Documente Academic
Documente Profesional
Documente Cultură
Rotator Cuff Reconstruction and Humeral Head Replacement Using Smaller Humeral Prostheses in Cuff Tear Arthropathy Patients Under 70 Years of Age
Încărcat de
Aurea De Jesus Romo0 evaluări0% au considerat acest document util (0 voturi)
64 vizualizări11 paginiIrreparable Rotator Cuff Tear, Cuff Reconstruction, Cuff Tear Arthropathy, Humeral Head
Replacement Using a Small Head
Titlu original
Rotator Cuff Reconstruction and Humeral Head Replacement Using Smaller Humeral Prostheses in Cuff Tear Arthropathy Patients under 70 Years of Age
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentIrreparable Rotator Cuff Tear, Cuff Reconstruction, Cuff Tear Arthropathy, Humeral Head
Replacement Using a Small Head
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
64 vizualizări11 paginiRotator Cuff Reconstruction and Humeral Head Replacement Using Smaller Humeral Prostheses in Cuff Tear Arthropathy Patients Under 70 Years of Age
Încărcat de
Aurea De Jesus RomoIrreparable Rotator Cuff Tear, Cuff Reconstruction, Cuff Tear Arthropathy, Humeral Head
Replacement Using a Small Head
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 11
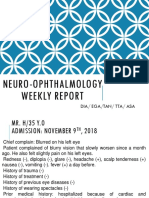
Open Journal of Orthopedics, 2014, 4, 263-272
Published Online October 2014 in SciRes. http://www.scirp.org/journal/ojo
http://dx.doi.org/10.4236/ojo.2014.410043
How to cite this paper: Miyoshi, N., Suenaga, N., Oizumi, N., Taniguchi, N. and Ito, H. (2014) Rotator Cuff Reconstruction
and Humeral Head Replacement Using Smaller Humeral Prostheses in Cuff Tear Arthropathy Patients under 70 Years of Age.
Open Journal of Orthopedics, 4, 263-272. http://dx.doi.org/10.4236/ojo.2014.410043
Rotator Cuff Reconstruction and Humeral
Head Replacement Using Smaller Humeral
Prostheses in Cuff Tear Arthropathy
Patients under 70 Years of Age
Naoki Miyoshi
1
, Naoki Suenaga
2
, Naomi Oizumi
2
, Noboru Taniguchi
3
, Hiroshi Ito
1
1
Department of Orthopaedic Surgery, Asahikawa Medical University, Asahikawa, Japan
2
The Upper Extremity Center of Joint Replacement and Endoscopic Surgery, Hokushin Hospital,
Sapporo, Japan
3
Department of Orthopaedic Surgery, Miyazaki University, Miyazaki, Japan
Email: mnao@asahikawa-med.ac.jp
Received 15 August 2014; revised 30 September 2014; accepted 16 October 2014
Copyright 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/
Abstract
Background: Most reverse shoulder arthroplasty (RSA) studies have shown good improvement in
arm elevation without improvements in external rotation (ER). In addition, high rates of compli-
cations after long-term RSA have been reported, suggesting that RSA should be limited to elderly
patients, especially those who are older than 70 years old. Since 2001, we have developed a strat-
egy of rotator cuff reconstruction with muscle transfer and humeral head replacement (HHR), us-
ing smaller humeral prostheses, in cuff tear arthropathy patients. The aim of the present study
was to investigate the clinical outcome of our strategy in patients under 70 years of age who had
irreparable rotator cuff tears and osteoarthritis. Materials and Methods: A total of 25 shoulders of
25 patients under 70 years of age (males, 15; females, 10) with irreparable cuff tears were treated
with HHR and cuff reconstruction. The average age at the time of surgery was 64.3 years (range, 55
- 69) and the average follow-up period was 38.7 months (range, 24 - 72). The cuff defect was re-
paired using a partial subscapularis transfer in 14 shoulders; nine shoulders required a latissimus
dorsi transfer, one required a pectoralis major transfer, and one required both a latissimus dorsi
and a pectoralis major transfer. Clinical outcomes were assessed with the range of motion (ROM),
UCLA score, Japanese Orthopaedic Association (JOA) score and postsurgical complications. Re-
sults: Shoulder pain was diminished in all patients after surgery. The preoperative UCLA and JOA
scores were 13.1 and 47.0 respectively, improving to 28.6 and 81.5 respectively after surgery. Ac-
tive forward flexion has improved from an average of 89.0 to 138.8, and the ER improved from an
average of 16.2 to 33.2. No complications occurred after surgery. Conclusion: Anatomical recon-
struction using smaller head humeral prostheses yielded favorable results and less complication,
N. Miyoshi et al.
264
compared with RSA. Considering another advantage of ability to retain glenoid bone stock, the
current procedure can be a useful option for irreparable rotator cuff tears with OA in patients un-
der 70 years old.
Keywords
Irreparable Rotator Cuff Tear, Cuff Reconstruction, Cuff Tear Arthropathy, Humeral Head
Replacement Using a Small Head
1. Introduction
Cuff tear arthropathy is a difficult shoulder joint problem. Recently, reverse shoulder arthroplasty (RSA) has
been performed worldwidely [1]-[6] with many RSA studies showing good improvements in arm elevation.
However, Favard et al. [2] noted that the Constant-Murley score was less than 30 points in 72% at 10 years after
RSA. Furthermore, high rates of complications, such as deltoid rupture, glenoid loosening, infection, neurologic
injury, dislocation, acromial fracture, and breakage of the prosthesis, can occur over the long-term after RSA.
Therefore, Boileau et al. [1] suggested that RSA should be limited to elderly patients, especially those over 70
years of age. It is thus necessary to consider alternative treatment option for younger patients with irreparable
rotator cuff tear with osteoarthritis (OA). In order to solve this problem, since 2001, we have developed a strat-
egy [7] to use a smaller humeral head for humeral head replacement (HHR) combined with cuff reconstruction
using remained subscapularis and teres minor, or tendon transfers. Using a smaller head allows easier recon-
struction of rotator cuff defects and medial shift of the center of rotation of the shoulder joint, which increases
the lever arm of the deltoid muscle. The aim of the present study was to investigate the clinical outcomes of our
strategy in patients under 70 years of age who had irreparable rotator cuff tears and OA.
2. Patients and Methods
This retrospective study involved 25 shoulders (17 right; 8 left) of 25 patients under 70 years of age (15 males;
10 females) with irreparable cuff tears that were treated with HHR and cuff reconstruction. The follow-up was
performed over a period of more than 24 months.
2.1. Surgical Procedure
All procedures were performed on patients in a beach-chair position under general anesthesia with a preopera-
tive interscalene block. A superior deltoid splitting approach between the anterior and middle fibers with pre-
servation of the coracoacromial arch was performed. Approximately 5 mm of the lateral side of the acromion
was resected to promote better healing of the repaired deltoid muscle, and the humeral head was exposed. After
confirming the size of the rotator cuff tear and evaluating the humeral head cartilage, HHR was performed when
it was not possible to suture the torn rotator cuff tendon to the top of the humeral head even after intra- and ex-
tra-articular mobilization of the cuff and the humeral head showed OA changes. After resection of the humeral
head at the level of anatomical neck, with guidance provided by the collar of the trial stem, the stem was in-
serted with a 40 angle of retroversion (Figure 1(a)). The retroversion should be greater than that for usual
humeral head replacement with intact cuff tendons to avoid antero-superior escape of the head. Impaction bone
grafting was performed during humeral stem insertion using cancellous bone from the resected humeral head
and an artificial bone tip (HA) (Figure 1(b)). At this point, the size of the humeral head was determined. A head
with a diameter that matched the osteotomy surface was initially selected; this was usually one-size smaller than
the original head because the humeral head diameter of the affected shoulder is usually larger than that of the
unaffected side. If the cuff could not be repaired with the selected humeral head, a thinner head with the same
diameter was then tried, and next, if necessary, a thinner head with a smaller diameter (at most 4 mm smaller)
was tried (Figure 1(d)). However, an even smaller head should not be used to avoid too much incongruity and
instability between the head and the glenoid. Fluoroscopy was used to confirm that the greater tubercle was not
higher than the selected humeral head. When the greater tubercle appeared to be higher (Figure 1(c)), it was
shaved to an appropriate height. If the cuff could still not be repaired with a smaller and thinner head, tendon
N. Miyoshi et al.
265
Figure 1. Operative image of humeral head replacement: (a) Resection of the humeral
head under the guidance of a trial stem; (b) A humeral stem inserted at 40 retrover-
sion with impaction bone grafting using cancellous bone from the resected humeral
head and an artificial bone tip (HA). White arrow: bone grafting using cancellous
bone from the resected humeral head and an artificial bone tip; (c) The height of the
humeral head prosthesis and greater tubercle measured radiographically. White arrow:
The greater tubercle is higher than the humeral head prosthesis; (d) The size of the
humeral head was determined. A head with a diameter that matched the osteotomy
surface was initially selected; this was usually one-size smaller than the original head.
If the cuff could not be repaired with the selected humeral head, a thinner head with
the same diameter was then tried, and next, if necessary, a thinner head with a smaller
diameter (at most 4 mm smaller) was tried.
transfers were considered as an adjunctive procedure. In most cases in this series, the supraspinatus and infras-
pinatus tendons were torn and remarkably retracted, and show severe degeneration and atrophy. In cases in
which the subscapularis and teres minor tendons remained intact, two thirds of the superior aspect of the intact
subscapularis muscle was detached subperiosteally (Figure 2(a)) and transferred antero-superiorly while the in-
tact teres minor tendon was lifted postero-superiorly. The teres minor and subscapularis tendons were side-to-
side sutured and then sutured laterally to the greater tubercle (Figure 2(b) and Figure 2(c)). Furthermore, if
possible, the supraspinatus and infraspinatus tendons were sutured at the medial site of the transferred subsca-
pularis and teres minor tendon (Figure 2(d)). If the anterosuperior part of the rotator cuff including the subsca-
pularis was deficient, a pectoralis major transfer was performed to cover the defect, adding the deltopectoral ap-
proach and passing the pars sternocostalis of the pectoralis major tendon under the conjoined tendon. If the
posterosuperior part of the rotator cuff including the teres minor was deficient, a latissimus dorsi transfer was
performed with an anterior approach, and the latissimus dorsi tendon was passed under the deltoid muscle.
The cuff defect was primarily repaired, including a partial subscapularis transfer, in 14 shoulders; nine shoul-
ders required a latissimus dorsi transfer, one required a pectoralis major transfer, and one required both a latis-
simus dorsi and a pectoralis major transfer.
2.2. Postoperative Treatment
An abduction pillow was used for eight weeks postoperatively. Active elevation in a sitting position from the
adducted position of the shoulder was permitted after 10 weeks, and isometric cuff exercises were initiated at 12
weeks. The patients were allowed to resume heavy work after sufficient muscle strength was evident, along with
range of motion (ROM) recovery, at six months or more postoperatively (Figure 3).
2.3. Clinical Evaluation
Clinical outcomes were assessed using the following criteria: ROM (active flexion, active external rotation [ER]
and internal rotation [IR]); the University of California, Los Angeles shoulder score (UCLA score); the shoulder
score of the Japanese Orthopaedic Association (JOA score) (Table 1); complications due to surgery.
Statistical analysis of the preoperative and postoperative data was performed using paired t-test. P values <
N. Miyoshi et al.
266
(a) (b)
(c) (d)
Figure 2. Operative image of cuff reconstruction: (a) Two thirds of the
superior aspect of the intact subscapularis and teres minor tendon has
been detached subperiosteally; (b) and (c) The intact teres minor tendon
has been lifted postero-superiorly while the subscapularis tendon, with a
partially resected attachment site, has been lifted anterio-superiorly. The
teres minor and subscapularis tendons have been side-to-side sutured
and then sutured laterally to the greater tubercle; (d) If possible, the su-
praspinatus and infraspinatus tendons were sutured at the medial site of
the transferred subscapularis and teres minor tendon.
Figure 3. The protocol of postoperative treatment.
0.05 was considered significant.
3. Results
In this study, the average patient age was 64.3 years (range, 55 - 69 years) and the average follow-up period was
38.7 months (range, 24 - 72 months) (Table 2). One of the patients (Table 2, Case 3) had history of a shoulder
dislocation. All patients reported none or mild shoulder pain after surgery. The mean preoperative UCLA and
JOA scores were 13.1 points (range, 6 - 19) and 47.0 points (range, 13 - 79.5), respectively, and both signifi-
cantly improved at the final follow-up to 28.6 points (range, 16 - 34) and 81.5 points (range, 59 - 93), respec-
tively (P < 0.0001 for both score improvements). Active forward flexion improved from an average of 89.0 to
N. Miyoshi et al.
267
Table 1. Japanese Orthopaedic Association (JOA) score.
I PAIN (30 Points)
None
30
Tenderness or minimal pain in sports or heavy labor 25
Minimal pain in ADL
20
15
Moderate and tolerable pain (Analgetic needed, occasional night pain) 10
Severe pain (ADL limited, frequent night pain) 5
Totally incapacitated because of pain 0
II FUNCTION (20 Points)
Strength in Abduction (5 Points)
Endurance (5 Points)
(To be measured at 90
degrees of abduction or
at possible abduction level.)
Normal 5
(Time in seconds of
holding 1 kg dumb-bell
horizontally with
elbow extended and
force arm pronated)
More than 10
seconds
5
Excellent 4
More than 3
seconds
3
Good 3
More than 2
seconds
1
Fair 2
Zero
0
Poor 1
Zero 0
Activities of Daily Living (10 Points)
Combing hair 1 Reaching opposite axilla 1
Making knot in back 1 Open and close sliding door 1
Reaching mouth 1 Reaching overhead shelf 1
Sleep on involved side 1 Self hygienic care 1
Reaching side pocket(jacket) 1 Wearing jacket 1
Subtract one point from above for each activity that cannot be carried out, specify;
1. 2. 3.
III RANGE OF MOTION (30 Points)
Elevation (15 Points) Exertal Rotation (9 Points) Internal Rotation (6 Points)
More than 150 degrees 15 More than 60 degrees 9 Above T12 spinous process 6
More than 120 degrees 12 More than 30 degrees 6 Above L5 spinous process 4
More than 90 degrees 9 More than 0 degrees 3 Gluteal
2
More than 60 degrees 6 More than 20 degrees 2 Below gluteal
0
More than 30 degrees 3 Less than 20 degrees 0
0 degree 0
IV ROENTGENOGRAPHIC EVALUATION (5 Points)
Normal
5
Moderate changes or subluxation 3
Advanced change or dislocation 0
V JOINT STABILITY (15 Points)
Normal
15
Slight instability or apprehension 10
Severe instability or history or state of subluxation 5
Relevant history or state of dislocation 0
N. Miyoshi et al.
268
Table 2. All cases in the present study.
Case Follow-up Age Sex Disease
Hamada
classification
Seebauer
classification
Surgical methods
1 40 60 M Cuff tear arthropathy 1 I A HHR
2 72 64 F Cuff tear arthropathy 1 I A HHR + LD
3 62 58 F Cuff tear arthropathy 1 I A HHR + LD + PMJ
4 50 69 F Cuff tear arthropathy 1 I A HHR + LD
5 24 63 M Cuff tear arthropathy 2 I A HHR
6 34 65 F Cuff tear arthropathy 2 I A HHR + LD
7 61 67 F Cuff tear arthropathy 2 I A HHR + LD
8 26 68 M Cuff tear arthropathy 3 I A HHR + PMJ
9 41 55 M Cuff tear arthropathy 3 I A HHR + Cofield
10 33 60 M Cuff tear arthropathy 3 II A HHR + LD
11 24 64 M Cuff tear arthropathy 3 II A HHR + LD
12 36 67 M Cuff tear arthropathy 1 I A HHR + Cofield
13 36 67 M Cuff tear arthropathy 3 II A HHR + LD
14 47 69 M Cuff tear arthropathy 3 I A HHR + Cofield
15 27 61 F Cuff tear arthropathy 1 I A HHR + Cofield
16 54 58 M Cuff tear arthropathy 3 I B HHR + LD
17 24 65 F Cuff tear arthropathy 2 II A HHR
18 66 69 F Cuff tear arthropathy 1 I A HHR + LD
19 31 68 M Cuff tear arthropathy 4 I B HHR
20 38 59 M Cuff tear arthropathy 2 I A HHR + Cofield
21 47 61 M Cuff tear arthropathy 2 II A HHR + LD
22 24 64 F Cuff tear arthropathy 3 II A HHR + Cofield
23 24 68 M Cuff tear arthropathy 3 II A HHR + Cofield
24 24 69 F Cuff tear arthropathy 1 I A HHR + Cofield
25 24 69 M Cuff tear arthropathy 4 II A HHR + Cofield
HHR: humeral head replacement; LD: latissimus dorsi transfer; PMJ: pectralis major transfer; Cofield: Subscapularis partial tendon transfer.
138.8 (P < 0.0004), and the ER improved from an average of 16.2 to 33.2 (P = 0.0055) postoperatively
(Figure 4 and Table 3). No complications, such as dislocations, infections, fractures, or nerve injuries, were
observed.
4. Discussion
Cuff tear arthropathy was introduced in 1977 by Neer [8]. Numerous studies [8]-[14] of the use of total shoulder
arthroplasty and HHR for this disease have been reported. However, due to concerns over loosening of the gle-
noid component after total shoulder arthroplasty, HHR has become the preferred treatment. In most reports on
HHR [8]-[14], complete repair of the rotator cuff was not possible; the clinical results included excellent pain
relief, but only modest functional improvements.
Among the few reports describing the long-term results of HHR, Goldberg et al. [11] [12] reported the sur-
gical techniques and their long-term results for 25 shoulders at a mean of 10 years postoperatively. None of the
patients reported severe pain or underwent revision surgery for problems related to the implant. In addition, 34
shoulders were also evaluated after undergoing HHR more than two years. The shoulder with complete coverage
of cuff showed a trend to improved outcomes compared with the shoulders with partial coverage. Furthermore, a
humeral head implant was sized by comparing with the resected humeral head fragment, and they suggested the
importance of not overstuffing the joint with a larger head. Regarding the size of the humeral head implant, Pol-
lock et al. [13] also suggested that some looseness of fit can be tolerated, but gross instability is unacceptable.
N. Miyoshi et al.
269
(a) (b)
Figure 4. Results from the present study: (a) Active motion (flexion, external rotation); (b) UCLA score and JOA score.
Table 3. Clinical results of all cases.
Case
Pre-operation Post-operation
UCLA score JOA score Flexion ER IR UCLA score JOA score Flexion ER IR
1 14 58 140 20
30 81.5 160 60 Th12
2 6 16 20 10 hip 32 68.5 160 10 L1
3 8 13 0 0 thigh 32 87.5 160 50 Th12
4 6 36 20 10 hip 32 85 165 45 hip
5 13 54 115 25 hip 31 89 135 40 L3
6 11 26 60 20 hip 29 77 130 20
7 10 32 30 30 L4 29 80 120 10 L5
8 19 57 150 35 L4 32 87 165 45 L3
9 13 45 80 60 hip 32 91 165 30 L3
10 13 37 60 20
26 70 150 30 L3
11 14 54 95 30 L3 30 78 160 60 L1
12 12 52 100 10 S 31 86 130 45 L4
13 11 33 50 30 L1 18 66.5 60 30 L3
14 14 51 145 20 L3 30 92 150 30 L1
15 13 42 95 15 Th12 29 79 130 20 L3
16 12 39 10 40 L2 30 89 170 60 hip
17 10 39 45 30 L3 21 72.5 100 30 L1
18 17 61 165 45 Th12 30 90 160 60 Th10
19 18 74 120 0 hip 34 93 150 0 L1
20 11 33 60 10 Th12 34 85 160 30 L4
21 15 55 130 10 L1 16 69 45 20
22 16 61 145 10 L1 29 89 150 30 S
23 18 76.5 135 45 L1 32 89.5 150 30 L3
24 19 79.5 165 30 Th10 30 84.5 165 35 Th12
25 14 52 90 20 L3 16 59 80 10 hip
ER: external rotation; IR: internal rotation; UCLA: University of California, Los Angeles; JOA: Japanese Orthopaedic Association.
N. Miyoshi et al.
270
As these previous reports suggested, HHR for cuff tear arthropathy can relieve pain, but cuff function is not
sufficiently restored with only repair of the torn cuff muscles that have usually developed atrophy and fatty- in-
filtration.
Previous studies have reported the use of various operative procedures for irreparable massive rotator cuff
tears, such as the patch method, the Debeyre-Patte procedure, partial repair, arthroscopic subacromial decom-
pression, and debridement. [15]-[17] At our institution, we have performed cuff reconstructions, combined with
latissimus dorsi tendon and pectoralis major tendon transfers, as the primary option for irreparable massive ro-
tator cuff tears, with the objective of restoring cuff function with healthy muscles instead of using deteriorated
torn muscles. However, since some reports [18] [19] have found OA progression after tendon transfer in patients
with cuff tear arthropathy and an irreparable rotator cuff tear with OA, we have performed HHR using a small
humeral head prosthesis in addition to cuff reconstruction.
Recently, RSA has been primarily indicated for irreparable rotator cuff tears. In many reports [1]-[6] describ-
ing RSA outcomes, good improvements in flexion have been reported, with only small improvements in ER.
The present study demonstrated that HHR performed using a small humeral head and cuff reconstruction for ir-
reparable rotator cuff tear in patients less than 70 years of age provided favorable results compared with pre-
viously reported RSA results, especially with respect to ER (Table 4). Some reports indicated that complications
occured in 14% - 68% of RSA cases [3]-[6], which is a relatively high complication rate. In contrast, in the
present study, dislocations, infections, fractures, nerve injuries, or other complications were not observed (Table
5).
Another advantage of our strategy is that the glenoid bone stock can be maintained after surgery. If further re-
vision surgery is eventually required, RSA can still be considered as a reconstruction option. Since the patients
included in the present study were relatively active, long-term follow-up is required to assess their continued
progress.
The disadvantages of the current surgical procedure are the requirement for tendon transfers and the compli-
cated postoperative treatment. Further follow-up is necessary to assess the long-term outcomes of the current
procedure. In the present study, three patients had postoperative forward flexion of less than 90. These cases
were Seebauers classification type IIA and Hamadas classification grade 3 or 4 on the X-ray evaluations. In a
future study, factors contributing to the poor results of this technique should be examined.
The small number of cases, short follow-up time and the fact that glenoid wear was not evaluated are the li-
mitations of the present study.
Table 4. Clinical results comparing the present study and RSA.
Shoulders, n
Mean age, years Follow-up Flex () ER ()
(range) (months) Pre post ope
Wall et al. [5] 191 72.7 (23 - 86) 39.9 86 137 8 6
RSA Werner et al. [6] 58 68 (44 - 84) 38 42 100 17 12
Sirveaux et al. [4] 77 73 (60 - 86) 44.5 73 138 3.5 11.2
Present study
25 64.3 (55 - 69) 38.7 89 138.8 16.2 33.2
RSA: reverse shoulder arthroplasty; Flex: flexion; ER: external rotation.
Table 5. Complications reported from RSA.
Shoulders, n Complication rate (%) Re-operation rate (%)
Wall et al. [5] 191 19 28
Werner et al. [6] 58 50 33
Sirveaux et al. [4] 80 16 3.8
Guery et al. [3] 66 14 11
Present study 25 0 0
N. Miyoshi et al.
271
5. Conclusions
HHR using small humeral head prostheses and cuff reconstruction for irreparable massive rotator cuff tears and
OA in patients less than 70 years of age showed favorable outcomes with active flexion and ER, with improve-
ments that were greater than those reported in the previous RSA studies.
The operative procedure used in the present study is considered particularly useful in relatively young people
for whom RSA is not considered to be the first option. And, with the glenoid bone stock remains, TSA or RSA
can be performed as a revision surgery at a later stage.
References
[1] Boileau, P., Watkinson, D., Hatzidakis, A.M. and Hovorka, I. (2006) The Grammont Reverse Shoulder Prosthesis:
Results in Cuff Tear Arthritis, Fracture Sequelae, and Revision Arthroplasty. Journal of Shoulder and Elbow Surgery,
15, 527-540. http://dx.doi.org/10.1016/j.jse.2006.01.003
[2] Favard, L., Levigne, C., Nerot, C., Gerver, C., Wilde, L.D. and Mole, D. (2011) Reverse Prostheses in Arthropathies
with Cuff Tear: Are Survivorship and Function Maintained Over Time? Clinical Orthopaedics and Related Research,
469, 2469-2475. http://dx.doi.org/10.1007/s11999-011-1833-y
[3] Guery, J., Favard, L., Sirveaux, F., Oudet, D., Mole, D. and Walch, G. (2006) Reverse Total Arthroplasty: Survivor-
ship Analysis of Eighty Replacements Followed for Five to Ten Years. The Journal of Bone and Joint Surgery, 88,
1742-1747. http://dx.doi.org/10.2106/JBJS.E.00851
[4] Sirveaux, F., Favard, L., Oudet, D., Huquet, D., Walch, G. and Mole, D. (2004) Grammont Inverted Total Shoulder
Arthroplasty in the Treatment of Glenohumeral Osteoarthritis with Massive Rupture of the Cuff: Results of a Multi-
center Study of 80 Shoulders. The Journal of Bone and Joint Surgery, 86, 388-395.
http://dx.doi.org/10.1302/0301-620X.86B3.14024
[5] Wall, B., Nove-Josserand, L., OConnor, D.P., Edwards, T.B. and Walch, G. (2007) Reverse Total Shoulder Arthrop-
lasty: A Review of Results According to Etiology. The Journal of Bone and Joint Surgery, 89, 1476-1485.
http://dx.doi.org/10.2106/JBJS.F.00666
[6] Werner, C.M.L., Steinmann, P.A., Gilbart, M. and Gerver, C. (2005) Treatment of Painful Pseudoparesis Due to Irre-
parable Rotator Cuff Dysfunction with the Delta III Reverse-Ball-and-Socket Total Shoulder Prosthesis. The Journal of
Bone and Joint Surgery, 87, 1476-1486.
[7] Yamane, S., Suenaga, N., Oizumi, N. and Funakoshi, T. (2011) Total Shoulder Arthroplasty and Humeral Head Re-
placement for Osteoarthritis and Cuff Tear Arthropathy in Patients 75 Years Old and Older. Katakansetsu, 35, 641-
644.
[8] Neer, C.S. 2nd, Craig, E.V. and Fukuda, H. (1983) Cuff Tear Arthropathy. The Journal of Bone and Joint Surgery,
65, 1232-1244.
[9] Arntz, C.T., Jackins, S. and Matsen, F.A. 3rd. (1993) Prosthetic Replacement of the Shoulder for the Treatment of De-
fects in the Rotator Cuff and the Surface of the Glenoid Joint. The Journal of Bone and Joint Surgery, 75, 485-491.
[10] Field, L.D., Dines, D.M., Zabinski, S.F. and Warren, R.F. (1997). Hemiarthroplasty of the Shoulder for Rotator Cuff
Arthropathy. Journal of Shoulder and Elbow Surgery, 6, 18-23. http://dx.doi.org/10.1016/S1058-2746(97)90066-5
[11] Goldberg, S.S., Bell, J.E., Kim, H.J., Bak, S.F., Levine, W.N. and Bigliani, L.U. (2008) Hemiarthroplasty for the Ro-
tator Cuff-Deficient Shoulder. The Journal of Bone and Joint Surgery, 90, 554-559.
http://dx.doi.org/10.2106/JBJS.F.01029
[12] Goldberg, S.S. and Bigliani, L.U. (2009) Hemiarthroplasty for the Rotator Cuff-Deficient Shoulder Surgical Tech-
nique. The Journal of Bone and Joint Surgery, 91, 22-29.
[13] Pollock, R.G., Deliz, E.D., Mcllveen, S.J., Flatow, E.L. and Bigliani, L.U. (1992) Prosthetic Replacement in Rotator
Cuff Deficient Shoulders. Journal of Shoulder and Elbow Surgery, 1, 173-186.
http://dx.doi.org/10.1016/1058-2746(92)90011-Q
[14] Sanchez-Sotelo, J., Cofield, R.H. and Rowland, C.M. (2001) Shoulder Hemiarthroplasty for Glenohumeral Arthritis
Associated with Severe Rotator Cuff Deficiency. The Journal of Bone and Joint Surgery, 83-A, 1814-1822.
[15] Duralde, X.A. and Bair, B. (2005) Massive Rotator Cuff Tears: The Result of Partial Rotator Cuff Repair. Journal of
Shoulder and Elbow Surgery, 14, 121-127. http://dx.doi.org/10.1016/j.jse.2004.06.015
[16] Haeri, G.B. and Wiley, A.M. (1981) Advancement of the Supraspinatus Muscle in the Repair of Ruptures of the Ro-
tator Cuff. The Journal of Bone and Joint Surgery, 63, 232-238.
[17] Labbe, M.R. (2006) Arthroscopic Technique for Patch Augmentation of Rotator Cuff Repairs. Arthroscopy, 22,
1136.e1-1136.e6.
N. Miyoshi et al.
272
[18] Aoki, M., Okamura, K., Fukushima, S., Takahashi, T. and Ogino, T. (1996) Transfer of Latissimus Dorsi for Irrepara-
ble Rotator-Cuff Tears. The Journal of Bone and Joint Surgery, 78-B, 761-766.
[19] Gerber, C. (1992) Latissimus Dorsi Transfer for the Treatment of Irreparable Tears of the Rotator Cuff. Clinical Or-
thopaedics and Related Research, 275, 152-160
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- GEOS-5 File Specification Variable Definition Glossary: 1 Three-Dimensional FieldsDocument11 paginiGEOS-5 File Specification Variable Definition Glossary: 1 Three-Dimensional FieldsAurea De Jesus RomoÎncă nu există evaluări
- Implementation of Hyogo Framework For Action in Makati CityDocument20 paginiImplementation of Hyogo Framework For Action in Makati CityAurea De Jesus RomoÎncă nu există evaluări
- Multivariate Notes r1Document54 paginiMultivariate Notes r1Aurea De Jesus RomoÎncă nu există evaluări
- Advanced Statistics With MatlabDocument5 paginiAdvanced Statistics With MatlabRohit Vishal Kumar100% (2)
- Climate Disaster Resilience of EducationDocument25 paginiClimate Disaster Resilience of EducationAurea De Jesus RomoÎncă nu există evaluări
- Quantitative Methods For Estimating Flood FatalitiesDocument31 paginiQuantitative Methods For Estimating Flood FatalitiesAurea De Jesus RomoÎncă nu există evaluări
- Assessing The Resilience of Delhi To Climate-RelatedDocument16 paginiAssessing The Resilience of Delhi To Climate-RelatedAurea De Jesus RomoÎncă nu există evaluări
- Flood ReportDocument176 paginiFlood ReportlineajonÎncă nu există evaluări
- Explorin The Social Impacts of Flood Risk and Flooding in ScotlndDocument157 paginiExplorin The Social Impacts of Flood Risk and Flooding in ScotlndAurea De Jesus RomoÎncă nu există evaluări
- Explorin The Social Impacts of Flood Risk and Flooding in ScotlndDocument157 paginiExplorin The Social Impacts of Flood Risk and Flooding in ScotlndAurea De Jesus RomoÎncă nu există evaluări
- Nhess 11 2107 2011Document17 paginiNhess 11 2107 2011Aurea De Jesus RomoÎncă nu există evaluări
- Towards An Integrated Flood Vulnerability IndexDocument87 paginiTowards An Integrated Flood Vulnerability IndexAurea De Jesus RomoÎncă nu există evaluări
- Resilience Adaptability and Transformability in SocialDocument9 paginiResilience Adaptability and Transformability in SocialAurea De Jesus RomoÎncă nu există evaluări
- Parametric and Physically Based Modelling Techniques For Flood Risk and Vulnerability Assessment A ComparisonDocument9 paginiParametric and Physically Based Modelling Techniques For Flood Risk and Vulnerability Assessment A ComparisonAurea De Jesus RomoÎncă nu există evaluări
- Implementation of Hyogo Framework For Action in Makati CityDocument20 paginiImplementation of Hyogo Framework For Action in Makati CityAurea De Jesus RomoÎncă nu există evaluări
- Flood ReportDocument176 paginiFlood ReportlineajonÎncă nu există evaluări
- Development and Climate ChangeDocument35 paginiDevelopment and Climate ChangeAurea De Jesus RomoÎncă nu există evaluări
- Modeling Vulnerability and Recilience To Climate ChangeDocument46 paginiModeling Vulnerability and Recilience To Climate ChangeAurea De Jesus RomoÎncă nu există evaluări
- Risk Assessment Methodology at Isla Del Carmen, MexicoDocument13 paginiRisk Assessment Methodology at Isla Del Carmen, MexicoKaritza KenyÎncă nu există evaluări
- Persuasive Presentations Chapters1 2 3Document25 paginiPersuasive Presentations Chapters1 2 3Aurea De Jesus RomoÎncă nu există evaluări
- Resilience Adaptability and Transformability in SocialDocument9 paginiResilience Adaptability and Transformability in SocialAurea De Jesus RomoÎncă nu există evaluări
- Water StorageDocument9 paginiWater StorageAurea De Jesus RomoÎncă nu există evaluări
- Parametric and Physically Based Modelling Techniques For Flood Risk and Vulnerability Assessment A ComparisonDocument9 paginiParametric and Physically Based Modelling Techniques For Flood Risk and Vulnerability Assessment A ComparisonAurea De Jesus RomoÎncă nu există evaluări
- Constructing A Holistic ApproachDocument17 paginiConstructing A Holistic ApproachAurea De Jesus RomoÎncă nu există evaluări
- Nhess 11 2107 2011Document17 paginiNhess 11 2107 2011Aurea De Jesus RomoÎncă nu există evaluări
- Jp1.25 Drought Monitoring Activities in NCDC'S Climate Monitoring BranchDocument6 paginiJp1.25 Drought Monitoring Activities in NCDC'S Climate Monitoring BranchAurea De Jesus RomoÎncă nu există evaluări
- The Potential Impact of Climate Chang On Taiwan... Ching-ChengDocument14 paginiThe Potential Impact of Climate Chang On Taiwan... Ching-ChengAurea De Jesus RomoÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Case Report CMV RetinitisDocument27 paginiCase Report CMV RetinitistaniamaulaniÎncă nu există evaluări
- Bedwetting TCMDocument5 paginiBedwetting TCMRichonyouÎncă nu există evaluări
- Neuro M Summary NotesDocument4 paginiNeuro M Summary NotesNishikaÎncă nu există evaluări
- 107 2021 High Speed Rail Corridor RegDocument3 pagini107 2021 High Speed Rail Corridor Rega siva sankarÎncă nu există evaluări
- Null 6 PDFDocument1 paginăNull 6 PDFSimbarashe ChikariÎncă nu există evaluări
- Chemistry Xi: Short Questions and 20% Long QuestionsDocument3 paginiChemistry Xi: Short Questions and 20% Long QuestionsSyed Nabeel HassanÎncă nu există evaluări
- Task 5 Banksia-SD-SE-T1-Hazard-Report-Form-Template-V1.0-ID-200278Document5 paginiTask 5 Banksia-SD-SE-T1-Hazard-Report-Form-Template-V1.0-ID-200278Samir Mosquera-PalominoÎncă nu există evaluări
- Big 9 Master SoalDocument6 paginiBig 9 Master Soallilik masrukhahÎncă nu există evaluări
- Brief RESUME EmailDocument4 paginiBrief RESUME Emailranjit_kadalg2011Încă nu există evaluări
- HUM110 Gilgamesh EssayDocument4 paginiHUM110 Gilgamesh EssaynsmeganÎncă nu există evaluări
- Dr. Nastiti K - Manajemen Asma Pada Anak 2018 PDFDocument72 paginiDr. Nastiti K - Manajemen Asma Pada Anak 2018 PDFagnesspratiwiÎncă nu există evaluări
- Castle 1-3K E ManualDocument26 paginiCastle 1-3K E ManualShami MudunkotuwaÎncă nu există evaluări
- Epicor Software India Private Limited: Brief Details of Your Form-16 Are As UnderDocument9 paginiEpicor Software India Private Limited: Brief Details of Your Form-16 Are As UndersudhadkÎncă nu există evaluări
- ACF5950 - Assignment # 7 Semester 2 2015: The Business Has The Following Opening Balances: Additional InformationDocument2 paginiACF5950 - Assignment # 7 Semester 2 2015: The Business Has The Following Opening Balances: Additional InformationkietÎncă nu există evaluări
- Chemical Reaction Engineering-II - R2015 - 10-04-2018Document2 paginiChemical Reaction Engineering-II - R2015 - 10-04-201818135A0806 MAKKUVA BHAVYAÎncă nu există evaluări
- The Vapour Compression Cycle (Sample Problems)Document3 paginiThe Vapour Compression Cycle (Sample Problems)allovid33% (3)
- Registration Statement (For Single Proprietor)Document2 paginiRegistration Statement (For Single Proprietor)Sherwin SalanayÎncă nu există evaluări
- Chemical Engineering Projects List For Final YearDocument2 paginiChemical Engineering Projects List For Final YearRajnikant Tiwari67% (6)
- How McDonald'sDocument2 paginiHow McDonald'spratik khandualÎncă nu există evaluări
- ZX110to330 ELEC E PDFDocument1 paginăZX110to330 ELEC E PDFYadi100% (1)
- 5SDD 71B0210Document4 pagini5SDD 71B0210Merter TolunÎncă nu există evaluări
- Solo ParentsDocument1 paginăSolo ParentsOZ CincoÎncă nu există evaluări
- Impact of Employee Motivation in The Banking SectorDocument48 paginiImpact of Employee Motivation in The Banking Sectormohd talalÎncă nu există evaluări
- Comparative Pharmacology For AnesthetistDocument162 paginiComparative Pharmacology For AnesthetistGayatri PalacherlaÎncă nu există evaluări
- AFMAN91-201 NewDocument458 paginiAFMAN91-201 NewbombtechÎncă nu există evaluări
- Itrogen: by Deborah A. KramerDocument18 paginiItrogen: by Deborah A. KramernycÎncă nu există evaluări
- S ELITE Nina Authors Certain Ivey This Reproduce Western Material Management Gupta Names Do OntarioDocument15 paginiS ELITE Nina Authors Certain Ivey This Reproduce Western Material Management Gupta Names Do Ontariocarlos menaÎncă nu există evaluări
- What Is A VolcanoDocument2 paginiWhat Is A VolcanonatachaÎncă nu există evaluări
- Royal British College IncDocument5 paginiRoyal British College IncLester MojadoÎncă nu există evaluări
- Alugbati Plant Pigment Extraction As Natural Watercolor SourceDocument6 paginiAlugbati Plant Pigment Extraction As Natural Watercolor SourceMike Arvin Serrano100% (1)