Documente Academic
Documente Profesional
Documente Cultură
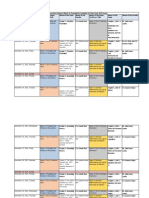
Differential Diagnosis of Valvular Heart Disease
Încărcat de
Abhisek Chatterjee0 evaluări0% au considerat acest document util (0 voturi)
689 vizualizări10 paginiDifferential Diagnosis of Valvular Heart Diseases by Abhisek Chatterjee
Drepturi de autor
© © All Rights Reserved
Formate disponibile
DOCX, PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDifferential Diagnosis of Valvular Heart Diseases by Abhisek Chatterjee
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca DOCX, PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
689 vizualizări10 paginiDifferential Diagnosis of Valvular Heart Disease
Încărcat de
Abhisek ChatterjeeDifferential Diagnosis of Valvular Heart Diseases by Abhisek Chatterjee
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca DOCX, PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 10
Differential diagnosis of valvular heart disease
Mitral Stenosis Mitral
Regurgitation
Aortic Stenosis Aortic Regurgitation Tricuspid
Stenosis
Tricuspid
Regurgitation
Inspection Malar flush,
precordial bulge,
and diffuse
pulsation in
young patients.
Usually prominent
and hyperdynamic
apical impulse to left
of MCL.
Sustained PMI,
prominent atrial
filling wave.
Hyperdynamic PMI to
left of MCL and
downward. Visible
carotid pulsations.
Pulsating nailbeds
(Quincke), head bob
(deMusset).
Giant a wave in
jugular pulse with
sinus rhythm.
Peripheral edema
or ascites, or
both.
Large v wave in
jugular pulse;
time with carotid
pulsation.
Peripheral edema
or ascites, or
both.
Palpation "Tapping"
sensation over
area of expected
PMI. Right
ventricular
pulsation left
third to fifth ICS
parasternally
Forceful, brisk PMI;
systolic thrill over
PMI. Pulse normal,
small, or slightly
collapsing.
Powerful,
heaving PMI to
left and slightly
below MCL.
Systolic thrill
over aortic area,
sternal notch, or
carotid arteries
Apical impulse
forceful and displaced
significantly to left
and downward.
Prominent carotid
pulses. Rapidly rising
and collapsing pulses
(Corrigan pulse).
Pulsating,
enlarged liver in
ventricular
systole.
Right ventricular
pulsation.
Systolic
pulsation of
liver.
when pulmonary
hypertension is
present. P
2
may
be palpable.
in severe
disease. Small
and slowly
rising carotid
pulse. If
bicuspid AS
check for delay
at femoral
artery to
exclude
coarctation.
Heart sounds,
rhythm, and blood
pressure
S
1
loud if valve
mobile. Opening
snap following
S
2
. The worse
the disease, the
closer the S
2
-
opening snap
interval.
S
1
normal or buried
in early part of
murmur (exception is
mitral prolapse where
murmur may be late).
Prominent third heart
sound when severe
MR. Atrial
fibrillation common.
A
2
normal, soft,
or absent.
Prominent S
4
.
Blood pressure
normal, or
systolic
pressure normal
with high
diastolic
S
1
normal or reduced,
A
2
loud. Wide pulse
pressure with diastolic
pressure < 60 mm Hg.
When severe, gentle
compression of
femoral artery with
diaphragm of
stethoscope may
S
1
often loud.
Atrial fibrillation
may be present.
Blood pressure
normal. Midsystolic
clicks may be present
and may be multiple.
pressure.
reveal diastolic flow
(Duroziez) and
pressure in leg on
palpation > 40 mm
Hg than arm (Hill).
Murmurs
Location and
transmission
Localized at or
near apex.
Diastolic rumble
best heard in left
lateral position;
may be
accentuated by
having patient
do sit-ups.
Rarely, short
diastolic
murmur along
lower left sternal
Loudest over PMI;
posteriorly directed
jets (ie, anterior
mitral prolapse)
transmitted to left
axilla, left
infrascapular area;
anteriorly directed
jets (ie, posterior
mitral prolapse) heard
over anterior
precordium. Murmur
unchanged after
Right second
ICS
parasternally or
at apex, heard in
carotid arteries
and
occasionally in
upper
interscapular
area. May
sound like MR
at apex
(Gallaverdin
Diastolic: louder
along left sternal
border in third to
fourth interspace.
Heard over aortic area
and apex. May be
associated with low-
pitched middiastolic
murmur at apex
(Austin Flint) due to
functional mitral
stenosis. If due to an
enlarged aorta,
Third to fifth ICS
along left sternal
border out to
apex.Murmur
increases with
inspiration.
Third to fifth
ICS along left
sternal border.
Murmur hard to
hear but
increases with
inspiration. Sit-
ups can increase
cardiac output
and accentuate.
border (Graham
Steell) in severe
pulmonary
hypertension.
premature beat. phenomenon),
but murmur
occurs after
S
1
and stops
before S
2
. The
later the peak in
the murmur, the
more severe the
AS.
murmur may radiate
to right sternal border.
Timing Relation of
opening snap to
A
2
important.
The higher the
LA pressure the
earlier the
opening snap.
Presystolic
accentuation
before S
1
if in
Pansystolic: begins
with S
1
and ends at or
after A
2
. May be late
systolic in mitral
valve prolapse.
Begins after S
1
,
ends before A
2
.
The more
severe the
stenosis, the
later the
murmur peaks.
Begins immediately
after aortic second
sound and ends before
first sound (blurring
both); helps
distinguish from MR.
Rumble often
follows audible
opening snap.
At times, hard to
hear. Begins
with S
1
and fills
systole.Increases
with inspiration.
sinus rhythm.
Graham Steell
begins with
P
2
(early
diastole) if
associated
pulmonary
hypertension.
Character Low-pitched,
rumbling;
presystolic
murmur merges
with loud S
1
.
Blowing, high-
pitched; occasionally
harsh or musical.
Harsh, rough. Blowing, often faint. As for mitral
stenosis.
Blowing, coarse,
or musical.
Optimum
auscultatory
conditions
After exercise,
left lateral
recumbency.
Bell chest piece
After exercise; use
diaphragm chest
piece. In prolapse,
findings may be more
Use stethoscope
diaphragm.
Patient resting,
leaning
Use stethoscope
diaphragm. Patient
leaning forward,
breath held in
Use stethoscope
bell. Murmur
usually louder and
at peak during
Use stethoscope
diaphragm.
Murmur usually
becomes louder
lightly applied. evident while
standing.
forward, breath
held in full
expiration.
expiration. inspiration.Patient
recumbent.
during
inspiration.
Radiography Straight left
heart border
from enlarged
LA appendage.
Elevation of left
mainstem
bronchus. Large
right ventricle
and pulmonary
artery if
pulmonary
hypertension is
present.
Calcification in
mitral valve in
rheumatic mitral
stenosis or in
Enlarged left
ventricle and LA.
Concentric left
ventricular
hypertrophy.
Prominent
ascending
aorta. Calcified
aortic valve
common.
Moderate to severe
left ventricular
enlargement.Aortic
root often dilated.
Enlarged right
atrium with
prominent SVC
and azygous
shadow.
Enlarged right
atrium and right
ventricle.
annulus in
calcific mitral
stenosis.
ECG Broad P waves
in standard
leads; broad
negative phase
of diphasic P in
V
1
. If
pulmonary
hypertension is
present, tall
peaked P waves,
right axis
deviation, or
right ventricular
hypertrophy
appears.
Left axis deviation or
frank left ventricular
hypertrophy. P waves
broad, tall, or notched
in standard
leads.Broad negative
phase of diphasic P in
V
1
.
Left ventricular
hypertrophy.
Left ventricular
hypertrophy.
Tall, peaked P
waves. Possible
right ventricular
hypertrophy.
Right axis usual.
Echocardiography
Two-dimensional
echocardiography
Thickened,
immobile mitral
valve with
anterior and
posterior leaflets
moving
together.
"Hockey stick"
shape to opened
anterior leaflet
in rheumatic
mitral stenosis.
Annular calcium
with thin leaflets
in calcific mitral
stenosis. LA
enlargement,
normal to small
left ventricle.
Thickened mitral
valve in rheumatic
disease; mitral valve
prolapse; flail leaflet
or vegetations may be
seen. Dilated left
ventricle in volume
overload. Operate for
left ventricular end-
systolic dimension >
4.5 cm.
Dense persistent
echoes from the
aortic valve
with poor
leaflet
excursion. Left
ventricular
hypertrophy late
in the disease.
Bicuspid valve
in younger
patients.
Abnormal aortic valve
or dilated aortic root.
Diastolic vibrations of
the anterior leaflet of
the mitral valve and
septum. In acute
aortic insufficiency,
premature closure of
the mitral valve
before the QRS.
When severe, dilated
left ventricle with
normal or decreased
contractility. Operate
when left ventricular
end-systolic
dimension > 5.0 cm.
In rheumatic
disease, tricuspid
valve thickening,
decreased early
diastolic filling
slope of the
tricuspid valve. In
carcinoid, leaflets
fixed, but no
significant
thickening.
Enlarged right
ventricle with
paradoxical
septal motion.
Tricuspid valve
often pulled
open by
displaced
chordae.
Orifice can be
traced to
approximate
mitral valve
orifice area.
Continuous and
color flow Doppler
and TEE
Prolonged
pressure half-
time across
mitral valve
allows
estimation of
gradient. MVA
estimated from
pressure half-
time. Indirect
evidence of
pulmonary
hypertension by
noting elevated
right ventricular
Regurgitant flow
mapped into LA. Use
of PISA helps assess
MR severity. TEE
important in
prosthetic mitral
valve regurgitation.
Increased
transvalvular
flow velocity;
severe AS when
peak jet > 4
m/sec (64 mm
Hg). Valve area
estimate using
continuity
equation is
poorly
reproducible.
Demonstrates
regurgitation and
qualitatively estimates
severity based on
percentage of left
ventricular outflow
filled with jet and
distance jet penetrates
into left ventricle.
TEE important in
aortic valve
endocarditis to
exclude abscess.
Mitral inflow pattern
describes diastolic
Prolonged
pressure half-time
across tricuspid
valve can be used
to estimate mean
gradient.Severe
tricuspid stenosis
present when
mean gradient > 5
mm Hg.
Regurgitant flow
mapped into
right atrium and
venae cavae.
Right ventricular
systolic pressure
estimated by
tricuspid
regurgitation jet
velocity.
systolic pressure
measured from
the tricuspid
regurgitation jet.
dysfunction.
A2, aortic second sound; AS, aortic stenosis; ICS, intercostal space; LA, left atrial; MCL, midclavicular line; MR, mitral
regurgitation; MVA, measured valve area; P2, pulmonary second sound; PISA, proximal isovelocity surface area; PMI, point of
maximal impulse; S1, first heart sound; S2, second heart sound; S4, fourth heart sound; SVC, superior vena cava; TEE,
transesophageal echocardiography; V1, chest ECG lead 1.
S-ar putea să vă placă și
- Ebstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDe la EverandEbstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsÎncă nu există evaluări
- CVS Examination EditedDocument134 paginiCVS Examination EditedThilak JayalathÎncă nu există evaluări
- Evaluation of Chest Pain in Primary Care Patients-AAFPDocument3 paginiEvaluation of Chest Pain in Primary Care Patients-AAFPnouval_iqbalÎncă nu există evaluări
- Pediatric Pharmacology: Dr. Putrya Hawa, M.Biomed Faculty of Medicine, UIIDocument27 paginiPediatric Pharmacology: Dr. Putrya Hawa, M.Biomed Faculty of Medicine, UIIAfied Fitrah100% (1)
- Tocolytic Agents and Anticonvulsants for Preterm LabourDocument95 paginiTocolytic Agents and Anticonvulsants for Preterm LabourPriya jÎncă nu există evaluări
- CKD PocketGuideDocument2 paginiCKD PocketGuidelayzierainÎncă nu există evaluări
- Common Cold AAFPDocument7 paginiCommon Cold AAFPAnonymous so6ZnlKywÎncă nu există evaluări
- Hypertensive Emergencies in The Emergency DepartmentDocument13 paginiHypertensive Emergencies in The Emergency DepartmentLuis Lopez RevelesÎncă nu există evaluări
- Nur 111 Session 6 Sas 1Document12 paginiNur 111 Session 6 Sas 1Zzimply Tri Sha UmaliÎncă nu există evaluări
- JVP - WL GanDocument1 paginăJVP - WL GanWeh Loong GanÎncă nu există evaluări
- Abdul Rahim Bin Mohamad Nor C 111 10 871: Prof - Dr.Peter Kabo, PHD, SPFK, SPJP (K), Fiha, FasccDocument38 paginiAbdul Rahim Bin Mohamad Nor C 111 10 871: Prof - Dr.Peter Kabo, PHD, SPFK, SPJP (K), Fiha, FasccAis KonorasÎncă nu există evaluări
- 10.08.07 Cardiac Tamponade HaagDocument16 pagini10.08.07 Cardiac Tamponade HaagfoetorÎncă nu există evaluări
- 5 Shock PPT EnglishDocument77 pagini5 Shock PPT EnglishKessi VikaneswariÎncă nu există evaluări
- Advanced Cardiac Life SupportDocument37 paginiAdvanced Cardiac Life SupportRoy Acosta GumbanÎncă nu există evaluări
- Suspecting Pulmonary Hypertension in The Dyspneic Patient: Who, When, and HowDocument92 paginiSuspecting Pulmonary Hypertension in The Dyspneic Patient: Who, When, and HowJonathan LongÎncă nu există evaluări
- Blood and Drugs Medicine NotesDocument39 paginiBlood and Drugs Medicine Notesrahuul prasadÎncă nu există evaluări
- Anti-Arrhythmic Agents For Pharmacy PDFDocument41 paginiAnti-Arrhythmic Agents For Pharmacy PDFKelvinTMaikanaÎncă nu există evaluări
- ECG InterpretationDocument48 paginiECG InterpretationKervayse St.ClairÎncă nu există evaluări
- Valvular Heart DiseaseDocument33 paginiValvular Heart Diseasesimran kaurÎncă nu există evaluări
- CVExamDocument10 paginiCVExamSarah TaiÎncă nu există evaluări
- Heart Failure: Low Output HF High Output HFDocument7 paginiHeart Failure: Low Output HF High Output HFJake BurrÎncă nu există evaluări
- Upper GIT BleedingDocument69 paginiUpper GIT BleedingSoleh Ramly100% (1)
- UTIDocument17 paginiUTIBongkotchakorn Mind PhonchaiÎncă nu există evaluări
- Renovascular Hypertension (RVH) SeminarDocument58 paginiRenovascular Hypertension (RVH) SeminarfaizalmasoodiÎncă nu există evaluări
- PANCE Prep Pearls Valvular Disease PDFDocument4 paginiPANCE Prep Pearls Valvular Disease PDFkatÎncă nu există evaluări
- Manage Stroke with Tests, Treatments & PreventionDocument27 paginiManage Stroke with Tests, Treatments & PreventionHanif SumonÎncă nu există evaluări
- Vasopressors in ShockDocument8 paginiVasopressors in ShockOrion JohnÎncă nu există evaluări
- Managemant Copd CPG MsiaDocument67 paginiManagemant Copd CPG MsiaNur Anis ZarimeÎncă nu există evaluări
- Fluid & Electrolytes Management (Nabil)Document78 paginiFluid & Electrolytes Management (Nabil)Ahmad Nabil Md RosliÎncă nu există evaluări
- ECG IMM 2020.docx.2Document25 paginiECG IMM 2020.docx.2Abdul QuyyumÎncă nu există evaluări
- ECG Workshop 2006Document15 paginiECG Workshop 2006Eggi ErlanggaÎncă nu există evaluări
- Valvular Heart DiseaseDocument2 paginiValvular Heart DiseaseAnonymous TVk12eX4Încă nu există evaluări
- Clinical Pediatric EvaluationDocument2 paginiClinical Pediatric EvaluationColeen VergaraÎncă nu există evaluări
- Medical Boards Step 2 Made Ridiculously Simple (Medicalstudyzone - Com)Document377 paginiMedical Boards Step 2 Made Ridiculously Simple (Medicalstudyzone - Com)Benyamin KhalevÎncă nu există evaluări
- Aortic StenosisDocument20 paginiAortic Stenosisvasarhely imolaÎncă nu există evaluări
- Beta BlockersDocument70 paginiBeta BlockersIrina Cabac-PogoreviciÎncă nu există evaluări
- Immunopharmacology: Dr. Hamad AlshabiDocument8 paginiImmunopharmacology: Dr. Hamad AlshabiHamad Alshabi100% (1)
- Arrhythmia Diagnosis and ManagementDocument44 paginiArrhythmia Diagnosis and ManagementanwarÎncă nu există evaluări
- Preventive CardiologyDocument28 paginiPreventive CardiologyerizonÎncă nu există evaluări
- Abdominal Swelling + AscitesDocument29 paginiAbdominal Swelling + AscitesDevina CiayadiÎncă nu există evaluări
- DM AAFP ManagementDocument8 paginiDM AAFP ManagementphilsguÎncă nu există evaluări
- Common MedicationsDocument4 paginiCommon MedicationsFatima CarricoÎncă nu există evaluări
- Treatment of Resistant and Refractory HypertensionDocument21 paginiTreatment of Resistant and Refractory HypertensionLuis Rodriguez100% (1)
- PericarditisDocument29 paginiPericarditisPavin KumarÎncă nu există evaluări
- VALVULAR HEART DISEASE GUIDEDocument69 paginiVALVULAR HEART DISEASE GUIDEAbanoub AwadallaÎncă nu există evaluări
- History Taking and Physical Examination of Cardiovascular System-The EssentialsDocument72 paginiHistory Taking and Physical Examination of Cardiovascular System-The EssentialsReena Joanella TimbreÎncă nu există evaluări
- UntitledDocument219 paginiUntitledSagit Nauman81Încă nu există evaluări
- Heartbeat Irregularities ExplainedDocument5 paginiHeartbeat Irregularities ExplainedKayelyn-Rose Combate100% (1)
- Core Topics in Internal MedicineDocument4 paginiCore Topics in Internal MedicineKristina Anne CoÎncă nu există evaluări
- CARDIOVASCULAR DISEASES: SIGNS, SYMPTOMS AND TREATMENT OF HEART FAILUREDocument27 paginiCARDIOVASCULAR DISEASES: SIGNS, SYMPTOMS AND TREATMENT OF HEART FAILURESanthoshi Sadhanaa SankarÎncă nu există evaluări
- Approach To Arrythmia RecognitionDocument64 paginiApproach To Arrythmia RecognitionSumiJoseÎncă nu există evaluări
- Common Bacteria by Site of Infection: Mouth Skin/Soft Tissue Bone and JointDocument72 paginiCommon Bacteria by Site of Infection: Mouth Skin/Soft Tissue Bone and JointMuthia FadhilaÎncă nu există evaluări
- CHAPTER 27 - Heart Failure With A Preserved Ejection FractionDocument15 paginiCHAPTER 27 - Heart Failure With A Preserved Ejection FractionReda SoÎncă nu există evaluări
- Chart Stimulated Recall SlidesDocument40 paginiChart Stimulated Recall Slidesnpr00Încă nu există evaluări
- Rokh 2e ST4 PDFDocument141 paginiRokh 2e ST4 PDFMahmud DipuÎncă nu există evaluări
- SurgeryDocument12 paginiSurgeryManusheeÎncă nu există evaluări
- Vital Signs Reference Chart - 1Document1 paginăVital Signs Reference Chart - 1l10n_assÎncă nu există evaluări
- ASCITESDocument25 paginiASCITESGanesh BabuÎncă nu există evaluări
- SchistosomiasisDocument6 paginiSchistosomiasisLyra LorcaÎncă nu există evaluări
- Registration For Internshala 2022-23 (Responses)Document26 paginiRegistration For Internshala 2022-23 (Responses)Abhisek ChatterjeeÎncă nu există evaluări
- Home-Made Hydraulic Ram PumpDocument87 paginiHome-Made Hydraulic Ram PumpZwq92y100% (3)
- BU StatuteDocument95 paginiBU StatuteAbhisek ChatterjeeÎncă nu există evaluări
- PharmacologyDocument23 paginiPharmacologyAbhisek ChatterjeeÎncă nu există evaluări
- Anchor NotesDocument3 paginiAnchor NotesAbhisek ChatterjeeÎncă nu există evaluări
- DAMS CRS - Obstetrics & Gynaecology (DAMS Comprehensive Review Series) - DAMSDocument46 paginiDAMS CRS - Obstetrics & Gynaecology (DAMS Comprehensive Review Series) - DAMSAbhisek ChatterjeeÎncă nu există evaluări
- DAMS CRS - Microbiology (DAMS Comprehensive Review Series) - DAMSDocument731 paginiDAMS CRS - Microbiology (DAMS Comprehensive Review Series) - DAMSAbhisek ChatterjeeÎncă nu există evaluări
- Fi - Exam Time Table Feb. 2022 Nur - VIIDocument2 paginiFi - Exam Time Table Feb. 2022 Nur - VIIAbhisek ChatterjeeÎncă nu există evaluări
- DAMS CRS - Preventive and Social Medicine (DAMS Comprehensive Review Series) - DAMSDocument1.483 paginiDAMS CRS - Preventive and Social Medicine (DAMS Comprehensive Review Series) - DAMSAbhisek ChatterjeeÎncă nu există evaluări
- Prospectus 2016-17 Final EditionDocument28 paginiProspectus 2016-17 Final EditionAbhisek ChatterjeeÎncă nu există evaluări
- Dams Crs - Psychiatry - DamsDocument250 paginiDams Crs - Psychiatry - DamsAbhisek Chatterjee100% (1)
- DAMS CRS - Obstetrics & Gynaecology (DAMS Comprehensive Review Series) - DAMSDocument36 paginiDAMS CRS - Obstetrics & Gynaecology (DAMS Comprehensive Review Series) - DAMSAbhisek ChatterjeeÎncă nu există evaluări
- ENDOCRINE PRACTICE Vol 21 No. 4 April 2015: Writing Committee CochairpersonsDocument72 paginiENDOCRINE PRACTICE Vol 21 No. 4 April 2015: Writing Committee CochairpersonsAbhisek ChatterjeeÎncă nu există evaluări
- ENDOCRINE PRACTICE Vol 21 No. 4 April 2015: Writing Committee CochairpersonsDocument72 paginiENDOCRINE PRACTICE Vol 21 No. 4 April 2015: Writing Committee CochairpersonsAbhisek ChatterjeeÎncă nu există evaluări
- Letter of RequestDocument1 paginăLetter of RequestJoniele Angelo AninÎncă nu există evaluări
- ECG AnalysisDocument158 paginiECG AnalysisAbhisek Chatterjee100% (1)
- Snakes in IndiaDocument30 paginiSnakes in IndiaAbhisek ChatterjeeÎncă nu există evaluări
- Pneumonia and Respirator... Ections in ChildrenDocument2 paginiPneumonia and Respirator... Ections in ChildrenAbhisek ChatterjeeÎncă nu există evaluări
- Jane AustenDocument6 paginiJane AustenAbhisek ChatterjeeÎncă nu există evaluări
- 1 ArteriesDocument12 pagini1 ArteriesAbhisek ChatterjeeÎncă nu există evaluări
- DNB Cet ReviewDocument96 paginiDNB Cet ReviewAbhisek ChatterjeeÎncă nu există evaluări
- Sequence TransformationDocument2 paginiSequence Transformationbrown222Încă nu există evaluări
- Booklet English 2016Document17 paginiBooklet English 2016Noranita ZakariaÎncă nu există evaluări
- MechanismDocument17 paginiMechanismm_er100Încă nu există evaluări
- Law of The Limiting FactorsDocument4 paginiLaw of The Limiting FactorsBiswajit DarbarÎncă nu există evaluări
- Academic Language Use in Academic WritingDocument15 paginiAcademic Language Use in Academic WritingDir Kim FelicianoÎncă nu există evaluări
- 1.9 Bernoulli's Equation: GZ V P GZ V PDocument1 pagină1.9 Bernoulli's Equation: GZ V P GZ V PTruong NguyenÎncă nu există evaluări
- NotesTransl 108 (1985) Larsen, Who Is This GenerationDocument20 paginiNotesTransl 108 (1985) Larsen, Who Is This GenerationluzuÎncă nu există evaluări
- Mapúa Welding Shop PracticeDocument7 paginiMapúa Welding Shop PracticeJay EmÎncă nu există evaluări
- Eco 301 Final Exam ReviewDocument14 paginiEco 301 Final Exam ReviewCảnh DươngÎncă nu există evaluări
- Epidemiological Cutoff Values For Antifungal Susceptibility TestingDocument36 paginiEpidemiological Cutoff Values For Antifungal Susceptibility Testingdadrrui100% (1)
- Strategicmanagement Finalpaper 2ndtrisem 1819Document25 paginiStrategicmanagement Finalpaper 2ndtrisem 1819Alyanna Parafina Uy100% (1)
- ALT Company Introduction 20170524.1Document51 paginiALT Company Introduction 20170524.1Terence WoonÎncă nu există evaluări
- Chapter 1-The Indian Contract Act, 1872, Unit 1-Nature of ContractsDocument10 paginiChapter 1-The Indian Contract Act, 1872, Unit 1-Nature of ContractsALANKRIT TRIPATHIÎncă nu există evaluări
- Rigor Mortis and Lividity in Estimating Time of DeathDocument2 paginiRigor Mortis and Lividity in Estimating Time of DeathfunnyrokstarÎncă nu există evaluări
- Course Introduction: Collection and Presentation of Data The Frequency Distribution Graphical Presentation of DataDocument61 paginiCourse Introduction: Collection and Presentation of Data The Frequency Distribution Graphical Presentation of DataShekinah Vingno LingcongÎncă nu există evaluări
- Thesis PromptsDocument7 paginiThesis Promptsauroratuckernewyork100% (2)
- ATB Farmacología 2Document194 paginiATB Farmacología 2Ligia CappuzzelloÎncă nu există evaluări
- Radiant Tube BurnersDocument18 paginiRadiant Tube BurnersRajeshÎncă nu există evaluări
- 1st ClassDocument18 pagini1st Classchitl.23bi14075Încă nu există evaluări
- Datasheet AD549Document14 paginiDatasheet AD549Trần Hồng VănÎncă nu există evaluări
- Learn R For Applied StatisticsDocument457 paginiLearn R For Applied StatisticsyasortyÎncă nu există evaluări
- 74VHCU04Document6 pagini74VHCU04Alexandre S. CorrêaÎncă nu există evaluări
- Pyrolysis ProjectDocument122 paginiPyrolysis ProjectSohel Bangi100% (1)
- Flow Through Pipes: Departmentofcivilengineering Presidency University, Bangalore-64 BY Santhosh M B Asstistant ProfessorDocument15 paginiFlow Through Pipes: Departmentofcivilengineering Presidency University, Bangalore-64 BY Santhosh M B Asstistant ProfessorSanthoshMBSanthuÎncă nu există evaluări
- Din en 912-2001Document37 paginiDin en 912-2001Armenak BaghdasaryanÎncă nu există evaluări
- Caribbean Studies - Lesson 8 - Concept and Indicator of Development PDFDocument37 paginiCaribbean Studies - Lesson 8 - Concept and Indicator of Development PDFDarrion BruceÎncă nu există evaluări
- Advisory Circular: Aircraft Maintenance Engineer Licence - Examination Subject 2 Aircraft Engineering KnowledgeDocument44 paginiAdvisory Circular: Aircraft Maintenance Engineer Licence - Examination Subject 2 Aircraft Engineering KnowledgejashkahhÎncă nu există evaluări
- HOW To Use Jmeter To Load Test T24Document27 paginiHOW To Use Jmeter To Load Test T24Hiếu KoolÎncă nu există evaluări
- 4439 Chap01Document28 pagini4439 Chap01bouthaina otÎncă nu există evaluări
- Douglas Frayne Sargonic and Gutian Periods, 2334-2113 BCDocument182 paginiDouglas Frayne Sargonic and Gutian Periods, 2334-2113 BClibrary364100% (3)