Documente Academic
Documente Profesional
Documente Cultură
Medial Column Foot System PDF
Încărcat de
MjidKarim0 evaluări0% au considerat acest document util (0 voturi)
75 vizualizări10 paginiThis document discusses the Rothbart foot structure (RFS), which arises from an embryological retention of talar supinatus. Specifically:
- RFS occurs when the talus fails to unwind during development, leaving the first metatarsal and big toe structurally elevated compared to the lesser metatarsals and toes.
- This forces the foot into excessive pronation during walking and draws the posture forward, leading to problems like pelvic tilt, rounded shoulders, and chronic pain over time as the body compensates.
- The document introduces a new medial column foot system designed to improve posture in patients with RFS. It claims to reduce pelvic tilt, shoulder protrusion, and forward head position,
Descriere originală:
Titlu original
Medial_Column_Foot_System.pdf
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentThis document discusses the Rothbart foot structure (RFS), which arises from an embryological retention of talar supinatus. Specifically:
- RFS occurs when the talus fails to unwind during development, leaving the first metatarsal and big toe structurally elevated compared to the lesser metatarsals and toes.
- This forces the foot into excessive pronation during walking and draws the posture forward, leading to problems like pelvic tilt, rounded shoulders, and chronic pain over time as the body compensates.
- The document introduces a new medial column foot system designed to improve posture in patients with RFS. It claims to reduce pelvic tilt, shoulder protrusion, and forward head position,
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
75 vizualizări10 paginiMedial Column Foot System PDF
Încărcat de
MjidKarimThis document discusses the Rothbart foot structure (RFS), which arises from an embryological retention of talar supinatus. Specifically:
- RFS occurs when the talus fails to unwind during development, leaving the first metatarsal and big toe structurally elevated compared to the lesser metatarsals and toes.
- This forces the foot into excessive pronation during walking and draws the posture forward, leading to problems like pelvic tilt, rounded shoulders, and chronic pain over time as the body compensates.
- The document introduces a new medial column foot system designed to improve posture in patients with RFS. It claims to reduce pelvic tilt, shoulder protrusion, and forward head position,
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 10
Medial column foot systems:
an innovative tool for improving
posture
. . . . . . . . . . . . . . . .
Brian A. Rothbart
Introduction
Morton (1935) describes a foot in
which the 1st metatarsal is shorter
than the 2nd, visually identied as a
deep 1st web space (Fig. 1). Clinical
studies uncover a foot in which the
1st metatarsal is structurally inverted
and elevated relative to the 2nd
metatarsal, referred to as the
Rothbart Foot Structure (RFS)
(Rothbart 1988). Morphologically,
Morton and Rothbart both foot
structures are the same: both arising
from an embryological retention of
talar supinatus. Rothbart (1988)
demonstrates that it is this elevated
position of the 1st metatarsal that
hyperpronates the walking foot.
Hyperpronation draws the posture
forward (Rothbart McCombs et al.
1992, Rothbart Yerratt 1994,
Rothbart Hansen et al. 1995,
Schneider 1995, Filner 1996, Liley
1996). The body adapts. Slowly and
progressively, strain and
deformation patterns develop
that lead the patient into
chronic pain (Rothbart
Esterbrook 1988, Rothbart
McCombs et al. 1992, Rothbart
Hansen et al. 1995, Petersen 1995,
Schneider 1995, Filner 1996, Liley
1996) (Fig. 2).
Travell and Simons (1992) state:
Mortons foot structure is a major
initiator and perpetuator of trigger
points. Since Mortons foot
structure and Rothbarts foot
structure (RFS) is the same foot
structure, it is logical to state RFS is
a major initiator and perpetuator of
trigger points.
An innovative medial column foot
system, designed to improve posture
in patients with Morton/Rothbarts
Foot Structure, is introduced. This
foot appliance visually, and at times
dramatically, reduces pelvic tilts
(unleveled pelvis), shoulder
protractions (rounded shoulders)
and forward head positions. The
drawn forward posture is reversed
(Fig. 3). And with improved
posture, trigger points/chronic pain
syndromes are more easily resolved.
Intuitively we know feet aect
posture. Engineers use this concept
daily: as goes the foundation (foot),
so goes the building (posture). This
article describes the footposture
relationship dynamically, e.g. the
impact the walking foot has on
posture.
Morton (1932) asserts a short 1st
metatarsal (relative to the 2nd and
3rd metatarsals) prevents the rst
metatarsal head from fully
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Journal of Bodywork and Movement Therapies (2002)
6(1), 37^46
r2002 Harcourt Publishers Ltd
doi: 10.1054/jbmt.2001.0261, available online at
http://www.idealibrary.comon
Brian A. Rothbart DPM, LEd, PhD
c/o Linda Penzabane, 1605-B Pacic RIM CT, PMB
21-#48, San Diego, CA 92154, USA
Correspondence to: B. Rothbart
E-mail: rothbart@prodigy.net.mx
Received July 2000
Revised September 2001
Accepted October 2001
P O D I AT R Y I N F L U E N C E S
37
JOURNAL OF BODYWORK AND MOVEMENT THERAPI ES JANUARY 2002
participating in weight bearing
(Fig. 1). While this concept appears
correct, it is only a partial
explanation of the pathodynamics
engaging hyperpronators.
Embryologically the foot goes
through a series of torsional changes
(Streeter 1945, Lash et al. 1997,
Aiton et al. 1995, McLachlan et al.
1997, ORahilly et al. 1987, Smith
1999, Jirasek & Keith 2001, Gasser
1975, Patten 1946). If these torsions
end prematurely (Tabibzadeh &
Pettersson 1995), the 1st metatarsal
and big toe (proximal phalanx
and hallux) remain structurally
elevated and inverted (in elevatus)
relative to the lesser metatarsals
and phalanges (Straus 1927,
Olivier 1962). It is this retained
elevatus that forces the walking
foot into hyperpronation
(Rothbart & Esterbrook 1988,
Rothbart & Hansen 1995, Filner
1996, Liley 1996). It is
hyperpronation that draws the
posture forward (Rothbart et al.
1992, Rothbart & Hansen 1995,
Schneider et al. 1995, Filner 1996,
Fig. 1 Deep 1st web space seen in Mortons
foot structure. The 1st web space (space
between the 1st and 2nd toes) is more
proximal (nearer to the heel) than the 2nd
web space.
Fig. 2 Chronic pain syndromes associated
with Rothbarts foot structure.
Fig. 3 BioImplosion. Gravity induced
skeletal shift. Hyperpronation shifts the
bodys center of gravity forward. The axial
framework responds by moving out of
vertical towards a forward, inward and
downward position (typical hyperpronation
pattern of left foot 4 right foot produces the
following postural pattern: left PSIS is
anterior [forward] and superior [higher]
relative to right PSIS, pelvis is unleveled, left
leg is functionally longer than right leg,
thoracic cage is rotated counterclockwise, left
shoulder is protracted [forward] and superior
[higher] relative to right shoulder). Cranial
and connective tissue compensations are
commonly initiated and/or perpetuated by
this forward postural shift which, in turn, can
be responsible for many of the chronic pain
conditions seen clinically. Adapted and
reproduced with permission from the
American Journal of Pain Management,
1995.
Box 1
1.0 Normal embryonic development (weeks 18 pf).
* Week 3 post fertilization (pf) lower limb bud appears
* Week 6 pf limb bud at right angles to rump: soles and posterior surfaces face cephalad
(Fig. 4, Right slide, top)
* Week 8 pf soles and posterior surface face one another (Fig. 4, right slide, middle, Fig. 5)
1.1 Normal foetal development (weeks 9 pf to full term).
* Week 9 pf primordial ankle and knee joints appear (Fig. 4 Left slide, bottom)
* Week 10 pf thigh and leg unwinding around longitudinal axis (Fig. 4, Right slide,
bottom)
* Week 11 pf calcaneal supinatus unwinding
* Week 12 pf talar {head} supinatus unwinding
* Week 36 pf heel and sole plantargrade to leg
1.2 Abnormal foetal development
* 1.21 Talar head fails to unwind: Rothbart foot structure
* 1.22 Calcaneus fails to unwind: Clubfoot deformity
38
JOURNAL OF BODYWORK AND MOVEMENT THERAPI ES JANUARY 2002
Rothbart
Liley 1996). And it is this forward
posture and ensuing compensations
that lead the patient into chronic
pain (Rothbart & Esterbrook 1988,
Rothbart et al. 1992, Rothbart &
Hansen 1995, Petersen 1995,
Schneider 1995, Filner 1996, Liley
1996) (Figs 2 and 3).
Section 1 (Embryology) briey
outlines [1] the normal ontogenetic
stages within the lower limb bud and
[2] the abnormal ontogenetic events
that result in either the Clubfoot
deformity (Cfd) or Rothbart foot
structure (RFS). (This paper does
not deal with the positional or
structural deformations that can
occur postnatally, e.g. rearfoot
varum from massive trauma to the
heel bone, leg length discrepancy
from sepsis of the femoral growth
plate, etc) Section 2 (RFS, clinical
signicance of PME) discusses RFS
impact on posture and gaiting, and
provides a methodology for
diagnosing RFS in the adult foot.
Section 3 (stabilizing RFS)
introduces an innovative foot
appliance that [1] reduces static and
dynamic hyperpronation and [2]
reverses postural shifts generated
from RFS.
Embryology
Ontogenetic retention of talar
supinatus: the Rothbart foot
structure
One thousand and six Egyptian feet
were evaluated for talar supinatus
(Sewell 1906). Angular variances, up
to 201, were reported. If the talar
head fails to unwind (remains in
supinatus), the navicular remains
relatively supinated (torsionally
twisted inward around its
longitudinal axis), and with it, the
internal cuneiform, 1st metatarsal
and big toe (Straus 1927, Olivier
1962). Rothbart terms the retained
structural elevation of the 1st
metatarsal and big toe: Primus
Metatarsus Elevatus (PME; see
Fig. 6). PME values are clinically
quantied using microwedges
(Fig. 7).
In the postnatal foot, the
navicular articulates with all three
cuneiforms. From a structuralist
view point, one might conclude that
the navicular impacts all three
cuneiforms. From an embryological
Fig. 4 Left slide, top: Week 3 pf. Limb bud appears as a swelling opposite the lower lumbars.
Right slide, top: Week 6 pf. Limb bud sits at right angles to rump of embryo. Soles of feet and
posterior compartments of leg and thigh face cephalad. Left slide, middle: Week 8 pf. Limb bud
has rotated 901 around its longitudinal axis. Soles and posterior surfaces of thigh and legs now
face one another. Right slide, middle: Week 8.5 pf. Primordial toes appear in the developing
foetus. Left slide, bottom: Week 9 pf. Primordial ankle and knee joints appear. Right slide,
bottom: Week 10 pf. Leg and thigh are unwinding around their longitudinal axes (clockwise left,
counterclockwise right) leaving the foot (calcaneus and talus) in supinatus. Adapted and
reproduced with permission from Visible Embryos r Mousework Inc.
Fig. 5 Frontal view embryo week 8.5 pf.
Lower limb bud is rotating 901 around its
longitudinal axis (clockwise left,
counterclockwise right). Posterior thigh and
leg compartments face one another, as do the
heels (calcaneal supinatus) and soles (talar
supinatus) of the feet. USPTO #6,092,314
Sheet 2, Figure 2. Adapted and reproduced
with permission from GRD BioTech Inc.,
2000.
39
JOURNAL OF BODYWORK AND MOVEMENT THERAPI ES JANUARY 2002
Medial column foot systems
perspective, this is not the case.
Straus (1927), Streeter (1945) and
Olivier (1962) depict that is the
unwinding of the talar head, that
determines the shape and contour of
the navicular, internal cuneiform,
1st metatarsal and big toe. That is,
the relative structural position of the
1st metatarsal/big toe is determined
by the sculpturing of the talar head.
Retention of postnatal talar
supinatus results in a visibly elevated
1st metatarsal/big toe (standing
position, subtalar joint neutral).
Ontogenetic retention of
calcaneal supinatus: the
Clubfoot deformity
If the calcaneus fails to unwind
(remains in relative supinatus), the
cuboid remains in supinatus, and
with it, the lateral two cuneiforms,
Fig. 6 Talar supinatus, frontal view, left
foot. Torsional unwinding of the talar
supinatus delineated (see upper diagrams, left
to right). As the talar head unwinds, Primus
Metatarsus Elevatus is decreased. Lower
diagram left illustrates retention of talar
supinatus and resulting twist and elevation of
the 1st metatarsal (PME) relative to the
ground. Lower diagram right illustrated
complete unwinding of the talar head and
resulting plantargrade position of the 1st
metatarsal relative to the ground. USPTO
#6,092,314 Sheet 3, Figure 4. Adapted and
reproduced with permission from GRD
BioTech Inc., 2000.
Fig. 7 Measuring PME. With the client
standing, locate the subtalar (talocalcaneal)
joint (21) as follows: one nger width below
and anterior to the medial malleolus (see
bottom photograph). Keeping your nger
over the subtalar joint space, have your client
transfer 90% of their weight to the other foot.
With your other free hand, slowly guide the
foot through pronation (inversion)
supination (eversion) until the margins of the
subtalar joint space feel parallel to one
another (see top photograph). If the subtalar
joint is pronated, the joint space disappears. If
the subtalar joint is supinated, the joint space
gaps. Slide the microwedge (110) under the
ball of the foot (1st metatarsal) until slight
resistance is met. Record the PME value o
the microwedge.
40
JOURNAL OF BODYWORK AND MOVEMENT THERAPI ES JANUARY 2002
Rothbart
lesser four metatarsals and
accompanying phalanges (Bohm
1929). The footplate unwinds heel to
toe (Streeter 1945, 1948, 1951), thus
the maxim: as goes the calcaneus, so
goes the talus. Retention of calcaneal
supinatus is always accompanied by
talar supinatus, the Clubfoot
deformity (Cfs) (Bohm 1929).
In the postnatal foot, the
calcaneus articulates with the
cuboid, which in turn articulates
with the navicular, lateral cuneiform
and lateral two metatarsals. From a
structuralist viewpoint, one might
conclude that the calcaneus only
impacts these structures. From an
embryological prospective, this is
not the case. Bohm (1929) describes
how the ontogenetic unwinding of
the calcaneus aects the lateral
column of the embryonic foot. That
is, the relative structural position of
the cuboid, the lateral two
cuneiforms and four lateral
metatarsals/phalanges are
determined by the sculpturing of the
calcaneus. Retention of calcaneal
supinatus in the prenatal foot is
manifested as the Cfd in the
postnatal foot.
RFS: clinical signicance
of PME
RFS is subtle in the newborns foot
due to the bulging longitudinal fat
pad and incomplete ossication of
the tarsal bones. At birth, the
primary ossication site of the talus
has already appeared (Sewell, 1906).
However, the onset of ossication of
the navicular is variable (2.74.0
years of age) and late compared to
the other tarsal bones (Caey 1972,
Lang 1972, Bardeen 1905, Hoeer et
al. 1962). The topographical
contouring of the inner longitudinal
arch (ILA) starts to develop between
12 and 16 months of age. A denite
ILA is present by age 2. By age
30 months, maximal inner
longitudinal arching is attained,
the apex corresponding to the
navicular tuberosity (Blais & Green
1956). As the ILA takes on its
adult contour and the navicular
bone ossies, PME becomes more
visible. However, measuring
PME in a child less than 4 years
of age is prone to error because
the navicular bone has not yet
ossied.
In the adult foot (aged 4 and
over), PME values between 10 mm
and 25 mm are pathognomic of
RFS. Flexible arches (higher arch
sitting than standing) and exible
atfeet (arch sitting, no arch
standing) are functional
compensations commonly
associated with RFS. The
supinatory strike, in which the
bodys weight is carried on the
outside margins of the heel, is
another common compensation
associated with RFS. Visual
inspection of the shoes reveals an
excessive wear pattern on the
outside margins of the heels. When
dealing with RFS, measuring
forefoot varum across the entire sole
(metatarsals 15) is a misdirected
clinical assessment, since talar
supinatus only aects the 1st
metatarsal.
A preliminary investigation
correlating PME values to
compensatory patterns in 37 infants,
ages 24, was undertaken at the
Bellevue Foot and Ankle Center in
Bellevue Washington (19881994).
Fig. 8 The neurovascular network sits posteriorly and inferiorly to the medial malleolus.
Hyperpronation associated with PME 420 mm (see left foot) can compress this network,
signicantly reducing blood ow and innervation to the bottom of the foot (see bottom, left
diagram).
41
JOURNAL OF BODYWORK AND MOVEMENT THERAPI ES JANUARY 2002
Medial column foot systems
The following factors were
measured: foot type (exible arches
or exible atfeet), position of feet
(pigeon-toed, straight or out-toed),
heel strike (inside or outside), and
PME values. The results suggest that
infants (under age 4) with PME
values 420 mm tend to adduct
(pigeon-toe). As children they are
typically inside heel strikers and at-
footed (exible at-feet). Infants
with 1119 mm PME tend to abduct
(out toe). As children they are
outside heel strikers and have
exible arches.
The above ndings provide a
possible pattern of compensations
associated with various PME
ranges. Infants with higher PME
values (420 mm) tend to
instinctively reduce (adapt to) their
dynamic hyperpronation by turning
their feet inward. Infants exhibiting
lower PME values (1119 mm) tend
to either fall into a mild to
moderate hyperpronation pattern
(feet turned outward), or adapt by
walking on the outsides of their feet
(feet straight forward). In both
cases, as children they appear to
have exible arches. The above
observations are insightful but not
denitive (26 of the 37 children
follow these patterns). This study
needs to be repeated using larger
sample sizes over a longer period of
time.
Clinical data compiled at GRD
BioTech Inc in Seattle Washington
(2001) collaborates earlier studies
linking higher PME values to RFS
(Rothbart et al. 1992, Cummings
1994, Schneider et al. 1995,
Rothbart & Hansen 1995). Three
hundred and seventeen patients were
measured with microwedges (Fig. 7).
Three hundred and six (96.5%)
demonstrated an RFS with a mean
PME of 16 mm (distance [freeway
space] between the 1st metatarsal
and ground, subtalar joint in neutral
[ joint congruity] position). Of these,
271 (88.5%) had exible arches
(mean PME of 14 mm), and 35
(11.5%) had exible at-feet (mean
PME of 24 mm). Ten (3.1%)
demonstrated a non-RFS (mean
PME of 6 mm). 1 (0.3%) had a
preclinical Cfd (PME of 37 mm).
The typical pronated posture
PME (410 mm) signicantly forces
the walking foot to roll inward,
forward and downward (typically
left foot 4 right foot) until the 1st
metatarsal reaches the ground
(Rothbart & Esterbrook 1988,
Rothbart et al. 1995, Schneider
1995, Filner 1996, Liley 1996). This
shifts the bodys center of gravity
forward and downward, which in
turn, pulls the innominates forward
and downward (typically
left4right). The pelvis is unleveled,
resulting in a functional leg length
discrepancy (left longer than right).
As these displacements cascade up
the axial framework, scoliotic and
kyphotic curves are exaggerated.
The thoracic cage twists (usually
counterclockwise). The shoulders.
protract (left4right) The right
shoulder drops. Cranially, the
maxilla moves anteriorly relative
to the mandible resulting in an
overjet bite. This gravity-induced
skeletal collapse is termed
BioImplosion (Rothbart et al.
1992, Rothbart & Yerratt 1994,
Schneider 1995, Petersen et al. 1995,
Filner 1996, Liley 1996), which over
time can initiate strain and trigger
point patterns, foot to jaw
(Rothbart et al. 1992, Rothbart &
Hansen 1995, Schneider 1995,
Fig. 9 Medial column system. Tactile feedback loop extending from the navicular to the hallux.
The system is sloped (60) medial to lateral. The vertical dimensioning discussed in the paper is
represented by line (62), which extends along the medial border of the foot. Typically arch
supports are not incorporated into the medial column system. Visual gait studies on 317 clients
delineate: 30% tactile feedback results in approximately 70% decrease in dynamic
hyperpronation (the 3070 rule). USPTO #6,092,314 Sheet 4, Figure 5. Adapted and reproduced
with permission from GRD BioTech Inc., 2000.
42
JOURNAL OF BODYWORK AND MOVEMENT THERAPI ES JANUARY 2002
Rothbart
Petersen 1995, Filner 1996, Liley
1996).* (See Fig. 2).
Johnson and Cross (1990)
describe a common compensatory
pattern (CCP) that is very similar to
the BioImploded posture outlined
above. Johnson and Cross link
posture to torsions within the pelvis.
Rothbart et al. (1992) link posture
to torsions (hyperpronation) within
the feet. Zink & Lawson (1979)
describe a disparent (atypical) CCP.
Interesting enough, this disparent
CCP closely parallels the Bio-
Imploded posture resulting from the
less common hyperpronation
pattern of right4left.
Hyperpronation associated with
PME 420 mm can mechanically
compress the posterior tibial vessels
(nerve, artery and vein) as they enter
the foot behind the medial
malleolus. This is quickly
determined by taking standing PT
pulses: foot neutral and then
pronated (Fig. 8).
From clinical observations, RFS
appears to be a dominant, single
autosomal Mendelian characteristic.
This would explain the familial
diathesis and the inordinate rate of
expansion in the genetic pool
(Garbalosa et al. 1994). Harris and
Beath (1949) evaluated the foot
structure of 3619 Canadian men.
Their study suggests a 40%
incidence of Mortons foot structure
(short 1st metatarsal). A more recent
investigation, presented at the
Annual Conference of the American
Academy of Pain Management
(Rothbart 1995), suggests a 95%
incidence of Morton/Rothbarts
foot structure (short and elevated
1st metatarsal).
Stabilizing RFS
Heel wedges and arch supports
Calcaneal wedging decreases
standing hyper-pronation.
Calcaneal wedging does not decrease
walking hyperpronation generated
from the elevated 1st metatarsal. In
fact, inverting the whole foot in this
fashion can increase the relative
elevation of the 1st metatarsal to the
ground, which in turn can increase
the hyperpronation generated at
heel-lift. In a similar fashion, arch
supports decrease midstance
hyperpronation, but are ineective
as the ball of the foot engages in
weight bearing. Paradoxically, arch
supports aect feet like
immobilization casts aect muscles:
function is improved at the price
Fig. 11 The Clubfoot deformity.
Fig. 10 Primus metatarsus elevatus table. A linear correlation is seen between PME values and
foot structure. Low PME values (o10 mm712 mm) are associated with a non-RFS. In the
absence of signicant soft tissue or cranial adaptations: midrange PME values (1025 mm7
12 mm) are associated with RFS, ranging from exible arches (1019 mm712 mm) to exible
atfeet (2535 mm712 mm). High PME values (440 mm) are associated with Clubfoot
deformities with overt arch deformation.
*For example, chronic shoulder protraction can
lead to a functional thoracic outlet syndrome.
43
JOURNAL OF BODYWORK AND MOVEMENT THERAPI ES JANUARY 2002
Medial column foot systems
of muscle strength. In time, these
same feet become weaker/more
pronated (when barefooted) than
they were prior to arch support
therapy. For this reason, the
author rarely uses heel wedges in
RFF, and judiciously only uses
arch supports in feet that are
functionally at.
Medial column systems
Medial column systems eectively
reduce dynamic hyperpronation
associated with RFS. The eect of
these systems extend from the
navicular, medial cuneiform, 1st
metatarsal bone, to the proximal
phalanx and hallux
(Fig. 9). With each step, a tactile
feedback loop is triggered that auto
corrects the hyperpronation being
initiated by the PME. The suggested
rule of thumb is: 30% tactile=70%
improvement (the 3070 rule is
observational, based on empirical
data derived through gait evaluation
of 317 patients at the GRD BioTech
facility, 19961998, and hence not
meant to be denitive or all
inclusive). For example, a 6 mm
medial column system (Fig. 9[62])
under a foot measuring 20 mm PME
(assuming no signicant
hypertonicity patterns or cranial
deformations) tends to decrease the
observable hyperpronation by
approximately 70%. Via
proprioception, this system provides
feedback to the big toe (proximal
phalanx and hallux) and 1st
metatarsal. All the other weight
bearing structures proximal to the
big toe and 1st metatarsal (ankle,
knee, pelvis, spine, neck, head and
jaw) tend to spontaneously correct
themselves around this change. The
bodys center of gravity shifts
posteriorly. The posture is visually
more vertical. The inner longitudinal
arch is not supported in feet with
exible arches. (Arch supports are
used in atfeet to facilitate the
transfer of vector forces across the
ILA). The heel is neither cupped nor
wedged.
Tactile feedback systems are
based on the observation that small
repetitive stimuli bring about
signicant changes. Interesting
enough, in terms of foot mechanics,
this occurs through kinesthetic
reposturing. The foot-brain
connection recognizes this
proprioceptive input as innately
correct. The foot is reminded
where it should be (not here, but
over there) and automatically
makes the adjustment. With each
step, the foot becomes stronger,
the posture straighter.
Hyperpronation is reduced.
And not surprisingly, as the soft
tissue and cranial adaptations are
addressed, the tactile input in the
medial column system may
require recalibration (adjustment).
An unexpected outcome using
foot tactile systems is the
observation that hypertonic
muscles can become disassociated
from Morton/Rothbarts foot
structure. That is, these short and
tight muscles evolve into self-
perpetuating loops. Their associated
pain referral patterns prove
intractable to foot therapy alone.
This underscores the importance of
concurrent foot and soft tissue
therapy when dealing with chronic
pain issues.
The medial column foot system is
used as a proprioceptive stimulator.
It is dimensioned to partially ll-in
the freeway space that exists
between the 1st metatarsal/big toe
and ground (Fig. 6). If this system is
dimensioned so that it completely
lls in the freeway space, it
becomes a supportive device. Such
devices over a period of time
weaken structure and should not
be used under the RFS. Using a
medial column foot system in a
non-RFS places a disruptive
upward load under the 1st
metatarsal head. This can
dramatically limit the range
of dorsiexion within the
1st metatarsal-phalangeal
articulation and lead to
a potential functional hallux
limitus.
Summation
The foetal development of the lower
limb bud, and specically the
footplate, is reviewed. Clinical
studies describe the impact talar
and calcaneal supinatus have on
the medial column of the foot:
incomplete unwinding of the
talar head results in the Morton/
Rothbart foot structure; in-
complete unwinding of the
calcaneus results in the Clubfoot
deformity (Fig. 11).
Zitzlesperger (1960) and
Elftmans (1960) foot models
demonstrate an inverse relationship
between pronation and arch
stability: as pronation increases,
arches atten. Clinical data from
GRD BioTech (2001) demonstrates
a similar inverse relationship
between PME (elevation of the 1st
metatarsal and big toe) and arch
stability: as PME increases, arch
stability decreases. PME values less
than 10 mm correlate to stable
arches (same arch height sitting or
standing). PME values between
10 mm and 20 mm correlate to
exible arches (higher arch sitting
than standing), 25 mm30 mm to
exible atfeet (arch sitting, no arch
standing), 35 mm40 mm to
inexible atfeet (no arch sitting
or standing), and 440 mm to rigid
and structurally deformed feet
(Fig. 11 the Clubfoot
deformity).
PME between 10 and 25 mm
are associated with RFS, a foot in
which the 1st metatarsal is short
and structurally elevated relative to
the lesser metatarsals. Rearfoot
posts destabilize the RFS.
Arch supports weaken the RFS.
And forefoot varum posts (Root
44
JOURNAL OF BODYWORK AND MOVEMENT THERAPI ES JANUARY 2002
Rothbart
et al. 1971) structurally strain the
RFS.**
Published studies link PME to
hyperpronation and hyper-
pronation to BioImplosion.
Dimensioning medial column
systems at 30% of the measured
PME tend to decrease dynamic
hyperpronation by 70%710%.
This in turn tends to reduce pelvic
tilts by 50%720%, shoulder
protractions by 40%720% and
forward head positions by
30%720%. In the absence of any
signicant psychological or
nutritional imbalances, hypertonic
muscles become signicantly
more amenable to long-term
resolution as posture becomes
more vertical.
REFERENCES
Aiton JF, McDonough A, McLachlan JC,
Whiten SC, Smart SD 1995 World Wide
Web Access to the British Universities
Human Embryo Database. Journal of
Anatomy 190: 149154
Cummins H 1929 The topographic history of
the volar pads in human embryo.
Contributions Embryology 20: 105
Bardeen CR 1905 Studies of the development
of the human skeleton. American Journal
Anatomy 4: 265
Blais MM, Green WT et al. 1956 Lengths of
the growing foot. Bone Joint Surgery,
38[A]: 998
Bohm M 1929 The embryologic origin of
clubfoot. Journal Bone Joint Surgery, 11:
2, 229
Caey JP 1972 Pediatric X-Ray Diagnosis.
Vol 2: 884. 6th Edition, YearBook
Medical Publishers, Chicago
Cichoke AJ 1999 The Back Pain Bible. Ch.
IV, pp 35. Keats Publishing, Chicago
Cummings G 199495 Personal
communications with Author and on
campus visit: Blind study-using
microwedges to measure vertical
dimensions under patients seen by
students. Clinical Director, Department
of Physical Therapy, Georgia State
University, Atlanta GA
Elftman H 1960 The transverse tarsal joint
and its control. Clinical Orthopedics
16: 41
Filner B et al. 1995 The relationship of
anterior upper torso muscular
dysfunction with structural
hyperpronation in chronic pain
patients. Annual Meeting, American
Academy of Pain Management, Dallas,
September
Filner B 1996 Postural Analysis: Dierential
Diagnosis. Annual Conference,
American Academy of Pain
Management, Washington DC
Gasser RF 1946 Atlas of Human Embryos.
Harper and Row Publishing, Hagerstown
Garbalosa JC et al. 1994 The frontal plane
relationship of the forefoot to the
rearfoot in an asymptomatic population.
JOSPT 24: 4, 200206
GRD BioTech Inc 2001 317 clients evaluated
between 19961998 using microwedges
and visual gait analysis, with and without
postural insoles. Seattle, WA
GRD BioTech Inc 2000 Foot Support
(Medial Column) System and Use in
Shoe Lasts. United States Patent Number
6,092,314. Seattle, WA, July
Harris RI, Beath T 1949 The short rst
metatarsal: Its incidence and clinical
signicance. Journal Bone Joint Surgery
[Am] 31: 553565
Hoerr LN et al. 1962 Radiographic Atlas of
Skeletal Development of the Foot and
Ankle A Standard Reference. Charles C
Thomas, Springeld
Jirasek JE, Keith LG 2001 An Atlas of
the Human Embryo and Fetus: A
photographic review of human prenatal
development. CRS Press, Parthenon
Publishers, 1st edition
Johnson K, Cross N 1990 Common
compensatory pattern and its relation
to lumbar facet angles. Journal
American Osteopathic Association
90: 942
Lang J et al. 1972 Praktische Anatomic Erster
Band Vierter Teil Bein und Statik,
p. 31. Berlin, Springer Verlag
Lash J, Alonso L, Benke L, Chang A,
Dietrich A, Nathan D 1997 Basic
Embryology Review Program: Embryo
images. University of Pennsylvania,
School of Medicine. Web Home Page:
http://www.med.upenn.edu.meded/
Liley P 1996 Postural analysis: Head guidance
and ground support. Annual Conference
American Academy Pain Management,
Washington DC
McLachlan JC, Aiton JF, Whiten SC,
Smart SD 1997 3-D Modeling of
Human Embryo Morphology using
QuickTime VR. In Molecular
Genetics of Human Development.
pp 227237, eds. Strachan T, Lindsay S
& Wilson D Bios Scientic Publishers
Ltd, Oxford
Morton DJ 1935 The Human Foot. Its
evolution, physiology and functional
disorders. Columbia University Press,
New York
Morton DJ 1932 Means for compensating for
foot abnormalities. US Patent Number
1,847,973, USPTO, March
ORahilly R, Gardner E et al. 1956 The
ectodermal thickening and ridge in the
limbs of staged human embryos. Journal
Embryology and Experimental
Morphology 4: 256
ORahilly R, Gardner E 1975 The timing and
sequence of events in the development of
the limbs in the human embryo.
Anatomical Embryology, 123
Olivier G 1962 Formation du Squelette
des members. pp 145189. Paris, vigot
Freres
Patten BM 1946 Human Embryology. The
Blakiston Company, Philadelphia
Petersen M et al. 1995 The relationship of
lower leg muscular dysfunction with
structural hyperpronation in chronic pain
syndrome patients. Posterboard
Presentation, Annual Conference,
American Academy Pain Management,
Dallas
Root ML, Orien WP, Weed JH, Hughes RJ
1971 Biomechanical examination of the
foot. 1st ed. Los Angeles: Clinical
Biomechanical Corporation
Rothbart BA, McCombs A, Riniker L 1992
BioImplosion. The treatment of chronic
pain syndrome. Posterboard
Presentation, Annual Conference,
American Academy of Pain
Management, Albuquerque
Rothbart BA 1995 Postural Kinetics. Two
studies presented: [1] Gait compensations
observed in 37 infants between 1988
1994. [2] PME taken on 3417 patients
between 19841995. Annual Conference,
American Academy of Pain
Management, Dallas
Rothbart BA, Yerratt M 1994 An innovative
mechanical approach to treating chronic
knee pain: A BioImplosion Model.
American Journal Pain Management
4: 3, 123128
Rothbart BA, Esterbrook L 1988 Excessive
Pronation: a major biomechanical
determinant in the development of
chondromalacia and pelvic lists. Journal
Manipulative Physiologic Therapeutics
11: 5, 373379
Rothbart BA, Liley P, Hansen K, Yerratt K
1995 Resolving chronic low back pain:
**Only the 1st metatarsal is in elevatus in the RFS.
Forefoot varum posts elevates metatarsals IIV.
The terms supinatus and varum have been used
interchangeably in the literature. By convention,
supinatus is used to describe a torsionally inverted
relationship in the prenatal foot. Varum is used to
describe the same torsional (structural) relationship
in the postnatal foot.
45
JOURNAL OF BODYWORK AND MOVEMENT THERAPI ES JANUARY 2002
Medial column foot systems
The foot connection. American Journal
Pain Management, 5: 3, 8489
Rothbart BA, Hansen K 1995 Postural
Analysis: Denition of terms.
Posterboard Presentation. Annual
Conference, American Academy Pain
Management, Dallas
Svae B 2000 Personal Communication
with Author, Postural Dynamics,
Seattle, WA
Schneider M et al. 1995 The importance of
controlling hyperpronation with a
postural control device in resolving
musculoskeletal pain in chronic
syndrome patients. Posterboard
Presentation, Annual Meeting,
American Academy Pain Management,
Dallas
Sewell RS 1906 A study of the astragalus
(talus). Part IV. Journal Anatomy
Physiology, Vol 40: 152
Smith BR 1999 Visualizing human embryos.
Scientic American 280: 7681
Smith BR, Hu DS, Johnson GA 1999
Magnetic resonance imaging of embryos:
An Internet resource for the study of
embryonic development. Computerized
Medical Imaging and Graphics
23: 3340
Straus WL 1927 Growth of the human foot
and its evolutionary signicance.
Contributions in Embryology 19: 95
Streeter GL 1945, 1948, 1951 Developmental
horizons in human embryos. In
Contributions to Embryology, Vols. 21,
32, 34. Washington DC. Carnegie
Institution of Washington
Tabibzadeh S, Pettersson TV 1995 An Atlas
of Human Embryogenesis. Frontiers in
BioScience. Website http://
bioscience.igh,cnrs.fr/atlases/fert/
embrper.htm
Travell JG, Simons DG 1992 Myofascial Pain
and Dysfunction. The Trigger Point
Manual. Vol. 2: 20, pp 379392, Williams
and Wilkins, Baltimore
Visible Embryos 2001 Embryos Slides.
Mouseworks Inc. Website:
WebMaster@visembryo.com
Zink JG, Lawson W 1979 An osteopathic
structural examination and function
interpretation of the soma. Osteopathic
Annals 7: 12
Zitzlesperger S 1960 the mechanics of the
foot based on the concept of the skeleton
as a statically indetermined space
framework. Clinical Orthopedics 16:
4763
46
JOURNAL OF BODYWORK AND MOVEMENT THERAPI ES JANUARY 2002
Rothbart
S-ar putea să vă placă și
- 2002 Medial Column Foot SystemsDocument10 pagini2002 Medial Column Foot SystemsprofessorrothbartÎncă nu există evaluări
- Biomechanical Foot Function - A Podiatric PerspectiveDocument7 paginiBiomechanical Foot Function - A Podiatric PerspectiveFisioterapi Kumala SurakartaÎncă nu există evaluări
- Anatomi AnkleDocument15 paginiAnatomi AnkleZera DirgantaraÎncă nu există evaluări
- Anatomy of The Ankle and FootDocument13 paginiAnatomy of The Ankle and FootRichard MillerÎncă nu există evaluări
- Entomology 322 Lab 5 Arthropod Appendages and LocomotionDocument9 paginiEntomology 322 Lab 5 Arthropod Appendages and LocomotionHumberto GiraldoÎncă nu există evaluări
- Protraction Class II Dental OcclusionDocument13 paginiProtraction Class II Dental OcclusionIlinca LupuÎncă nu există evaluări
- Improving Ankle and Knee Joint Stability: Proprioceptive Balancefit Discs DrillsDe la EverandImproving Ankle and Knee Joint Stability: Proprioceptive Balancefit Discs DrillsÎncă nu există evaluări
- The Biomechanics of The FootDocument7 paginiThe Biomechanics of The FootKhaledAbuzÎncă nu există evaluări
- Functional Anatomy and Muscle Action of The FootDocument14 paginiFunctional Anatomy and Muscle Action of The FootalmaformaÎncă nu există evaluări
- Knee Anatomy Osseous Structures: Concept InformationDocument19 paginiKnee Anatomy Osseous Structures: Concept InformationRachel BlackburnÎncă nu există evaluări
- Pronation Supination1Document7 paginiPronation Supination1José Enrique Castillo NavaÎncă nu există evaluări
- Movement Profile - Right Hook Boxing-ScribdDocument8 paginiMovement Profile - Right Hook Boxing-ScribdTuan Ha NgocÎncă nu există evaluări
- Ljudsko Telo OrganizacijaDocument10 paginiLjudsko Telo OrganizacijaMiljan MadicÎncă nu există evaluări
- Short Right Leg 1Document4 paginiShort Right Leg 1Simo AsterÎncă nu există evaluări
- Biomechanics of Ankle and FootDocument40 paginiBiomechanics of Ankle and FootNujella BalajiÎncă nu există evaluări
- Biomechanics and Pathophysiology of Flat FootDocument12 paginiBiomechanics and Pathophysiology of Flat FootGeorge FernandoÎncă nu există evaluări
- BFO - AnatomyDocument33 paginiBFO - AnatomynovitaÎncă nu există evaluări
- Foot Biomechanics and Relation To The Gait Cycle: 10.5005/jp-Journals-10040-1093Document5 paginiFoot Biomechanics and Relation To The Gait Cycle: 10.5005/jp-Journals-10040-1093Carmen Cuerdo del RíoÎncă nu există evaluări
- ANAT20006 2020: MSK Practice Quiz Short Answer Question Model AnswersDocument3 paginiANAT20006 2020: MSK Practice Quiz Short Answer Question Model AnswersJenniferChenÎncă nu există evaluări
- Pathomechanics of Structural Foot DeformitiesDocument12 paginiPathomechanics of Structural Foot DeformitiesVinay KumarÎncă nu există evaluări
- Denoix1999 Funcional EspaldaDocument34 paginiDenoix1999 Funcional Espaldaalejandro sotoÎncă nu există evaluări
- The Difference RFS PCFD and Mortons FootDocument4 paginiThe Difference RFS PCFD and Mortons FootprofessorrothbartÎncă nu există evaluări
- Ankle JointDocument84 paginiAnkle JointPoojitha reddy MunnangiÎncă nu există evaluări
- Biomechanics of Ankle and FootDocument15 paginiBiomechanics of Ankle and FootJaime Aguilera100% (1)
- Foot and Ankle Injuries of The AthleteDocument24 paginiFoot and Ankle Injuries of The AthleteSurgicalgownÎncă nu există evaluări
- Solomon Ankle Injury PDFDocument9 paginiSolomon Ankle Injury PDFHikmah Wahid AkbarÎncă nu există evaluări
- B1fe PDFDocument13 paginiB1fe PDFKiki Apdillah FeriÎncă nu există evaluări
- Dynamic Structure of The Human Foot Herbert and ElftmanDocument10 paginiDynamic Structure of The Human Foot Herbert and ElftmantriptykhannaÎncă nu există evaluări
- Kinesiology of The HipDocument13 paginiKinesiology of The HipRadoje DakićÎncă nu există evaluări
- Short Right Leg 2Document11 paginiShort Right Leg 2Simo Aster100% (2)
- Ankle N Foot 1&2Document54 paginiAnkle N Foot 1&2YusraÎncă nu există evaluări
- Activiy AnalysisDocument13 paginiActiviy AnalysisSean Loran100% (2)
- Year 11 PDHPE Body in MotionDocument27 paginiYear 11 PDHPE Body in MotiontkÎncă nu există evaluări
- Futura Primus Flexible Great Toe FinalDocument12 paginiFutura Primus Flexible Great Toe FinalNasfikurÎncă nu există evaluări
- Chapter 6 - Muscles of Upper LimbDocument61 paginiChapter 6 - Muscles of Upper LimbMahendran Jayaraman100% (1)
- 02 Handout 2 (4) 2Document5 pagini02 Handout 2 (4) 2Senpai LeonÎncă nu există evaluări
- Design of Load Bearing JointsDocument11 paginiDesign of Load Bearing JointsRohit GothwalÎncă nu există evaluări
- Biology Form 5 Notes Chapter 2 Human SkeletalDocument22 paginiBiology Form 5 Notes Chapter 2 Human SkeletalzuraidaÎncă nu există evaluări
- 02 SkeletalsystemDocument18 pagini02 SkeletalsystemhorozukaÎncă nu există evaluări
- Kinematics of The Ankle and Foot.Document31 paginiKinematics of The Ankle and Foot.Sneha ParveenÎncă nu există evaluări
- Section One: Clinical ObservationDocument10 paginiSection One: Clinical ObservationKhushboo DurejaÎncă nu există evaluări
- Biomechanical Basis of Foot Orthotic PrescriptionDocument6 paginiBiomechanical Basis of Foot Orthotic PrescriptionDusan OrescaninÎncă nu există evaluări
- Manual Therapy: Birgit Castelein, Ann Cools, Thierry Parlevliet, Barbara CagnieDocument6 paginiManual Therapy: Birgit Castelein, Ann Cools, Thierry Parlevliet, Barbara CagnieGuilherme SerpaÎncă nu există evaluări
- Gait AnalysisDocument49 paginiGait AnalysisKrishna KumariÎncă nu există evaluări
- Module 1 2 in Oae 113 Human Anatomy PhysiologyDocument13 paginiModule 1 2 in Oae 113 Human Anatomy PhysiologyJack ElchaÎncă nu există evaluări
- Anatomy Summary BasicDocument54 paginiAnatomy Summary BasicDungani AllanÎncă nu există evaluări
- Prediction of Biological Profile From Foot Dimensions: Could Body Weight and Arch Height Affect Accuracy?Document7 paginiPrediction of Biological Profile From Foot Dimensions: Could Body Weight and Arch Height Affect Accuracy?Ahmad SyaukatÎncă nu există evaluări
- Effect Posture Lumbar SpineDocument5 paginiEffect Posture Lumbar SpineCharlie HigginsÎncă nu există evaluări
- Maam Recio Reviewer PrelimDocument14 paginiMaam Recio Reviewer PrelimJonnifer LagardeÎncă nu există evaluări
- Apps To Functional Anatomy Lecture 6Document9 paginiApps To Functional Anatomy Lecture 6jenÎncă nu există evaluări
- Tut BManklefutcisDocument71 paginiTut BManklefutcisosteoferdianÎncă nu există evaluări
- Phy Class 9Document4 paginiPhy Class 9r jeet ranjanÎncă nu există evaluări
- Anatomia y Biomecanica Pie TobilloDocument21 paginiAnatomia y Biomecanica Pie TobilloJoel OntiverosÎncă nu există evaluări
- Analysis of MovementDocument18 paginiAnalysis of MovementEfren Jonicel Daguio Domingo50% (2)
- Tugas Mendeley 1. Sumber BukuDocument6 paginiTugas Mendeley 1. Sumber BukuAbyudya Rafif KurniawanÎncă nu există evaluări
- ProQuestDocuments 2022 03 01Document11 paginiProQuestDocuments 2022 03 01Éoghan McCulloughÎncă nu există evaluări
- The Natural Rotator Cuff Healing Guide: Heal Your Cuff, Rid the Pain All On Your Own With Natural ExercisesDe la EverandThe Natural Rotator Cuff Healing Guide: Heal Your Cuff, Rid the Pain All On Your Own With Natural ExercisesEvaluare: 5 din 5 stele5/5 (1)
- Practical Problem Solving Questions Foot and AnkleDocument2 paginiPractical Problem Solving Questions Foot and Anklesirish413Încă nu există evaluări
- Foot & Ankle OBDocument229 paginiFoot & Ankle OBAhmed ShehataÎncă nu există evaluări
- Banton BiomechanicsDocument9 paginiBanton BiomechanicsIoan AndraÎncă nu există evaluări
- Pelvis (Innominate) Diagnosis - Pelvis: Possible DiagnosesDocument4 paginiPelvis (Innominate) Diagnosis - Pelvis: Possible DiagnosesMjidKarimÎncă nu există evaluări
- Omt The Core Prevention and Treatment of Low Back Pain PDFDocument115 paginiOmt The Core Prevention and Treatment of Low Back Pain PDFMjidKarimÎncă nu există evaluări
- Corrective ExercisesDocument47 paginiCorrective ExercisesZachary Lee100% (10)
- CFJ 2015 04 Hip Long 6 PDFDocument11 paginiCFJ 2015 04 Hip Long 6 PDFMjidKarimÎncă nu există evaluări
- Alignment Exercise PDFDocument10 paginiAlignment Exercise PDFMjidKarimÎncă nu există evaluări
- 10-2-13 945am Diagnosis and Treament of Scapular Injuries T - Goodwin PDFDocument68 pagini10-2-13 945am Diagnosis and Treament of Scapular Injuries T - Goodwin PDFMjidKarimÎncă nu există evaluări
- Quiqz FLCH Card OsteoDocument391 paginiQuiqz FLCH Card OsteoMjidKarimÎncă nu există evaluări
- HandsOn Muscle TherapyDocument38 paginiHandsOn Muscle TherapyPhoenixRising61100% (2)
- 2009 Sacrum DiagnosisDocument9 pagini2009 Sacrum DiagnosisMjidKarimÎncă nu există evaluări
- +++++cervical Diagnosis PDFDocument7 pagini+++++cervical Diagnosis PDFMjidKarimÎncă nu există evaluări
- ++++++++ Pthomechanic PDFDocument27 pagini++++++++ Pthomechanic PDFMjidKarimÎncă nu există evaluări
- Malocclusions Linked To Abnormal Foot Motion PDFDocument6 paginiMalocclusions Linked To Abnormal Foot Motion PDFMjidKarimÎncă nu există evaluări
- HandsOn Muscle TherapyDocument38 paginiHandsOn Muscle TherapyPhoenixRising61100% (2)
- Structure/Muscle Information Landmarks: Head Neck and Face Mastoid ProcessDocument9 paginiStructure/Muscle Information Landmarks: Head Neck and Face Mastoid ProcessMjidKarimÎncă nu există evaluări
- Podiatry Review July 2011 PDFDocument4 paginiPodiatry Review July 2011 PDFMjidKarimÎncă nu există evaluări
- OsteopathicEvaluationandTreatmentofSacroiliacJointProblems PDFDocument63 paginiOsteopathicEvaluationandTreatmentofSacroiliacJointProblems PDFMjidKarimÎncă nu există evaluări
- Richard Ogden, DO, FACOFP, FAAFP Kansas Association of Osteopathic MedicineDocument38 paginiRichard Ogden, DO, FACOFP, FAAFP Kansas Association of Osteopathic MedicineMjidKarimÎncă nu există evaluări
- Biomechanics Powerpoint PDFDocument12 paginiBiomechanics Powerpoint PDFMjidKarimÎncă nu există evaluări
- OsteopathicEvaluationandTreatmentofSacroiliacJointProblems PDFDocument63 paginiOsteopathicEvaluationandTreatmentofSacroiliacJointProblems PDFMjidKarimÎncă nu există evaluări
- Biomechanics Powerpoint PDFDocument12 paginiBiomechanics Powerpoint PDFMjidKarimÎncă nu există evaluări
- Tapingtecniques PDFDocument28 paginiTapingtecniques PDFMjidKarimÎncă nu există evaluări
- Facial Changes Linked To Abnormal Foot Motion PDFDocument8 paginiFacial Changes Linked To Abnormal Foot Motion PDFMjidKarimÎncă nu există evaluări
- Positive Health Sept2011 PDFDocument4 paginiPositive Health Sept2011 PDFMjidKarimÎncă nu există evaluări
- Muscle Energy Technique Powerpoint PDFDocument21 paginiMuscle Energy Technique Powerpoint PDFMjidKarim0% (1)
- Biomechanics Powerpoint PDFDocument12 paginiBiomechanics Powerpoint PDFMjidKarimÎncă nu există evaluări
- Malocclusions Linked To Abnormal Foot Motion PDFDocument6 paginiMalocclusions Linked To Abnormal Foot Motion PDFMjidKarimÎncă nu există evaluări
- Facial Changes Linked To Abnormal Foot Motion PDFDocument8 paginiFacial Changes Linked To Abnormal Foot Motion PDFMjidKarimÎncă nu există evaluări
- Conversational Hypnosis CD1Document26 paginiConversational Hypnosis CD1MjidKarimÎncă nu există evaluări
- G10 Bio CellsDocument6 paginiG10 Bio CellsswacaneÎncă nu există evaluări
- Winter Course Allocation Report (Updated On 18dec2015)Document274 paginiWinter Course Allocation Report (Updated On 18dec2015)ASEEMÎncă nu există evaluări
- BTC023Document2 paginiBTC023jaskirat singhÎncă nu există evaluări
- Your Kaplan Medical Timeline PDFDocument6 paginiYour Kaplan Medical Timeline PDFpinkyÎncă nu există evaluări
- Gentamicin in NeonatusDocument9 paginiGentamicin in NeonatusSalsabila RaniahÎncă nu există evaluări
- c20 Microbiology Tortora TestbankDocument19 paginic20 Microbiology Tortora Testbankwhitewave25100% (1)
- Altitude Adaptation Through Hematocrit Change RevisarDocument8 paginiAltitude Adaptation Through Hematocrit Change RevisarMiguel Angel Santacruz VasquezÎncă nu există evaluări
- Evidence-Based Medicine: Lucman, Hakeymah Lunag, Tara Jane Magaoay, CheyserineDocument71 paginiEvidence-Based Medicine: Lucman, Hakeymah Lunag, Tara Jane Magaoay, CheyserinereadmeamllionÎncă nu există evaluări
- Redox-Potential and Immune-Endothelial Axis States of Pancreases in Type 2 Diabetes Mellitus in ExperimentsDocument6 paginiRedox-Potential and Immune-Endothelial Axis States of Pancreases in Type 2 Diabetes Mellitus in ExperimentsEdisher TsivtsivadzeÎncă nu există evaluări
- Module 08: Genetics: Student ObjectivesDocument9 paginiModule 08: Genetics: Student ObjectivesŞterbeţ RuxandraÎncă nu există evaluări
- Essential, Trace, and Nonessential Ions-1Document3 paginiEssential, Trace, and Nonessential Ions-1John AndanÎncă nu există evaluări
- Virus Dynamics Mathematical Principles of ImmunoloDocument12 paginiVirus Dynamics Mathematical Principles of ImmunoloDhiman NathÎncă nu există evaluări
- Haemophilus InfluenzaeDocument16 paginiHaemophilus Influenzaehasan benokriÎncă nu există evaluări
- Fab Classification of Aml PDFDocument2 paginiFab Classification of Aml PDFBenÎncă nu există evaluări
- Questions BasedDocument69 paginiQuestions Baseds007750Încă nu există evaluări
- Stress: What? Why? When? How?Document15 paginiStress: What? Why? When? How?Marjorie HerreraÎncă nu există evaluări
- Protective Effect of Allium Cepa L. (Onion) Against Potassium Bromate-Induced Hematological, Biochemical and Histopathological Alterations in RatsDocument7 paginiProtective Effect of Allium Cepa L. (Onion) Against Potassium Bromate-Induced Hematological, Biochemical and Histopathological Alterations in RatsInternational Journal of Innovative Science and Research TechnologyÎncă nu există evaluări
- TRANSFAC and JASPAR PWMs TableDocument9 paginiTRANSFAC and JASPAR PWMs Tablealya ghinaÎncă nu există evaluări
- 4092 24437 1 PBDocument13 pagini4092 24437 1 PBCloudcynaraaÎncă nu există evaluări
- General ToxicologyDocument57 paginiGeneral ToxicologyOhoodÎncă nu există evaluări
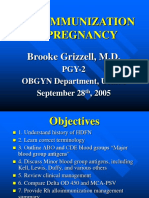
- Alloimmunization in Pregnancy: Brooke Grizzell, M.DDocument40 paginiAlloimmunization in Pregnancy: Brooke Grizzell, M.DhectorÎncă nu există evaluări
- Perspective Summer2012Document24 paginiPerspective Summer2012api-161635461Încă nu există evaluări
- Animalhealth Flyer Vetmax Aiv CO125306Document2 paginiAnimalhealth Flyer Vetmax Aiv CO125306Yoana GulenovaÎncă nu există evaluări
- Rage Against The Machine: Advancing The Study of Aggression Ethology Via Machine LearningDocument20 paginiRage Against The Machine: Advancing The Study of Aggression Ethology Via Machine LearningCony GSÎncă nu există evaluări
- Big Data in HealthcareDocument3 paginiBig Data in HealthcareDavies Ngugi MÎncă nu există evaluări
- Phenotypic Characterization of Class II MalocclusionDocument88 paginiPhenotypic Characterization of Class II MalocclusionPoonam K JayaprakashÎncă nu există evaluări
- 012 Analysis of Reticulocyte Parameters On The Sysmex XEDocument8 pagini012 Analysis of Reticulocyte Parameters On The Sysmex XEblanket_thÎncă nu există evaluări
- Principles of Capture - PrintableDocument51 paginiPrinciples of Capture - PrintableNguyen Thi Phuong NhiÎncă nu există evaluări
- NCP DMDocument4 paginiNCP DMStef Bernardo67% (3)
- Inheritance Biology IGCSE WorksheetDocument2 paginiInheritance Biology IGCSE WorksheetJia Ru100% (2)