Documente Academic
Documente Profesional
Documente Cultură
Acute Pain Management
Încărcat de
Anonymous SQNcItqXQnDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Acute Pain Management
Încărcat de
Anonymous SQNcItqXQnDrepturi de autor:
Formate disponibile
Print: Section 3.
Analgesia, Anesthesia, and Sedation
Page 1 of 9
Print | Close Window
Note: Large images and tables on this page may necessitate printing in landscape mode.
|
Emergency Medicine Manual, 6th Edition > Section 3. Analgesia, Anesthesia, and Sedation >
INTRODUCTION
Acute pain is present in 50% to 60% of all emergency department (ED) patients. Factors that
may contribute to the underuse of sedation and analgesia in the ED include communication
barriers between patient and physician, lack of knowledge about sedative and analgesic agents,
and fear of adverse events. Procedural sedation and analgesia (PSA) often is needed for painful
interventions or diagnostic studies.
CLINICAL FEATURES
Physiologic responses to pain and anxiety include increased heart rate, blood pressure, and
respiratory rate. Behavioral changes include facial expressions, posturing, crying, and
vocalization. Because subjective impressions may be inaccurate, pain is best assessed with
objective scales. Pain relief is a dynamic process, and reassessment is mandatory.
EMERGENCY DEPARTMENT CARE AND DISPOSITION
Pharmacologic and nonpharmacologic interventions may be helpful for treating anxiety and pain in
the ED.
Nonpharmacologic interventions:
May be used alone or adjunctively.
Include:
the application of heat or cold
immobilization and elevation of injured extremities
explanation and reassurance
music
biofeedback
guided imagery
distraction.
Communication with the patient in pain should be gentle, unhurried, and appropriate for the
developmental stage of the patient.
Discussing a painful intervention with a pediatric patient immediately before the procedure may
decrease the anxiety created by anticipation.
Parents should be included in pediatric interventions to help alleviate anxiety.
If physical restraint is required for a child, the parents should not be responsible for restraining
their child.
When pharmacologic intervention is needed, the selection of agent should be guided by:
need for sedation or analgesia
route of delivery
desired duration of effects.
Systemic Analgesia and Sedation
GENERAL
Indications for PSA include:
abscess drainage
wound management
mk:@MSITStore:E:\EMERGENCY%20MEDICINE\EMERGENCY%20MEDICINE... 31/03/2014
Print: Section 3. Analgesia, Anesthesia, and Sedation
Page 2 of 9
tube thoracostomy
orthopedic manipulation
cardioversion
diagnostic studies.
Analgesia is relief from the perception of pain.
Minimal sedation is a drug-induced state characterized by normal responses to voice and normal
cardiac and ventilatory functions.
Moderate sedation and analgesia (conscious sedation) are characterized by responsiveness to
voice or light tactile stimulation with normal cardiac and ventilatory functions.
Deep sedation and analgesia are characterized by responsiveness to repeated or painful
stimulation, potentially inadequate ventilation, and potential loss of protective reflexes.
PREPARATION
When PSA is performed, necessary equipment includes:
a continuous cardiac monitor and pulse oximetry
oxygen
suction
immediate availability of appropriate-size resuscitation equipment.
The patient should be under constant observation by a provider trained in airway management.
Informed consent should be obtained.
BP, heart rate, respiratory rate, and level of consciousness should be assessed at baseline and
every 510 mins.
The analgesic or sedative agents chosen should be individualized to the patient and the planned
procedure.
The agents used for PSA often have a narrow therapeutic index.
Therefore, the agents should be administered in small, incremental IV doses, with adequate time
between doses to determine peak effect.
Other routes of administration may be appropriate (especially in children) but provide less ability
to titrate the dose to produce the desired effect.
All patients undergoing PSA should be reassessed continuously.
Patients experiencing transient respiratory depression frequently can be managed by bag-maskvalve ventilation; however, some patients will require intubation.
Reversal agents:
Pre-calculated doses should be available:
naloxone 0.1 mg/kg (up to 2 mg) q23 mins until the desired effect of reversing opiateinduced respiratory depression
flumazenil 0.01 0.02 mg/kg (up to 0.2 mg) q12 mins until the desired effect of reversing
benzodiazepine-induced respiratory depression.
Because the half-lives of naloxone and flumazenil may be shorter than those of the drugs they
reverse, patients who require reversal should be observed for a prolonged period to avoid rebound
respiratory depression.
Flumazenil should not be used in patients on chronic benzodiazepine or tricyclic antidepressant
therapy due to the risk of seizure.
Flumazenil is not recommended to routinely "wake up" patients from PSA.
NON-OPIATE ANALGESICS
Acetaminophen:
Anti-inflammatory and analgesic that can be used alone for mild pain or adjunctively with
opiates for moderate to severe pain.
15 mg/kg PO or PR q6 hrs
Dosing is not age dependent.
May be hepatotoxic > 140 mg/kg/day.
NSAIDs (aspirin, naproxen, indomethacin, ibuprofen, and ketorolac):
mk:@MSITStore:E:\EMERGENCY%20MEDICINE\EMERGENCY%20MEDICINE... 31/03/2014
Print: Section 3. Analgesia, Anesthesia, and Sedation
Page 3 of 9
Anti-inflammatory and analgesic agents with opiate-sparing effects.
Ketorolac (0.51 mg/kg IM or IV, up to 60 mg IM or 30 mg IV) is the only parenteral NSAID
available in the US.
Ibuprofen (10 mg/kg PO) is safe in children > 6 mos.
Adverse effects include:
renal dysfunction
platelet dysfunction
impaired coagulation
gastrointestinal irritation.
Aspirin should be avoided in children because of an association with Reye syndrome.
OPIATES
Opiates are the agents of choice for moderate to severe pain and for procedural analgesia.
Side effects of opiates include:
respiratory depression
nausea and vomiting
confusion
pruritus
urinary retention.
Opiates are relatively contraindicated in patients with:
hemodynamic instability
respiratory compromise
altered mental status.
Morphine:
Is a naturally occurring opiate.
Peak effect at 1530 mins and a duration of 2 to 4 hrs (Table 10-1).
Morphine releases histamine and therefore may cause hypotension.
Meperidine is a synthetic derivative of morphine whose use is no longer recommended in the ED
for multiple reasons, including increased risk of hypotension from histamine release, production of a
metabolite (normeperidine) with CNS toxicity, and potential for a fatal reaction when coadministered with MAOIs.
The Demerol, Phenergan, and Thorazine cocktail, previously used for pediatric PSA, is no longer
recommended because of its unreliable efficacy, the potential for respiratory depression, and a
variable duration of action that may last several hrs.
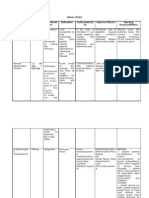
Table 10-1 Drugs Used for Procedural Sedation and Analgesia
Drug
Dose*
Peak
Effect
Morphine
0.050.1 mg/kg IV
1030 min 24 h
Releases histamine
Fentanyl
12 mcg/kg IV
2.510
min
3090 min
Does not release histamine
Midazolam
0.01 mg/kg IV
12 min
60 min
Respiratory depression
Propofol
0.2 mg/kg per min
infusion
67 min
510 min
Respiratory depression, deep
sedation
Etomidate
0.1 mg/kg IV
2030 s
23 min
Respiratory depression, deep
sedation
Ketamine
12 mg/kg IV
5 min
3060 min
Avoid with elevated intracranial
pressure
3060 s
10 min
Avoid in patients with seizure
disorders
Methohexital 1 mg/kg IV
Duration of
Effect
Notes
mk:@MSITStore:E:\EMERGENCY%20MEDICINE\EMERGENCY%20MEDICINE... 31/03/2014
Print: Section 3. Analgesia, Anesthesia, and Sedation
Page 4 of 9
*Incremental doses, given in small intravenous amounts, allow adequate time for the development and
assessment of peak effect.
Fentanyl:
Is a synthetic opiate.
Almost immediate onset of action and a 30- to 90-min duration (see Table 10-1).
Its rapid onset makes it the opiate of choice for most brief PSA procedures.
Fentanyl is less likely to cause respiratory depression and hypotension than are other opiates.
Respiratory depression may be more common in patients with alcohol or benzodiazepine
ingestion.
Administering fentanyl slowly over 35 mins can minimize respiratory depression.
Chest wall rigidity unresponsive to naloxone may occur at higher doses (515 mcg/kg),
potentially necessitating neuromuscular blockade and mechanical ventilation.
Adjunctive agents such as hydroxyzine (0.5 mg/kg PO or IM) or benzodiazepines frequently are
administered with opiates.
These agents may have opiate dose-sparing effects, although the data are scant.
Should be used only to relieve symptoms such as nausea or anxiety.
SEDATION
Benzodiazepines:
Are the most commonly used sedative agents for PSA in the ED.
Provide sedation, anxiolysis, amnesia, and anticonvulsant effects.
Side effects include cardiovascular and respiratory depression, especially when used in
combination with alcohol or opiates and in the elderly.
Midazolam:
5-min onset of effect and a 30- to 45-min duration of effect.
Most commonly used benzodiazepine for PSA (see Table 10-1).
The duration of effect may be increased substantially in obese patients, and children may
develop paradoxical inconsolability that is reversed by flumazenil.
Diazepam, a benzodiazepine with a duration of effect of 26 hrs, may be useful for longer
procedures.
Barbiturates:
Are sedative agents without analgesic or amnestic properties.
Side effects include:
laryngospasm
hypotension
respiratory depression
CNS depression (especially when administered with opiates or benzodiazepines).
Pentobarbital has a 30-sec onset of effect and a 30- to 60-min duration of effect when
administered IV.
Methohexital has a 30- to 60-sec onset of effect and a 10-min duration of effect when
administered IV (see Table 10-1).
Methohexital, which has been used PR in children, may precipitate seizures and should not be
used in patients with a seizure disorder.
Propofol:
Is an anesthetic agent with antiemetic properties administered by IV infusion (see Table 10-1).
Has an onset of effect of 510 mins and a duration of effect upon withdrawal of 510 mins.
Side effects include dose-related cardiovascular depression with decreases in systolic BP of 25
40%.
Because amnesia is not reliably produced in PSA doses of propofol, an adjunctive analgesic or
amnestic agent may be needed.
Etomidate:
mk:@MSITStore:E:\EMERGENCY%20MEDICINE\EMERGENCY%20MEDICINE... 31/03/2014
Print: Section 3. Analgesia, Anesthesia, and Sedation
Page 5 of 9
Has a 20- to 30-sec onset of effect and a 2- to 3-min duration of effect.
Is a sedative agent with minimal cardiovascular depression (see Table 10-1).
Side effects include:
nausea and vomiting
myoclonus
adrenal insufficiency (with long-term infusion).
Respiratory and CNS depressions may occur, especially when administered with opiates or
benzodiazepines.
Chloral hydrate:
Is a sedative agent that was used commonly in pediatric patients requiring painless diagnostic
procedures (dose 2575 mg/kg PO or PR).
Side effects include:
nausea and vomiting
paradoxical delirium
airway obstruction
death.
Because of its delayed onset of effect (4560 mins) and its prolonged duration (several hours),
it is no longer recommended for routine use in the ED.
Ketamine:
Is a dissociative analgesic with sedative and amnestic properties that causes minimal respiratory
depression (see Table 10-1).
May be administered IV, IM, PO, or PR.
Ketamine may cause:
increased intracranial and intraocular pressure
hypersalivation
bronchorrhea
bronchodilation
laryngospasm
a hallucinatory emergence reaction in older children and adults.
It is a direct myocardial depressant and vasodilator, although its CNS effects usually result in
mild tachycardia and vasoconstriction.
Atropine (0.01 mg/kg IV or IM) may be used adjunctively to control hypersalivation.
Midazolam (0.01 mg/kg IM or IV or 0.1 mg/kg PO) may attenuate the emergence reaction, but
it may cause respiratory depression and delayed ketamine metabolism.
Ketamine is contraindicated in:
children 3 mos and younger
those with airway abnormalities
history of CHF or hypertension
acute closed head or eye injury
altered mental status or psychosis
CNS mass
poorly controlled seizure disorder
glaucoma.
Nitrous oxide:
Is an inhaled agent with analgesic, sedative, and dissociative properties.
It can be used alone or in conjunction with local anesthetics.
Is delivered as a 3050% mixture with a min. of 30% O2.
It should be self-administered through a demand-valve apparatus with a scavenger device.
Has a 3- to 5-min onset of effect and a duration of effect on withdrawal of 35 mins.
Nitrous oxide has minimal respiratory or cardiovascular effects but may cause nausea and
vomiting.
mk:@MSITStore:E:\EMERGENCY%20MEDICINE\EMERGENCY%20MEDICINE... 31/03/2014
Print: Section 3. Analgesia, Anesthesia, and Sedation
Page 6 of 9
It is contraindicated in:
patients who have recently been sedated with another agent
those with altered mental status
balloon-tipped catheters
dyspnea
severe COPD
pneumothorax
eye injury
middle ear effusion
bowel obstruction.
DISPOSITION
Patients are eligible for discharge only when fully recovered.
When discharged, the patient must be accompanied by an adult and should not drive or operate
machinery for 24 hrs.
Because many of the agents used for PSA produce anterograde amnesia, discharge instructions
must be given to responsible accompanying adults.
Local and Regional Anesthesia
GENERAL
Local and regional anesthetics are essential tools for ED pain management.
Agents can be administered topically, by infiltration directly into the area to be anesthetized or into
the area of the peripheral nerves supplying the area to be anesthetized, and IV. This discussion
focuses on topical and infiltrative anesthesia.
There are two classes of local anesthetics (LAs), amides and esters.
Amides include prilocaine, lidocaine, bupivacaine, and mepivacaine.
Esters include procaine and tetracaine.
Toxicity of LAs:
Is related to the total dose and the rate of plasma concentration increase and is increased in the
setting of hypoxia, hypercarbia, and acidosis.
The rate of plasma concentration increase is dependent on the vascularity of the site being
infiltrated.
Therefore, the maximum dose of LAs that can be administered for intercostal block is one tenth
the SC dose.
Toxic effects include:
confusion
seizures
coma
myocardial depression
dysrhythmias.
Allergic reactions to LAs:
Are uncommon and usually due to a metabolite (in esters) or a preservative (in amides).
If an allergy is suspected, the best approach is to use a preservative-free agent from the other
class of LAs.
Alternatively, diphenhydramine or benzyl alcohol may be used as an LA in the setting of a true
allergy to conventional LAs.
LAs often cause pain during administration. Factors that may decrease the pain of infiltration
include:
using slow injection through a 27- or 30-gauge needle
injecting through the wound margin
using warm solution
using buffered (with bicarbonate) solution.
mk:@MSITStore:E:\EMERGENCY%20MEDICINE\EMERGENCY%20MEDICINE... 31/03/2014
Print: Section 3. Analgesia, Anesthesia, and Sedation
Page 7 of 9
Epinephrine (1:100,000):
Is often added to LAs before administration.
Addition of epinephrine increases the duration of anesthesia, provides wound hemostasis, and
slows systemic absorption.
Epinephrine causes vasoconstriction and therefore should be avoided in an end-arterial field
such as the digits, pinna, nose, and penis.
Lidocaine:
Is the most commonly used LA in the ED.
Has a 2- to 5-min onset of effect and a 1- to 2-hr duration of effect.
The max dose of infiltrative lidocaine is 4.5 mg/kg without or 7 mg/kg with epinephrine.
Lidocaine is buffered to decrease the pain of injection by adding 1 mL NaHCO3 to 9 mL lidocaine.
Bupivacaine:
Has an onset of effect of 37 mins and a duration of effect of 90 mins to 6 hrs.
Is preferred for prolonged procedures.
The max dose of infiltrative bupivacaine is 2 mg/kg without or 3 mg/kg with epinephrine.
Buffering of bupivacaine is accomplished with 1 mL NaHCO3 to 29 mL bupivacaine.
Procaine and tetracaine are ester anesthetics most commonly used in patients with allergies to
amide anesthetics.
DIGITAL BLOCKS
Finger and toe blocks are advantageous because:
less anesthetic is needed
better anesthesia is obtained
tissues are not distorted.
The onset of anesthesia is delayed when compared with that of LA.
Neurovascular status must be assessed and documented before the procedure.
Lidocaine and bupivacaine are the most commonly used agents and depend on the time needed to
perform the procedure.
Epinephrine should not be used in these procedures.
Complications include nerve injury and intravascular injection leading to systemic toxicity.
Always aspirate before injecting to avoid inadvertent intravascular injection of LA.
Procedure for digital blocks:
Sterile preparation of the skin, followed by the introduction of a 27-gauge or smaller needle into
the skin (a skin wheal may be raised before deeper injection) and into one side of the extensor
tendon of the affected finger just proximal to the web.
After aspiration, approximately 1 mL LA is injected into the tissue on the dorsal surface of the
extensor tendon.
The needle is advanced toward the palm until its tip is seen beneath the volar skin at the base of
the finger just distal to the web.
After aspiration, 1 mL LA is injected.
Before removing the needle, redirect it across the opposite side of the finger and inject approx.
1 mL across the dorsal digital nerve.
5 mins later, repeat the procedure on the opposite side of the finger (Fig. 10-1).
Alternate method:
Inject a 27-gauge needle into the web space between the affected and an adjacent finger while
directing the needle to the metacarpal joint of the affected finger.
After aspiration, inject 12 mL into the area of the digital nerve.
Before removal of the needle, advance the needle first dorsally and then volarly, and inject 1 mL
LA; repeat on the opposite side.
Toes can be blocked in similar fashion.
Great toes also can be blocked with a modified collar block.
mk:@MSITStore:E:\EMERGENCY%20MEDICINE\EMERGENCY%20MEDICINE... 31/03/2014
Print: Section 3. Analgesia, Anesthesia, and Sedation
Page 8 of 9
A 27-gauge needle is introduced to the dorsolateral aspect of the base of the toe until it
blanches the plantar skin.
As the needle is withdrawn, 1.5 mL LA is injected.
Before the needle is removed, it is passed under the skin on the dorsal aspect of the toe, and
1.5 mL LA is injected as the needle is withdrawn.
The needle is reintroduced through the anesthetized skin on the dorsomedial aspect of the toe
and advanced until the plantar skin is blanched; as the needle is withdrawn, 1.5 mL LA is injected.
Fig. 10-1.
Needle positions for digital nerve block.
LOCAL ANESTHETIC INFILTRATION
LAs can provide anesthesia at a site by infiltrating directly into the site or by infiltrating around the
peripheral nerves supplying the site.
The most common use of LA is infiltration for wound repair or invasive painful procedures.
When repairing wounds, LA can be infiltrated into the wound margins or as a "field block"
surrounding the wound.
When infiltrating intact skin, raising a wheal may cause less pain on subsequent infiltration.
LA also can be used in orthopedic procedures, such as fracture and joint reduction, by directly
injecting the LA into the affected joint or fracture hematoma.
For some wounds, LA infiltration around the peripheral nerves is advantageous due to
decreased total LA required and decreased pain at the site of injection.
This is most commonly used for procedures involving the hand, digits, or foot.
Before a regional block, it is imperative to assess neurovascular status.
During administration, the syringe plunger must be drawn back to avoid intravascular injection
mk:@MSITStore:E:\EMERGENCY%20MEDICINE\EMERGENCY%20MEDICINE... 31/03/2014
Print: Section 3. Analgesia, Anesthesia, and Sedation
Page 9 of 9
of LA.
Onset of effect of anesthesia with peripheral nerve blocks often is delayed (up to 15 mins).
TOPICAL ANESTHETICS
Topical anesthetics, which can eliminate the need for LA infiltration into some wounds, are applied
painlessly, do not distort wound edges, and may provide hemostasis.
Common preparations include:
tetracaine adrenaline cocaine (TAC)
lidocaine epinephrine tetracaine (LET)
lidocaine prilocaine (EMLA)
various preparations of lidocaine.
TAC is no longer commonly used due to regularity issues and adverse effects such as seizures,
respiratory arrest, and death.
LET is applied by placing a LET-saturated cotton ball or gauze pad onto the wound for a minimum
of 2030 mins.
Neither TAC nor LET should be used on mucous membranes or in end-artery fields.
Topical lidocaine:
Is marketed in a solution, cream, jelly, or ointment.
Viscous lidocaine can be used for the temporary relief of inflamed mucous membranes.
Lidocaine jelly can be used to facilitate the insertion of urinary catheters, nasogastric tubes, and
fiberoptic scopes.
As with infiltrative use of lidocaine, care must be taken not to exceed maximal doses.
EMLA:
Cream composed of lidocaine and prilocaine.
Used on intact skin to relieve the pain associated with venipuncture, arterial puncture, port
access, and other superficial skin procedures.
Has a 45- to 60-min onset of effect and a 60-min duration upon withdrawal.
Because prilocaine may cause methemoglobinemia, EMLA should be used with caution in infants
< 3 mos and avoided in patients predisposed to methemoglobinemia.
For further reading in Emergency Medicine: A Comprehensive Study Guide, 6th ed., see
Chapter 36, "Acute Pain Management in the Adult Patient," by Gary D. Zimmer; Chapter 38,
"Procedural Sedation and Analgesia," by David D. Nicolaou; Chapter 134, "Acute Pain
Management and Procedural Sedation in Children," by Michael N. Johnston and Erica Liebelt;
and Chapter 37, "Local and Regional Anesthesia," by Eric Higginbotham and Robert J. Vissers.
Copyright 2007 The McGraw-Hill Companies. All rights reserved.
Privacy Notice. Any use is subject to the Terms of Use and Notice. Additional Credits and Copyright Information.
mk:@MSITStore:E:\EMERGENCY%20MEDICINE\EMERGENCY%20MEDICINE... 31/03/2014
S-ar putea să vă placă și
- Unity of Health Through Yogaand Islamic ShalatDocument6 paginiUnity of Health Through Yogaand Islamic ShalatAnonymous SQNcItqXQnÎncă nu există evaluări
- 7903 35982 3 PBDocument9 pagini7903 35982 3 PBEl-yes Yonirazer El-BanjaryÎncă nu există evaluări
- Between the Backbone and the Ribs: Quran on Male Sexual FunctionDocument3 paginiBetween the Backbone and the Ribs: Quran on Male Sexual FunctionAnonymous SQNcItqXQnÎncă nu există evaluări
- Fasting EffectsDocument5 paginiFasting EffectsAnonymous SQNcItqXQnÎncă nu există evaluări
- 01-185.PDF. Shalat Geriatri Pasien #Document4 pagini01-185.PDF. Shalat Geriatri Pasien #Aad IbrahimÎncă nu există evaluări
- Fasting Effects1 PDFDocument4 paginiFasting Effects1 PDFAnonymous SQNcItqXQnÎncă nu există evaluări
- Biomechanical Response of Upper Body Muscles during Salat and Child's PoseDocument4 paginiBiomechanical Response of Upper Body Muscles during Salat and Child's PoseAnonymous SQNcItqXQnÎncă nu există evaluări
- Cardiothoracic TraumaDocument8 paginiCardiothoracic TraumaAnonymous SQNcItqXQnÎncă nu există evaluări
- 6.1 Smart Business Networks - How The Network WinsDocument8 pagini6.1 Smart Business Networks - How The Network WinsAnonymous SQNcItqXQnÎncă nu există evaluări
- Cyber Security Concerns For Emergency ManagementDocument21 paginiCyber Security Concerns For Emergency ManagementAnonymous SQNcItqXQnÎncă nu există evaluări
- Human Genetics and IslamDocument8 paginiHuman Genetics and IslamAnonymous SQNcItqXQnÎncă nu există evaluări
- Qatar Interprofessional Health Council - IPE For QatarDocument9 paginiQatar Interprofessional Health Council - IPE For QatarAnonymous SQNcItqXQnÎncă nu există evaluări
- GI Disorders and CuresDocument19 paginiGI Disorders and CurespjsworldÎncă nu există evaluări
- Puncture Wounds and Mammalian BitesDocument6 paginiPuncture Wounds and Mammalian BitesAnonymous SQNcItqXQnÎncă nu există evaluări
- Glide Well Notes 7Document8 paginiGlide Well Notes 7Amirah SyahirahÎncă nu există evaluări
- Surgery BasicsDocument6 paginiSurgery Basicssharu4291Încă nu există evaluări
- Syria and Assyria Synonyms?Document7 paginiSyria and Assyria Synonyms?marfosdÎncă nu există evaluări
- Leni MardawatiDocument6 paginiLeni MardawatiFeranita AbdurrahmanÎncă nu există evaluări
- PT GARUDA INDONESIA E-TICKET RECEIPT FOR HENRI PERWIRA NEGARADocument2 paginiPT GARUDA INDONESIA E-TICKET RECEIPT FOR HENRI PERWIRA NEGARAAnonymous SQNcItqXQnÎncă nu există evaluări
- Guanabana - Soursop PDFDocument2 paginiGuanabana - Soursop PDFAj GuanzonÎncă nu există evaluări
- Specific Indications in Clinical PracticeDocument58 paginiSpecific Indications in Clinical PracticeOccult Librarian100% (5)
- Charachteristics of A Muslim PhysicianDocument3 paginiCharachteristics of A Muslim PhysicianAnonymous SQNcItqXQnÎncă nu există evaluări
- Efek Bekam1Document2 paginiEfek Bekam1Anonymous SQNcItqXQnÎncă nu există evaluări
- The Syrian Conflict For DummiesDocument17 paginiThe Syrian Conflict For DummiesAnonymous SQNcItqXQnÎncă nu există evaluări
- Guanabana - Soursop PDFDocument2 paginiGuanabana - Soursop PDFAj GuanzonÎncă nu există evaluări
- Khutbah Jumat 2Document5 paginiKhutbah Jumat 2Anonymous SQNcItqXQnÎncă nu există evaluări
- Qadha' Qadar2Document3 paginiQadha' Qadar2Anonymous SQNcItqXQnÎncă nu există evaluări
- From Cell To System, From Mechanism To DiseaseDocument2 paginiFrom Cell To System, From Mechanism To DiseaseAnonymous SQNcItqXQnÎncă nu există evaluări
- Psycho-Spiritual Strategies in Treating Addiction PatientsDocument5 paginiPsycho-Spiritual Strategies in Treating Addiction PatientsAnonymous SQNcItqXQn100% (1)
- Charachteristics of A Muslim PhysicianDocument3 paginiCharachteristics of A Muslim PhysicianAnonymous SQNcItqXQnÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Analgetik Antipiretik AntiinflamasiDocument76 paginiAnalgetik Antipiretik AntiinflamasiranifebÎncă nu există evaluări
- 4a Rota-Vaccine Administration KenyaDocument21 pagini4a Rota-Vaccine Administration KenyaSandraÎncă nu există evaluări
- Drug StudyDocument9 paginiDrug StudyAysaaa DCÎncă nu există evaluări
- CIS Importers ListDocument2 paginiCIS Importers ListAmit SakpalÎncă nu există evaluări
- Daftar Obat-ObatanDocument8 paginiDaftar Obat-Obatanklinik keluargaÎncă nu există evaluări
- Pill Mill-Mori Dalton IndictmentDocument16 paginiPill Mill-Mori Dalton IndictmentSouthern Maryland OnlineÎncă nu există evaluări
- PRELIMSDocument21 paginiPRELIMSPrincess NicoleÎncă nu există evaluări
- Sildenafil Citrate: Sexual DysfunctionDocument8 paginiSildenafil Citrate: Sexual DysfunctionPits MitsÎncă nu există evaluări
- CNS Drugs: Drugs Acting On Central Nervous SystemDocument17 paginiCNS Drugs: Drugs Acting On Central Nervous Systemreza_juÎncă nu există evaluări
- Ondansetron 4Mg Tablets (Ondansetron Hydrochloride) PL 04543/0509 Ondansetron 8Mg Tablets (Ondansetron Hydrochloride) PL 04543/0510Document47 paginiOndansetron 4Mg Tablets (Ondansetron Hydrochloride) PL 04543/0509 Ondansetron 8Mg Tablets (Ondansetron Hydrochloride) PL 04543/0510Santosh VarmaÎncă nu există evaluări
- Cara Efektif Melakukan Stock OpnameDocument126 paginiCara Efektif Melakukan Stock OpnameDita PrimandariÎncă nu există evaluări
- Drug Study ArraDocument5 paginiDrug Study ArraPaul ManaloÎncă nu există evaluări
- Katzung LaxativesDocument6 paginiKatzung LaxativesLonnieAllenVirtudesÎncă nu există evaluări
- Chapter 10Document45 paginiChapter 10Hannah BuquironÎncă nu există evaluări
- BPT Question BankDocument10 paginiBPT Question BankRoydenPTÎncă nu există evaluări
- Daftar Harga HD Juni 2020Document34 paginiDaftar Harga HD Juni 2020Kean KhamidaaÎncă nu există evaluări
- Procto Synalar-N Rectal Cream FormulationDocument2 paginiProcto Synalar-N Rectal Cream FormulationSasho BojadzievÎncă nu există evaluări
- Stok Opname & Pengajuan 09 NovemberDocument24 paginiStok Opname & Pengajuan 09 NovemberAnnisa duaÎncă nu există evaluări
- Format OpnameDocument21 paginiFormat OpnamerestutiyanaÎncă nu există evaluări
- Drug Abuse and Addiction Quiz AnswersDocument10 paginiDrug Abuse and Addiction Quiz AnswersDanyal NadeemÎncă nu există evaluări
- Introduction To PharmacologyDocument50 paginiIntroduction To PharmacologyAbdishakour Hassa.100% (1)
- WHO Pharm 2-2023Document19 paginiWHO Pharm 2-2023Paola Cristini Gama SilvaÎncă nu există evaluări
- Steroids QuizDocument3 paginiSteroids Quizfaqed ilzakiraÎncă nu există evaluări
- Vendedores 01-12-22 ExcelDocument54 paginiVendedores 01-12-22 ExcelDaniel Gonzalez Amaro100% (1)
- Ncma216: BSN 2Nd Year 1St Semester Prelim 2021: Bachelor of Science in Nursing 2YADocument32 paginiNcma216: BSN 2Nd Year 1St Semester Prelim 2021: Bachelor of Science in Nursing 2YAMARIA STEPHANY DELA CRUZ100% (1)
- Panadol Osteo Product InformationDocument5 paginiPanadol Osteo Product Informationsalema2Încă nu există evaluări
- Rle Lectures Medications: Arturo G. Garcia JR RN, MSN, U.S RNDocument33 paginiRle Lectures Medications: Arturo G. Garcia JR RN, MSN, U.S RNMaria Paula Amor GeronimoÎncă nu există evaluări
- Tiaft Drug Concentration Reference TableDocument20 paginiTiaft Drug Concentration Reference TablerodrigoÎncă nu există evaluări
- 10 Rights of Drug Administration With Nursing ImplicationsDocument3 pagini10 Rights of Drug Administration With Nursing ImplicationsJet Bautista100% (6)
- German RemediesDocument2 paginiGerman RemediesbhuvaneshkmrsÎncă nu există evaluări