Documente Academic
Documente Profesional
Documente Cultură
NY State Trans Healthcare Regulation Dec. 2014
Încărcat de
housingworks0 evaluări0% au considerat acest document util (0 voturi)
257 vizualizări4 paginiNY State Trans Healthcare Regulation Dec. 2014
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentNY State Trans Healthcare Regulation Dec. 2014
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
257 vizualizări4 paginiNY State Trans Healthcare Regulation Dec. 2014
Încărcat de
housingworksNY State Trans Healthcare Regulation Dec. 2014
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 4
RULE MAKING
ACTIVITIES
Each rule making is identified by an I.D. No., which consists
of 13 characters. For example, the I.D. No.
AAM-01-96-00001-E indicates the following:
AAM
-the abbreviation to identify the adopting agency
01
-the State Register issue number
96
-the year
00001
-the Department of State number, assigned upon
receipt of notice.
E
-Emergency Rule Makingpermanent action
not intended (This character could also be: A
for Adoption; P for Proposed Rule Making; RP
for Revised Rule Making; EP for a combined
Emergency and Proposed Rule Making; EA for
an Emergency Rule Making that is permanent
and does not expire 90 days after filing.)
Italics contained in text denote new material. Brackets
indicate material to be deleted.
NOTICE OF ADOPTION
Certificate of Public Advantage
I.D. No. HLT-38-13-00007-A
Filing No. 985
Filing Date: 2014-12-02
Effective Date: 2014-12-17
PURSUANT TO THE PROVISIONS OF THE State Administrative Procedure Act, NOTICE is hereby given of the following action:
Action taken: Addition of Subpart 83-1 to Title 10 NYCRR.
Statutory authority: Public Health Law, section 2999-bb
Subject: Certificate of Public Advantage.
Purpose: For the health care industry to obtain reasonable protections
from antitrust liability through an active state oversight program.
Substance of final rule: The proposed rule would add a new Subpart 83-1
to 10 NYCRR titled Certificate of Public Advantage.
Section 83-1.1 Contains definitions for purposes of this Subpart, including definitions for Attorney General, Certificate of Public Advantage,
Cooperative Agreement, Federal or State Antitrust Laws, Health
Care Provider, Mental Hygiene Agency, Person, Planning Process
and Primary Service Area.
Section 83-1.2 Certificate of Public Advantage. Describes the effect of
obtaining a Certificate of Public Advantage (COPA) and sets forth the
basic contents of an application.
Section 83-1.3 Public notice. Provides for public notice of an application, by both the department and each party to the agreement or proposed
agreement for which approval is sought.
Section 83-1.4 Fees for applications and monitoring. Sets forth fees and
costs to be paid in relation to applications and renewals.
Section 83-1.5 Review process. Sets forth the factors to be considered
by the Department in its review of applications for a COPA.
Section 83-1.6 Issuance of a Certificate of Public Advantage. Provides
for consultation with the Attorney General, the mental hygiene agencies
(as appropriate), and the Public Health and Health Planning Council
(PHHPC) in the issuance of a COPA, sets forth examples of conditions
which may be imposed in the issuance of a COPA, and provides for the
period for which such COPA may be valid.
Section 83-1.7 Record keeping. Requires the Department to maintain a
record of all Cooperative Agreements for which COPAs are in effect and a
copy of the certificate, including any conditions imposed in it.
Section 83-1.8 Modification and termination. Provides that any material modification of an approved Cooperative Agreement is subject to the
prior review and approval of the Department in consultation with the Attorney General, mental hygiene agencies (as appropriate), and the PHHPC,
and that any party to a Cooperative Agreement covered by a COPA must
file notice of such termination with the Department at least thirty days
prior to the termination. The notice of termination will be provided by the
Department to the Attorney General and the mental hygiene agencies (as
appropriate).
Section 83-1.9 Periodic reports. Requires periodic filing of reports of
activity pursuant to a COPA, and sets forth the frequency and contents of
such reports.
Section 83-1.10 Review after issuance of Certificate of Public
Advantage. Provides for Department review of reports, and includes provisions addressing corrective measures the Department may take under
certain circumstances.
Section 83-1.11 Application for renewal. Provides for renewal of an approved COPA.
Section 83-1.12 Revocation. Provides for revocation of a COPA by the
Department under certain circumstances, and a procedure for doing so.
Section 83-1.13 Hearing rights. Provides for a right of hearing prior to
the Departments revocation of a COPA.
Section 83-1.14 Voluntary surrender. Allows for the voluntary surrender of a COPA.
Section 83-1.15 Effect of consultation or recommendations. Clarifies
treatment of input received pursuant to consultations with, or recommendations from, the Attorney General, mental hygiene agencies (as appropriate), or the PHHPC.
Section 83-1.16 Certificate of need and other requirements. Provides
that nothing in this Subpart shall relieve parties from any responsibility for
compliance with laws or regulations governing certificate of need or other
approval or notice submission requirements.
A copy of the full text of the regulatory proposal is available on the
Department of Health website (www.health.ny.gov).
Final rule as compared with last published rule: Nonsubstantive changes
were made in sections 83-1.1(c)(2), 83-1.2(b)(2) and (3).
Revised rule making(s) were previously published in the State Register
on August 27, 2014.
Text of rule and any required statements and analyses may be obtained
from: Katherine Ceroalo, DOH, Bureau of House Counsel, Reg. Affairs
Unit, Room 2438, ESP Tower Building, Albany, NY 12237, (518) 4737488, email: regsqna@health.ny.gov
Revised Regulatory Impact Statement, Revised Regulatory Flexibility
Analysis, Revised Rural Area Flexibility Analysis and Revised Job
Impact Statement
Changes made to the last published rule do not necessitate revision to the
previously published RIS, RFA, RAFA or JIS.
Assessment of Public Comment
A Notice of Proposed Rule Making was published in the State Register
on September 18, 2013. The proposed regulations were revised in light of
public comments received and a Notice of Revised Rule Making was
published in the State Register on August 27, 2014. During the public
comment period for the revised rulemaking, comments were received from
hospitals, hospital associations, health plan associations, and a bar
association. Clarifications and technical, non-substantive changes have
been made to the regulations in light of the comments received. The
regulations will take effect today pursuant to a Notice of Adoption filed in
Rule Making Activities
todays State Register. The full text of the regulations and Assessment of
Public Comment is available on the Department of Healths website.
All comments received were reviewed and evaluated. In response to
comments, section 83-1.1(c)(2) has been revised to clarify certain types of
transactions for which a COPA may be available. In addition, technical
clarifications were made to section 83-1.2(b)(2) and (3). As explained
below, other suggestions were not incorporated because they were inconsistent with the statutory authority underlying the proposed rulemaking or
concerned issues outside the scope of the proposed rulemaking.
A number of comments related to the intersection of the Certificate of
Public Advantage (COPA) and the Delivery System Reform Incentive
Payment (DSRIP). As noted in the comments and responses, the Department has indicated that Performing Provider Systems (PPSs) may submit
COPA applications along with their DSRIP Project Plan applications. In
response to a number of comments, the Department advises that it soon
will issue Frequently Asked Questions to assist PPSs in submitting COPA
applications which will address the matters raised.
A number of comments expressed concern about the Attorney Generals ability to seek retroactive enforcement of state antitrust laws, which
they assert is inconsistent with the statutory purpose underlying the COPA
regulations. In response, the Department notes that the proposed regulations achieve the statutes intent to provide state action immunity under
the state and federal antitrust laws for collaborative arrangements that
promote improved quality, efficiency of and access to health care services
through the COPA process, while preserving the Attorney Generals
authority as authorized by law.
The Assessment of Public Comment is available on the Department of
Healths website at www.health.ny.gov.
PROPOSED RULE MAKING
NO HEARING(S) SCHEDULED
Transgender Related Care and Services
I.D. No. HLT-50-14-00001-P
PURSUANT TO THE PROVISIONS OF THE State Administrative Procedure Act, NOTICE is hereby given of the following proposed rule:
Proposed Action: Amendment of section 505.2(l) of Title 18 NYCRR.
Statutory authority: Public Health Law, sections 201 and 206; and Social
Services Law, sections 363-a and 365-a(2)
Subject: Transgender Related Care and Services.
Purpose: To authorize Medicaid coverage for transgender related care and
services.
Text of proposed rule: Subdivision (l) of section 505.2 is repealed and a
new subdivision (l) is added to read as follows:
(l) Gender dysphoria treatment. As provided in this subdivision, payment is available for medically necessary hormone therapy and/or gender
reassignment surgery for the treatment of gender dysphoria.
(2) Hormone therapy, whether or not in preparation for gender reassignment surgery, may be covered for individuals 18 years of age or older.
(3) Gender reassignment surgery may be covered for an individual
who is 18 years of age or older, or 21 years of age or older if the surgery
will result in sterilization, and has letters from two qualified New York
State licensed health professionals who have independently assessed the
individual and are referring the individual for the surgery. One of these
letters must be from a psychiatrist or psychologist with whom the individual has an established and ongoing relationship. The other letter may be
from a licensed psychiatrist, psychologist, physician or licensed clinical
social worker acting within the scope of his or her practice, who has only
had an evaluative role with the individual. Together, the letters must establish that the individual:
(i) has a persistent and well-documented case of gender dysphoria;
(ii) has received hormone therapy appropriate to the individual's
gender goals, which shall be for a minimum of 12 months in the case of an
individual seeking genital surgery, unless such therapy is medically
contraindicated or the individual is otherwise unable to take hormones;
(iii) has lived for 12 months in a gender role congruent with the
individuals gender identity, and has received mental health counseling,
as deemed medically necessary, during that time;
(iv) has no other significant medical or mental health conditions
that would be a contraindication to gender reassignment surgery, or if so,
that those are reasonably well-controlled prior to the gender reassignment surgery; and
(v) has the capacity to make a fully informed decision and to
consent to the treatment.
(4) Payment will not be made for the following services and
procedures:
NYS Register/December 17, 2014
(i) cryopreservation, storage, and thawing of reproductive tissue,
and all related services and charges;
(ii) reversal of genital and/or breast surgery;
(iii) reversal of surgery to revise secondary sex characteristics;
(iv) reversal of any procedure resulting in sterilization; and
(v) cosmetic surgery, services, and procedures, including but not
limited to:
(a) abdominoplasty, blepharoplasty, neck tightening, or removal
of redundant skin;
(b) breast augmentation;
(c) breast, brow, face, or forehead lifts;
(d) calf, cheek, chin, nose, or pectoral implants;
(e) collagen injections;
(f) drugs to promote hair growth or loss;
(g) electrolysis, unless required for vaginoplasty;
(h) facial bone reconstruction, reduction, or sculpturing, including jaw shortening and rhinoplasty;
(i) hair transplantation;
(j) lip reduction;
(k) liposuction;
(l) thyroid chondroplasty; and
(m) voice therapy, voice lessons, or voice modification surgery.
(5) For purposes of this subdivision, cosmetic surgery, services, and
procedures refers to anything solely directed at improving an individuals
appearance.
(6) All legal and program requirements related to providing and claiming reimbursement for sterilization procedures must be followed when
transgender care involves sterilization.
Text of proposed rule and any required statements and analyses may be
obtained from: Katherine Ceroalo, DOH, Bureau of House Counsel, Reg.
Affairs Unit, Room 2438, ESP Tower Building, Albany, NY 12237, (518)
473-7488, email: regsqna@health.ny.gov
Data, views or arguments may be submitted to: Same as above.
Public comment will be received until: 45 days after publication of this
notice.
This rule was not under consideration at the time this agency submitted
its Regulatory Agenda for publication in the Register.
Regulatory Impact Statement
Statutory Authority:
Social Services Law (SSL) section 363-a and Public Health Law section 201(1)(v) provide that the Department is the single State agency
responsible for supervising the administration of the States medical assistance (Medicaid) program and for adopting such regulations, which
shall be consistent with law, and as may be necessary to implement the
States Medicaid program. SSL section 365-a authorizes Medicaid coverage for specified medical care, services and supplies, together with such
medical care, services and supplies as authorized in the regulations of the
Department.
Legislative Objective:
Section 365-a of the SSL requires Medicaid to pay for part or all of the
cost of medical, dental, and remedial care, services, and supplies that are
necessary to prevent, diagnose, correct or cure conditions that cause acute
suffering, endanger life, result in illness or infirmity, interfere with a
person's capacity for normal activity, or threaten some significant
handicap.
Needs and Benefits:
The proposed regulations would change Medicaid policy with respect
to payment for treatments to address gender dysphoria. Gender dysphoria
is the diagnosis given to persons whose gender at birth is contrary to the
one they identify with, and who experience clinically significant distress
as a result. Gender dysphoria may be manifested by a strong desire to be
treated as the other gender or to be rid of ones sex characteristics, or by a
strong conviction that one has feelings and reactions typical of the other
gender.
Treatments for gender dysphoria include counseling, hormone therapy,
and gender reassignment surgery. Gender reassignment surgery (GRS) is
a term for the surgical procedures by which the physical appearance and
function of a persons existing sexual characteristics are altered to
resemble those of the other sex.
Section 505.2(l) of 18 NYCRR, related to Medicaid payment for physicians services, currently prohibits payment for any care, services, drugs,
or supplies rendered in connection with GRS. At the time the regulation
was originally promulgated in 1998, there was a lack of consensus regarding the safety and efficacy of GRS, and many health care payers, including the federal Medicare program, considered it an experimental procedure requiring further long-term study.
Since that time, a body of credible medical evidence has been developed
supporting the conclusion that GRS is a safe and effective treatment for
gender dysphoria in medically necessary cases, and is no longer considered
NYS Register/December 17, 2014
experimental. Significantly, in May of 2014, the Federal Government
through the Departmental Appeals Board of the Department of Health and
Human Services ruled that Medicare could no longer deny coverage of
GRS on the grounds that it is it is ineffective, unsafe, experimental, or
controversial, that it has a high rate of complication or has not been
subjected to controlled, long-term studies, or that the criteria for diagnosing gender dysphoria is inconsistent or problematic.
Given these developments, the Department is updating its Medicaid
coverage policy. The proposed amendments would repeal the existing text
of section 505.2(l) and replace it with a description of the express
parameters within which the Medicaid program would now cover hormone
therapy and/or GRS for the treatment of gender dysphoria.
Hormone therapy prescribed for adults with gender dysphoria would
now be covered whether or not in preparation for GRS.
GRS would now be covered for persons who are referred for the treatment by two New York State licensed health professionals acting within
the scope of their practices. The minimum age for coverage would be 18
years of age unless the GRS would result in sterilization, in which case
federal Medicaid rules require a minimum age of 21. The health professionals would have to provide letters stating that the patient: has a persistent and well-documented case of gender dysphoria; has received hormone
therapy appropriate to the patients gender goals, which shall be for a minimum of 12 months in the case of genital surgery, unless such therapy is
medically contradicted or the patient is unable to take hormones; has lived
for 12 months in a gender role consistent with the individuals gender
identity and has received mental health counseling, as deemed medically
necessary, during that time; has no other significant medical or mental
health conditions that would be a contraindication to GRS, or any such
conditions are reasonably well-controlled; and has the capacity to provide
informed consent for the treatment.
Medicaid would not pay to reverse gender reassignment surgeries or
sterilization procedures. Further, Medicaid would not pay for the cryopreservation, storage, or thawing of reproductive tissue. Finally, Medicaid
would not pay for cosmetic services and procedures that are solely directed
at improving the patients appearance. The proposed amendments list services and procedures that would generally be considered cosmetic and
ancillary to the GRS, and therefore not medically necessary.
Costs:
Costs to Regulated Parties:
The proposed amendment would add a new covered benefit under the
States Medicaid program. The amendment would not increase costs to
regulated parties.
Costs to State Government:
Adding coverage of transgender care and services to the Medicaid benefit package will increase costs to the State. To estimate these costs, the
Department looked at the number of Medicaid recipients who receive
mental health services based on a diagnosis of gender dysphoria (currently
353 natal males and 308 natal females). The Department estimated the
percentage of natal males and natal females who would seek hormone
therapy only, partial GRS, or full GRS. Then, using typical costs for the
types of care and services that would be implicated (including mental
health counseling, hormone therapy, laboratory services, and surgeries
specific to male-to-female and female-to-male reassignment), the Department calculated the total, annual State share of expenditures related to the
expansion of coverage for transgender care and services to be approximately $6,737,000.
Costs to Local Governments:
Local social services districts share of Medicaid costs is statutorily
capped; therefore, there will be no additional costs to local governments
as a result of the proposed amendment.
Costs to the Department of Health:
There will be no additional costs to the Department.
Local Government Mandates:
This amendment will not impose any program, service, duty, additional
cost, or responsibility on any county, city, town, village, school district,
fire district, or other special district.
Paperwork:
In order to perform and claim Medicaid reimbursement for GRS, physicians would have to receive letters from two qualified mental health
professionals who independently assessed the patient and are referring
him or her for the surgery. One of these letters would be from the patients
psychotherapist, with whom the patient has an established and ongoing
relationship. The other letter could be from a mental health professional
who has only had an evaluative role with the patient. These letters would
need to establish that the patient meets the prerequisites set forth in the
regulation for the surgery.
Duplication:
There are no duplicative or conflicting rules identified.
Alternatives:
Alternatives to the proposed amendment would not comply with exist-
Rule Making Activities
ing New York law and current medical science. Specifically, one alternative to the proposed amendment would be to maintain the current prohibition on Medicaid payment for care, services, drugs, or supplies rendered
in connection with GRS. However, SSL section 365-a authorizes Medicaid
payment for medically necessary care to correct or cure conditions that
can cause acute suffering and interfere with a persons capacity for normal
activity, a criterion that gender dysphoria meets.
Another alternative would be to provide coverage for all services and
procedures performed in connection with gender reassignment, even services and procedures that are solely cosmetic. However, federal and State
law limit Medicaid coverage to payment solely for medically necessary
care, services, and supplies. Therefore the Department is required to make
a distinction between surgical procedures that are primary to gender reassignment, and thus medically necessary and coverable, and procedures
performed solely for cosmetic reasons, which are not. This is consistent
with the States broader Medicaid coverage policy, which prohibits coverage of cosmetic procedures for Medicaid recipients.
Federal Standards:
The proposed regulations do not exceed any minimum federal standards.
Compliance Schedule:
Regulated parties should be able to comply with the proposed regulations when they become effective.
Regulatory Flexibility Analysis
No regulatory flexibility analysis is required pursuant to section 202(b)(3)(a) of the State Administrative Procedure Act. The proposed amendment would add a new covered benefit under the States Medicaid
program. It would not impose an adverse economic impact on small businesses or local governments, and it would not impose reporting, record
keeping or other compliance requirements on small businesses or local
governments.
Rural Area Flexibility Analysis
A Rural Area Flexibility Analysis for the proposed amendment is not being submitted because the amendment would not impose any adverse
impact or significant reporting, record keeping or other compliance
requirements on public or private entities in rural areas. There would be
no professional services, capital, or other compliance costs imposed on
public or private entities in rural areas as a result of the proposed
amendments.
Job Impact Statement
A Job Impact Statement for the proposed amendment is not being submitted because it is apparent from the nature and purpose of the amendment
that it would not have a substantial adverse impact on jobs and/or employment opportunities.
Office of Mental Health
NOTICE OF ADOPTION
Clinic Treatment Programs
I.D. No. OMH-40-14-00007-A
Filing No. 977
Filing Date: 2014-12-02
Effective Date: 2014-12-17
PURSUANT TO THE PROVISIONS OF THE State Administrative Procedure Act, NOTICE is hereby given of the following action:
Action taken: Amendment of Part 599 of Title 14 NYCRR.
Statutory authority: Mental Hygiene Law, sections 7.09, 31.04, 43.01 and
43.02; Social Services Law, sections 364, 364-a and 364-j
Subject: Clinic Treatment Programs.
Purpose: Adjust billing units associated with reimbursement of clinic services; allow flexibility in delivery of complex care management.
Text or summary was published in the October 8, 2014 issue of the Register, I.D. No. OMH-40-14-00007-P.
Final rule as compared with last published rule: No changes.
Text of rule and any required statements and analyses may be obtained
from: Sue Watson, NYS Office of Mental Health, 44 Holland Avenue,
Albany, NY 12229, (518) 474-1331, email: Sue.Watson@omh.ny.gov
Assessment of Public Comment
The agency received no public comment.
Rule Making Activities
Office for People with
Developmental Disabilities
NOTICE OF ADOPTION
HCBS Waiver Community Habilitation Services
I.D. No. PDD-41-14-00006-A
Filing No. 978
Filing Date: 2014-12-02
Effective Date: 2014-12-17
PURSUANT TO THE PROVISIONS OF THE State Administrative Procedure Act, NOTICE is hereby given of the following action:
Action taken: Amendment of Subpart 635-10 of Title 14 NYCRR.
Statutory authority: Mental Hygiene Law, sections 13.07, 13.09(b) and
16.00
Subject: HCBS Waiver Community Habilitation Services.
Purpose: To amend proposed Community Habilitation regulations that
were adopted on October 1, 2014.
Text or summary was published in the October 15, 2014 issue of the Register, I.D. No. PDD-41-14-00006-EP.
Final rule as compared with last published rule: No changes.
Text of rule and any required statements and analyses may be obtained
from: Regulatory Affairs Unit, OPWDD, 44 Holland Avenue, 3rd Floor,
Albany, NY 12229, (518) 474-1830, email: rau.unit@opwdd.ny.gov
Additional matter required by statute: Pursuant to the requirements of the
State Environmental Quality Review Act, OPWDD, as lead agency, has
determined that the action described herein will have no effect on the
environment, and an E.I.S is not needed.
Assessment of Public Comment
The agency received no public comment.
NYS Register/December 17, 2014
S-ar putea să vă placă și
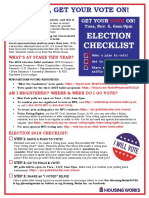
- Housing Works "What's Your Voting Plan?!" Sheet 2018Document1 paginăHousing Works "What's Your Voting Plan?!" Sheet 2018housingworksÎncă nu există evaluări
- NYC World AIDS Day 2015 Coalition Event SaveTheDate Flyer EnglishDocument1 paginăNYC World AIDS Day 2015 Coalition Event SaveTheDate Flyer EnglishhousingworksÎncă nu există evaluări
- End AIDS NY 2020 Coalition, World AIDS Day 2018 Resources ListingDocument3 paginiEnd AIDS NY 2020 Coalition, World AIDS Day 2018 Resources ListinghousingworksÎncă nu există evaluări
- Housing Works Get Out The Vote, Election Day 2018 Fact SheetDocument1 paginăHousing Works Get Out The Vote, Election Day 2018 Fact SheethousingworksÎncă nu există evaluări
- #ICantBreathe/ Dec. 2014-Jan. 2015 Calls-to-Action Flyer, Housing Works Advocacy ActionsDocument2 pagini#ICantBreathe/ Dec. 2014-Jan. 2015 Calls-to-Action Flyer, Housing Works Advocacy ActionshousingworksÎncă nu există evaluări
- Civil Society and Communities Declaration To End HIV: Human Rights Must Come FirstDocument7 paginiCivil Society and Communities Declaration To End HIV: Human Rights Must Come FirsthousingworksÎncă nu există evaluări
- New York State Ending The AIDS Epidemic Blueprint Summary One-SheetDocument2 paginiNew York State Ending The AIDS Epidemic Blueprint Summary One-SheethousingworksÎncă nu există evaluări
- 2018 NYC LGBT March Route MapDocument1 pagină2018 NYC LGBT March Route MaphousingworksÎncă nu există evaluări
- Housing Works Get Out The Vote Election Day 2017Document1 paginăHousing Works Get Out The Vote Election Day 2017housingworksÎncă nu există evaluări
- Hillary Clinton Agenda and Meeting Notes 5.12.16Document9 paginiHillary Clinton Agenda and Meeting Notes 5.12.16Housing WorksÎncă nu există evaluări
- DOHMH Notes On Gov Exec Budget, 2.8.17Document2 paginiDOHMH Notes On Gov Exec Budget, 2.8.17housingworksÎncă nu există evaluări
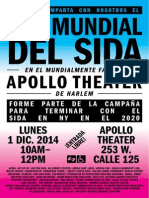
- NYC World AIDS Day Coalition Program, 12-1-14, Harlem's World Famous ApolloDocument4 paginiNYC World AIDS Day Coalition Program, 12-1-14, Harlem's World Famous ApollohousingworksÎncă nu există evaluări
- Housing Works April 2017 Town Hall Call-to-ActionDocument2 paginiHousing Works April 2017 Town Hall Call-to-ActionhousingworksÎncă nu există evaluări
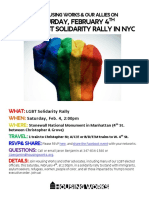
- NYC LGBT Solidarity Rally Flyer For 2 4 17 ExternalDocument1 paginăNYC LGBT Solidarity Rally Flyer For 2 4 17 ExternalhousingworksÎncă nu există evaluări
- May 2016 AIDS Advocates Consensus Policy Paper W EndorsersDocument17 paginiMay 2016 AIDS Advocates Consensus Policy Paper W EndorsershousingworksÎncă nu există evaluări
- AIDS - Free USA 2025 Indiv Sign-On Petition For 2016 Prez Candidates (Download Copy)Document2 paginiAIDS - Free USA 2025 Indiv Sign-On Petition For 2016 Prez Candidates (Download Copy)housingworksÎncă nu există evaluări
- Media Advisory 10.27 AIDS Community Press Conf RE Cuomo Ebola Quarantine FINALDocument1 paginăMedia Advisory 10.27 AIDS Community Press Conf RE Cuomo Ebola Quarantine FINALhousingworksÎncă nu există evaluări
- Housing Works World AIDS Day 2014 CoalitionEvent FlyerSaveTheDate, EnglishDocument1 paginăHousing Works World AIDS Day 2014 CoalitionEvent FlyerSaveTheDate, EnglishhousingworksÎncă nu există evaluări
- Housing Works Trans Day of Rememberance 2014 Event FlyerDocument1 paginăHousing Works Trans Day of Rememberance 2014 Event FlyerhousingworksÎncă nu există evaluări
- Quarantine - Leadership Letter FINAL 10 26 14Document6 paginiQuarantine - Leadership Letter FINAL 10 26 14housingworksÎncă nu există evaluări
- Nigerian LGBTers Invite To 1/12/15 Veil of Silence Doc ScreeningDocument1 paginăNigerian LGBTers Invite To 1/12/15 Veil of Silence Doc ScreeninghousingworksÎncă nu există evaluări
- Housing Works World AIDS Day 2014 CoalitionEvent FlyerSaveTheDate, SpanishDocument1 paginăHousing Works World AIDS Day 2014 CoalitionEvent FlyerSaveTheDate, SpanishhousingworksÎncă nu există evaluări
- Undetectables Project September 2014 2Document11 paginiUndetectables Project September 2014 2housingworksÎncă nu există evaluări
- Task Force End of AIDS NYS, Opening Remarks, 10.14.14, CKingDocument3 paginiTask Force End of AIDS NYS, Opening Remarks, 10.14.14, CKinghousingworksÎncă nu există evaluări
- Braking AIDS Ride 2014. 9/12-9/14, Cheering Stations GuideDocument1 paginăBraking AIDS Ride 2014. 9/12-9/14, Cheering Stations GuidehousingworksÎncă nu există evaluări
- 2014 IBJ JusticeMakers Award Applications LetterDocument2 pagini2014 IBJ JusticeMakers Award Applications LetterhousingworksÎncă nu există evaluări
- Harrison - Brooklyn ONAP Presentation 8.8.14Document15 paginiHarrison - Brooklyn ONAP Presentation 8.8.14housingworksÎncă nu există evaluări
- O'Connell and Feldman - Manhattan ONAP Presentation 8.7.14Document9 paginiO'Connell and Feldman - Manhattan ONAP Presentation 8.7.14housingworksÎncă nu există evaluări
- Harrison - Brooklyn ONAP Presentation 8.8.14Document15 paginiHarrison - Brooklyn ONAP Presentation 8.8.14housingworksÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Cot DLP Science 6-Simple Machines With AnnotationsDocument9 paginiCot DLP Science 6-Simple Machines With AnnotationsChii Chii100% (21)
- Department of Education: Accomplishment Report On Project Reap (Reading Enhancement Activities For Pupils) S.Y. 2021-2022Document4 paginiDepartment of Education: Accomplishment Report On Project Reap (Reading Enhancement Activities For Pupils) S.Y. 2021-2022Louisse Gayle AntuerpiaÎncă nu există evaluări
- Research into Coma, Esdaile and Sichort States offers New InsightsDocument10 paginiResearch into Coma, Esdaile and Sichort States offers New Insightscoach rismanÎncă nu există evaluări
- Counselling Skills and Techniques GuideDocument29 paginiCounselling Skills and Techniques GuideWanda Lywait100% (1)
- ResearchDocument41 paginiResearchAngel82% (11)
- Sample Chapter - The Ultimate EU Test Book 2013 Administrator (AD) Edition - FreeDocument31 paginiSample Chapter - The Ultimate EU Test Book 2013 Administrator (AD) Edition - FreeAndras Baneth0% (2)
- Communication & Emotional IntelligenceDocument22 paginiCommunication & Emotional IntelligenceRaghuram Bhandari100% (1)
- Definition of Terms: Maed-FilipinoDocument14 paginiDefinition of Terms: Maed-FilipinoMarceline Ruiz0% (1)
- Test Bank in Edcon2: Social Dimension of EducationDocument20 paginiTest Bank in Edcon2: Social Dimension of EducationPaul john caguingÎncă nu există evaluări
- Writing A Concept Paper 190319200413Document24 paginiWriting A Concept Paper 190319200413Julieto Sumatra JrÎncă nu există evaluări
- ADEC - International Community Branch 2016-2017Document23 paginiADEC - International Community Branch 2016-2017Edarabia.comÎncă nu există evaluări
- 10 Sales TechDocument9 pagini10 Sales TechHamdy AlyÎncă nu există evaluări
- Reading and Writing 4 Q: Skills For Success Unit 4 Student Book Answer KeyDocument3 paginiReading and Writing 4 Q: Skills For Success Unit 4 Student Book Answer KeyPoornachandra50% (2)
- OYH Assessment ManualDocument53 paginiOYH Assessment ManualLizPattison9275% (12)
- Ian Angel B. Osnan BECED III Ece 13: Science in Early Childhood Education Faculty: Ms. Dachel LaderaDocument4 paginiIan Angel B. Osnan BECED III Ece 13: Science in Early Childhood Education Faculty: Ms. Dachel LaderaWowie OsnanÎncă nu există evaluări
- Math Grade 7 DLL Q2 W1Document3 paginiMath Grade 7 DLL Q2 W1thalia alfaroÎncă nu există evaluări
- Develop Competency Based Learning MaterialsDocument33 paginiDevelop Competency Based Learning MaterialsEm Boquiren Carreon0% (1)
- Leiter-3 Manual P 46 Corrected SecondsDocument1 paginăLeiter-3 Manual P 46 Corrected SecondsDidenko MarinaÎncă nu există evaluări
- MonologuesDocument7 paginiMonologuesJiggy Derek Mercado0% (2)
- How To Lift Depression Quickly and SafelyDocument4 paginiHow To Lift Depression Quickly and SafelyHuman Givens Publishing Official50% (2)
- Teacher Interview ResponseDocument6 paginiTeacher Interview Responseapi-163091177Încă nu există evaluări
- Patient Centred Leadership in PracticeDocument11 paginiPatient Centred Leadership in Practicerafskall100% (1)
- Aleppo SyriaDocument3 paginiAleppo SyriaKimÎncă nu există evaluări
- New TermDocument97 paginiNew TermEthan PhilipÎncă nu există evaluări
- MAPEH G08 1st Periodical TestDocument3 paginiMAPEH G08 1st Periodical TestDana Reyes100% (2)
- Hello LoveDocument7 paginiHello LoveKrisTin Magbanua Jocson100% (3)
- Teacher Talk and Learner TalkDocument9 paginiTeacher Talk and Learner TalkWong Choy WanÎncă nu există evaluări
- Math 4 Week 6Document10 paginiMath 4 Week 6Julie Ann UrsulumÎncă nu există evaluări
- Patient Safety and Quality Care MovementDocument9 paginiPatient Safety and Quality Care Movementapi-300362983Încă nu există evaluări
- Ratan Tata and His Enterprising SkillsDocument10 paginiRatan Tata and His Enterprising Skillsstarbb100% (1)