Documente Academic
Documente Profesional
Documente Cultură
Card Adverse Events
Încărcat de
Danonino12Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Card Adverse Events
Încărcat de
Danonino12Drepturi de autor:
Formate disponibile
Division of Medical Education
Disclosing
Adverse
Events
Communication Skills Program
csp.medicine.dal.ca
(902) 494-6307
The PAMAP Model*
P repare
A cknowledge & Apologize
ManagetheClinicalProblem
A nalyze & Investigate
P revent
* Joan Evans, John Muir, & Heather MacLeod, (2012).
Division of Medical Education, Dalhousie University
Prepare
Gather the facts
Review the medical record and consult with others involved
Consider consulting the Canadian Medical Protective Assoc.
Set the time and place for the meeting
Meet as soon as possible after the event
Set aside protected time for a face-to-face meeting
Sit at eye level with patient and avoid barriers such as a desk
Adverse Event: any event that results in unintended harm
to the patient, and is related to care/services provided,
rather than to the patients underlying medical condition.
Harm: an outcome that negatively affects a patients
health and/or quality of life.
Consider who will be present
Ask patient who they would like to have present - ask
permission to share personal information prior to the meeting
Health care providers involved - to establish consistent
understanding of facts
Physician colleague(s) if patient will be transferred to their care
The most responsible physician at time of event has an
ethical and professional obligation to lead the discussion
and answer the patients clinical questions
Be sensitive to patient/family cultural and language needs include a professionally trained interpreter as needed
Plan what you will say
Rehearseconsider how you will explain what happened,
express your concern and regret and respond to the
patients emotional reaction
Focus on the existing facts - avoid speculation and blame
Acknowledge & Apologize
Be honest and transparent - convey a genuine desire to help
the patient
Your posture, tone of voice and demeanor all need to be
congruent with the expression of regret and empathy
Acknowledge that something unexpected has happened
- introduce the topic with words such as something has
happened and we need to talk about it
Impress upon the patient how seriously you are taking the
situation
Speak at a comfortable slow rate - repeat information as needed
Solicit the patient/familys perspective of what happened in the
event - ask them to tell you their experience in their own words
Reassure the patient/family, as appropriate, that harm did
not result from anything they did or did not do
Let the patient know you understand why she/he is upset acknowledge patients concerns and feelings (eg. frustration,
shock, anger)
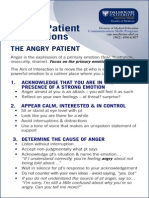
If patient reacts with anger, do not respond with
defensiveness or resentment
Express your regret/concern/sorrow as appropriate - apologize
It is critical that patients and their families not
feel abandoned by their physician after an adverse
event. Good communication at this time can restore
and even strengthen the patient-doctor relationship.
The Apology
The apology is a genuine expression of being sorry for
what has happened.
The exact words used will vary depending on the nature
of the adverse event, the nature of the harm, and the
relationship between the patient and physician
The words Im sorry should be part of any apology
Use a personal approach - use I or We
Apologize to convey regret alone, or regret with
responsibility as appropriate:
Regret Alone: Im (or were) sorry this happened to you
Regret with Responsibility: Im sorry that I (or we)
harmed you by...
In most provinces, legislation expressly prevents apologies
from being taken as an admission of legal liability.
As of 2011, provinces and territories that have apology
legislation include: AB, BC, MB, NL, NS, NU, ON, PEI, SK
Canadian Disclosure Guidelines: Being Open with Patients and
Families. Canadian Patient Safety Institute, Edmonton, AB, 2011.
Gallagher, T.H., & Lucas, M.H. (2005). Should we disclose
harmful medical errors to patients? If so, how? J Clin Outcome
Manag, 12 (5), 253-259.
The term error should be avoided in disclosure
discussions because it often misrepresents the
reason for the adverse event and implies blame and
negligence.
Manage the Clinical Problem
Find out what the patient already knows and is experiencing
- it is helpful to know if your information is consistent with
that already given by others
Describe the current clinical condition and any future care
needs
Give your recommendation as to how best to manage the
current medical condition - include alternate treatments/
investigations, risks/benefits
Be sensitive to what the patient is ready to hear - avoid
overloading the patient
Allow time and silence for the patient to reflect on
information
Respond honestly to patient questions - if you dont know
the answer to a question, tell the patient you dont know, but
that you will try to find out
Check for understanding - repeat information as needed
Analyze & Investigate What Happened
Reassure the patient that an investigation will be undertaken
(or is underway) to answer how or why the event occurred share any analysis to date
Keep the patient informed of progress (if patient wishes) arrange a follow-up meeting to discuss any new facts
Prevent Further Harm/Events
Confirm the next clinical steps such as investigations,
treatments, consultations, or a transfer of care to another
physician or facility
Explain the steps that will be taken to prevent the adverse
event from happening again - to this patient, to any patient
Make other members of the health care team aware of the
patients condition and care needs
Document the clinical care and discussions in a factual manner
Adapted from:
Communicating with your patient about harm. Disclosure of Adverse
Events. Suggestions to help CMPA members meet their patients clinical,
information and emotional needs after an adverse event. The Canadian
Medical Protective Association, 2008.
S-ar putea să vă placă și
- Breaking Bad NewsDocument25 paginiBreaking Bad Newslight tweenÎncă nu există evaluări
- Patient Assessment: by Grace MwanikiDocument48 paginiPatient Assessment: by Grace MwanikiPatience WaithiraÎncă nu există evaluări
- Difficult Patient and Dealing With Difficult PatientDocument22 paginiDifficult Patient and Dealing With Difficult Patientmhmtrgnn67Încă nu există evaluări
- Comunicação Utentes Com MedoDocument4 paginiComunicação Utentes Com MedoMafaldaPereira184Încă nu există evaluări
- SPIKES ProtocolDocument4 paginiSPIKES ProtocolKassem Gharaibeh100% (1)
- Breaking Bad NewsDocument4 paginiBreaking Bad NewsHussam KabakbjiÎncă nu există evaluări
- Breaking The Bad NewsDocument20 paginiBreaking The Bad NewsHandoyoÎncă nu există evaluări
- Counselling, Breaking Bad NewsDocument26 paginiCounselling, Breaking Bad NewsArief NorddinÎncă nu există evaluări
- Chapter 2 D-P CommunicationDocument30 paginiChapter 2 D-P CommunicationEINSTEIN2DÎncă nu există evaluări
- Plab 2 Notes Day 2Document14 paginiPlab 2 Notes Day 2Adnan Al JafaryÎncă nu există evaluări
- PAL Pack 2011 KI UpdateDocument41 paginiPAL Pack 2011 KI UpdateLuveon TangÎncă nu există evaluări
- Physician Assistant PANCE & PANRE: a QuickStudy Laminated Reference GuideDe la EverandPhysician Assistant PANCE & PANRE: a QuickStudy Laminated Reference GuideÎncă nu există evaluări
- Pom MidtermsDocument692 paginiPom MidtermsGwyneth MendozaÎncă nu există evaluări
- Give Explanation and Delivering Bad NewsDocument35 paginiGive Explanation and Delivering Bad NewsNorman AjxÎncă nu există evaluări
- Seminar 3 1Document16 paginiSeminar 3 1Maya BendelianiÎncă nu există evaluări
- Dr. Abdulmoneam Saleh Family Physician, JBFM, HSFM Dept. of Family & Community Medicine University of TabukDocument35 paginiDr. Abdulmoneam Saleh Family Physician, JBFM, HSFM Dept. of Family & Community Medicine University of TabukKholoud KholoudÎncă nu există evaluări
- Adult Physical AssessmentDocument18 paginiAdult Physical AssessmentHa HahahahahaÎncă nu există evaluări
- Interviewing and The Health HistoryDocument18 paginiInterviewing and The Health HistoryWendz BouvierÎncă nu există evaluări
- Card Explanation PlanningDocument4 paginiCard Explanation PlanningDanonino12Încă nu există evaluări
- Spikes Protocol For Breaking Bad NewsDocument25 paginiSpikes Protocol For Breaking Bad Newsumibrahim100% (2)
- Breaking Bad News MainDocument51 paginiBreaking Bad News MainGiftie AdegbosinÎncă nu există evaluări
- Dr. Ali's Uworld Notes For Step 2 CKDocument8 paginiDr. Ali's Uworld Notes For Step 2 CKnaimÎncă nu există evaluări
- (From Buckman, How To Break Bad News) : Learning ObjectivesDocument8 pagini(From Buckman, How To Break Bad News) : Learning ObjectivesEmanuel RiveroÎncă nu există evaluări
- Pedia History TakingDocument6 paginiPedia History TakingShaula de OcampoÎncă nu există evaluări
- Pemicu 2Document131 paginiPemicu 2Haha RowlingÎncă nu există evaluări
- Nta Level 4 Semester 2 Lecture Notes: Building A Therapeutic Relationship in History TakingDocument17 paginiNta Level 4 Semester 2 Lecture Notes: Building A Therapeutic Relationship in History Takingrwigema fredÎncă nu există evaluări
- Plab 2 Notes Day 2Document14 paginiPlab 2 Notes Day 2Beaulah0% (1)
- Lec3 CA Communication SkillsDocument25 paginiLec3 CA Communication Skillsoha37229Încă nu există evaluări
- Breaking Bad NewsDocument6 paginiBreaking Bad NewsAdil IslamÎncă nu există evaluări
- Comunicar Co Utentes ZangadosDocument4 paginiComunicar Co Utentes ZangadosMafaldaPereira184Încă nu există evaluări
- Anatomy AETCOM Questions and Answers SR. NO. Subtopic Competency Number Name Description Xiv Aetcom Core/ YDocument8 paginiAnatomy AETCOM Questions and Answers SR. NO. Subtopic Competency Number Name Description Xiv Aetcom Core/ YAyesha Singh100% (3)
- Consumer Protection Act (CPA / COPRA) Related To Medical ProfessionDocument3 paginiConsumer Protection Act (CPA / COPRA) Related To Medical Professionveera rajaÎncă nu există evaluări
- Counselling and Communication Skills in PediatricsDocument24 paginiCounselling and Communication Skills in PediatricsOmar HamwiÎncă nu există evaluări
- Therapeutic CommunicationDocument13 paginiTherapeutic CommunicationRainiela GloriosoÎncă nu există evaluări
- Module 2 Fundamentals of Skilled InterviewingDocument15 paginiModule 2 Fundamentals of Skilled Interviewingdarius bautistaÎncă nu există evaluări
- Foundations of Clinical Medicine-1 Summer 2014 Semester: History TakingDocument63 paginiFoundations of Clinical Medicine-1 Summer 2014 Semester: History Takingparanoea911100% (1)
- Discharge Planning 2017-InstructorDocument18 paginiDischarge Planning 2017-Instructorejeroth1991Încă nu există evaluări
- Informed ConsentDocument14 paginiInformed Consentpixisom201Încă nu există evaluări
- Liviu Oprea, MD, PHD: Associate Professor in Bioethics and Behavioural SciencesDocument44 paginiLiviu Oprea, MD, PHD: Associate Professor in Bioethics and Behavioural SciencesItdoesntMatterÎncă nu există evaluări
- AttitudeDocument10 paginiAttitudeShahbaz AAnsariÎncă nu există evaluări
- Managing Difficult PatientsDocument18 paginiManaging Difficult PatientsrakeshÎncă nu există evaluări
- Savio Case Presentation Format 2024Document156 paginiSavio Case Presentation Format 2024Jeamine Talaver PalenciaÎncă nu există evaluări
- Basic Concepts of Communication With Patient and FamilyDocument29 paginiBasic Concepts of Communication With Patient and FamilyRiska Aprilia67% (3)
- Introduction To Block Medical CommunicationDocument24 paginiIntroduction To Block Medical CommunicationAgung PramaswariÎncă nu există evaluări
- Dzinos MedicineDocument455 paginiDzinos MedicineCollen Lihaka100% (2)
- Breaking Bad News (BHP)Document3 paginiBreaking Bad News (BHP)nadiaayud100% (1)
- Doctor Patient RealationshipDocument9 paginiDoctor Patient RealationshipSara EamranÎncă nu există evaluări
- Clinical AssignmentDocument9 paginiClinical AssignmentkomalÎncă nu există evaluări
- Ics Observation and RecommendationsDocument2 paginiIcs Observation and RecommendationsVineeÎncă nu există evaluări
- Patient Education Learning NeedDocument12 paginiPatient Education Learning NeedMessayu FathasariÎncă nu există evaluări
- Accurate Diagnosis Relies Firmly On The Foundation of Accurate and Inclusive History and Competently Performed Physical ExaminationDocument28 paginiAccurate Diagnosis Relies Firmly On The Foundation of Accurate and Inclusive History and Competently Performed Physical ExaminationMalueth AnguiÎncă nu există evaluări
- Penyampaian Berita BurukDocument3 paginiPenyampaian Berita BurukBirgitta FajaraiÎncă nu există evaluări
- Legal Issues Emergency Medicine (Final)Document97 paginiLegal Issues Emergency Medicine (Final)GerardChanÎncă nu există evaluări
- 629f66541310c Clinical Methods 1Document26 pagini629f66541310c Clinical Methods 1theonlinegeekhubÎncă nu există evaluări
- Medical History Vs Nursing History & Setting The SceneDocument4 paginiMedical History Vs Nursing History & Setting The Scenemaynard baird100% (1)
- Ethical Dilemmas of Respiratory TherapistsDocument39 paginiEthical Dilemmas of Respiratory TherapistsJohn Carlo TanÎncă nu există evaluări
- Patient Pharmacist InteractionDocument25 paginiPatient Pharmacist InteractionaneecaÎncă nu există evaluări
- Doctor Patient Relationship Muk March 2021Document28 paginiDoctor Patient Relationship Muk March 2021Deborah Chemutai100% (1)
- Doctor Patient Effective Communication SkillsDocument4 paginiDoctor Patient Effective Communication SkillsAgit ZÎncă nu există evaluări
- CCLSP Study Report1Document168 paginiCCLSP Study Report1Danonino12Încă nu există evaluări
- The Influence of Controllled Motivation - Maladaptive, Buffering, or Additive EffectsDocument17 paginiThe Influence of Controllled Motivation - Maladaptive, Buffering, or Additive EffectsDanonino12Încă nu există evaluări
- Ana Are MDocument1 paginăAna Are MDanonino12Încă nu există evaluări
- New Microsoft Word DocumentDocument1 paginăNew Microsoft Word DocumentDanonino12Încă nu există evaluări
- OT24Vx16 Final ProgramDocument24 paginiOT24Vx16 Final ProgramDanonino12Încă nu există evaluări
- Specialolympics BowlingDocument131 paginiSpecialolympics BowlingDanonino12Încă nu există evaluări
- EFDS Inclusive Comms Guide Accessible PDF APRIL 2014 FINALDocument23 paginiEFDS Inclusive Comms Guide Accessible PDF APRIL 2014 FINALDanonino12Încă nu există evaluări
- Social Work LesothoDocument15 paginiSocial Work LesothoDanonino12Încă nu există evaluări
- OT24Vx16 Final ProgramDocument24 paginiOT24Vx16 Final ProgramDanonino12Încă nu există evaluări
- Physical Therapists' Nonverbal Communication Predicts Geriatric Patients' Health OutcomesDocument10 paginiPhysical Therapists' Nonverbal Communication Predicts Geriatric Patients' Health OutcomesDanonino12Încă nu există evaluări
- Card Adverse EventsDocument4 paginiCard Adverse EventsDanonino12Încă nu există evaluări
- Peer Observation of Teaching PDFDocument24 paginiPeer Observation of Teaching PDFDanonino12Încă nu există evaluări
- Card Breaking Bad NewsDocument2 paginiCard Breaking Bad NewsDanonino12Încă nu există evaluări
- Card Explanation PlanningDocument4 paginiCard Explanation PlanningDanonino12Încă nu există evaluări
- Role of Social Worker in Disability ServicesDocument2 paginiRole of Social Worker in Disability ServicesDanonino12Încă nu există evaluări
- Card Angry PatientDocument2 paginiCard Angry PatientDanonino12100% (1)
- Card Medical HistoryDocument4 paginiCard Medical HistoryDanonino12Încă nu există evaluări
- Giving Effective Feedback: To Learners & ColleaguesDocument2 paginiGiving Effective Feedback: To Learners & ColleaguesDanonino12Încă nu există evaluări
- Card Medical HistoryDocument4 paginiCard Medical HistoryDanonino12Încă nu există evaluări
- Moving TogetherDocument142 paginiMoving TogethergontrustÎncă nu există evaluări
- Aloba PocketCard BypageDocument4 paginiAloba PocketCard BypageDanonino12Încă nu există evaluări
- Card Explanation PlanningDocument4 paginiCard Explanation PlanningDanonino12Încă nu există evaluări
- Giving Effective Feedback: To Learners & ColleaguesDocument2 paginiGiving Effective Feedback: To Learners & ColleaguesDanonino12Încă nu există evaluări
- Card Angry PatientDocument2 paginiCard Angry PatientDanonino12100% (1)
- Card Breaking Bad NewsDocument2 paginiCard Breaking Bad NewsDanonino12Încă nu există evaluări
- Card Breaking Bad NewsDocument2 paginiCard Breaking Bad NewsDanonino12Încă nu există evaluări
- Card Adverse EventsDocument4 paginiCard Adverse EventsDanonino12Încă nu există evaluări
- Aloba PocketCard BypageDocument4 paginiAloba PocketCard BypageDanonino12Încă nu există evaluări