Documente Academic
Documente Profesional
Documente Cultură
Treatment Modality For Advanced Oral Submucous Fibrosis
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Treatment Modality For Advanced Oral Submucous Fibrosis
Drepturi de autor:
Formate disponibile
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS)
e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 14, Issue 2 Ver. VII (Feb. 2015), PP 76-79
www.iosrjournals.org
Treatment Modality for Advanced Oral Submucous Fibrosis
1
Dr. Kanwaldeep Singh Soodan, 2Dr. Pratiksha Priyadarshni,
3
Dr. Rajesh Kshirsagar, 4Dr. Avneet Kaur, 5Dr. Puneet Singh Soodan
1
Reader, Dept. Of Oral & Maxillofacial Surgery M. M. Dental College & Hospital, Mullana
2
Tutor, Dept. Of Oral & Maxillofacial Surgery M. M. Dental College & Hospital, Mullana
3
Professor, Dept. Of Oral & Maxillofacial Surgery Bharati Vidyapeeth Dental College & Hospital, Pune
4
Senior Resident, Dept. Of Microbiology Govt. Medical College & Hospital, Jammu
5
Senior Resident, Dept. Of Dermatology Hind Institute of Medical sciences & hospital, Lucknow
Abstract: Oral submucous fibrosis (OSMF), which presents with a severe degree of trismus, is a great surgical
challenge. The surgical procedures include excision of fibrous bands with or without coverage of the surgically
created defect. The use of vascularised flaps such as the palatal pedicled flap, tongue flaps, use of buccal fat
pad and nasolabial flaps are becoming increasingly popular. We present a case of advanced oral submucous
fibrosis treated with bilateral inferiorly based nasolabial flaps.
Key Words: Oral Submucous Fibrosis, Fibrous bands, Vascularised flaps
I.
Case Report
A 35 years old male reported with a chief complaint of burning sensation and limitation of mouth
opening since 3 years. He had been a gutkha chewer for the past 11 years; consuming approximately 5 packets
per day. Interincisal opening (IIO) was 13 mm [Fig-1].
Fig-1: Preoperative interincisal opening was 13mm
Fibrous bands were palpable bilaterally on the buccal mucosa and retromolar region, blanched and
leathery floor of the mouth, the palate was involved and the uvula was shrunken. Given the nature of
presentation and the advanced nature of the disease, it was decided to proceed with inferiorly based nasolabial
flaps for management.
II.
Surgical Procedure
The treatment plan was discussed with the patient and an informed consent was signed. After thorough
medical and anaesthetic evaluation, the patient was prepared for surgical intervention. The procedure was
carried out under general anesthesia. Intubation was carried out using a flexible bronchoscope. The patient
received preoperative antibiotics, premedication and other suitable medications. The intraoral incisions were
made bilaterally to incise the fibrous bands using a knife along the buccal mucosa at the level of occlusal plane.
Incision began from the anterior faucial pillars and extended up to 1cm from the corner of mouth. The collagen
bands were incised up to the muscle layer. After the release of fibrotic bands, a defect of approximately 5.5 cm x
2 cm was created. Using Fergusson's mouth gag forcible mouth opening was carried out. Interincisal distance
was 50 mm measured and a bite block was placed [Fig-2].
DOI: 10.9790/0853-14277679
www.iosrjournals.org
76 | Page
Treatment Modality for Advanced Oral Submucous Fibrosis
Fig-2: Intraoperative interincisal opening was 50mm
All third molars were removed at this stage. The marking for the bilateral inferiorly based nasolabial
flap design was done using methylene blue ink. The flap was outlined on cheek and raised with sufficient
subcutaneous tissue and fat to ensure a good blood supply but remained superficial to facial muscles. The
medial incision line followed the nasolabial fold on superior two thirds and was placed 3-4mm medial in inferior
one third. The base of flap was 1.5 to 2.5cm wide. Width greater than this makes rotation of flap difficult while
narrower than this can compromise the blood supply. The medial and lateral incision lines tapered superiorly
approximately 0.5 to 0.75cm inferior to medial canthus. The inferior limit of the flap was at the level of oral
commissure because just below this several branches of facial artery or inferior labial artery pass into nasolabial
skin and subcutaneous tissue. Flap was raised from superior to inferior in supramuscular plane by using
dissecting scissors and electrocautery. The angular branch was tied off. The transbuccal tunnel was made in the
region of the modiolus just medial to the pedicle. The flap was then transferred into the oral cavity in a tension
free manner [Fig-3].
Fig-3: The flap was then transferred into the oral cavity in a tension free manner
The intraoral flap was sutured by placing interrupted sutures using 3-0 vicryl. Donor site was closed
primarily in layers using 3 - 0 vicryl suture for deeper layer and 5 - 0 Ethilon for final skin closure. Nasogastric
feeding was carried out for 7 days postoperatively. A mouth prop was placed between the teeth to maintain the
interincisal distance for first 48 hours. The mouth was covered with wet gauze to prevent dryness of mouth and
was maintained wet by pouring saline. The prop was removed intermittently, every two hours for fifteen
minutes. Interincisal opening was measured daily for first 7 days and physiotherapy was advised. Mouth
opening exercises using Hiesters mouth gag were taught. IIO was maintained over 35 mm for 7 days during
immediate postoperative period. Flap viability was checked using needle prick at the most distal tip of flap in
the retromolar area after 24 hrs, 48 hours, and 7 days and after pedicle division respectively. Success of the flap
was determined 7 days after pedicle division by reassessment of vascularity, adaptability to underlying surface
and appropriate coverage of the raw surface following excision of bands and evaluation of scar. Usefulness of
flap was determined by assessing whether flap dimensions were adequate to cover the denuded area and if it
prevented scar contracture thus maintaining the increased interincisal opening. All sutures were removed on the
seventh postoperative day. The patient was advised to use combination of Vitamin E cream (Evion) and Benzoyl
Peroxide Cream 2.5% (Persol forte) twice daily after suture removal. Flap division and correction of the
DOI: 10.9790/0853-14277679
www.iosrjournals.org
77 | Page
Treatment Modality for Advanced Oral Submucous Fibrosis
unaesthetic triangular base of the scar was done after three weeks. Patient was evaluated for IIO and various
other parameters regarding the surgical procedure daily for first seven days then weekly till four weeks and then
monthly for first six months. On sixth month post operative, IIO was found to be maintained to 38mm [Fig-4].
Fig-4: On sixth month post operative, IIO was found to be maintained to 38mm
Intraorally flaps were found to be successful [Fig-5a and 5b].
a
b
Fig-5]: On sixth month post operative, flaps were found to be successful. (a) Left intraoral view. (b) Right
intraoral view.
III.
Discussion
Pindborg (1966) defined Oral Submucous Fibrosis as A chronic progressive scarring disease of oral
cavity and oropharynx characterized by epithelial atrophy and juxtaepithelial inflammatory reaction with
progressive fibrosis of lamina propria and deeper connective tissues resulting in stiffness of oral mucosa and
causing progressive decrease in mouth opening[1].
Oral submucous fibrosis (OSMF) is defined as a chronic disease of oral mucosa characterized by
inflammation and progressive fibrosis of the lamina propria and deeper connective tissue layers. The
pathogenesis of the disease is not well established, but is believed to be multifactorial [2]. A number of factors
trigger the disease process by causing a juxtaepithelial inflammatory reaction in the oral mucosa. Suggested
contributory factors include areca nut chewing, ingestion of chillies, nutritional deficiencies, genetic and
immunologic processes and other factors. Presenting symptoms are burning pain, progressive inability to open
the mouth, difficulty in mastication and swallowing. Speech and hearing deficits may occur because of
involvement of the tongue and the eustachian tubes [2, 3].Oral submucous fibrosis is a potential premalignant
condition with an incidence of oral cancer in 3 - 7.6% cases [3, 4].
The treatment for patients afflicted with oral submucous fibrosis focuses on relieving the symptoms
and improving the mouth opening by therapeutic and/or surgical means. Medical management, which forms the
first line of treatment, includes topical, intralesional and systemic medications. The commonly used agents
include placental extracts, steroids, vitamins and hyaluronidase. However, the role of these medications in
advanced cases of oral submucous fibrosis with established restricted mouth opening is limited.
DOI: 10.9790/0853-14277679
www.iosrjournals.org
78 | Page
Treatment Modality for Advanced Oral Submucous Fibrosis
According to Khanna and Andrade's grouping of OSMF based on clinical and histopathologic features,
it is a well established fact that in oral submucous fibrosis there is decreased vascularity to the affected
region by fibrosis due to contraction and narrowing of blood vessels as a result of increased pressure on them by
fibrous tissue bands [4]. Medicinal modalities of treatment like topical application of gold, iodides &
intralesional injection of hyaluronidase, hydrocortisone, placental extract & triamcinolone along with oral
administration of vitamins, iron supplement and antioxidants are of temporary benefit and are of limited use in
treating moderately advanced and advanced cases of OSMF.
In patients with moderate to advanced oral submucous fibrosis, surgical therapy is beneficial.
Materials used for covering the defect following the excision of bands include skin grafts, tongue flaps, buccal
fat pat, amnion graft, nasolabial flaps and palatal island flaps. Additional procedures like temporalis myotomy
and bilateral coronoidectomy may be performed to enhance mouth opening.
The use of nasolabial flaps in treatment of OSMF is more suitable for juxtaposed defects, in particular
those of buccal mucosa, and is becoming increasingly popular. The nasolabial flap provides a good example of
the transposition flap principle. The reason of it showing satisfactory results could be the fact that it is not a part
of the crippled oral disease. In older patients, the donor scar is quite inconspicuous.
Kavarna NM and Bhatena HM in their article in 1987 have reported that bilateral full thickness
nasolabial flaps have been used successfully in three patients to give long-term relief of severe trismus caused
by oral submucous fibrosis [5]. They had used two-stage flap measuring approximately 41.52 cm bilaterally.
The pedicle were divided after 3 weeks and insetting of flap was done such that divided base of flaps come up to
the vermilion border at angle of mouth. They had achieved an average mouth opening of 25 mm.
S.Bhattacharya, MSD Jaiswal (1990) used inferiorly based nasolabial flap to cover buccal defects
caused by incising fibrosed bands [6]. They advocated incorporation of underlying vessel in the flap & selective
defattening of the flap and its pedicle to improve arc of rotation.
Gomes DC, Chaudhri C conducted study on 12 patients of oral malignancy of buccal mucosa region
with severe oral submucous fibrosis [7]. The malignant buccal mucosa sites were reconstructed with pectoralis
myocutaneous flaps after wide local resection. They advocated release of opposite nonmalignant fibrosed buccal
mucosa and reconstruction with inferiorly based nasolabial flaps. All their patients had preoperative IIO of
1.5cm or less. The average mouth opening at 3 months was 3.13 cm and average follow up period was 13.08
months. No reduction in mouth opening had been noted during that period.
SM Balaji in his article stating study of 19 patients has compared nasolabial flap to tongue flap for
covering defects created by excision of fibrous bands [8]. He had used inferiorly based nasolabial flap but
rotated 180 so that skin faces the raw buccal surface and suturing the margins of mucosa to the flap closes the
defect in mucosa. On comparison of graft shrinkage, post operative mouth opening, need for secondary surgery,
functional disfigurement and esthetic outcome of surgery, nasolabial flaps interpolated into the oral cavity offer
an expedient solution to soft tissue deficit produced after excision of bands.
References
[1].
[2].
[3].
[4].
[5].
[6].
[7].
[8].
Pindborg JJ, et al. Oral Submucous Fibrosis. Oral Surg Oral Med Oral Pathol Oral Radiol. 1966; 22:764-78.
Canniff JP, Harvey W, Harris M. Oral submucous fibrosis: its pathogenesis and management. Br Dent J. 1986; 160: 429-34.
Rajendran R. Oral submucous fibrosis: etiology, pathogenesis and future research. Bulletin of the World Health Organisation, 1994;
72(6): 985-96.
Khanna J.N., Andrade NN. Oral submucous fibrosis: a new concept in surgical management Report of 100 cases. Int J Oral
Maxillofac Surg. 1995; 24: 433-39.
Kaverana NM, Bhathena HM. Surgery for severe trismus in submucous fibrosis. Br J Plast Surg. 1987; 40: 407-09.
Bhattacharya S, MSD Jaiswal. Island nasolabial flaps. IJPS 1990; 23 (2):83-87.
Gomes C, Chaudhri C. Total oral reconstruction for cancers associated with advanced oral submucous fibrosis. Annals of Plast.
Surg. 2003; 51: 283-89.
Balaji SM. Comparison of nasolabial and tongue flaps in the correction of OSMF. J Maxillofac Oral Surg. 2004; 3: 12-17.
DOI: 10.9790/0853-14277679
www.iosrjournals.org
79 | Page
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Manual de RCP - NEONATAL - 7°ED PDFDocument328 paginiManual de RCP - NEONATAL - 7°ED PDFNatanael Librado97% (29)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Effect of Instructional Methods and Locus of Control On Students' Speaking Ability (An Experimental Study in State Senior High School 01, Cibinong Bogor, West Java)Document11 paginiThe Effect of Instructional Methods and Locus of Control On Students' Speaking Ability (An Experimental Study in State Senior High School 01, Cibinong Bogor, West Java)International Organization of Scientific Research (IOSR)Încă nu există evaluări
- Study The Changes in Al-Ahwaz Marshal Using Principal Component Analysis and Classification TechniqueDocument9 paginiStudy The Changes in Al-Ahwaz Marshal Using Principal Component Analysis and Classification TechniqueInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- Philosophical Analysis of The Theories of Punishment in The Context of Nigerian Educational SystemDocument6 paginiPhilosophical Analysis of The Theories of Punishment in The Context of Nigerian Educational SystemInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- Effects of Formative Assessment On Mathematics Test Anxiety and Performance of Senior Secondary School Students in Jos, NigeriaDocument10 paginiEffects of Formative Assessment On Mathematics Test Anxiety and Performance of Senior Secondary School Students in Jos, NigeriaInternational Organization of Scientific Research (IOSR)100% (1)
- Project Based Learning Tools Development On Salt Hydrolysis Materials Through Scientific ApproachDocument5 paginiProject Based Learning Tools Development On Salt Hydrolysis Materials Through Scientific ApproachInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- Development of Dacum As Identification Technique On Job Competence Based-Curriculum in High Vocational EducationDocument5 paginiDevelopment of Dacum As Identification Technique On Job Competence Based-Curriculum in High Vocational EducationInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- Enhancing Pupils' Knowledge of Mathematical Concepts Through Game and PoemDocument7 paginiEnhancing Pupils' Knowledge of Mathematical Concepts Through Game and PoemInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- Students' Perceptions of Grammar Teaching and Learning in English Language Classrooms in LibyaDocument6 paginiStudents' Perceptions of Grammar Teaching and Learning in English Language Classrooms in LibyaInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- Need of Non - Technical Content in Engineering EducationDocument3 paginiNeed of Non - Technical Content in Engineering EducationInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- Necessary Evils of Private Tuition: A Case StudyDocument6 paginiNecessary Evils of Private Tuition: A Case StudyInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- Child Mortality Among Teenage Mothers in OJU MetropolisDocument6 paginiChild Mortality Among Teenage Mothers in OJU MetropolisInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- Youth Entrepreneurship: Opportunities and Challenges in IndiaDocument5 paginiYouth Entrepreneurship: Opportunities and Challenges in IndiaInternational Organization of Scientific Research (IOSR)100% (1)
- Geohydrological Study of Weathered Basement Aquifers in Oban Massif and Environs Southeastern Nigeria: Using Remote Sensing and Geographic Information System TechniquesDocument14 paginiGeohydrological Study of Weathered Basement Aquifers in Oban Massif and Environs Southeastern Nigeria: Using Remote Sensing and Geographic Information System TechniquesInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- Microencapsulation For Textile FinishingDocument4 paginiMicroencapsulation For Textile FinishingInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- Comparison of Psychological Variables Within Different Positions of Players of The State Junior Boys Ball Badminton Players of ManipurDocument4 paginiComparison of Psychological Variables Within Different Positions of Players of The State Junior Boys Ball Badminton Players of ManipurInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- Comparison of Explosive Strength Between Football and Volley Ball Players of Jamboni BlockDocument2 paginiComparison of Explosive Strength Between Football and Volley Ball Players of Jamboni BlockInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- Investigation of Wear Loss in Aluminium Silicon Carbide Mica Hybrid Metal Matrix CompositeDocument5 paginiInvestigation of Wear Loss in Aluminium Silicon Carbide Mica Hybrid Metal Matrix CompositeInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- Comparison of Selected Anthropometric and Physical Fitness Variables Between Offencive and Defencive Players of Kho-KhoDocument2 paginiComparison of Selected Anthropometric and Physical Fitness Variables Between Offencive and Defencive Players of Kho-KhoInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- Lipoproteins and Lipid Peroxidation in Thyroid DisordersDocument6 paginiLipoproteins and Lipid Peroxidation in Thyroid DisordersInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- Advancing Statistical Education Using Technology and Mobile DevicesDocument9 paginiAdvancing Statistical Education Using Technology and Mobile DevicesInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- Study of Effect of Rotor Speed, Combing-Roll Speed and Type of Recycled Waste On Rotor Yarn Quality Using Response Surface MethodologyDocument9 paginiStudy of Effect of Rotor Speed, Combing-Roll Speed and Type of Recycled Waste On Rotor Yarn Quality Using Response Surface MethodologyInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- Factors Affecting Success of Construction ProjectDocument10 paginiFactors Affecting Success of Construction ProjectInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- A Review On Refrigerants, and Effects On Global Warming For Making Green EnvironmentDocument4 paginiA Review On Refrigerants, and Effects On Global Warming For Making Green EnvironmentInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- Application of Xylanase Produced by Bacillus Megaterium in Saccharification, Juice Clarification and Oil Extraction From Jatropha Seed KernelDocument8 paginiApplication of Xylanase Produced by Bacillus Megaterium in Saccharification, Juice Clarification and Oil Extraction From Jatropha Seed KernelInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- Comparative Effect of Daily Administration of Allium Sativum and Allium Cepa Extracts On Alloxan Induced Diabetic RatsDocument6 paginiComparative Effect of Daily Administration of Allium Sativum and Allium Cepa Extracts On Alloxan Induced Diabetic RatsInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- Core Components of The Metabolic Syndrome in Nonalcohlic Fatty Liver DiseaseDocument5 paginiCore Components of The Metabolic Syndrome in Nonalcohlic Fatty Liver DiseaseInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- Auxin Induced Germination and Plantlet Regeneration Via Rhizome Section Culture in Spiranthes Sinensis (Pers.) Ames: A Vulnerable Medicinal Orchid of Kashmir HimalayaDocument4 paginiAuxin Induced Germination and Plantlet Regeneration Via Rhizome Section Culture in Spiranthes Sinensis (Pers.) Ames: A Vulnerable Medicinal Orchid of Kashmir HimalayaInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- Research Analysis On Sustainability Opportunities and Challenges of Bio-Fuels Industry in IndiaDocument7 paginiResearch Analysis On Sustainability Opportunities and Challenges of Bio-Fuels Industry in IndiaInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- Parametric Optimization of Single Cylinder Diesel Engine For Specific Fuel Consumption Using Palm Seed Oil As A BlendDocument6 paginiParametric Optimization of Single Cylinder Diesel Engine For Specific Fuel Consumption Using Palm Seed Oil As A BlendInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- What is a phobia? Types, causes and treatmentDocument3 paginiWhat is a phobia? Types, causes and treatmentLaura La Novia ImaginariaÎncă nu există evaluări
- Human Male Reproductive SystemDocument2 paginiHuman Male Reproductive Systemmilviepaz100% (1)
- Types of Medical Equipment, Rooms and Departments in HospitalDocument22 paginiTypes of Medical Equipment, Rooms and Departments in HospitalAfriza EffendiÎncă nu există evaluări
- Hydration by Subcutaneous InfusionDocument11 paginiHydration by Subcutaneous Infusionrene_smithÎncă nu există evaluări
- Dr. Rajendran'S Institute of Medical Education: Cvs - Anatomy (45 MCQS)Document15 paginiDr. Rajendran'S Institute of Medical Education: Cvs - Anatomy (45 MCQS)suckeydluffyÎncă nu există evaluări
- Slides 3 - Internal AnatomyDocument45 paginiSlides 3 - Internal AnatomyCWT2010100% (1)
- 1 Al ZahrawiDocument6 pagini1 Al ZahrawiAL-Khawaldeh Hamza0% (1)
- 1 s2.0 S0007193505800223 MainDocument12 pagini1 s2.0 S0007193505800223 Mainadamos1945Încă nu există evaluări
- White Sleep: Noise and InductionDocument3 paginiWhite Sleep: Noise and InductionMariaÎncă nu există evaluări
- Approach To Sick NeonateDocument47 paginiApproach To Sick NeonateblitheleevsÎncă nu există evaluări
- Phimosis and ParaphimosisDocument3 paginiPhimosis and ParaphimosisJoshua PowersÎncă nu există evaluări
- High-Risk Pregnancy Premature Rupture of Membranes (PROM)Document3 paginiHigh-Risk Pregnancy Premature Rupture of Membranes (PROM)elimcangcoÎncă nu există evaluări
- SterilizationDocument6 paginiSterilizationMaria Ella Joanne DapitonÎncă nu există evaluări
- English Lesson Plan for Grade 5 Semester 2Document11 paginiEnglish Lesson Plan for Grade 5 Semester 2Ngh WirawanÎncă nu există evaluări
- Health and Social Welfare Laws - 042915Document12 paginiHealth and Social Welfare Laws - 042915gmcamaymayanÎncă nu există evaluări
- Bilateral Hypoplastic or Aplastic Posterior Tibial ArteryDocument2 paginiBilateral Hypoplastic or Aplastic Posterior Tibial ArteryPaul HartingÎncă nu există evaluări
- NRP (Neonatal Resuscitation Program) 6th Edition 2 of 5Document88 paginiNRP (Neonatal Resuscitation Program) 6th Edition 2 of 5iamlucil100% (4)
- Medical Errors and The Importance of Second Opinions in RadiologyDocument10 paginiMedical Errors and The Importance of Second Opinions in RadiologyMetis MDÎncă nu există evaluări
- Nur 195 Long Exam P2 Rle 1 - 1Document21 paginiNur 195 Long Exam P2 Rle 1 - 1Marga WreatheÎncă nu există evaluări
- Inotropic and Vasoactive Drugs in Pediatric ICUDocument6 paginiInotropic and Vasoactive Drugs in Pediatric ICUCandy RevolloÎncă nu există evaluări
- Sterling Hospital charges index guideDocument112 paginiSterling Hospital charges index guideAnimesh JainÎncă nu există evaluări
- Pediatric Vital Signs Reference Chart PedsCasesDocument1 paginăPediatric Vital Signs Reference Chart PedsCasesAghnia NafilaÎncă nu există evaluări
- SEO-Optimized Title for Mastoidectomy and Cholesteatoma ChapterDocument27 paginiSEO-Optimized Title for Mastoidectomy and Cholesteatoma ChapterCondurache Ilie-AndreiÎncă nu există evaluări
- History and Development of Nursing as a ProfessionDocument4 paginiHistory and Development of Nursing as a Professionnitu_kalita3Încă nu există evaluări
- Considerations On The Use of Neonatal and Pediatric ResuscitationDocument15 paginiConsiderations On The Use of Neonatal and Pediatric ResuscitationrsmitrahuadaÎncă nu există evaluări
- Pregnancy Constipation and DiarrheaDocument15 paginiPregnancy Constipation and DiarrheaAry GuhtamaÎncă nu există evaluări
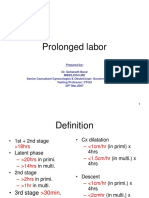
- Prolonged Labor Diagnosis and ManagementDocument8 paginiProlonged Labor Diagnosis and ManagementMadhu Sudhan PandeyaÎncă nu există evaluări
- The Will of Allah or Gross Medical NegligenceDocument3 paginiThe Will of Allah or Gross Medical NegligenceProf ZaffarÎncă nu există evaluări
- Responsibilities of Chief NurseDocument4 paginiResponsibilities of Chief NursejeckjeckÎncă nu există evaluări