Documente Academic
Documente Profesional
Documente Cultură
Oligohydramnios
Încărcat de
salamredDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Oligohydramnios
Încărcat de
salamredDrepturi de autor:
Formate disponibile
Oligohydramnios
Nancy Chescheir MD
Basics
Description
Oligohydramnios (oligo) refers to pathologically low volumes of AF.
Age-Related Factors
Not uniquely related to maternal age
Rare in 1st trimester
Epidemiology
The incidence of oligohydramnios ranges from 0.55% or more, depending on the
patient population, high risk factors, and GA.
Risk Factors
Vascular compromise
PROM
Medication use:
o
ACE inhibitors
NSAIDs
Pathophysiology
Abnormal production of AF:
o Poor placental perfusion in response to decreased intravascular volume
or BP, fetus preferentially perfuses vital organs, decreases GFR,
reduces urine production (prerenal)
Abnormal fetal renal function: Any problem that prevents bilateral
renal function or causes complete lower urinary tract obstruction
(postrenal)
Renal toxicity (ACE inhibitors, NSAIDs) nephrosis; (renal)
Loss of fluid:
o
PROM
Prolonged early severe oligo can results in pulmonary hypoplasia, facial and
limb abnormalities.
Cord compression with severe oligo
Associated Conditions
HTN
Severe diabetes
Lupus
Smoking
Unexplained MSAFP elevation
IUGR
Post-dates pregnancy
Placental abnormality:
Chronic abruption
Infarction
Circumvallate
Fetal abnormality:
o
Bilateral renal disease:
Agenesis, multicystic dysplastic kidneys
Lower urinary tract obstruction
Posterior urethral valves
Diagnosis
Signs and Symptoms
History
Typically not helpful
Physical Exam
Size < dates by 3 cm in normal-sized woman
Tests
Imaging
US required to make diagnosis:
Fetal crowding
MVP <1 cm is strictest definition
AFI <5 cm
With subjective oligohydramnios, use color Doppler to confirm that fluid
pocket isn't really loop of cord
Search for anomalies.
May require amnioinfusion to see well
Blue tap with indigo carmine if PROM is suspected but unconfirmed.
Doppler may be useful; color confirms renal artery presence; umbilical artery
assessment if IUGR
Treatment
General Measures
Weigh risks of continuing pregnancy vs. neonatal morbidity and mortality
risks and consider delivery.
Efforts to improve perfusion:
Avoid smoking, ACE inhibitors, NSAIDs
Decrease maternal stress
Complete bed rest not likely helpful, but avoid aerobic exercise.
PROM therapy with latency antibiotics if appropriate
Maternal fluid hydration not useful except for severe maternal dehydration
Pregnancy-Specific Issues
Make as complete a diagnosis as possible.
By Trimester
With absent fetal renal function or urine output, oligohydramnios occurs after
~16 weeks.
With known risk factors, actively assess AF volume at intervals after
intervention is considered.
Risks for Mother
Increased risk for cesarean delivery
Risks for Fetus
Related primarily to etiology, duration
Cord compression with IUFD, possible CNS injury possible
P.411
Medication (Drugs)
Steroids if anticipate preterm birth
Followup
Disposition
Issues for Referral
Perinatal consultation if known or suspected fetal anomaly, severe IUGR, severe
maternal vascular disease
Prognosis
Related to underlying cause, duration, and severity of oligohydramnios
Patient Monitoring
Fetus
If potentially viable fetus, consider fetal monitoring:
o Cord compressions: Variable decelerations
o
Placental insufficiency: Late decelerations, loss of variability
Consider amnioinfusion in labor
Prepare for pulmonary hypoplasia if severe oligohydramnios from 20 weeks or
so.
Miscellaneous
Clinical Pearls
Oligohydramnios is a sign of another problemfind the problem.
Send the placenta to pathology lab if etiology not known.
High index of suspicion for IUGR, placental insufficiency
Abbreviations
ACEAngiotensin-converting enzyme
AFAmniotic fluid
AFIAmniotic fluid index
GAGestational age
GFRGlomerular filtration rate
IUGRIntrauterine growth restriction
MSAFPMaternal serum -fetoprotein
MVPMaximal vertical pocket
PROMPremature rupture of membranes
Codes
ICD9-CM
658.0 Oligohydramnios
761.2 Oligohydramnios affecting fetus or newborn.
Patient Teaching
Stop smoking
Perform fetal kick counts
Details related to underlying diagnosis if known
Limitations of US: Not a good predictor of pulmonary hypoplasia
Cord accidents can be sudden, unpredictable, lethal
S-ar putea să vă placă și
- Polyhydraminos and OligohydraminosDocument11 paginiPolyhydraminos and OligohydraminosMelissa Catherine ChinÎncă nu există evaluări
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDe la EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsÎncă nu există evaluări
- Multiple PregnancyDocument20 paginiMultiple PregnancyNurul Fahmiza TumiranÎncă nu există evaluări
- DEFINITION: Abortion Is The Expulsion or Extraction From Its MotherDocument10 paginiDEFINITION: Abortion Is The Expulsion or Extraction From Its MothermOHAN.SÎncă nu există evaluări
- OB GDM CasepresDocument102 paginiOB GDM Casepreskitten garciaÎncă nu există evaluări
- Hypoxic Ischemic EncephalopathyDocument7 paginiHypoxic Ischemic EncephalopathyJennesse May Guiao IbayÎncă nu există evaluări
- Intrauterine Growth Restriction IUGR: TH THDocument2 paginiIntrauterine Growth Restriction IUGR: TH THZahra AlaradiÎncă nu există evaluări
- Obgyn Anemia in Pregnancy For UG ClassDocument35 paginiObgyn Anemia in Pregnancy For UG ClassimranÎncă nu există evaluări
- 68 Abnormal PeuperiumDocument44 pagini68 Abnormal PeuperiumGodsonYeboah-AwudziÎncă nu există evaluări
- Ectopic Pregnancy - OMDocument9 paginiEctopic Pregnancy - OMrheindÎncă nu există evaluări
- Ectopic Pregnancy: DR .Urmila KarkiDocument27 paginiEctopic Pregnancy: DR .Urmila KarkiBasudev chÎncă nu există evaluări
- Post Abortion CareDocument35 paginiPost Abortion CareNatukunda DianahÎncă nu există evaluări
- Ectopic PregnancyDocument26 paginiEctopic PregnancysandhyakrishnanÎncă nu există evaluări
- CPD, Dystocia, Fetal Distress OutputDocument8 paginiCPD, Dystocia, Fetal Distress OutputJohn Dave AbranÎncă nu există evaluări
- Case PresentationDocument36 paginiCase PresentationSaba TariqÎncă nu există evaluări
- Definition of Placenta PreviaDocument3 paginiDefinition of Placenta Previashan6ersÎncă nu există evaluări
- Harika Priyanka. K Asst. Professor AconDocument30 paginiHarika Priyanka. K Asst. Professor AconArchana MoreyÎncă nu există evaluări
- EclampsiaDocument47 paginiEclampsiarranindyaprabasaryÎncă nu există evaluări
- Ectopic PregnancyDocument11 paginiEctopic PregnancyPrincess BalloÎncă nu există evaluări
- Amniotic Fluid Embolism (AFE)Document26 paginiAmniotic Fluid Embolism (AFE)sanjivdas100% (1)
- Abortion: DEFINITION-Abortion Is The Separation Partial orDocument77 paginiAbortion: DEFINITION-Abortion Is The Separation Partial orPadmaÎncă nu există evaluări
- 5 Asphyxia NeonetrumDocument27 pagini5 Asphyxia NeonetrumRana VandanaÎncă nu există evaluări
- Breech PresentationDocument85 paginiBreech Presentationwidya vannesaÎncă nu există evaluări
- 22 Cephalo-Pelvic DisproportionDocument32 pagini22 Cephalo-Pelvic DisproportionNirupama KsÎncă nu există evaluări
- Complications of 3 Stage of LabourDocument17 paginiComplications of 3 Stage of LabourshravaniÎncă nu există evaluări
- Uterine ProlapseDocument11 paginiUterine ProlapseMelDred Cajes BolandoÎncă nu există evaluări
- NCM - Pregancy Induced HypertensionDocument5 paginiNCM - Pregancy Induced HypertensionZam PamateÎncă nu există evaluări
- CPDDocument14 paginiCPDmaezuÎncă nu există evaluări
- Ectopic PregnancyDocument26 paginiEctopic PregnancyDavid SitinjakÎncă nu există evaluări
- Endometriosis PresentationDocument58 paginiEndometriosis PresentationBRI KUÎncă nu există evaluări
- Pregnancy Induced Hypertension (Pih)Document56 paginiPregnancy Induced Hypertension (Pih)shandi23100% (5)
- Sample Obg Case SheetDocument10 paginiSample Obg Case SheetKamil AlchalisÎncă nu există evaluări
- IUFDDocument2 paginiIUFDnurseon0% (1)
- Case Study Missed Miscarriage Dilation and CurettageDocument48 paginiCase Study Missed Miscarriage Dilation and CurettageEsther Ellise AbundoÎncă nu există evaluări
- CLINICAL PRESENTATION ON IugrDocument24 paginiCLINICAL PRESENTATION ON Iugrsaleha sultanaÎncă nu există evaluări
- Cord Presentation ProlapseDocument10 paginiCord Presentation ProlapseJHONESSA LAYOSÎncă nu există evaluări
- Case StudyDocument7 paginiCase Studymark kennethÎncă nu există evaluări
- Multifetal Pregnancy: Amr Nadim, MDDocument36 paginiMultifetal Pregnancy: Amr Nadim, MDsharenÎncă nu există evaluări
- Pregnancy Induced HypertensionDocument52 paginiPregnancy Induced HypertensionJoy GloryÎncă nu există evaluări
- Pyloric StenosisDocument5 paginiPyloric Stenosisensoooooooooo100% (1)
- Threatened AbortionDocument1 paginăThreatened AbortionKEn PilapilÎncă nu există evaluări
- Abnormalities of Amniotic Fluid: Presented by Ms. K.D. Sharon Final Year MSC (N) Obstetrics and Gynaecology NursingDocument32 paginiAbnormalities of Amniotic Fluid: Presented by Ms. K.D. Sharon Final Year MSC (N) Obstetrics and Gynaecology Nursingkalla sharonÎncă nu există evaluări
- Placenta PreviaDocument11 paginiPlacenta PreviaHomerÎncă nu există evaluări
- Complications of The Third Stage of LabourDocument6 paginiComplications of The Third Stage of LabourSong QianÎncă nu există evaluări
- Incomplete Abortion: A Mini Case Study OnDocument22 paginiIncomplete Abortion: A Mini Case Study OnSunny MujmuleÎncă nu există evaluări
- Pregnancy Induced HypertensionDocument3 paginiPregnancy Induced HypertensionunagraciaÎncă nu există evaluări
- EpisiotomyDocument18 paginiEpisiotomyAnnapurna DangetiÎncă nu există evaluări
- Post Partum HemorrhageDocument40 paginiPost Partum HemorrhageGita GirsangÎncă nu există evaluări
- Preterm LabourDocument18 paginiPreterm LabourRutu RajÎncă nu există evaluări
- Pregnancy Induced Hypertension: DefinitionDocument7 paginiPregnancy Induced Hypertension: Definitionkristine hinaresÎncă nu există evaluări
- OBG DrugsDocument30 paginiOBG DrugsSANAÎncă nu există evaluări
- Puerperal SepsisDocument4 paginiPuerperal SepsisSonali NayakÎncă nu există evaluări
- Shoulder DystociaDocument22 paginiShoulder Dystociaamulan_aÎncă nu există evaluări
- Govt College of Nursig Mbs Hospital, Kota: A Case Study On EclampsiaDocument21 paginiGovt College of Nursig Mbs Hospital, Kota: A Case Study On EclampsiaShalabh JoharyÎncă nu există evaluări
- Poly and OligohydramniosDocument39 paginiPoly and OligohydramniosMohamed Atef MohamedÎncă nu există evaluări
- Hypertensive Disorder in PregnancyDocument56 paginiHypertensive Disorder in PregnancyESCA GabrielÎncă nu există evaluări
- Normal Labor: Ms. Mayuri Patel Sandra Shroff Rofel College of Nursing, VapiDocument48 paginiNormal Labor: Ms. Mayuri Patel Sandra Shroff Rofel College of Nursing, Vapivimmy47100% (1)
- Antepartum HaemorrhageDocument18 paginiAntepartum HaemorrhageOjambo Flavia100% (1)
- Anemia in PregnancyDocument79 paginiAnemia in Pregnancypat duaÎncă nu există evaluări
- MCQ On MenopauseDocument4 paginiMCQ On Menopausesalamred100% (3)
- ةعومجم نم لا Reports ةيطغم جهنملا ءاشنا لا مكبجعت: Report of toxicologyDocument14 paginiةعومجم نم لا Reports ةيطغم جهنملا ءاشنا لا مكبجعت: Report of toxicologysalamredÎncă nu există evaluări
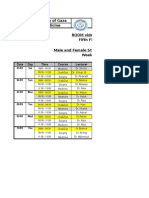
- Islamic University of Gaza Faculty of Medicine ROOM Video Conf. Fifth Floor Male and Female Students - 6th Year Week 1Document2 paginiIslamic University of Gaza Faculty of Medicine ROOM Video Conf. Fifth Floor Male and Female Students - 6th Year Week 1salamredÎncă nu există evaluări
- Ortho OSCE 2008Document3 paginiOrtho OSCE 2008salamredÎncă nu există evaluări
- MCQ Psy Exam Group BDocument17 paginiMCQ Psy Exam Group BsalamredÎncă nu există evaluări
- RadiologyDocument5 paginiRadiologysalamredÎncă nu există evaluări
- MCQs Psy Exam44 First GroupDocument7 paginiMCQs Psy Exam44 First Groupsalamred100% (3)
- SurgeryDocument10 paginiSurgeryIbrahem Y. NajjarÎncă nu există evaluări
- Longitudinal Esophagotomy (Hellers) 4 Frey"s Syndrome: Sever InfectionDocument4 paginiLongitudinal Esophagotomy (Hellers) 4 Frey"s Syndrome: Sever InfectionsalamredÎncă nu există evaluări
- MCQDocument11 paginiMCQsalamredÎncă nu există evaluări
- Choose The Best Appropriate Answerfor Each of The Following QuestionsDocument12 paginiChoose The Best Appropriate Answerfor Each of The Following QuestionssalamredÎncă nu există evaluări
- A) Basic Surgical SciencesDocument27 paginiA) Basic Surgical SciencessalamredÎncă nu există evaluări
- Dr:-Ashraf .I. ObaidDocument22 paginiDr:-Ashraf .I. ObaidsalamredÎncă nu există evaluări
- اسبيرو طويل مهم جدا الثلاثاءDocument22 paginiاسبيرو طويل مهم جدا الثلاثاءsalamredÎncă nu există evaluări
- Systemic Lupus Erythematosus (Sle) : Presented By: Dr. Walaa MousaDocument13 paginiSystemic Lupus Erythematosus (Sle) : Presented By: Dr. Walaa MousasalamredÎncă nu există evaluări
- Forceps Delivery and Vacuum ExtractionDocument8 paginiForceps Delivery and Vacuum ExtractionsalamredÎncă nu există evaluări
- Vulvovaginal CandidiasisDocument5 paginiVulvovaginal CandidiasissalamredÎncă nu există evaluări
- Drug AbuseDocument38 paginiDrug AbuseARIF-UR-REHMAN100% (4)
- Lymphoid Leukemia in DogsDocument15 paginiLymphoid Leukemia in Dogstaner_soysurenÎncă nu există evaluări
- Topical Steroids DermatologyDocument23 paginiTopical Steroids DermatologyRitika Agarwal100% (1)
- 1 - Introduction of CytopathologyDocument41 pagini1 - Introduction of CytopathologyAyu Rizky Fitriawan AyuÎncă nu există evaluări
- Out of Stock Items List - Till Last Week.27 JunDocument65 paginiOut of Stock Items List - Till Last Week.27 Junmanuella AÎncă nu există evaluări
- Chakra-Chart Deborah KingDocument2 paginiChakra-Chart Deborah KingLaura Dafina Drãguț100% (2)
- 616062692662Document34 pagini616062692662ABHISHEK YADAVÎncă nu există evaluări
- Theory Application 4.2.10Document80 paginiTheory Application 4.2.10shoba088083% (6)
- CHAMPP Part 1 20130104 NewDocument240 paginiCHAMPP Part 1 20130104 NewMarcu QuerubinÎncă nu există evaluări
- LaQshya Quality Improvement Cycles Resource MaterialDocument344 paginiLaQshya Quality Improvement Cycles Resource Materialkparasher100% (1)
- Surgical Scrubbing Workbook 2020Document19 paginiSurgical Scrubbing Workbook 2020Alistair LauÎncă nu există evaluări
- ProRoot MTA BrochureDocument12 paginiProRoot MTA BrochureAdela FechetaÎncă nu există evaluări
- Unit 1 Chap 1 and 2Document7 paginiUnit 1 Chap 1 and 2Ariane Grace OcampoÎncă nu există evaluări
- Great Critical Care ReliefDocument9 paginiGreat Critical Care ReliefBenedict FongÎncă nu există evaluări
- A Case Study On MalariaDocument10 paginiA Case Study On MalariaAnant KumarÎncă nu există evaluări
- Engel 1980 The Clinical Application of of The Biopsychosocial Model PDFDocument10 paginiEngel 1980 The Clinical Application of of The Biopsychosocial Model PDFDiego Almanza HolguinÎncă nu există evaluări
- Comprehensive Examination 1Document53 paginiComprehensive Examination 1Love Gonzales90% (21)
- Renal Trauma: Schwartz Principle of Surgery 10Th EditionDocument31 paginiRenal Trauma: Schwartz Principle of Surgery 10Th EditionMustika RanyÎncă nu există evaluări
- Juvenile Idiopathic Arthritis in A Premature Baby: Rare Case ReportDocument3 paginiJuvenile Idiopathic Arthritis in A Premature Baby: Rare Case ReportKevin Wladimir ChanchicochaÎncă nu există evaluări
- Fped 2019 00227Document7 paginiFped 2019 00227Syaifudin LutfiÎncă nu există evaluări
- PlagueDocument31 paginiPlaguelulondon1Încă nu există evaluări
- AgonistsDocument25 paginiAgonistsOfficially RandomÎncă nu există evaluări
- Characteristics of Healthcare ProviderDocument2 paginiCharacteristics of Healthcare ProviderFlora Arcenal100% (1)
- Pharmacoeconomics - Part IIIDocument29 paginiPharmacoeconomics - Part IIISima JabbariÎncă nu există evaluări
- Gonorrhea Case Study 2009Document4 paginiGonorrhea Case Study 2009Garrett Batang100% (3)
- Vitreous Hemorrhage: Retina Eye Specialists Retina Eye SpecialistsDocument2 paginiVitreous Hemorrhage: Retina Eye Specialists Retina Eye SpecialistsMarcel Antek CivilÎncă nu există evaluări
- Quantum Techniques Client ManualDocument42 paginiQuantum Techniques Client ManualVeres Beatrix100% (4)
- PaediatricTuina Elisa RossiDocument7 paginiPaediatricTuina Elisa Rossideemoney3100% (1)
- Case Analysis 13 - Hirschsprungs DiseaseDocument5 paginiCase Analysis 13 - Hirschsprungs DiseaseAHOUR PANGILAYANÎncă nu există evaluări
- Keith R Poskitt - Chronic Ulceration of The LegDocument5 paginiKeith R Poskitt - Chronic Ulceration of The LegKovoor LedchumananÎncă nu există evaluări
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDe la EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsÎncă nu există evaluări
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDe la EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDEvaluare: 5 din 5 stele5/5 (3)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDe la EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionEvaluare: 4 din 5 stele4/5 (404)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDe la EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityEvaluare: 4 din 5 stele4/5 (32)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDe la EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeEvaluare: 2 din 5 stele2/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDe la EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)De la EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Evaluare: 3 din 5 stele3/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDe la EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedEvaluare: 4.5 din 5 stele4.5/5 (82)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDe la EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsEvaluare: 4 din 5 stele4/5 (4)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDe la EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisEvaluare: 4.5 din 5 stele4.5/5 (42)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDe la EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsEvaluare: 5 din 5 stele5/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossDe la EverandThe Obesity Code: Unlocking the Secrets of Weight LossEvaluare: 4 din 5 stele4/5 (6)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesDe la EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesEvaluare: 4.5 din 5 stele4.5/5 (1412)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDe la EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeEvaluare: 4.5 din 5 stele4.5/5 (254)
- The Marshmallow Test: Mastering Self-ControlDe la EverandThe Marshmallow Test: Mastering Self-ControlEvaluare: 4.5 din 5 stele4.5/5 (60)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisDe la EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisEvaluare: 5 din 5 stele5/5 (8)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.De la EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Evaluare: 4.5 din 5 stele4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDe la EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityEvaluare: 4.5 din 5 stele4.5/5 (6)
- To Explain the World: The Discovery of Modern ScienceDe la EverandTo Explain the World: The Discovery of Modern ScienceEvaluare: 3.5 din 5 stele3.5/5 (51)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedDe la EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedEvaluare: 4 din 5 stele4/5 (61)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDe la EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisEvaluare: 3.5 din 5 stele3.5/5 (2)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDe la EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryEvaluare: 4 din 5 stele4/5 (46)