Documente Academic
Documente Profesional
Documente Cultură
Pad Vs PVD Chart
Încărcat de
JonathonTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Pad Vs PVD Chart
Încărcat de
JonathonDrepturi de autor:
Formate disponibile
CHAPTER 38 Vascular Disorders
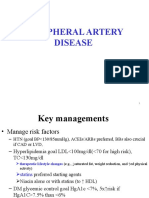
TABLE 38-2
CHARACTERISTIC
Peripheral pulses
Capillary refill
Ankle-brachial index
Edema
Hair
Ulcer
Location
Margin
Drainage
Tissue
Pain
Nails
Skin color
COMPARISON OF PERIPHERAL
ARTERY AND VENOUS DISEASE
PERIPHERAL
ARTERY
DISEASE
Tips of toes,
foot, or lateral
malleolus
Rounded,
smooth, looks
punched out
Minimal
Near medial malleolus
Thin, shiny, taut
Skin temperature
Cool, temperature
gradient down
the leg
Rarely occurs
Rarely occurs
Dermatitis
Pruritus
VENOUS DISEASE
Present; may be difficult
to palpate with edema
<3 sec
>0.91
Lower leg edema
Skin texture
COLLABORATIVE CARE
Peripheral Artery Disease
Diagnostic
Decreased or
absent
>3 sec
<0.70
Absent unless
leg constantly
in dependent
position
Loss of hair on
legs, feet, toes
Black eschar
or pale pink
granulation
Intermittent
claudication
or rest pain in
foot; ulcer may
or may not be
painful
Thickened; brittle
Dependent rubor;
elevation pallor
TABLE 38-3
875
Health history and physical examination, including palpation of
peripheral pulses
Doppler ultrasound studies
Segmental blood pressures
Ankle-brachial index
Duplex imaging
Angiogram
Magnetic resonance angiography
Collaborative Therapy
Hair may be present
or absent
Irregularly shaped
Moderate to large
amount
Yellow slough or
dark red, ruddy
granulation
Dull ache or heaviness
in calf or thigh; ulcer
often painful
Normal or thickened
Bronze-brown
pigmentation; varicose
veins may be visible
Skin thick, hardened,
and indurated
Warm, no temperature
gradient
Frequently occurs
Frequently occurs
PAD, the Doppler can determine the degree of blood flow.
Apalpable pulse and a Doppler pulse are not equivalent, and
the terms are not interchangeable. Segmental blood pressures
are obtained (using Doppler ultrasound and a sphygmomanometer) at the thigh, below the knee, and at ankle level while
the patient is supine. A drop in segmental BP of greater than
30mm Hg suggests PAD.
The ankle-brachial index (ABI) is performed using a handheld Doppler. The ABI is calculated by dividing the ankle systolic BPs by the higher of the left and right brachial systolic BP.17
A normal ABI is 0.91 to 1.30 and indicates adequate BP in the
extremities. An ABI between 0.71 and 0.90 indicates mild PAD,
between 0.41 and 0.70 indicates moderate PAD, and less than
0.40 indicates severe PAD. The ABI also is used after revascularization to monitor bypass graft patency. An ABI has limited
usefulness when arteries are calcified and noncompressible, as
occurs in patients with diabetes mellitus. In these patients, the
ABI frequently is falsely elevated.
Angiography and magnetic resonance angiography delineate
the location and extent of PAD. In addition, they provide information on inflow and outflow vessels to plan for surgery (see
Table 32-6).
Cardiovascular disease risk factor modification
Smoking cessation
Regular physical exercise
Achieve/maintain ideal body weight
Follow Dietary Approaches to Stop Hypertension (DASH) diet
(see Table 33-7)
Tight glucose control in diabetics
Tight blood pressure control
Treatment of hyperlipidemia and hypertriglyceridemia (see
Table 34-6)
Antiplatelet agent (aspirin or clopidogrel [Plavix])
Angiotensin-converting enzyme inhibitors (see Table 33-8)
Treatment of claudication symptoms
Structured walking/exercise program
Cilostazol (Pletal)
Pentoxifylline (Trental)
Nutrition therapy
Proper foot care (Table 49-22)
Percutaneous transluminal balloon angioplasty with or without
stent
Percutaneous transluminal atherectomy
Percutaneous transluminal cryoplasty
Peripheral artery bypass surgery
Patch graft angioplasty, often in conjunction with bypass surgery
Endarterectomy (for localized stenosis but rarely done)
Thrombolytic therapy (for acute ischemia only)
Amputation
Collaborative Care
Table 38-3 summarizes the collaborative care for a patient
with PAD.
Risk Factor Modification. Due to the high risk for MI, ischemic stroke, and CVD-related death, the first treatment goal is to
aggressively modify CVD risk factors in all patients with PAD
regardless of the severity of symptoms.9,29,30 Risk factors need
to be modified not only with drug therapy but also with lifestyle
changes on the part of the patient and caregiver (see Table 34-5).
Nurse-led clinics have been effective for managing CVD risk factors with PAD.31
Smoking cessation is essential in the management of patients
with PAD to reduce the risk of CVD events and mortality.
Smoking cessation is a complex and difficult process with a high
incidence of smoking relapse. All patients with PAD should
have access to comprehensive smoking cessation interventions.
(Tables 12-4, 12-5, 12-6, and 12-7 discuss smoking cessation.)
Current guidelines recommend aggressive lipid management for all PAD patients with the following goals: low-density
lipoprotein (LDL) less than 100 mg/dL, triglycerides less than
150 mg/dL, and high-density lipoprotein (HDL) greater than
40 mg/dL.9,29 Although dietary change is also recommended,
this alone is unlikely to achieve these goals. Research indicates
that treatment of PAD patients with a statin (e.g., simvastatin
S-ar putea să vă placă și
- Managing Cardiovascular Complications in DiabetesDe la EverandManaging Cardiovascular Complications in DiabetesÎncă nu există evaluări
- Review Article: Peripheral Arterial Disease in Diabetes - A ReviewDocument28 paginiReview Article: Peripheral Arterial Disease in Diabetes - A ReviewTeisha JVÎncă nu există evaluări
- Diabetes and Peripheral Artery DiseaseDocument30 paginiDiabetes and Peripheral Artery DiseasedrbrdasÎncă nu există evaluări
- Hypertension ManagementDocument47 paginiHypertension ManagementBagus Andi PramonoÎncă nu există evaluări
- CAD - Ischemic Heart Disease: AtherosclerosisDocument5 paginiCAD - Ischemic Heart Disease: Atherosclerosisbri ngÎncă nu există evaluări
- Diagnosis and Management in Peripheral Artery Disease EditedDocument5 paginiDiagnosis and Management in Peripheral Artery Disease Editedwahyu suparnoÎncă nu există evaluări
- Cardiovascular Physical TherapDocument7 paginiCardiovascular Physical TherapJadie Prenio100% (4)
- Cardiovascular Disease and Risk ManagementDocument25 paginiCardiovascular Disease and Risk ManagementYhang L TamaÎncă nu există evaluări
- PAD Handout 4thDocument27 paginiPAD Handout 4thdawitÎncă nu există evaluări
- Aztor Cme NewDocument59 paginiAztor Cme NewSheikh Sharfuddin RajeevÎncă nu există evaluări
- Cardio Ms Hand OutDocument10 paginiCardio Ms Hand OutVictor ShonÎncă nu există evaluări
- Lipids Module 4Document16 paginiLipids Module 4angelmedurÎncă nu există evaluări
- Secondary Prevention SlideDocument14 paginiSecondary Prevention Slideagungnugoho4247Încă nu există evaluări
- Angina Pectoris Treatment & Management - Medical Care, Surgical Care, PreventionDocument20 paginiAngina Pectoris Treatment & Management - Medical Care, Surgical Care, Preventionblack_eagel100% (1)
- Arterial Diseases 1Document32 paginiArterial Diseases 1ningappaÎncă nu există evaluări
- EpidemiologyDocument5 paginiEpidemiologyMylene MendozaÎncă nu există evaluări
- DiabetesClinicalPaper en 2011Document24 paginiDiabetesClinicalPaper en 2011Okky Winang SaktyawanÎncă nu există evaluări
- Prof - Dr.Medhat Ashmawy Professor of Cardiology, Tanta UniversityDocument104 paginiProf - Dr.Medhat Ashmawy Professor of Cardiology, Tanta UniversityThe department of cardiovascular medicineÎncă nu există evaluări
- Nicyela Vascular DiseaseDocument21 paginiNicyela Vascular DiseaseNicyela JillienÎncă nu există evaluări
- Management PADDocument8 paginiManagement PADAnonymous Af24L7Încă nu există evaluări
- Cardiovascular Complication in CKD 28.8.18Document65 paginiCardiovascular Complication in CKD 28.8.18Hemanth PrakashÎncă nu există evaluări
- Diagnosis and Treatment of Peripheral Arterial DiseaseDocument5 paginiDiagnosis and Treatment of Peripheral Arterial Diseasedrpiratheepan4274Încă nu există evaluări
- TOPIC1Chronic Forms of Coronary Heart DiseaseDocument3 paginiTOPIC1Chronic Forms of Coronary Heart DiseaseAdi PomeranzÎncă nu există evaluări
- Hipertensi - Interna - Dr. MuzakkirDocument43 paginiHipertensi - Interna - Dr. MuzakkirFarnida JamhalÎncă nu există evaluări
- Deep Vein Thrombosis (DVT)Document15 paginiDeep Vein Thrombosis (DVT)arcci balinasÎncă nu există evaluări
- U World Cardiac FinalDocument15 paginiU World Cardiac FinalAcohCChaoÎncă nu există evaluări
- Hypertension: Dr. Lucia Mazur-Nicorici Md. PHDDocument34 paginiHypertension: Dr. Lucia Mazur-Nicorici Md. PHDValerianBîcosÎncă nu există evaluări
- Coronary Artery Disease-Cad OR Ischaemic Heart Disease - IhdDocument99 paginiCoronary Artery Disease-Cad OR Ischaemic Heart Disease - IhdMwanja MosesÎncă nu există evaluări
- Coronary Artery Disease-Cad OR Ischaemic Heart Disease - IhdDocument99 paginiCoronary Artery Disease-Cad OR Ischaemic Heart Disease - IhdMwanja MosesÎncă nu există evaluări
- Oleh: Bagian Ilmu Penyakit Dalam FK Universitas Sultan Agung Semarang 2012Document40 paginiOleh: Bagian Ilmu Penyakit Dalam FK Universitas Sultan Agung Semarang 2012Mbenk NjoeÎncă nu există evaluări
- HYPERTENSIONDocument11 paginiHYPERTENSIONGargiÎncă nu există evaluări
- Diagnosis and Therapy of Artery Coronary Disease in Type 2 Diabetes MellitusDocument12 paginiDiagnosis and Therapy of Artery Coronary Disease in Type 2 Diabetes MellitusSoraya OlyfiaÎncă nu există evaluări
- Chap253-Heart Failure ManagementDocument42 paginiChap253-Heart Failure ManagementDoctor CastleÎncă nu există evaluări
- Chapter 23 Drugs For HyperlipidemiaDocument61 paginiChapter 23 Drugs For HyperlipidemiaIchsan FajriÎncă nu există evaluări
- Trans-Atlantic Inter-Society Consensus Document IIDocument52 paginiTrans-Atlantic Inter-Society Consensus Document IIAnonymous pTQIbWT2i9Încă nu există evaluări
- Unit 4 Coronary Artery Disease and Ischaemic Heart Disease: StructureDocument37 paginiUnit 4 Coronary Artery Disease and Ischaemic Heart Disease: StructurebtaleraÎncă nu există evaluări
- Increased Arterial Blood PressureDocument25 paginiIncreased Arterial Blood PressureAjmalÎncă nu există evaluări
- Applicability of Recent Dyslipidemia Guidelines in Clinical PracticeDocument4 paginiApplicability of Recent Dyslipidemia Guidelines in Clinical PracticeDokter FebyanÎncă nu există evaluări
- The MERCURY I OpenDocument12 paginiThe MERCURY I OpenSharmil IyapillaiÎncă nu există evaluări
- Clinical Management of Stable Coronary Artery Disease in Type 2 Diabetes MellitusDocument5 paginiClinical Management of Stable Coronary Artery Disease in Type 2 Diabetes MellitusAnonymous ZUaUz1wwÎncă nu există evaluări
- Overview:: (Apresoline) (Loniten)Document31 paginiOverview:: (Apresoline) (Loniten)TaikoÎncă nu există evaluări
- Approaches To Peripheral Artery Disease in DiabetesDocument18 paginiApproaches To Peripheral Artery Disease in DiabetesNabita AuliaÎncă nu există evaluări
- Prof - Dr.Medhat Ashmawy Professor of Cardiology, Tanta UniversityDocument104 paginiProf - Dr.Medhat Ashmawy Professor of Cardiology, Tanta UniversityIvana LmsÎncă nu există evaluări
- Chronic Complications of Diabetes MellitusDocument40 paginiChronic Complications of Diabetes MellitusironÎncă nu există evaluări
- Stroke UpdatedDocument36 paginiStroke UpdatedSammon TareenÎncă nu există evaluări
- Peripheral Vascular Disease - Wikipedia, The Free EncyclopediaDocument5 paginiPeripheral Vascular Disease - Wikipedia, The Free EncyclopediaDr. Mohammed AbdulWahab AlKhateebÎncă nu există evaluări
- Takayasu's Arteritis HHDocument33 paginiTakayasu's Arteritis HHusamadaifallahÎncă nu există evaluări
- تقرير ضغط الدمDocument10 paginiتقرير ضغط الدمlyh355754Încă nu există evaluări
- Nefropat Vasc Rom CursDocument40 paginiNefropat Vasc Rom CursancutazÎncă nu există evaluări
- Cardiogenik SyokDocument19 paginiCardiogenik SyokekaÎncă nu există evaluări
- Hypertension: Eu MBCHB 4 DR D M KillingoDocument73 paginiHypertension: Eu MBCHB 4 DR D M KillingoMalueth AnguiÎncă nu există evaluări
- Hypertension: Hypertension Is One of The Most Common Worldwide Diseases Afflicting Humans. BecauseDocument8 paginiHypertension: Hypertension Is One of The Most Common Worldwide Diseases Afflicting Humans. BecauseKramojÎncă nu există evaluări
- Hypertension in Geriatric PopulationDocument52 paginiHypertension in Geriatric PopulationDiana TiganucÎncă nu există evaluări
- Diabetes Mellitus Dan Hipertensi Diabetic Hypertension UPP 2015Document14 paginiDiabetes Mellitus Dan Hipertensi Diabetic Hypertension UPP 2015CANDRIAÎncă nu există evaluări
- Hypertension: Medical Management and Nutritional ApproachesDocument65 paginiHypertension: Medical Management and Nutritional ApproachesWelki VernandoÎncă nu există evaluări
- Blood Pressure Management in Patients With Diabetes: Clinical Trial Evidence For BP ControlDocument8 paginiBlood Pressure Management in Patients With Diabetes: Clinical Trial Evidence For BP ControlNovita WulandariÎncă nu există evaluări
- Peripheral Vascular DiseasesDocument23 paginiPeripheral Vascular Diseaseslectureslides22Încă nu există evaluări
- CardiologyDocument20 paginiCardiologycnnc21Încă nu există evaluări
- Medications - ADHDDocument1 paginăMedications - ADHDJonathonÎncă nu există evaluări
- Chapter 047Document13 paginiChapter 047JonathonÎncă nu există evaluări
- Chapter 34 - Introduction To The Endocrine SystemDocument11 paginiChapter 34 - Introduction To The Endocrine SystemJonathonÎncă nu există evaluări
- Chapter 25 - Muscle RelaxantsDocument12 paginiChapter 25 - Muscle Relaxantslarry blueÎncă nu există evaluări
- Chapter 39 - Introduction To The Reproductive SystemDocument13 paginiChapter 39 - Introduction To The Reproductive SystemJonathonÎncă nu există evaluări
- NCLEX Cram SheetDocument8 paginiNCLEX Cram SheetKaloy Kamao100% (5)
- The BestDocument1 paginăThe BestJonathonÎncă nu există evaluări
- Chapter 15 - Introduction To The ImmuneDocument13 paginiChapter 15 - Introduction To The ImmuneJonathonÎncă nu există evaluări
- Chapter 56 - Introduction To The Gastrointestinal SystemDocument11 paginiChapter 56 - Introduction To The Gastrointestinal SystemJonathonÎncă nu există evaluări
- Chapter 58 - Drugs Affecting Gastrointestinal MotilityDocument12 paginiChapter 58 - Drugs Affecting Gastrointestinal MotilityJonathonÎncă nu există evaluări
- Chapter 54 - Drugs Acting On The Upper Respiratory TractDocument13 paginiChapter 54 - Drugs Acting On The Upper Respiratory TractJonathonÎncă nu există evaluări
- Chapter 57 - Drugs Affecting Gastrointestinal SecretionsDocument11 paginiChapter 57 - Drugs Affecting Gastrointestinal SecretionsJonathonÎncă nu există evaluări
- Chapter 55 - Drugs Acting On The Lower Respiratory TractDocument13 paginiChapter 55 - Drugs Acting On The Lower Respiratory TractJonathonÎncă nu există evaluări
- Hyperthyroidism Care MapDocument7 paginiHyperthyroidism Care MapJonathonÎncă nu există evaluări
- Acs DXDocument2 paginiAcs DXJonathonÎncă nu există evaluări
- Chapter 59 - Antiemetic AgentsDocument11 paginiChapter 59 - Antiemetic AgentsJonathonÎncă nu există evaluări
- Illeal Conduit Care MapDocument1 paginăIlleal Conduit Care MapJonathonÎncă nu există evaluări
- Care Map UtiDocument1 paginăCare Map UtiJonathonÎncă nu există evaluări
- ECG HandoutDocument3 paginiECG HandoutJonathonÎncă nu există evaluări
- Hyperthyroidism Care MapDocument1 paginăHyperthyroidism Care MapJonathonÎncă nu există evaluări
- Incontinence Types ofDocument1 paginăIncontinence Types ofJonathonÎncă nu există evaluări
- CancerDocument5 paginiCancerJonathonÎncă nu există evaluări
- Acs DXDocument6 paginiAcs DXJonathonÎncă nu există evaluări
- Pad Vs PVD ChartDocument1 paginăPad Vs PVD ChartJonathonÎncă nu există evaluări
- Endocrine PharmDocument2 paginiEndocrine PharmfranjoyÎncă nu există evaluări
- Stages of DevelopmentDocument1 paginăStages of DevelopmentJonathonÎncă nu există evaluări
- Infection Control ChartDocument11 paginiInfection Control ChartbrittanyÎncă nu există evaluări
- Endocrine PharmDocument2 paginiEndocrine PharmJonathonÎncă nu există evaluări
- Antibiotics-AntiInfectives 2Document1 paginăAntibiotics-AntiInfectives 2JonathonÎncă nu există evaluări
- Cardiac System MedicationsDocument4 paginiCardiac System MedicationsfranjoyÎncă nu există evaluări
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDe la EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsÎncă nu există evaluări
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDe la EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisEvaluare: 4.5 din 5 stele4.5/5 (42)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDe la EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeEvaluare: 2 din 5 stele2/5 (1)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDe la EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsEvaluare: 5 din 5 stele5/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDe la EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityEvaluare: 4 din 5 stele4/5 (24)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDe la EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedEvaluare: 5 din 5 stele5/5 (80)
- The Obesity Code: Unlocking the Secrets of Weight LossDe la EverandThe Obesity Code: Unlocking the Secrets of Weight LossEvaluare: 4 din 5 stele4/5 (6)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDe la EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDe la EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsEvaluare: 4.5 din 5 stele4.5/5 (169)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDe la EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDEvaluare: 5 din 5 stele5/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDe la EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityEvaluare: 4 din 5 stele4/5 (3)
- Gut: the new and revised Sunday Times bestsellerDe la EverandGut: the new and revised Sunday Times bestsellerEvaluare: 4 din 5 stele4/5 (392)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDe la EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeEvaluare: 4.5 din 5 stele4.5/5 (253)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDe la EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsEvaluare: 3.5 din 5 stele3.5/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDe la EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisEvaluare: 3.5 din 5 stele3.5/5 (2)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningDe la EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningEvaluare: 4 din 5 stele4/5 (3)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.De la EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Evaluare: 4.5 din 5 stele4.5/5 (110)
- To Explain the World: The Discovery of Modern ScienceDe la EverandTo Explain the World: The Discovery of Modern ScienceEvaluare: 3.5 din 5 stele3.5/5 (51)
- An Autobiography of Trauma: A Healing JourneyDe la EverandAn Autobiography of Trauma: A Healing JourneyEvaluare: 5 din 5 stele5/5 (2)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDe la EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessEvaluare: 4.5 din 5 stele4.5/5 (328)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDe la EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisEvaluare: 4 din 5 stele4/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDe la EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryEvaluare: 4 din 5 stele4/5 (44)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisDe la EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisEvaluare: 4 din 5 stele4/5 (9)