Documente Academic
Documente Profesional
Documente Cultură
Konsensus Hipertiroid
Încărcat de
DiethaKusumaningrumDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Konsensus Hipertiroid
Încărcat de
DiethaKusumaningrumDrepturi de autor:
Formate disponibile
34
The Indonesian Society of Endocrinology
Indonesian Clinical Practice Guidelines for Hyperthyroidism
Feature Article
Indonesian Clinical Practice Guidelines for Hyperthyroidism
The Indonesian Society of Endocrinology
Task Force on Thyroid Diseases
Abstract
Hyperthyroidism remains as one of the major thyroid disorders in Indonesia.The Indonesian Task Force on Thyroid
Diseases determined that hyperthyroidism represents a priority area in need of updated evidence-based practice
guidelines.The aim of the guidelines is to provide the best evidence-based recommendations for diagnostic evaluation
and management of hyperthyroidism in the adult population. The following article summarizes the guidelines.
Keywords: hyperthyroidism, clinical practice guidelines, Indonesia
Introduction
In the Republic of Indonesia, the prevalence of
hyperthyroidism stands at 6.9% (latest Indonesian Basic
Health Research data which was performed in 2007 with
TSH cut-off level < 0.55 mIU/L). Scientific advances
relevant to this topic are reported in a diverse array of
literature, including subspecialty publications in
endocrinology, pediatrics, nuclear medicine, and surgery,
making it challenging for clinicians, especially in
Indonesia, to keep abreast of new developments.
The Indonesian Clinical Practice Guidelines for
Hyperthyroidism is a project of the Indonesian Task Force
on Thyroid Diseases, which is a collaboration of
Indonesian endocrinologists caring for individuals with
hyperthyroidism. The objective of this project is to develop
clinical practice guidelines on the screening, diagnosis and
management of hyperthyroidism which reflect the current
best evidence on optimal medical practice and incorporate
local data into the recommendations. It is not the intent of
these guidelines to replace clinical judgment and
individual decision making. Each recommendation should
be evaluated in light of these elements in order that
optimal patient care is delivered.
Summary of
development
the
methodology
for
guidelines
The guidelines were developed by the Indonesian Task
Force on Thyroid Diseases. The Task Force reviewed
available literatures on hyperthyroidism. The Task Force
was able to obtain valuable feedback and suggestions to
include additional evidence from the literature and to
consider alternative interpretation of data. The
________________________________________
ISSN 0857-1074
Printed in the Philippines
Copyright 2012 by the JAFES
Received April 27, 2012. Accepted April 27, 2012.
34
www.asean-endocrinejournal.org
www.asean-endocrinejournal.org
participants contributed to and influenced the form of the
final guidelines, making it a comprehensive report from
various geographical origins and medical disciplines.
Summary of recommendations
Definitions
Hyperthyroidism is a clinical condition caused by
increased synthesis and secretion of hormones by the
thyroid gland which affects the entire body.
Thyrotoxicosis is defined as clinical manifestations related
to increased thyroid hormone levels.
Epidemiology
Graves' disease (GD) persists as the most frequentlyencountered etiology of hyperthyroidism causing
approximately 60-80% of all cases of thyrotoxicosis
worldwide. It is also more frequently found in females
with a female-to-male ratio of 8:1 and apparently
manifests in the third and fourth decades of life.
Clinical signs and symptoms
The signs and symptoms of hyperthyroidism are diverse
and are mostly determined by the subject's age and the
presence of prior organ disorders. Young patients
typically complain of excessive sympathetic nerve
symptoms, such as anxiety, hyperactivity and tremors,
while the elderly commonly complain of cardiovascular
symptoms
(cardiomyopathy,
arrhythmia)
and
unexplained weight loss.
The most commonly encountered symptoms in
thyrotoxicosis are the following: nervousness and anxiety;
excessive sweating, warm skin and heat intolerance;
irritability; palpitations; hyperdefecation; easy fatigability;
Correspondence: Secretariat of the Indonesian Society of Endocrinology
Division of Endocrinology and Metabolism, Department of Internal
Medicine, Faculty of Medicine
University of Indonesia, Cipto Mangunkusumo National Hospital
Jalan Salemba 6, Central Jakarta,
DKI Jakarta 10431
Telephone numbers: +62213100075, +62213907703
Fax. +62213928658, +62213928659
E-mail. endo_id@indo.net.id.
34
Vol. 27 No. 1 May 2012
Indonesian Clinical Practice Guidelines for Hyperthyroidism
weight loss with increased appetite (Von Mullers
paradox) and menstrual disorders.
While the most frequently observed clinical signs are as
follows: thyroid gland hypertrophy or struma;
hyperactivity; tachycardia or atrial fibrillation; systolic
hypertension; warm and increased perspiration of the
skin; tremor; muscle fatigue; ocular disorders such as
Mobius sign (impaired ocular convergence), von Graefes
sign (the failure of the upper eyelid to follow promptly
and smoothly the downward movement of the eyeball),
Joffroys sign (the facial muscles remain immobile when
the eyeballs are rolled upward ), Stellwags sign
(infrequent and incomplete blinking of the eyes), lid lag
( the upper eyelid lags behind the upper edge of the iris as
the eye moves downward), exophthalmos and its
following consequences e.g., conjunctivitis, corneal ulcer,
palpebral edema, optic neuritis and optic atrophy.
Diagnosis of hyperthyroidism
To distinguish between hyperthyroidism and other
causes of thyrotoxicosis, a radioactive iodine uptake
(RAIU) should be performed. Hyperthyroidism has
high RAIU while the other etiologies havelow or near
absent
radioactive iodine uptake.The assessment of
hyperthyroidism manifestations, and especially potential
cardiovascular and neuromuscular complications, is
essential to formulating an appropriate treatment plan.
Clinical evaluation
Biochemical evaluation of TSH and thyroid hormones is
the most important initial diagnostic test for individuals
suspected of hyperthyroidism/ thyrotoxic crisis based on
clinical manifestations.
When there is inconsistency among the clinical signs and
symptoms, or when clinical manifestations are subtle, or
confirmatory biochemical testing is not readily accessible,
it may be helpful to use a diagnostic index called the
Wayne' s index. This is a scoring system that has been
developed since 1972 to help improve the diagnostic
accuracy of clinical assessment.
The Indonesian Society of Endocrinology
35
Biochemical evaluation
Overt hyperthyroidism is characterized by suppressed
TSH (<0.01 mU/L) and excess thyroid hormones in serum.
Serum TSH
Serum TSH measurement has the highest sensitivity and
specificity of any single blood test and is used as an initial
screening test for hyperthyroidism. In hyperthyroidism,
serum TSH will be less than 0.01 mU/L or even
undetectable.
Serum thyroid hormones
To assess the severity of the condition and to improve
diagnostic accuracy, both TSH and free T4 levels should be
assessed at the time of the initial evaluation. In overt
hyperthyroidism, usually both serum free T 4 and T3
estimates are elevated, and serum TSH is < 0.01 mU/L or
undetectable. In milder hyperthyroidism, serum T 4 and
free T4 estimates can be normal, only serum T3 may be
elevated, and serum TSH will be less than 0.01 mU/L (or
undetectable) called T3 thyrotoxicosis. Assays for
estimating free T3 are less widely-validated than those for
free T4, and therefore measurement of total T 3 is frequently
preferred in clinical practice.
Subclinical hyperthyroidism is defined as a normal serum
free T4 estimate and normal total T 3 or free T3 estimate,
with subnormal serum TSH concentration.
TRAb (thyrotropin receptor antibody)
This approach is utilized when a thyroid scan and uptake
are unavailable or contraindicated (e.g., during pregnancy
and lactation).
Imaging
Radioactive iodine uptake (RAIU) and thyroid scanning
RAIU should be performed when the clinical presentation
of thyrotoxicosis is not diagnostic of GD. A thyroid scan
should be added in the presence of thyroid nodularity.
Table 1. Waynes index of signs and symptoms scoring system in diagnostic approach of hyperthyroidism
Symptoms of recent onset and/or increased severity
Dyspnea on effort
Palpitations
Tiredness
Preference for heat
Preference for cold
Excessive sweating
Nervousness
Appetite : increased
decreased
Weight : increased
decreased
Scores
(+)1
(+)2
(+)2
(-) 5
(+)5
(+)3
(+)2
(+)3
(-) 3
(-) 3
(+)3
Signs
Palpable thyroid
Bruit over thyroid
Exophthalmos
Lid retraction
Lid lag
Hyperkinesis
Hands : hot
moist
Casual pulse rate :
> 80/min
> 90/min
Atrial fibrillation
Only if present
Only if absent
(+)3
(+)2
(+)2
(+)2
(+)1
(+)4
(+)2
(+)1
(-) 3
(-) 2
(+)3
(+)4
(-) 3
-
(-) 2
(-) 2
(-) 1
Total score interpretation:
> 19 = toxic
11-19 = equivocal
< 11 = euthyroid/not toxic
Vol. 27 No. 1 May 2012
www.asean-endocrinejournal.org
36
The Indonesian Society of Endocrinology
Ultrasonography (USG)
USG is performed with the patient in the supine position
and the neck hyper-extended. USG can detect thyroid
lobes or lesions as small as 2 mm. It can distinguish solid
nodules from simple and complex cysts. It can estimate
thyroid size, give a rough estimate of tissue density, show
vascular flow and velocity and aid in placing a needle for
diagnostic purpose. Doppler studies may be added while
executing ultrasonography.
Fine needle aspiration biopsy (FNAB)
In GD, FNAB is necessary if a nodule is found within the
thyroid to distinguish benign from malignant nodules
which may occur. We recommend an USG-guided FNAB.
Management
The management of hyperthyroidism involves 3 interrelated aspects:
1. Inhibition of thyroid hormone synthesis and
secretion (ATDs)
2. Destruction or reduction of thyroid tissue mass
(radioactive iodine therapy or surgery)
3. Minimalization of thyroid hormone effects on
peripheral tissues (beta-blocker therapy)
Judicious decision-making in choosing the most wellsuited therapy depends on several factors, such as the
severity of hyperthyroidism, age, struma size and the
presence of comorbidities.
Specific management for Graves' Disease
There are 3 treatment modalities that can be
used:antithyroid drugs (ATDs), radioactive iodine therapy
and thyroidectomy.
ATDs are suggested in GD patients with the following
conditions:
a. Patients with high likelihood of remission
(patients, especially females, with mild disease,
small goiters, and negative or low-titer TRAb)
b. Elderly or others with comorbidities increasing
surgical risk or with limited life expectancy
c. Individuals in nursing homes or other care
facilities who may have limited longevity and are
unable to follow radiation safety regulations
d. Patients with previously operated or irradiated
necks
e. Moderate-to-severe
active
Graves
ophthalmopathy (GO)
Radioactive iodine therapy is highly favored in GD
patients with the following clinical conditions:
a. Females planning a pregnancy in the future (in
more than 46 months following radioiodine
therapy, provided thyroid hormone levels are
normal),
b. Individuals with comorbidities increasing
surgical risk
www.asean-endocrinejournal.org
Indonesian Clinical Practice Guidelines for Hyperthyroidism
c.
d.
Patients with previously operated or externally
irradiated necks, or lack of access to a highvolume thyroid surgeon
Contraindications to ATDs use
Surgical procedures are recommended in patients with GD
with the following conditions:
a. Symptomatic compression or large goiters (80 g)
b. Relatively low uptake of radioactive iodine
c. When thyroid malignancy is documented or
suspected (e.g., suspicious or indeterminate
cytology);
d. Large
nonfunctioning,
photopenic
or
hypofunctioning nodule
e. Coexisting
hyperparathyroidism
requiring
surgery
f. Females planning a pregnancy in <46 months
(i.e., before thyroid hormone levels would be
normal if radioactive iodine were chosen as
therapy), especially if TRAb levels are
particularly high
g. Patients with moderate-to-severe active GO
Contraindications to a particular modality as treatment
for Graves hyperthyroidism:
1. Radioactive
iodine
therapy:
Definite
contraindications include:
a. Pregnancy and lactation
b. Coexisting thyroid cancer or suspicion of
thyroid cancer
c. Individuals unable to comply with radiation
safety guidelines
d. Females planning a pregnancy within 46
months
e. Severe and active GO
2. ATDs
Definite contraindications to long-term ATD
therapy include previous known major
adversereactions to ATDs
3. Surgery
Definite contraindications might include:
a. Substantial
comorbidity
such
cardiopulmonary disease
b. End-stage cancer
c. Other debilitating disorders
as
1. Management of GD using ATDs
There are 2 classes of ATDs available:thiouracil
(propylthiouracil (PTU)) and imidazoles (methimazole
(MMI), carbimazole and thiamazole).
PTU is suggested as the preferred drug in the following
conditions: during the first trimester of pregnancy; thyroid
storm or thyroid crisis; and among those with history of
allergy or intolerance to anti-thyroid drugs and who
refuse to undergo radioactive iodine or surgical therapies.
Vol. 27 No. 1 May 2012
Indonesian Clinical Practice Guidelines for Hyperthyroidism
Combination of ATDs with low-dosage L-thyroxine as
hormone replacement therapy is generally not
recommended.
The Indonesian Society of Endocrinology
37
The initial dose of PTU is high, starting with 100-200 mg
three times daily, depending on the severity of the
hyperthyroidism. As the clinical findings and thyroid
function tests return to normal, reduction to a
maintenance PTU dose of 50 mg two or three times daily,
even once daily is usually possible as the maintenance
dose.
Follow-up within the first 13 months after radioactive
iodine therapy for GD should include an assessment of
free T4 and total T3. If after 3 months follow-up, the
patient remains thyrotoxic, a second dose of radioactive
iodine therapy shall
be considered. Transient
hypothyroidism following radioactive iodine therapy can
rarely occur during 6 months following iodine therapy,
with subsequent complete recovery of thyroid function.
Therefore, hypothyroidism occurring during those first 6
months does not necessitate a thyroid hormone
replacement therapy.
As with PTU, at the start of MMI therapy, higher doses are
advised (1020 mg daily) to restore euthyroidism,
following which the dose can be titrated to a maintenance
level (generally 510 mg daily). MMI has the benefit of
once-a-day administration and a reduced risk of major
side effects compared to PTU.
Thyroid hormone replacement therapy should be given
accordingly for a lifetime basis. Every patient who
undergo radioactive iodine therapy should be thoroughly
explained regarding the occurrence of post therapy
hypothyroidism and other substantial information related
to radioactive iodine therapy.
An assessment of serum free T4 should be obtained about
4 weeks after initiation of therapy, until euthyroid levels
are achieved with the minimal dose of medication. Once
the patient is euthyroid, biochemical testing and clinical
evaluation can be undertaken at intervals of 23 months.
3. Surgical management of patients with GD
Whenever possible, patients with GD undergoing
thyroidectomy should be rendered euthyroid. In
exceptional circumstances, when it is not possible to
render a patient with GD euthyroid prior to thyroidectomy, the need for thyroidectomy is urgent, or when the
patient is allergic to antithyroid medication, the patient
should be adequately treated with beta-blockade and
potassium iodide in the immediate preoperative period.
Before initiating antithyroid drug therapy, requesting for
baseline blood tests, primarily differential white blood cell
count, bilirubin and transaminases may be considered.
2. Radioactive iodine therapy in GD
Patients with GD who are at increased risk for complications due to worsening of hyperthyroidism (i.e., those
who are extremely symptomatic or have free T4 estimates
23 times the upper limit of normal) should be treated
with beta-adrenergic blockade and/or ATDs prior to
radioactive iodine therapy.
If given as pretreatment, MMI should be discontinued 35
days before the administration of radioactive iodine,
restarted 37 days later, and generally tapered over 46
weeks as thyroid function normalizes.
A pregnancy test should be obtained within 48 hours prior
to treatment in any female with childbearing potential
who is to be treated with radioactive iodine. The treating
physician should obtain this test and verify a negative
result prior to administering radioactive iodine.
Approximately 2 weeks after and prior to radioactive
iodine therapy, high-iodine-containing foods such as
seafoods and iodine-containing drugs are strictly
prohibited. During 3 days following a radioactive iodine
therapy, patients should be advised not to stay close (less
than 5 meters in radius of distance) with children aged less
than 13 years old and pregnant women. Patients are
strictly prohibited to get pregnant in 6 months following
radioactive iodine therapy; contraceptives are advisable
during that period.
Vol. 27 No. 1 May 2012
Surgical complications following thyroidectomy in GD
patients are relatively scarce, i.e., hypoparathyroidism and
vocal cord paralysis. Improved patient outcome,
specifically complication rate, has been shown to be independently associated with high thyroidectomy surgeon
volume.
Prognosis
GD prognosis is well-reflected with remission and relapse
rates. Remission rates among adults are higher than
children.
ATDs are able to induce permanent remission in 30-50%
cases. If relapse occurs in GD patients treated with ATDs,
then destructive therapy is more likely to be a more
appropriate option. Following 12-18 months of ATDs
administration, approximately more than 50% of patients
will develop a relapse. Several studies reported that a high
TSH-R Ab level prior to therapy discontinuation
suspectedly related to high relapse rate.
T3/T4 ratio of more than 20 is related to more than 80%
relapse risk. Low TSH level 4 weeks after ATDs
discontinuation has been correlated with relapse
occurrence in 70% cases. There is a correlation between
thyroid volume and blood flow, in which this finding
strengthened previous known correlation between large
struma and high risk to recur. Superior thyroid artery
www.asean-endocrinejournal.org
38
The Indonesian Society of Endocrinology
blood flow also has already been known as one of relapse
risk predictors.
All patients shall be strictly-monitored for relapse
occurrence after discontinuation of ATDs. Approximately
75% relapse events occurred in the first 3 months after
discontinuation. If relapse does occur, further ATDs
administration in a longer period shall be prescribed or
destructive therapy is likely to be considered.
Hyperthyroidism in pregnancy
Patients with GD require prompt treatment with ATDs
and should undergo frequent monitoring for signs of fetal
and maternal hyper- and hypothyroidism. ATDs are now
considered the mainstay of therapy for hyperthyroidism
during pregnancy to help prevent perinatal complications.
Diagnosis
Clinical features that may indicate the presence of
significant hyperthyroidism include failure to gain weight,
heart intolerance, excessive sweating, and tachycardia,
beyond that normally associated with pregnancy.
Therefore clinical diagnosis indices such as Waynes index
is not appropriate to be used to diagnose hyperthyroidism
in pregnancy.
We have to be aware of thyrotoxicosis in molar pregnancy
when pulse rate > 100 bpm and/or when the fundus of
uterus larger than 20 gestational weeks. (Bandung Study,
1992)
Biochemical evaluation
The diagnosis of hyperthyroidism in pregnancy should be
made using serum TSH values, and either total T4 and T3
(with total T4 and T3 reference range adjusted at 1.5 times
the nonpregnant range) or free T4 and free T3 estimations
(with trimester-specific normal reference ranges).
In the first trimester serum TSH may be transiently
suppressed (< 0.2 U/L), at time of peak hCG level and
this must be considered in making diagnosis. Free T 4 is the
parameter that has been most closely correlates with good
fetal outcome. Serum TSH may still be suppressed in these
patients and should not be used as the sole guide in
treatment, although normalization of maternal TSH
during ATDs therapy may indicate a need to reduce the
dose of ATDs.
TRAb
GD as the cause of hyperthyroidism in pregnancy may be
diagnosed from typical clinical findings, including the
presence of GO and/or serum TRAb in hyperthyroid
patients. TRAb levels should be measured when the
etiology remains unclear.
TRAb measurement is indicated when the etiology could
not be ascertained. Other indications are fetal tachycardia,
fetal goiter on USG and intrauterine growth restriction.
www.asean-endocrinejournal.org
Indonesian Clinical Practice Guidelines for Hyperthyroidism
Complications
Patients with this disorder should be treated at centers
with specific expertise in this area. Maternal
complicationas are miscarriage, pregnancyinduced
hypertension, preterm delivery, congestive heart failure,
thyroid storm and placenta abruption. Fetal complications
are low birth weight, prematurity, small for gestational
age, intrauterine growth restriction, stillbirth and thyroid
dysfunction.
Management
Effective treatment of hyperthyroidism during pregnancy
is necessary to prevent maternal, fetal, and neonatal
complications. ATDs remain the treatment of choice for
hyperthyroidism during pregnancy. The goal is to use the
lowest possible dosage of antithyroid medication
necessary to maintain the free T4 in the upper one-third of
the reference range or just above the normal range.
Transient hCG-mediated thyrotropin suppression in early
pregnancy should not be treated with antithyroid drug
therapy.
Antithyroid drug therapy
Propylthiouracyl and methimazole should be used for
hyperthyroidism due to GD that requires treatment during
pregnancy. Propylthiouracil should be used when
antithyroid drug therapy is started during the first
trimester. Methimazole should be used when antithyroid
drug therapy is started after the first trimester.
The initial recommended PTU dosage is 100 to 450 mg
daily, depending on symptoms and results of thyroid
function tests. The total dosage is divided into 3 daily
doses. Methimazole can be initiated at 10 to 20 mg daily in
1 dose.
The dose of ATD should be kept as low as possible. Blockreplacement therapy consisting of ATD plus levothyroxine
should not be used in pregnancy. If a woman receiving
such therapy becomes pregnant, therapy should be
changed to an ATDs alone.
-Adrenergic blockers, such as propranolol, 10 to 40 mg
every 4 to 6 hous, or atenolol, 25 to 50 mg daily, are also
recommended for treatment of hyperadrenergic
symptoms present in hyperthyroidism, but should be
discontinued once symptoms resolve or within the first
few weeks of treatment.
Monitoring
At the initiation of therapy, women should be monitored
every 2 weeks for titration of antythyroid drug dosage; the
dosage should be decreased with the improvement of
symptoms and signs (eg, weight gain and normalization of
pulse rate) and free T4.Once the free T4 target is achieved,
thyroid tests may be repeated every 2 to 4 weeks to keep
the patients free T4 in the upper reference range with the
lowest possible dosage of antithyroid drug. The presence
Vol. 27 No. 1 May 2012
Indonesian Clinical Practice Guidelines for Hyperthyroidism
The Indonesian Society of Endocrinology
of detectable TSH is an indication to decrease the
antithyroid drug dosage.
References
Patients who achieve euthyroidism with minimal dosages
of ATDs and have a short duration of symptoms,
undetectable or low TRAb titers, and small goiters may be
able to discontinue ATDs during the last 4 to 8 weeks of
pregnancy. Discontinuing medication before 32 weeks
gestation is not recommended because of the possibility
that hyperthyroidism may recur.
2.
Other management alternatives
Radioactive iodine therapy is contraindicated in
pregnancy and lactation. A pregnancy test is mandatory
for any woman of childbearing age who is receiving either
diagnostic or therapeutic doses of radioactive iodine.
When thyroidectomy is necessary for the treatment of
hyperthyroidism during pregnancy, the surgery should be
performed if possible during the second trimester.
Although it is the safest time, it is not without risk (4.5%5.5% risk of preterm labor).
Breast feeding
MMI and PTU both appear in breast milk in small
concentrations. However, because of potential to progress
into hepatic necrosis in either mother or child from
maternal PTU use, MMI is the preferred ATD in nursing
mothers.
Patient counseling
Patients taking methimazole who decide to become
pregnant should get a pregnancy test at the earliest
suggestion of pregnancy and be switched to
propylthiouracil as soon as possible in the first trimester
and changed back to methimazole at the beginning of the
second trimester. Similarly, we suggest that patients
started on propylthiouracil during the first trimester be
switched to methimazole at the beginning of the second
trimester.
Prepregnancy counselling for all patients with
hyperthyroidism or a history of hyperthyroidism is
imperative. Before conception, a hyperthyroid patient may
be offered ablative by iodine 131 (131I) or surgery or
definitive treatment or medical therapy
Risks associated with both PTU and methimazole should
be informed to patients. Close monitoring and follow-up
throughout pregnancy with frequent blood tests and
adjustment of ATDs are needed since reduction in drug
dosages are commonly required.
Authors Disclosure
This review was written independently; no company or
institution supported it financially. Authors declared no inherent
conflicts of interest..
Vol. 27 No. 1 May 2012
1.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
39
Abraham-Nordling M TO, Hamberger B, et al. GD: A long-term
quality-of-life follow up of patients randomized to treatment with
ATDs, radioiodine, or surgery. Thyroid. 2005;15:1279-86.
Adesina O. Expensive but unreliable: Wayne index to the rescue.
Endocrine Abstracts. 2010;21: 367.
Allahabadia A, Daykin J, Holder RL, Sheppard MC, Gough SCL,
Franklyn JA. Age and gender predict outcome of treatment for
Graves hyperthyroidism. J Clin Endocrinol Metab. 2000;85:1038-42.
ATA/AACE Guidelines 2011. Hyperthyroidism and other causes of
thyrotoxicosis: Management guidelines of the American Thyroid
Association and American Association of Clinical Endocrinologist.
Endocr Pract. 2011;17:3.
Bahn RS, Burch HB, Cooper DS et al. Hyperthyroidism and other
causes of thyrotoxicosis: Management guidelines of the American
Thyroid Association and American Association of Clinical
Endocrinologists. Endocr Pract. 2011;3:e1-e65.
Chan GW, Mandel SJ. Therapy Insight: Management of GD during
pregnancy. Nat Clin Pract Endocrinol Metab. 2007;3(6):470-478
Cinemre H, Bilir C, Gokosmanoglu F, Akdemir N, Erdogmus B,
Buyukkaya. Predictors of time to remission and treatment failure in
patients with Graves disease treated with propylthiourasil. Clin
Invest Med. 2009;32(3):E199-205.
Davies TF, Larsen PR. Thyrotoxicosis. In: Williams Texbook of
Medicine. Editors: Kronenberg HM, Melmed S, Polonsky KS, Larsen
PR. 11th ed. Saunders Elsevier, Philadelphia. 2008; 333- 375.
Djokomoeljanto R. Pengobatan medik hipertiroidisme. Dalam Adam
JMF (Ed): Endokrinologi Praktis. Diabetes Melitus, Tiroid,
Hiperlipidemia. Ujung Pandang. 1989:185-194.
Djokomoeljanto. Kelenjar Tiroid, hipotiroidisme, dan hipertiroidisme.
Dalam: Buku Ajar Ilmu Penyakit Dalam. Editor: Sudoyo AW,
Setiyohadi B, Alwi I, Simadibrata M, Setiati S. Edisi keempat-Jilid III.
Pusat Penerbitan Departemen Penyakit Dalam FK Universitas
Indonesia. 2006;195565.
Djokomoeljanto R. Tirotoksikosis. In: Djokomoeljanto R, ed. Buku
Ajar Tiroidologi Klinik. Semarang: Badan Penerbit Universitas
Diponegoro. 2007;217.
Glinoer D. Thyroid disease during pregnancy.In Braverman LE &
Utiger RD. (eds) Werber& Ingbars. The Thyroid A Fundamental and
Clinical Text. 2005;1086-105.
Hegedus l, Bennedbaek FN. Nonisotopic techniques of thyroid
imaging. In Braverman LE & Utiger RD (eds) Werber & Ingbars. The
Thyroid A Fundamental and Clinical Text. 2005; 373-383.
Kariadi SHKS. Thyrotoxicosis in hydatidiform mole patients:
Prevalence and evaluation of hCG level, heart rate and uterus size. In.
de Escobar M, de Vijlder JJM, Butz S. Hostalek U (eds). The Thyroid
and Brain Stuttgart:Schsttsuer. 2002;344.
Mandel SJ. Diagnosis and Treatment of Thyroid Disease During
Pregnancy In DeGroot LJ and Jameson JL (eds). Endocrinology 5 th Ed.
Elsevier Saunders. 2006;3437-50.
Patil-Sisodia K, Mestman JH. Graves hyperthyroidism and
pregnancy: A clinical update. Endocr Pract. 2010;16(1):118.
Pekonen F , Althan H, Stenman UH, Ylikorkala O. Chorionic
gonadotropin (hCG) and thyroid function in early human pregnancy:
Circadian variation and evidence of intrinsic thyrotopic activity of
hCG.J Clin Endocrinol Metab. 1998;66:853.
Soeatmadji DW. Disfungsi tiroid subklinis: hipotiroidisme subklinis
dan hipertiroidisme subklinis. In: Djokomoeljanto R, ed. Buku Ajar
Tiroidologi Klinik. Semarang: Badan Penerbit Universitas
Diponegoro. 2007.
Tunbridge WM ED, Hall R, et al. The spectrum of thyroid disease in a
community: The Whickham survey. Clin Endocrinol (Oxf).
1977;7:481-93.
Wallaschofski H, Miehle K, Mayer A, Tuschy U, Hentschel B, Paschke
R. Prediction of remission or relapse for Graves hyperthyroidism by
the combined determination of stimulating, blocking and binding
TSH-receptor antibodies after the withdrawal of antithyroid drug
treatment. Horm Metab Res. 2002;34:383-8.
www.asean-endocrinejournal.org
S-ar putea să vă placă și
- Timebomb:The Global Epidemic of Multi-Drug Resistant TuberculosisDe la EverandTimebomb:The Global Epidemic of Multi-Drug Resistant TuberculosisEvaluare: 3.5 din 5 stele3.5/5 (2)
- Tugas MSCT Rhino 2 Scan Rikha FixDocument29 paginiTugas MSCT Rhino 2 Scan Rikha FixRikha LiemiyahÎncă nu există evaluări
- Kolestasis Intrahepatal Vs EkstrahepatalDocument4 paginiKolestasis Intrahepatal Vs EkstrahepatalrikarikaÎncă nu există evaluări
- Shock - Types Pathophysiology and Management: DR - Ravichandra Kumar Anaesthesia ResidentDocument64 paginiShock - Types Pathophysiology and Management: DR - Ravichandra Kumar Anaesthesia ResidentHarika BandaruÎncă nu există evaluări
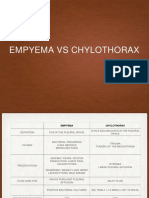
- EmpyemaDocument17 paginiEmpyemadeo_gratias14Încă nu există evaluări
- Correlation Between Body Mass Index and Intraocular Pressure at Eye Clinic Mangusada Hospital, BaliDocument3 paginiCorrelation Between Body Mass Index and Intraocular Pressure at Eye Clinic Mangusada Hospital, BaliKarina NathaniaÎncă nu există evaluări
- Refleksi Kasus IPE Dan IPECP - Sisilia Dwi Andini Putri 2020401163Document27 paginiRefleksi Kasus IPE Dan IPECP - Sisilia Dwi Andini Putri 2020401163Albinarta YanotamaÎncă nu există evaluări
- Nyeri FlankDocument15 paginiNyeri FlankMuhammad Thoriqur Rohman Al-KhotamiÎncă nu există evaluări
- Children With Henoch Schonlein Purpura 2.0Document13 paginiChildren With Henoch Schonlein Purpura 2.0soniaÎncă nu există evaluări
- Osteoartritis: Dr. Dewi Nur Fiana.,Sp - KFRDocument28 paginiOsteoartritis: Dr. Dewi Nur Fiana.,Sp - KFRgita cahayaÎncă nu există evaluări
- Hipertensi JNC 8Document7 paginiHipertensi JNC 8Elisse StephanieÎncă nu există evaluări
- n378.008 Iris Website Staging of CKD PDFDocument8 paginin378.008 Iris Website Staging of CKD PDFrutebeufÎncă nu există evaluări
- Vaginismus A Review of The Literature On The Classification Diagnosis, Etiology and Treatment TranslateDocument14 paginiVaginismus A Review of The Literature On The Classification Diagnosis, Etiology and Treatment TranslateErliana FaniÎncă nu există evaluări
- Pityriasis Rosea - Background, Pathophysiology, EtiologyDocument4 paginiPityriasis Rosea - Background, Pathophysiology, EtiologysyahrulroziÎncă nu există evaluări
- PDF Lecture 9 Benign Soft Tissue TumorsDocument131 paginiPDF Lecture 9 Benign Soft Tissue TumorsMuhammad Rizqi100% (1)
- CRS SolDocument25 paginiCRS SolDiga Ana RusfiÎncă nu există evaluări
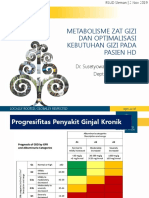
- Seminar HD-RSUD Sleman 2019Document36 paginiSeminar HD-RSUD Sleman 2019herkamaya100% (1)
- Djenkolism ToxificationDocument5 paginiDjenkolism ToxificationSilvia RizkaÎncă nu există evaluări
- Taping OA Genu Dr. SIsca Susantio, Sp. KFRDocument11 paginiTaping OA Genu Dr. SIsca Susantio, Sp. KFRDsk IndryÎncă nu există evaluări
- Responsi Stemi Dr. Tuko SP - JP FixDocument56 paginiResponsi Stemi Dr. Tuko SP - JP FixcintaÎncă nu există evaluări
- MataDocument163 paginiMataadelÎncă nu există evaluări
- Cara Hitung Jasa JKNDocument4 paginiCara Hitung Jasa JKNmuhammad iqbalÎncă nu există evaluări
- Operasi Monokular Recess Resect Dengan Teknik: Hangback Pada Exotropia Deviasi BesarDocument10 paginiOperasi Monokular Recess Resect Dengan Teknik: Hangback Pada Exotropia Deviasi BesarBlack Clover IdÎncă nu există evaluări
- Kurva Z Score WhoDocument21 paginiKurva Z Score WhoFenty IswarÎncă nu există evaluări
- 13 - 266fourniers Gangrene PDFDocument5 pagini13 - 266fourniers Gangrene PDFMochamad RizalÎncă nu există evaluări
- Referat Malaria SerebralDocument42 paginiReferat Malaria SerebralLivia HanisamurtiÎncă nu există evaluări
- Retinopati DiabetikDocument5 paginiRetinopati DiabetikMuhammad Afriadi HamdanÎncă nu există evaluări
- Hipertensi-Krisis Dr. HendroDocument35 paginiHipertensi-Krisis Dr. Hendroyudhagp100% (1)
- Disentri Et Causa Bacteria: Jl. Kutai Raya, Perumnas-3, Tangerang Kecamatan Curug, Kab. Tangerang, Provinsi Banten)Document14 paginiDisentri Et Causa Bacteria: Jl. Kutai Raya, Perumnas-3, Tangerang Kecamatan Curug, Kab. Tangerang, Provinsi Banten)Denny LeeÎncă nu există evaluări
- Tutorial SSWALFA by IDI SurabayaDocument6 paginiTutorial SSWALFA by IDI Surabayaaji100% (1)
- Patogenesis Dan Patofisiologi Carcinoma Mammae: Reproduc. Factors Lifesyle FactorsDocument4 paginiPatogenesis Dan Patofisiologi Carcinoma Mammae: Reproduc. Factors Lifesyle FactorsStefanus SanÎncă nu există evaluări
- Cataract 20surgery 2029 05 2008 131224024457 Phpapp01Document61 paginiCataract 20surgery 2029 05 2008 131224024457 Phpapp01Bboy ToonÎncă nu există evaluări
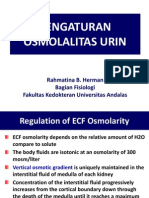
- Kuliah 3. Pengaturan Osmolalitas UrinDocument19 paginiKuliah 3. Pengaturan Osmolalitas UrinAnnisa DamayantiÎncă nu există evaluări
- Gir (Glucose Infussion Rate)Document9 paginiGir (Glucose Infussion Rate)arawindahaniastriÎncă nu există evaluări
- Asma Management 08 - 09 - 07Document81 paginiAsma Management 08 - 09 - 07botolkecapÎncă nu există evaluări
- Salter BAB 16Document126 paginiSalter BAB 16Yobbi Arissaputra100% (1)
- 1 - Perbandingan Teknik Endoscopic Third VentriculostomyDocument10 pagini1 - Perbandingan Teknik Endoscopic Third VentriculostomyKathryn TurnerÎncă nu există evaluări
- Disabilties and Deformities in Leprosy Seminar14!4!2017Document21 paginiDisabilties and Deformities in Leprosy Seminar14!4!2017Rohit GuptaÎncă nu există evaluări
- Casp RCT Checklist PDFDocument4 paginiCasp RCT Checklist PDFMaria TamarÎncă nu există evaluări
- Babygram PDFDocument22 paginiBabygram PDFArtikelWanitaDanKehamilanÎncă nu există evaluări
- Congenital Adrenal HyperplasiaDocument2 paginiCongenital Adrenal HyperplasiaesyÎncă nu există evaluări
- Abnormal Pupil, How To DoDocument8 paginiAbnormal Pupil, How To DoUNHAS OphthalmologyÎncă nu există evaluări
- Blighted OvumDocument4 paginiBlighted Ovummaria50% (2)
- Burat-Buret Echo Romi Revised PDFDocument2 paginiBurat-Buret Echo Romi Revised PDFAsma.denmiÎncă nu există evaluări
- Karakteristik Klinis Dan Hasil Implantasi Lensa Intra Okular Iris Claw Pada Kasus Afakia Di Rumah Sakit Mata Cicendo - Azalia LatuasanDocument10 paginiKarakteristik Klinis Dan Hasil Implantasi Lensa Intra Okular Iris Claw Pada Kasus Afakia Di Rumah Sakit Mata Cicendo - Azalia Latuasanwasobiru isbiruÎncă nu există evaluări
- Buku AJar Infeksi Dan Pediatrik Tropis IDAIDocument31 paginiBuku AJar Infeksi Dan Pediatrik Tropis IDAIAndika SiswantaÎncă nu există evaluări
- HDDocument23 paginiHDSardjitoÎncă nu există evaluări
- Basic Life Support (BLS) Support (Acls) : Dan Advance Cardiac LifeDocument27 paginiBasic Life Support (BLS) Support (Acls) : Dan Advance Cardiac LifeRuth AngeliaÎncă nu există evaluări
- Abdominal Pain in Children - Dr. Hermanto SP - BaDocument41 paginiAbdominal Pain in Children - Dr. Hermanto SP - Bajimmy_junÎncă nu există evaluări
- The Effect of Zinc Supplementation in Adult Patients With Acute Diarrhea PDFDocument5 paginiThe Effect of Zinc Supplementation in Adult Patients With Acute Diarrhea PDFAsrori AzharÎncă nu există evaluări
- Morning Report CKDDocument20 paginiMorning Report CKDjoe joeÎncă nu există evaluări
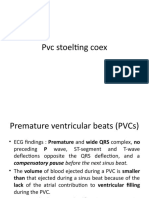
- PVC Stoelting Coex 1Document29 paginiPVC Stoelting Coex 1Rudy SiahaanÎncă nu există evaluări
- 11 - 206memahami DispareuniaDocument8 pagini11 - 206memahami DispareuniaResti Puteri Apriyuslim0% (1)
- HyperthyroidismDocument14 paginiHyperthyroidismDian JuliantyÎncă nu există evaluări
- Hypertiroid FixDocument11 paginiHypertiroid FixtiwiÎncă nu există evaluări
- American Thyroid Association Guidelines For Detection of Thyroid DysfunctionDocument5 paginiAmerican Thyroid Association Guidelines For Detection of Thyroid DysfunctionUdsanee SukpimonphanÎncă nu există evaluări
- 183 612 1 PBDocument10 pagini183 612 1 PBayu permata dewiÎncă nu există evaluări
- Hyperthyroidism UpToDateDocument19 paginiHyperthyroidism UpToDatepck846737Încă nu există evaluări
- Hyperthyroidism: Sudiarto, MNDocument21 paginiHyperthyroidism: Sudiarto, MNerikaÎncă nu există evaluări
- Thyroid ScoreDocument6 paginiThyroid ScoreleozdmÎncă nu există evaluări
- Thesis About My DadDocument8 paginiThesis About My Dadbsqxd5g1100% (1)
- Upper-Intermediate Family Warm-Up (Pair Work) : EsprimsDocument6 paginiUpper-Intermediate Family Warm-Up (Pair Work) : Esprimsهيفا 'ءÎncă nu există evaluări
- Chapter 5. Crim 3. JD JjsDocument10 paginiChapter 5. Crim 3. JD JjsgapoymackyÎncă nu există evaluări
- Is Maternal Depressive Symptomatology Effective On Success of Exclusive Breastfeeding During Postpartum 6 Weeks?Document6 paginiIs Maternal Depressive Symptomatology Effective On Success of Exclusive Breastfeeding During Postpartum 6 Weeks?Yessica Vega GolerÎncă nu există evaluări
- The Three Structures of PersonalityDocument60 paginiThe Three Structures of PersonalityHaydee Kristine A. Luzon - LabastillaÎncă nu există evaluări
- Gestational DiabetesDocument15 paginiGestational DiabetesAbdulJabar RiadhÎncă nu există evaluări
- English 7: First Quarter Worksheet No. 3 Reading IntensivelyDocument3 paginiEnglish 7: First Quarter Worksheet No. 3 Reading IntensivelyJerome BautistaÎncă nu există evaluări
- Territorial Profiles Montreal Lasalle 2019 2020Document3 paginiTerritorial Profiles Montreal Lasalle 2019 2020Artur NaÎncă nu există evaluări
- Mothers' Affect in The Homework Context: The Importance of Staying PositiveDocument11 paginiMothers' Affect in The Homework Context: The Importance of Staying Positivecool MsA-LÎncă nu există evaluări
- Unit 2: Disease Prevention: Pkids' Infectious Disease WorkshopDocument21 paginiUnit 2: Disease Prevention: Pkids' Infectious Disease WorkshopCharlene Fadrigon-OtazuÎncă nu există evaluări
- OBDocument9 paginiOBDennis ArevaloÎncă nu există evaluări
- Effectiveness of Biological Nurturing On Early Breastfeeding Problems: A Randomized Controlled TrialDocument10 paginiEffectiveness of Biological Nurturing On Early Breastfeeding Problems: A Randomized Controlled TrialevaÎncă nu există evaluări
- Sgpta Attendance 12Document1 paginăSgpta Attendance 12Cristyn B.BinadayÎncă nu există evaluări
- Postpartum PDFDocument6 paginiPostpartum PDFPatrícia OliveiraÎncă nu există evaluări
- Emotion Coaching - The StepsDocument2 paginiEmotion Coaching - The StepsJulie SharpÎncă nu există evaluări
- Blood Relations Questions Specially For Sbi Po PrelimsDocument15 paginiBlood Relations Questions Specially For Sbi Po Prelims3667 Kirandeep KaurÎncă nu există evaluări
- Unit 2 - Lesson 2Document3 paginiUnit 2 - Lesson 2Resyn Faye CortezÎncă nu există evaluări
- Wiktionary:Requested Entries (Hindi) /multilingual List of Indian Family Relation NamesDocument4 paginiWiktionary:Requested Entries (Hindi) /multilingual List of Indian Family Relation Namesshukla dhavalÎncă nu există evaluări
- Continental Steel Manufacturing Corporation v. Montano, G.R. No. 182836Document6 paginiContinental Steel Manufacturing Corporation v. Montano, G.R. No. 182836Daryl CruzÎncă nu există evaluări
- SSP113Document67 paginiSSP113Jay VaronaÎncă nu există evaluări
- MUHD ADLI - 2021470038 - RAP1203D - DRAFT EC EditDocument3 paginiMUHD ADLI - 2021470038 - RAP1203D - DRAFT EC EditMOHAMMAD FIRDAUS MOHAMMAD ZAMANIÎncă nu există evaluări
- Sexology: PrdgressinDocument603 paginiSexology: PrdgressinEmotyÎncă nu există evaluări
- Business Plan EditedDocument24 paginiBusiness Plan EditedEduardo Anerdez86% (14)
- Animal Behavior Practice SheetDocument5 paginiAnimal Behavior Practice SheetSelman PepeljakÎncă nu există evaluări
- NNJDocument20 paginiNNJLatifah AlsahaleyÎncă nu există evaluări
- Group 2 PR2Document19 paginiGroup 2 PR2Enzo JurozÎncă nu există evaluări
- Baguio City National High School Senior High School: ST STDocument5 paginiBaguio City National High School Senior High School: ST STTom AngÎncă nu există evaluări
- My ResumeDocument3 paginiMy Resumeapi-698893280Încă nu există evaluări
- 17.b. Digest Bartolome Vs SSSDocument2 pagini17.b. Digest Bartolome Vs SSSWhoopiJaneMagdozaÎncă nu există evaluări
- Child and Adolescent Development: (Source: Action For The Right of Children (ARC) .PDF)Document25 paginiChild and Adolescent Development: (Source: Action For The Right of Children (ARC) .PDF)June LegaspiÎncă nu există evaluări
- The Obesity Code: Unlocking the Secrets of Weight LossDe la EverandThe Obesity Code: Unlocking the Secrets of Weight LossEvaluare: 4 din 5 stele4/5 (6)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDe la EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityEvaluare: 4 din 5 stele4/5 (28)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDe la EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsÎncă nu există evaluări
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDe la EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeEvaluare: 2 din 5 stele2/5 (1)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDe la EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDEvaluare: 5 din 5 stele5/5 (2)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDe la EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionEvaluare: 4 din 5 stele4/5 (404)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDe la EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsEvaluare: 5 din 5 stele5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDe la EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisEvaluare: 4.5 din 5 stele4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDe la EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedEvaluare: 5 din 5 stele5/5 (81)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDe la EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsEvaluare: 3.5 din 5 stele3.5/5 (3)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDe la EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisEvaluare: 4 din 5 stele4/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDe la EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityEvaluare: 4 din 5 stele4/5 (3)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDe la EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningDe la EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningEvaluare: 4 din 5 stele4/5 (3)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)De la EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Încă nu există evaluări
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDe la EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisEvaluare: 3.5 din 5 stele3.5/5 (2)
- Gut: the new and revised Sunday Times bestsellerDe la EverandGut: the new and revised Sunday Times bestsellerEvaluare: 4 din 5 stele4/5 (392)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDe la EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryEvaluare: 4 din 5 stele4/5 (44)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.De la EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Evaluare: 4.5 din 5 stele4.5/5 (110)
- The Marshmallow Test: Mastering Self-ControlDe la EverandThe Marshmallow Test: Mastering Self-ControlEvaluare: 4.5 din 5 stele4.5/5 (58)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDe la EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessEvaluare: 4.5 din 5 stele4.5/5 (328)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingDe la EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingEvaluare: 4 din 5 stele4/5 (1138)
- Troubled: A Memoir of Foster Care, Family, and Social ClassDe la EverandTroubled: A Memoir of Foster Care, Family, and Social ClassEvaluare: 4.5 din 5 stele4.5/5 (27)