciesDocument79 paginiPediatric Emergenciesأحمد سعد الديوه جيÎncă nu există evaluări
- Advantages and Disadvantages of Mobile PhoneDocument13 paginiAdvantages and Disadvantages of Mobile PhoneFahad G100% (6)
- Resume Tutorial A Skenario 1 Blok 14Document74 paginiResume Tutorial A Skenario 1 Blok 14Istaz MaulanaÎncă nu există evaluări
- Factors Influencing The Use of Prevention of Motherto-Child Transmission of HIV (PMTCT) Services in Ilala District, Dar Es Salaam TanzaniaDocument9 paginiFactors Influencing The Use of Prevention of Motherto-Child Transmission of HIV (PMTCT) Services in Ilala District, Dar Es Salaam TanzaniaInternational Journal of Innovative Science and Research Technology100% (1)
- ANC (Ante Natal Care) GuidelineDocument46 paginiANC (Ante Natal Care) Guidelinejason wotavizkanÎncă nu există evaluări
- 1517-Article Text-5844-1-10-20081031 PDFDocument6 pagini1517-Article Text-5844-1-10-20081031 PDFJohn Bryan JamisonÎncă nu există evaluări
- Human BrucellosisDocument33 paginiHuman BrucellosisNolie Lovarya HarukaÎncă nu există evaluări
- Detection of Brucella Species in ApparentlyDocument21 paginiDetection of Brucella Species in ApparentlyHubdar Ali KolachiÎncă nu există evaluări
- Cancer and EnvironmentDocument47 paginiCancer and Environmentandra1982Încă nu există evaluări
- FermentationDocument22 paginiFermentationSundar SkÎncă nu există evaluări
- Epidemiological and Clinical Characteristics of Hookwormrelated Cutaneous Larva MigransDocument9 paginiEpidemiological and Clinical Characteristics of Hookwormrelated Cutaneous Larva MigransShelyAzradÎncă nu există evaluări
- PBL TUMBUH KEMBANG DAN GERIATRI Group 15 Modul 1Document57 paginiPBL TUMBUH KEMBANG DAN GERIATRI Group 15 Modul 1Nurfi Resni Fitra RamdaÎncă nu există evaluări
- Kuliah TuberkulosisDocument64 paginiKuliah TuberkulosisLeonardÎncă nu există evaluări
- Health Belief Model On The Determinants of Human Papilloma Virus Vaccination in Women of Reproductive Age in Surakarta, Central JavaDocument11 paginiHealth Belief Model On The Determinants of Human Papilloma Virus Vaccination in Women of Reproductive Age in Surakarta, Central Javaadilla kusumaÎncă nu există evaluări
- Journal Fluor AlbusDocument14 paginiJournal Fluor AlbusMsharaniaÎncă nu există evaluări
- VOD - SOS in HSCTDocument25 paginiVOD - SOS in HSCTKim-Thinh Nguyen ThiÎncă nu există evaluări
- IRC Kenya - Reducing Malnutrition in Hagadera and Kakuma Camps (2011)Document26 paginiIRC Kenya - Reducing Malnutrition in Hagadera and Kakuma Camps (2011)Matija KovacÎncă nu există evaluări
- FFTDocument7 paginiFFTmist73Încă nu există evaluări
- Monkeypox FAQsDocument3 paginiMonkeypox FAQsAnonymous UpWci5Încă nu există evaluări
- Guildelines For Hiv Testing NacoDocument165 paginiGuildelines For Hiv Testing NacoNagendra Singh BeniwalÎncă nu există evaluări
- Jurnal RubellaDocument2 paginiJurnal RubellaAlif SpiritÎncă nu există evaluări
- Pola Imunologi Janin Dalam Kehamilan Dengan Toxoplasmosis: Khairunnisa Abd Rauf A.Zakaria Amien Octo ZulkarnainDocument18 paginiPola Imunologi Janin Dalam Kehamilan Dengan Toxoplasmosis: Khairunnisa Abd Rauf A.Zakaria Amien Octo ZulkarnainArdian Zaka RAÎncă nu există evaluări
- What Is This Fetal Anomaly?Document8 paginiWhat Is This Fetal Anomaly?Dagnechew DegefuÎncă nu există evaluări
- WHO Analgesic LadderDocument2 paginiWHO Analgesic LadderAndi PakdheeÎncă nu există evaluări
- Brucellosis: Aka: Mediterranean Fever, Malta Fever, Gastric Remittent Fever, and Undulant FeverDocument11 paginiBrucellosis: Aka: Mediterranean Fever, Malta Fever, Gastric Remittent Fever, and Undulant Feverfairuz160194Încă nu există evaluări
- Animal Health and Livestock Services Act 2055 NepalDocument13 paginiAnimal Health and Livestock Services Act 2055 NepalSuraj SubediÎncă nu există evaluări
- Brucellosis: Synonyms in AnimalsDocument5 paginiBrucellosis: Synonyms in AnimalsVenkatapradeepÎncă nu există evaluări
- Jurnal UrolithiasisDocument6 paginiJurnal UrolithiasisAliimah KhairiyahÎncă nu există evaluări
- Enteral Nutrition of Preterm BabyDocument54 paginiEnteral Nutrition of Preterm Babylordoftheweb100% (5)
- Overview of Mallory - Weiss SyndromeDocument3 paginiOverview of Mallory - Weiss SyndromeLeslyAgredaNavarroÎncă nu există evaluări
- Human Papilloma Virus: Incubation PeriodDocument4 paginiHuman Papilloma Virus: Incubation PeriodArabelle GOÎncă nu există evaluări
- CMV VirusDocument8 paginiCMV VirusKalpavriksha1974Încă nu există evaluări
- Prenatal DiagnosticDocument60 paginiPrenatal DiagnosticNisaÎncă nu există evaluări
- Induce NetropeniaDocument7 paginiInduce NetropeniaPoldo ReinaldoÎncă nu există evaluări
- Polydactyly - A Review IjirrDocument4 paginiPolydactyly - A Review IjirrDewi AlfiyaniÎncă nu există evaluări
- ESBLDocument7 paginiESBLJonathan WelchÎncă nu există evaluări
- 2011 - Metformin - Multi-Faceted Protection Against CancerDocument22 pagini2011 - Metformin - Multi-Faceted Protection Against CancerVladDaculÎncă nu există evaluări
- Congenital Rubella Syndrome-Case ReportDocument4 paginiCongenital Rubella Syndrome-Case ReportErlina WahyuÎncă nu există evaluări
- Recent Update in The Management of Invasive Fungal InfectionDocument30 paginiRecent Update in The Management of Invasive Fungal Infectionanoop61100% (2)
- Zoonotic Bacteria: BrucellaDocument13 paginiZoonotic Bacteria: BrucellaNagender UpadhyayÎncă nu există evaluări
- Autologous - OmaDocument55 paginiAutologous - OmaOmprakashÎncă nu există evaluări
- Jurnal Flour Albus 1Document7 paginiJurnal Flour Albus 1rinda makuriÎncă nu există evaluări
- Patogenesis Kematian Covid 19Document24 paginiPatogenesis Kematian Covid 19dony kristianÎncă nu există evaluări
- Teknik Analisis Biologi Moleku PDFDocument40 paginiTeknik Analisis Biologi Moleku PDFACHMAD HAIRIL AffanÎncă nu există evaluări
- Bahan Kuliah HIV-AIDSDocument17 paginiBahan Kuliah HIV-AIDSKiki Rizky Andani NasutionÎncă nu există evaluări
- Night BlindnessDocument18 paginiNight BlindnessNicholas RedlyÎncă nu există evaluări
- Hurler Syndrome (Biochem Repot)Document5 paginiHurler Syndrome (Biochem Repot)Kristine Abegail CantillerÎncă nu există evaluări
- Diseases of Children in The Subtropics and TropicsDocument1.092 paginiDiseases of Children in The Subtropics and TropicscaptaincandyÎncă nu există evaluări
- Hepatitis BDocument22 paginiHepatitis BLina VmaleÎncă nu există evaluări
- Failure To ThriveDocument19 paginiFailure To Thriveapi-662340011Încă nu există evaluări
- Nutritional Management of Cystic FibrosisDocument56 paginiNutritional Management of Cystic FibrosisReine Salamoun100% (1)
- Anemi Aplastik Dan MielodisplasiaDocument34 paginiAnemi Aplastik Dan MielodisplasiaRoby KieranÎncă nu există evaluări
- Seminars in Oncology: Male Breast Cancer: Epidemiology and Risk FactorsDocument6 paginiSeminars in Oncology: Male Breast Cancer: Epidemiology and Risk FactorsGina Kristina NanginÎncă nu există evaluări
- Laboratory Diagnosis of HIV Infection: Kamal KishoreDocument7 paginiLaboratory Diagnosis of HIV Infection: Kamal KishoreanastasialantangÎncă nu există evaluări
- Table - Diseases Notifiable To The OIEDocument1 paginăTable - Diseases Notifiable To The OIEЂорђе100% (1)
- Pharmacogenomics: From Discovery to Clinical ImplementationDe la EverandPharmacogenomics: From Discovery to Clinical ImplementationShowkat Ahmad GanieÎncă nu există evaluări
- Mother-To-Child Transmission (MTCT) of Hiv/AidsDocument23 paginiMother-To-Child Transmission (MTCT) of Hiv/AidsParamita ArdiyantiÎncă nu există evaluări
- Infodatin AIDSDocument8 paginiInfodatin AIDSGedeAriyanaKusumaÎncă nu există evaluări
- Syndrome) Merupakan Kumpulan GejalaDocument16 paginiSyndrome) Merupakan Kumpulan GejalaGenoveva Maditias Dwi PertiwiÎncă nu există evaluări
- Epidural JurnalDocument3 paginiEpidural JurnalGenoveva Maditias Dwi PertiwiÎncă nu există evaluări
- Jurnal Faktor Puberrtas DiniDocument36 paginiJurnal Faktor Puberrtas DiniGenoveva Maditias Dwi PertiwiÎncă nu există evaluări
- Anemia Aplastic JournalDocument13 paginiAnemia Aplastic JournalGenoveva Maditias Dwi PertiwiÎncă nu există evaluări
- Systemic Lupus Erythematosus: Pathogenesis and Clinical FeaturesDocument30 paginiSystemic Lupus Erythematosus: Pathogenesis and Clinical FeaturesOrion JohnÎncă nu există evaluări
- Neural Tube Defects.Document34 paginiNeural Tube Defects.ChosenÎncă nu există evaluări
- Trends in Midwifry and ObstetricsDocument8 paginiTrends in Midwifry and ObstetricsVarna MohanÎncă nu există evaluări
- NCMA111-HAS-lec.-NURSING-PROCESS-CRITICAL-THINKING-INTRO-TO-HA-v.2022Document54 paginiNCMA111-HAS-lec.-NURSING-PROCESS-CRITICAL-THINKING-INTRO-TO-HA-v.2022sharlinecatuday08Încă nu există evaluări
- Clinico-Pathological Conference: Presented by The Department of Internal MedicineDocument3 paginiClinico-Pathological Conference: Presented by The Department of Internal MedicineCloudy ClaudÎncă nu există evaluări
- SOPDocument2 paginiSOPNIGEL SAANAÎncă nu există evaluări
- Article: Vitamin B12 Deficiency: Case Report and Review of LiteratureDocument6 paginiArticle: Vitamin B12 Deficiency: Case Report and Review of LiteratureSilvia Emy RarasÎncă nu există evaluări
- RoomDocument524 paginiRoomSeba FounderÎncă nu există evaluări
- Sigma-Alrich SDS (Year 2020)Document9 paginiSigma-Alrich SDS (Year 2020)BigbearBigbearÎncă nu există evaluări
- The BioCassava Plus Program Biofortification of CaDocument24 paginiThe BioCassava Plus Program Biofortification of CaNodir PazÎncă nu există evaluări
- Review Article: Impact of Chinese Herbal Medicine On American Society and Health Care System: Perspective and ConcernDocument7 paginiReview Article: Impact of Chinese Herbal Medicine On American Society and Health Care System: Perspective and ConcernAnonymous 6OPLC9UÎncă nu există evaluări
- Haloperidol Drug StudyDocument2 paginiHaloperidol Drug StudyLanzen DragneelÎncă nu există evaluări
- Disability ManagementDocument346 paginiDisability Managementsollu786_889163149Încă nu există evaluări
- CHCICS305A Provide Behaviour Support in The Context of Individualised PlansDocument100 paginiCHCICS305A Provide Behaviour Support in The Context of Individualised PlansBhakta Chand ThakuriÎncă nu există evaluări
- Lesson 1 The Stuart Stress Adaptation ModelDocument50 paginiLesson 1 The Stuart Stress Adaptation ModelMaria Victoria A. PraxidesÎncă nu există evaluări
- Plete Angelinesimulation Assignment ActivityDocument2 paginiPlete Angelinesimulation Assignment ActivityRoel John Atamosa CasilacÎncă nu există evaluări
- Case Based Discussion 2-Adjustment Disorder Year 5 Rotation 5Document26 paginiCase Based Discussion 2-Adjustment Disorder Year 5 Rotation 5Priya GKÎncă nu există evaluări
- Water Demand FluctuationsDocument6 paginiWater Demand FluctuationsfieqaÎncă nu există evaluări
- Dream Job EssayDocument4 paginiDream Job Essaysirthana697547Încă nu există evaluări
- University of Waterloo - 2016 CIW National Report - How Are Canadians Really Doing?Document96 paginiUniversity of Waterloo - 2016 CIW National Report - How Are Canadians Really Doing?RBeaudryCCLEÎncă nu există evaluări
- Educational Thinkers and Their Contributions - Swami Vivekananda, MahathmaDocument3 paginiEducational Thinkers and Their Contributions - Swami Vivekananda, MahathmaAmanÎncă nu există evaluări
- Drug and Alcohol Awareness ClassDocument71 paginiDrug and Alcohol Awareness ClassRinkish DalliahÎncă nu există evaluări
- DSWD Programs and ServicesDocument12 paginiDSWD Programs and ServicesKathryn Krystal R Lanuza100% (2)
- IVTDocument11 paginiIVTNoorwashilaÎncă nu există evaluări
- Teaching Philosophy Assignment Patricia AnyasoDocument6 paginiTeaching Philosophy Assignment Patricia Anyasoodunze1Încă nu există evaluări
- ACOSDocument14 paginiACOSDejan ŽujovićÎncă nu există evaluări
- Signs of Vitamin b12 DeficiencyDocument9 paginiSigns of Vitamin b12 DeficiencyMark JonesÎncă nu există evaluări
- Grade 3 DLL Mapeh 3 q1 Week 3Document3 paginiGrade 3 DLL Mapeh 3 q1 Week 3Edza Formentera SasaritaÎncă nu există evaluări