Documente Academic
Documente Profesional
Documente Cultură
CBCT Dosimetry: Orthodontic Considerations
Încărcat de
griffone1Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
CBCT Dosimetry: Orthodontic Considerations
Încărcat de
griffone1Drepturi de autor:
Formate disponibile
CBCT Dosimetry: Orthodontic Considerations
Sharon L. Brooks
This article reviews the general principles of radiation biology and dose
measurement. Effective doses for typical imaging examinations used in
orthodontics include: panoramic, 5.5 to 22 microsieverts (Sv); cephalometric, 2.4 to 6.2 Sv; large field-of-view cone beam CT, 58.9 to 1025.4 Sv. This
can be compared with average annual natural background radiation of 3000
Sv/yr. Issues of radiation risk, particularly for children, as well as mechanisms
for dose reduction are discussed. (Semin Orthod 2009;15:14-18.) 2009 Elsevier
Inc. All rights reserved.
he discovery of x-rays more than 100 years
ago brought about an era of increased
diagnostic capability in the healing arts. As
technology improved, clinicians moved from
simple bitewing and periapical intraoral radiographs to larger, more complex extraoral
views. It is hard to imagine an orthodontic
office today that does not use panoramic and
cephalometric radiographs to help make a
thorough assessment of the orthodontic patient before beginning treatment. Today many
orthodontic offices are substituting cone beam
computed tomography (CBCT) images for the
traditional orthodontic views for all patients,
while others are adding this type of imaging
only in specific types of cases, such as those
with impacted canines or requiring orthognathic surgery. It is expected that the use of
CBCT in orthodontics, as well as in other dental specialties, will continue to grow at a rapid
rate, bringing up the question about the radiation dose required for this type of imaging
and whether it is justified.
It did not take long after the discovery of
x-rays for the first reports of radiation injury to
From the University of Michigan School of Dentistry, Ann
Arbor, MI.
Address correspondence to Sharon L. Brooks, DDS, MS, University of Michigan School of Dentistry, Department of Periodontics and
Oral Medicine, 1011 N. University Avenue, Ann Arbor, MI 481091078. Phone: 734-764-1595; Fax: 734-764-2469; E-mail: slbrooks@
umich.edu
2009 Elsevier Inc. All rights reserved.
1073-8746/09/1501-0$30.00/0
doi:10.1053/j.sodo.2008.09.002
14
appear. Of course, the dose levels in the early
days were very high and the equipment not very
good, but there were numerous reports of radiation burns and the induction of cancer. One of
the pioneers of dental radiology, Dr. C. Edmund
Kells, developed cancer on his hands and arms,
due to prolonged exposure to the x-ray beam,
which led to more and more surgery and his
eventual suicide.1
Because we no longer use the very high doses
of the past, it is unlikely that we will ever see the
types of radiation injuries also seen in the past.
However, does that mean that there is no risk of
biological damage from the doses currently in
use? If the answer to that question is no, can we
measure the magnitude of the risk and then
make a judgment about whether this level of risk
is acceptable or not?
It has been observed for many years that
groups of individuals who received radiation exposure for a variety of conditions showed an
elevated risk of developing cancer.2 In the past
radiation was used to treat ankylosing spondylitis, a type of arthritis, postchildbirth mastitis, and
tonsillitis, among other conditions, which increased incidence of leukemia, breast cancer,
and thyroid cancer, respectively, leading to the
discontinuation of this practice. These groups of
patients, along with the large number of people
living in the Japanese cities of Hiroshima and
Nagasaki at the time of the dropping of the
atomic bomb at the end of World War II, make
up the population that has been studied to determine the relationship between radiation and
cancer.
Seminars in Orthodontics, Vol 15, No 1 (March), 2009: pp 14-18
CBCT Dosimetry
Much of the information we have on radiation
risks is based on a careful epidemiologic analysis of
these populations, looking at radiation doses received and radiation effects observed. Mathematical models were then developed to try to explain
the observations. Because the information is incomplete for all dose levels, there is some uncertainty in the exact shape of the dose-response
curve. However, even though the exact risk is
not known, there is little doubt that radiation
has an effect on the human body even at low
doses.
It is well known that radiation is a carcinogen,
along with various chemicals, viruses, and probably other entities. X-rays striking the nucleus of
a cell can disrupt cell mitosis and damage DNA,
leading to mutations that can be passed on to
future generations of the same cells (somatic
mutation) or to future offspring (genetic mutation). Some of the mutations may be lethal,
leading to cell death, some may modify the function of the cell to a lesser or greater degree,
perhaps by affecting the production of enzymes,
and some may change the cell enough to induce
cancer, when coupled with other initiator or
promoter entities.
The body has some DNA repair mechanisms
available, but these may not be sufficient to repair all DNA breaks, particularly if they occur in
both strands or if large pieces of the DNA are
removed or rearranged. Thus, the nonrepaired
damage can accumulate in the body.
There are many varieties of radiation-associated effects that can occur in the body. In one
type, described as deterministic, there appears
to be no damage until a certain threshold of
radiation is received. Once beyond the threshold, the severity of the damage is proportional to
the radiation dose. Examples of this type of effect include skin reddening, hair loss, and salivary gland dysfunction.
Other types of radiation effects, most notably
carcinogenesis and genetic mutations, are examples of stochastic effects, in which there is no
threshold for radiation damage but where the
probability of an effect is proportional to the
radiation dose. In this situation, it is possible that
a single hit of radiation can produce a nonrepaired mutation of the DNA that can lead to
cancer several years in the future. There is no
guarantee that the subject will ever develop cancer as a result of the radiation, but the more
15
radiation that is received, the more chances that
something will occur.
Not all cells in the body have the same degree
of sensitivity to radiation. In general, cells that
are dividing rapidly over several generations, are
primitive or immature, and are nonspecialized
are at higher risk for radiation effects due to the
impact of radiation on DNA and cell division.
Children are considered to be more sensitive to
radiation than adults, an issue in orthodontic
imaging due to the high proportion of children
in an orthodontic practice.
General Principles of Radiation
Dosimetry
To evaluate radiation risks from various imaging
techniques, radiation doses must be measured.
It is relatively easy for a health physicist to place
an ionization chamber in the x-ray beam used
for intraoral and cephalometric radiography
and determine the amount of radiation that
strikes the patient, but unfortunately, this procedure does not make it easy or even possibleto compare radiation doses for the various
imaging examinations. For example, in panoramic radiographs and CBCT imaging, the xray beam moves around the patients head, partially or totally, depending on technique, and
different parts of the anatomy receive different
amounts of radiation, depending on their location with respect to the center of rotation. The
surface exposure, while easy to measure, also
does not take into account the size of the radiation beam or the radiosensitivity of the tissues
exposed.
To allow a meaningful comparison of radiation dose, and thus risk, radiation exposures are
frequently converted to effective doses, measured in Sieverts (Sv or milli- [mSv] or micro[Sv]). In the calculation, the radiation dose to
specific tissues is measured, adjusted for amount
of that tissue in the field of view, and weighted
based on radiation sensitivity of the tissue. The
weighted tissue/organ doses are then summed
to produce the effective dose. This could be
thought simplistically as a weighted average of the
dose over the entire body. When this is done, the
dose for various imaging techniques can be compared. Comparisons can also be done with other
whole body doses, such as background radiation.
16
S.L. Brooks
The tissues/organs used to calculate the effective dose are specified by the International
Commission on Radiological Protection (ICRP).
While ICRP is an international advisory group,
which does not have force of law, its recommendations are accepted worldwide and form the
basis for much of radiation protection.
The organs used to calculate effective dose
for imaging of the head include the bone marrow, thyroid, esophagus, skin, bone surface, salivary glands, brain, and remainder tissues.3,4
The dose to the thyroid contributes the most to
the effective dose from dental imaging, but salivary glands, even though they have a lower
weighting factor, are also a significant component of the effective dose due to their location in
the field of view.
Typical Orthodontic Radiation Doses
Effective radiation doses for various imaging examinations used in orthodontic practice have
been calculated and published in the literature.
In general, there is little difference in the dose
for digital panoramic and cephalometric images
compared with their film-based counterparts, in
large measure due to the use of intensifying
screens with the film imaging that reduces the
required dose. The situation is not the same for
intraoral imaging, in which the digital images
are compared with direct exposure film that
requires a higher exposure.
Effective doses in the literature are expressed
using one of two ICRP criteria: the 1990 report3
or the 2007 report4 (available earlier in draft
form), with the major difference being in the
handling of dose to the salivary glands. In the
earlier report the salivary glands were considered as part of the remainder organs and as
such received a low weighting. In the 2007 report the salivary glands have been removed from
the remainder and have their own weighting.
Because the salivary glands receive a relatively
large dose in dental imaging, due to their location, considering them separately leads to a
higher calculated effective dose. In reading the
literature on effective dose, it is important to
determine which ICRP report was used to calculate the dose since this will affect any comparisons made.
Published effective doses for digital panoramic radiographs range from 5.5 to 22.0 Sv,
when the salivary glands are considered 2.4-6.2
Sv without,5,6 while digital cephalometric radiographs have effective doses of 2.2 to 3.4 Sv
with salivary glands, 1.6 to 1.7 Sv without.7,8
Therefore, a typical panoramic cephalometric
orthodontic examination will expose the patient
to 7.5 to 25.4 Sv effective dose (with salivary
glands). This compares with an average annual
natural (not including medical imaging or consumer products) background radiation dose in
the United States of 3.0 mSv (3000 Sv).9 See
Table 1.
CBCT Doses
In the last few years, the number of CBCT systems available has increased dramatically. Unfortunately, published dosimetry data are not available for most of these machines, although work
is under way to test them. Data have been pub-
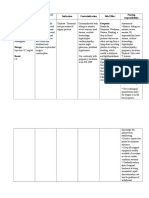
Table 1. Effective Doses of Imaging Examinations Used in Orthodontics
Examination
E Sv (without sal gl)
E Sv (with sal gl)
Reference
Panoramic (digital)
Cephalometric (digital)
CBCT (full FOV)
NewTom 9000
NewTom 3G
MercuRay
i-CAT (9)
i-CAT (12)
Conventional CT
Background radiation
2.4-6.2
1.6-1.7
5.5-22.0
2.2-3.4
5
7
36.3
44.5
846.9
68.7
134.8
42 to 657
3 mSv/yr, 8 Sv/d
77.9
58.9
1025.4
104.5
193.4
6
10
Reported in 11
Reported in 9
All doses are from the literature and are expressed as effective dose (E) in Sv. They may be reported as without/with salivary
glands (sal gl), which refers to how the dose to the salivary gland is treated in the calculation of the effective dose. The dose
with salivary glands is probably a better representation of the real risk since the salivary glands are directly exposed during
maxillofacial imaging. FOV field of view.
CBCT Dosimetry
lished on four of the large field-of-view systems:
the NewTom 9000 (QR, Verona, Italy), NewTom
3G, CB MercuRay (Hitachi Medical Systems, Tokyo, Japan), and the i-CAT (Imaging Sciences
International, Hatfield, PA).10,11 See Table 1.
There are a number of factors that will affect
the radiation dose produced by a CBCT system:
the imaging parameters used (kVp, mAs);
pulsed beam versus continuous beam; amount,
type, and shape of beam filter; full 360 rotation
versus lesser rotation; and limited versus full
field of view. Some of these factors, such as type
of beam and filtration, are unique to a specific
machine, while other factors, such as field of
view, are under the control of the operator.
In general, the smaller the field of view, the
lower the radiation dose.10 Since the effective
dose is computed from a weighted summation of
doses to various organs, removing some organs
from the path of the x-ray beam will reduce the
effective dose. For example, since the radiation
received by the thyroid gland contributes a large
amount to the effective dose, limiting the beam
to the maxilla instead of the whole head produces a lower effective dose.
In orthodontics, if CBCT is being used to
replace the standard panoramic and cephalometric radiographs, it may not be possible to
reduce the height of the beam and still obtain
the desired information. On the other hand, if
the CBCT is being used to supplement other
imaging in specific cases, such as for the assessment of impacted canines, beam height can be
reduced to cover only the area of interest without exposing the entire head.
Operators of some CBCT machines have the
opportunity to affect radiation dose by the imaging parameters they select. Some machines
allow the operator to select tube potential and
current (kVp, mA), others use a fixed setting,
and still others use a smart beam that bases the
parameters on patient size. Using higher settings
increases the signal-to-noise ratio (SNR) but also
increases the dose. A higher SNR may look prettier, but it has not been shown to increase the
diagnostic quality of the image.12 It does not
affect the density and contrast of the image:
these are controlled by image processing of the
data and can be adjusted on the monitor by the
operator.
17
Radiation in ChildrenAs Low as
Reasonably Achievable (ALARA)
Concerns have been raised in medical imaging
about the increased use of CT scans in children
because of the higher susceptibility of children
to the effects of radiation, with increased numbers of cancers predicted for the future of these
exposed children.13 In general, radiation doses
from medical CT scanners are higher than from
CBCT, but if CBCT becomes widespread in orthodontics, the collective dose to children could
be quite high. Even with the lowest dose CBCT
scanner on the market, the radiation dose is
higher with a full head scan than it is with panoramic and cephalometric radiographs.
The risk of cancer development as a result of
CBCT is not specifically known, particularly for
children. The effective dose calculations have
been used to try to estimate risk, usually expressed in terms of X number of excess cancers
per Y persons. Almost all of the risk estimates
have been based on adults because most of the
epidemiologic information available is on
adults. Using the ICRP probability coefficient of
6.0 102 Sv1 and the effective doses including
salivary glands,3,5-7,10 the risk estimates of cancer
induction or other stochastic effect are 0.3 to 1.3
10 6 for a dental panoramic radiograph, 0.1
to 0.2 10 6 for a cephalometric, and 3.5 to
61.5 10 6 for a full field-of-view CBCT.
At this point it is unknown whether the
information provided by a CBCT is sufficiently
greater than for traditional orthodontic imaging to justify its routine use in children. On
the other hand, it is also not clear whether the
estimated risk is significant enough to worry
about at all.
However, since stochastic effects of radiation
increase with exposure and the effects are not
seen for many years after exposure, the prudent
course is to apply the ALARA (As Low As Reasonably Achievable) principle to orthodontic imaging, as it is to other areas of radiation protection.14,15 That means that research should be
done to determine the true value of the extra
information in the diagnosis and management
of orthodontic cases, including the elucidation
of selection criteria that will identify those situations where the 3D information makes a substantial contribution to case management. Efforts should also be made by the manufacturers
18
S.L. Brooks
of CBCT equipment to reduce the radiation
dose produced by their machines and by the
operators to use the equipment in ways that will
keep the dose as low as possible while still obtaining the needed information. This may include reducing the height of the beam when a
full head view is not required and reducing the
imaging parameters to the lowest that would still
provide the desired information. In this way the
benefits of CBCT imaging can by realized while
the risks are minimized.
References
1. Langland OE, Langlais RP: Early pioneers of oral and
maxillofacial radiology. Oral Surg Oral Med Oral Pathol
Oral Radiol Endod 80:496-511, 1995
2. National Research Council: Health risks from exposure to low levels of ionizing radiation. BEIR VII Phase
2. Washington, DC, National Academies Press, 2006
3. International Commission on Radiological Protection:
1990 Recommendations. ICRP Publication 60. Ann
ICRP 21:1-201, 1991
4. International Commission on Radiological Protection:
2007 Recommendations. ICRP Publication 103. Ann
ICRP 37:1-332, 2008
5. Gijbels F, Jacobs R, Debaveye D, et al: Dosimetry of
digital panoramic imaging. Part I: Patient exposure.
Dentomaxillofac Radiol 34:145-149, 2005
6. Ludlow JB, Davies-Ludlow LE, Brooks SL: Dosimetry of
two extraoral direct digital imaging devices: NewTom
cone beam CT and Orthophos Plus DS panoramic unit.
Dentomaxillofac Radiol 32:229-234, 2003
7. Gijbels F, Sanderink G, Wyatt J, et al: Radiation doses of
indirect and direct digital cephalometric radiography.
Br Dent J 197:149-152, 2004
8. Visser H, Rodig T, Hermann KP: Dose reduction by
direct-digital cephalometric radiography. Angle Orthodont 71:159-163, 2001
9. Frederiksen NL: Health physics. In: White SC, Pharoah
MJ, eds: Oral radiology, principles and interpretation.
5th ed. St Louis, Mosby, 2004
10. Ludlow JB, Davies-Ludlow LE, Brooks SL, et al: Dosimetry of 3 CBCT units for oral and maxillofacial radiology:
CB Mercuray, NewTom 3G and i-CAT. Dentomaxillofac
Radiol 35:219-226, 2006
11. Mah JK, Danforth RA, Bumann A, et al: Radiation absorbed in maxillofacial imaging with a new dental computed tomography device. Oral Surg Oral Med Oral
Pathol Oral Radiol Endod 96:508-513, 2003
12. Swan KA: Image quality and radiation dose in cone
beam computed tomography for orthodontics. Masters
thesis, University of Michigan, 2007
13. MacNeil JS: Children highly vulnerable to imaging radiation. Pediatric News 2006 40:47. Available at: http://
www.pediatricnews.com (Accessed 26 June 2008)
14. Brand JW, Gibbs SJ, Edwards M, et al: Radiation protection in dentistry. NCRP Report No. 145, 2003
15. Farman AG: ALARA still applies [editorial]. Oral Surg
Oral Med Oral Pathol Oral Radiol Endod 100:395-397,
2005
S-ar putea să vă placă și
- Fixed Orthodontic Appliances: A Practical GuideDe la EverandFixed Orthodontic Appliances: A Practical GuideEvaluare: 1 din 5 stele1/5 (1)
- Essential Tissue Healing of the Face and NeckDe la EverandEssential Tissue Healing of the Face and NeckEvaluare: 5 din 5 stele5/5 (2)
- Clinical Practice Management in Orthodontics An OverviewDocument12 paginiClinical Practice Management in Orthodontics An OverviewCVVR SreedharÎncă nu există evaluări
- Understanding Masticatory Function in Unilateral CrossbitesDe la EverandUnderstanding Masticatory Function in Unilateral CrossbitesÎncă nu există evaluări
- Healers Versus Stealers: How to Outsmart the Thief in Your Dental PracticeDe la EverandHealers Versus Stealers: How to Outsmart the Thief in Your Dental PracticeÎncă nu există evaluări
- Orthodontics in the Vertical Dimension: A Case-Based ReviewDe la EverandOrthodontics in the Vertical Dimension: A Case-Based ReviewÎncă nu există evaluări
- Digital Planning and Custom Orthodontic TreatmentDe la EverandDigital Planning and Custom Orthodontic TreatmentK. Hero BreuningÎncă nu există evaluări
- BiomechanicsDocument33 paginiBiomechanicsMohammed bilalÎncă nu există evaluări
- THE ORTHODONTIC ROADMAP: GUIDELINES FOR THE DIAGNOSIS AND TREATMENT OF ORTHODONTIC MALOCCLUSIONSDe la EverandTHE ORTHODONTIC ROADMAP: GUIDELINES FOR THE DIAGNOSIS AND TREATMENT OF ORTHODONTIC MALOCCLUSIONSÎncă nu există evaluări
- A Beginners Guide To Lateral Cephalometric RadiographsDocument4 paginiA Beginners Guide To Lateral Cephalometric RadiographsClaudiaÎncă nu există evaluări
- Mandibular Incisor Extraction TherapyDocument10 paginiMandibular Incisor Extraction TherapyLeonardo LamimÎncă nu există evaluări
- Rapid MaxillaryDocument24 paginiRapid MaxillaryDon George GeojanÎncă nu există evaluări
- Wits Appraisalnof Jaw Disharmony by JOHNSONDocument20 paginiWits Appraisalnof Jaw Disharmony by JOHNSONDrKamran MominÎncă nu există evaluări
- Space AnalysisDocument43 paginiSpace AnalysismarieÎncă nu există evaluări
- Extractions in Orthodontics PDFDocument2 paginiExtractions in Orthodontics PDFJohnÎncă nu există evaluări
- Journal Club1 / Orthodontic Courses by Indian Dental AcademyDocument19 paginiJournal Club1 / Orthodontic Courses by Indian Dental Academyindian dental academyÎncă nu există evaluări
- The Orthodontics Effective RoleDocument31 paginiThe Orthodontics Effective RoleHamza BelhajÎncă nu există evaluări
- Cephalometric LandmarksDocument139 paginiCephalometric LandmarksNapakedHirunyakowitÎncă nu există evaluări
- Principles of The Alexander DisciplineDocument5 paginiPrinciples of The Alexander DisciplineSarah Fauzia SiregarÎncă nu există evaluări
- Geriatric Dentistry: Caring for Our Aging PopulationDe la EverandGeriatric Dentistry: Caring for Our Aging PopulationÎncă nu există evaluări
- Interpretation Basics of Cone Beam Computed TomographyDe la EverandInterpretation Basics of Cone Beam Computed TomographyEvaluare: 4 din 5 stele4/5 (1)
- Tweed ProfileDocument60 paginiTweed ProfileJu Ju WareeratÎncă nu există evaluări
- Exo OrthoDocument8 paginiExo OrthoEndriyana NovitasariÎncă nu există evaluări
- Ceph HandoutDocument18 paginiCeph Handoutwaheguru13he13Încă nu există evaluări
- Analysis of Diagnostic RecordsDocument78 paginiAnalysis of Diagnostic RecordsAtika Iftikhar MirÎncă nu există evaluări
- Space Analysis Golden 2023 SuliDocument39 paginiSpace Analysis Golden 2023 SuliHarsin BakrÎncă nu există evaluări
- Andrews Keys of OcclusionDocument21 paginiAndrews Keys of OcclusionbhargaviÎncă nu există evaluări
- Practical Techniques For Achieving Improved Accuracy in Bracket PositioningDocument14 paginiPractical Techniques For Achieving Improved Accuracy in Bracket Positioninganon-976413Încă nu există evaluări
- Interceptive Orthodontics: A Practical Guide to Occlusal ManagementDe la EverandInterceptive Orthodontics: A Practical Guide to Occlusal ManagementÎncă nu există evaluări
- Class II - DD and MX PDFDocument14 paginiClass II - DD and MX PDFserahÎncă nu există evaluări
- Consent in Orthodontics: Advice Sheet 4 British Orthodontic SocietyDocument10 paginiConsent in Orthodontics: Advice Sheet 4 British Orthodontic SocietyfarisÎncă nu există evaluări
- Abo GradingDocument11 paginiAbo GradingSonu RajuÎncă nu există evaluări
- Fundamentals of Occlusion and RestorativeDocument9 paginiFundamentals of Occlusion and RestorativePhạm Văn KhoaÎncă nu există evaluări
- Sunday, March 2, 2008: Important Orthodontic StudiesDocument6 paginiSunday, March 2, 2008: Important Orthodontic StudiesXnb HajiÎncă nu există evaluări
- 2.the Six Keys To Normal Occlusion - AndrewsDocument10 pagini2.the Six Keys To Normal Occlusion - AndrewsLudovica CoppolaÎncă nu există evaluări
- Help Me Prepare: Dental School Interview PreparationDe la EverandHelp Me Prepare: Dental School Interview PreparationÎncă nu există evaluări
- Newer Orthodontic Archwires Imparting EfDocument244 paginiNewer Orthodontic Archwires Imparting EfSelvaArockiamÎncă nu există evaluări
- Diagnostic Limitations of Cephalometrics in OrthodonticsDocument6 paginiDiagnostic Limitations of Cephalometrics in OrthodonticsDevata RaviÎncă nu există evaluări
- Moving The TeethDocument117 paginiMoving The TeethThirunavukkarasu Srinivasan100% (2)
- Model Analysis OrthoDocument48 paginiModel Analysis OrthoFourthMolar.comÎncă nu există evaluări
- Cone Beam Tomography in Orthodontics PDFDocument8 paginiCone Beam Tomography in Orthodontics PDFdruzair007Încă nu există evaluări
- 2.assessment of Dental Crowding in Mandibular Anterior Region by Three Different MethodsDocument3 pagini2.assessment of Dental Crowding in Mandibular Anterior Region by Three Different MethodsJennifer Abella Brown0% (1)
- 1 Introduction and Ideal OcclusionDocument33 pagini1 Introduction and Ideal OcclusionJASPREETKAUR0410100% (1)
- Alexander DisiplineDocument17 paginiAlexander DisiplineAshish SharmaÎncă nu există evaluări
- A History of Dentistry from the most Ancient Times until the end of the Eighteenth CenturyDe la EverandA History of Dentistry from the most Ancient Times until the end of the Eighteenth CenturyÎncă nu există evaluări
- 3D-CT Evaluation of Facial Asymmetry in Patients With Maxillofacial DeformitiesDocument9 pagini3D-CT Evaluation of Facial Asymmetry in Patients With Maxillofacial DeformitiesR KÎncă nu există evaluări
- Bone Grafting Techniques for Maxillary ImplantsDe la EverandBone Grafting Techniques for Maxillary ImplantsÎncă nu există evaluări
- LP 3 - Cephalometric TWEED AnalysisDocument47 paginiLP 3 - Cephalometric TWEED AnalysisAlexandraÎncă nu există evaluări
- Motivation, Compliance and Satisfaction in Orthodontic TreatmentDocument16 paginiMotivation, Compliance and Satisfaction in Orthodontic TreatmentAkram AlsharaeeÎncă nu există evaluări
- Open Bite CaseDocument10 paginiOpen Bite CaseezfreshÎncă nu există evaluări
- The Midline Diagnosis and Treatment ARTUROCAMACHODocument10 paginiThe Midline Diagnosis and Treatment ARTUROCAMACHOMiguel AngelÎncă nu există evaluări
- New Concept of Arch FormDocument16 paginiNew Concept of Arch FormRiddhi Rathi Shet100% (1)
- Space Regainers in Pediatric DentistryDocument6 paginiSpace Regainers in Pediatric DentistryDiba Eka DiputriÎncă nu există evaluări
- 8IAOAM Program BookDocument42 pagini8IAOAM Program Bookgriffone1Încă nu există evaluări
- 4 Removable Orthodontic Appliance Don't Want To Upload? Get Unlimited Downloads As A MemberDocument1 pagină4 Removable Orthodontic Appliance Don't Want To Upload? Get Unlimited Downloads As A Membergriffone1Încă nu există evaluări
- Skii in Japan Pg-802Document6 paginiSkii in Japan Pg-802griffone1Încă nu există evaluări
- Skii in Japan Pg-802Document6 paginiSkii in Japan Pg-802griffone1Încă nu există evaluări
- Ghosts Color PDFDocument1 paginăGhosts Color PDFgriffone1Încă nu există evaluări
- 1Document1 pagină1griffone1Încă nu există evaluări
- Spiros Zinelis, William A. Brantley Auth., Theodore Eliades Eds. Research Methods in Orthodontics A Guide To Understanding Orthodontic ResearchDocument224 paginiSpiros Zinelis, William A. Brantley Auth., Theodore Eliades Eds. Research Methods in Orthodontics A Guide To Understanding Orthodontic Researchgriffone1Încă nu există evaluări
- White Spot Lesions During Orthodontic83642257155-T1Document7 paginiWhite Spot Lesions During Orthodontic83642257155-T1griffone1Încă nu există evaluări
- Halloween Color PDFDocument2 paginiHalloween Color PDFgriffone1Încă nu există evaluări
- Spiros Zinelis, William A. Brantley Auth., Theodore Eliades Eds. Research Methods in Orthodontics A Guide To Understanding Orthodontic ResearchDocument224 paginiSpiros Zinelis, William A. Brantley Auth., Theodore Eliades Eds. Research Methods in Orthodontics A Guide To Understanding Orthodontic Researchgriffone1Încă nu există evaluări
- Wjo - 9 - 1THE RISK OF FIRE OR ELECTRIC SHOCK, CAREFULLY FOLLOW THESE INSTRUCTIONS. - Lee - 9Document10 paginiWjo - 9 - 1THE RISK OF FIRE OR ELECTRIC SHOCK, CAREFULLY FOLLOW THESE INSTRUCTIONS. - Lee - 9griffone1Încă nu există evaluări
- Maxilary Second Molar ExtractionDocument32 paginiMaxilary Second Molar Extractiongriffone1Încă nu există evaluări
- For More Books, Periodicals and Etc. About Orthodontics, ClickDocument1 paginăFor More Books, Periodicals and Etc. About Orthodontics, Clickgriffone1Încă nu există evaluări
- Informed Consent and Contributory Negligence: Litigation, Legislation, and EthicsDocument3 paginiInformed Consent and Contributory Negligence: Litigation, Legislation, and Ethicsgriffone1Încă nu există evaluări
- White Spot Lesions During Orthodontic83642257155-T1Document7 paginiWhite Spot Lesions During Orthodontic83642257155-T1griffone1Încă nu există evaluări
- During The Last Quarter of The 20thDocument7 paginiDuring The Last Quarter of The 20thgriffone1Încă nu există evaluări
- This Report Describes The Chewing PatternsDocument1 paginăThis Report Describes The Chewing Patternsgriffone1Încă nu există evaluări
- The Virtual Patient Specific-Model and The Virtual Dental Model10Document3 paginiThe Virtual Patient Specific-Model and The Virtual Dental Model10griffone1Încă nu există evaluări
- 1 Friction GeneratedDocument1 pagină1 Friction Generatedgriffone1Încă nu există evaluări
- Comparing Cone Beam Computed Tomography Systems From An Orthodontic Perspective08Document5 paginiComparing Cone Beam Computed Tomography Systems From An Orthodontic Perspective08griffone1Încă nu există evaluări
- 09comparing Cone Beam Computed Tomography Systems From An OrthodonticDocument7 pagini09comparing Cone Beam Computed Tomography Systems From An Orthodonticgriffone1Încă nu există evaluări
- During The Last Quarter of The 20thDocument7 paginiDuring The Last Quarter of The 20thgriffone1Încă nu există evaluări
- C one beam computed tomography 03Document1 paginăC one beam computed tomography 03griffone1Încă nu există evaluări
- Cone Beam Computed Tomography For OrthodontistsDocument2 paginiCone Beam Computed Tomography For Orthodontistsgriffone1Încă nu există evaluări
- The Radiology DecisionDocument5 paginiThe Radiology Decisiongriffone1Încă nu există evaluări
- A Few Comments On An Elegant Answer in Search of Useful Questions05Document2 paginiA Few Comments On An Elegant Answer in Search of Useful Questions05griffone1Încă nu există evaluări
- Seminars in Orthodontics EDITOR 01Document1 paginăSeminars in Orthodontics EDITOR 01griffone1Încă nu există evaluări
- Erratum: Seminars in Orthodontics, Vol 17, No 1 (March), 2011: P 88Document1 paginăErratum: Seminars in Orthodontics, Vol 17, No 1 (March), 2011: P 88griffone1Încă nu există evaluări
- C one beam computed tomography 03Document1 paginăC one beam computed tomography 03griffone1Încă nu există evaluări
- Seminars in Orthodontics: VOL 17, NO 1 MARCH 2011Document2 paginiSeminars in Orthodontics: VOL 17, NO 1 MARCH 2011griffone1Încă nu există evaluări
- Managing Tumor Lysis Syndrome.2Document4 paginiManaging Tumor Lysis Syndrome.2Caballero X CaballeroÎncă nu există evaluări
- Care of The Ventilated ChildDocument5 paginiCare of The Ventilated ChildBrahadheeswaran KannanÎncă nu există evaluări
- RS5573 FONA 1000S User Manual 6476381 Ver2 201604 EN CN Reg SADocument36 paginiRS5573 FONA 1000S User Manual 6476381 Ver2 201604 EN CN Reg SAJuan carlos Isaza gÎncă nu există evaluări
- Evaluation Entomological WarfareDocument62 paginiEvaluation Entomological WarfareReid Kirby100% (1)
- Obstetric Nursing Study GuideDocument69 paginiObstetric Nursing Study GuideValerie100% (3)
- 4.1 Fixator Extern Circular IlizarovDocument10 pagini4.1 Fixator Extern Circular IlizarovTudorica AdrianÎncă nu există evaluări
- Therapeutic Management of Clinical Mastitis in Goat: A Case StudyDocument5 paginiTherapeutic Management of Clinical Mastitis in Goat: A Case StudyIJAR JOURNALÎncă nu există evaluări
- Bahasa Inggris Kel.12Document10 paginiBahasa Inggris Kel.12Egi Satya FralazendaÎncă nu există evaluări
- Ingles 4 TareaDocument6 paginiIngles 4 TareayuruannyÎncă nu există evaluări
- Module Answers 1 60 MCN 2Document151 paginiModule Answers 1 60 MCN 2bekbekk cabahug100% (6)
- Philippine College of Science and Technology College of NursingDocument21 paginiPhilippine College of Science and Technology College of NursingAijem RyanÎncă nu există evaluări
- Abdullah M. Kharbosh, B.SC., PharmDocument27 paginiAbdullah M. Kharbosh, B.SC., PharmsrirampharmaÎncă nu există evaluări
- Breastfeeding and Down SyndromeDocument239 paginiBreastfeeding and Down SyndromeSim M ChangÎncă nu există evaluări
- Influence of Infection at The Time of Root Filling On The Outcome of Endodontic Treatment of Teeth With Apical Periodontitis Sjogren 1997Document10 paginiInfluence of Infection at The Time of Root Filling On The Outcome of Endodontic Treatment of Teeth With Apical Periodontitis Sjogren 1997abcder1234Încă nu există evaluări
- Long-Term Evaluation of Periodontal TherapyDocument16 paginiLong-Term Evaluation of Periodontal TherapyRanuch TakÎncă nu există evaluări
- Medicago Sativa LloydDocument4 paginiMedicago Sativa LloydDr Rushen SinghÎncă nu există evaluări
- Women S Health MidtermDocument30 paginiWomen S Health MidtermKatarzyna CiesielskaÎncă nu există evaluări
- Jcih 2007Document29 paginiJcih 2007Ankur BanerjeeÎncă nu există evaluări
- A Guide For G6PDDocument4 paginiA Guide For G6PDshimeath delrosarioÎncă nu există evaluări
- Burn Management by Tajuu Seid: Surgical WardDocument33 paginiBurn Management by Tajuu Seid: Surgical Wardelias adugnaÎncă nu există evaluări
- Thyroid Eye Disease Diagnosis and TreatmentDocument486 paginiThyroid Eye Disease Diagnosis and TreatmentUnsmil UnguÎncă nu există evaluări
- Yaman Walid KassabDocument282 paginiYaman Walid KassabHeryanti PusparisaÎncă nu există evaluări
- An Essay On The End-Of-Life Care in ChildrenDocument4 paginiAn Essay On The End-Of-Life Care in ChildrenThinashe MaswahuÎncă nu există evaluări
- Ficha Tecnica ANTIGENO 120006841 v3 Panbio COVID-19 Ag Nasopharyngeal IFU BoDocument132 paginiFicha Tecnica ANTIGENO 120006841 v3 Panbio COVID-19 Ag Nasopharyngeal IFU BoYessica Marisol Custodio ReinosoÎncă nu există evaluări
- 1-29-20 Diabetes Protocol Draft With Pandya and Alvarez EditsDocument12 pagini1-29-20 Diabetes Protocol Draft With Pandya and Alvarez Editsapi-552486649Încă nu există evaluări
- Communication and Swallowing Disorders (Speech)Document27 paginiCommunication and Swallowing Disorders (Speech)Asma JamaliÎncă nu există evaluări
- IsoketDocument2 paginiIsoketJaessa FelicianoÎncă nu există evaluări
- College of Nursing: Name: Krizia Mae A. Mendoza Section: BSN 2-1Document9 paginiCollege of Nursing: Name: Krizia Mae A. Mendoza Section: BSN 2-1Nikki Coleen SantinÎncă nu există evaluări
- Infant Overdose Risk With Liquid Vitamin DDocument2 paginiInfant Overdose Risk With Liquid Vitamin DsakuraleeshaoranÎncă nu există evaluări
- Abiraterone Acetate Plus Prednisone Versus Placebo Abiratetone LancetDocument9 paginiAbiraterone Acetate Plus Prednisone Versus Placebo Abiratetone LancetMahesh TamhaneÎncă nu există evaluări