Documente Academic
Documente Profesional
Documente Cultură
DKA Canadian Protocol
Încărcat de
play_wright2084Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
DKA Canadian Protocol
Încărcat de
play_wright2084Drepturi de autor:
Formate disponibile
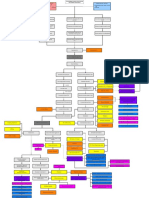
Emergency Room Management Guidelines
for the Child with Type 1 Diabetes
Diabetic Ketoacidosis (DKA)
History (some or all of)
Clinical Signs generally include
Deep sighing respirations (Kussmaul breathing)
with no wheeze or rhonchi
Smell of ketones on breath
Lethargy/drowsiness
Dehydration mild to severe
Polyuria
Polydipsia
Weight loss
Abdominal pain
Tiredness
Vomiting
Confusion
Difficulty breathing
Urine ketones/glucose
Capillary glucose STAT in ER
Venous blood glucose, gases, electrolytes, urea, creatinine
Other as indicated
Confirm DKA
Ketonuria
Glucose >11 mmol/L
pH <7.3
Hypotension (PALS Values)
Age
<1 month
1 month to 1 year
1 to 10 years
>10 years
Serum Bicarbonate <18 mmol/L
Consult Pediatrician immediately
Vascular Decompensation
Systolic BP (mm/Hg)
< or = 60
< or = 70
< or = 70 + (2 x age in years)
< or = 90
No Vascular
Decompensation
(with or without coma)
Hypotension (see box)
Decreased level of consciousness
THEN
Clinically Dehydrated
Hyperventilating
OR
Vomiting
Normal BP
(lying and sitting)
Decrease to 5 - 7 ml/kg/hr with
Potassium Chloride as noted below
Only infuse Sodium Bicarbonate
(1 - 2 mEq/kg over 1 hour) if:
1. Life-threatening hyperkalemia
2. Inotrope-resistant shock
3. Cardiac Arrest
Normal Saline
7 ml/kg over 1st hour
with Potassium Chloride
as noted below
THEN 3.5 - 5 ml/kg/hr
Oral hydration
S/C insulin
(see illness rules)
Resuscitation
Assess airway and breathing
Apply 100% oxygen by mask
Normal Saline 10 ml/kg to
expand vascular space
Minimally dehydrated
Tolerating fluids orally
Normal bowel sounds
Normal mental status
After 1st Hour of IV Fluids
If history of voiding within last hour and Potassium <5.5 mmol/L, add 40 mEq/L of Potassium Chloride to IV fluid
Aim to keep Potassium between 4 - 5 mEq/L
Continuous insulin infusion 0.1 units/kg/hr = 1ml/kg/hr (of solution of 25 units of
Regular Insulin in 250 ml Normal Saline). Include this amount in total fluid intake.
DO NOT GIVE BOLUS OF INSULIN
Continuous cardio-respiratory monitoring (with EKG tracing)
Neurological deterioration
Headache, irritability,
decreased level of consciousness,
decreased HR
First rapidly exclude hypoglycemia
by capillary blood glucose
measurement
THEN
Treat for cerebral edema
Acidosis not
improving
Acidosis improving
Blood glucose <15 mmol/L
OR
Blood glucose falls >5 mmol/L/h
after 1st hour of fluids
Change IV to D5/Normal Saline
with Potassium as above
Decrease insulin to 0.04 - 0.05 U/kg/hr =
0.4 - 0.5 ml/kg/hr of standard solution as above
Blood glucose <10mmol/L change to
D10/Normal Saline with Potassium as above
(in 3 - 4 hours)
Check insulin
delivery system
Consider sepsis
Contact Tertiary
Pediatric
Diabetes Centre
20% Mannitol 5 ml/kg over 20 minutes
If Sodium has declined, administer
2 - 4 ml/kg of 3% saline over 10 - 20 min.
THEN
Normal Saline @ maintenance IV rate
Decrease insulin to 0.04 - 0.05 U/kg/hr =
0.4 - 0.5 ml/kg/hr of standard solution as above
Contact Tertiary Pediatric Diabetes Centre
Admit to ICU
Improvement
Clinically well
Tolerating oral fluids
Ph >7.3
Bicarbonate >18mmol/L
Start S/C insulin
Stop IV insulin hour after S/C dose of rapid-acting
or 1 hour after S/C dose of regular insulin
Determine cause of DKA
Contact regional Pediatric Diabetes Education Centre
Observation and Monitoring
Hourly blood glucose (capillary)
Aim for a decrease in blood glucose of 5 mmol/L/h
Strict hourly documentation of fluids input/output
Calculate and review fluids balance at least every 4 hours
Hourly, at least, assessment of neurological status for a minimum of 24 hours
2 - 4 hours after start of IV electrolytes, venous gases then Q2-4h
Follow Effective Osmolality = (2x measured Sodium + measured blood glucose)
Avoid a decrease of >2 - 3 mmol/L/hr in effective osmolality by increasing IV sodium concentration
Emergency Room Management Guidelines
for the Child with Type 1 Diabetes
Hypoglycemia (moderate or severe)
History
Clinical Signs
Recent hypoglycemic event requiring treatment by another
person with Glucagon or oral glucose especially if
Increased confusion
Decreased consciousness
AND/
OR
Seizures
Hemiparesis
Any localizing neurological findings
Altered state of consciousness
Obtain a blood glucose (capillary)
Electrolytes and Gases not usually necessary
IF child is active, alert, and tolerating oral fluids well, then encourage
glucose-containing drinks at least at maintenance fluid rate
OTHERWISE
Start IV at least 5% glucose in saline at maintenance rate, regardless of blood glucose level
If drowsy, and any neurological impairment, localized or generalized:
IV Bolus of 0.25 - 0.5 grams/kg of 50% glucose (0.5 - 1.0 ml/kg) OR 25% glucose (1 - 2 ml/kg)
Continue IV glucose until:
1. Child has no further neurological signs and
2. Child is no longer drowsy, confused, irrational or restless.
(May take up to 12 hours if hypoglycemic encephalopathy is present)
3. Maintain blood glucose >8 mmol/L as above until IV fluids discontinued
4. Then, change to oral sugar-containing fluids
Discharge
Discharge ONLY when child is
Fully alert
Tolerating oral fluids and
Free of neurological signs.
Observation and Monitoring
Determine cause and arrange for follow-up
Decrease all insulin doses by 20% for next 24 hrs
Renew prescription for Glucagon if used
Intercurrent Illness
If emesis 2x in past 4 hours,
keep NPO for 4 - 6 hours
No emesis BUT
Not drinking
No emesis
Tolerating fluids
Capillary glucose
Venous blood glucose, gases,
urea, electrolytes
Urine ketones
Capillary glucose
Venous blood glucose, gases, electrolytes, urea
Urine ketones
IV fluids
Maintenance IV fluids
4 ml/kg/hr for 1st 10 kg
2 ml/kg/hr for next 10 kg
1 ml/kg/hr for next 10 kg
Hyperglycemic
Hypoglycemic
Do not omit insulin
Use S/C insulin unless acidotic (see DKA guidelines)
If Blood Glucose >11 mmol/L and mod-large
ketones, then give usual insulin PLUS extra short
or rapid-acting Q4h [10 - 20% of TOTAL (N&R or H)
daily dose]
Do not omit insulin
Decrease next scheduled insulin dose by 10 - 20%
If not tolerating oral fluids then follow IV
as per hypoglycemia guidelines
Otherwise encourage carbohydrate-containing fluids
Discharge
Tolerating oral fluids
No other reason for hospitalization
Replace usual meal plan with carbohydrate-containing fluids
Observation and Monitoring
Input & Output Q4h
Blood glucose Q2-4h (keep within 4 -10 mmol/L)
Test urine for ketones
Catalogue No. 013306 17,800 April/09 2009 Queens Printer for Ontario
Severely dehydrated
Normal Saline (10 ml/kg) over 1 hour
If glucose >20 mmol/L then
Normal Saline at maintenance volumes
If glucose <20 mmol/L then D5W./
Normal Saline at maintenance volumes
Once voiding, add Potassium Chloride
S-ar putea să vă placă și
- APA - DSM 5 Depression Bereavement Exclusion PDFDocument2 paginiAPA - DSM 5 Depression Bereavement Exclusion PDFDaniel NgÎncă nu există evaluări
- CASE PRESENTATION Nadhirah RahimDocument60 paginiCASE PRESENTATION Nadhirah RahimNadhirah Rahim100% (1)
- Ardra NakshatraDocument8 paginiArdra NakshatraANTHONY WRITER50% (2)
- Palliative EnciesDocument96 paginiPalliative EnciesnandanÎncă nu există evaluări
- CBT - Emergency Medicine EditedDocument14 paginiCBT - Emergency Medicine Editedchristy IÎncă nu există evaluări
- Daily Diabetes Meal Planning GuideDocument8 paginiDaily Diabetes Meal Planning GuidelilianaenÎncă nu există evaluări
- Daily Diabetes Meal Planning GuideDocument8 paginiDaily Diabetes Meal Planning GuidelilianaenÎncă nu există evaluări
- Diabetic Ketoacidosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDe la EverandDiabetic Ketoacidosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsÎncă nu există evaluări
- DM CBLDocument18 paginiDM CBLbpt2Încă nu există evaluări
- Progeny Case StudiesDocument45 paginiProgeny Case Studiesplay_wright2084Încă nu există evaluări
- Hyperosmolar Hyperglycemic Nonketotic Syndrome HHNSDocument12 paginiHyperosmolar Hyperglycemic Nonketotic Syndrome HHNSKyle Ü D. CunanersÎncă nu există evaluări
- Pink Panther - Diabetes Management - Chapter 12Document22 paginiPink Panther - Diabetes Management - Chapter 12jennmoyer100% (1)
- Diabetic Foot Case PresentationDocument58 paginiDiabetic Foot Case PresentationZH. omg sarÎncă nu există evaluări
- ACOG Abnormal Uterine Bleeding DiagnosisDocument11 paginiACOG Abnormal Uterine Bleeding DiagnosisJimmy Crack CornsÎncă nu există evaluări
- Family and Pediatric Dentistry Business PlanDocument27 paginiFamily and Pediatric Dentistry Business PlanSiti Latifah Maharani100% (1)
- Stroke EmergencyDocument56 paginiStroke EmergencyNachchakorn Dell100% (1)
- Alert Medical Series: Emergency Medicine Alert IIIDe la EverandAlert Medical Series: Emergency Medicine Alert IIIÎncă nu există evaluări
- Hypercalcemia, (High Blood Calcium) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDe la EverandHypercalcemia, (High Blood Calcium) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsÎncă nu există evaluări
- VARGA D/10 or DASAMA "MAHAT PHALAM" DASAMSA OR KARMAMSA OR SWARGAMSADocument11 paginiVARGA D/10 or DASAMA "MAHAT PHALAM" DASAMSA OR KARMAMSA OR SWARGAMSAANTHONY WRITER100% (3)
- Dka and HHSDocument25 paginiDka and HHSMouhammad Dawoud100% (2)
- Acid - Base Balance & Abg AnalysisDocument71 paginiAcid - Base Balance & Abg AnalysisMohan KrishnaÎncă nu există evaluări
- ROYAL COLLEGE - Diabetic Ketoacidosis. Update On ManagementDocument3 paginiROYAL COLLEGE - Diabetic Ketoacidosis. Update On ManagementFatos KatanolliÎncă nu există evaluări
- Alawlaqi - Obesity FinalDocument26 paginiAlawlaqi - Obesity FinalMotea Alawlaqi100% (1)
- Brain Gate ReportDocument31 paginiBrain Gate ReportRahul Bansal50% (4)
- CKD PathophysiologyDocument1 paginăCKD Pathophysiologylloyd_santino67% (3)
- Disorders of Calcium and Phosphate MetabolismDocument20 paginiDisorders of Calcium and Phosphate MetabolismAhmed Noureldin AhmedÎncă nu există evaluări
- Diabetic Ketoacidosis Management GuideDocument33 paginiDiabetic Ketoacidosis Management GuideGrace UlyÎncă nu există evaluări
- Emergency Diabetes 2023 - Septian Mixrova SebayangDocument30 paginiEmergency Diabetes 2023 - Septian Mixrova SebayangFiqri DzulfaqqorÎncă nu există evaluări
- Endocrine Emergencies CompiledDocument102 paginiEndocrine Emergencies CompiledSubhkanish RavindraÎncă nu există evaluări
- Acid-Base BalanceDocument28 paginiAcid-Base Balanceps4only100% (1)
- Journal article analyzes relationship between facial type and occlusal forcesDocument8 paginiJournal article analyzes relationship between facial type and occlusal forcesAlexandra FocaÎncă nu există evaluări
- Reading All That Jazz - Body ClockDocument4 paginiReading All That Jazz - Body ClockMehran EltÎncă nu există evaluări
- DKA, HHS and hypoglycemia guidelinesDocument30 paginiDKA, HHS and hypoglycemia guidelineskuncupcupu1368Încă nu există evaluări
- DKA Emergency Management GuideDocument18 paginiDKA Emergency Management GuideDr. Mamunul AbedinÎncă nu există evaluări
- DKA management guidelinesDocument27 paginiDKA management guidelinesjun sianÎncă nu există evaluări
- Diabetic Ketoacidosis in PaediatricDocument11 paginiDiabetic Ketoacidosis in PaediatricSana Anam JahanÎncă nu există evaluări
- Dka Vs Hhs Edit 1Document25 paginiDka Vs Hhs Edit 1Razeen RiyasatÎncă nu există evaluări
- Management of Diabetes Emergencies''Document85 paginiManagement of Diabetes Emergencies''Princewill SeiyefaÎncă nu există evaluări
- Dka GuidelineDocument16 paginiDka GuidelineGhada HusseinÎncă nu există evaluări
- Type 1 Diabetes: Diabetic Ketoacidos ISDocument16 paginiType 1 Diabetes: Diabetic Ketoacidos ISapi-551073862Încă nu există evaluări
- DKA and HHSDocument16 paginiDKA and HHSGepengCungkringÎncă nu există evaluări
- Euglycemic DkaDocument15 paginiEuglycemic DkaVemuri SrinivasÎncă nu există evaluări
- Insulin, Oral Hypoglycaemic Agents, GlucagonDocument63 paginiInsulin, Oral Hypoglycaemic Agents, GlucagonBhavesh kunvarÎncă nu există evaluări
- Diabetic Ketoacidosis (D.K.A) Beaumont Hospital Protocol: DiagnosisDocument1 paginăDiabetic Ketoacidosis (D.K.A) Beaumont Hospital Protocol: Diagnosislouglee9174100% (1)
- Euglycemic KetoacidosisDocument7 paginiEuglycemic KetoacidosisMuhammad BilalÎncă nu există evaluări
- Hypertensive Emergencies: Sulaiman Usaid G. MBCHB V Facilatator: DR Jack TDocument44 paginiHypertensive Emergencies: Sulaiman Usaid G. MBCHB V Facilatator: DR Jack TUsaid SulaimanÎncă nu există evaluări
- DKADocument12 paginiDKAAisha SyedÎncă nu există evaluări
- 3a Emergency Care DKA (UK) FINALDocument40 pagini3a Emergency Care DKA (UK) FINALDrsarfaraz SiddiquiÎncă nu există evaluări
- DKA Draft 1 AM - Drawio 2Document1 paginăDKA Draft 1 AM - Drawio 2Dud AccÎncă nu există evaluări
- Diabetic Ketoacidosis:: Evidence Based ReviewDocument4 paginiDiabetic Ketoacidosis:: Evidence Based ReviewgracedumaÎncă nu există evaluări
- Case Presentation: Andreas Crede EM RegistrarDocument15 paginiCase Presentation: Andreas Crede EM RegistrarHeru WahyudiÎncă nu există evaluări
- Dka ChartDocument2 paginiDka Chartmrsothea100% (1)
- SGLT2i Beyond Glycemic ControlDocument55 paginiSGLT2i Beyond Glycemic ControlSwapnaÎncă nu există evaluări
- Management of Diabetes Ketoacidosis in PregnancyDocument19 paginiManagement of Diabetes Ketoacidosis in PregnancySudhir PaulÎncă nu există evaluări
- Diabetic Ketoacidosis in Pregnancy: Diagnosis of DKADocument7 paginiDiabetic Ketoacidosis in Pregnancy: Diagnosis of DKA123someone123Încă nu există evaluări
- Conceptual Map - Diabetic KetoacidosisDocument2 paginiConceptual Map - Diabetic KetoacidosisLovie Japhet LopezÎncă nu există evaluări
- DkaDocument38 paginiDkaHam SotheaÎncă nu există evaluări
- Pediatric DKA: Section I: Scenario DemographicsDocument8 paginiPediatric DKA: Section I: Scenario DemographicsSherein ShalabyÎncă nu există evaluări
- Hospital Management System SoftwareDocument11 paginiHospital Management System SoftwareNikesh Solanki50% (2)
- DKA Treatment and Management GuideDocument13 paginiDKA Treatment and Management GuideMabelle Blancada ConsultaÎncă nu există evaluări
- Rash BookDocument12 paginiRash BookPhoebe UsmleÎncă nu există evaluări
- Clinical Order Set DKA AdultDocument2 paginiClinical Order Set DKA AdultBashar Al-HamaidehÎncă nu există evaluări
- Diabetic KetoacidosisDocument5 paginiDiabetic Ketoacidosislpickering33Încă nu există evaluări
- Pediatric DKA: Section I: Scenario DemographicsDocument7 paginiPediatric DKA: Section I: Scenario DemographicsSugi DenyÎncă nu există evaluări
- Diabetic Ketoacidosis and Hyperosmolar Hyperglycaemic StateDocument55 paginiDiabetic Ketoacidosis and Hyperosmolar Hyperglycaemic StateEva PrimanandaÎncă nu există evaluări
- 2020 JCI TOYP ToolkitDocument21 pagini2020 JCI TOYP ToolkitDoina LazarÎncă nu există evaluări
- 3-Diabetes Update PresentationDocument85 pagini3-Diabetes Update PresentationLucy Naomi Besitimur100% (1)
- Pratley New Treatments For Type 2 DiabetesDocument85 paginiPratley New Treatments For Type 2 DiabetesMia DangaÎncă nu există evaluări
- Endocrine and Metabolic EmergenciesDocument320 paginiEndocrine and Metabolic EmergenciesReem Ben Omran100% (1)
- Management of Acute Glomerulonephritis in Children: Children's Services Medical GuidelinesDocument7 paginiManagement of Acute Glomerulonephritis in Children: Children's Services Medical GuidelinesdaypranitaÎncă nu există evaluări
- Diabetic KetoacidosisDocument22 paginiDiabetic KetoacidosispoktaviantiÎncă nu există evaluări
- DKADocument6 paginiDKAtiffarub91% (11)
- Acute Complications of Diabetes MellitusDocument43 paginiAcute Complications of Diabetes MellitusalphaphoenixÎncă nu există evaluări
- TOLL FREE NOsDocument7 paginiTOLL FREE NOsSushil DhawaleÎncă nu există evaluări
- Skin Cancer BrochDocument8 paginiSkin Cancer Brochplay_wright2084Încă nu există evaluări
- 9780723434276Document12 pagini9780723434276Kashphia ZamanÎncă nu există evaluări
- Ann Oncol 2012 Pacini Vii110 9Document10 paginiAnn Oncol 2012 Pacini Vii110 9play_wright2084Încă nu există evaluări
- Thyroid Eye Disease - Protruding, IrritatedeyesDocument1 paginăThyroid Eye Disease - Protruding, Irritatedeyesplay_wright2084Încă nu există evaluări
- The Diagnosis and Management of Primary Hypothyroidism Revised Statement 14 June 2011 2Document4 paginiThe Diagnosis and Management of Primary Hypothyroidism Revised Statement 14 June 2011 2play_wright2084Încă nu există evaluări
- Ata Hypothyroidism BrochureDocument3 paginiAta Hypothyroidism Brochureplay_wright2084Încă nu există evaluări
- ATA DTC Guidelines 2009Document51 paginiATA DTC Guidelines 2009이호원Încă nu există evaluări
- WIC PEPB 344 ThyroidDsrdrs05 11Document5 paginiWIC PEPB 344 ThyroidDsrdrs05 11play_wright2084Încă nu există evaluări
- The Diagnosis and Management of Primary Hypothyroidism Revised Statement 14 June 2011 2Document4 paginiThe Diagnosis and Management of Primary Hypothyroidism Revised Statement 14 June 2011 2play_wright2084Încă nu există evaluări
- HypothyroidismDocument5 paginiHypothyroidismplay_wright2084Încă nu există evaluări
- Negative Effects of Cabbage - Healthy Eating - SF GateDocument5 paginiNegative Effects of Cabbage - Healthy Eating - SF Gateplay_wright2084Încă nu există evaluări
- Nutritional Management of DiabetesDocument74 paginiNutritional Management of Diabetesplay_wright2084Încă nu există evaluări
- Sleep in EpilepsyDocument8 paginiSleep in Epilepsyplay_wright2084Încă nu există evaluări
- Thyroid Function Tests - Managing Side Effects - ChemocareDocument4 paginiThyroid Function Tests - Managing Side Effects - Chemocareplay_wright2084Încă nu există evaluări
- Ashlesa NakshatraDocument8 paginiAshlesa Nakshatraplay_wright2084Încă nu există evaluări
- Epilepsy Syndromes and SleepDocument24 paginiEpilepsy Syndromes and Sleepplay_wright2084Încă nu există evaluări
- Kempenhaeghe 13 TH Epilepsy SleepDocument8 paginiKempenhaeghe 13 TH Epilepsy Sleepplay_wright20840% (1)
- APPI Guide To Health and Nutrition 2nd EditionDocument188 paginiAPPI Guide To Health and Nutrition 2nd Editionshivshekar100% (1)
- Type 2 Diabetes and DietDocument3 paginiType 2 Diabetes and Dietpratyusha201Încă nu există evaluări
- Sleep in EpilepsyDocument8 paginiSleep in Epilepsyplay_wright2084Încă nu există evaluări
- Epilepsy Syndromes and SleepDocument24 paginiEpilepsy Syndromes and Sleepplay_wright2084Încă nu există evaluări
- Final File Hypo GuidelinesDocument41 paginiFinal File Hypo Guidelinesroatfatchuri100% (1)
- Cytology PosterDocument1 paginăCytology PostermosherruÎncă nu există evaluări
- Rhopalurus Junceus: and The Treatment of CancerDocument17 paginiRhopalurus Junceus: and The Treatment of CancerAmalia Tri UtamiÎncă nu există evaluări
- Coxa PlanaDocument8 paginiCoxa PlanaLorebell100% (2)
- CS PresentationDocument38 paginiCS PresentationMarriam Malik100% (3)
- Common Child Psychiatric DisordersDocument30 paginiCommon Child Psychiatric DisordersabrihamÎncă nu există evaluări
- Surgery CssDocument13 paginiSurgery CssNaren ShanÎncă nu există evaluări
- 'NEXtCARE UAE - ASOAP FormDocument1 pagină'NEXtCARE UAE - ASOAP FormMohyee Eldin RagebÎncă nu există evaluări
- Anaphylaxis Reaction & Drug Allergy 2Document47 paginiAnaphylaxis Reaction & Drug Allergy 2telusurÎncă nu există evaluări
- Complaints Data Collection LetterDocument4 paginiComplaints Data Collection LetterthrinathÎncă nu există evaluări
- Dental and Craniomaxillofacial Implant SurgeryDocument35 paginiDental and Craniomaxillofacial Implant SurgeryJean Carlos Barbosa FerreiraÎncă nu există evaluări
- Name of The Hospital - Teaching Hospital, Karapitiya: Case 7 Puerperal PsychosisDocument13 paginiName of The Hospital - Teaching Hospital, Karapitiya: Case 7 Puerperal PsychosisCharith Rukmal KodituwakkuÎncă nu există evaluări
- Dall Miles Surgical ProtocolDocument16 paginiDall Miles Surgical Protocolfarnaz_2647334Încă nu există evaluări
- SedativesDocument3 paginiSedativesOana AndreiaÎncă nu există evaluări
- Jurnal PENDHL 1025-Article Text-1!10!20180829Document8 paginiJurnal PENDHL 1025-Article Text-1!10!20180829FZSWÎncă nu există evaluări
- Mondor's Disease of The BreastDocument8 paginiMondor's Disease of The Breast"/tmp/upload/b7ba6c5935afd58a114d8ff5e467b9faecf0fc5a60b6599e95ec2666920612624/DSC00025.JPG"Încă nu există evaluări
- Gaumard Catálogo 2014Document232 paginiGaumard Catálogo 2014renucha2010Încă nu există evaluări
- 102 WHO Guidelines On CD4 and VL For ART Doherty PDFDocument33 pagini102 WHO Guidelines On CD4 and VL For ART Doherty PDFDimar KenconoÎncă nu există evaluări
- Joyce Travelbee: Human-to-Human RelationshipDocument20 paginiJoyce Travelbee: Human-to-Human RelationshipJamesBuensalidoDellavaÎncă nu există evaluări
- A Soft-Tissue Cephalometric Analysis and Its Use in Orthodontic Treatment Planning. Part IDocument28 paginiA Soft-Tissue Cephalometric Analysis and Its Use in Orthodontic Treatment Planning. Part IJorge Ramírez100% (1)
- FCPS II Nephrology Clinical and VivaDocument2 paginiFCPS II Nephrology Clinical and Vivateena6506763Încă nu există evaluări
- Question Excerpt From 96Document5 paginiQuestion Excerpt From 96Lorainne FernandezÎncă nu există evaluări
- ICH E2E GuidelineDocument20 paginiICH E2E Guidelinetito1628Încă nu există evaluări