Documente Academic
Documente Profesional
Documente Cultură
Case Report: Implementation of Measurement Instruments in Physical Therapist Practice: Development of A Tailored Strategy
Încărcat de
NelsonRodríguezDeLeónTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Case Report: Implementation of Measurement Instruments in Physical Therapist Practice: Development of A Tailored Strategy
Încărcat de
NelsonRodríguezDeLeónDrepturi de autor:
Formate disponibile
Case Report
Implementation of Measurement
Instruments in Physical Therapist
Practice: Development of a
Tailored Strategy
J.G. Anita Stevens, Anna J.M.H. Beurskens
Background and Purpose. The use of measurement instruments has become
a major issue in physical therapy, but their use in daily practice is infrequent. The
aims of this case report were to develop and evaluate a plan for the systematic
implementation of 2 measurement instruments frequently recommended in Dutch
physical therapy clinical guidelines: the Patient-Specific Complaints instrument and
the Six-Minute Walk Test.
Case Description. A systematic implementation plan was used, starting with a
problem analysis of aspects of physical therapist practice. A literary search, structured
interviews, and sounding board meetings were used to identify barriers and facilitators. Based on these factors, various strategies were developed through the use of a
planning model for the process of change.
Outcomes. Barriers and facilitators were revealed in various domains: physical
therapists competence and attitude (knowledge and resistance to change), organization (policy), patients (different expectations), and measurement instruments (feasibility). The strategies developed were adjustment of the measurement instruments,
a self-analysis list, and an education module. Pilot testing and evaluation of the
implementation plan were undertaken. The strategies developed were applicable to
physical therapist practice. Self-analysis, education, and attention to the practice
organization made the physical therapists aware of their actual behavior, increased
their knowledge, and improved their attitudes toward and their use of measurement
instruments.
J.G.A. Stevens, PT, MSc, is Researcher and Teacher, Center of
Research Autonomy and Participation of People With Chronic Illnesses, Department of Physiotherapy, Zuyd University, Nieuw
Eyckholt 300, PO Box 550, 6400
AN Heerlen, the Netherlands. Address all correspondence to Ms
Stevens at: a.stevens@hszuyd.nl.
A.J.M.H. Beurskens, PT, PhD, is Associate Professor, Center of Research Autonomy and Participation of People With Chronic
Illnesses, Department of Physiotherapy, Zuyd University.
[Stevens JGA, Beurskens AJMH.
Implementation of measurement
instruments in physical therapist
practice: development of a tailored strategy. Phys Ther. 2010;
90:953961.]
2010 American Physical Therapy
Association
Discussion. The use of a planning model made it possible to tailor multifaceted
strategies toward various domains and phases of behavioral change. The strategies
will be further developed in programs of the Royal Dutch Society for Physical
Therapy. Future studies should examine the use of measurement instruments as an
integrated part of the process of clinical reasoning. The focus of future studies should
be directed not only toward physical therapists but also toward the practice organization and professional associations.
Post a Rapid Response to
this article at:
ptjournal.apta.org
June 2010
Volume 90
Number 6
Physical Therapy f
953
Implementation of Measurement Instruments
onitoring the health status
of patients through the use
of outcome measures is considered to be an aspect of good clinical practice in physical therapy.13
The clinical guidelines of the Royal
Dutch Society for Physical Therapy
recommend the use of measurement
instruments. Until now, this recommendation has been implemented in
a passive way by mailing the clinical
practice guidelines containing the
measurement instruments. Despite
the overall positive attitude of physical therapists, the daily use of outcome measures in physical therapist
practice is remarkably low.2,4 8
In Europe and Australia, implementation is a common term for what in
the United States is called knowledge translation or exchange. In this
article, the term implementation,
which means a systematic process
in which innovations or changes of
proven value become structurally
embedded in professional practice,
was used. It is well known that passive implementation strategies are
not effective.9,10 Systematic reviews
of the effectiveness of implementation interventions have shown that
strategies should be targeted toward
specific barriers to and facilitators of
change that have been assessed in a
thorough problem analysis of the target group and setting.9,1118 Although
education is an important strategy,
implementation should not be restricted to educational interventions
for individual health professionals
only. Factors concerning practice
policy and organization, patients,
Available With
This Article at
ptjournal.apta.org
Audio Abstracts Podcast
This article was published ahead of
print on April 22, 2010, at
ptjournal.apta.org.
954
Physical Therapy
Volume 90
and the measurement instruments
themselves also are important.4,12
The Dutch Scientific College of Physiotherapy of the Royal Dutch Society
for Physical Therapy has made a systematic approach to the implementation of outcome measures in daily
practice a focal point of its policy.
The aims of this case report were to
develop and evaluate a systematic implementation plan for the use of 2
measurement instruments frequently
recommended in Dutch physical
therapy clinical guidelines: the PatientSpecific Complaints (PSC) instrument,19 which is comparable to the
Pain-Specific Functional Scale,20 and
the Six-Minute Walk Test (6MWT).21
To meet our aims, we sought answers
to 2 questions:
1. Which barriers and facilitators
contribute to the use of the PSC
and 6MWT in physical therapist
practice?
2. Which implementation strategies
can be tailored to these barriers
and facilitators and applied to
physical therapist practice?
Target Setting
The implementation plan was aimed
at physical therapists in private practice in the community. This group is
the largest group of physical therapists in the Netherlands; they are easily accessible and are not restricted
by complicated and formal institutional rules. It also appears that these
physical therapists use fewer measurement instruments than their colleagues in hospitals and other
institutions.7
Development and
Application of the Process
As a guideline for a systematic approach, the implementation model
of Grol et al10 was used. The 5 steps
in this model and the methods used
in this case report are shown in the
Figure.
Number 6
Step 1: Proposal for
Improvement
We focused on the implementation
of 2 easily applicable measurement
instruments that are frequently recommended in Dutch physical therapy guidelines. The first instrument
was the PSC, a Dutch instrument that
is comparable to the Pain-Specific
Functional Scale.19,20 In both instruments, patients must list 3 activities
and score them. Differences are the
scoring method (visual analog scale
versus numerical rating scale), the
time frame on which the score is
based (1 week versus 1 day), and the
availability of a sample activity list in
the PSC to help patients identify
their main complaint. The second instrument was the 6MWT, which is
used to assess the aerobic exercise
capacity of a patient by measuring
the walking track length in 6
minutes.21
Step 2: Problem Analysis
To obtain a complete and valid overview of relevant barriers and facilitators, we used various methods to collect information. First, a literature
search of the PubMed and Cochrane
databases was carried out to identify
studies about barriers and facilitators
in the use of measurement instruments and clinical guidelines. From
this information a topic list was formulated (the list is available on request from the authors). Second,
physical therapists in several private
practices were interviewed. We
searched for a wide variety in terms
of expertise and number of employees and considered the use of clinimetrics (purposive sampling).
The
semistructured
interviews
(45 60 minutes) were digitally audiotaped, summarized, and member
checked by the physical therapists.
The interviews started with general
inquiries on the following themes:
information about the practice, patient categories, and measurement
instruments used. Thereafter, open
June 2010
Implementation of Measurement Instruments
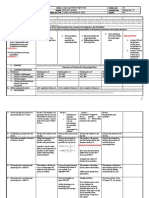
Figure.
Implementation model of Grol et al10 and the methods used in this case report. KNGFKoninklijk Nederland Genootschap voor
Fysiotherapie (Royal Dutch Society for Physical Therapy).
questions were asked about perceived barriers and facilitators in the
use of measurement instruments in
daily practice. At the end of each
interview, the topic list was presented to the interviewees, and additional relevant items could be indicated. The barriers and facilitators
identified were ordered in various
domains: the physical therapist, the
organization, patients, and the measurement instruments themselves.
The number of interviews was estimated at between 15 and 20, and the
interviews were stopped when a saturation of data was reached.22
Step 3: Development of
Implementation Strategies
The information from step 2 guided
the selection of both the type and
June 2010
the specific content of the implementation strategies developed; a
planning model for the process of
change was used.10,16 In addition, a
literature survey on how to select
and tailor strategies to the information from the problem analysis was
performed. Until now, not many implementation studies have been
based on a problem analysis. Therefore, studies about the effect of implementation on general health were
used. The results from both the literature search and the interviews were
discussed with the project group
(experts in the field of guideline implementation) and a sounding board
(the interviewed physical therapists).
Subsequently, implementation strategies were selected and developed.
Steps 4 and 5: Testing and
Evaluation of the
Implementation Plan
In the literature, recommendations
were made about testing interventions initially in small groups, in
which active education and professional support seemed to be effective in improving physical therapists
attitudes and adherence.4,23,24 Therefore, pilot testing of the implementation plan was undertaken with 2
groups of physical therapists from 4
physical therapist practices. The
evaluation focused on feasibility and
readjustment of the strategies developed. The results of the first pilot
program were used to make adjustments in the second pilot program. It
was not our intention to evaluate the
effectiveness of the strategies, but the
Volume 90
Number 6
Physical Therapy f
955
Implementation of Measurement Instruments
Table 1.
Summary of Barriers to and Facilitators of the Use of Measurement Instruments Reported in the Interviews
Domain
Barriers
Facilitators
Physical therapist
Competence
Attitude
Lack of knowledge, education, routine, and
experience
Sufficient knowledge and education
Diagnosis focused on ICFa domain: body
functions
Measurement instruments are already used in
daily routine
Resistance to change
Readiness to change
No conviction of additional value on the plan
of care
Positive attitude toward the use of
measurement instruments
Being overloaded with information
Conviction of contribution to quality of physical
therapy care
Headstrong in own working method
Defining therapy outcome otherwise
Lack of confidence in own skills
Organization
Practice
Takes too much time
Patient computer system
No financial compensation
Colleagues
Patient
Absence of practice policy
Presence of practice policy
Lack of discussions, meetings, and feedback
from colleagues
Regular meetings and feedback from colleagues
No adherence to the agreements made
Innovative team and cooperative colleagues
Different expectations and preferences: needs
no measurement instruments, wants only
therapy, and puts pressure on therapist
Patient wants objectives to evaluate outcome of
therapy
Linguistic problems and lack of understanding
Measurement instrument
Poor availability
Good availability
Difficult choice
Feasibility: extensive, difficult interpretation,
and unclear instructions
a
ICFInternational Classification of Functioning, Disability and Health.
therapists were asked whether their
knowledge, attitudes, and use of measurement instruments had changed.
Outcome
Step 2: Problem Analysis
All of the physical therapists who
were invited for the interviews attended the interviews. After 11 interviews with 13 physical therapists, a
saturation of data was reached, and
the interviewing was stopped. The
physical therapists, whose ages
ranged from 22 to 54 years (median43), were interviewed in the
southern region of the Netherlands.
Their working experience varied
from 2 to 30 years (median21), and
956
Physical Therapy
Volume 90
the number of colleagues in the practice varied from 1 to 11 (median6).
The interviewed physical therapists
specialized in different areas. The report of the interview was sent to
each therapist for member checking, and the reports were all in
agreement.
The 13 therapists indicated that they
were familiar with the PSC and
6MWT, but less than half of them
indicated that they used these measures. Almost all interviewed physical therapists were motivated to use
the instruments and were convinced
of the additional value. Barriers and
Number 6
facilitators reported in the interviews are summarized in Table 1.
In the sounding board, discussions
about the identified barriers and facilitators took place. During these
discussions, some physical therapists
were very honest and admitted that
they did not use the measurement
instruments as often as they claimed.
Because of the gap between claiming
to use and actually using the instruments, the physical therapists made
a commitment to use the PSC and
6MWT for 1 month and then discuss
their experiences in a subsequent
meeting. In the second meeting,
they indicated that the instruments
June 2010
Implementation of Measurement Instruments
Table 2.
Planning Model for the Process of Changea
Domain
Phase of Behavioral Change and
Implementation Goals
Implementation Strategies
Physical therapist
Competence
Orientation:
Awareness, interest, and involvement
Insight:
Increasing knowledge and understanding
Attitude
Insight:
Insight into own working method
Acceptance:
Positive attitude and motivation
Intention and decision to change
Change:
Confirmation of the benefit
Organization
Education:
Homework tasks
Practical training and role playing
Self-analysis list:
Increasing awareness, self-reflection, and insight
into own working method
Education:
Discussions about resistance, advantage, and
added value of clinimetrics
Coaching style, own responsibility, individual
learning goals, and interactions with colleagues
Insight:
Insight into own working method
Self-analysis list:
Insight into practice policy
Acceptance:
Positive attitude and motivation
Intention and decision to change
Education:
Discussions and agreements with colleagues,
development of practice policy, and formulation
of learning and practice goals
Change:
Implementation in daily practice
Preservation of change:
Integration in daily routines
Anchoring in the organization
Measurement instrument
KNGF:
Dissemination by publications
Offering education possibilities
Insight:
Increasing knowledge and understanding
Acceptance:
Positive attitude and motivation
Change:
Implementation in daily practice
KNGF:
Embedding in future electronic patient dossier
Adjustments in PSC and 6MWT:
Increasing feasibility and simplifying instructions
Extending PSC activity lists
Education:
Practical training and homework tasks
Formulation of practice policy
Preservation of change:
Integration in daily routines
Anchoring in the organization
a
The developed implementation strategies are based on various domains and phases of behavioral change, each with specific implementation goals.10,16
KNGFKoninklijk Nederland Genootschap voor Fysiotherapie (Royal Dutch Society for Physical Therapy), PSCPatient-Specific Complaints instrument,
6MWTSix-Minute Walk Test.
were useful in daily practice. For
example, 1 therapist previously
thought that he could not use the
instruments because his patients
only wanted therapy and no measurements; however, the patients appreciated the use of the measurement instruments and asked him to
use them regularly to monitor their
progress. These experiences led to
the identification of new barriers and
facilitators, which made the implementation a cyclic process.
June 2010
Step 3: Development of
Implementation Strategies
There is no consensus about the
best general implementation strategy.9,17,25,26 It is clear, however, that
active, multifaceted strategies tailored to a problem analysis are the
most effective.13,16,18,24 In addition,
different models of behavioral
change are recommended, but there
is no agreement about which model
should be used.10,12,14 16 Grol and
colleagues10,16 described a planning
model for the process of change in
which different theories of behavioral change are integrated to induce
changes in professional behavior. Table 2 shows various domains, phases
of behavioral change (orientation, insight, acceptance, change, and preservation of change), and specific implementation goals. On the basis of
this information, we tailored the outcome of the problem analysis to the
appropriate implementation strategies. The definitive strategies, resulting from the project group and
sounding board discussions, were
Volume 90
Number 6
Physical Therapy f
957
Implementation of Measurement Instruments
critically evaluated and readjusted
several times. An overview of these
strategies is shown in Table 2.
To improve the feasibility of using
the PSC and 6MWT, we made several
adjustments:
The instructions were slightly adjusted to improve interpretation.
The original PSC was developed for
patients with low back pain, and
the sample activity list contained
activities with which only those patients would have difficulties. A list
of sample activities was made for
patients with other disorders.
The visual analog scale of the original PSC was replaced with an 11point numerical rating scale. Practical use by the physical therapists
and information from the literature
revealed that this scoring method
was more feasible for some (older)
patients.27 Changing the visual analog scale to a numerical rating scale
did not change the principle of the
test; the scoring methods are highly
correlated.28 A numerical rating
scale also is used in the PainSpecific Functional Scale.20
A self-analysis list was developed to
provide insight into and selfawareness of barriers and phases of
behavioral change. This list was
based on a questionnaire on the selfreported use of outcome measures in
physical therapy and was obtained,
along with other items, from the
problem analysis.7 It contained 3 sections with questions concerning the
phases of change for the physical
therapist, the organization and its
policy, and an inventory of the actual
use of measurement instruments in
daily practice. A few examples of
questions from sections 1 and 2,
rated on a Likert scale, are shown in
the Appendix. The self-analysis list
was pretested by the physical therapists of the sounding board and was
used as a guide for the education
module.
958
Physical Therapy
Volume 90
An education module focusing on
the physical therapist and the practice organization was developed.
The aims of the education module
were to provide insight into the use
of measurement instruments and
phases of behavioral change, to optimize the use of the PSC and 6MWT
in the process of clinical reasoning,
and to fit the use of the PSC and
6MWT to practice policy. The education module consisted of 3 sessions of 2.5 hours. The first 2 sessions were planned to take place
within 1 month, and the last session
was planned to take place after 2
months. The program was not completely determined in advance but
was tailored to the professionals. Active teaching methods, such as discussion and role playing, were used
in a coaching style instead of a teaching style. We expected the attendees
to show an active learning attitude,
initiative, and responsibility.
Steps 4 and 5: Testing and
Evaluation of the
Implementation Plan
Pilot testing and evaluation of the
implementation plan were undertaken. The adjusted instruments, the
self-analysis list, and the education
program were tested with 2 groups
of physical therapists from 4 private
practices in the community. The first
group consisted of colleagues from
the same practice (n11); the second group consisted of colleagues
from 3 different practices (n10).
After each session, the process and
the program were evaluated orally;
after the third session, an evaluation
form was filled out.
The strategies developed could be
applied to physical therapist practice. The evaluation of the adjusted
measurement instruments was positive. The adjusted instructions were
easier to interpret, and the additional
activity lists were useful for determining treatment goals. The selfanalysis list appeared to be valuable
Number 6
because physical therapists became
aware of their own barriers in daily
practice. The link with their phases
of behavioral change was revealing
and stimulated them to use the instruments in daily practice. Working
with heterogeneous groups made it
difficult to accommodate the individual barriers of the physical therapists
but, on the other hand, they could
learn from one another.
After the evaluation of the first pilot
education program, the second program was adjusted at several points.
The program became more fixed in
advance. In the first session, attendees began to devise a practice policy.
Individual learning goals were discussed, and homework tasks were
checked. More time was allocated
for practical rehearsal of the tests.
The outline of the final education
program is shown in Table 3.
All of the physical therapists appreciated the active teaching methods,
discussions, and role playing during
training. Developing a practice policy was an issue of major importance, especially for the preservation
of change. During busy daily practice, the therapists never took the
time to discuss these matters.
The physical therapists indicated
that they were interested in practicing with other instruments besides
the PSC and 6MWT and would appreciate sets of short, feasible, and
methodologically sound instruments. At the last meeting, most
physical therapists indicated that
they actually used both instruments.
Discussion
In this report, we have shown that it
is possible to develop and evaluate a
systematic implementation plan for
the use of 2 measurement instruments. A thorough analysis was used
to identify practical barriers and facilitators. In the interviews and discussions, we could continue asking
June 2010
Implementation of Measurement Instruments
Table 3.
Outline of the Education Programa
Day
1
Main Issues
Goals
Working Methods
Introduction
Explicating expectations of therapists:
active learning attitude, responsibility,
initiative, active teaching methods, and
coaching style
Plenary
Self-analysis list
Insight into own working method and
phase of behavior
Individual
Individual learning goals and practice
policy
Responsibility for own learning process in
professional and practice organization
domains
Working group of 3 or 4 people
Advantages and disadvantages of
PSC and 6MWT
Insight and acceptance
Plenary
Training on PSC: clarification of the
patients main complaint
Increasing knowledge and practical skills
Working group of 3 or 4 people
Homework on PSC
Using PSC in practice for the next month
Plenary
Evaluation of the session
Reflection
Plenary
Results of self-analysis list
Insight on working method and phase of
behavior
Presentation
Evaluation of homework task
Insight and acceptance
Plenary
Training on 6MWT: standardization
and interpretation
Knowledge and practical skills
Working group of 3 or 4 people
Use of measurement instruments in
practice policy
Integration in the practice organization to
obtain (or preserve) change
Working group of 3 of 4 people
Homework on 6MWT
Using 6MWT in practice for the next 2 mo
Plenary
Evaluation of the session
Reflection
Plenary
Evaluation of homework task
Insight and acceptance
Plenary
Theory of clinimetrics
Insight and knowledge
Lecture
Step-by-step plan to search for other
measurement instruments
Transfer to the use of other instruments
Lecture
Evaluation of practice policy
Integration in the practice organization to
obtain (preserve) change
Working group of 3 or 4 people
Integration of instruments in clinical
reasoning and daily practice
Preservation of behavioral change
Plenary
Written and oral evaluations of total
education module
Reflection
Plenary and individual
PSCPatient-Specific Complaints instrument, 6MWTSix-Minute Walk Test.
about underlying thoughts and possible solutions and strategies. In this
way, the problem analysis produced
a larger amount of information than
earlier reports, in which only written
inquiries were used.4 8,29 31 The revealed factors matched the barriers
and facilitators described in the
literature.4,6 8,29,30,32
Many studies2,4 8,14,29 32 have focused on identifying the extent of
use of measurement instruments as
well as factors that affect that use.
June 2010
We took the additional steps of developing various strategies based on
these factors and evaluating their applicability in a pilot program in several physical therapist practices. The
involvement of a sounding board
during the development phase guaranteed interest in and acceptance of
the implementation strategies by the
target group.12,14,15
Starting education with self-analysis
provides therapists with the opportunity to formulate their own learn-
ing goals, and trainers can tailor strategies to the professionals as well as
the organization. This approach
has been recommended in other
studies.13,18
Using the planning model of Grol
and colleagues10,16 for the process of
change, we were able to tailor multifaceted strategies to various barriers and phases of behavioral change.
In this way, a change in behavior was
initiated. The physical therapists indicated that they used the measure-
Volume 90
Number 6
Physical Therapy f
959
Implementation of Measurement Instruments
ment instruments more often, and
they were convinced that doing so
contributed to the process of clinical reasoning. For the preservation
of change, more time is needed.
It is evident that quality improvements should start with small, simple
projects.23 This case report involved
a small group of selected physical
therapists in the southern region of
the Netherlands; therefore, generalization of the results is unjustifiable.
Further studies and additional designs with other measurement instruments are needed to evaluate the
effects of implementation strategies.
Our recommendations for the policy
of the Royal Dutch Society for Physical Therapy are as follows. First, information about measurement instruments should be disseminated
through publication in professional
journals, newsletters, and guidelines.
This strategy represents the orientation phase, in which awareness of
the existence and use of measurement instruments is an important issue. The information should not be
restricted to the measurement instruments alone but also should focus on
how to use and interpret the results
of the instruments in daily practice.
Second, educational opportunities
should be offered for physical therapists to increase their knowledge
and skills regarding the use of these
and other measurement instruments
in the process of clinical reasoning,
with attention to behavioral change.
This education should be included
in mainstream physical therapist
schools. Third, the measurement instruments should be embedded in
the future electronic patient dossier.
The actual use of measurement instruments should not be the only objective in implementation programs.
The integration of the instruments in
the process of clinical reasoning is of
major importance. Therefore, future
programs should focus not only on
960
Physical Therapy
Volume 90
the physical therapist but also on the
practice organization and professional associations.
Both authors provided concept/idea/project
design, writing, and project management.
Ms Stevens provided data collection and
analysis. Dr Beurskens provided fund procurement and facilities/equipment.
The authors are grateful to members of
the project group (Dr Rob de Bie, Dr Erik
Hendriks, Mr Pieter Wolters, Dr Raymond
Swinkels, Mrs Anja van den Donk, and Mr
John Meijers) and the sounding board (the
physical therapists interviewed).
This work was funded by the Dutch Scientific
College Physiotherapy of the Royal Dutch
Society for Physical Therapy (TD/2008/01).
This work, in part, was presented at the Annual Congress of the Royal Dutch Society for
Physical Therapy; November 9, 2007; Amsterdam, the Netherlands.
This article was received March 30, 2009, and
was accepted February 24, 2010.
DOI: 10.2522/ptj.20090105
References
1 Glasziou P, Irwig L, Mant D. Monitoring in
chronic disease: a rational approach. BMJ.
2005;330:644 648.
2 Haigh R, Tennant A, Biering-Sorensen F,
et al. The use of outcome measures in
physical medicine and rehabilitation
within Europe. J Rehabil Med. 2001;33:
273278.
3 Jette DU, Bacon K, Batty C, et al. Evidencebased practice: beliefs, attitudes, knowledge, and behaviors of physical therapists.
Phys Ther. 2003;83:786 805.
4 Abrams D, Davidson M, Harrick J, et al.
Monitoring the change: current trends in
outcome measure usage in physiotherapy.
Man Ther. 2006;11:46 53.
5 Leemrijse CJ, Plas GM, Hofhuis H, van den
Ende CH. Compliance with the guidelines
for acute ankle sprain for physiotherapists
is moderate in the Netherlands: an observational study. Aust J Physiother. 2006;52:
293299.
6 Maher C, Williams M. Factors influencing
the use of outcome measures in physiotherapy management of lung transplant
patients in Australia and New Zealand. Physiother Theory Pract. 2005;21:201217.
7 Van Peppen RP, Maissan FJ, Van Genderen
FR, et al. Outcome measures in physiotherapy management of patients with
stroke: a survey into self-reported use, and
barriers to and facilitators for use. Physiother Res Int. 2008;13: 255270.
Number 6
8 Pisters M, Leemrijse C. Het gebruik van
aanbevolen meetinstrumenten in de fysiotherapiepraktijk. Weten is nog geen meten! [The use of measurement instruments
in physiotherapy practice. Knowing it
isnt measuring it!] Nederlands Tijdschrift
voor Fysiotherapie. 2007;5:176 180.
9 Grimshaw JM, Shirran L, Thomas R, et al.
Changing provider behavior: an overview
of systematic reviews of interventions.
Med Care. 2001;39(8 suppl 2):112145.
10 Grol R, Wensing M, Eccles M. Improving
Patient Care: The Implementation of
Change in Clinical Practice. Edinburgh,
Scotland: Elsevier Butterworth Heineman;
2005.
11 Grimshaw JM, McAuley LM, Bero LA, et al.
Systematic reviews of the effectiveness of
quality improvement strategies and programmes. Qual Saf Health Care. 2003;12:
298 303.
12 Berwick DM. Disseminating innovations in
health care. JAMA. 2003;289:1969 1975.
13 Bosch M, van der Weyden T, Wensing MG,
Grol R. Tailoring quality improvement interventions to identified barriers: a multiple case analysis. J Eval Clin Pract. 2007;
13:161168.
14 Garland AF, Kruse M, Aarons GA. Clinicians and outcome measurement: whats
the use? J Behav Health Serv Res. 2003;
30:393 405.
15 Grol R, Grimshaw JM. From best evidence
to best practice: effective implementation
of change in patients care. Lancet. 2003;
362:12251230.
16 Grol R, Wensing M. What drives change:
barriers to and incentives for achieving
evidence-based practice. Med J Aust.
2004;180(6 suppl):S57S60.
17 Haines A, Kuruvilla S, Borchert M. Bridging the implementation gap between
knowledge and action for health. Bull
World Health Organ. 2004;82:724 731;
discussion 732.
18 Shaw B, Cheater F, Baker R, et al. Tailored
interventions to overcome identified barriers to change: effects on professional
practice and health care outcomes.
Cochrane Database Syst Rev. 2005;3:
CD005470.
19 Beurskens AJ, de Vet HC, Koke AJ. Responsiveness of functional status in low
back pain: a comparison of different instruments. Pain. 1996;65:7176.
20 Stratford PW, Gill C, Westaway M, Binkley
JM. Assessing disability and change on individual patients: a report of a patientspecific measure. Physiother Can. 1995;
47:258 263.
21 Butland RJ, Pang J, Gross ER, et al. Two-,
six-, and 12-minute walking tests in respiratory disease. Br Med J (Clin Res Ed).
1982;284:16071608.
22 Strauss ALC. Basics of Qualitative Research: Techniques and Procedures for
Developing Grounded Theory. Thousand
Oaks, CA: Sage Publications; 1998.
June 2010
Implementation of Measurement Instruments
23 Geboers H, Mokkink H, van Montfort P,
et al. Continuous quality improvement in
small general medical practices: the attitudes of general practitioners and other
practice staff. Int J Qual Health Care.
2001;13:391397.
24 van der Wees PJ, Jamtvedt G, Rebbeck T,
et al. Multifaceted strategies may increase
implementation of physiotherapy clinical
guidelines: a systematic review. Aust J
Physiother. 2008;54:233241.
25 Bekkering GE, Engers AJ, Wensing M, et al.
Development of an implementation strategy
for physiotherapy guidelines on low back
pain. Aust J Physiother. 2003;49:208 214.
26 Grimshaw JM, Thomas RE, MacLennan G,
et al. Effectiveness and efficiency of guideline dissemination and implementation
strategies. Health Technol Assess. 2004;8:
iiiiv, 172.
27 Peters ML, Patijn J, Lame I. Pain assessment
in younger and older pain patients: psychometric properties and patient preference
of five commonly used measures of pain
intensity. Pain Med. 2007; 8:601 610.
28 Williamson A, Hoggart B. Pain: a review of
three commonly used pain rating scales.
J Clin Nurs. 2005;14:798 804.
29 Metcalfe CL, Lewin R, Wisher S, et al. Barriers to implementing the evidence base in
four NHS therapies: dieticians, occupational therapists, physiotherapists, speech
and language therapists. Physiotherapy.
2001;87:433 441.
30 Pollock AS, Legg L, Langhorne P, Sellars C.
Barriers to achieving evidence-based
stroke rehabilitation. Clin Rehabil. 2000;
14:611 617.
31 Jette DU, Halbert J, Iverson C, et al. Use of
standardized outcome measures in physical therapist practice: perceptions and applications. Phys Ther. 2009;89:125135.
32 Copeland JM, Taylor WJ, Dean SG. Factors
influencing the use of outcome measures
for patients with low back pain: a survey
of New Zealand physical therapists. Phys
Ther. 2008;88:14921505.
Appendix.
Examples of Questions in the Self-Analysis Lista
Questions
Fully
Disagree
Disagree
Neither
Agree nor
Disagree
Agree
Fully
Agree
Section 1: questions about yourself
I am able to interpret the outcome of measurement
instruments in the right way
I think it is important to document patient data in
an objective way
I think that the use of measurement instruments
does not take too much of my time
The use of measurement instruments is a fixed part
of my methodical approach
Section 2: questions about policy in your practice
In my practice, enough measurement instruments
are available
My supervisor supports employees in using
measurement instruments
The colleagues in my practice use measurement
instruments
a
The complete list is available on request from the authors.
June 2010
Volume 90
Number 6
Physical Therapy f
961
Reproduced with permission of the copyright owner. Further reproduction prohibited without permission.
S-ar putea să vă placă și
- Action Plan in School LibraryDocument3 paginiAction Plan in School LibraryRosanno David93% (15)
- Education: Nur Atiqah Nabilah RazaliDocument1 paginăEducation: Nur Atiqah Nabilah RazaliAtiqah Nabilah RazaliÎncă nu există evaluări
- KN ClinicalGuidelines2Document2 paginiKN ClinicalGuidelines2Mhmd IrakyÎncă nu există evaluări
- Use of Patient Preference Studies in HTA Decision Making: A NICE PerspectiveDocument5 paginiUse of Patient Preference Studies in HTA Decision Making: A NICE Perspectiveaxel pqÎncă nu există evaluări
- Outcome Assessment in Routine Clinical Practice inDocument21 paginiOutcome Assessment in Routine Clinical Practice inicuellarfloresÎncă nu există evaluări
- Medidas en FT ImporDocument10 paginiMedidas en FT Imporleidy tatiana clavijo canoÎncă nu există evaluări
- Conjoint in HEALTH ResearchDocument17 paginiConjoint in HEALTH ResearchDiana Tan May KimÎncă nu există evaluări
- COSMINDocument9 paginiCOSMINTamires NunesÎncă nu există evaluări
- Patient-Reported Physical Activity Questionnaires A Systematic Review of Content and FormatDocument18 paginiPatient-Reported Physical Activity Questionnaires A Systematic Review of Content and FormatHanif FakhruddinÎncă nu există evaluări
- Published Researches in The Year 2010Document16 paginiPublished Researches in The Year 2010hsrimediaÎncă nu există evaluări
- Which Tool GuideDocument10 paginiWhich Tool GuideVina EmpialesÎncă nu există evaluări
- Patient CenteredDocument12 paginiPatient CenteredNina NaguyevskayaÎncă nu există evaluări
- Smart Body Metric Measuring MachineDocument22 paginiSmart Body Metric Measuring MachineIshimwe Moise SeboÎncă nu există evaluări
- GeografoDocument19 paginiGeografoSzelca Frien ZuñigaÎncă nu există evaluări
- 556-Appropriateness of Clinical Decision Support - Final White Paper-Wei WuDocument15 pagini556-Appropriateness of Clinical Decision Support - Final White Paper-Wei Wuapi-398506399Încă nu există evaluări
- Review Literature Hand Hygiene ComplianceDocument5 paginiReview Literature Hand Hygiene Complianceixevojrif100% (1)
- Developing A Theory-Based Instrument To Assess The Impact of Continuing Professional Development Activities On Clinical Practice: A Study ProtocolDocument6 paginiDeveloping A Theory-Based Instrument To Assess The Impact of Continuing Professional Development Activities On Clinical Practice: A Study ProtocolSjktraub PahangÎncă nu există evaluări
- Etoshow QuityDocument8 paginiEtoshow QuityAr JayÎncă nu există evaluări
- The Common Threads in ProgramDocument5 paginiThe Common Threads in Programdate6Încă nu există evaluări
- Fasilita RefDocument10 paginiFasilita RefsukrangÎncă nu există evaluări
- Quality Improvement ModelsDocument64 paginiQuality Improvement ModelsShahin Patowary100% (2)
- Implications in Practice and Conclusions - EditedDocument11 paginiImplications in Practice and Conclusions - EditedAtanas WamukoyaÎncă nu există evaluări
- Work-Related Medical RehabilitDocument12 paginiWork-Related Medical RehabilitMonicawindyÎncă nu există evaluări
- HospitalDocument7 paginiHospitalBENNY WAHYUDIÎncă nu există evaluări
- Utility of Evidence Based NursngDocument12 paginiUtility of Evidence Based NursngrovicaÎncă nu există evaluări
- An To Patient-Reported Outcome Measures (Proms) in PhysiotherapyDocument7 paginiAn To Patient-Reported Outcome Measures (Proms) in PhysiotherapyAline VidalÎncă nu există evaluări
- Policy FrameworksDocument61 paginiPolicy FrameworksaninnaninÎncă nu există evaluări
- 2016 Slade CERTDocument30 pagini2016 Slade CERTdamicarbo_297070015Încă nu există evaluări
- Implementation Strategies and Outcomes For Occupational Therapy in Adult Stroke Rehabilitation: A Scoping ReviewDocument26 paginiImplementation Strategies and Outcomes For Occupational Therapy in Adult Stroke Rehabilitation: A Scoping ReviewNataliaÎncă nu există evaluări
- Short-And Long-Term Effects of A Quality Improvement Collaborative On Diabetes ManagementDocument10 paginiShort-And Long-Term Effects of A Quality Improvement Collaborative On Diabetes ManagementBhisma SyaputraÎncă nu există evaluări
- Outcome Research Methodology: BY Sumaira Naz BSN, MPHDocument40 paginiOutcome Research Methodology: BY Sumaira Naz BSN, MPHFatima AnxariÎncă nu există evaluări
- JHD 11 jhd220549Document19 paginiJHD 11 jhd220549NataliaÎncă nu există evaluări
- Module 7 - EBP 2012-2013Document1 paginăModule 7 - EBP 2012-2013EspilfoviÎncă nu există evaluări
- Physical Therapy Tests in Stroke RehabilitationDocument22 paginiPhysical Therapy Tests in Stroke Rehabilitationmehdi.chlif4374Încă nu există evaluări
- Updated Integrated FrameworkDocument17 paginiUpdated Integrated FrameworkE. Jimmy Jimenez TordoyaÎncă nu există evaluări
- Applying The Analytic Hierarchy Process in Healthcare Research: A Systematic Literature Review and Evaluation of ReportingDocument27 paginiApplying The Analytic Hierarchy Process in Healthcare Research: A Systematic Literature Review and Evaluation of Reportingnormand67Încă nu există evaluări
- 1 Pressure Ulcer Case StudyDocument6 pagini1 Pressure Ulcer Case StudyTony MutisyaÎncă nu există evaluări
- A Comparative Analysis of Six Audit Systems For Mental Health NursingDocument10 paginiA Comparative Analysis of Six Audit Systems For Mental Health NursingByArdieÎncă nu există evaluări
- Clinical PracticeDocument10 paginiClinical PracticeLenny Ronalyn QuitorianoÎncă nu există evaluări
- Research Article Postop Recovery ProfileDocument8 paginiResearch Article Postop Recovery ProfileNi'mahÎncă nu există evaluări
- Value Based Healthcare Initiatives in Practice A.5Document26 paginiValue Based Healthcare Initiatives in Practice A.5Mario Luna BracamontesÎncă nu există evaluări
- Factors Influencing The Implementation of Clinical Guidelines ForDocument11 paginiFactors Influencing The Implementation of Clinical Guidelines ForFhiserra RharaÎncă nu există evaluări
- A Treatment Schedule of Conventional Physical Therapy Provided To Enhance Upper Limb Sensorimotor Recovery After Stroke Expert Criterion Validity and Intra-Rater ReliabilityDocument10 paginiA Treatment Schedule of Conventional Physical Therapy Provided To Enhance Upper Limb Sensorimotor Recovery After Stroke Expert Criterion Validity and Intra-Rater ReliabilityGeraldo MoraesÎncă nu există evaluări
- A Practical Guide To Using Service User Feedback Outcome ToolsDocument99 paginiA Practical Guide To Using Service User Feedback Outcome ToolsPeter LawsonÎncă nu există evaluări
- MS-747 - Unit 23 - FORIDADocument24 paginiMS-747 - Unit 23 - FORIDANijam DulonÎncă nu există evaluări
- Updated Integrated Framework For Making Clinical Decisions Across The Lifespan and Health ConditionsDocument13 paginiUpdated Integrated Framework For Making Clinical Decisions Across The Lifespan and Health ConditionsmaryelurdesÎncă nu există evaluări
- Clinical Practice Guideline For Physical Therapist Management of People With Rheumatoid ArthritisDocument16 paginiClinical Practice Guideline For Physical Therapist Management of People With Rheumatoid Arthritis1541920001 LUIS GUILLERMO PAJARO FRANCO ESTUDIANTE ACTIVO ESPECIALIDAD MEDICINA INTERNAÎncă nu există evaluări
- Eip Gpe Eqc 2003 1Document24 paginiEip Gpe Eqc 2003 1rhuÎncă nu există evaluări
- IFOMPT Examination Cervical Spine Doc September 2012 DefinitiveDocument37 paginiIFOMPT Examination Cervical Spine Doc September 2012 DefinitiveMichel BakkerÎncă nu există evaluări
- SGPP Bestpracticescriteria en 0Document11 paginiSGPP Bestpracticescriteria en 0testÎncă nu există evaluări
- Omeract 3-799Document4 paginiOmeract 3-799damien333Încă nu există evaluări
- Healthcare Analytics 012Document9 paginiHealthcare Analytics 012bennettsabastin186Încă nu există evaluări
- tmp7BD7 TMPDocument25 paginitmp7BD7 TMPFrontiersÎncă nu există evaluări
- Rounsaville. A Stage of Behavioral Therapies ResearchDocument10 paginiRounsaville. A Stage of Behavioral Therapies ResearchRubí Corona TápiaÎncă nu există evaluări
- 2016 Article 1371Document10 pagini2016 Article 1371boyÎncă nu există evaluări
- Introduction to Clinical Effectiveness and Audit in HealthcareDe la EverandIntroduction to Clinical Effectiveness and Audit in HealthcareÎncă nu există evaluări
- 5com. Med - Mang.modified11Document22 pagini5com. Med - Mang.modified11Saad MotawéaÎncă nu există evaluări
- 2020 Model and Process For Nutrition and Dietetic Practice 1Document20 pagini2020 Model and Process For Nutrition and Dietetic Practice 1Saba TanveerÎncă nu există evaluări
- Implementation of A Multidisciplinary Guideline For Low Back Pain Process Evaluation Among Health Care ProfessionalsDocument12 paginiImplementation of A Multidisciplinary Guideline For Low Back Pain Process Evaluation Among Health Care Professionalscallisto69Încă nu există evaluări
- Integrated Care PathwayDocument3 paginiIntegrated Care PathwayFitri EmiÎncă nu există evaluări
- Ghid de OsteoporozaDocument55 paginiGhid de OsteoporozaMarius Creanga100% (1)
- 9.50 - 10.35 Mark Laslett Patho-Anatomic SourcesDocument78 pagini9.50 - 10.35 Mark Laslett Patho-Anatomic SourcesNelsonRodríguezDeLeónÎncă nu există evaluări
- Unraveling The Challenge of Head and Face Pain: EditorialDocument1 paginăUnraveling The Challenge of Head and Face Pain: EditorialNelsonRodríguezDeLeónÎncă nu există evaluări
- PolarityDocument13 paginiPolarityNelsonRodríguezDeLeónÎncă nu există evaluări
- Physical Exercise Intervention in Depressive Disorders: Meta-Analysis and Systematic ReviewDocument14 paginiPhysical Exercise Intervention in Depressive Disorders: Meta-Analysis and Systematic ReviewNelsonRodríguezDeLeónÎncă nu există evaluări
- Unstable Surface Improves Quadriceps:Hamstring Co-Contraction For Anterior Cruciate Ligament Injury Prevention StrategiesDocument6 paginiUnstable Surface Improves Quadriceps:Hamstring Co-Contraction For Anterior Cruciate Ligament Injury Prevention StrategiesNelsonRodríguezDeLeónÎncă nu există evaluări
- Research Booklet LLLT July2014Document36 paginiResearch Booklet LLLT July2014NelsonRodríguezDeLeónÎncă nu există evaluări
- A Randomized Clinical Trial of The Effectiveness of Mechanical Traction For Sub-Groups of Patients With Low Back Pain: Study Methods and RationaleDocument10 paginiA Randomized Clinical Trial of The Effectiveness of Mechanical Traction For Sub-Groups of Patients With Low Back Pain: Study Methods and RationaleNelsonRodríguezDeLeónÎncă nu există evaluări
- Yoga and Distractibility: Lee N. Burkett, PH.D., Megan A. Todd, M.S., Troy Adams, PH.DDocument11 paginiYoga and Distractibility: Lee N. Burkett, PH.D., Megan A. Todd, M.S., Troy Adams, PH.DNelsonRodríguezDeLeónÎncă nu există evaluări
- Activity Design For SSG Election 2021Document3 paginiActivity Design For SSG Election 2021ROZEL MALIFICIADO100% (2)
- Parent Presentation-Spring Registration Resources 9-11 2 22Document29 paginiParent Presentation-Spring Registration Resources 9-11 2 22api-548723359Încă nu există evaluări
- Task-Based Language Teaching (TBLT)Document17 paginiTask-Based Language Teaching (TBLT)AlexanderBarreraÎncă nu există evaluări
- Lesson Plan-MicroteachingDocument2 paginiLesson Plan-MicroteachingSella RanatasiaÎncă nu există evaluări
- Teaching Pronunciation Without Using Imitation: Why and How - Messum (2012)Document7 paginiTeaching Pronunciation Without Using Imitation: Why and How - Messum (2012)Pronunciation ScienceÎncă nu există evaluări
- Sean M. SullivanDocument1 paginăSean M. Sullivanapi-309930792Încă nu există evaluări
- Lesson 1 TPDocument2 paginiLesson 1 TPapi-228848608Încă nu există evaluări
- DLL Math Grade10 Quarter3 Week10 (Palawan Division)Document8 paginiDLL Math Grade10 Quarter3 Week10 (Palawan Division)MICHAEL MAHINAYÎncă nu există evaluări
- Regional Safeguarding Standards During Online Interaction With Learners 1Document85 paginiRegional Safeguarding Standards During Online Interaction With Learners 1Tanglaw Laya May PagasaÎncă nu există evaluări
- Theories of LLDocument55 paginiTheories of LLMoe ElÎncă nu există evaluări
- SOCSTUD 102 (World Hist & Civ 1)Document17 paginiSOCSTUD 102 (World Hist & Civ 1)Frederick W GomezÎncă nu există evaluări
- Susan Pinker Review ArticleDocument2 paginiSusan Pinker Review ArticleMuhammad Ali NasirÎncă nu există evaluări
- Dividing Fractions Performance TaskDocument9 paginiDividing Fractions Performance TaskRyan McLeanÎncă nu există evaluări
- Cbar 2Document14 paginiCbar 2Chessa Mae PelongcoÎncă nu există evaluări
- MRF (MT) - Surname, First Name - Sy2022-2023Document2 paginiMRF (MT) - Surname, First Name - Sy2022-2023Romeo PilongoÎncă nu există evaluări
- LeannacrewsresumestcDocument3 paginiLeannacrewsresumestcapi-250337748Încă nu există evaluări
- Grammar Lesson Plan, English. Year4Document1 paginăGrammar Lesson Plan, English. Year4Kasthuri Bai ThangarajahÎncă nu există evaluări
- CPARW1Document2 paginiCPARW1Glenda ValerosoÎncă nu există evaluări
- Certification Manual 5 20180511Document51 paginiCertification Manual 5 20180511Grupo Musical EuforiaÎncă nu există evaluări
- I. Objectives: Daily Lesson Log School: Grade Level: Teacher: Learning Area: Teaching Date: Quarter: Teaching TimeDocument5 paginiI. Objectives: Daily Lesson Log School: Grade Level: Teacher: Learning Area: Teaching Date: Quarter: Teaching TimeMelanie BitangÎncă nu există evaluări
- Evaluation of ExercisesDocument78 paginiEvaluation of Exercisestitoglasgow100% (1)
- Classification of Standardized Achievement Test TestsDocument6 paginiClassification of Standardized Achievement Test TestskamilbismaÎncă nu există evaluări
- Notes For Letter of ExplanationDocument4 paginiNotes For Letter of ExplanationHHÎncă nu există evaluări
- DLL in Math Week 4, Q3Document4 paginiDLL in Math Week 4, Q3Leonard Plaza100% (3)
- Em 314Document32 paginiEm 314Aristotle GonzalesÎncă nu există evaluări
- English As A Second Language GuidelinesDocument10 paginiEnglish As A Second Language GuidelinesNataliaÎncă nu există evaluări
- Reflection Paper in Multigrade SchoolDocument7 paginiReflection Paper in Multigrade SchoolEden Aniversario0% (1)
- Community Helpers LessonDocument4 paginiCommunity Helpers Lessonapi-302422167Încă nu există evaluări